Abstract
Objectives
We aimed to prospectively evaluate the prevalence of long-standing groin pain and related MRI findings in contact sports.
Methods
This case–control study followed three male elite-level soccer, ice-hockey and bandy teams (102 players) for 2 years. All athletes with long-standing groin pain lasting >30 days and age-matched controls (1:3) from the same teams were examined clinically, using pelvic MRI and Hip and Groin Outcome Scores (HAGOS). Primary outcome measures were annual prevalence of groin pain and underlying MRI findings.
Results
The annual prevalence of chronic groin pain was 7.5%. Training characteristics and pain scores of athletes were similar in all teams. On MRI, there was no significant difference in the percentage of pubic bone marrow oedema (p = 0.80) between symptomatic players (8/15; 53%) versus controls (20/43; 47%), but adductor tendinopathy and degenerative changes at the pubic symphysis were twice more common among players with pain. Rectus muscle or iliopsoas pathology were seldom observed. Lower HAGOS subscales (p < 0.01) were recorded in players who experienced groin pain compared with the controls.
Conclusion
Long-standing groin pain was observed annually in 1 of 14 athletes in contact sports. Abnormalities in the pubic symphysis were common MRI findings in both symptomatic and asymptomatic players.
Trial registration number
Keywords: groin, injuries, MRI
What are the findings?
The annual prevalence of long-standing groin pain was 7.5%.
The percentage of pubic bone marrow oedema in MRI was 50% in both symptomatic and asymptomatic players, that is, it did not correlate well with groin pain.
Other pathological MRI findings at the pubic symphysis were also common in both symptomatic and asymptomatic players.
How might it impact on clinical practice in the near future?
MRI is often used in the diagnostic workup of athletes with long-standing groin pain.
Positive MRI findings do not necessarily correlate with long-standing groin pain.
Introduction
In retrospective cohort studies, the prevalence of long-standing groin pain ranges between 5% and 10% in athletes and the season incidence is nearly 7%.1–3 Common causes include tendinopathies of adductor, iliopsoas or rectus abdominis muscles, protrusion of the posterior wall of inguinal canal (‘sportsman’s hernia’) or impingement of the hip joint.1–5 Sometimes, a multidisciplinary investigation may reveal simultaneous multiple reasons.6 7 First-line management includes rest, physiotherapy, anti-inflammatory analgesics, local corticosteroid injections or seldom operative management.8 9
Athletes with long-standing groin pain often display characteristic MRI findings.3 10–12 Four main radiological abnormalities appear consistently in the symptomatic groin: degenerative changes at the pubic symphyseal joint, pathology at the adductor muscle insertion, pubic bone marrow oedema (BME) and a secondary cleft sign.11 These MRI findings may also appear in pain-free players.12–15 In some cases, only posterior inguinal wall deficiency is observed on ultrasonography.8 16 In the present prospective case–control study, we aimed to investigate the annual prevalence of long-standing groin pain in three contact sport clubs and define the exact diagnosis behind groin symptoms using clinical investigation and MRI.
Methods
Patients
Three elite-level male contact sport teams (soccer, ice-hockey and bandy) including 102 players were invited to join into this prospective observational case–control study. All players aged >18 years were followed for 2 years from August 2015 to July 2017 to find out the prevalence of long-standing groin pain (>30 days). The symptomatic athletes and their controls (ratio 1:3) matched by same sport, age and athletic exposure were included (figure 1). Control athletes were hip and groin injury free for last 6 months.
Figure 1.
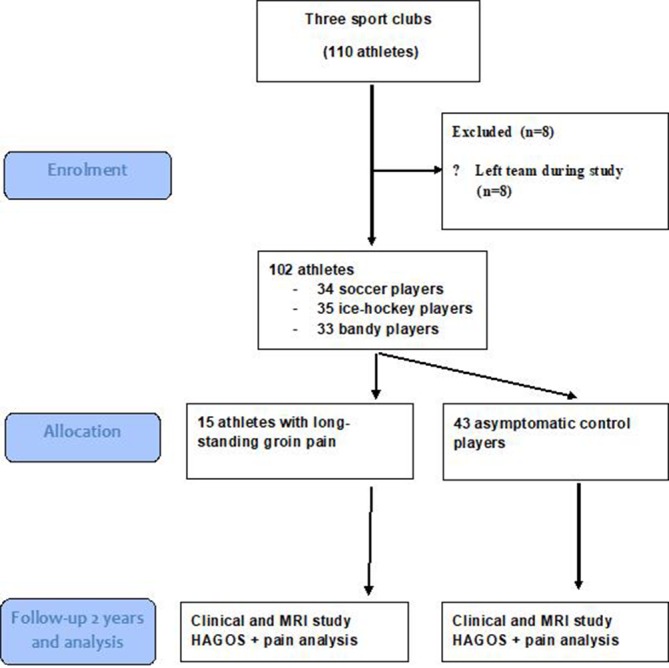
Flow diagram of the study. HAGOS, Hip and Groin Outcome Scores.
The aetiology and diagnosis of long-standing groin pain were always based on patient history, physical examination and MR imaging. The location of groin pain (visual analogue pain scores, VAS≥3; range 0–10) had to be in the lower abdomen near the inguinal ligament with or without tenderness over the pubic symphysis or at the proximal insertion of adductors. Pain scores (VAS) during rest and exercise were carefully recorded at the initiation of pain and weekly after that until recovery. Clinical examination findings were divided according to Doha agreement meeting (adductor-related, inguinal-related, pubic related, iliopsoas-related, hip-related groin pain).16
The main endpoint was the annual prevalence of long-standing groin pain in each team. Other outcome measures were VAS scores and exact clinical as well as MRI findings. Hip and Groin Outcome Score (HAGOS) Questionnaire was used to determine the severity of groin injuries.17 All participants (15 symptomatic vs 43 asymptomatic control players) underwent identical standardised and reliable clinical examination, HAGOS questionnaire and MRI scans (1.5 Tesla) of the pelvis.
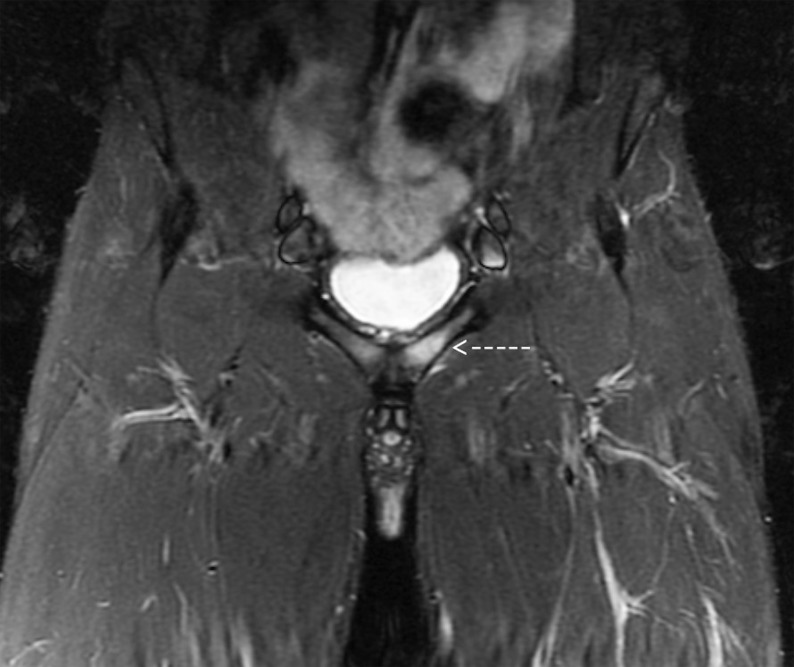
MRI
Athletes were imaged using a 1.5 Tesla MRI system (GE Healthcare 1.5 T Optima MR360, Chicago, Illinois, USA), and participants lying supine with a surface coil centred at the pubic symphysis and covering the pelvic area. The MRI was performed using routine T1-weighed and T2-weighted and short T1 inversion recovery, that is, STIR sequences (coronal and axial STIR; TR 4000 ms and TE 42/50 ms; slice thickness 5 mm). T1-weighted sequence was fast spin echo (FSE) TI 150/170 (coronal T1 FSE and axial T1 FSE; TR 490 ms and TE minFull; slice thickness 4 mm/5 mm). The duration of abdominal MRI was typically 40–50 min. Abnormal findings in the pelvic MRI including BME, an increased signal or tear from the insertion of the adductor, iliopsoas, rectus abdominis or other pelvic muscles were recorded. Pubic BME was graded as 0 (no oedema), I (mild, <1 cm), II (moderate, 1–2 cm) or III (heavy, >2 cm; figure 2). Other recorded pubic MR findings included fatty infiltration around the symphysis, secondary cleft sign and sclerosis/cysts/erosion or disc herniation at the pubic symphysis.15 18 Hip pathologies (excessive intra-articular fluid, labrum tears, impingement) were also recorded. All MRI scans were reviewed independently by two experienced radiologists (SB and HH), blinded to all clinical information on study participants.
Figure 2.
Pubic bone marrow oedema in MRI was graded as 0 (no oedema), I (mild, <1 cm), II (moderate, 1–2 cm) or III (heavy,>2 cm).
Ethics
Checklist of items of case–control cohort studies (Strengthening the Reporting of Observational Studies in Epidemiology statement; http://www.strobe-statement.org) was followed when reporting the data. All participants provided written informed consent according to the Helsinki Declaration. The project was approved by the local ethical committee on health research and registered into Clinical Trials (ClinicalTrials.gov identifier: NCT02560480).
The statistical analysis was carried out by using SPSS for Windows, V.20.0 (IBM SPSS, Chicago, IL, USA). Statistical evaluation was performed using Fisher’s exact test between the groups. The comparison between median VAS scores was analysed using Student’s t-test or analysis of variance. A p value of <0.05 was regarded as significant for both tests. 95% CI was reported when evaluating the HAGOS data.
Results
The prevalence of long-standing groin pain was 15/102 players (annually 7.5 %). Groin pain was reported in 6, 7 and 2 soccer, ice-hockey and bandy players, respectively (table 1). Acute or subacute (<30 days) groin injuries were two times to three times more frequent than long-standing symptoms. Except higher median age of bandy players and higher body mass index in ice-hockey players, duration of groin symptoms, pain scores and training characteristics were rather similar in all teams. The annual number of games was almost double in ice-hockey league compared with other contact sports (table 1).
Table 1.
Characteristics of male athletes with (n=15) or without (n=43) long-standing groin pain
| Soccer (n=22) | Ice-hockey (n=23) | Bandy (n=13) | P value* | ||||
| Pain group | Controls | Pain group | Controls | Pain group | Controls | ||
| Number of athletes | 6 | 16 | 7 | 16 | * | 11 | 0.6011 |
| Age (years, median ±SD) | 23±5.1 | 22±2.2 | 27±7.4 | 25±6.5 | 31±0.7 | 28±3.2 | 0.0033 |
| BMI (kg/cm2, median ±SD) | 23±1.1 | 23±1.4 | 26±1.7 | 25±2.0 | 25±1.8 | 23±0.8 | 0.0116 |
| Symptoms (months, median ±SD) | 4.0±1.4 | – | 3.1±1.0 | – | 3.5±1.6 | – | 0.4495 |
| Pain scores (0–100, median ±SD) | 5.3±2.2 | 0.8±0.9 | 5.7±0.9 | 1.1±0.9 | 6.5±0.7 | 0.1±0.1 | 0.6502 |
| Right/left/bilateral pain* | 2/4/0 | – | 2/4/1 | – | 2/0/0 | – | 0.4324 |
| Length of training season (months) | 6 | 4 | 4 | 0.82 | |||
| Length of competing season (months) | 6 | 8 | 8 | 0.8894 | |||
| Training per week (hours) | 10–15 | 12–15 | 8–12 | 0.6855 | |||
| Number of games/year: | 40 | 70 | 35 | 0.0017 | |||
*P values are distributed between different sports.
BMI, body mass index; VAS, visual analoque score.
The prevalence of BME was equal in the symptomatic versus asymptomatic players (8/15; 53% vs 20/43; 47 %, p=0.799). Table 2 shows the prevalence of BME in absolute numbers in soccer (5/6 vs 8/16), ice-hockey (2/7 vs 9/16) and in bandy (1/2 vs 3/11) in the symptomatic versus asymptomatic players, respectively. There were no statistically significant differences in the percentage of BME between symptomatic and asymptomatic players.
Table 2.
BME at the pubic symphysis on MRI scans in male athletes with (n=15) or without (n=43) long-standing groin pain in different sports
| Group | BME (%) | Grade of BME | |||
| 0 | I (<1 cm) | II (1–2 cm) | III (>2 cm) | ||
| Groin pain ( n = 15 ): | |||||
| Soccer (n=6) | 5/6 (83) | 1 | 1 | 2 (1 bilateral) | 2 bilateral |
| Ice-hockey(n=7) | 2/7 (29) | 5 | 0 | 1 bilateral | 1 bilateral |
| Bandy (n=2) | 1/2 (50) | 1 | 1 | 0 | 0 |
| Controls ( n = 43 ): | |||||
| Soccer (n=16) | 8/16 (50) | 8 | 5 | 3 (1 bilateral) | 0 |
| Ice-hockey(n=16) | 9/16 (56) | 7 | 5 | 3 | 1 |
| Bandy (n=11) | 3/11 (27) | 8 | 3 | 0 | 0 |
BME, bone marrow oedema.
Long-standing groin pain was related either to adductors (n=5), inguinal canal (n=6), pubic symphysis (n=6) or hip/iliopsoas area (n=3). Only one symptomatic soccer player had a normal pelvic MRI. All others had multiple abnormalities on their MRI scans (table 3). Adductor tendinopathy and degenerative changes at the symphysis pubis were almost twice as frequent in symptomatic versus in pain-free athletes (table 3, figure 3). Rectus or iliopsoas pathologies were rare in both groups (table 3). Pelvic MRI revealed three other types of muscular injuries in the symptomatic group (two proximal hamstring injuries in ice-hockey and bandy player, one sartorius injury in soccer). Two control players from the ice-hockey team had an asymptomatic gluteus medius muscle injury and obturator externus injury at MRI. There were lower HAGOS subscales in ice-hockey and soccer players who experienced hip and/or groin pain than in controls (table 4).
Table 3.
Abnormal MRI findings in male athletes with (n=15) or without (n=43) long-standing groin pain in different sports.
| Total | Soccer | Ice-hockey | Bandy | ||||
| Pain/control | Pain group* | Controls† | Pain group* | Controls† | Pain group* | Controls† | |
| Adductor tendinopathy | 9/4 | 3 | 2 | 5 | 2 | 1 | 0 |
| Fat infiltration at pubis | 9/4 | 4 | 2 | 4 | 1 | 1 | 1 |
| Secondary cleft sign | 8/5 | 4 | 2 | 3 | 3 | 1 | 0 |
| Sclerosis/cysts/ erosion at the PS | 13/9 | 5 | 4 | 7 | 5 | 1 | 0 |
| Disc herniation | 11/16 | 5 | 2 | 4 | 4 | 2 | 0 |
| Rectus tendinopathy | 1/2 | 0 | 0 | 1 | 2 | 0 | 0 |
| Iliopsoas pathology | 2/0 | 1 | 0 | 1 | 0 | 0 | 0 |
| Other muscle pathology | 3/2 | 1 | 0 | 1 | 2 | 1 | 0 |
| Hip pathology | 2/1 | 1 | 0 | 1 | 1 | 0 | 0 |
*Pain group means athletes with long-standing groin pain.
†Control group means athletes without long-standing groin pain.
PS, pubic symphysis.
Figure 3.
An MRI (STIR sequence) of symptomatic soccer player groin. Grade III bone marrow oedema (arrow) is demonstrated in the left pubic symphysis with an adductor longus injury (bright signal below pubic bone).
Table 4.
HAGOS scores in asymptomatic soccer versus ice-hockey players compared with players with long-standing groin/hip pain
| HAGOS | Asymptomatic | Groin/hip pain | P value* |
| Median (25th–75th) | Median (25th–75th) | ||
| Soccer | |||
| Pain | 100 (100–100) | 98 (93–100) | <0.01 |
| Symptoms | 89 (77–97) | 78 (76–90) | <0.01 |
| ADL | 100 (100–100) | 98 (93–100) | <0.01 |
| Sport/Rec | 96 (92–100) | 81 (67–94) | <0.01 |
| PA | 100 (100–100) | 99 (94–100) | <0.01 |
| QL | 98 (95–100) | 90 (87–98) | <0.01 |
| Ice-hockey | |||
| Pain | 100 (97–100) | 90 (85–95) | <0.01 |
| Symptoms | 89 (78–94) | 61 (57–82) | <0.01 |
| ADL | 100 (97–100) | 90 (85–95) | <0.01 |
| Sport/Rec | 90 (88–96) | 75 (62–95) | <0.01 |
| PA | 98 (97–100) | 97 (90–98) | <0.01 |
| QL | 95 (94–100) | 87 (85–95) | <0.01 |
*P values are distributed between asymptomatic and symptomatic athletes in soccer and ice-hockey.
ADL, activities in daily living; HAGOS, Hip and Groin Outcome Score; PA, participation in physical activity; QL, quality of living; Sport/Rec, sport and recreational activities.
Discussion
Main outcome
Our study indicated that an annual prevalence of groin pain was 7.5%. This is less than reported previously in Denmark from subelite soccer teams.19 In that study, 695 soccer players from 40 teams (divisions 1–4), some 49% (95% CI: 45% to 52%) reported hip or groin pain during the previous season. Of these, 31% (95% CI: 26% to 36%) reported pain for >6 weeks. In another study, 190 players from nine Dutch professional soccer clubs reported severe groin symptoms in 24% and within-season incidence of groin injury in 11%.20 One retrospective register study from Finland reported groin injuries in 9.0% of elite soccer players.6 The difference in prevalence rates of groin pain between our study and others may be due to different level of studied athletes (elite vs sub-elite levels). Furthermore, season incidence of pain is always lower than whole year incidence.
The present study extends previous reports that positive MRI findings were common in both symptomatic and asymptomatic athletes in contact sports. Reactive changes (oedema) in the symphysis pubis may be as a consequence of overuse or subclinical contact injury particularly in soccer and ice-hockey and very often represent painless findings.12 13 In bandy players, the direct pelvic contact occurs more seldom than in ice-hockey and therefore groin injuries may be less frequently observed. Radiographical findings at the symphysis are often observed as reactive sclerosis at the pubic symphysis.13 21 A recent 18-month follow-up trial reported that extensive BME on STIR sequences may predict a poor clinical outcome, that is, the athletes with extensive BME recovered less likely to high-level sports activity.22 In contrast to this, we found that BME was as common in symptomatic as in asymptomatic players.
Four clinical entities involved in the long-standing groin pain were recently described as pubic-, adductor-, inguinal canal- (with or without rectus abdominis injuries) and iliopsoas-related groin pain.15 16 The advantage of pelvic MRI is to detect concurrent injuries, as in our study (proximal hamstring, rectus femoris or gluteal muscle tears). Laxity of the posterior wall of the inguinal canal can be studied clinically using finger/coughing test, by ultrasound or by using fast MRI sequence with Valsalva maneuver.23 24 Asymptomatic MRI findings (tendinosis, calcifications, cortical erosions) are common in athletes and care should be taken when assessing the MRI abnormalities versus groin pain.25 We still need well-designed controlled studies to find out how many asymptomatic athletes have adductor-related changes in MRI or weakness of the posterior wall without any relation of groin pain ever.26 27
Limitations
A limitation of our study was the small number of patients from three different sports. The strengths of this study are the prospective data collection including standardised MRI, as well as a relatively long follow-up period. Furthermore, the MRI scans were blindly reviewed by two experienced musculoskeletal radiologists. Minimum reporting standards on radiology of long-standing groin pain were followed carefully in our study.11 15 18 27 The majority of MRI studies have focused on its use for pubic and adductor-related groin pain.11 28 29 There are very few studies examining the use of MRI in iliopsoas or inguinal canal-related groin pain in athletes. Branci et al developed recently a standardised MRI evaluation protocol (Copenhagen Standardised MRI protocol) for use in athletes with groin pain.15 18 Ducouret et al utilised axial and coronal T1-weighted, axial-oblique proton density weighted with fat saturation (in symphysis plane), gadolinium contrast enhancement and Valsalva maneuver.24 They found that MRI has diagnostic accuracy of 78%, 100% sensitivity, 69% specificity in evaluating long-standing groin pain when compared with surgical findings. This means that at present, we are not aware 100% how well pathological MRI correlates to long-standing groin pain and particularly surgical pathologies.
Conclusion
Long-standing groin pain has an annual prevalence of 7.5%. The percentage of BME was 50% in both symptomatic and asymptomatic players, and it does not correlate well to groin pain.
Acknowledgments
We thank the volunteer asymptomatic athletes who participated in the MRI study and our MRI department for high-quality imaging service.
Footnotes
Contributors: HP was responsible for the conception and design of the study, recruitment of participants, data collection and drafting. HH and SB contributed to interpretation of the radiological findings and had full access to all data. LR contributed to interpretation of the data and revision of the manuscript. The final manuscript was approved by all authors.
Funding: This trial was financially supported by the Competitive State Research Financing of the Expert Responsibility Area of Kuopio University Hospital. Financial support was also received from Orton Orthopaedic Hospital, Helsinki, Finland (the Ministry of Social Affairs and Health grant, 9310/478).
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; internally peer reviewed.
References
- 1. Litwin DEM, Sneider EB, McEnaney PM, et al. Athletic pubalgia (sports hernia). Clin Sports Med 2011;30:417–34. 10.1016/j.csm.2010.12.010 [DOI] [PubMed] [Google Scholar]
- 2. Nam A, Brody F. Management and therapy for sports hernia. J Am Coll Surg 2008;206:154–64. 10.1016/j.jamcollsurg.2007.07.037 [DOI] [PubMed] [Google Scholar]
- 3. Gouttebarge V, Veenstra E, Goedegebuure S, et al. Professional football players at risk for non-acute groin injuries during the first half of the season: a prospective cohort study in the Netherlands. J Back Musculoskelet Rehabil 2018;31:15–21. 10.3233/BMR-150427 [DOI] [PubMed] [Google Scholar]
- 4. Swan KG, Wolcott M. The athletic hernia: a systematic review. Clin Orthop Relat Res 2007;455:78–87. 10.1097/BLO.0b013e31802eb3ea [DOI] [PubMed] [Google Scholar]
- 5. Rankin AT, Bleakley CM, Cullen M. Hip joint pathology as a leading cause of groin pain in the sporting population: a 6-year review of 894 cases. Am J Sports Med 2015;43:1698–703. 10.1177/0363546515582031 [DOI] [PubMed] [Google Scholar]
- 6. Paajanen H, Ristolainen L, Turunen H, et al. Prevalence and etiological factors of sport-related groin injuries in top-level soccer compared to non-contact sports. Arch Orthop Trauma Surg 2011;131:261–6. 10.1007/s00402-010-1169-1 [DOI] [PubMed] [Google Scholar]
- 7. Smedberg SG, Broome AE, Gullmo A, et al. Herniography in athletes with groin pain. Am J Surg 1985;149:378–82. 10.1016/S0002-9610(85)80112-4 [DOI] [PubMed] [Google Scholar]
- 8. Minnich JM, Hanks JB, Muschaweck U, et al. Sports hernia: diagnosis and treatment highlighting a minimal repair surgical technique. Am J Sports Med 2011;39:1341–9. 10.1177/0363546511402807 [DOI] [PubMed] [Google Scholar]
- 9. Paajanen H, Brinck T, Hermunen H, et al. Laparoscopic surgery for chronic groin pain in athletes is more effective than nonoperative treatment: a randomized clinical trial with magnetic resonance imaging of 60 patients with sportsman's hernia (athletic pubalgia). Surgery 2011;150:99–107. 10.1016/j.surg.2011.02.016 [DOI] [PubMed] [Google Scholar]
- 10. Davies AG, Clarke AW, Gilmore J, et al. Review: imaging of groin pain in the athlete. Skeletal Radiol 2010;39:629–44. 10.1007/s00256-009-0768-9 [DOI] [PubMed] [Google Scholar]
- 11. Branci S, Thorborg K, Nielsen MB, et al. Radiological findings in symphyseal and adductor-related groin pain in athletes: a critical review of the literature. Br J Sports Med 2013;47:611–9. 10.1136/bjsports-2012-091905 [DOI] [PubMed] [Google Scholar]
- 12. Daigeler A, Belyaev O, Pennekamp WH, et al. MRI findings do not correlate with outcome in athletes with chronic groin pain. J Sports Science and Med 2007;6:71–6. [PMC free article] [PubMed] [Google Scholar]
- 13. Lovell G, Galloway H, Hopkins W, et al. Osteitis pubis and assessment of bone marrow edema at the pubic symphysis with MRI in an elite junior male soccer squad. Clin J Sport Med 2006;16:117–22. 10.1097/00042752-200603000-00006 [DOI] [PubMed] [Google Scholar]
- 14. Paajanen H, Hermunen H, Karonen J. Pubic magnetic resonance imaging findings in surgically and conservatively treated athletes with osteitis pubis compared to asymptomatic athletes during heavy training. Am J Sports Med 2008;36:117–21. 10.1177/0363546507305454 [DOI] [PubMed] [Google Scholar]
- 15. Branci S, Thorborg K, Bech BH, Hojlund BB, et al. MRI findings in soccer players with long-standing adductor-related groin pain and asymptomatic controls. Br J Sports Med 2015;49:681–91. 10.1136/bjsports-2014-093710 [DOI] [PubMed] [Google Scholar]
- 16. Weir A, Brukner P, Delahunt E, et al. Doha agreement meeting on terminology and definitions in groin pain in athletes. Br J Sports Med 2015;49:768–74. 10.1136/bjsports-2015-094869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Thorborg K, Branci S, Stensbirk F, et al. Copenhagen hip and groin outcome score (HAGOS) in male soccer: reference values for hip and groin injury-free players. Br J Sports Med 2014;48:557–9. 10.1136/bjsports-2013-092607 [DOI] [PubMed] [Google Scholar]
- 18. Branci S, Thorborg K, Bech BH, et al. The Copenhagen standardised MRI protocol to assess the pubic symphysis and adductor regions of athletes: outline and intratester and intertester reliability. Br J Sports Med 2015;49:692–9. 10.1136/bjsports-2014-094239 [DOI] [PubMed] [Google Scholar]
- 19. Thorborg K, Rathleff MS, Petersen P, et al. Prevalence and severity of hip and groin pain in sub-elite male football: a cross-sectional cohort study of 695 players. Scand J Med Sci Sports 2017;27:107–14. 10.1111/sms.12623 [DOI] [PubMed] [Google Scholar]
- 20. Langhout R, Tak I, van Beijsterveldt A-M, et al. Risk factors for groin injury and groin symptoms in Elite-Level soccer players: a cohort study in the Dutch professional Leagues. J Orthop Sports Phys Ther 2018;48:704–12. 10.2519/jospt.2018.7990 [DOI] [PubMed] [Google Scholar]
- 21. Lentz SS. Osteitis pubis: a review. Obstet Gynecol Surv 1995;50:310–5. [DOI] [PubMed] [Google Scholar]
- 22. Gaudino F, Spira D, Bangert Y, et al. Osteitis pubis in professional football players: MRI findings and correlation with clinical outcome. Eur J Radiol 2017;94:46–52. 10.1016/j.ejrad.2017.07.009 [DOI] [PubMed] [Google Scholar]
- 23. Vasileff WK, Nekhline M, Kolowich PA, et al. Inguinal hernia in athletes: role of dynamic ultrasound. Sports Health 2017;9:414–21. 10.1177/1941738117717009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ducouret E, Reboul G, Dalmay F, et al. MRI in chronic groin pain: sequence diagnostic reliability compared to systematic surgical assessment. Skeletal Radiol 2018;47:649–60. 10.1007/s00256-017-2824-1 [DOI] [PubMed] [Google Scholar]
- 25. Pesquer L, Reboul G, Silvestre A, et al. Imaging of adductor-related groin pain. Diagn Interv Imaging 2015;96:861–9. 10.1016/j.diii.2014.12.008 [DOI] [PubMed] [Google Scholar]
- 26. Paajanen H, Montgomery A, Simon T, et al. Systematic review: laparoscopic treatment of long-standing groin pain in athletes. Br J Sports Med 2015;49:814–8. 10.1136/bjsports-2014-094544 [DOI] [PubMed] [Google Scholar]
- 27. Delahunt E, Thorborg K, Khan KM, et al. Minimum reporting standards for clinical research on groin pain in athletes. Br J Sports Med 2015;49:775–81. 10.1136/bjsports-2015-094839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Mullens FE, Zoga AC, Morrison WB, et al. Review of MRI technique and imaging findings in athletic pubalgia and the "sports hernia". Eur J Radiol 2012;81:3780–92. 10.1016/j.ejrad.2011.03.100 [DOI] [PubMed] [Google Scholar]
- 29. Bou Antoun M, Reboul G, Ronot M, et al. Imaging of inguinal-related groin pain in athletes. Br J Radiol 2018;91 10.1259/bjr.20170856 [DOI] [PMC free article] [PubMed] [Google Scholar]