Abstract
Amyloid-β (Aβ) has been closely implicated in the pathogenesis of cerebral amyloid angiopathy (CAA) and Alzheimer’s disease (AD), the major causes of dementia. Thus, Aβ could be a target for the treatment of these diseases, for which, currently, there are no established effective treatments. Taxifolin is a bioactive catechol-type flavonoid present in various plants, such as herbs, and it exhibits pleiotropic effects including anti-oxidant and anti-glycation activities. Recently, we have demonstrated that taxifolin inhibits Aβ fibril formation in vitro and have further shown that it improves cerebral blood flow, facilitating Aβ clearance in the brain and suppressing cognitive decline in a mouse model of CAA. These findings suggest the novel therapeutic potentials of taxifolin for CAA. Furthermore, recent extensive studies have reported several novel aspects of taxifolin supporting its potential as a therapeutic drug for AD and metabolic diseases with a high risk for dementia as well as for CAA. In this review, we have summarized the recent advances in taxifolin research based on in vitro, in vivo, and in silico approaches. Furthermore, we have discussed future research directions on the potential of taxifolin for use in novel therapeutic strategies for CAA, AD, and metabolic diseases with an increased risk for dementia.
Keywords: cerebral amyloid angiopathy, Alzheimer’s disease, amyloid-β fibril formation, taxifolin
1. Introduction
Cerebral amyloid angiopathy (CAA), pathologically characterized by the deposition of amyloid-β (Aβ) within small cerebral arteries, is a major cause of cerebrovascular diseases. Approximately 40% of intracerebral hemorrhage (ICH) cases are associated with moderate or severe CAA in the UK [1]. Currently, there are no established treatments for CAA [2]. Despite great advances in ischemic stroke care, long-term prognosis of ICH remains a cause for concern [3].
We have recently reported that taxifolin, a catechol-type flavonoid with strong anti-oxidant and anti-glycation activities, inhibits Aβ aggregation, thus reducing cerebrovascular Aβ accumulation. This review mainly focuses on the potential of taxifolin as a novel treatment for CAA and other diseases.
2. Cerebral Amyloid Angiopathy
2.1. Overlapped Pathophysiologies Between Cerebral Amyloid Angiopathy and Alzheimer’s Disease
Aβ accumulates in the cerebral vessel walls, causing smooth muscle cell degeneration, vessel wall thickening, luminal narrowing, and concentric wall splitting (double barreling) [4]. These vascular pathologies are hallmarks of CAA and cause variable degrees of cerebral hemorrhage. In addition to symptomatic intracranial hemorrhage, asymptomatic cerebral microbleeds (CMBs) and superficial siderosis are frequently found on T2* gradient-recalled echo or susceptibility-weighted magnetic resonance imaging [5,6]. Lobar, but not deep, CMBs are especially related to cerebrovascular Aβ accumulation. Thus, multiple, strictly lobar CMBs could be a useful marker for the diagnosis of CAA [7]. CAA also induces ischemic strokes. In addition to macroinfarcts [8], cerebral microinfarctions (CMIs) are associated with cognitive impairment [9]. Reportedly, patients with CAA have a greater number of CMIs than controls [10], and the number occasionally exceeds 1000 [11].
CAA plays a pivotal role in the pathogenesis of dementia. CAA is extremely common in sporadic Alzheimer’s disease (AD) [12], suggesting a strong, bidirectional relationship between AD and CAA. Furthermore, CAA increases the odds of AD and is associated with increased cognitive decline [13]. Cognitive changes are likely to be associated with CAA-related pathologies such as cerebral hemorrhage and infarcts. Therefore, preventing cerebrovascular amyloidosis is believed to be a novel therapeutic approach not only for CAA but also for dementia.
2.2. Strategies to Tackle Cerebral Amyloid Angiopathy
Overproduction of Aβ or failure to eliminate it results in its accumulation; several investigations regarding sporadic AD and CAA have shown that the latter is critical [14,15], suggesting that promoting Aβ clearance would be a therapeutic approach for CAA [16]. The necessity of promoting Aβ clearance has been demonstrated in a clinical trial of Aβ immunization. In AN-1792-vaccinated AD patients, parenchymal Aβ plaques diminished, and cerebrovascular Aβ accumulation and CAA deteriorated [17,18]; this may be explained by the excessive antibody-solubilized senile plaque Aβ that is redeposited in the cerebral vasculature [19,20]. Aβ distribution in CAA as well as vaccinated AD cases closely corresponds to the intramural periarterial drainage (IPAD) route, which is one of the major systems related to Aβ elimination [21]. The IPAD route is also termed perivascular lymphatic drainage [22]. Interstitial fluid (ISF) and solutes including Aβ are believed to be cleared from the gray matter through the IPAD route, which is a space between two basement membranes in the walls of the cerebral capillaries and arteries [23,24]. IPAD has been shown to be impaired in the aging mouse brain and in the presence of CAA [25]. Furthermore, we have previously demonstrated that cilostazol, a selective inhibitor of type-3 phosphodiesterase, promotes IPAD, resulting in the maintenance of vascular integrity, amelioration of Aβ deposits, and prevention of cognitive decline [26]. Promotion of IPAD is now considered as a promising strategy to treat CAA.
Inhibiting Aβ assembly would be another potential approach to treat CAA as well as AD. The Aβ protein is secreted from an Aβ precursor protein (APP) through sequential proteolytic processing by β- and γ-secretases [27]. There are two major forms of Aβ: Aβ40 and Aβ42; Aβ42 is more neurotoxic because of its higher hydrophobicity, which subsequently results in faster aggregation. Aβ42 accumulation is marked in parenchymal senile plaques in AD brains, whereas Aβ40 accumulation is abundant in CAA and is closely related to cerebrovascular dysfunction [28,29,30]. Both Aβ molecules are generated in neurons as a monomer [31] and then aggregate to form oligomers, protofibrils, and fibrils through intermolecular β-sheet formation, thereby exhibiting various degrees of toxicity [32]. Aβ fibril formation is mediated by a nuclear-dependent polymerization process, which comprises nuclear and elongation phases [33,34,35].
Importantly, not only insoluble Aβ fibrils but also soluble Aβ including oligomers and protofibrils can induce neuronal and cerebrovascular injuries. Cerebrovascular dysfunction has been observed even before the appearance of insoluble Aβ accumulation around vessels in rodent models [36,37], which suggests that soluble Aβ is likely to impair cerebrovascular integrity and cognitive function in early stages of AD [37,38,39]. Therefore, the prevention of Aβ aggregation, especially in the early phase of CAA, is needed.
3. Therapeutic Potentials of Taxifolin for Cerebral Amyloid Angiopathy and Alzheimer’s Disease
3.1. Therapeutic Effects of Taxifolin on Cerebral Amyloid Angiopathy
Despite studies demonstrating pathological roles of Aβ in CAA, no effective treatments for CAA have been established. However, accumulating evidence has suggested the emerging effectiveness of taxifolin as a potential agent in the prevention and treatment of Aβ-associated cognitive dysfunction. Historically, oxidative stress has been reportedly closely implicated in the pathogenesis of age-related cognitive dysfunction, because the rate of oxidative metabolism is higher in the central nervous system than that in other tissues, and oxidative damage in the brain progresses with aging [40]. Furthermore, Aβ is also involved in the production of reactive oxygen species and causes neuronal dysfunction [33]. Therefore, dietary intervention with antioxidants has been expected to alleviate oxidative damage in the brain [40], thereby leading to reduced risk of cognitive dysfunction. Based on this possibility, extensive studies extracted a diverse array of compounds from various plants, characterized them, and addressed the potential neuroprotective effects of various antioxidants. During the course of these researches, taxifolin, a bioactive constituent of various plants, including onions, milk thistle, French maritime bark, and Douglas fir bark [41,42], was found and has become a topic of a great interest as a potential novel therapeutic target. Its biochemical and safety profiles have already been established [43,44]. Taxifolin is known to possess multiple pharmacological actions, such as anti-oxidation, advanced glycation end products (AGE) formation suppression, and mitochondrial protection, and has received increasing attention because of its potential efficacy in the treatment of various diseases including malignancies, cardiovascular diseases, chronic hepatitis, hyperlipidemia, and neurocognitive disorders [45].
We have recently addressed the potential therapeutic effects of taxifolin using in vitro and in vivo approaches and provided the first evidence delineating the novel beneficial effects of taxifolin on CAA [45]. The thioflavin T fluorescence assay and transmission electron microscopy imaging performed by us revealed that the addition of taxifolin to an Aβ40 solution significantly inhibited the aggregation of Aβ40 in vitro, indicating a novel suppressive effect of taxifolin on Aβ40 fibril formation [45]. Furthermore, we investigated the inhibitory effects of taxifolin on Aβ40 fibril formation in vivo using a mouse model of CAA, which expresses the human APP gene with Swedish/Dutch/Iowa triple mutations in neurons and also exhibits vasculotropic dominant accumulations of Aβ40 with respect to Aβ42 [45,46]. Quantitative analyses using filter trap assay and enzyme-linked immunosorbent assay showed that the cerebral levels of Aβ oligomers were decreased in the taxifolin group mice, which were fed taxifolin-containing chow, compared with the control group mice, which were fed standard chow. Therefore, these findings indicate that orally administered taxifolin has a novel preventive effect on Aβ40 fibril formation in the brains of CAA model mice [45].
We further addressed the effects of taxifolin on the pathogenesis of CAA using these mice [45]. The elimination half-life of taxifolin was found to be less than 1 h; thus, only a relatively small amount of taxifolin could pass the blood–brain barrier. Experiments to assess spatial learning and reference memory revealed that taxifolin significantly suppressed cognitive impairment in these mice compared with controls. As expected from taxifolin’s inhibitory effects on Aβ40 fibril formation, immunohistochemical analysis showed that it reduced the cerebrovascular accumulation of Aβ40 in CAA model mice compared with controls. Furthermore, laser speckle flowmetry indicated that taxifolin significantly restored the reduced cerebral blood flow in CAA model mice. Notably, in conjunction with the reduced cerebral Aβ oligomer levels and improved cerebral blood flow, blood Aβ40 levels were elevated in the taxifolin group mice compared with controls, suggesting that taxifolin facilitated the clearance of Aβ40 from the brain into systemic circulation; this would lead to a neuroprotective effect, contributing to cognitive impairment prevention [45].
3.2. Inhibitory Effects of Taxifolin on Amyloid-β42 Fibril Formation
Regarding Aβ42 fibril formation, which is closely implicated in AD pathogenesis, a previous meticulous study analyzed the effects of taxifolin on Aβ42 aggregation and β-sheet formation using wild-type Aβ42 or mutant Aβ42 carrying substituted amino acids [34]. The results demonstrated a novel mechanism of action of taxifolin in the inhibition of Aβ42 aggregation. The mechanism is related to the chemical structure of taxifolin: a catechol-type flavonoid, which possesses 3′,4′-dihydroxyl groups on the B-ring [34]. The catechol structure of taxifolin first autoxidizes and then forms o-quinone on the B-ring. This oxidized form, in turn, reacts with Aβ42 by targeting Lys16 and/or Lys28 of Aβ42, resulting in the production of Aβ42–taxifolin adducts. Importantly, Lys16 and Lys28 are located in the intermolecular β-sheet region of Aβ42. Therefore, the Aβ42–taxifolin adduct formation contributes to the inhibition as well as to the destabilization of Aβ42 aggregation, suppressing the elongation phase rather than the nucleation phase in the process of Aβ42 fibril formation [34].
3.3. Suppressive Effects of Taxifolin on Neuronal Amyloid-β Production
In addition to the biochemical properties of taxifolin that play a role in suppressing Aβ42 fibril formation, it is of importance to discuss the physiological significance of taxifolin in the prevention and/or treatment of cognitive impairment. Sequential cleavage of APP by secretases generates Aβ; the rate-limiting step in this process is the cleavage by β-site secretase enzyme (BACE1) [47,48,49]. As the expression levels and activity of BACE1 are elevated in the brains of AD patients [50,51], there is a possibility that Aβ production and fibril formation are enhanced in these patients. Several studies have addressed the underlying mechanisms regulating BACE1 gene expression [48,52,53]. Aβ42 induces the activation of JAK2 signaling pathway, which then mediates the activation of STAT3 signaling pathway [48]. The elevated STAT3 signaling, in turn, activates NF-κB signaling, which enhances the promoter activity of BACE1, thereby upregulating BACE1 transcription [48,52,53]. These signaling cascades promote amyloidogenesis, leading to neuronal injury and cognitive dysfunction.
To address the physiological significance of taxifolin in the suppression of cognitive decline, a study examined whether taxifolin is involved in attenuating signaling pathways for BACE1 expression using a mouse neuroblastoma N2a Swe cell line [48]. This cell line carries a human APP Swedish mutation and, when activated, the cells overexpress the gene, producing Aβ. Biochemical and immunocytochemical analyses revealed that the addition of taxifolin to the in vitro culture of these cells upregulated both the expression and the activity levels of SIRT1 [48], a deacetylase involved in the growth, differentiation, and survival of neurons [54]. Furthermore, the taxifolin-stimulated SIRT1 pathway reduced the activation of STAT3 signaling pathway, thereby downregulating BACE1 expression [48]. Together, these studies suggest novel functions of taxifolin besides the prevention of Aβ42 aggregation: taxifolin exhibits suppressive effects on neuronal Aβ production and subsequent Aβ fibril formation through reduction of BACE1 levels by stimulating SIRT1-mediated inhibition of STAT3 signaling pathway. Notably, the authors further demonstrated that cilostazol also exhibits beneficial effects on N2a cells, as observed with taxifolin treatment, by activating the SIRT1 pathway, alleviating the STAT3 pathway, downregulating BACE1 expression, and reducing Aβ production [48]. In particular, their finding that concurrent treatment with taxifolin and cilostazol results in synergistic suppressive effects on Aβ production and on neuronal cell death suggests novel potential therapeutic strategies for CAA as well as AD. In addition, the SIRT1 pathway stimulated by taxifolin and cilostazol might contribute to neurogenesis and cognitive function by potentially upregulating neuroprotective factors such as brain-derived neurotrophic factor [54].
3.4. Potential Therapeutic Effects of Taxifolin on Alzheimer’s Disease
Inflammation in the brain has been highly implicated in the pathogenesis of AD through the acceleration of amyloidosis [55] and neuronal cell death [48,56]. Studies have reported that in neurons, the activation of a proinflammatory mediator cytosolic phospholipase A2 (cPLA2) contributes to age-associated cognitive impairment [57] as well as AD pathogenesis [58,59]. Aβ42 can activate cPLA2 [60,61], which is responsible for the main enzymatic process of metabolizing arachidonic acid; this ultimately results in the production of prostaglandin E2 (PGE2), which is a neuroinflammatory molecule [42,61,62]. Both cPLA2 and PGE2 have been reported to cause synapse damage [63].
A recent study has investigated the effects of taxifolin on cPLA2-related inflammatory pathway and Aβ-induced neurotoxicity using the human neuroblastoma SH-SY5Y cell line and mouse primary hippocampal neurons [42]. Biochemical analysis revealed that the in vitro treatment of neurons with Aβ42 resulted in elevated levels of both cPLA2 and PGE2. Furthermore, live cell imaging showed that incubation with Aβ42 inhibited the formation of neuronal dendritic filopodia and dendritic spines. In contrast, the addition of taxifolin to these cultures seemed to combat Aβ42-induced neurotoxicity; taxifolin significantly prevented the increase in cPLA2 and PGE2 levels as well as the inhibition of dendritic filopodia and dendritic spines formation in neurons incubated with Aβ42. These data suggest that taxifolin exhibits neuroprotective effects besides its suppressive effects on Aβ production through the downregulation of BACE1 expression [48].
Using a mouse model of AD based on the hippocampal injection of Aβ42, the authors further examined the effects of intraperitoneal administration of taxifolin on the levels of cPLA2 and of the synaptic marker post-synaptic density protein-95 (PSD-95) and on cognitive function [42]. In line with the findings of the in vitro experiments, taxifolin suppressed the increase in cPLA2 and PGE2 levels in the hippocampus in Aβ42-injected mice. Moreover, Aβ42 injection reduced PSD-95 levels in the hippocampus, but taxifolin treatment significantly suppressed these reductions. Furthermore, animal experiments designed to test recognition and spatial memories reported that Aβ42-injected mice exhibited deficits in cognitive function, whereas taxifolin treatment improved this cognitive impairment. These results suggest that taxifolin exhibits suppressive effects on cognitive impairment in the preclinical settings of AD, potentially through pleiotropic functions including inhibition of Aβ42 fibril formation [34], suppression of Aβ42 production [48], and/or alleviation of Aβ42-induced neurotoxicity [42].
4. Therapeutic Potentials of Taxifolin for Metabolic Diseases with A High Risk for Neurodegenerative Diseases
4.1. Effects of Taxifolin on Diabetes
Epidemiological studies have reported diabetes to be a high-risk factor for dementia, including AD and vascular dementia [64,65,66]. Potential mechanisms underlying diabetes-related dementia include multifactorial pathways such as Aβ accumulation, neuroinflammation, small vessel infarcts, and neurodegeneration in the brain [64,65,66,67,68]. Accordingly, prevention and treatment of diabetes is critical to reduce the risk of development and progression of dementia.
Detailed findings regarding the effects of taxifolin on diabetes are limited, but a recent study has demonstrated the anti-diabetic effects of taxifolin and its mechanisms of action through in vivo and in silico approaches [69]. The authors used a rat model of diabetes in which pancreatic β-cells were depleted by intraperitoneal injection of alloxan. They found that taxifolin administration via an intragastric route significantly reduced blood glucose levels in the diabetic rats compared with controls (without taxifolin). To elucidate the underlying mechanisms of the hypoglycemic effects of taxifolin, the authors next examined the effects of taxifolin on α-amylase, a carbohydrate-metabolizing enzyme that elevates blood glucose levels; inhibition of α-amylase is effective in the treatment of diabetes [69,70]. Taxifolin treatment significantly reduced serum amylase activity in diabetic rats compared with controls, consistent with its glucose-lowering effects. These studies suggest that taxifolin exhibits hypoglycemic effects through the reduction of α-amylase activity in diabetic rats [69].
The authors further addressed the potential direct action of taxifolin on α-amylase with computational and docking studies, comprising ligand–receptor docking studies, free-energy calculations, and molecular dynamics simulations [69]. In the flexible docking simulations, the authors selected the bioinformatically determined best-docked poses of the taxifolin–α-amylase complex and analyzed the binding modes of taxifolin with α-amylase. The analysis revealed that taxifolin interacts with the residues Trp59, Tyr62, Glu233, and Asp300 present at the active site of α-amylase through a π–π interaction with the benzene rings of Trp59 and Tyr62 and an H-bond interaction with Glu233 and Asp300. In addition, using a molecular mechanics-based scoring method for binding free-energy calculation, the authors showed that van der Waals and nonpolar solvation-free energies also contribute to the binding affinity of taxifolin for α-amylase. Furthermore, the authors examined the dynamic behavior of the taxifolin–α-amylase complex through molecular dynamics simulations, considering the potential effects of solvent, temperature, and pressure on the complex formation, and confirmed the stable conformation of taxifolin at the active site of α-amylase. Accordingly, these in vivo and in silico findings indicate that taxifolin binds to the active site of α-amylase and inhibits its activity, thus leading to improvement of hyperglycemia [69].
4.2. Effects of Taxifolin on Diabetic Nephropathy
Diabetic nephropathy is a serious diabetic complication [71], and chronic kidney diseases (CKDs) are epidemiologically a high-risk factor for dementia [72,73,74]. Reportedly, in a mouse model of CKD, chronic renal dysfunction resulted in elevated oxidative stress levels in the brain, leading to cognitive impairment [75]. Thus, the prevention and improvement of CKDs would contribute to reduce the dementia risk.
Recent studies have reported the novel renal protective effects of taxifolin using a rat model of diabetes, which was developed through pancreatic β-cell depletion with an intraperitoneal streptozotocin injection [71,76]. Taxifolin treatment significantly improved the renal function profiles in diabetic rats compared with controls, in parallel with improved glucose metabolism [71,76]. Consistent with these results, further histological analyses revealed that taxifolin suppressed necrotic cell death in the renal tissue [76] and alleviated renal fibrosis by inhibiting extracellular matrix accumulation and mesangial matrix expansion [71]. Furthermore, biochemical analyses showed that taxifolin reduced the activation of high-glucose-stimulated proinflammatory pathways in rat and human kidney cell lines [71] as well as in renal tissue from diabetic rats [76]. Taxifolin also reduced the levels of reactive oxygen species produced by these kidney cell lines, which were stimulated with high glucose [71]. These findings indicate the potential renal protective effects of taxifolin in diabetic conditions, further supporting its potential beneficial effects on dementia.
4.3. Effects of Taxifolin on Obesity
Obesity has been implicated in the development of dementia in later life [77]; however, a recent study has reported an inverse association between body mass index and dementia incidence [78]. Thus, the potential effect of obesity on dementia incidence remains controversial. Obesity is a high-risk factor for diabetes, cardiovascular diseases, and CKDs [79], which, in turn, are risk factors for dementia [64,65,66,72,73,74,80]. Therefore, improvement in obesity would be beneficial for reducing dementia risk.
Recent reports have demonstrated novel roles of taxifolin in improving obesity [81,82]. The authors analyzed the effects of orally administered taxifolin on a rat model of diet-induced obesity (high-fat diet). The taxifolin group showed significant reductions in body weight and serum cholesterol and triglycerides levels compared with the controls (without taxifolin treatment) [81]. Taxifolin also improved hyperglycemia and insulin resistance as well as oxidative stress levels [82]. Furthermore, it elevated gene expression levels of mitochondrial uncoupling protein-1 and carnitine palmitoyltransferase I, markers for fat oxidation and energy expenditure of the energy-consuming brown adipose tissue [82]. Together, these findings suggest a novel anti-obesity effect of taxifolin, potentially mediated through an improvement of glucose and lipid metabolism as well as of energy homeostasis [81,82], although the mechanistic details underlying these effects remain to be elucidated.
5. Future Perspectives
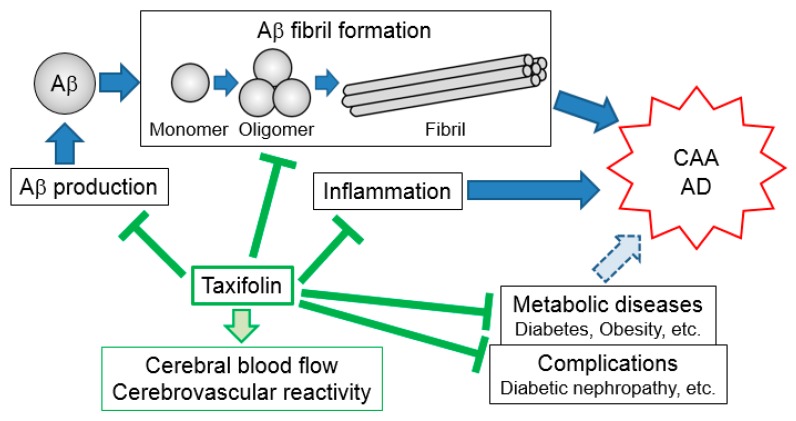
Aβ fibril formation plays pathological roles in neuronal injury. In particular, Aβ40 and Aβ42 aggregates are mainly implicated in the pathogenesis of CAA and AD, respectively. Recent advances in taxifolin research have provided novel insights into its pleiotropic beneficial actions, which include inhibition of Aβ fibril formation [34,45], suppression of Aβ production [48], and facilitation of Aβ clearance [45], contributing to the suppression of the development and progression of Aβ-associated cognitive dysfunction. Furthermore, taxifolin has been shown to improve metabolic diseases with a high risk for neurodegenerative diseases and their complications [69,71,76,81,82]. These findings suggest that taxifolin is a key molecule in the prevention and treatment of cognitive dysfunction as well as metabolic diseases with an increased risk for neurodegenerative diseases (Figure 1, Table 1).
Figure 1.
Pleiotropic beneficial effects of taxifolin. Taxifolin suppresses Aβ production, fibril formation, and neuroinflammation in the brain. It also ameliorates cerebrovascular dysfunction. Furthermore, taxifolin beneficially affects certain metabolic diseases with a high risk for neurodegenerative diseases and their complications. These direct and indirect effects of taxifolin would contribute to preventing and/or treating Aβ-associated cognitive dysfunction including CAA and AD. Aβ: amyloid-β; CAA: cerebral amyloid angiopathy; AD: Alzheimer’s disease.
Table 1.
Favorable effects of taxifolin on AD and CAA.
| Pharmacological Effects | Targets | Mechanisms |
|---|---|---|
| Suppressing Aβ production | Neuron | Reduction of BACE1 levels |
| Inhibiting Aβ aggregation | Lys residues of Aβ | Aβ–taxifolin adduct formation |
| Anti-inflammation | Neuron | Reduction of cPLA2 and PGE2 levels |
| Increasing CBF and CVR | Vascular endothelial and/or mural cells | Amelioration of Aβ toxicity Anti-oxidation Anti-glycation |
| Reducing hyperglycemia | α-amylase | Taxifolin–α-amylase complex |
| Reducing body weight | Brown adipose tissue | Increased energy expenditure |
| Renal protective effects in diabetic conditions | Renal tissue | Anti-fibrosis Anti-oxidation |
BACE1: β-site secretase enzyme; CBF: cerebral blood flow; CVR: cerebrovascular reactivity; cPLA2: cytosolic phospholipase A2; PGE2; prostaglandin E2.
Emerging research has indicated physiological roles of taxifolin, which has raised new issues for further investigation. One such issue is to identify the molecular targets and/or receptors of taxifolin. In addition to its binding to Aβ and α-amylase [34,45,69], taxifolin modulates the phenotypes of cells and animals [42,45,48,69,71,76,81,82], suggesting that taxifolin also potentially binds to receptors/transcription factors which would subsequently affect intracellular signal transduction and gene expression profiles. Determining the molecular mechanisms of taxifolin-stimulated signaling pathways would provide significant clues for the identification of novel molecular targets to prevent and treat cognitive dysfunction and metabolic diseases.
Another important issue is the modification and/or synthesis of novel bioactive molecules based on taxifolin. In a study, 191 taxifolin metabolites were detected in various tissues of taxifolin-fed rats [41], and it is possible that each of these metabolites has a different functional significance. Accordingly, further bioinformatical and experimental approaches using these data will lead to the development of novel bioactive therapeutic molecules which exhibit improved taxifolin-related cell type- or tissue type-specific activities, depending on the disease type.
Finally, issues yet to be addressed include the clinical significance of taxifolin. Future interventional studies in humans should aim to determine the effects of taxifolin on prevention and treatment of cognitive impairment as well as metabolic diseases; these studies would contribute to developing novel strategies for reducing disease risk. In this respect, a double-blind, placebo-controlled, randomized early phase II study is in progress (“Cilostazol for prevention of conversion from mild cognitive impairment (MCI) to Dementia (COMCID) study), which is aimed at evaluating the efficacy and safety of cilostazol in patients with mild cognitive impairment [83]. The beneficial effects of cilostazol on neuronal cell lines have been found to be similar to those of taxifolin [48], even though they were based on in vitro results; thus, the findings of the COMCID study will allow us to gain insights into the clinical potential of taxifolin. Furthermore, investigating the efficacy and safety of the co-treatment with taxifolin and cilostazol would help establish novel therapeutic strategies for CAA and AD.
In conclusion, recent studies on taxifolin have provided a better understanding of its mechanisms of action and have highlighted its physiological significance and therapeutic potential for Aβ-related cognitive impairment as well as for metabolic diseases with an increased risk for neurodegenerative diseases. It should be noted that there has been no new drug approved for the treatment of AD over the past 15 years, despite extensive research and clinical trials with candidate drugs targeting Aβ accumulation [84]. This may increase the possibility that Aβ accumulation is a by-product of the AD process rather than a cause, thereby suggesting the importance to address alternative hypotheses to the amyloid cascade hypothesis [84]. However, Aβ has been recently associated with cytotoxicity; therefore, Aβ should be targeted for the treatment of AD and CAA. In this respect, findings from Aβ immunization studies in which antibody-solubilized Aβ from the senile plaque redeposited in the cerebral vasculature and exacerbated CAA [17,18,19,20], as described earlier, suggest that not only prevention of Aβ aggregation but also efficient clearance of Aβ should be a key strategy for the treatment of AD and CAA [16]. Furthermore, other cytotoxic mediators in the brain include proinflammatory cytokines and reactive oxygen species, and identifying these factors would also be useful for the development of treatments for AD and CAA. In this context, this present study provides the first evidence that orally administered taxifolin suppressed Aβ expression, reduced proinflammatory cytokine levels, alleviated oxidative tissue damage, and reduced the markers of apoptotic cell death in the brain of CAA model mice [85]. Together with results demonstrating the effective clearance of Aβ [44], these findings highlight the use of taxifolin as a potential novel therapeutic target for AD and CAA. Future basic and clinical studies aimed at clarifying the molecular mechanisms underlying taxifolin’s pleiotropic beneficial effects would open new avenues for preemptive medicine for dementia and address its causative metabolic dysfunctions.
Acknowledgments
We wish to thank Kazuya Muranaka at Kyoto Medical Center for his technical assistance. We would like to thank Enago (www.enago.jp) for the English language review.
Abbreviations
| AD | Alzheimer’s disease |
| Aβ | Amyloid-β |
| CAA | Cerebral amyloid angiopathy |
| IPAD | Intramural periarterial drainage |
Funding
This work was supported in part by Grant-in-Aid for Scientific Research (C) to M.T. (JSPS KAKENHI Grant Number JP19K07927), Grant-in-Aid for Young Scientists (B) to S.S. (JP17K14958), Grant-in-Aid for Scientific Research (C) to T.I. (JP19K11760), and Grant-in-Aid for Scientific Research (B) to N.S.-A. (JP18H02737), and by Grant-in-Aid for Exploratory Research to N.S.-A. (JP18K19769), from Japan Society for the Promotion of Science. This study was also supported in part by a grant from Takeda Science Foundation to M.T., a grant from Health Science University to M.T., a grant from the Intramural Research Fund (29-6-15) for Cerebrovascular Diseases of National Cerebral and Cardiovascular Center to S.S., a grant from Smoking Research Foundation to N.S.-A. (128), and a grant from the National Hospital Organization for collaborative clinical research to N.S.-A. (H26-NHO-02).
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- 1.Rodrigues M.A., Samarasekera N., Lerpiniere C., Humphreys C., McCarron M.O., White P.M., Nicoll J.A.R., Sudlow C.L.M., Cordonnier C., Wardlaw J.M., et al. The Edinburgh CT and genetic diagnostic criteria for lobar intracerebral haemorrhage associated with cerebral amyloid angiopathy: Model development and diagnostic test accuracy study. Lancet Neurol. 2018;17:232–240. doi: 10.1016/S1474-4422(18)30006-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Smith E.E., Greenberg S.M. β-amyloid, blood vessels, and brain function. Stroke. 2009;40:2601–2606. doi: 10.1161/STROKEAHA.108.536839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sennfalt S., Norrving B., Petersson J., Ullberg T. Long-Term Survival and Function After Stroke. Stroke. 2018 doi: 10.1161/STROKEAHA.118.022913. [DOI] [PubMed] [Google Scholar]
- 4.Yamada M. Cerebral amyloid angiopathy: Emerging concepts. J. Stroke. 2015;17:17–30. doi: 10.5853/jos.2015.17.1.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Greenberg S.M., Al-Shahi Salman R., Biessels G.J., van Buchem M., Cordonnier C., Lee J.M., Montaner J., Schneider J.A., Smith E.E., Vernooij M., et al. Outcome markers for clinical trials in cerebral amyloid angiopathy. Lancet Neurol. 2014;13:419–428. doi: 10.1016/S1474-4422(14)70003-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Charidimou A., Linn J., Vernooij M.W., Opherk C., Akoudad S., Baron J.C., Greenberg S.M., Jager H.R., Werring D.J. Cortical superficial siderosis: Detection and clinical significance in cerebral amyloid angiopathy and related conditions. Brain. 2015;138:2126–2139. doi: 10.1093/brain/awv162. [DOI] [PubMed] [Google Scholar]
- 7.Chiang G.C., Cruz Hernandez J.C., Kantarci K., Jack C.R., Weiner M.W., Alzheimer’s Disease Neuroimaging Initiative Cerebral Microbleeds, CSF p-Tau, and Cognitive Decline: Significance of Anatomic Distribution. AJNR Am. J. Neuroradiol. 2015;36:1635–1641. doi: 10.3174/ajnr.A4351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tsai H.H., Pasi M., Tsai L.K., Chen Y.F., Lee B.C., Tang S.C., Fotiadis P., Huang C.Y., Yen R.F., Gurol M.E., et al. Distribution of Lacunar Infarcts in Asians With Intracerebral Hemorrhage: A Magnetic Resonance Imaging and Amyloid Positron Emission Tomography Study. Stroke. 2018;49:1515–1517. doi: 10.1161/STROKEAHA.118.021539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Saito S., Yamamoto Y., Ihara M. Mild Cognitive Impairment: At the Crossroad of Neurodegeneration and Vascular Dysfunction. Curr. Alzheimer Res. 2015;12:507–512. doi: 10.2174/1567205012666150530202508. [DOI] [PubMed] [Google Scholar]
- 10.Van Rooden S., Goos J.D., van Opstal A.M., Versluis M.J., Webb A.G., Blauw G.J., van der Flier W.M., Scheltens P., Barkhof F., van Buchem M.A., et al. Increased number of microinfarcts in Alzheimer disease at 7-T MR imaging. Radiology. 2014;270:205–211. doi: 10.1148/radiol.13130743. [DOI] [PubMed] [Google Scholar]
- 11.Westover M.B., Bianchi M.T., Yang C., Schneider J.A., Greenberg S.M. Estimating cerebral microinfarct burden from autopsy samples. Neurology. 2013;80:1365–1369. doi: 10.1212/WNL.0b013e31828c2f52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kalaria R.N. Neuropathological diagnosis of vascular cognitive impairment and vascular dementia with implications for Alzheimer’s disease. Acta Neuropathol. 2016;131:659–685. doi: 10.1007/s00401-016-1571-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Boyle P.A., Yu L., Nag S., Leurgans S., Wilson R.S., Bennett D.A., Schneider J.A. Cerebral amyloid angiopathy and cognitive outcomes in community-based older persons. Neurology. 2015;85:1930–1936. doi: 10.1212/WNL.0000000000002175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Iturria-Medina Y., Sotero R.C., Toussaint P.J., Evans A.C., Alzheimer’s Disease Neuroimaging I. Epidemic spreading model to characterize misfolded proteins propagation in aging and associated neurodegenerative disorders. PLoS Comput. Biol. 2014;10:e1003956. doi: 10.1371/journal.pcbi.1003956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mawuenyega K.G., Sigurdson W., Ovod V., Munsell L., Kasten T., Morris J.C., Yarasheski K.E., Bateman R.J. Decreased clearance of CNS β-amyloid in Alzheimer’s disease. Science. 2010;330:1774. doi: 10.1126/science.1197623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Saito S., Ihara M. New therapeutic approaches for Alzheimer’s disease and cerebral amyloid angiopathy. Front. Aging Neurosci. 2014;6:290. doi: 10.3389/fnagi.2014.00290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nicoll J.A., Wilkinson D., Holmes C., Steart P., Markham H., Weller R.O. Neuropathology of human Alzheimer disease after immunization with amyloid-beta peptide: A case report. Nat. Med. 2003;9:448–452. doi: 10.1038/nm840. [DOI] [PubMed] [Google Scholar]
- 18.Patton R.L., Kalback W.M., Esh C.L., Kokjohn T.A., Van Vickle G.D., Luehrs D.C., Kuo Y.M., Lopez J., Brune D., Ferrer I., et al. Amyloid-beta peptide remnants in AN-1792-immunized Alzheimer’s disease patients: A biochemical analysis. Am. J. Pathol. 2006;169:1048–1063. doi: 10.2353/ajpath.2006.060269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Verbeek M.M., Kremer B.P., Rikkert M.O., Van Domburg P.H., Skehan M.E., Greenberg S.M. Cerebrospinal fluid amyloid beta(40) is decreased in cerebral amyloid angiopathy. Ann. Neurol. 2009;66:245–249. doi: 10.1002/ana.21694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.van Etten E.S., Verbeek M.M., van der Grond J., Zielman R., van Rooden S., van Zwet E.W., van Opstal A.M., Haan J., Greenberg S.M., van Buchem M.A., et al. beta-Amyloid in CSF: Biomarker for preclinical cerebral amyloid angiopathy. Neurology. 2017;88:169–176. doi: 10.1212/WNL.0000000000003486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Weller R.O., Sharp M.M., Christodoulides M., Carare R.O., Mollgard K. The meninges as barriers and facilitators for the movement of fluid, cells and pathogens related to the rodent and human CNS. Acta Neuropathol. 2018;135:363–385. doi: 10.1007/s00401-018-1809-z. [DOI] [PubMed] [Google Scholar]
- 22.Morris A.W.J., Carare R.O., Schreiber S., Hawkes C.A. The Cerebrovascular Basement Membrane: Role in the Clearance of β-amyloid and Cerebral Amyloid Angiopathy. Front. Aging Neurosci. 2014;6:251. doi: 10.3389/fnagi.2014.00251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Arbel-Ornath M., Hudry E., Eikermann-Haerter K., Hou S., Gregory J.L., Zhao L., Betensky R.A., Frosch M.P., Greenberg S.M., Bacskai B.J. Interstitial fluid drainage is impaired in ischemic stroke and Alzheimer’s disease mouse models. Acta Neuropathol. 2013;126:353–364. doi: 10.1007/s00401-013-1145-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Morris A.W.J., Sharp M.M., Albargothy N.J., Fernandes R., Hawkes C.A., Verma A., Weller R.O., Carare R.O. Vascular basement membranes as pathways for the passage of fluid into and out of the brain. Acta Neuropathol. 2016;131:725–736. doi: 10.1007/s00401-016-1555-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hawkes C.A., Hartig W., Kacza J., Schliebs R., Weller R.O., Nicoll J.A., Carare R.O. Perivascular drainage of solutes is impaired in the ageing mouse brain and in the presence of cerebral amyloid angiopathy. Acta Neuropathol. 2011;121:431–443. doi: 10.1007/s00401-011-0801-7. [DOI] [PubMed] [Google Scholar]
- 26.Maki T., Okamoto Y., Carare R.O., Hase Y., Hattori Y., Hawkes C.A., Saito S., Yamamoto Y., Terasaki Y., Ishibashi-Ueda H., et al. Phosphodiesterase III inhibitor promotes drainage of cerebrovascular β-amyloid. Ann. Clin. Transl. Neurol. 2014;1:519–533. doi: 10.1002/acn3.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hardy J., Selkoe D.J. The amyloid hypothesis of Alzheimer’s disease: Progress and problems on the road to therapeutics. Science. 2002;297:353–356. doi: 10.1126/science.1072994. [DOI] [PubMed] [Google Scholar]
- 28.Niwa K., Younkin L., Ebeling C., Turner S.K., Westaway D., Younkin S., Ashe K.H., Carlson G.A., Iadecola C. Aβ1-40-related reduction in functional hyperemia in mouse neocortex during somatosensory activation. Proc. Natl. Acad. Sci. USA. 2000;97:9735–9740. doi: 10.1073/pnas.97.17.9735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Niwa K., Carlson G.A., Iadecola C. Exogenous Aβ1-40 reproduces cerebrovascular alterations resulting from amyloid precursor protein overexpression in mice. J. Cereb. Blood Flow Metab. 2000;20:1659–1668. doi: 10.1097/00004647-200012000-00005. [DOI] [PubMed] [Google Scholar]
- 30.Park L., Zhou P., Koizumi K., El Jamal S., Previti M.L., Van Nostrand W.E., Carlson G., Iadecola C. Brain and circulating levels of Aβ1-40 differentially contribute to vasomotor dysfunction in the mouse brain. Stroke. 2013;44:198–204. doi: 10.1161/STROKEAHA.112.670976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Weller R.O., Hawkes C.A., Carare R.O., Hardy J. Does the difference between PART and Alzheimer’s disease lie in the age-related changes in cerebral arteries that trigger the accumulation of Abeta and propagation of tau? Acta Neuropathol. 2015;129:763–766. doi: 10.1007/s00401-015-1416-1. [DOI] [PubMed] [Google Scholar]
- 32.Ono K., Yamada M. Low-n oligomers as therapeutic targets of Alzheimer’s disease. J. Neurochem. 2011;117:19–28. doi: 10.1111/j.1471-4159.2011.07187.x. [DOI] [PubMed] [Google Scholar]
- 33.Ono K., Hamaguchi T., Naiki H., Yamada M. Anti-amyloidogenic effects of antioxidants: Implications for the prevention and therapeutics of Alzheimer’s disease. Biochim. Biophys. Acta. 2006;1762:575–586. doi: 10.1016/j.bbadis.2006.03.002. [DOI] [PubMed] [Google Scholar]
- 34.Sato M., Murakami K., Uno M., Nakagawa Y., Katayama S., Akagi K., Masuda Y., Takegoshi K., Irie K. Site-specific inhibitory mechanism for amyloid β42 aggregation by catechol-type flavonoids targeting the Lys residues. J. Biol. Chem. 2013;288:23212–23224. doi: 10.1074/jbc.M113.464222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hsu F., Park G., Guo Z. Key Residues for the Formation of Abeta42 Amyloid Fibrils. ACS Omega. 2018;3:8401–8407. doi: 10.1021/acsomega.8b00887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Park L., Koizumi K., El Jamal S., Zhou P., Previti M.L., Van Nostrand W.E., Carlson G., Iadecola C. Age-dependent neurovascular dysfunction and damage in a mouse model of cerebral amyloid angiopathy. Stroke. 2014;45:1815–1821. doi: 10.1161/STROKEAHA.114.005179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Han B.H., Zhou M.L., Abousaleh F., Brendza R.P., Dietrich H.H., Koenigsknecht-Talboo J., Cirrito J.R., Milner E., Holtzman D.M., Zipfel G.J. Cerebrovascular dysfunction in amyloid precursor protein transgenic mice: Contribution of soluble and insoluble amyloid-β peptide, partial restoration via γ-secretase inhibition. J. Neurosci. 2008;28:13542–13550. doi: 10.1523/JNEUROSCI.4686-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Han B.H., Zhou M.L., Johnson A.W., Singh I., Liao F., Vellimana A.K., Nelson J.W., Milner E., Cirrito J.R., Basak J., et al. Contribution of reactive oxygen species to cerebral amyloid angiopathy, vasomotor dysfunction, and microhemorrhage in aged Tg2576 mice. Proc. Natl. Acad. Sci. USA. 2015;112:E881–E890. doi: 10.1073/pnas.1414930112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Haass C., Selkoe D.J. Soluble protein oligomers in neurodegeneration: Lessons from the Alzheimer’s amyloid β-peptide. Nat. Rev. Mol. Cell Biol. 2007;8:101–112. doi: 10.1038/nrm2101. [DOI] [PubMed] [Google Scholar]
- 40.Youdim K.A., Shukitt-Hale B., Joseph J.A. Flavonoids and the brain: Interactions at the blood-brain barrier and their physiological effects on the central nervous system. Free Radic. Biol. Med. 2004;37:1683–1693. doi: 10.1016/j.freeradbiomed.2004.08.002. [DOI] [PubMed] [Google Scholar]
- 41.Yang P., Xu F., Li H.F., Wang Y., Li F.C., Shang M.Y., Liu G.X., Wang X., Cai S.Q. Detection of 191 Taxifolin Metabolites and Their Distribution in Rats Using HPLC-ESI-IT-TOF-MSn. Molecules. 2016;21:1209. doi: 10.3390/molecules21091209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wang Y., Wang Q., Bao X., Ding Y., Shentu J., Cui W., Chen X., Wei X., Xu S. Taxifolin prevents beta-amyloid-induced impairments of synaptic formation and deficits of memory via the inhibition of cytosolic phospholipase A2/prostaglandin E2 content. Metab. Brain Dis. 2018;33:1069–1079. doi: 10.1007/s11011-018-0207-5. [DOI] [PubMed] [Google Scholar]
- 43.Booth A.N., Deeds F. The toxicity and metabolism of dihydroquercetin. J. Am. Pharm. Assoc. Am. Pharm. Assoc. 1958;47:183–184. doi: 10.1002/jps.3030470310. [DOI] [PubMed] [Google Scholar]
- 44.Schauss A.G., Tselyico S.S., Kuznetsova V.A., Yegorova I. Toxicological and Genotoxicity Assessment of a Dihydroquercetin-Rich Dahurian Larch Tree (Larix gmelinii Rupr) Extract (Lavitol) Int. J. Toxicol. 2015;34:162–181. doi: 10.1177/1091581815576975. [DOI] [PubMed] [Google Scholar]
- 45.Saito S., Yamamoto Y., Maki T., Hattori Y., Ito H., Mizuno K., Harada-Shiba M., Kalaria R.N., Fukushima M., Takahashi R., et al. Taxifolin inhibits amyloid-beta oligomer formation and fully restores vascular integrity and memory in cerebral amyloid angiopathy. Acta Neuropathol. Commun. 2017;5:26. doi: 10.1186/s40478-017-0429-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Davis J., Xu F., Deane R., Romanov G., Previti M.L., Zeigler K., Zlokovic B.V., Van Nostrand W.E. Early-onset and robust cerebral microvascular accumulation of amyloid β-protein in transgenic mice expressing low levels of a vasculotropic Dutch/Iowa mutant form of amyloid β-protein precursor. J. Biol. Chem. 2004;279:20296–20306. doi: 10.1074/jbc.M312946200. [DOI] [PubMed] [Google Scholar]
- 47.Vassar R., Bennett B.D., Babu-Khan S., Kahn S., Mendiaz E.A., Denis P., Teplow D.B., Ross S., Amarante P., Loeloff R., et al. Beta-secretase cleavage of Alzheimer’s amyloid precursor protein by the transmembrane aspartic protease BACE. Science. 1999;286:735–741. doi: 10.1126/science.286.5440.735. [DOI] [PubMed] [Google Scholar]
- 48.Park S.Y., Kim H.Y., Park H.J., Shin H.K., Hong K.W., Kim C.D. Concurrent Treatment with Taxifolin and Cilostazol on the Lowering of beta-Amyloid Accumulation and Neurotoxicity via the Suppression of P-JAK2/P-STAT3/NF-kappaB/BACE1 Signaling Pathways. PLoS ONE. 2016;11:e0168286. doi: 10.1371/journal.pone.0168286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sun J., Roy S. The physical approximation of APP and BACE-1: A key event in Alzheimer’s disease pathogenesis. Dev. Neurobiol. 2018;78:340–347. doi: 10.1002/dneu.22556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Fukumoto H., Cheung B.S., Hyman B.T., Irizarry M.C. Beta-secretase protein and activity are increased in the neocortex in Alzheimer disease. Arch. Neurol. 2002;59:1381–1389. doi: 10.1001/archneur.59.9.1381. [DOI] [PubMed] [Google Scholar]
- 51.Stockley J.H., Ravid R., O’Neill C. Altered beta-secretase enzyme kinetics and levels of both BACE1 and BACE2 in the Alzheimer’s disease brain. FEBS Lett. 2006;580:6550–6560. doi: 10.1016/j.febslet.2006.10.076. [DOI] [PubMed] [Google Scholar]
- 52.Buggia-Prevot V., Sevalle J., Rossner S., Checler F. NFkappaB-dependent control of BACE1 promoter transactivation by Abeta42. J. Biol. Chem. 2008;283:10037–10047. doi: 10.1074/jbc.M706579200. [DOI] [PubMed] [Google Scholar]
- 53.Chen C.H., Zhou W., Liu S., Deng Y., Cai F., Tone M., Tone Y., Tong Y., Song W. Increased NF-kappaB signalling up-regulates BACE1 expression and its therapeutic potential in Alzheimer’s disease. Int. J. Neuropsychopharmacol. 2012;15:77–90. doi: 10.1017/S1461145711000149. [DOI] [PubMed] [Google Scholar]
- 54.Gomes B.A.Q., Silva J.P.B., Romeiro C.F.R., Dos Santos S.M., Rodrigues C.A., Goncalves P.R., Sakai J.T., Mendes P.F.S., Varela E.L.P., Monteiro M.C. Neuroprotective Mechanisms of Resveratrol in Alzheimer’s Disease: Role of SIRT1. Oxid. Med. Cell. Longev. 2018;2018:8152373. doi: 10.1155/2018/8152373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Philippens I.H., Ormel P.R., Baarends G., Johansson M., Remarque E.J., Doverskog M. Acceleration of Amyloidosis by Inflammation in the Amyloid-Beta Marmoset Monkey Model of Alzheimer’s Disease. J. Alzheimers Dis. 2017;55:101–113. doi: 10.3233/JAD-160673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sastre M., Klockgether T., Heneka M.T. Contribution of inflammatory processes to Alzheimer’s disease: Molecular mechanisms. Int. J. Dev. Neurosci. 2006;24:167–176. doi: 10.1016/j.ijdevneu.2005.11.014. [DOI] [PubMed] [Google Scholar]
- 57.Hermann P.M., Watson S.N., Wildering W.C. Phospholipase A2—nexus of aging, oxidative stress, neuronal excitability, and functional decline of the aging nervous system? Insights from a snail model system of neuronal aging and age-associated memory impairment. Front. Genet. 2014;5:419. doi: 10.3389/fgene.2014.00419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sagy-Bross C., Kasianov K., Solomonov Y., Braiman A., Friedman A., Hadad N., Levy R. The role of cytosolic phospholipase A2 alpha in amyloid precursor protein induction by amyloid beta1-42 : Implication for neurodegeneration. J. Neurochem. 2015;132:559–571. doi: 10.1111/jnc.13012. [DOI] [PubMed] [Google Scholar]
- 59.Qu B., Gong Y., Gill J.M., Kenney K., Diaz-Arrastia R. Heterozygous knockout of cytosolic phospholipase A2alpha attenuates Alzheimer’s disease pathology in APP/PS1 transgenic mice. Brain Res. 2017;1670:248–252. doi: 10.1016/j.brainres.2017.06.021. [DOI] [PubMed] [Google Scholar]
- 60.Shelat P.B., Chalimoniuk M., Wang J.H., Strosznajder J.B., Lee J.C., Sun A.Y., Simonyi A., Sun G.Y. Amyloid beta peptide and NMDA induce ROS from NADPH oxidase and AA release from cytosolic phospholipase A2 in cortical neurons. J. Neurochem. 2008;106:45–55. doi: 10.1111/j.1471-4159.2008.05347.x. [DOI] [PubMed] [Google Scholar]
- 61.Bate C., Williams A. cAMP-Inhibits Cytoplasmic Phospholipase A(2) and Protects Neurons against Amyloid-beta-Induced Synapse Damage. Biology (Basel) 2015;4:591–606. doi: 10.3390/biology4030591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Brummett A.M., Navratil A.R., Bryan J.D., Woolard M.D. Janus kinase 3 activity is necessary for phosphorylation of cytosolic phospholipase A2 and prostaglandin E2 synthesis by macrophages infected with Francisella tularensis live vaccine strain. Infect. Immun. 2014;82:970–982. doi: 10.1128/IAI.01461-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Bate C., Williams A. Alpha-Synuclein-induced synapse damage in cultured neurons is mediated by cholesterol-sensitive activation of cytoplasmic phospholipase A2. Biomolecules. 2015;5:178–193. doi: 10.3390/biom5010178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ohara T., Doi Y., Ninomiya T., Hirakawa Y., Hata J., Iwaki T., Kanba S., Kiyohara Y. Glucose tolerance status and risk of dementia in the community: The Hisayama study. Neurology. 2011;77:1126–1134. doi: 10.1212/WNL.0b013e31822f0435. [DOI] [PubMed] [Google Scholar]
- 65.Chatterjee S., Peters S.A., Woodward M., Mejia Arango S., Batty G.D., Beckett N., Beiser A., Borenstein A.R., Crane P.K., Haan M., et al. Type 2 Diabetes as a Risk Factor for Dementia in Women Compared With Men: A Pooled Analysis of 2.3 Million People Comprising More Than 100,000 Cases of Dementia. Diabetes Care. 2016;39:300–307. doi: 10.2337/dc15-1588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Morley J.E. Diabetes: The diabetic brain. Nat. Rev. Endocrinol. 2017;13:570–571. doi: 10.1038/nrendo.2017.111. [DOI] [PubMed] [Google Scholar]
- 67.Biessels G.J., Staekenborg S., Brunner E., Brayne C., Scheltens P. Risk of dementia in diabetes mellitus: A systematic review. Lancet Neurol. 2006;5:64–74. doi: 10.1016/S1474-4422(05)70284-2. [DOI] [PubMed] [Google Scholar]
- 68.Hirabayashi N., Hata J., Ohara T., Mukai N., Nagata M., Shibata M., Gotoh S., Furuta Y., Yamashita F., Yoshihara K., et al. Association Between Diabetes and Hippocampal Atrophy in Elderly Japanese: The Hisayama Study. Diabetes Care. 2016;39:1543–1549. doi: 10.2337/dc15-2800. [DOI] [PubMed] [Google Scholar]
- 69.Rehman K., Chohan T.A., Waheed I., Gilani Z., Akash M.S.H. Taxifolin prevents postprandial hyperglycemia by regulating the activity of alpha-amylase: Evidence from an in vivo and in silico studies. J. Cell. Biochem. 2019;120:425–438. doi: 10.1002/jcb.27398. [DOI] [PubMed] [Google Scholar]
- 70.Rosak C., Mertes G. Critical evaluation of the role of acarbose in the treatment of diabetes: Patient considerations. Diabetes Metab. Syndr. Obes. 2012;5:357–367. doi: 10.2147/DMSO.S28340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ding T., Wang S., Zhang X., Zai W., Fan J., Chen W., Bian Q., Luan J., Shen Y., Zhang Y., et al. Kidney protection effects of dihydroquercetin on diabetic nephropathy through suppressing ROS and NLRP3 inflammasome. Phytomedicine. 2018;41:45–53. doi: 10.1016/j.phymed.2018.01.026. [DOI] [PubMed] [Google Scholar]
- 72.Seliger S.L., Siscovick D.S., Stehman-Breen C.O., Gillen D.L., Fitzpatrick A., Bleyer A., Kuller L.H. Moderate renal impairment and risk of dementia among older adults: The Cardiovascular Health Cognition Study. J. Am. Soc. Nephrol. 2004;15:1904–1911. doi: 10.1097/01.ASN.0000131529.60019.FA. [DOI] [PubMed] [Google Scholar]
- 73.Helmer C., Stengel B., Metzger M., Froissart M., Massy Z.A., Tzourio C., Berr C., Dartigues J.F. Chronic kidney disease, cognitive decline, and incident dementia: The 3C Study. Neurology. 2011;77:2043–2051. doi: 10.1212/WNL.0b013e31823b4765. [DOI] [PubMed] [Google Scholar]
- 74.Takae K., Hata J., Ohara T., Yoshida D., Shibata M., Mukai N., Hirakawa Y., Kishimoto H., Tsuruya K., Kitazono T., et al. Albuminuria Increases the Risks for Both Alzheimer Disease and Vascular Dementia in Community-Dwelling Japanese Elderly: The Hisayama Study. J. Am. Heart Assoc. 2018;7 doi: 10.1161/JAHA.117.006693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Fujisaki K., Tsuruya K., Yamato M., Toyonaga J., Noguchi H., Nakano T., Taniguchi M., Tokumoto M., Hirakata H., Kitazono T. Cerebral oxidative stress induces spatial working memory dysfunction in uremic mice: Neuroprotective effect of tempol. Nephrol. Dial. Transplant. 2014;29:529–538. doi: 10.1093/ndt/gft327. [DOI] [PubMed] [Google Scholar]
- 76.Zhao Y., Huang W., Wang J., Chen Y., Huang W., Zhu Y. Taxifolin attenuates diabetic nephropathy in streptozotocin-induced diabetic rats. Am. J. Transl. Res. 2018;10:1205–1210. [PMC free article] [PubMed] [Google Scholar]
- 77.Kivipelto M., Ngandu T., Fratiglioni L., Viitanen M., Kareholt I., Winblad B., Helkala E.L., Tuomilehto J., Soininen H., Nissinen A. Obesity and vascular risk factors at midlife and the risk of dementia and Alzheimer disease. Arch. Neurol. 2005;62:1556–1560. doi: 10.1001/archneur.62.10.1556. [DOI] [PubMed] [Google Scholar]
- 78.Qizilbash N., Gregson J., Johnson M.E., Pearce N., Douglas I., Wing K., Evans S.J.W., Pocock S.J. BMI and risk of dementia in two million people over two decades: A retrospective cohort study. Lancet Diabetes Endocrinol. 2015;3:431–436. doi: 10.1016/S2213-8587(15)00033-9. [DOI] [PubMed] [Google Scholar]
- 79.Collaboration N.C.D.R.F. Trends in adult body-mass index in 200 countries from 1975 to 2014: A pooled analysis of 1698 population-based measurement studies with 19.2 million participants. Lancet. 2016;387:1377–1396. doi: 10.1016/S0140-6736(16)30054-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Moll van Charante E.P., Richard E., Eurelings L.S., van Dalen J.W., Ligthart S.A., van Bussel E.F., Hoevenaar-Blom M.P., Vermeulen M., van Gool W.A. Effectiveness of a 6-year multidomain vascular care intervention to prevent dementia (preDIVA): A cluster-randomised controlled trial. Lancet. 2016;388:797–805. doi: 10.1016/S0140-6736(16)30950-3. [DOI] [PubMed] [Google Scholar]
- 81.Zekry S.H., Abo-elmatty D.M., Zayed R.A., Radwan M.M., ElSohly M.A., Hassanean H.A., Ahmed S.A. Effect of metabolites isolated from Cuscuta pedicellata on high fat diet-fed rats. Med. Chem. Res. 2015;24:1964–1973. doi: 10.1007/s00044-014-1269-5. [DOI] [Google Scholar]
- 82.Mehanna E.T., El-Sayed N.M., Ibrahim A.K., Ahmed S.A., Abo-Elmatty D.M. Isolated compounds from Cuscuta pedicellata ameliorate oxidative stress and upregulate expression of some energy regulatory genes in high fat diet induced obesity in rats. Biomed. Pharmacother. 2018;108:1253–1258. doi: 10.1016/j.biopha.2018.09.126. [DOI] [PubMed] [Google Scholar]
- 83.Saito S., Kojima S., Oishi N., Kakuta R., Maki T., Yasuno F., Nagatsuka K., Yamamoto H., Fukuyama H., Fukushima M., et al. A multicenter, randomized, placebo-controlled trial for cilostazol in patients with mild cognitive impairment: The COMCID study protocol. Alzheimers Dement (NY) 2016;2:250–257. doi: 10.1016/j.trci.2016.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Panza F., Lozupone M., Logroscino G., Imbimbo B.P. A critical appraisal of amyloid-beta-targeting therapies for Alzheimer disease. Nat. Rev. Neurol. 2019;15:73–88. doi: 10.1038/s41582-018-0116-6. [DOI] [PubMed] [Google Scholar]
- 85.Inoue T., Saito S., Tanaka M., Yamakage H., Kusakabe T., Shimatsu A., Ihara M., Satoh-Asahara N. Pleiotropic neuroprotective effects of taxifolin in cerebral amyloid angiopathy. Proc. Natl. Acad. Sci. USA. 2019 doi: 10.1073/pnas.1901659116. [DOI] [PMC free article] [PubMed] [Google Scholar]