Abstract
Ovarian cancer (OC) has the worst prognosis among all malignancy types in females worldwide according to epidemiological studies in 2017. Although radiotherapy, chemotherapy and surgical treatment are the most common treatment methods, their curative effects are not satisfactory. The present study aimed to examine the role of cluster of differentiation 44 variant 6 (CD44v6) in the molecular mechanism of the proliferation and tumorigenicity of OC cells, and provide a novel target for the clinical treatment of OC. A total of 46 clinical samples were collected, including 24 malignant ovarian tumor tissue samples and 22 benign ovarian tissue samples. Expression of CD44v6 and nuclear factor-κB (NF-κB) in these samples was detected by reverse transcription-quantitative polymerase chain reaction (RT-qPCR) and immunohistochemistry. The A2780 OC cell line was used to establish a normal control group, a negative control group and a CD44v6-small interfering (si)RNA transfection group. The expression of CD44v6 and NF-κB mRNA was detected in each group by RT-qPCR. The proliferation, invasion and migration abilities of the cells were then assessed by Transwell and colony formation assays. Additionally, immunofluorescence was used to detect nuclear NF-κB expression. CD44v6 and NF-κB mRNA expression levels were significantly increased in malignant ovarian tumor tissues, compared with normal ovarian tissues (P<0.01), and immunohistochemistry demonstrated similar results. In the CD44v6-siRNA group, NF-κB mRNA expression was significantly reduced, compared with the control and negative control (both P<0.01) groups. Transwell and colony formation assays demonstrated that the migration, invasion and colony formation abilities of OC cells in the CD44v6-siRNA group were significantly reduced, compared with the control and negative control (both P<0.01) groups. Immunofluorescence results demonstrated that the expression of NF-κB in the cytoplasm and nucleus of the CD44v6-siRNA group was also markedly reduced, compared with the other two groups. In conclusion, CD44v6 may participate in the proliferation of OC cells through activation of the NF-κB pathway and these observations may provide a novel therapeutic target for the clinical treatment of OC.
Keywords: ovarian cancer, cluster of differentiation 44 variant 6, nuclear factor-κB, invasion, migration
Introduction
Ovarian cancer (OC) affects one in every 70 females and is one of the most severe gynecologic malignancies, with a 5-year survival rate of <50% if diagnosed at a late stage in the USA between 2011 and 2015 (1). There are no notable symptoms of early OC and no effective screening tools are available (2). The majority of patients with OC are generally asymptomatic until tumor progression and metastasis occur, and >66% of tumors are already in an advanced stage upon diagnosis (3). Once clinically diagnosed as high-grade epithelial OC, treatment outcomes are poor, even following surgery and appropriate chemotherapy (4). Therefore, clarification of the key molecular events that are associated with the development of OC may provide potential molecular targets for the clinical treatment of advanced epithelial OC.
Cluster of differentiation 44 (CD44), a leukocyte differentiation antigenic determinant, is a multi-structural and multi-functional cell surface adhesion molecule that is involved in the homing, activation, movement, and cell-cell and cell-matrix interactions of lymphocytes (5,6). This molecule is widespread and has a number of subtypes, which can be divided into standard CD44s and variant CD44s (CD44v1-v10), which are involved in the regulation of numerous physiological and pathological processes (7). The key role of CD44 is to provide defense against inflammatory processes by cellular transmigration and cell signaling. Saegusa et al (8) demonstrated that CD44 can inhibition the spread and metastasis of local tumors. Additionally, a number of studies indicated that CD44 is a specific cell surface marker of cancer stem cells in certain solid tumors, including OC (9–14). Notably, studies suggested that variant CD44s are associated with the occurrence and development of various malignancies, including pancreatic (15), breast (16) and colorectal cancer (17). Among these variants, CD44v6 is the most associated with tumor invasion and metastasis (18,19).
CD44v6 has been demonstrated to be a beneficial prognostic factor of a variety of cancer types, including those of the stomach (20), head and neck (21), prostate (22) and lung (23). Additionally, investigations identified that CD44v6 may serve a vital role in tumor progression and pervasion (24–27). It has been reported that CD44v6 may participate in the metastasis of OC by mediating OC cell adhesion and migration (19). In OC, changes occurring in the extracellular environment are crucial for tumorigenesis and progression, as well as for intraperitoneal transmission (28). The extracellular matrix molecules versican and hyaluronic acid interact with CD44 and serve a pivotal role in OC metastasis (29). Certain studies demonstrated that CD44v6 is only upregulated in tumor tissues during OC cell adhesion and metastasis, indicating that CD44v6, as an adhesion molecule, may participate in OC cell adhesion and metastasis (30–32).
Nuclear factor-κB (NF-κB), a transcription factor, is widely identified in mammalian cells and is a key factor in tumor anti-apoptotic mechanisms (33). This molecule can regulate the cell cycle and facilitate cell proliferation by activating the transcription of cyclin D1 (34). Additionally, NF-κB is involved in the regulation of tumorigenesis, invasion and metastasis (35). NF-κB inhibits apoptosis via the regulation of the transcription of anti-apoptotic genes, including B-cell lymphoma (Bcl)-2, Bcl-extra large and X-linked inhibited of apoptosis (36,37). Furthermore, NF-κB can accelerate tumor invasion and metastasis by regulating matrix metalloproteinase-9 and intercellular adhesion molecule-1 expression, and by degrading the extracellular matrix (38,39). Activated or abnormally expressed NF-κB can be detected in numerous malignancy types, including leukemia, breast cancer, liver cancer and thyroid cancer (40). Sasaki et al (41) investigated gastric cancer tissues and identified that NF-κB expression is associated with tumor size, lymph node invasion, invasion depth and peritoneal metastasis. Activated NF-κB promotes the transcription of apoptotic genes, resulting in the proliferation of tumor cells. NF-κB has been demonstrated to be a pro-survival and pro-inflammatory transcription factor that can promote cancer development (42). Therefore, the specific inhibition of NF-κB is considered a potential therapeutic target. Studies reported that the use of NF-κB inhibitors, including Eriocalyxin B, may prevent the recurrence of OC (43–45).
The present study hypothesized that CD44v6 may affect the proliferation, migration and invasion of OC cells via the NF-κB pathway. To the best of our knowledge, no previous studies investigated the association between these two molecules in the molecular mechanism of OC development. Therefore, the present study detected CD44v6 and NF-κB expression in human ovarian tissues. CD44v6 gene knockout was performed in OC cells to detect the expression levels of CD44v6 and NF-κB, and examine the associations between the expression of CD44v6, and cellular proliferation, migration and invasion. The nuclear translocation of NF-κB was further detected by immunofluorescence to investigate molecules that may cause the development of OC.
Materials and methods
Tissue specimens
A total of 46 fresh surgical specimens, including 24 malignant and 22 benign ovarian neoplasms, were collected between June 2016 and February 2017. Patients with multiple tumors were excluded. All patients were female, the age range of the patients was 30–60 years and the mean age was 50±2.34 years. The Medical Ethics Committee of Medical College of Wuhan University (Wuhan, China) approved the present study and written informed consent was obtained from all participants. All tissue specimens were from primary tumors and were histologically verified by pathologists who were blind to the study at the Department of Pathology, Renmin Hospital of Wuhan University (Wuhan, China) to confirm the diagnosis, histological type and tumor grade (46).
Cells and cell culture
The human serous OC cell line A2780, obtained from the American Type Culture Collection (Manassas, VA, USA), was cultured in RPMI-1640 medium (catalog no. SH30022; HyClone; GE Healthcare Life Sciences, Logan, UT, USA) supplemented with 10% fetal bovine serum (FBS; catalog no. 141215; Hangzhou HuaAn Biotechnology Co., Ltd., Hangzhou, China), and 100 U/ml penicillin and streptomycin in a 5% CO2 atmosphere at 37°C.
Small interfering RNA (siRNA) knockdown of CD44v6
A2780 cells were transiently transfected with siRNA obtained from Shanghai Integrated Biotech Solutions Co., Ltd. (Shanghai, China). This included siRNA against CD44v6 (5′-GCCAACATTCATTCAATAC-3′) and negative control siRNA (5′-GCCTTACTTACAACAATAC-3′). siRNA (100 nM) was transfected using Lipofectamine® 2000 (catalog no. 11668019; Invitrogen; Thermo Fisher Scientific, Inc., Waltham, MA, USA), according to the manufacturer's protocol. Following transfection, the cells were incubated at 37°C in a CO2 incubator for 24 or 48 h prior to being harvested for reverse transcription-quantitative polymerase chain reaction (RT-qPCR). Stably transfected cells were maintained from wells with only one green fluorescent clone.
Immunohistochemistry
The obtained ovarian tissue was fixed in 4% paraformaldehyde for 10 h at room temperature. The tissue sections were then cut to a thickness of 0.4 cm. Paraffin slices were placed in an oven at 65°C on a baking sheet for 2 h, dewaxed in water and washed three times with PBS for 5 min each time. The slices were placed in EDTA buffer (catalog no. AS1016; Wuhan Boster Biological Technology, Ltd., Wuhan, China) for microwave antigen retrieval at medium power until boiling, then at low power until boiling at 10 min intervals. Slides were washed with PBS three times following cooling for 5 min each time. Slides were placed in 3% hydrogen peroxide solution and then incubated for 10 min at room temperature in the dark. Slides were washed with PBS three times for 5 min each time, dried and blocked with 5% bovine serum albumin (BSA; Roche Diagnostics, Basel, Switzerland; catalog no. 10735078001) for 20 min at room temperature. The BSA solution was removed and ~50 µl diluted primary antibodies against CD44v6 (catalog no. 8242; 1:50; CST Biological Reagents Co., Ltd., Shanghai, China) and NF-κB (catalog no. ab78960; 1:200; Abcam, Cambridge, UK) were added to each section overnight at 4°C. The slides were washed three times with PBS for 5 min each time. Following the removal of PBS solution, 100 µl horseradish peroxidase-labeled goat anti-rabbit IgG secondary antibody (catalog no. AS-1107; 1:200; Aspen Biotechnology Co., Ltd. Wuhan, China) was added to each section and the sections were incubated at 37°C for 50 min. The slides were washed with PBS three times for 5 min each time. The PBS solution was then removed, 3,3′-diaminobenzidine (50–100 µl) was added to each slice and color development was monitored using a light microscope (magnification, ×400). Following color development, the slide was washed with water and counterstained with hematoxylin for 2 min at room temperature. Hydrochloric acid alcohol (1%) was used for differentiation for ~1 sec and the slide was then washed with water. The slide was dehydrated using an ethanol gradient (75, 90 and 100% each for 10 min), cleared in xylene and sealed with a neutral gum seal.
RNA extraction and complementary DNA (cDNA) synthesis
For the transfected/control cells, the medium was carefully removed from the cell culture dish with a pipette and 1 ml pre-cooled PBS solution at 4°C was added. The residual medium was gently removed, PBS solution was added by pipette and 1 ml TRIzol® (catalog no. 15596-026; Invitrogen; Thermo Fisher Scientific, Inc.) was added. The solution was repeatedly pipetted around the bottom of the flask to ensure the cells were fully covered by TRIzol. Chloroform (250 µl; catalog no. 10006818; Sinopharm Chemical Reagent Co., Ltd., Shanghai, China) was added and mixed well, and then the solution was placed on ice for 10 min. The mixture was centrifuged at 4°C and 10,000 × g for 10 min. The supernatant (400 µl) was carefully transferred to a 1.5-ml Eppendorf tube and an equal volume of 4°C pre-cooled isopropanol (catalog no. 80109218; Sinopharm Chemical Reagent Co., Ltd.) was added. The solution was inverted to mix and then incubated at −20°C for 15 min. The solution was centrifuged at 4°C and 10,000 × g for 10 min. The liquid was carefully removed and 1 ml 75% ethanol, pre-cooled at 4°C, was added. The RNA was precipitated three times, and the RNA pellet was washed and centrifuged at 4°C and 10,000 × g for 5 min. The RNA was dried for 10 min, and then the ethanol was volatilized thoroughly, and 10 µl RNase-free water was added to fully dissolve the RNA.
For human tissue samples, ~100 mg of tissue was placed on ice using a sterile tool and thoroughly ground in 1 ml of pre-cooled TRIzol. The homogenate was carefully poured into a 1.5-ml Eppendorf tube and chloroform (250 µl) was added. The mixture was mixed well and incubated on ice for 5 min. The aforementioned protocol was then performed for the remaining steps of RNA extraction.
cDNA synthesis was performed using a PrimeScript™ RT reagent kit with gDNA Eraser (catalog no. RR047A; Takara Bio, Inc., Otsu, Japan), and the following reaction solution was placed on ice: 2.0 µl 5X gDNA Eraser buffer, 1.0 µl gDNA Eraser and 10.0 µl RNA, all from the PrimeScript RT reagent kit. The mixture was then placed at 42°C for 2 min and incubated at 4°C for 5 min. The following reaction solution was added to the Eppendorf tube containing RNA and placed on ice: 1.0 µl PrimeScript RT Enzyme mix I, 1.0 µl RT Primer mix, 4.0 µl 5X PrimeScript Buffer 2 and 4.0 µl RNase-free dH2O, all from the kit. The reaction solution was then placed in a PCR machine at 37°C for 15 min, 85°C for 5 sec and temporally kept at 4°C for 10 min. The reaction fixture was finally stored at −20°C.
RT-qPCR
PCR was performed using a Step One™ Real-Time PCR system (Thermo Fisher Scientific, Inc.) with the following conditions: 2 min at 50°C, followed by 40 cycles at 95°C for 10 min, 95°C for 15 sec and 60°C for 1 min. Each 10-µl reaction contained 5.0 µl SYBR® Premix Ex Taq (Takara Bio, Inc.), 0.2 µl forward primer (final concentration, 0.2 µM), 0.2 µl reverse primer (final concentration, 0.2 µM), ROX reference dye, 1.0 µl cDNA and 3.4 µl ddH2O. The threshold cycle value (Cq) was recorded for all samples for both the target gene and the reference gene GAPDH. Melt curve analysis was performed for each run. The relative gene expression of the target gene was calculated as ΔCq and was determined by subtracting the Cq of the reference gene from the Cq of the target gene. Differential expression of the target gene in the control, negative control and CD44v6 siRNA groups was calculated as ∆∆Cq (47), as determined by subtracting the ΔCq of the CD44v6 siRNA group from the ΔCq of the matched control group. Primer sequences are presented in Table I.
Table I.
Primers used for polymerase chain reaction.
| Primer | Sequence | Amplification length, bp |
|---|---|---|
| GAPDH | Forward, 5′-GGTCGGAGTCAACGGATTTG-3′ | 218 |
| Reverse, 5′-GGAAGATGGTGATGGGATTTC-3′ | ||
| CD44v6 | Forward, 5′-GCCTTTGATGGACCAATTACC-3′ | 266 |
| Reverse, 5′-TCATTCCTATTGGTAGCAGGGA-3′ | ||
| NF-κB | Forward, 5′-CGCATCCAGACCAACAACA-3′ | 208 |
| Reverse, 5′-TGCCAGAGTTTCGGTTCAC-3′ |
NF-κB, nuclear factor-κB; CD44v6, cluster of differentiation variant 6.
Colony formation assay
Monolayer-cultured A2780 cells in the logarithmic growth phase were digested with 0.25% trypsin and the suspension was pipetted until the cells were fully dispersed. Subsequently, the cells were suspended in RPMI-1640 medium with 10% FBS. The cells were then plated at a density of 300 cells/plate in 35-mm plates, which were then incubated at 37°C in an atmosphere containing 5% CO2 for ~14 days, with fresh RPMI-1640 medium with 10% FBS provided every 3 days. When macroscopic colonies appeared in the medium, the culture was terminated. Subsequently, 4% formaldehyde was added for 20 min at room temperature to fix the cells. Following two washes with PBS (pH 7.4), the cells were stained with Wright-Giemsa dye complex for 5 min at room temperature. Colonies were counted using an inverted light microscope (magnification, ×400). Colonies with >50 cells were counted. The cloning rate was calculated as follows: Clone formation rate=cloning/inoculation cells ×100%.
Cell invasion and migration assays
Matrigel was diluted (1:5) and coated on the upper surface of a polycarbonate membrane (12-mm diameter and 8-mm pore size) in a Transwell filter (EMD Millipore, Billerica, MA, USA). The transfected A2780 cells were cultured to logarithmic growth phase. The cells were digested, washed with PBS and serum-free RPMI-1640 medium, and then suspended in serum-free RPMI-1640 medium. Each group of cells (4×105) was added to the upper chamber and 500 µl RPMI-1640 containing 10% FBS was added to the lower chamber. Following incubation in a 5% CO2 incubator at 37°C for 16 h, the cells were fixed with 4% paraformaldehyde at room temperature for 20 min and stained with crystal violet at room temperature for 30 min to determine how many cells had invaded the lower surface of the filter. The invaded cells were counted by light microscope (magnification, ×400) and the mean number of cells in at least three fields per well was calculated. The experiment was repeated three times. The migration assay was similar, except that Matrigel was not added to the upper membrane.
Immunofluorescence
Firstly, the transfected A2780 cells were cultured on glass slides coated with poly-L-lysine and washed on the slides in PBS three times. The cells were then fixed in 4% paraformaldehyde for 30 min at room temperature and washed two times with PBS. The cells were then permeabilized with 0.5% Triton X-100 and 0.25% Tween 20 in TBS for 15 min, and incubated with Image iT FX Signal Enhancer (Invitrogen; Thermo Fisher Scientific, Inc.) for 30 min at room temperature in a humid chamber. Following blocking with 5% BSA for 20 min at room temperature, the cells were washed. Primary antibodies against CD44v6 (catalog no. 8242; 1:500; CST Biological Reagents Co., Ltd.) and NF-κB (catalog no. ab78960; 1:1,000; Abcam) were added and the cells were incubated overnight at 4°C. Subsequently, Alexa Fluor-conjugated secondary antibodies (CY3 labeled goat anti-rabbit, catalog no. AS-1109; 1:50; Aspen Biotechnology Co., Ltd.) were added and the cells were incubated for 1 h at room temperature prior to being washed with PBS and 1% Tween 20. The cells were then incubated with DAPI in the dark for 5 min at room temperature. Excess DAPI was rinsed off with PBS and 1% Tween 20, and the slides were blotted dry with water-absorbent paper. The slides were then sealed with anti-fluorescence quencher and images were obtained using a fluorescent microscope (magnification, ×400).
Statistical analysis
SPSS 20.0 software (IBM Corp., Armonk, NY, USA) was used to analyze the data. Data are presented as the mean ± standard deviation and are representative of three individual experiments. An unpaired Student's t-test was used to compare two groups and three or more groups were analyzed by one-way analysis of variance (ANOVA) followed by a post hoc Bonferroni test. mRNA expression levels of CD44v6 and NF-κB in the tissue samples were compared using an unpaired Student's t-test. CD44v6 and NF-κB mRNA expression levels in different cells were analyzed by ANOVA followed by a post hoc Bonferroni test. The number of migrating and invading cells, and the number of colonies were compared by one-way ANOVA followed by a post-hoc Bonferroni correction test. P<0.05 was considered to indicate a statistically significant difference.
Results
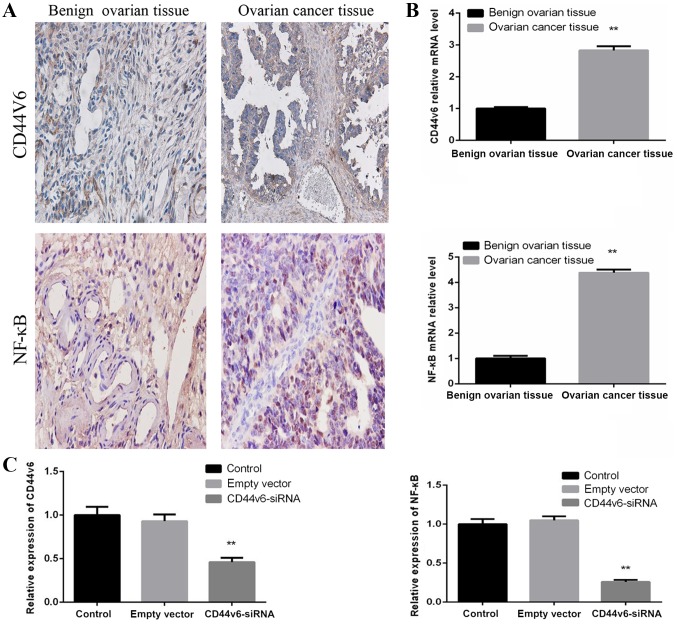
Expression of CD44v6 and NF-κB in OC and normal ovarian tissue samples
To determine whether CD44v6 and NF-κB are abnormally expressed in OC tissues, OC tissue samples and benign ovarian tissue samples were collected. Immunohistochemical analysis supported the observation that OC tissues exhibit increased levels of CD44v6 and NF-κB proteins, compared with normal ovarian tissue (Fig. 1A). The CD44v6 and NF-κB mRNA levels were detected by RT-qPCR, which revealed that CD44v6 and NF-κB mRNA levels in OC tissues were significantly increased, compared with normal ovarian tissues (P<0.01; Fig. 1B). These data demonstrated that the expression of CD44v6 and NF-κB is upregulated in OC tissue, compared with normal ovarian tissue.
Figure 1.
CD44v6 and NF-κB expression in ovarian cancer tissues and an ovarian cancer cell line. (A) Immunohistochemical analysis of CD44v6 and NF-κB in benign ovarian tissue and malignant ovarian tumor tissue (×400 magnification). Brown represents positive expression of CD44v6 and NF-κB. CD44v6 was predominantly located on the cell membrane and NF-κB was primarily located in the nucleus of cancer tissue. (B) CD44v6 and NF-κB mRNA expression levels in benign ovarian tissue and malignant ovarian tumor tissue. **P<0.01 vs. benign ovarian tissue. (C) Relative mRNA expression levels of CD44v6 and NF-κB in different groups, including the control, empty vector and CD44v6-siRNA groups. No significant difference was identified between the control and empty vector groups. A significant difference was revealed between the control and CD44v6-siRNA groups. Data are presented as the mean ± standard deviation. **P<0.01 vs. control group. NF-κB, nuclear factor-κB; siRNA, small interfering RNA; CD44v6, cluster of differentiation variant 6.
CD44v6-siRNA decreases NF-κB mRNA expression in OC cells
To further investigate whether NF-κB is affected by CD44v6 expression in OC cells, the A2780 OC cell line was used to generate a normal control group, an empty vector control group and a CD44v6-siRNA transfection group. The mRNA levels of CD44v6 and NF-κB were then detected in each group. The results demonstrated that there was no significant difference in the mRNA levels of CD44v6 and NF-κB between the normal control group and the empty vector control group. However, compared with the normal control group, the siRNA-transfected group exhibited significantly reduced expression levels of CD44v6 and NF-κB (P<0.01; Fig. 1C). This observation indicates that NF-κB mRNA expression levels are affected by CD44v6 expression.
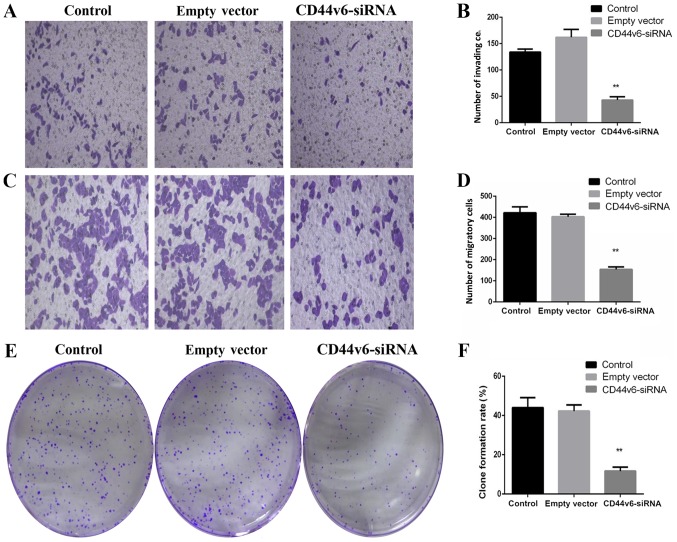
CD44v6-siRNA impairs the proliferation, migration and invasion of OC cells
To determine whether knockdown of CD44v6 affects OC cell proliferation, migration and invasion, OC cell Transwell and colony formation experiments were performed. The results demonstrated the effect of silencing CD44v6 on the proliferation and invasion of A2780 cells. As presented in Fig. 2, in vitro Transwell invasion assays revealed that following the silencing of CD44v6, the number of invading cells per field in the CD44v6 siRNA group (43.25±3.02) was significantly reduced, compared with that in the control group (134.39±9.69; P<0.01; Fig. 2A and B). The transwell migration assays demonstrated that the number of migratory cells per field in the CD44v6 siRNA group (154.45±21.75) markedly decreased compared with the control group (421.67±48.95; P<0.01; Fig. 2C and D). Similarly, the colony formation ability in the CD44v6-siRNA group was significantly reduced, compared with the control group (P<0.01; Fig. 2E and F).
Figure 2.
CD44v6-siRNA impairs the proliferation, migration and invasion of ovarian cancer cells. (A) Representative figures of invading cells in different groups (magnification, ×200). (B) Quantification of the invasion ability of the control group (134.39±9.69), empty vector group (175.34±29.64) and CD44v6-siRNA group (43.25±3.02) was assessed by 0.1% crystal violet staining. (C) Representative figures of migratory cells in different groups (magnification, ×200). (D) Quantification of the migration ability of the control group (421.67±48.95), empty vector group (403.25±20.75) and CD44v6-siRNA group (154.45±21.75) was assessed by 0.1% crystal violet staining. The Transwell migration assays demonstrated that the number of migratory and invading cells per field in the CD44v6 siRNA group significantly decreased compared with the control group (P<0.01). (E) Representative figures of colony formation ability. (F) Quantification of the colony formation ability of the control group, empty vector group and CD44v6-siRNA group. A total of 300 cells were seeded per well. The colony formation rate=number of colonies/number of cells seeded ×100%. The data are presented as the mean ± standard deviation. **P<0.01 vs. control group. siRNA, small interfering RNA; CD44v6, cluster of differentiation variant 6.
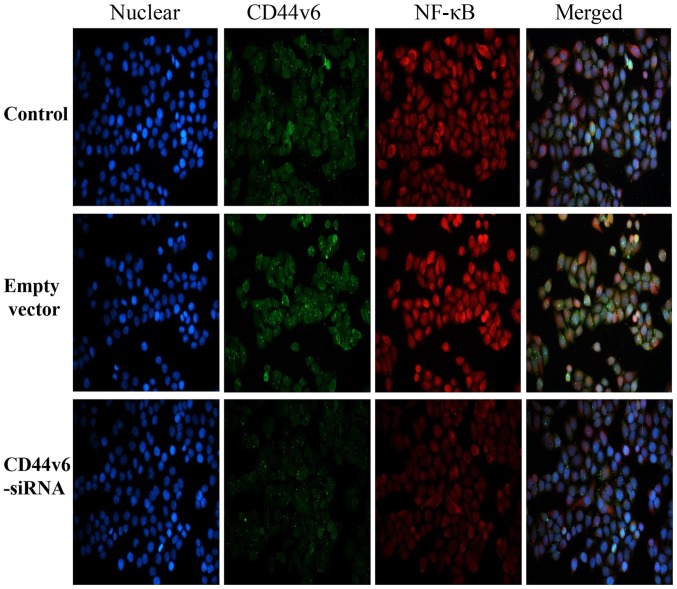
CD44v6-siRNA impairs the NF-κB pathway in OC cells
The aforementioned PCR results demonstrated that NF-κB mRNA expression was significantly reduced following knockdown of CD44v6. To investigate whether silencing CD44v6 affects the expression of NF-κB and its nuclear translocation, the expression of NF-κB in each group was detected by immunofluorescence. As demonstrated in Fig. 3, the fluorescence intensity of NF-κB in the CD44v6-siRNA group was markedly reduced, compared with the control group, which indicates that the NF-κB pathway may affect CD44v6 expression.
Figure 3.
Immunofluorescence of the control, empty vector and CD44v6-siRNA groups. Blue represents the nucleus, green represents expression of CD44v6 and red represents expression of NF-κB. siRNA, small interfering RNA; NF-κB, nuclear factor-κB; CD44v6, cluster of differentiation variant 6.
Discussion
The present study investigated the effects of NF-κB pathway inhibition by CD44v6 knockdown in OC cells. It was identified that CD44v6-siRNA OC cells exhibit decreased invasion ability and disrupted NF-κB activation.
In addition to the present study, previous studies also examined the expression of CD44v6 in the ovary to investigate the association between CD44v6 and the development of OC (27,48,49). The results from the present study are in agreement with a study by Tjhay et al (49), which demonstrated that CD44v6-positive OC cells possess an increased capacity for migration and invasion. Additionally, Zhang et al (31) reported that the expression of CD44v6 mRNA was significantly elevated in clinical samples of benign ovarian tumor and OC, and no significant differences were revealed in CD44v6 expression between normal ovarian tissue and benign ovarian tumor at the protein level. However, the authors identified that expression of CD44v6 in OC was significantly increased, compared with that in normal ovaries and benign ovarian tumors, which is in agreement with the present results.
Using western blot analysis, Tjhay et al (49) compared the expression of epithelial-mesenchymal transition (EMT) regulatory proteins, including E-cadherin, N-cadherin, fibronectin and vimentin, in fluorescence-activated cell sorting (FACS)-sorted CD44v6-positive cells with that in FACS-sorted CD44v6-negative cells. Compared with FACS-sorted CD44v6-negative cells, E-cadherin expression was downregulated in FACS-sorted CD44v6-positive cells, and N-cadherin, fibronectin, and vimentin expression was increased in CD44v6-positive cells. In contrast to immortalized normal cells, prostate cancer cells with CD44v6 suppression demonstrated downregulated EMT markers and reduced tumorigenic potential (50). These observations indicate that a subpopulation of CD44v6-positive cells may regulate the metastatic ability of OC cells by influencing EMT. Additionally, a previous study demonstrated that CD44v6-positive OC cells serve a pivotal role in disseminated metastatic tumors of the pelvic peritoneum and exhibit potential as metastatic initiators in OC mouse models (51). CD44v6-positive cancer cells possess a significant effect on the survival of patients with OC (52). CD44v6 has been demonstrated to promote OC metastasis by mediating ovarian tumor cell invasion into the peritoneum (49). Furthermore, siRNA knockdown of CD44v6 expression has been demonstrated to decrease the ability of SKOV3 cells to adhere and migrate, indicating that CD44v6 may be involved in mediating tumor cell adhesion and migration during metastasis (53), an observation that is consistent with the present results. Overall, this indicates that CD44v6 expression is associated with the progression, metastasis and recurrence of epithelial OC.
NF-κB generally exists as a dimer, most commonly with the p50 and p65 subunits. In a non-stimulated state, NF-κB binds to inhibitor of κB (IκB) in a non-activated form in the cytoplasm. When cells receive an external stimulus, IκB is phosphorylated and degraded, allowing NF-κB to translocate to the nucleus, resulting in NF-κB activation. The nuclear localization signal on NF-κB is then exposed in response to various cytokines, growth factors, apoptosis-associated factors and other target genes (54). Combined with the basic sequence, this results in increased nuclear transcription, which is involved in a number of human pathophysiological processes, including the inflammatory and immune responses (55,56). Numerous studies demonstrated that NF-κB regulates apoptosis through the following pathways: i) Direct regulation of apoptotic genes; ii) regulation of the S phase of the cell cycle, which interferes with the cellular response to apoptotic signals; and iii) interaction with certain cellular apoptosis proteins (54,56,57). NF-κB controls a number of features of cancer cells by modulating the transcriptional activation of genes involved in cell proliferation, angiogenesis, metastasis and apoptosis arrest (57).
NF-κB is one of the most significant molecules involved in inflammation and innate immunity and has been demonstrated to be an important endogenous tumor promoter (58). NF-κB serves a supervisory role in regulating transformation and inflammation in the context of cancer and inflammatory cells (59). NF-κB activation in cancer cells is responsible for the progression of inflammation-associated cancer; conversely, inhibiting NF-κB activation can inhibit tumor growth (55). The present study observed that NF-κB mRNA levels were reduced when CD44v6 was knocked down. Furthermore, immunofluorescence demonstrated that NF-κB expression was also inhibited. These results indicated that CD44v6 may participate in the proliferation and metastasis of OC via activation of the NF-κB pathway.
This hypothesis is supported by a number of other studies. Kawana et al (60) first demonstrated a direct association between CD44 and Toll-like receptors (TLRs) by detecting the activation of NF-κB, which is the principal signal transducer of TLR signaling in CD44-deficient bone marrow macrophages. The results indicated that the cytoplasmic domain of CD44 serves a regulatory role in TLR signaling and results in NF-κB activation by zymosan or lipopolysaccharide. Bourguignon et al (61) revealed that the downregulation of CD44 expression by treatment with CD44 siRNA not only effectively blocks CD44s association with TLR2, TLR4 and myeloid differentiation primary response 88 (MyD88) in MDA-MB-231 cells treated with low-molecular-weight hyaluronan (LMW-HA), but also significantly inhibits LMW-HA-mediated signaling and function, including NF-κB-mediated transcriptional activation, interleukin (IL)-1β/IL-8 gene expression and protein production. These results strongly indicate that CD44 and TLR2/4-associated MyD88 serve important roles in regulating NF-κB p65-specific transcriptional activation, in addition to cytokine/chemokine gene expression and protein production in MDA-MB-231 cells in response to LMW-HA treatment. Therefore, it is plausible that LMW-HA-mediated NF-κB p65 signaling and cytokine/chemokine production are functionally coupled in a CD44-dependent manner in breast tumor cells.
Therefore, it is reasonable to suggest that the mechanism by which CD44v6 causes tumor cell proliferation and metastasis is associated with its ability to induce NF-κB activation. This characteristic may serve an important role in the potential use of chemotherapeutic drugs that target this critical molecular mechanism for the treatment of OC.
In conclusion, the biological and molecular heterogeneity of OC is a highly promising research area, and studies may provide novel insights into the diagnosis and treatment of OC as well as breakthroughs in the treatment and prognosis of advanced ovarian epithelial cancer. CD44v6 may promote the proliferation, invasion and migration of OC cells by activating the NF-κB pathway. CD44v6 in cancer cells may represent a potential molecular therapeutic target to prevent the initiation of proliferation and metastasis of OC cells. However, which specific molecular signaling pathways downstream of CD44v6 affect the NF-κB pathway and which upstream molecules regulate the expression of CD44v6 requires further research. Observations from future studies may provide more effective targets for the treatment of OC.
Acknowledgements
Not applicable.
Funding
The present study was supported by the Science and Technology Department of Hubei Province Science and Technology Support Program Project (grant no. 2015BCA313), the Independent Research Project of Wuhan University (grant no. 413000117) and the Special Fund for Clinical Medicine Research of Chinese Medical Association (grant no. 17020310700).
Availability of data and materials
All data generated or analyzed during the present study are included in this published article.
Authors' contributions
YC and XY conceived the study. YW designed the experiments and performed the majority of them. XY contributed to the acquisition of data, data analysis and interpretation of the data. LZ contributed to the cell experiments. YW and SX performed cell culture and collected clinical samples. YW wrote the manuscript. All authors read and approved the final manuscript.
Ethics approval and consent to participate
The Medical Ethics Committee of Medical College of Wuhan University (Wuhan, China) approved this study and written informed consent was obtained from all participants.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Towne SD., Jr Socioeconomic, Geospatial, and Geopolitical disparities in access to health care in the US 2011-2015. Int J Environ Res Public Health. 2017;14:573. doi: 10.3390/ijerph14060573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Torre LA, Trabert B, DeSantis CE, Miller KD, Samimi G, Runowicz CD, Gaudet MM, Jemal A, Siegel RL. Ovarian cancer statistics, 2018. CA Cancer J Clin. 2018;68:284–296. doi: 10.3322/caac.21456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yap TA, Carden CP, Kaye SB. Beyond chemotherapy: Targeted therapies in ovarian cancer. Nat Rev Cancer. 2009;9:167–181. doi: 10.1038/nrc2583. [DOI] [PubMed] [Google Scholar]
- 4.Kujawa KA, Lisowska KM. Ovarian cancer-from biology to clinic. Postepy Hig Med Dosw (Online) 2015;69:1275–1290. doi: 10.5604/17322693.1184451. (In Polish) [DOI] [PubMed] [Google Scholar]
- 5.Screaton GR, Bell MV, Bell JI, Jackson DG. The identification of a new alternative exon with highly restricted tissue expression in transcripts encoding the mouse Pgp-1 (CD44) homing receptor. Comparison of all 10 variable exons between mouse, human, and rat. J Biol Chem. 1993;268:12235–12238. [PubMed] [Google Scholar]
- 6.Jackson DG, Buckley J, Bell JI. Multiple variants of the human lymphocyte homing receptor CD44 generated by insertions at a single site in the extracellular domain. J Biol Chem. 1992;267:4732–4739. [PubMed] [Google Scholar]
- 7.Prochazka L, Tesarik R, Turanek J. Regulation of alternative splicing of CD44 in cancer. Cell Signal. 2014;26:2234–2239. doi: 10.1016/j.cellsig.2014.07.011. [DOI] [PubMed] [Google Scholar]
- 8.Saegusa M, Machida D, Hashimura M, Okayasu I. CD44 expression in benign, premalignant, and malignant ovarian neoplasms: Relation to tumour development and progression. J Pathol. 1999;189:326–337. doi: 10.1002/(SICI)1096-9896(199911)189:3<326::AID-PATH425>3.0.CO;2-6. [DOI] [PubMed] [Google Scholar]
- 9.Zhang S, Balch C, Chan MW, Lai HC, Matei D, Schilder JM, Yan PS, Huang TH, Nephew KP. Identification and characterization of ovarian cancer-initiating cells from primary human tumors. Cancer Res. 2008;68:4311–4320. doi: 10.1158/0008-5472.CAN-08-0364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yae T, Tsuchihashi K, Ishimoto T, Motohara T, Yoshikawa M, Yoshida GJ, Wada T, Masuko T, Mogushi K, Tanaka H, et al. Alternative splicing of CD44 mRNA by ESRP1 enhances lung colonization of metastatic cancer cell. Nat Commun. 2012;3:883. doi: 10.1038/ncomms1892. [DOI] [PubMed] [Google Scholar]
- 11.Zoller M. CD44: Can a cancer-initiating cell profit from an abundantly expressed molecule? Nat Rev Cancer. 2011;11:254–267. doi: 10.1038/nrc3023. [DOI] [PubMed] [Google Scholar]
- 12.Dallas MR, Liu G, Chen WC, Thomas SN, Wirtz D, Huso DL, Konstantopoulos K. Divergent roles of CD44 and carcinoembryonic antigen in colon cancer metastasis. FASEB J. 2012;26:2648–2656. doi: 10.1096/fj.12-203786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ishimoto T, Nagano O, Yae T, Tamada M, Motohara T, Oshima H, Oshima M, Ikeda T, Asaba R, Yagi H, et al. CD44 variant regulates redox status in cancer cells by stabilizing the xCT subunit of system xc(−) and thereby promotes tumor growth. Cancer Cell. 2011;19:387–400. doi: 10.1016/j.ccr.2011.01.038. [DOI] [PubMed] [Google Scholar]
- 14.Nagano O, Okazaki S, Saya H. Redox regulation in stem-like cancer cells by CD44 variant isoforms. Oncogene. 2013;32:5191–5198. doi: 10.1038/onc.2012.638. [DOI] [PubMed] [Google Scholar]
- 15.Li XP, Zhang XW, Zheng LZ, Guo WJ. Expression of CD44 in pancreatic cancer and its significance. Int J Clin Exp Pathol. 2015;8:6724–6731. [PMC free article] [PubMed] [Google Scholar]
- 16.Ouhtit A, Rizeq B, Saleh HA, Rahman MM, Zayed H. Novel CD44-downstream signaling pathways mediating breast tumor invasion. Int J Biol Sci. 2018;14:1782–1790. doi: 10.7150/ijbs.23586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Abbasian M, Mousavi E, Arab-Bafrani Z, Sahebkar A. The most reliable surface marker for the identification of colorectal cancer stem-like cells: A systematic review and meta-analysis. J Cell Physiol. 2019;234:8192–8202. doi: 10.1002/jcp.27619. [DOI] [PubMed] [Google Scholar]
- 18.Gunthert U, Hofmann M, Rudy W, Reber S, Zöller M, Haussmann I, Matzku S, Wenzel A, Ponta H, Herrlich P. A new variant of glycoprotein CD44 confers metastatic potential to rat carcinoma cells. Cell. 1991;65:13–24. doi: 10.1016/0092-8674(91)90403-L. [DOI] [PubMed] [Google Scholar]
- 19.Liotta LA, Delisi C, Saidel G, Kleinerman J. Micrometastases formation: A probabilistic model. Cancer Lett. 1977;3:203–208. doi: 10.1016/S0304-3835(77)95675-0. [DOI] [PubMed] [Google Scholar]
- 20.Okayama H, Kumamoto K, Saitou K, Hayase S, Kofunato Y, Sato Y, Miyamoto K, Nakamura I, Ohki S, Sekikawa K, Takenoshita S. CD44v6, MMP-7 and nuclear Cdx2 are significant biomarkers for prediction of lymph node metastasis in primary gastric cancer. Oncol Rep. 2009;22:745–755. doi: 10.3892/or_00000496. [DOI] [PubMed] [Google Scholar]
- 21.Kawano T, Nakamura Y, Yanoma S, Kubota A, Furukawa M, Miyagi Y, Tsukuda M. Expression of E-cadherin, and CD44s and CD44v6 and its association with prognosis in head and neck cancer. Auris Nasus Larynx. 2004;31:35–41. doi: 10.1016/j.anl.2003.09.005. [DOI] [PubMed] [Google Scholar]
- 22.Gu H, Shang P, Zhou C. Expression of CD44v6 and E-cadherin in prostate carcinoma and metastasis of prostate carcinoma. Zhonghua Nan Ke Xue. 2004;10(38):32–34. (In Chinese) [PubMed] [Google Scholar]
- 23.Afify AM, Tate S, Durbin-Johnson B, Rocke DM, Konia T. Expression of CD44s and CD44v6 in lung cancer and their correlation with prognostic factors. Int J Biol Markers. 2011;26:50–57. doi: 10.5301/JBM.2011.6291. [DOI] [PubMed] [Google Scholar]
- 24.Stickeler E, Vogl FD, Denkinger T, Mobus VJ, Kreienberg R, Runnebaum IB. Soluble CD44 splice variants and pelvic lymph node metastasis in ovarian cancer patients. Int J Mol Med. 2000;6:595–601. doi: 10.3892/ijmm.6.5.595. [DOI] [PubMed] [Google Scholar]
- 25.Sun Y, Shen Z, Ji X. Study on the relationship between CD44v6, p53 gene mutation and ovarian carcinoma metastasis. Zhonghua Fu Chan Ke Za Zhi. 2000;35:225–228. (In Chinese) [PubMed] [Google Scholar]
- 26.Bar JK, Grelewski P, Popiela A, Noga L, Rabczynski J. Type IV collagen and CD44v6 expression in benign, malignant primary and metastatic ovarian tumors: Correlation with Ki-67 and p53 immunoreactivity. Gynecol Oncol. 2004;95:23–31. doi: 10.1016/j.ygyno.2004.06.046. [DOI] [PubMed] [Google Scholar]
- 27.Hong SC, Song JY, Lee JK, Lee NW, Kim SH, Yeom BW, Lee KW. Significance of CD44v6 expression in gynecologic malignancies. J Obstet Gynaecol Res. 2006;32:379–386. doi: 10.1111/j.1447-0756.2006.00422.x. [DOI] [PubMed] [Google Scholar]
- 28.Liotta LA, Delisi C, Saidel G, Kleinerman J. Micrometastases formation: A probabilistic model. Cancer Lett. 1977;3:203–208. doi: 10.1016/S0304-3835(77)95675-0. [DOI] [PubMed] [Google Scholar]
- 29.Ricciardelli C, Lokman NA, Ween MP, Oehler MK. Women in Cancer Thematic Review: Ovarian cancer-peritoneal cell interactions promote extracellular matrix processing. Endocr Relat Cancer. 2016;23:T155–T168. doi: 10.1530/ERC-16-0320. [DOI] [PubMed] [Google Scholar]
- 30.Ween MP, Oehler MK, Ricciardelli C. Role of versican, hyaluronan and CD44 in ovarian cancer metastasis. Int J Mol Sci. 2011;12:1009–1029. doi: 10.3390/ijms12021009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhang HF, Hu P, Fang SQ. Understanding the role of CD44V6 in ovarian cancer. Oncol Lett. 2017;14:1989–1992. doi: 10.3892/ol.2017.6377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kuhn S, Koch M, Nubel T, Ladwein M, Antolovic D, Klingbeil P, Hildebrand D, Moldenhauer G, Langbein L, Franke WW, et al. A complex of EpCAM, claudin-7, CD44 variant isoforms, and tetraspanins promotes colorectal cancer progression. Mol Cancer Res. 2007;5:553–567. doi: 10.1158/1541-7786.MCR-06-0384. [DOI] [PubMed] [Google Scholar]
- 33.Afify A, Purnell P, Nguyen L. Role of CD44s and CD44v6 on human breast cancer cell adhesion, migration, and invasion. Exp Mol Pathol. 2009;86:95–100. doi: 10.1016/j.yexmp.2008.12.003. [DOI] [PubMed] [Google Scholar]
- 34.Sokolova O, Naumann M. NF-kB signaling in gastric cancer. Toxins (Basel) 2017;9(pii):E119. doi: 10.3390/toxins9040119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Olivier S, Robe P, Bours V. Can NF-kappaB be a target for novel and efficient anti-cancer agents? Biochem Pharmacol. 2006;72:1054–1068. doi: 10.1016/j.bcp.2006.07.023. [DOI] [PubMed] [Google Scholar]
- 36.Xie DH, Tang XD, Xia SJ, Tan JM, Wang XH, Cai Y. Expression of NF-kappa B in human bladder cancer and its clinical significance. Ai Zheng. 2002;21:663–667. (In Chinese) [PubMed] [Google Scholar]
- 37.Pommier Y, Sordet O, Antony S, Hayward RL, Kohn KW. Apoptosis defects and chemotherapy resistance: Molecular interaction maps and networks. Oncogene. 2004;23:2934–2949. doi: 10.1038/sj.onc.1207515. [DOI] [PubMed] [Google Scholar]
- 38.Takada Y, Kobayashi Y, Aggarwal BB. Evodiamine abolishes constitutive and inducible NF-kappaB activation by inhibiting IkappaBalpha kinase activation, thereby suppressing NF-kappaB-regulated antiapoptotic and metastatic gene expression, up-regulating apoptosis, and inhibiting invasion. J Biol Chem. 2005;280:17203–17212. doi: 10.1074/jbc.M500077200. [DOI] [PubMed] [Google Scholar]
- 39.Felx M, Guyot MC, Isler M, Turcotte RE, Doyon J, Khatib AM, Leclerc S, Moreau A, Moldovan F. Endothelin-1 (ET-1) promotes MMP-2 and MMP-9 induction involving the transcription factor NF-kappaB in human osteosarcoma. Clin Sci (Lond) 2006;110:645–654. doi: 10.1042/CS20050286. [DOI] [PubMed] [Google Scholar]
- 40.Chen Y, Li R, Wang R, Liu Z. The significance of nuclear factor kappa Bp65 (NF kappa Bp65) expression on the vascular endothelial cells of rectum adenocarcinoma of human. Hua Xi Yi Ke Da Xue Xue Bao. 2001;32:196–199. (In Chinese) [PubMed] [Google Scholar]
- 41.Sasaki N, Morisaki T, Hashizume K, Yao T, Tsuneyoshi M, Noshiro H, Nakamura K, Yamanaka T, Uchiyama A, Tanaka M, Katano M. Nuclear factor-kappaB p65 (RelA) transcription factor is constitutively activated in human gastric carcinoma tissue. Clin Cancer Res. 2001;7:4136–4142. [PubMed] [Google Scholar]
- 42.Hodge JC, Bub J, Kaul S, Kajdacsy-Balla A, Lindholm PF. Requirememt of Rho A activity for increased nuclear factor kappa B activity and PC23 human prostate cancer cell invasion. Cancer Res. 2003;63:1359–1364. [PubMed] [Google Scholar]
- 43.Jana A, Krett NL, Guzman G, Khalid A, Ozden O, Staudacher JJ, Bauer J, Baik SH, Carroll T, Yazici C, Jung B. NFkB is essential for activin-induced colorectal cancer migration via upregulation of PI3K-MDM2 pathway. Oncotarget. 2017;8:37377–37393. doi: 10.18632/oncotarget.16343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ning Y, Xu M, Cao X, Chen X, Luo X. Inactivation of AKT, ERK and NF-κB by genistein derivative, 7-difluoromethoxyl-5,4′-di-n-octylygenistein, reduces ovarian carcinoma oncogenicity. Oncol Rep. 2017;38:949–958. doi: 10.3892/or.2017.5709. [DOI] [PubMed] [Google Scholar]
- 45.Zhang S, Leng T, Zhang Q, Zhao Q, Nie X, Yang L. Sanguinarine inhibits epithelial ovarian cancer development via regulating long non-coding RNA CASC2-EIF4A3 axis and/or inhibiting NF-κB signaling or PI3K/AKT/mTOR pathway. Biomed Pharmacother. 2018;102:302–308. doi: 10.1016/j.biopha.2018.03.071. [DOI] [PubMed] [Google Scholar]
- 46.Lu Z, Chen J. Introduction of WHO classification of tumours of female reproductive organs, fourth edition. Zhonghua Bing Li Xue Za Zhi. 2014;43:649–650. (In Chinese) [PubMed] [Google Scholar]
- 47.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 48.Wang J, Xiao L, Luo CH, Zhou H, Zeng L, Zhong J, Tang Y, Zhao XH, Zhao M, Zhang Y. CD44v6 promotes β-catenin and TGF-β expression, inducing aggression in ovarian cancer cells. Mol Med Rep. 2015;11:3505–3510. doi: 10.3892/mmr.2015.3145. [DOI] [PubMed] [Google Scholar]
- 49.Tjhay F, Motohara T, Tayama S, Narantuya D, Fujimoto K, Guo J, Sakaguchi I, Honda R, Tashiro H, Katabuchi H. CD44 variant 6 is correlated with peritoneal dissemination and poor prognosis in patients with advanced epithelial ovarian cancer. Cancer Sci. 2015;106:1421–1428. doi: 10.1111/cas.12765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ni J, Cozzi PJ, Hao JL, Beretov J, Chang L, Duan W, Shigdar S, Delprado WJ, Graham PH, Bucci J, et al. CD44 variant 6 is associated with prostate cancer metastasis and chemo-/radioresistance. Prostate. 2014;74:602–617. doi: 10.1002/pros.22775. [DOI] [PubMed] [Google Scholar]
- 51.Zhang HF, Hu P, Fang SQ. Understanding the role of CD44V6 in ovarian cancer. Oncol Lett. 2017;14:1989–1992. doi: 10.3892/ol.2017.6377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Shi J, Zhou Z, Di W, Li N. Correlation of CD44v6 expression with ovarian cancer progression and recurrence. BMC Cancer. 2013;13:182. doi: 10.1186/1471-2407-13-182. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 53.Motohara T, Fujimoto K, Tayama S, Narantuya D, Sakaguchi I, Tashiro H, Katabuchi H. CD44 Variant 6 as a predictive biomarker for distant metastasis in patients with epithelial ovarian cancer. Obstet Gynecol. 2016;127:1003–1011. doi: 10.1097/AOG.0000000000001420. [DOI] [PubMed] [Google Scholar]
- 54.Pramanik KC, Makena MR, Bhowmick K, Pandey MK. Advancement of NF-κB signaling pathway: A novel target in pancreatic cancer. Int J Mol Sci. 2018;19(pii):E3890. doi: 10.3390/ijms19123890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.DiDonato JA, Mercurio F, Karin M. NF-κB and the link between inflammation and cancer. Immunol Rev. 2012;246:379–400. doi: 10.1111/j.1600-065X.2012.01099.x. [DOI] [PubMed] [Google Scholar]
- 56.Huang S, Robinson JB, Deguzman A, Bucana CD, Fidler IJ. Blockade of nuclear factor-kappaB signaling inhibits angiogenesis and tumorigenicity of human ovarian cancer cells by suppressing expression of vascular endothelial growth factor and interleukin 8. Cancer Res. 2000;60:5334–5339. [PubMed] [Google Scholar]
- 57.Malinen M, Niskanen EA, Kaikkonen MU, Palvimo JJ. Crosstalk between androgen and pro-inflammatory signaling remodels androgen receptor and NF-κB cistrome to reprogram the prostate cancer cell transcriptome. Nucleic Acids Res. 2017;45:619–630. doi: 10.1093/nar/gkw855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Luo JL, Maeda S, Hsu LC, Yagita H, Karin M. Inhibition of NF-kappaB in cancer cells converts inflammation-induced tumor growth mediated by TNFalpha to TRAIL-mediated tumor regression. Cancer Cell. 2004;6:297–305. doi: 10.1016/j.ccr.2004.08.012. [DOI] [PubMed] [Google Scholar]
- 59.Perkins ND. The diverse and complex roles of NF-κB subunits in cancer. Nat Rev Cancer. 2012;12:121–132. doi: 10.1038/nrc3204. [DOI] [PubMed] [Google Scholar]
- 60.Kawana H, Karaki H, Higashi M, Miyazaki M, Hilberg F, Kitagawa M, Harigaya K. CD44 suppresses TLR-mediated inflammation. J Immunol. 2008;180:4235–4245. doi: 10.4049/jimmunol.180.6.4235. [DOI] [PubMed] [Google Scholar]
- 61.Bourguignon LY, Wong G, Earle CA, Xia W. Interaction of low molecular weight hyaluronan with CD44 and toll-like receptors promotes the actin filament-associated protein 110-actin binding and MyD88-NFκB signaling leading to proinflammatory cytokine/chemokine production and breast tumor invasion. Cytoskeleton (Hoboken) 2011;68:671–693. doi: 10.1002/cm.20544. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during the present study are included in this published article.