Abstract
Home practice is a major component of mind-body programs, yet little is known about how to optimize the amount of prescribed home practice in order to achieve an effective “dose” of practice while minimizing participant burden. This study tested how varying the amount of home practice in a mind-body program impacts compliance and stress reduction, and whether prescribing a flexible home practice schedule increases compliance. Eighty-four stressed participants undergoing a 12-week yoga program were randomized to low, medium, and high home practice conditions. The medium condition allowed participants the flexibility to choose one of two amounts of practice each day. The low practice group exhibited the highest compliance (91%) compared to the medium and low practice groups (~60%), but exhibited the lowest total practice time, and did not significantly reduce stress. The high practice group was the only group to achieve significant stress-reduction, which was maintained 12 weeks post program. Prescribing a flexible home practice schedule did not increase compliance. Results suggest that prescribing higher practice doses may maximize practice time and symptom reduction despite lower compliance.
Keywords: Mind-body, yoga, stress, home practice
1. Introduction
Yoga and meditation-based programs reduce stress and alleviate symptoms of a broad range of mental and physical ailments (Balasubramaniam, Telles, & Doraiswamy, 2013; Chiesa & Serretti, 2011). Prescribed daily home practice is commonly regarded as one of the key therapeutic elements of these programs and as essential for treatment benefit as exercise is for muscle growth (Kabat-Zinn, 1990). Home practice is often viewed within the framework of skill development which requires regular rehearsal for mastery and gaining the desired outcome (Parsons, Crane, Parsons, Fjorback, & Kuyken, 2017). Maximizing amount of home practice is thus a high priority in mind-body interventions (Crane et al., 2014). However, home practice may pose a burden on participants, and a compliance is highly variable (Parsons et al., 2017). Importantly, the relationship between amount of prescribed practice, the degree to which participants comply with their prescribed practice, and clinical outcome is currently unclear.
Many mind-body studies do not report the relationship between home practice compliance and outcome (Carmody & Baer, 2009), and those which do have found mixed results (Vettese, Toneatto, Stea, & Wang, 2009). Some studies have found that amount of home practice is correlated with stress reduction (e.g. Davis, Fleming, Bonus, & Baker, 2007; Quach, Gibler, & Mano, 2017) and other clinical outcomes (e.g. Crane et al., 2014; Grow, Collins, Harrop, & Marlatt, 2015) while other studies have not (e.g. Cadmus-Bertram et al., 2013; Davidson & Kabat-Zinn, 2004; Speed-Andrews, Stevinson, Belanger, Mirus, & Courneya, 2010). A recent meta-analysis of Mindfulness-Based interventions (Parsons et al., 2017) found substantial heterogeneity in the amount of reported home practice, with a weak (r=.26) yet statistically significant association between self-reported home practice and outcome. However, the correlational/observational approach in these studies may be severely confounded by individual differences and other factors. A randomized examination of the effects of home practice is thus needed in order to determine the specific and causal role of home practice.
A specific strategy which may improve individuals’ propensity to comply with a home practice regimen is increasing participants’ sense of autonomy and personal choice. Autonomy can predispose individuals to comply with requests and instructions (Guéguen & Pascual, 2000), and is associated with interest, a positive emotional tone, and persistence in behavioral change (Deci & Ryan, 1987). Importantly, a sense of autonomy facilitates intrinsic (“want-to” rather than “have-to”) motivation, which involves action out of personal interest, excitement, enhances performance, and promotes goal attainment (Deci, 1975; Deci & Ryan, 1987). However, to our knowledge the effects of increasing individuals’ sense of autonomy and personal choice on practice compliance has not been examined.
To disambiguate the relationships among prescribed amount of home practice, actual time spent practicing, compliance and outcome, we randomized participants enrolled in a yoga program to one of three amounts of prescribed home practice; low, medium, and high. Prescribed practice lengths were determined based on popular mind-body programs which commonly prescribe 40 minutes a day (e.g. Kabat-Zinn, 1990; Segal, Williams, & Teasdale, 2013) and other popular methods of practice such as the Headspace mobile app which rely on short 10-minute practice sessions. The practice frequency of 6 days a week was similarly chosen in order to match the frequency prescribed in other popular mind-body interventions (Bowden, Gaudry, An, & Gruzelier, 2012; Kabat-Zinn, 1990; Raghuram, Deshpande, & Nagendra, 2008; Segal, Williams, & Teasdale, 2013a). We hypothesized that the low practice group (10 minutes per day) would have higher compliance than the high practice (40 minutes a day) and medium practice groups, but lowest total practice time. To test the potential effects of autonomy on compliance, the medium practice group contained a novel element of flexibility. This group was instructed to practice 10 minutes 3 days a week and 40 minutes 3 days a week, with the autonomy to choose which days to practice each amount in a way that best fits their needs. We hypothesized that this increased autonomy and flexibility would promote the highest amount of practice.
2. Methods
2.1. Participants and Procedure
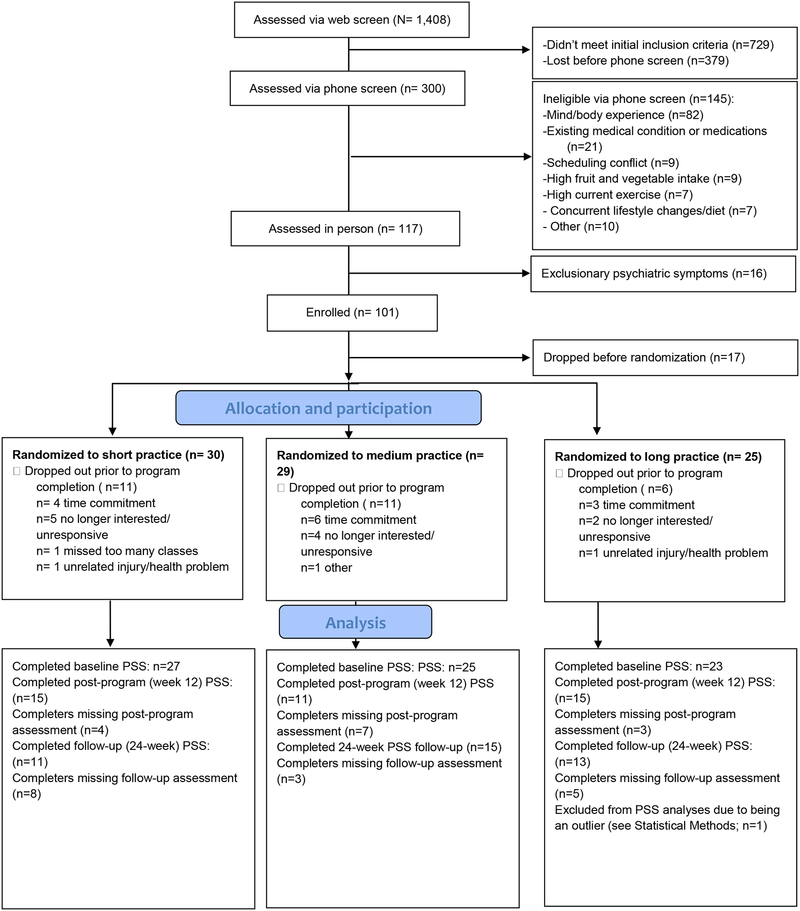
The study was part of a larger study examining the effects of yoga on health behaviors including diet and exercise, which will be reported elsewhere (Braun et al., in preparation). Recruitment began in April 2015 and follow-up assessments concluded in October 2016. Sample size was determined based on power calculations of the larger study dietary measures. Participants were recruited from two sites, the greater Boston Area and Eastern Connecticut via online advertisements for a stress reduction program, in public transit and direct mail advertisements. Potential participants completed a web survey and phone screen, followed by an in-person screening appointment where they provided written informed consent and completed the Mini International Neuropsychiatric Interview (MINI; Sheehan et al., 1997), the Eating Disorders module from the Structured Clinical Interview (SCID), and a BMI assessment. Participants had to be between the ages of 23 and 67. Exclusion criteria, implemented as part of the larger study, included an exercise regimen of more than 180 minutes per week (based on Haskell et al., 2007), daily consumption of 5 or more servings of fruits and vegetables, current diagnosis of psychiatric illness as determined by the MINI and SCID eating disorder module, significant previous meditation/yoga experience (defined as ≥12 classes in last 3 years or more than 20 classes in lifetime), medications that alter appetite, and medical conditions that would limit the ability to exercise or do yoga. Following screening, 117 volunteers gave informed consent. Eighty-four participants were randomized. Participant flow and available data are detailed in Figure 1. Participants received the program for free and were remunerated up to $100 for completing study assessments. The study protocol was approved by the Institutional Review Boards (IRB) of Massachusetts General Hospital and the University of Connecticut and monitored by Westat. The protocol is registered in Clinicaltrials.gov (NCT02098018).
Figure 1:
Participant Flow
Participants were randomized with equal allocation ratio into one of three groups (see Table 1) in blocks of 6 stratified by gender at each class site/location (Boston or Eastern Connecticut). The randomization list was generated via an algorithm on SealedEnvelope.com and imported into RedCap, where the randomization module was used to assign participants to groups. Randomization occurred after the first class in an effort to randomize participants who have shown enough commitment to show up for at least one class. Participants in the “low practice” group were instructed to practice 10 minutes a day 6 days a week, participants in the “medium” group were instructed to practice 40 min a day 3 days a week and 10 min a day 3 days a week, and participants in the “high practice” group were instructed to practice 40 minutes a day 6 days a week for the duration of the 12-week program. No differences were found between groups in age (F(2,81)=0.76,p=.47), gender (X2(2)=0.38, p=.83), race (X2(6)=1.83, p=.93), or level of education (X2(4)=1.05, p=.64; Table 1). The perceived stress questionnaire was completed using RedCap and homework logs (M=8.28, SD=3.85 for study completers) were handed to an unblinded research assistant.
Table 1.
Group characteristics
| Low practice | Medium practice | High practice | |
|---|---|---|---|
| N | 30 | 29 | 25 |
| % female | 70 | 72 | 68 |
| % male | 30 | 28 | 32 |
| Average age (SD) | 39.03 (14.81) | 36.72 (13.43) | 41.48 (14.07) |
| Race | |||
| % White | 63 | 55 | 68 |
| % Asian | 17 | 14 | 12 |
| % Black/African American | 3 | 3 | 4 |
| % Other/Mixed/Not reported | 17 | 28 | 16 |
| Education | |||
| % Some college or less | 10 | 4 | 8 |
| % 2 or 4 year college | 50 | 41 | 56 |
| % Graduate school | 40 | 55 | 36 |
2.2. Stress reduction program
The 12-week Kripalu Yoga program was comprised of two segments: 1) an 8-week manualized protocol with 2-hour weekly sessions that included 25–30 minutes of didactic content, 20–25 minutes of experiential exercises and 75–90 minutes of yoga practice, followed by 2) four weekly 90-minute yoga classes without didactic content. The 8-week protocol was created and piloted by collaborators at the Kripalu Center for Yoga and Health, and modified for use with this population by the second author, a 200-hour certified yoga therapist and 500-hour certified Kripalu yoga teacher. The two-segment intervention design was implemented to give participants theoretical and applied grounding in important yogic practices and concepts before offering standard yoga classes.
Each session of the 8-week manualized protocol comprised a didactic section including group discussion (25–30 min), an experiential section in which participants practiced specific yogic techniques (20–25 min), and a full yoga class (75–90 min). Session themes were as follows: Introduction to Kripalu Yoga (Session 1), Witness Consciousness (a concept similar to mindfulness, Session 2), Finding Your Edge (avoiding over or under-efforting, Session 3), Breathe Relax Feel Watch Allow (BRFWA; a Kripalu-based stress reduction technique), BRFWA during Yoga (Session 4) and during daily life activities (Session 5); Self-Kindness (Session 6), Body Wisdom (listening to one’s body, Session 7), and Autonomy (developing a home practice, Session 8). The remaining four weeks of classes comprised of 5–10 minutes of centering (e.g., meditation on the breath), posture warm-ups (10–20 min.), standing posture flow including sun salutations (30–40 min.), cool-down poses (10–20 min.), and final relaxation (7–10 min).
2.3. Home practice and compliance
Participants were assigned daily home practice materials corresponding to the group to which they were randomized, including videos of appropriate length (10 minutes, 40 minutes, or both) demonstrating posture flows. Home practice and compliance for each week were assessed via a written log that participants turned in at the following week’s class.
2.4. Self-reported Stress
Stress levels were assessed through the Perceived Stress Scale (PSS; Cohen, Kamarck, & Mermelstein, 1983) at baseline, 8 weeks, 12 weeks (post-program), and 24 weeks (follow-up). The PSS is a 10-item scale designed to evaluate the extent to which one perceives situations in one’s life as stressful. Participants are instructed to indicate how often they felt or thought a particular way (e.g. “In the last month, how often have you been upset because of something that happened unexpectedly?”) in the form of a number between 0–4. Higher scores indicate higher perceived stress. In the current sample the PSS had good internal consistency (Cronbach’s Alpha=.87).
2.5. Statistical Methods
To assess the effects of prescribed home practice on actual home practice and compliance, one-way Analyses of Variance (ANOVA) were used, with group (low, medium, and high practice) as the independent variable. Practice time compliance was computed by dividing participants’ average minutes of weekly home practice by their assigned home practice minutes (i.e. 60 minutes for the low practice group, 150 minutes for the medium group and 240 minutes for the high practice group). For example, a person in the low practice group who practiced 30 minutes a week on average received a compliance score of 30/60=0.5.
To assess the relationship between amount of prescribed home practice and stress reduction, a random intercept linear mixed model was used with PSS as the dependent variable to account for within-subject correlation, while also providing estimates for group, time, and their interactions. This method uses maximum likelihood methods of parameter estimation and does not require complete cases (Jennrich & Schluchter, 1986). Time was examined as a continuous or categorical predictor, and selected as categorical based on graphical examination, as well as AIC/BIC evaluation. Following evaluation of several models of correlation structure using AIC/BIC, compound symmetry was selected as optimal. Participants scoring beyond 2.5 SDs of the mean on the main outcome measures were excluded as outliers. All between-group analyses are repeated while covarying for Gender and Site (Boston or Eastern Connecticut) in order to control for their potential effects given that the randomization procedure stratified participants by these variables.
3. Results
3.1. Group differences in home practice and compliance
The ANOVA examining group differences in actual practice time (see Statistical Methods) yielded a significant effect for group (F(2,59)=11.21, p<.001, ηp2=.28, see Table 2 for means). Post-hoc contrast comparisons revealed that the high practice group practiced more than both the low practice group (F(1,59)=22.15, p<.001, ηp2=0.27) and, contrary to our hypothesis, the medium practice group (F(1,59)=9.05, p=.004, ηp2=0.13). This remained significant after adding Gender and Site (Boston or Eastern Connecticut) as covariates (F(2,57)=10.77, p<.001). A similar ANOVA conducted on average number of days practiced per week was non-significant (F(2,59)=0.01, p=.99). An ANOVA conducted on practice time compliance scores (see Statistical Methods) with group as the independent variable did not reach statistical significance (F(2,59)=2.30, p=.11). To specifically test our hypothesis that the low practice group would have the highest compliance, home practice compliance scores of the low practice group were contrasted with those of the medium and high practice groups. The low practice group showed higher compliance than the medium and high practice groups together (F(1,59)=4.48, p=.04). The medium group by itself did not significantly differ from the low practice group (F(1,59)=2.65, p=.11), or from the high practice group (F(1,59)=0.07, p=.79). Including Gender and Site as covariates yielded similar differences between the low practice group and the medium and high practice groups (F(1,57=4.54, p=.037).
Table 2.
Practice time and compliance means (SDs in parentheses)
| Low practice | Medium practice | High practice | |
|---|---|---|---|
| 60 | 150 | 240 | |
| Average weekly minutes practice | 54.85 (44.71) | 87.00 (64.43) | 151.13 (87.14) |
| Average weekly days practice | 4.04 (1.66) | 4.08 (1.88) | 4.12 (1.96) |
| Average minutes compliance | 91% (75%) | 58% (43%) | 63% (36%) |
| Average days compliance | 67% (28%) | 68% (31%) | 69% (33%) |
3.2. Prescribed home practice and perceived stress
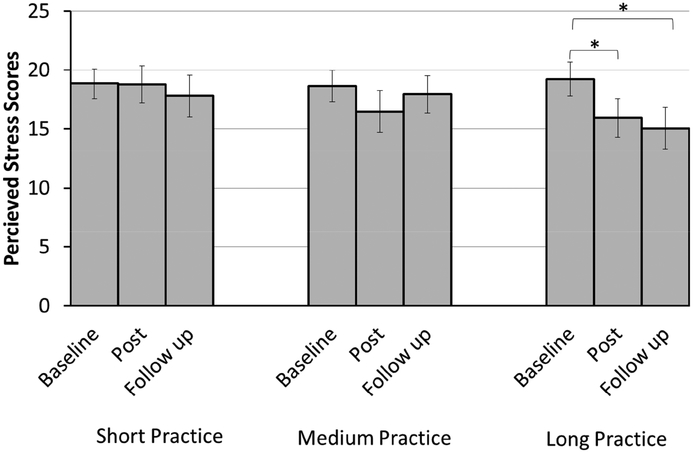
To test whether the program overall reduced stress within the linear mixed model (see Statistical Methods section), we contrasted baseline PSS scores with post-program PSS scores. The contrast was just-significant, with post-program PSS scores (M=17.13, std error=0.94) being lower than baseline scores (M=18.90, std error=0.77; t(139.901)=1.94, p=.05, Cohen’s d=0.27). The group X time interaction was non-significant (F(6,130.555)=0.73, p=.62), indicating that the effect of time on stress reduction was not significantly different across groups. To determine the minimal prescribed home practice dose effective for stress reduction, contrasts comparing baseline with post-program PSS scores for groups were conducted. Only the high practice group exhibited significant reductions in PSS scores from baseline (M=19.23, std error=1.43) to post-program (M=15.93, std error=1.64; t(131.820)=2.15, p=.03; Cohen’s d=0.38; maximal t(132.743)=1.29, p=.20) for the low and medium groups). These differences remained significant at 24 weeks, i.e.12 weeks following program completion (M=15.06, std error=1.76; t(132.554)=2.503, p=.014, Cohen’s d=0.47 for the high practice group; maximal t(138.32)=0.60, p=.55 for the low / medium groups; see Figure 2). When including Gender and Site as covariates, these pre-post (t(130.963)=2.013, p=.046) and pre-follow-up (t(131.89.)=2.384, p=.019) differences in perceived stress reduction for the high group remained significant.
Figure 2.
Self-reported stress at baseline, immediately following the program, and 12 weeks after program completion (error bars represent standard error)
4. Discussion
Despite home practice being a major component of mind-body programs, the impact of prescribed practice dose on compliance and clinical outcome remains unclear. In the current study, the low practice group had the highest rates of practice-time compliance but the lowest actual practice time, and did not significantly reduce stress. The medium and high practice groups had lower rates of compliance but greater actual practice time. Importantly, only the high practice group, who reported practicing the most, significantly reduced stress, and maintained this effect 12 weeks after program completion. These results are the first to indicate a causal link between prescribed home practice dose and symptom reduction, so that only prescribing high practice results in such clinical benefit. Furthermore, results constitute novel evidence indicating that prescribing low amounts of home practice boosts compliance, but results in lower overall practice. It may therefore be advisable in such programs to prescribe higher amounts of home practice, despite the entailed lower compliance rates, due to the increased overall practice time and significant symptom reduction.
One of the novel elements of the study was inclusion of a medium practice condition, which allowed participants the flexibility to choose days to practice 40 minutes and days to practice 10 minutes to fit their schedule. The intention was to increase participants’ sense of autonomy and personal choice. However, our hypothesis that this group would practice the most was not supported. It is possible that the increased flexibility in this condition was not sufficient to elicit an increased sense of autonomy, considering that participants were still required to choose between two home practice options based on an external referent. If so, participants’ choice may have been a controlled choice, which is associated with depletion of energy and self-control, rather than an autonomous choice which is not (see Moller, Deci, & Ryan, 2006). This, however, remains speculative given the lack of direct assessment of perceived degree of autonomy. Moreover, as this group additionally differed from the low and high group in prescribed practice time, it is uncertain whether any potential group differences can be attributed to participants’ ability to choose or the specific amount of prescribed practice time.
A significant limitation of the study is the modest sample size and relatively high drop-out rate. This results in low power, raising the possibility that additional effects were missed. The linear-mixed model analyses applied for the main findings was chosen in part to make use of all available data and minimize the effect of missing data. Additionally, amount of home practice was self-reported, which may be potentially biased or inaccurate. Our use of weekly self-report logs, nevertheless, may have minimized some retrospective report biasing and potential social desirability effects (Sylvia, Bernstein, Hubbard, Keating, & Anderson, 2014). Future studies with larger samples and other clinical outcome metrics are warranted to further support the causal link between prescribed home practice and clinical outcome in mind-body interventions.
5. Conclusion
Our preliminary results suggest that prescribing high home practice doses results in significant symptom reduction and maximizes the dose of time spent practicing. This indicates that mind-body programs may benefit from prescribing higher doses of practice despite the lower compliance. Levels of compliance are not impacted by a flexible home practice regimen.
Highlights.
Only high doses of prescribed home practice yielded significant stress reduction
These remained significant 12 weeks following completion of the mind-body program
Such benefits occurred despite lower levels of home practice compliance in this group
Prescribing a flexible home practice schedule did not increase compliance
Overall mind-body interventions may benefit from prescribing high home practice doses
Funding:
This study was funded by the National Institutes of Health (R34-AT007197 and R01-AG-048351).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest: The authors declare that they have no conflict of interest
References
- Balasubramaniam M, Telles S, & Doraiswamy PM (2013). Yoga on our minds: A systematic review of yoga for neuropsychiatric disorders. Frontiers in Psychiatry, 3, 1–16. 10.3389/fpsyt.2012.00117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowden D, Gaudry C, An SC, & Gruzelier J (2012). A comparative randomised controlled trial of the effects of brain wave vibration training, Iyengar yoga, and mindfulness on mood, well-being, and salivary cortisol. Evidence-Based Complementary and Alternative Medicine, 2012(1), 13 10.1155/2012/234713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cadmus-Bertram L, Littman AJ, Ulrich CM, Stovall R, Ceballos RM, McGregor BA, … McTiernan A (2013). Predictors of Adherence to a 26-Week Viniyoga Intervention Among Post-Treatment Breast Cancer Survivors. The Journal of Alternative and Complementary Medicine, 19(9), 751–758. 10.1089/acm.2012.0118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carmody J, & Baer RA (2009). How long does a mindfulness-based stress reduction program need to be? A review of class contact hours and effect sizes for psychological distress. Journal of Clinical Psychology. 10.1002/jclp.20555 [DOI] [PubMed] [Google Scholar]
- Chiesa A, & Serretti A (2011). Mindfulness based cognitive therapy for psychiatric disorders: A systematic review and meta-analysis. Psychiatry Research, 187(3), 441–453. [DOI] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, & Mermelstein R (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24(4), 385–396. [PubMed] [Google Scholar]
- Crane C, Crane RS, Eames C, Fennell MJV, Silverton S, Williams JMG, & Barnhofer T (2014). The effects of amount of home meditation practice in Mindfulness Based Cognitive Therapy on hazard of relapse to depression in the Staying Well after Depression Trial. Behaviour Research and Therapy, 63, 17–24. 10.1016/j.brat.2014.08.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson RJ, & Kabat-Zinn J (2004). Alterations in brain and immune function produced by mindfulness meditation. Psychosomatic Medicine, 66(1), 149–152. 10.1097/00006842-200401000-00023 [DOI] [PubMed] [Google Scholar]
- Davis JM, Fleming MF, Bonus KA, & Baker TB (2007). A pilot study on mindfulness based stress reduction for smokers. BMC Complementary and Alternative Medicine, 7, 1–7. 10.1186/1472-6882-7-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deci EL (1975). Intrinsic motivation. New York: Plenum Press. [Google Scholar]
- Deci EL, & Ryan RM (1987). The support of autonomy and the control of behavior. Journal of Personality and Social Psychology, 53(6), 1024–1037. 10.1037/0022-3514.53.6.1024 [DOI] [PubMed] [Google Scholar]
- Grow JC, Collins SE, Harrop EN, & Marlatt GA (2015). Addictive Behaviors Enactment of home practice following mindfulness-based relapse prevention and its association with substance-use outcomes. Addictive Behaviors, 40, 16–20. 10.1016/j.addbeh.2014.07.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guéguen N, & Pascual A (2000). Evocation of freedom and compliance: The "but you are free of…" technique. Current Research in Social Psychology, 5(18), 1–7. [Google Scholar]
- Haskell WL, Lee IM, Pate RR, Powell KE, Blair SN, Franklin BA, … Bauman A (2007). Physical activity and public health: Updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Medicine and Science in Sports and Exercise, 39(8), 1423–1434. 10.1249/mss.0b013e3180616b27 [DOI] [PubMed] [Google Scholar]
- Jennrich RI, & Schluchter MD (1986). Unbalanced repeated-measures models with structured covariance matrices. Biometrics, 42(4), 805–820. 10.2307/2530695 [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J (1990). Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain, and Illness. New York: Delta Trade. [Google Scholar]
- Moller AC, Deci EL, & Ryan RM (2006). Choice and Ego-Depletion : The Moderating Role of Autonomy Choice and Ego-Depletion : The Moderating Role of Autonomy. Personality and Social Psychology Bulletin, 32(8), 1024–1036. 10.1177/0146167206288008 [DOI] [PubMed] [Google Scholar]
- Parsons CE, Crane C, Parsons LJ, Fjorback LO, & Kuyken W (2017). Home practice in Mindfulness-Based Cognitive Therapy and Mindfulness-Based Stress Reduction: A systematic review and meta-analysis of participants’ mindfulness practice and its association with outcomes. Behaviour Research and Therapy, 95, 29–41. 10.1016/j.brat.2017.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quach D, Gibler RC, & Mano KEJ (2017). Does Home Practice Compliance Make a Difference in the Effectiveness of Mindfulness Interventions for Adolescents ? Mindfulness, 8, 495–504. 10.1007/s12671-016-0624-7 [DOI] [Google Scholar]
- Raghuram N, Deshpande S, & Nagendra H (2008). A randomized control trial of the effect of yoga on verbal aggressiveness in normal healthy volunteers. International Journal of Yoga, 1(2), 76 10.4103/0973-6131.41034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segal ZV, Williams JMG, & Teasdale JD (2013a). Mindfulness-based cognitive therapy for depression (2nd ed.). New York: Guilford Press. [Google Scholar]
- Segal ZV, Williams JMG, & Teasdale JD (2013b). Mindfulness-Based Cognitive Therapy for Depression. Guilford Press. [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Janavs J, Weiller E, Keskiner A, … Dunbar GC (1997). The validity of the Mini International Neuropsychiatric Interview (MINI) according to the SCID-P and its reliability. European Psychiatry, 12(5), 232–241. 10.1016/S0924-9338(97)83297-X [DOI] [Google Scholar]
- Speed-Andrews AE, Stevinson C, Belanger LJ, Mirus JJ, & Courneya KS (2010). Pilot Evaluation of an Iyengar Yoga Program for Breast Cancer Survivors. Cancer Nursing, 33(5), 369–381. 10.1097/NCC.0b013e3181cfb55a [DOI] [PubMed] [Google Scholar]
- Sylvia LG, Bernstein EE, Hubbard JL, Keating L, & Anderson EJ (2014). Practical guide to measuring physical activity. Journal of the Academy of Nutrition and Dietetics, 114(2), 199–208. 10.1016/j.jand.2013.09.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vettese LC, Toneatto T, Stea JN, & Wang JJ (2009). Do Mindfulness Meditation Participants Do Their Homework ? And Does It Make a Difference ? A Review of the Empirical Evidence. Journal of Cognitive Psychotherapy, 23(3), 198–225. 10.1891/0889-8391.23.3.198 [DOI] [Google Scholar]