Abstract
Objective
Insufficient sleep duration and quality has negative effects on athletic performance, injury susceptibility and athlete development. This study aimed to assess the sleep characteristics of professional Qatar Stars League (QSL) soccer players.
Methods
In a cross-sectional study, QSL players (n=111; 23.7±4.8 years) completed three questionnaires to screen sleep disorders: (1) Pittsburgh Sleep Quality Index (PSQI), (2) Insomnia Severity Index (ISI) and (3) Epworth Sleepiness Scale (ESS). Poor sleep quality was defined as PSQI≥5, excessive daytime sleepiness was defined by ESS>8 and insomnia was defined as ISI≥11.
Results
The prevalence of poor sleep quality (PSQI≥5) was 68.5%, with subthreshold insomnia (ISI≥11) 27.0% and daytime sleepiness 22.5% (ESS>8). Sleep quality was positively associated with insomnia (r=0.42, p<0.001) and daytime sleepiness (r=0.23, p=0.018). Age, anthropometry, body composition and ethnicity were not associated with any of the reported sleep quality parameters.
Conclusion
The prevalence of poor sleep quality (68.5%) reported should concern practitioners. Increasing awareness of the importance of sleep relative to athletic performance, recovery, injury and illness appears prudent. Further, regular qualitative/quantitative sleep monitoring may help target subsequent evidence-informed interventions to improve sleep in those demonstrating undesirable sleep traits.
Keywords: soccer, Middle East, Arab, Pittsburgh Sleep Quality Index (PSQI), Insomnia Severity Index (ISI), Epworth Sleepiness Scale (ESS)
Key messages.
Two-thirds of professional soccer players living in Qatar have poor sleep quality.
One-third of professional soccer players report excessive daytime sleepiness, subclinical insomnia and insufficient sleep.
Poor sleep quality was associated with subclinical insomnia and excessive daytime sleepiness.
Introduction
Insufficient sleep duration and quality has negative effects on athletic performance,1 injury susceptibility,2–4 illness risk,5 wound healing,6 academic performance,7 8 holistic well-being and athlete development.9 Appropriate sleep durations recommended by the National Sleep Foundation (NSF) for adolescents and adults are approximately 8–10 hours10 with no specific recommendations for athletic populations. However, in the Middle East in particular, individuals obtain insufficient sleep relative to these recommendations across adults (6.2±1.7 hours)11 and adolescents (7 hours),12 13 including adolescent academy soccer players (6.3– 7.3 hours).14
In the Middle East, cultural explanations of these region-specific deficiencies in sleep duration centre around an environment that lends itself to early morning and late evening. The extreme heat makes athletic competition and training difficult during daylight hours and socialising is more conducive when the sun is setting/rising. In addition to the culturally expected commitments and day-to-day activities, the Islamic practice of first prayer with sunrise or fasting during the holy month of Ramadan13 exacerbates sleep.9 12 14 A plethora of inter-related self-imposed (eg, screen-time use, social media interaction, caffeine intake, and so on) and externally imposed (eg, training commitments, fixture scheduling, travel demands, media/sponsor commitments, doping control commitments, high-arousal postevening training/competition, and so on) sociopsychological factors interact with the region-specific nuances outlined above12 14 challenging professional soccer players within the Middle East to obtain sufficient sleep duration and quality.
Although sleep quality is a holistically complex construct15 (eg, dependent on sleep efficiency, latency and wake after sleep onset, and indirectly associated with subjects’ perception of sleep quality and level of sleepiness),16 17 various quantitative (eg, actigraphy) and qualitative (eg, questionnaires) approaches have been employed with athletes to gain some understanding of their sleep behaviours. Among athletes, the sleep hygiene varies with age18 and generally poor sleep quality is linked with adiposity.19 However, aside from data on adolescent academy soccer players14 there is a paucity of evidence to inform practice, particularly from professional soccer players in the Middle East. Indeed, despite having adequate knowledge of the relationship between sleep and athletic performance, less than half of professional teams surveyed monitored sleep in their players or promoted sleep hygiene.20 Therefore, ascertaining the qualitative sleep characteristics and prevalence of sleep disorders from adult professional soccer players and associated factors would be of benefit to, and inform the practice of, practitioners within the Middle East. The objective of this study, therefore, was to determine the prevalence of sleep disorders and sleep behaviours among professional Qatar Stars League (QSL) soccer players. It was hypothesised that many of these athletes would report poor sleep quality and have a high prevalence of sleep disorders such as insomnia and daytime sleepiness.
Methods
Study design and settings
This study was a cross-sectional survey of male professional soccer players from the QSL. The data were collected as part of routine sport science screening across 2 weeks, during a mandatory and routine clinical visit. The questionnaires were administered at Aspetar (Orthopaedic and Sports Medicine Hospital) at the start of a competitive season (1 month prior to Ramadan). The researchers attained approval from team managers prior to the team’s scheduled appointment. While the players were waiting for routine clinical testing, three researchers approached the players with study information, consent forms and research questionnaires.
Participants
Out of the 12 teams approached, eight QSL teams volunteered to participate within this study. Participants were male professional soccer players (aged 18–35 years) from the premier soccer league in Qatar, the QSL. Only those players contracted to a QSL team and provided signed informed consent were eligible for inclusion. Those with current or recent illness/injury were excluded because their condition or use of medications may influence their sleep and introduce bias. Of 128 eligible participants approached, 111 (86.7%) volunteered to participate and provided complete responses to all administered questionnaires (table 1 provides player characteristics including age, anthropometrics and ethnicity).
Table 1.
Characteristics of the participants (n=111)
| Variable | Mean±SD | |
| Age (years) | 23.7±4.8 | |
| Weight (kg) | 71.0±9.9 | |
| Height (cm) | 176.9±5.9 | |
| Body mass index | 22.8±2.1 | |
| Lean mass (kg) | 56.4±6.4 | |
| Body fat (%) | 20.6±4.4 | |
| Ethnicity | n (%) | |
| Qatari | 62 (55.9) | |
| Other Middle East | 27 (24.3) | |
| Africa | 11 (9.9) | |
| Persia | 9 (8.1) | |
| Asia | 1 (0.9) | |
| Europe | 1 (0.9) | |
| Time to bed | ||
| Before 23:00 | 6 (5.4) | |
| 23:00 to 01:00 | 64 (57.4) | |
| 01:00 to 03:00 | 29 (26.1) | |
| 03:00 or later | 12 (10.8) | |
| Wake-up time | ||
| Before 06:00 | 10 (9.0) | |
| 06:00 to 09:00 | 45 (40.5) | |
| 09:00 to 12:00 | 48 (43.2) | |
| 12:00 and later | 8 (7.2) | |
| Pittsburgh Sleep Quality Index (PSQI) | ||
| PSQI <5 | 35 (31.5) | |
| PSQI ≥5 (poor sleep quality) | 76 (68.5) | |
| Insomnia Severity Index (ISI) | ||
| ISI <11 | 81 (73.0) | |
| ISI ≥11 (subclinical insomnia) | 30 (27.0) | |
| Epworth Sleepiness Scale (ESS) | ||
| ESS ≤8 | 86 (77.5) | |
| ESS >8 (excessive daytime sleepiness) | 25 (22.5) | |
Data collection
Height and weight of the participants were assessed using a standardised protocol (Seca 242, Germany), with body composition determined by dual-energy X-ray absorptiometry (GE Medical System Lunar, Madison, Wisconsin, USA) using Encore software (V.12.10). Researchers administered three validated questionnaires to assess sleep disorders and sleep behaviour in a standardised quiet and interruption-free area of the clinic. Questionnaires in paper form were administered face to face in English or Arabic, predominately the latter, with completion times ranging from 15 to 20 min. Both English and Arabic versions of the three questionnaires are valid and reliable and have seen use in athletic populations21 as well as among Middle Eastern populations.22
The Pittsburgh Sleep Quality Index (PSQI) is a valid and reliable questionnaire15 to determine subjective sleep quality across the past month. The sensitivity of PSQI against polysomnography (PSG) is reported as 75.0% within a population similar to that used within the present design. The PSQI consists of 19 items to assess seven components of sleep: (1) sleep quality, (2) sleep duration, (3) sleep latency, (4) sleep efficiency, (5) sleep disturbances, (6) use of sleep drugs and (7) daytime dysfunction. The PSQI can provide a composite score of sleep quality and quantity (range: 0–21) with higher scores indicating poor sleep quality or more sleep difficulties. A PSQI threshold score ≥5 was used to indicate poor sleep quality23 and has been used in similar populations.24
The Epworth Sleepiness Scale (ESS) determines a general yet validated level of daytime sleepiness.25 When compared with overnight PSG, ESS was negatively and significantly correlated with sleep latency.26 Specifically, the probability of a participant falling asleep in eight different situations that people usually although not necessarily face daily is determined. The ESS consists of eight items and yields a score ranging from 0 to 24, with a higher score indicating greater daytime sleepiness. Commonly employed thresholds were adopted (0–8, normal; >8, excessive daytime sleepiness).27 The ESS instrument has been used in similar designs and populations.1
The Insomnia Severity Index (ISI) determines subjective symptoms of insomnia across the past month, specifically (1) sleep onset, (2) maintenance and (3) satisfaction with the current sleep pattern. When compared with PSG, ISI was significantly and positively correlated with wake after sleep onset and negatively correlated with sleep efficiency.28 The questionnaire is valid and reliable.28 It consists of seven items and asks participants to provide ratings on a 5-point Likert scale in which 0 means ‘no problem’ and 4 means ‘very severe problem’. The sum of ISI scores ranges from 0 to 28 points, with higher scores indicating insomnia. Commonly adopted thresholds were used, with ≥11 suggesting subthreshold insomnia and ≥15 suggesting clinical insomnia.28
Statistical analysis
Paper copy questionnaires were compiled into a Microsoft Excel document by the same research assistant. The data were then entered, coded and analysed using SPSS software (SPSS, V.21.0). Continuous variables for ESS, PSQI and ISI scores are presented as the mean±SD. All continuous variables were assessed for normal distribution using Shapiro-Wilk test prior to data analysis. Categorical variables such as PSQI sleep components, ESS, PSQI and ISI threshold categories are presented as frequency and percentage. One-way analysis of variance was performed to compare the mean scores of PSQI, ESS and ISI across ethnicity (eg, Qatari, Other Middle East and Others). Multiple comparisons were adjusted using a Bonferroni correction. Pearson’s correlation coefficient was used to determine the correlation between age, anthropometry and body composition with ESS, PSQI and ISI scores. Independent samples t-test was performed to compare age, anthropometry and body composition between PSQI, ESS and ISI threshold. A two-tailed alpha p value <0.05 was used to determine statistical significance.
Results
The prevalence of players with poor sleep quality (PSQI ≥5) was 68.5% (n=76/111), excessive daytime sleepiness (ESS >8) was 22.5% (n=25/111) and subclinical insomnia (ISI >11) was 27.0% (n=30/111) (table 1).
Figure 1 shows the frequency distribution of PSQI, ISI and ESS in this population. Players (16.2%; n=18) woke up in the middle of the night or early morning with concerning frequency per week (three or more occasions (~17%), once or twice (~26%)) for a multitude of reasons with a visit to the bathroom most resonating (29.7% frequency). Approximately 10% (n=11) of players indicated use of sleep medications within the past month (table 2).
Figure 1.
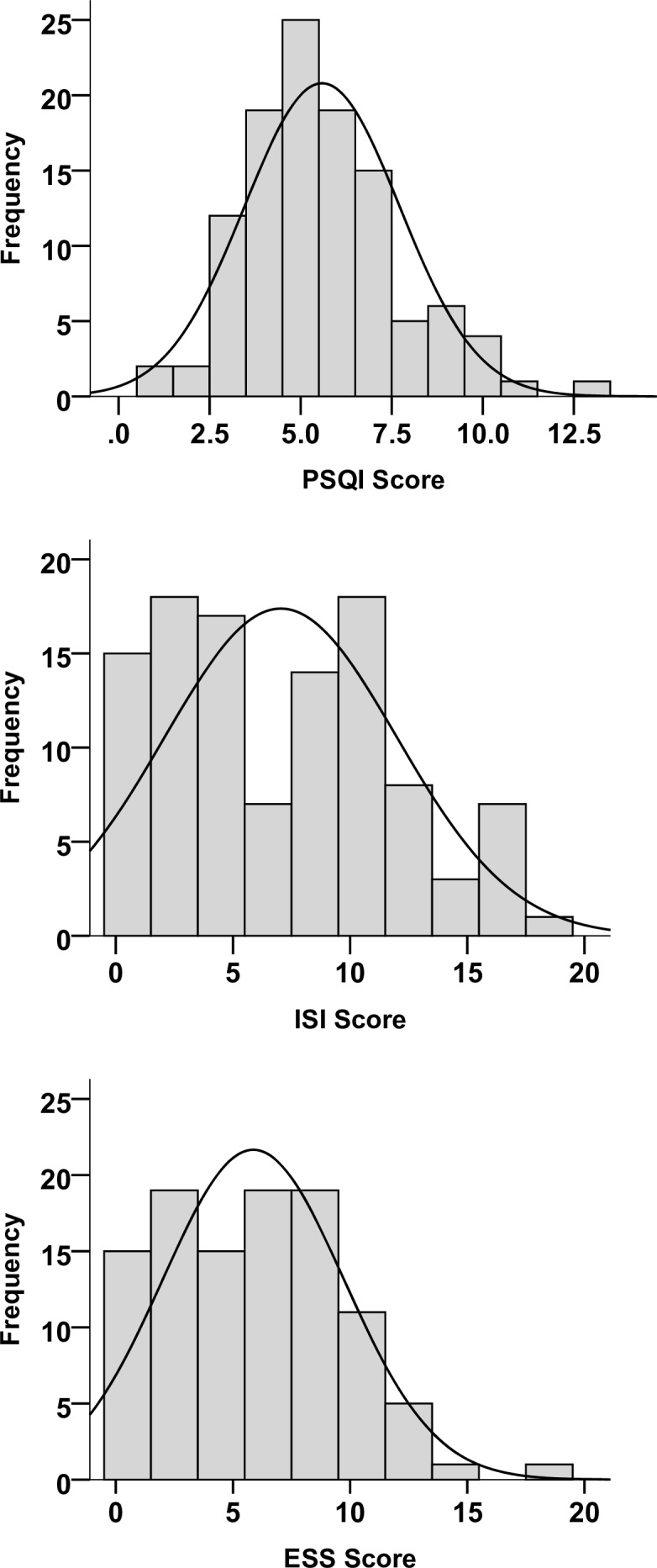
Histogram showing the distribution of Pittsburgh Sleep Quality Index (PSQI), Insomnia Severity Index (ISI) and Epworth Sleepiness Scale (ESS) among the participants.
Table 2.
Components of PSQI (n=111)
| Subjective sleep quality | ||
| Very good | 6 (5.4) | |
| Fairly good | 32 (28.8) | |
| Fairly bad | 60 (54.1) | |
| Very bad | 13 (11.7) | |
| Sleep latency (min) | ||
| ≤15 | 36 (32.4) | |
| 16–30 | 49 (44.1) | |
| 31–60 | 23 (20.7) | |
| >60 | 3 (2.7) | |
| Sleep duration (hours) | ||
| >7 | 72 (64.9) | |
| 6–7 | 20 (18.0) | |
| 5–6 | 19 (17.1) | |
| <5 | 0 (0.0) | |
| Sleep efficiency (%) | ||
| >85 | 107 (96.4) | |
| 75–84 | 4 (3.6) | |
| 65–74 | 0 (0.0) | |
| <65 | 0 (0.0) | |
| Sleep disturbances score (greater score indicates more frequent sleep disturbances) | ||
| 0 | 9 (8.1) | |
| 1 | 87 (78.4) | |
| 2 | 12 (10.8) | |
| 3 | 3 (2.7) | |
| Use of sleep medication | ||
| Not during the past month | 100 (90.1) | |
| Less than once a week | 7 (6.3) | |
| Once or twice a week | 2 (1.8) | |
| Three or more times a week | 2 (1.8) | |
| Daytime dysfunction score (higher score indicates greater daytime dysfunction) | ||
| 0 | 11 (9.9) | |
| 1 | 83 (74.8) | |
| 2 | 15 (13.5) | |
| 3 | 2 (1.8) | |
PSQI, Pittsburgh Sleep Quality Index.
PSQI was positively correlated with ISI (r=0.418, p<0.001) and ESS (r=0.231, p=0.017) scores. PSQI, ISI or ESS was not correlated with age, height, weight or body composition. However, players with excessive daytime sleepiness (ESS>8) were more likely to have a lower body mass index (BMI) compared with players without daytime sleepiness (21.8±2.4 vs 23.0±1.9, p=0.008) (table 3). PSQI, ESS and ISI were similar comparing Qataris, Other Middle East and Others (p>0.148).
Table 3.
Sleep quality, subclinical insomnia and daytime sleepiness thresholds in association with age, body composition and overall sleep assessment scores
| Pittsburgh Sleep Quality Index (PSQI) | Insomnia Severity Index (ISI) | Epworth Sleepiness Scale (ESS) | |||||||
| PSQI<5 (n=35) |
PSQI≥5* (n=76) |
P value | ISI<11 (n=81) |
ISI≥11† (n=30) |
P value | ESS≤8 (n=83) |
ESS>8‡ (n=25) |
P value | |
| Age | 23.4±4.9 | 23.9±4.8 | 0.611 | 24.2±5.0 | 22.5±4.2 | 0.100 | 24.2±5.0 | 22.4±4.2 | 0.117 |
| Body fat (%) | 20.3±3.8 | 20.7±4.7 | 0.658 | 20.5±4.4 | 20.9±4.6 | 0.686 | 20.6±4.5 | 20.6±4.3 | 0.997 |
| Boyd mass index | 22.4±1.5 | 22.9±2.2 | 0.270 | 23.0±2.0 | 22.1±2.1 | 0.054 | 23.0±1.9 | 21.8±2.4 | 0.008 |
| Total sleep time (hours) | 8.5±1.2 | 7.8±1.6 | 0.045 | 8.0±1.4 | 8.0±1.7 | 0.943 | 7.9±1.4 | 8.2±1.8 | 0.472 |
| PSQI score | 3.04±0.8 | 6.6±1.7 | <0.001 | 5.1±1.9 | 6.9±2.1 | <0.001 | 5.3±2.1 | 6.7±1.8 | 0.002 |
| ISI score | 4.0±3.7 | 8.4±4.9 | <0.001 | 4.6±3.3 | 13.3±2.4 | <0.001 | 6.10±4.7 | 10.1±4.5 | <0.001 |
| ESS score | 5.0±3.7 | 6.2±3.9 | 0.129 | 5.1±3.7 | 7.8±3.7 | <0.001 | 4.3±2.6 | 11.0±2.3 | <0.001 |
*PSQI≥5: Poor sleep quality.
†ISI≥11: Subthreshold insomnia.
‡ESS>8: Excessive daytime sleepiness.
Discussion
The prevalence of sleep disorders among professional soccer players was 68.5%. Further, a concerning level of poor sleep quality (PSQI), daytime sleepiness (ESS) and moderately severe clinical insomnia (ISI) was seen in players (see table 2 and figure 1) alongside self-reported insufficient sleep durations compared with established NSF guidelines (8–10 hours).10 The high sleep efficiency observed in this population (96.4% of the sample had sleep efficiency >85) is indicative of insufficient sleep durations, given short sleepers may have high sleep efficiency. However, short sleepers may also have very poor sleep efficiency when quantity and quality are both impaired, for example, in the case of insomnia.
Late bedtimes (bedtime ~00:24) and sleep interruptions (~13%) likely contributed to the self-reported poor sleep quality of players in this study. Insufficient sleep duration and quality has negative effects on athletic performance,1 injury susceptibility,2–4 illness risk,5 wound healing,6 academic performance,7 8 holistic well-being and athlete development.9 Indeed, the late bedtimes observed in this population suggest an evening chronotype and/or delayed sleep phase syndrome, which are implicated in sleep debt and chronic underperformance.29 While the present study did not directly access the relationship between sleep and the afore-described athletic performance relevant effects, the self-reported sleep characteristics are not facilitative of optimal athletic performance and recovery, and long-term athlete development. Therefore, the self-reported sleep results will be of concern to practitioners in the Middle East. Indeed, average sleep quality in the present study (PSQI: 5.6±2.1) was poor compared with elite Australian football (Australian Football League) players (PSQI 4.3±1.6)30 and elite European soccer players (PSQI 3.6±2.4),31 but comparable (5.6±2.3) across a mixed sample of highly trained team sport athletes (predominately Rugby 7’s/15’s and cricket).24 The prevalence of clinical sleep disturbance (PSQI ≥5) in this study was 68.5%, this was higher compared with Brazilian multisports elite athletes (38%)32 and team sports athletes (50%).24
Cultural and environmental factors likely dictate late bedtimes and early rising in QSL players, resulting in suboptimal sleep durations, as detailed elsewhere.9 12 14 Specifically, early morning and/or late evening training/competition within high environmental temperatures33 alongside late evening nutritional needs and early morning prayer are not conducive to the recommended earlier sleep onset times to offset early rising, in order to gain sufficient NSF endorsed (7–9 hours) sleep durations.14 These factors combine to provoke late evening active meal digestion,34 various inflammatory biological cascades35 and increased arousal and body temperatures,36 37 when players are attempting to sleep. These can all negatively influence favourable sleep characteristics34–37 and appropriate nutritional intake,38 39 thus holistic player recovery is likely impeded.40 41 Alongside these challenges the player still has to engage in their everyday activities and commitments, potentially limiting further their time available for sleep. It appears, at least superficially, that changing training/competition scheduling would be an easy solution with regard to enhancing time available for player sleep; however, as outlined here and elsewhere9 14 it is simply not feasible given the holistic local environment. Appropriate daytime nap scheduling may have some utility within the presented paradigm to increase sleep durations and favourably influence performance recovery.42–46
Uninterrupted sleep, particularly in the initial stages of sleep, enhances sleep quality47 and other holistic quality of life measures.48 Leading player explanations for the sleep disturbances surfaced in the present data were a visit to bathroom (27.9%) and ‘feeling too cold’ (13.5%). Players likely consume large volumes of fluid/food in a relatively short space of time after evening training/competition alongside persistently high body core temperatures. There is natural decrease in the core body temperature during sleep initiation49 and this may potentially explain sleep disturbances, that is, ‘feeling too cold’ in addition to the common practice in the region whereof air-conditioning being set too low for a full night’s comfortable sleep when evening temperatures are high. It is therefore not surprising that the need to visit the bathroom and feeling too cold are reported as predominant factors for sleep disturbances within the present population. Appropriate aggressive postcompetition/training cooling manoeuvres50–52 alongside optimally prescribed fluid intake volume and composition (to reduce urine losses)53 may reduce the frequency of these disturbances. A recent study among youth soccer players demonstrated that hot showers prior to bedtime can improve sleep latency by 7 min and sleep efficiency by 2%.54 Sleep disturbances in the present study (13.5%, table 2) are lower compared with elite team sports players from Australasia (34.6%),24 however the present experimental design does not provide insight into the mechanism(s) behind these differences aside from the demographic of players.24
The median body fat % of the athletes included in this study was 19.8% with IQR of (17.3%–24.1%), this could be viewed as relatively high, although body fat % was not associated with any PSQI, ISI or ESS-derived outcomes. The association of BMI and sleep disorders is described as U-shaped relationship with lower BMI and obesity presenting a higher risk for the presence of a sleep disorder.55 The present data found that the average BMI of players with ESS >8 was lower compared with players with normal ESS scores (table 3). Approximately 10% of players reported sleep medication use, similar to the 2014 National Collegiate Athletic Association report where 10% of miscellaneous substance use was represented by sleep medication.56
The presented data and discussion thereof must be tempered by the experimental limitations presented. Indeed, sleep was not assessed quantitatively and a non-athletic control group was not employed, future designs would benefit from such inclusions. However, in practice, the ability to quantitatively assess a large sample of players sleep via actigraphy and/or PSG has practical and logistical limitations.9 Therefore, the easily administrable qualitative questionnaire approach may offer a practically compatible first-step (triage) towards identifying sleep issues within large squads of players allowing economical prescription of quantitative assessment of valid player subsets. A recent systematic review and meta-analysis of studies that monitored sleep among team sports athletes supports this notion, they concluded that sleep efficiency using actigraphy or PSQI are both indicative of sleep quality.57 Future research could benefit from employing the methods adopted here, at different stages of the season (which could include Ramadan), to provide greater understanding of the magnitude of challenge these athletes face to obtain appropriate sleep across a season. Unfortunately, data related to injury and illness were not accessible for the population used within the present design, other similar designs would benefit from the inclusion of such measures. In addition, there was a general response/recall bias because the sleep characteristics reported were based on the recall of sleep behaviour within the preceding month. While the PSQI is a valid instrument to measure sleep characteristics, it does not capture the duration of daytime naps. It is quite possible that athletes in our study compensate for the lack of adequate night-time sleep with naps. Interpretation of the presented data should be conducted carefully relative to these experimental limitations.
Practical applications
The employed questionnaires in this study quickly (15–20 min per player) revealed worrying sleep characteristics in many players and thus practitioners may consider the employed questionnaire battery as a simple time-efficient approach to identify (triage) a subset of players from a large squad, who may benefit from further sleep-specific medical support and/or quantitative sleep assessment. The data reinforce the need for player and staff education regarding the importance of sleep relative to various aspects of athlete development, training, competition, recovery and health, and the need for regular sleep focused screening, monitoring and assessment within athletes; particularly within team sports athletes. Miles et al20 identified barriers to such an approach (mainly lack of resources, busy schedule and lack of knowledge of sleep hygiene) to promote/incorporate healthy sleep behaviour among soccer teams. Providing player and practitioner focused palatable educational resources may facilitate building a culture of healthy sleep behaviours and hygiene within a soccer team environment.
Conclusion
The data demonstrate players had insufficient sleep duration yet good sleep efficiency, but struggle with poor sleep quality, insomnia and daytime sleepiness. Education of the players and their support network regarding the outlined positive influence appropriate sleep can have on various athletic performance and recovery centric agendas outlined above appears prudent, particularly within the present population. This easily administrable qualitative questionnaire battery may offer a practically compatible first-step (triage) towards identifying sleep issues within large squads of players, allowing economical prescription of further quantitative assessment of valid player subsets.
Acknowledgments
We thank all QSL team players and staff for volunteering their participation within the present study, without which the project would not have been possible.
Footnotes
LT and FEM contributed equally.
Contributors: KK, AF and CPH contributed to experimental design and data collection. KK and AF did the data analysis. All authors contributed to the manuscript drafting, revising critically for important intellectual content and agreed to the submitted version of the manuscript.
Funding: The publication of this article was funded by the Qatar National Library.
Competing interests: None declared.
Patient consent for publication: Not required.
Ethics approval: The study was approved by the IRB at Aspetar and the Shafallah Medical Genetics Centre (Doha, Qatar) (IRB No: 2012-00X).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Data are available upon reasonable request.
References
- 1. Mah CD, Mah KE, Kezirian EJ, et al. The effects of sleep extension on the athletic performance of collegiate basketball players. Sleep 2011;34:943–50. 10.5665/SLEEP.1132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Luke A, Lazaro RM, Bergeron MF, et al. Sports-related injuries in youth athletes: is overscheduling a risk factor? Clin J Sport Med 2011;21:307–14. 10.1097/JSM.0b013e3182218f71 [DOI] [PubMed] [Google Scholar]
- 3. Milewski MD, Skaggs DL, Bishop GA, et al. Chronic lack of sleep is associated with increased sports injuries in adolescent athletes. J Pediatr Orthop 2014;34:129–33. 10.1097/BPO.0000000000000151 [DOI] [PubMed] [Google Scholar]
- 4. Drew MK, Raysmith BP, Charlton PC. Injuries impair the chance of successful performance by sportspeople: a systematic review. Br J Sports Med 2017;51:1209–14. 10.1136/bjsports-2016-096731 [DOI] [PubMed] [Google Scholar]
- 5. Hausswirth C, Louis J, Aubry A, et al. Evidence of disturbed sleep and increased illness in overreached endurance athletes. Med Sci Sports Exerc 2014;46:1036–45. 10.1249/MSS.0000000000000177 [DOI] [PubMed] [Google Scholar]
- 6. Smith TJ, Wilson MA, Karl JP, et al. Impact of sleep restriction on local immune response and skin barrier restoration with and without 'multi-nutrient' nutrition intervention. J Appl Physiol 1985;2017 jap.00547.2017. [DOI] [PubMed] [Google Scholar]
- 7. Curcio G, Ferrara M, De Gennaro L. Sleep loss, learning capacity and academic performance. Sleep Med Rev 2006;10:323–37. 10.1016/j.smrv.2005.11.001 [DOI] [PubMed] [Google Scholar]
- 8. Sivertsen B, Glozier N, Harvey AG, et al. Academic performance in adolescents with delayed sleep phase. Sleep Med 2015;16:1084–90. 10.1016/j.sleep.2015.04.011 [DOI] [PubMed] [Google Scholar]
- 9. Taylor L, Chrismas BCR, Dascombe B, et al. The importance of monitoring sleep within adolescent athletes: athletic, academic, and health considerations. Front Physiol 2016;7 10.3389/fphys.2016.00101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hirshkowitz M, Whiton K, Albert SM, et al. National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health 2015;1:40–3. 10.1016/j.sleh.2014.12.010 [DOI] [PubMed] [Google Scholar]
- 11. BaHammam A, Alkhunizan M, Lesloum R, et al. Prevalence of sleep-related accidents among drivers in Saudi Arabia. Ann Thorac Med 2014;9:236–41. 10.4103/1817-1737.140138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Merdad RA, Merdad LA, Nassif RA, et al. Sleep habits in adolescents of Saudi Arabia; distinct patterns and extreme sleep schedules. Sleep Med 2014;15:1370–8. 10.1016/j.sleep.2014.06.008 [DOI] [PubMed] [Google Scholar]
- 13. Farooq A, Herrera CP, Almudahka F, et al. A prospective study of the Physiological and neurobehavioral effects of Ramadan fasting in Preteen and teenage boys. J Acad Nutr Diet 2015;115:889–97. 10.1016/j.jand.2015.02.012 [DOI] [PubMed] [Google Scholar]
- 14. Fowler PM, Paul DJ, Tomazoli G, et al. Evidence of sub-optimal sleep in adolescent middle Eastern Academy soccer players which is exacerbated by sleep intermission proximal to dawn. Eur J Sport Sci 2017:1–9. [DOI] [PubMed] [Google Scholar]
- 15. Buysse DJ, Reynolds CF, Monk TH, et al. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res 1989;28:193–213. 10.1016/0165-1781(89)90047-4 [DOI] [PubMed] [Google Scholar]
- 16. Bertolazi AN, Fagondes SC, Hoff LS, et al. Validation of the Brazilian Portuguese version of the Pittsburgh sleep quality index. Sleep Med 2011;12:70–5. 10.1016/j.sleep.2010.04.020 [DOI] [PubMed] [Google Scholar]
- 17. Wilkinson K, Shapiro C. Development and validation of the Nonrestorative Sleep Scale (NRSS). J Clin Sleep Med 2013;9:929–37. 10.5664/jcsm.2996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Thun E, Bjorvatn B, Flo E, et al. Sleep, circadian rhythms, and athletic performance. Sleep Med Rev 2015;23:1–9. 10.1016/j.smrv.2014.11.003 [DOI] [PubMed] [Google Scholar]
- 19. Capers PL, Fobian AD, Kaiser KA, et al. A systematic review and meta-analysis of randomized controlled trials of the impact of sleep duration on adiposity and components of energy balance. Obesity Reviews 2015;16:771–82. 10.1111/obr.12296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Miles KH, Clark B, Fowler PM, et al. Sleep practices implemented by team sport coaches and sports science support staff: a potential Avenue to improve athlete sleep? J Sci Med Sport 2019. 10.1016/j.jsams.2019.01.008. [Epub ahead of print: 19 Jan 2019]. [DOI] [PubMed] [Google Scholar]
- 21. Herrera CP. Total sleep time in Muslim football players is reduced during Ramadan: a pilot study on the standardized assessment of subjective sleep-wake patterns in athletes. J Sports Sci 2012;30(Suppl 1):S85–S91. 10.1080/02640414.2012.676666 [DOI] [PubMed] [Google Scholar]
- 22. Bener A, Al-Hamaq A. Sleep quality and excessive daytime sleepiness in a Arab diabetic population. Biomedical Research 2010;21:333–40. [Google Scholar]
- 23. Buysse DJ, Ancoli-Israel S, Edinger JD, et al. Recommendations for a standard research assessment of insomnia. Sleep 2006;29:1155–73. 10.1093/sleep/29.9.1155 [DOI] [PubMed] [Google Scholar]
- 24. Swinbourne R, Gill N, Vaile J, et al. Prevalence of poor sleep quality, sleepiness and obstructive sleep apnoea risk factors in athletes. Eur J Sport Sci 2016;16:850–8. 10.1080/17461391.2015.1120781 [DOI] [PubMed] [Google Scholar]
- 25. Johns MW, sleepiness D. Snoring, and obstructive sleep apnea. the Epworth Sleepiness Scale. Chest 1993;103:30–6. [DOI] [PubMed] [Google Scholar]
- 26. Johns MW. A new method for measuring daytime sleepiness: the Epworth Sleepiness Scale. Sleep 1991;14:540–5. 10.1093/sleep/14.6.540 [DOI] [PubMed] [Google Scholar]
- 27. Kumar S. Bhatia M Fau - Behari M, Behari M. Excessive daytime sleepiness in Parkinson's disease as assessed by Epworth Sleepiness Scale (ESS). Sleep Med 2003;4:339–42. [DOI] [PubMed] [Google Scholar]
- 28. Bastien CH. Vallieres A Fau - Morin CM, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med 2001;2:297–307. [DOI] [PubMed] [Google Scholar]
- 29. Postolache TT, Hung T-M, Rosenthal RN, et al. Sports chronobiology consultation: from the lab to the arena. Clin Sports Med 2005;24:415–56. xiv 10.1016/j.csm.2005.01.001 [DOI] [PubMed] [Google Scholar]
- 30. Van Ryswyk E, Weeks R, Bandick L, et al. A novel sleep optimisation programme to improve athletes' well-being and performance. Eur J Sport Sci 2017;17:144–51. 10.1080/17461391.2016.1221470 [DOI] [PubMed] [Google Scholar]
- 31. Rijken NH, Soer R, de Maar E, et al. Increasing performance of professional soccer players and elite track and field athletes with peak performance training and biofeedback: a pilot study. Appl Psychophysiol Biofeedback 2016;41:421–30. 10.1007/s10484-016-9344-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. FTdS B, Barbosa DG, Andrade RD, et al. Sleep and musculoskeletal complaints among elite athletes of SANTA Catarina. Revista Dor 2015;16:102–8. [Google Scholar]
- 33. Al-Mohannadi AS, Farooq A, Burnet A, et al. Impact of climatic conditions on physical activity: a two-year cohort study in the Arabian Gulf region. JPAH 2016. 10.1123/jpah.0593 [DOI] [PubMed] [Google Scholar]
- 34. Atkinson G, Reilly T. Circadian variation in sports performance. Sports Med 1996;21:292–312. 10.2165/00007256-199621040-00005 [DOI] [PubMed] [Google Scholar]
- 35. Cunniffe B, Hore AJ, Whitcombe DM, et al. Time course of changes in immuneoendocrine markers following an international rugby game. Eur J Appl Physiol 2010;108:113–22. 10.1007/s00421-009-1200-9 [DOI] [PubMed] [Google Scholar]
- 36. Roky R, Iraki L, HajKhlifa R, et al. Daytime alertness, mood, psychomotor performances, and oral temperature during Ramadan intermittent fasting. Ann Nutr Metab 2000;44:101–7. 10.1159/000012830 [DOI] [PubMed] [Google Scholar]
- 37. Vgontzas AN, Chrousos GP, Sleep CGP. Sleep, the hypothalamic-pituitary-adrenal axis, and cytokines: multiple interactions and disturbances in sleep disorders. Endocrinol Metab Clin North Am 2002;31:15–36. 10.1016/S0889-8529(01)00005-6 [DOI] [PubMed] [Google Scholar]
- 38. Shorten AL, Wallman KE, Guelfi KJ. Acute effect of environmental temperature during exercise on subsequent energy intake in active men. Am J Clin Nutr 2009;90:1215–21. 10.3945/ajcn.2009.28162 [DOI] [PubMed] [Google Scholar]
- 39. Wasse LK, King JA, Stensel DJ, et al. Effect of ambient temperature during acute aerobic exercise on short-term appetite, energy intake, and plasma acylated ghrelin in recreationally active males. Appl Physiol Nutr Metab 2013;38:905–9. 10.1139/apnm-2013-0008 [DOI] [PubMed] [Google Scholar]
- 40. Fullagar HHK, Duffield R, Skorski S, et al. Sleep and recovery in team sport: current sleep-related issues facing professional Team-Sport athletes. Int J Sports Physiol Perform 2015;10:950–7. 10.1123/ijspp.2014-0565 [DOI] [PubMed] [Google Scholar]
- 41. Fullagar HHK, Skorski S, Duffield R, et al. Sleep and athletic performance: the effects of sleep loss on exercise performance, and physiological and cognitive responses to exercise. Sports Med 2015;45:161–86. 10.1007/s40279-014-0260-0 [DOI] [PubMed] [Google Scholar]
- 42. Faraut B, Nakib S, Drogou C, et al. Napping reverses the salivary interleukin-6 and urinary norepinephrine changes induced by sleep restriction. J Clin Endocrinol Metab 2015;100:E416–E426. 10.1210/jc.2014-2566 [DOI] [PubMed] [Google Scholar]
- 43. Thornton HR, Delaney JA, Duthie GM, et al. Effects of Pre-Season training on the sleep characteristics of professional Rugby League players. Int J Sports Physiol Perform 2017:1–23. [DOI] [PubMed] [Google Scholar]
- 44. Thornton HR, Duthie GM, Pitchford NW, et al. Effects of a two-week high intensity training cAMP on sleep activity of professional Rugby League athletes. Int J Sports Physiol Perform 2016:1–19. [DOI] [PubMed] [Google Scholar]
- 45. Pitchford NW, Bishop DJ, Bartlett JD. Resting to recover: influence of sleep extension on recovery following high-intensity exercise. Ruhr, Germany: European College of Sport Science Annual Congress, 2017. [Google Scholar]
- 46. Simpson NS, Gibbs EL, Matheson GO. Optimizing sleep to maximize performance: implications and recommendations for elite athletes. Scand J Med Sci Sports 2017;27:266–74. 10.1111/sms.12703 [DOI] [PubMed] [Google Scholar]
- 47. Bliwise DL, Holm-Larsen T, Goble S. Increases in duration of first uninterrupted sleep period are associated with improvements in PSQI-measured sleep quality. Sleep Med 2014;15:1276–8. 10.1016/j.sleep.2014.05.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Weiss JP, Herschorn S, Albei CD, et al. Efficacy and safety of low dose desmopressin orally disintegrating tablet in men with nocturia: results of a multicenter, randomized, double-blind, placebo controlled, parallel group study. J Urol 2013;190:965–72. 10.1016/j.juro.2012.12.112 [DOI] [PubMed] [Google Scholar]
- 49. Dijk DJ, Duffy JF, Czeisler CA. Contribution of circadian physiology and sleep homeostasis to age-related changes in human sleep. Chronobiol Int 2000;17:285–311. 10.1081/CBI-100101049 [DOI] [PubMed] [Google Scholar]
- 50. Bongers CCWG, Hopman MTE, Eijsvogels TMH. Cooling interventions for athletes: an overview of effectiveness, physiological mechanisms, and practical considerations. Temperature 2017;4:60–78. 10.1080/23328940.2016.1277003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Ihsan M, Watson G, Abbiss CR. What are the physiological mechanisms for post-exercise cold water immersion in the recovery from prolonged endurance and intermittent exercise? Sports Med 2016;46:1095–109. 10.1007/s40279-016-0483-3 [DOI] [PubMed] [Google Scholar]
- 52. Stephens JM, Halson S, Miller J, et al. Cold-water immersion for athletic recovery: One size does not fit all. Int J Sports Physiol Perform 2017;12:2–9. 10.1123/ijspp.2016-0095 [DOI] [PubMed] [Google Scholar]
- 53. Burke LM, King C. Ramadan fasting and the goals of sports nutrition around exercise. J Sports Sci 2012;30(Suppl 1):S21–S31. 10.1080/02640414.2012.680484 [DOI] [PubMed] [Google Scholar]
- 54. Whitworth-Turner C, Di Michele R, Muir I, et al. A shower before bedtime may improve the sleep onset latency of youth soccer players. Eur J Sport Sci 2017;17:1119–28. 10.1080/17461391.2017.1346147 [DOI] [PubMed] [Google Scholar]
- 55. Chen Y, Kartsonaki C, Clarke R, et al. Characteristics and correlates of sleep duration, daytime napping, snoring and insomnia symptoms among 0.5 million Chinese men and women. Sleep Medicine 2018;44:67–75. 10.1016/j.sleep.2017.11.1131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Taylor L, Chrismas BCR, Dascombe B, et al. Sleep medication and athletic Performance—The evidence for practitioners and future research directions. Front Physiol 2016;7 10.3389/fphys.2016.00083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Claudino JG, J Gabbett T, de Sá Souza H, et al. Which parameters to use for sleep quality monitoring in team sport athletes? A systematic review and meta-analysis. BMJ Open Sport Exerc Med 2019;5:e000475 10.1136/bmjsem-2018-000475 [DOI] [PMC free article] [PubMed] [Google Scholar]


