Abstract
The principal objective of this study was to determine the anti-staphylococcal potential of ethanol extracts of propolis (EEPs). A total of 20 samples of propolis collected from apiaries located in different regions of Poland were used in the study. The two-fold broth microdilution method revealed some important differences in the antimicrobial activity of investigated EEPs. Up to the concentration of 4096 µg/mL no activity was observed against Gram-negative bacteria (E. coli and P. aeruginosa). Staphylococci exhibited much higher susceptibility. The highest efficiency observed for EEP12 and EEP20 (MIC values ranged between 32 and 256 µg/mL). However, the achievement of bactericidal effect usually required higher concentrations. In the case of clinical isolates of S. aureus MBC values for EEP12 and EEP20 ranged from 512 to 1024 µg/mL. The HPLC analysis revealed that these two products contained a higher concentration of flavonoids (flavonols, flavones, and flavanones) compared to other investigated EEPs. In checkerboard test, a synergistic anti-staphylococcal effect was observed for the action of EEP20 in combination with amikacin, kanamycin, gentamycin, tetracycline, and fusidic acid (all these antibiotics inhibit protein synthesis). Moreover, the investigated EEPs effectively eradicated staphylococcal biofilm. The obtained results clearly confirm the high anti-staphylococcal potential of propolis harvested in Polish apiaries.
Keywords: propolis, S. aureus, biofilm, synergism, flavonoids
1. Introduction
Based on the World Health Organization reports, the resistance of bacteria to well-known antibiotics is becoming a major global health challenge [1]. One of the groups of bacteria which have evolved mechanisms of resistance to a plethora of antibiotics currently in use for human and animal therapies are staphylococci, particularly Staphylococcus aureus. They are responsible for a broad spectrum of difficult to treat diseases including skin and ocular infections, foodborne illness, pneumonia, meningitis, endocarditis, and osteomyelitis. High pathogenicity of S. aureus is based on the production of a wide array of virulence factors that include protein A, coagulase, collagenase, hyaluronidase, hemolysins, lipases, different toxins, adhesive proteins and also proteins affecting the biofilm formation. These bacteria are very ubiquitous in the environment. Moreover, it colonizes approximately 30% of all humans—usually asymptomatically, however, any insufficiency of the host’s immune system poses a risk of infection development [2,3]. Due to the growing frequency of isolation of staphylococcal strains resistant to currently used antibiotics, their high virulence potential and common presence in environmental, there is an urgent need to search for new agents as well as therapy systems effective against these bacteria. The most promising alternative, non-antibiotic agents that exhibit anti-staphylococcal (including MRSA isolates) activity include: bacteriocins [4,5], bacteriophages [6,7], peptidoglycan hydrolases [8] compounds of plant origin - plant extracts, essential oils and their components [9,10,11,12] and silver nanoparticles [9,13]. Selection of resistant strains can be limited by combined therapy—simultaneous use of at least two antibiotics/agents that affect different molecular targets [14,15]. Another interesting approach for the treatment of infectious disease is photodynamic therapy [16,17] and some research groups developed new vaccines that seem to be effective in the prophylaxis of staphylococcal infections [18,19,20].
A promising but still an underestimated group of potential antimicrobial agents are bee products, especially bee propolis [11,21]. It is a highly agglutinative, resinous substance of complex chemical composition, that is collected by bees from flower and leaf buds. Some of its ingredients, mainly polyphenols, and flavonoids, exhibit high antimicrobial activity. As a consequence, bees use this product for the protection against dangerous pathogens from the hive environment [22]. Because of its’ antimicrobial potential propolis became one of the most common and important agents used in folk medicine in different regions of the world for the treatment of infections [23]. The chemical composition of raw propolis depends on many factors, among them the geographical location of apiary—species of plants that are available for bees, and environmental conditions (e.g., weather, the season of the year) are the most important. In general, it consists of 50% resin, 30% vegetable and bee wax, 10% essential oils, 5% pollen and 5% various other substances, including organic pollutants [24]. Propolis-containing extracts exhibit broad spectrum biological activity, including antiseptic, antifungal, bacteriostatic, astringent, antioxidant, diastolic, anti-inflammatory, and anesthetic properties [24,25,26]. In this work, we have tested the activity of ethanol extracts of propolis (EEPs) gathered in different regions of Poland against planktonic and biofilm-related cells of S. aureus. Additionally, we have investigated the chemical composition and antioxidant potential of collected samples of propolis as well as synergistic interactions of ethanol extracts of propolis (EEPs) with antibacterial antibiotics. The obtained results revealed the high antistaphylococcal potential of Polish propolis. However, important differences in activity and chemical composition of different samples were noted.
2. Results
2.1. Antibacterial Activity of Ethanol Extracts of Propolis (EEP). Determination of MIC (Minimum Inhibitory Concentration) and MBC (Minimum Bactericidal Concentration) Parameters
The research revealed important differences in the activity of ethanol extracts of Polish propolis against Gram-positive and Gram-negative bacteria (Table 1). Up to the concentration of 4096 µg/mL no activity was observed against both investigated reference strains of Gram-negative bacteria, namely E. coli ATCC 25922 and P. aeruginosa ATCC 27853. Neither growth inhibition nor bactericidal effect was observed. Much better results were obtained with Staphylococci. However, some important differences were observed between the investigated samples. The highest susceptibility was exhibited by S. epidermidis ATCC 12228, with MIC and MBC values in the range of concentrations between 32 µg/mL (three and two products, respectively) and 512 µg/mL (five and six products respectively). Both S. aureus strains exhibited slightly higher resistance with MIC values between 128 and 512 µg/mL. However, in contrast to S. epidermidis, the bactericidal effect usually required higher concentrations of extracts in comparison to concentrations required for growth inhibition. The same values of MIC and MBC were observed with the eight extracts when tested against S. aureus ATCC 29213.
Table 1.
Antibacterial activity of ethanol extracts of propolis (EEPs) collected from apiaries located in different regions of Poland tested against reference strains of bacteria.
| No. EEP. | MIC and MBC (µg/mL) Against Different Strains of Bacteria | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| S. aureus ATCC 25923 | S. aureus ATCC 29213 | S. epidermidis ATCC 12228 | E. coli ATCC 25922 | P. aeruginosa ATCC 27853 | ||||||
| MIC | MBC | MIC | MBC | MIC | MBC | MIC | MBC | MIC | MBC | |
| 1 | 256 | 2084 | 256 | 256 | 64 | 64 | >4096 | >4096 | >4096 | >4096 |
| 2 | 256 | 2084 | 128 | 1024 | 32 | 64 | >4096 | >4096 | >4096 | >4096 |
| 3 | 512 | 4096 | 512 | 4096 | 512 | 512 | >4096 | >4096 | >4096 | >4096 |
| 4 | 256 | 4096 | 256 | 256 | 64 | 64 | >4096 | >4096 | >4096 | >4096 |
| 5 | 256 | 2084 | 256 | 2048 | 64 | 128 | >4096 | >4096 | >4096 | >4096 |
| 6 | 256 | 1024 | 256 | 256 | 128 | 128 | >4096 | >4096 | >4096 | >4096 |
| 7 | 256 | 2048 | 256 | 4096 | 128 | 256 | >4096 | >4096 | >4096 | >4096 |
| 8 | 512 | >4096 | 512 | 4096 | 512 | 512 | >4096 | >4096 | >4096 | >4096 |
| 9 | 256 | 4096 | 256 | 1024 | 64 | 64 | >4096 | >4096 | >4096 | >4096 |
| 10 | 256 | 4096 | 256 | 4096 | 64 | 64 | >4096 | >4096 | >4096 | >4096 |
| 11 | 256 | 512 | 256 | 512 | 32 | 32 | >4096 | >4096 | >4096 | >4096 |
| 12 | 128 | 512 | 128 | 128 | 64 | 64 | >4096 | >4096 | >4096 | >4096 |
| 13 | 512 | 4096 | 512 | 512 | 512 | 512 | >4096 | >4096 | >4096 | >4096 |
| 14 | 512 | 2048 | 512 | 512 | 256 | 256 | >4096 | >4096 | >4096 | >4096 |
| 15 | 512 | >4096 | 512 | 1024 | 256 | 512 | >4096 | >4096 | >4096 | >4096 |
| 16 | 512 | 2048 | 256 | 512 | 512 | 512 | >4096 | >4096 | >4096 | >4096 |
| 17 | 256 | 2048 | 256 | 512 | 256 | 256 | >4096 | >4096 | >4096 | >4096 |
| 18 | 256 | 512 | 256 | 256 | 128 | 128 | >4096 | >4096 | >4096 | >4096 |
| 19 | 512 | 1024 | 512 | 512 | 512 | 512 | >4096 | >4096 | >4096 | >4096 |
| 20 | 128 | 256 | 128 | 128 | 32 | 32 | >4096 | >4096 | >4096 | >4096 |
The high anti-staphylococcal potential of propolis collected in Polish apiaries was confirmed for clinical isolates, including 16 methicillin-susceptible strains (MSSA) and five isolates that were methicillin-resistant (MRSA). The investigation was performed for six EEPs. Based on the activity level against reference strains of S. aureus, the selected products were classified as: highly active (EEPs 12 and 20); medium active (EEPs 4 and 6) and low active (EEPs 3 and 8). The results presented in Table 2 confirm that EEPs with numbers 12 and 20 exhibited slightly stronger activity against all strains tested, and satisfactory activity was also observed for EEP no. 6. It is important to note that EEPs 12 and 20 effectively eliminated (not only inhibited growth) bacterial cells of all strains tested, with MBC values in the range from 512 to 1024 µg/mL. Other samples, particularly EEP3 and EEP8, but also EEPs 4 and 6, were less effective in the elimination of staphylococcal cells. No differences in the susceptibility were observed between MSSA and MRSA isolates.
Table 2.
Antibacterial activity of selected ethanolic extracts of propolis collected from Polish apiaries against clinical isolates of S. aureus (MSSA and MRSA).
| Strain No. | MIC and MBC (µg/mL) against Clinical Isolates of S. aureus | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| EEP 4 | EEP 3 | EEP 6 | EEP 8 | EEP 12 | EEP 20 | |||||||
| MIC | MBC | MIC | MBC | MIC | MBC | MIC | MBC | MIC | MBC | MIC | MBC | |
| 1 | 128 | 2048 | 512 | >2048 | 128 | 2048 | 256 | >2048 | 256 | 512 | 128 | 512 |
| 2 | 256 | >2048 | 512 | >2048 | 128 | >2048 | 512 | >2048 | 128 | 1024 | 256 | 1024 |
| 3 | 256 | >2048 | 512 | >2048 | 256 | >2048 | 256 | >2048 | 128 | 1042 | 128 | 1024 |
| 4 | 256 | >2048 | 512 | >2048 | 128 | 2048 | 512 | >2048 | 256 | 512 | 256 | 512 |
| 5 | 256 | >2048 | 256 | >2048 | 128 | >2048 | 512 | >2048 | 128 | 512 | 128 | 512 |
| 6 | 256 | >2048 | 512 | >2048 | 128 | 1024 | 256 | >2048 | 128 | 1024 | 128 | 512 |
| 7 | 128 | >2048 | 512 | >2048 | 128 | 2048 | 512 | >2048 | 256 | 1024 | 128 | 512 |
| 8 | 256 | >2048 | 512 | >2048 | 128 | 512 | 512 | >2048 | 256 | 1024 | 128 | 512 |
| 9 | 256 | >2048 | 512 | >2048 | 128 | 1024 | 512 | >2048 | 128 | 512 | 128 | 512 |
| 10 | 64 | 1024 | 512 | >2048 | 512 | 1024 | 32 | >2048 | 32 | 1024 | 64 | 1024 |
| 11 | 256 | 1024 | 512 | >2048 | 256 | 1024 | 512 | >2048 | 128 | 512 | 128 | 512 |
| 12 | 256 | 1024 | 512 | >2048 | 128 | 2048 | 512 | >2048 | 128 | 512 | 128 | 1024 |
| 13 | 256 | 2048 | 512 | >2048 | 128 | 1024 | 512 | >2048 | 128 | 512 | 128 | 512 |
| 14 | 256 | 2048 | 512 | >2048 | 128 | 1024 | 512 | >2048 | 256 | 512 | 128 | 512 |
| 15 | 256 | >2048 | 512 | >2048 | 256 | 512 | 512 | >2048 | 128 | 1024 | 128 | 1024 |
| 16 | 256 | 2048 | 512 | >2048 | 512 | 1024 | 128 | >2048 | 128 | 512 | 256 | 512 |
| 17 * | 256 | 1024 | 512 | 2048 | 128 | 2048 | 512 | >2048 | 256 | 512 | 128 | 512 |
| 18 * | 128 | 1024 | 256 | >2048 | 64 | 512 | 256 | >2048 | 128 | 512 | 128 | 512 |
| 19 * | 256 | 512 | 512 | >2048 | 128 | 512 | 512 | >2048 | 128 | 512 | 128 | 512 |
| 20 * | 512 | 1024 | 512 | >2048 | 256 | 512 | 512 | >2048 | 256 | 512 | 256 | 512 |
| 21 * | 256 | 512 | 1024 | >2048 | 256 | 512 | 1024 | >2048 | 256 | 512 | 128 | 512 |
* Methicillin-resistant.
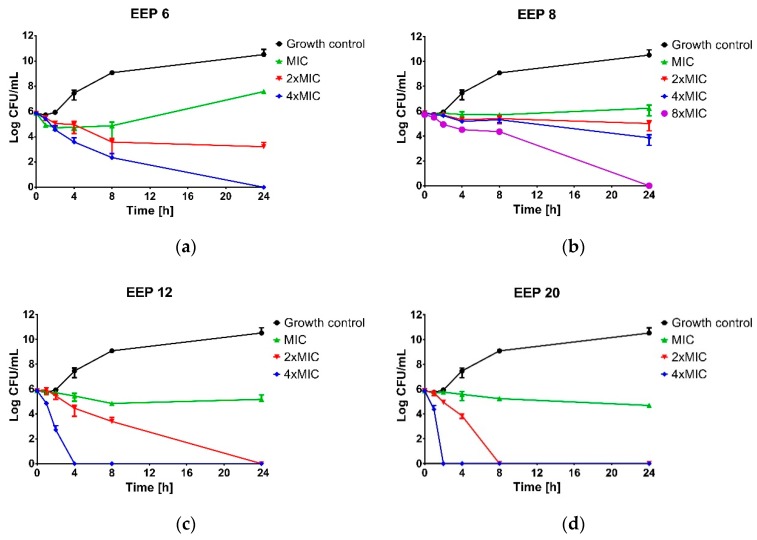
2.2. Kinetics of the Bactericidal Action of EEPs
Important differences in antimicrobial activity of the propolis samples harvested by Polish beekeepers were observed with the time-kill kinetic assay (Figure 1). As expected, all EEPs at MICs resulted in only growth inhibition effect with S. aureus ATCC 25923. The same result was observed for EEP6 and EEP8 at a concentration of 2 × MIC and 4 × MIC for EEP8. Even at the concentrations of 4 × MIC and 8 × MIC (for EEP6 and EEP8, respectively) the complete elimination of viable cells of S. aureus ATCC 25923 required extended incubation up to 24 h. Higher bactericidal efficiency was observed for EEP12 and EEP20. Both of these EEPs inactivated the bacteria at the concentration of 2 × MIC, however, slightly higher activity was observed with EEP20. With EEP20, the bactericidal effect was achieved after 8 h, while EEP12 required 24 h of incubation. At the concentration of 4 × MIC, complete inactivation of bacteria was achieved after 2 and 4 h for EEP20 and EEP12, respectively.
Figure 1.
Kill-time assay for selected ethanolic extracts of propolis (EEPs) tested against S. aureus ATCC 25923 at or above the MIC. The growth control contained no extracts. (A) EEP 6, (B) EEP 8, (C) EEP 12, (D) EEP 20. The results are presented as means ± SD (n = 3). Data without error bars indicates that the SD is too small to be observed on the graph.
2.3. Combined Action of EEPs with Known Antibacterial Antibiotics
The most active product, EEP20, was selected for analysis of interactions between propolis components and common antibacterial antibiotics. According to the guidelines proposed by Odds (2003), the combination of two antimicrobial agents is considered synergistic when the ΣFIC is ≤0.5, indifferent when the ΣFIC value is between 0.5 and 4.0, and antagonistic when the ΣFIC is ≥4.0 [27]. The results of our study are presented in Table 3.
Table 3.
The results of checkerboard analysis of drug interaction between EEP20 and different antibiotics against S. aureus ATCC 25923.
| Agent | MIC (µg/mL) | FIC | ΣFIC | Interpretation | |
|---|---|---|---|---|---|
| Alone | Combination | ||||
| EEP 20 | 128 | 16 | 0.125 | 0.375 | Synergy |
| Amikacin | 1 | 0.25 | 0.25 | ||
| EEP 20 | 128 | 32 | 0.25 | 0.5 | Synergy |
| Kanamycin | 2 | 0.5 | 0.25 | ||
| EEP 20 | 128 | 32 | 0.25 | 0.5 | Synergy |
| Gentamicin | 0.125 | 0.0312 | 0.25 | ||
| EEP 20 | 128 | 16 | 0.125 | 0.375 | Synergy |
| Tetracycline | 0.5 | 0.125 | 0.25 | ||
| EEP 20 | 128 | 16 | 0.125 | 0.625 | Indifferent * |
| Chloramphenicol | 4 | 2 | 0.5 | ||
| EEP 20 | 128 | 16 | 0.125 | 0.375 | Synergy |
| Fusidic acid | 0.5 | 0.125 | 0.25 | ||
| EEP 20 | 128 | 16 | 0.125 | 0.625 | Indifferent * |
| Erythromycin | 0.5 | 0.25 | 0.5 | ||
| EEP 20 | 128 | 16 | 0.125 | 0.625 | Indifferent * |
| Linezolid | 4 | 2 | 0.5 | ||
| EEP 20 | 128 | 128 | 1 | 2 | Indifferent |
| Levofloxacin | 0.125 | 0.125 | 1 | ||
| EEP 20 | 128 | 32 | 0.25 | 0.750 | Indifferent * |
| Norfloxacin | 0.5 | 0.25 | 0.5 | ||
| EEP 20 | 128 | 128 | 1 | 2 | Indifferent |
| Rifampicin | 0.015 | 0.015 | 1 | ||
| EEP 20 | 128 | 32 | 0.25 | 0.750 | Indifferent * |
| Mupirocin | 0.25 | 0.125 | 0.5 | ||
| EEP 20 | 128 | 64 | 0.5 | 1 | Indifferent |
| Bacitracin | 32 | 16 | 0.5 | ||
| EEP 20 | 128 | 64 | 0.5 | 0.625 | Indifferent * |
| Oxacillin | 0.25 | 0.062 | 0.125 | ||
| EEP 20 | 128 | 64 | 0.5 | 1 | Indifferent |
| Ampicillin | 0.25 | 0.125 | 0.5 | ||
| EEP 20 | 128 | 64 | 0.5 | 1 | Indifferent |
| Teicoplanin | 2 | 1 | 0.5 | ||
Indifferent *—according to the classification proposed by Odds combined therapy with these values of ΣFIC should be classified as indifferent, however, some slight decrease of MIC values of both agents (used in combination) was observed.
The synergistic effect (ΣFICI ≤ 0.5) was observed for five out of 16 investigated agents, namely: amikacin, kanamycin, gentamycin, tetracycline, and fusidic acid. Interestingly, the mode of action of all these antibiotics is inhibition of protein synthesis. Interactions of other agents (n = 11) with EEP20 formally have been classified as indifferent (ΣFICI > 0.5). However, some positive interactions of combined treatments (relatively low value of ΣFIC—between 0.5 and 1.0) was observed in the case of the following four inhibitors of translation process: chloramphenicol, erythromycin, mupirocin, linezolid, oxacillin (affects cell wall synthesis), and norfloxacin (affects the process of DNA translation). No antagonistic interaction (ΣFIC ≥ 4) was identified in the study.
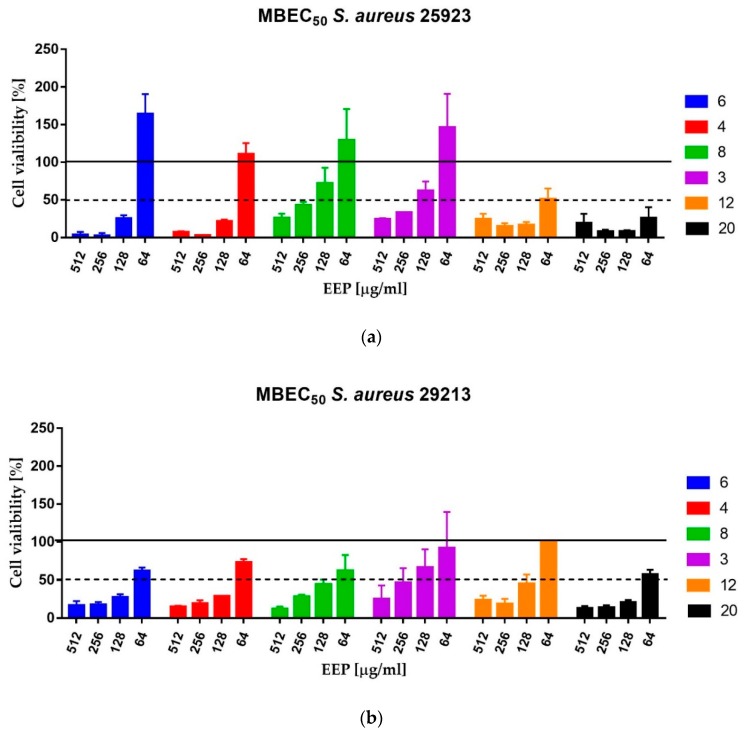
2.4. The Activity of EEPs Against Staphylococci Growing in the Form of Biofilms
Bacterial biofilms, including Staphylococcus spp., exhibit extremely high resistance to most antimicrobial agents, including antibiotics [28,29]. As a consequence, infections caused by staphylococcal biofilm are very difficult for eradication. The investigated extracts of propolis, particularly EEPs 6, 4, 12 and 20 effectively eradicated biofilm of both strains tested using MBEC50 values up to 128 µg/mL. In fact, in the case of S. aureus ATCC 25923, only residual growth was observed in the medium containing EEPs at concentrations higher than MBEC50, and only slightly lower susceptibility was observed for S. aureus ATCC 29213. Similarly, with planktonic cells, EEP3 and EEP8 exhibited lower efficacy (Table 1, Table 3 and Figure 2).
Figure 2.
Anti-biofilm activity of selected EEPs against S. aureus ATCC 25923 (A) and S. aureus ATCC 29213 (B).
2.5. Antioxidant Potential and Total Phenolic Content
In addition to the antimicrobial potential, an important advantage of propolis is its’ high antioxidant activity. Herein, we found that all EEPs tested contained a high concentration of polyphenols. The total phenolic content ranged from 96.10 to 197.07 mg GAE/g of the product, with EEP6 having the lowest level and the highest observed with EEP20 (Table 4). The other most active (antimicrobial) product, namely EEP12 also contained a high concentration of polyphenols (195.07 mg GAE/g of the product). However, two other products rich in polyphenols (EEP8 and EEP15) were found as less active against Staphylococci. The EEPs with numbers 12, 20 and 8 also exhibited the highest antioxidant activity in DPPH assay, with IC50, µg/mL values of 11.00, 14.55 and 15.10, respectively. The lowest antioxidant potential was identified for EEP6 (IC50, µg/mL—75.06). However, the EEP15 (rich in polyphenols) was found to have moderate antioxidant activity (IC50, µg/mL—26.65). These results clearly indicate that there is no direct relationship between total phenolic content and antimicrobial or antioxidant activity of EEPs tested.
Table 4.
Antioxidant activity of EEPs and total phenolic content.
| EEP’s Number | DPPH [IC50, µg/mL] | Total Phenolic Content [mg GAE/g] |
|---|---|---|
| 1 | 31.49 | 122.34 ± 5.9 |
| 2 | 27.86 | 159.84 ± 4.9 |
| 3 | 23.63 | 107.7 ± 5.6 |
| 4 | 39.80 | 132.01 ± 3.6 |
| 5 | 45.62 | 130.94 ± 0.4 |
| 6 | 75.06 | 96.10 ± 2.2 |
| 7 | 56.49 | 128.88 ± 3.6 |
| 8 | 15.10 | 182.28 ± 7.1 |
| 9 | 22.63 | 157.01 ± 5.0 |
| 10 | 27.45 | 131.13 ± 7.1 |
| 11 | 21.29 | 158.71 ± 4.3 |
| 12 | 11.00 | 195.07 ± 3.2 |
| 13 | 26.94 | 130.07 ± 0.9 |
| 14 | 24.08 | 157.16 ± 8.2 |
| 15 | 25.65 | 182.88 ± 2.4 |
| 16 | 24.07 | 151.19 ± 5.2 |
| 17 | 23.52 | 144.22 ± 2.5 |
| 18 | 31.28 | 132.68 ± 2.1 |
| 19 | 25.95 | 140.59 ± 8.2 |
| 20 | 14.59 | 197.07 ± 3.0 |
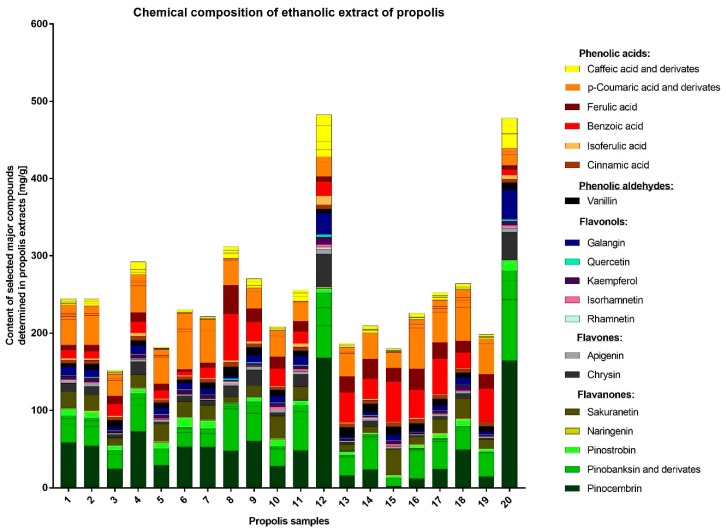
2.6. Determination of Chemical Composition of EEPs with UHPLC-DAD-QqTOF-MS
A total of 69 compounds were identified in the EEP samples by UHPLC-DAD-QqTOF-MS. The chemical profiles of all the samples were characterized by the presence of a large variety of phenolic acids and flavonoids (flavonols, flavones, flavanones) as well as and their esters (mostly of p-coumaric and caffeic acids, pinobanksin) (Table 5 and Figure 3). The quantities of the major compounds were determined by UHPLC-DAD and expressed in mg/g of extract. The most abundant compounds were pinocembrin (up to 167.71), pinobanksin-3-O-acetate (up to 78.99), benzoic acid (up to 60.26), and p-coumaric acid (up to 52.83). Nevertheless, the amount of individual compounds varied greatly between the samples (Table 6). Important differences in concentrations and chemical composition of the polyphenols that were present in two most active (against staphylococci) products EEP12 and EEP20 were noted. In comparison to other investigated EEPs, these two products contained a higher concentration of flavonoids (flavonols, flavones, and flavanones) and lower levels (in percentage) of phenolic acids, especially p-coumaric, ferulic, benzoic acids, and their derivatives. EEP12 and EEP20 were especially rich in pinocembrin, pinostrobin, pinobanksin and its derivatives (flavonones), chrysin (flavone) and galangin (flavonol), which appears to be crucial for the high anti-staphylococcal activity of these two propolis samples. Interestingly, EEP8, which was also recognized as a product rich in polyphenols and with high antioxidant activity contained a lower concentration of flavonoids and higher amount of acids which seems not to be very active in the inactivation or inhibition of the growth of bacteria. Thus, the detailed analysis partly explained the observed previously lack of correlation between total phenolic content and antimicrobial/antioxidant activity of the products. However, a significant effort would be required to fully understand the link between antimicrobial/antioxidant potential and chemical composition of propolis, which would be crucial for the prediction of the health-promoting properties of this product.
Table 5.
Compounds identified in propolis samples by UHPLC-DAD-QTOF-MS.
| No. | Component | RT [min] | UV max [nm] | [M − H+]− | Reference | Sample Number | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | ||||||
| 1 | 4-Hydroxybenzoic acid a,b,c | 7.32 | 256 | 137.0248 | [30] | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| 2 | 3-Hydroxybenzoic acid b,c | 8.00 | 296, 233 | 137.0245 | [30] | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| 3 | Caffeic acid a,b,c | 11.02 | 323, 295sh | 179.0351 | [31,32,33,34,35,36,37,38] | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| 4 | Vanillin a,b,c | 12.41 | 310, 280, 230 | 151.0404 | [36,38] | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| 5 | Benzoic acid a,b,c | 13.46 | 274, 230 | 121.0296 | [36,38] | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| 6 | p-Coumaric acid a,b,c | 13.81 | 310, 300sh | 163.0401 | [31,32,33,34,35,36,37,38] | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| 7 | Ferulic acid a,b,c | 14.63 | 322, 298sh | 193.0497 | [31,32,33,34,36,37] | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| 8 | Isoferulic acid a,b,c | 14.74 | 324, 300sh | 193.0497 | [31,32,33,36,37,38] | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| 9 | 4-Methoxybenzoic acid a,b,c | 15.06 | 256 | nd | [30] | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| 10 | 4-Hydroxy-3-methoxycinnamaldehyde a,b,c | 15.39 | 339, 301sh | 177.0554 | [30] | + | + | + | + | + | tr | + | + | + | + | + | + | + | + | + | + | + | + | + | tr |
| 11 | Dimethylcaffeic acid (DMCA) b,c | 16.40 | 324, 294sh | 207.0659 | [33,37] | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| 12 | Cinnamic acid a,b,c | 16.75 | 278 | 147.0451 | [33,36,37,39] | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| 13 | Caffeic acid ethyl ester | 17.29 | 322, 298 | 207.0670 | [40] | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| 14 | Pinobanksin-5-methylether b,c | 17.32 | 288 | 285.0762 | [32,33,35,37] | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| 15 | Quercetin a,b,c | 17.89 | 364, 270sh, 265 | 301.0349 | [33,36,37,39] | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| 16 | Luteolin a,b,c | 17.94 | 345, 254 | 285.0412 | [30,39] | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| 17 | Pinobanksin a,b,c | 18.44 | 292 | 271.0611 | [31,32,33,37] | + | + | + | + | + | + | + | + | + | + | + | + | + | + | tr | + | + | + | + | + |
| 18 | Quercetin-3-methyl ether b,c | 18.45 | 355, 268sh, 255 | 315.0497 | [33] | tr | tr | tr | tr | tr | tr | tr | tr | tr | tr | tr | tr | tr | tr | tr | tr | tr | tr | tr | tr |
| 19 | Chrysin-5-methyl ether b,c | 18.70 | 314sh, 264 | 267.0663 | [35,41] | + | tr | tr | tr | – | tr | tr | tr | + | tr | + | + | tr | tr | – | – | tr | tr | tr | + |
| 20 | Naringenin a,b,c | 18.92 | 289 | 271.0612 | [37,41] | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| 21 | Apigenin a,b,c | 19.26 | 338, 290sh, 263 | 269.0450 | [33,37,39] | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| 22 | Kaempferol a,b,c | 19.44 | 366, 295sh, 265 | 285.0403 | [31,36,37,39] | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| 23 | 1,3-Di-p-coumaroylglycerol ** b,c | 19.57 | 312, 300sh | 383.1129 | [31] | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| 24 | Isorahmnetin a,b,c | 19.72 | 371, 268sh, 256 | 315.0502 | [31,32,36,37,39,41] | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| 25 | p-Coumaroyl-feruloylglycerol b,c | 19.85 | 316, 298sh | 413.1240 | [37] | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| 26 | 2-Acetyl-1,3-di-caffeoylglycerol b,c | 19.92 | 328, 298sh | 457.1470 | [34,37,42] | + | + | + | + | + | - | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| 27 | Luteolin-5-methyl ether b,c | 20.06 | 350, 298sh, 267 | 299.0549 | [33] | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| 28 | Galangin-5-methyl ether b,c | 20.26 | 352, 300sh, 260 | 283.0602 | [32,33] | + | + | + | + | + | tr | tr | tr | + | + | + | + | + | + | tr | tr | + | tr | + | + |
| 29 | Quercetin-3,3′-dimethyl ether b,c | 20.36 | 356, 269sh, 255 | 329.0651 | [33,37] | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| 30 | Caffeic acid butyl or isobutyl ester b, c | 20.73 | 326, 298sh | 235.0972 | [31,43] | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| 31 | Rhamnetin (quercetin-7-methyl ether) b,c | 20.91 | 356, 268sh, 256 | 315.0504 | [37,39,44] | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| 32 | Caffeic acid prenyl or isoprenyl ester I b,c | 21.04 | 325, 298sh | 247.0979 | [32,33,35,36,37] | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| 33 | 2-Acetyl-1-caffeoyl-3-p-coumaroylglycerol b,c | 21.22 | 316, 299sh | 441.1182 | [31,34,37,42] | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| 34 | Caffeic acid prenyl or isoprenyl ester II b,c | 21.23 | 324, 298sh | 247.0976 | [32,33,35,36,37] | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| 35 | Caffeic acid prenyl or isoprenyl ester III b,c | 21.33 | 325, 298sh | 247.0973 | [32,33,35,36,37] | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| 36 | 2-Acetyl-1-caffeoyl-3-feruloylglycerol b,c | 21.50 | 322, 300sh | 471.1300 | [34,42] | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| 37 | Caffeic acid benzyl ester b,c | 21.64 | 328, 298sh | 269.0818 | [32,33,37] | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| 38 | Quercetin-3,7-dimethyl ether b,c | 21.65 | 356, 268sh, 256 | 329.0659 | [30,37] | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| 39 | Chrysin a,b,c | 21.93 | 312sh, 268 | 253.0505 | [31,33,34,35,36,37] | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| 40 | Pinocembrin a,b,c | 22.12 | 290 | 255.0666 | [33,34,35,36,37] | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| 41 | Caffeic acid pentyl or isopentyl ester b,c | 22.25 | 326, 298sh | 249.1141 | [43,45] | tr | tr | tr | tr | tr | tr | tr | tr | tr | tr | tr | tr | tr | tr | – | tr | tr | tr | tr | + |
| 42 | Sakuranetin b,c | 22.38 | 290 | 285.0773 | [36,37,41] | + | + | + | + | + | + | + | + | + | + | + | tr | + | + | + | + | + | + | + | tr |
| 43 | Caffeic acid phenethyl ester (CAPE) b,c | 22.40 | 325, 295 | 283.0986 | [32,33,37] | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| 44 | Galangin a,b,c | 22.43 | 360, 266, | 269.0454 | [30,31,32,33,35,37] | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| 45 | Acacetin (Apigenin-4′-methyl ether) a,b,c | 22.48 | 335, 299sh, 268 | 283.0621 | [36,37,41] | tr | tr | tr | tr | tr | tr | tr | tr | tr | tr | tr | tr | tr | tr | tr | tr | tr | tr | tr | tr |
| 46 | 2-Acetyl-1,3-di-p-coumaroylglycerol ** b,c | 22.72 | 312, 300 | 425.1232 | [31,37,42] | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| 47 | Pinobanksin 3-O-acetate b,c | 22.80 | 295 | 313.0713 | [31,32,33,37] | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| 48 | Kaempferide (kaempferol-4′-methyl ether) b,c | 22.93 | 365, 267 | 299.0555 | [30,36] | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| 49 | p-Coumaric acid prenyl or isoprenyl ester I b,c | 23.11 | 311, 299sh | 231.1028 | [32,33,35] | + | tr | tr | tr | tr | tr | tr | tr | + | tr | + | + | tr | tr | tr | – | tr | tr | tr | + |
| 50 | 2-Acetyl-3-p-coumaroyl-1-feruloylglycerol ** b,c | 23.12 | 318, 299sh | 455.134 | [31,34] | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| 51 | Methoxychrysin b,c | 23.21 | 310sh, 266, 245sh | 283.0611 | [32,33,46] | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| 52 | p-Coumaric acid prenyl or isoprenyl ester II b,c | 23.38 | 310, 299sh | 231.1025 | [32,33,35] | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| 53 | p-Coumaric acid prenyl or isoprenyl ester III b,c | 23.52 | 311, 299sh | 231.1028 | [32,33,35] | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| 54 | 2-Acetyl-1,3-di-feruloylglycerol b,c | 23.62 | 328, 298sh | 485.1423 | [31,34,47] | tr | tr | tr | tr | + | tr | + | + | + | + | + | + | + | + | + | + | + | tr | + | tr |
| 55 | p-Coumaric acid benzyl ester b,c | 23.88 | 312, 298sh | 253.0870 | [31,32,33] | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| 56 | Caffeic acid cinnamyl ester b,c | 24.32 | 326, 300sh | 295.0971 | [33,37,46] | + | + | + | + | + | + | + | + | + | + | + | + | + | + | tr | + | + | + | + | + |
| 57 | Ferulic acid benzyl ester * b,c | 24.62 | 326, 298 | 283.0968 | [31,38,48] | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| 58 | Pinobanksin 3-O-propanoate b,c | 25.05 | 294 | 327.0876 | [32,33,37] | + | + | + | + | – | – | tr | + | + | + | + | + | + | + | + | – | + | tr | tr | + |
| 59 | p-Coumaric acid phenethyl ester b,c | 25.06 | 310, 300sh | 267.1033 | [35] | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| 60 | p-Coumaric acid pentyl or isopentyl ester I b,c | 25.16 | 310, 298sh | 233.1190 | [43] | + | + | + | + | + | + | + | + | + | + | + | + | + | tr | + | + | + | + | + | + |
| 61 | p-Coumaric acid pentyl or isopentyl ester II b,c | 25.26 | 311, 298sh | 233.1192 | [43] | + | + | + | + | + | + | + | tr | + | + | + | + | + | + | tr | + | + | + | + | + |
| 62 | p-Coumaric acid cinnamyl ester b,c | 26.83 | 312, 300sh | 279.1024 | [37] | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| 63 | Pinobanksin 3-O-butanoate or isobutanoate b,c | 26.92 | 293 | 341.1022 | [32,33] | + | + | + | + | tr | tr | + | + | + | + | + | + | + | + | tr | tr | tr | tr | tr | tr |
| 64 | Pinostrobin chalcone b,c | 26.93 | 339, 287sh | 269.0823 | [37] | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| 65 | Pinobanksin 3-O-pentenoate or isopentenoate b,c | 27.06 | 295 | 353.1025 | [37,44,49] | + | + | + | + | – | tr | + | + | + | + | + | + | + | + | tr | tr | + | tr | + | + |
| 66 | Pinostrobin (pinocembrin-7-methyl ether) a,b,c | 27.20 | 289 | 269.0811 | [37] | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| 67 | Pinobanksin 3-O-pentanoate or isopentanoate b,c | 27.69 | 292 | 355.1188 | [32,33,37] | + | + | + | + | tr | tr | + | + | + | + | + | + | + | + | tr | tr | + | + | + | + |
| 68 | Metoxycinnamic acid cinnamyl ester b,c | 27.74 | 280 | 293.2122 | [33,46] | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| 69 | Pinobanksin 3-O-hexanoate b,c | 28.21 | 282 | 369.1347 | [32,33,46,49] | + | + | + | + | tr | tr | + | + | + | + | + | + | + | + | tr | tr | + | + | tr | + |
* Component tentatively identified; ** Glycerol substitution condition predicted according to comparison with GC-MS data; a Confirmed with standard; b Confirmed with HR-MS, MS/MS (data not shown) and/or UV; c Confirmed with references; nd—Ion not detected in applied analytical conditions; + compound detected; − compound not detected; tr—compound found in traces.
Figure 3.
The chemical composition of investigated EEPs.
Table 6.
The content of selected major compounds determined in propolis extracts by UHPLC-DAD (data are expressed as mg/g of extracts).
| No. | Compound | Rt [min] | Sample Number | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | |||
| 1 | Caffeic acid | 11.02 | 2.94 | 2.91 | 1.90 | 4.43 | 1.59 | 2.19 | 2.09 | 4.73 | 3.80 | 1.93 | 4.01 | 13.86 | 2.15 | 3.22 | 1.67 | 3.72 | 3.91 | 4.06 | 2.30 | 8.59 |
| 2 | Vanillin | 12.41 | 4.34 | 7.49 | 8.96 | 6.64 | 6.47 | 4.26 | 7.66 | 12.01 | 10.14 | 7.60 | 6.82 | 5.48 | 11.69 | 10.75 | 10.40 | 8.64 | 8.17 | 6.18 | 6.12 | 8.83 |
| 3 | Benzoic acid | 13.46 | 10.38 | 9.29 | 15.10 | 14.30 | 10.61 | 5.08 | 13.8 | 60.26 | 24.67 | 22.15 | 15.35 | 18.57 | 39.02 | 25.20 | 51.66 | 36.41 | 45.86 | 20.13 | 42.90 | 6.84 |
| 4 | p-Coumaric acid | 13.81 | 32.50 | 32.25 | 20.04 | 34.70 | 29.44 | 41.84 | 32.8 | 31.87 | 18.9 | 22.92 | 24.39 | 15.31 | 28.62 | 31.14 | 20.10 | 52.83 | 39.28 | 43.61 | 36.97 | 13.69 |
| 5 | Ferulic acid | 14.63 | 6.61 | 8.14 | 10.39 | 11.74 | 8.90 | 2.92 | 5.87 | 37.11 | 17.65 | 15.21 | 13.42 | 6.38 | 20.36 | 26.04 | 17.52 | 27.46 | 21.12 | 15.06 | 18.73 | 5.60 |
| 6 | Isoferulic acid | 14.74 | 2.28 | 2.32 | 1.60 | 4.00 | 1.00 | 1.15 | 1.12 | 2.58 | 2.95 | 1.11 | 4.50 | 11.55 | 1.10 | 2.14 | 0.99 | 1.57 | 1.07 | 1.10 | 1.05 | 5.40 |
| 7 | Dimethylcaffeic acid a | 16.40 | 0.15 | 0.75 | 0.49 | 2.24 | 0.20 | 0.24 | 0.22 | 0.47 | 0.17 | 0.19 | 0.11 | 9.60 | 0.17 | 0.13 | 0.13 | 0.13 | 0.27 | 0.16 | 0.16 | 0.43 |
| 8 | Cinnamic acid | 16.75 | 4.34 | 4.52 | 4.42 | 5.88 | 4.21 | 4.65 | 4.44 | 5.71 | 4.95 | 4.30 | 4.79 | 5.40 | 5.10 | 4.76 | 5.67 | 5.20 | 5.31 | 4.83 | 4.95 | 4.54 |
| 9 | Pinobanksin 5-methylether c | 17.32 | 3.55 | 3.80 | 1.09 | 6.01 | 0.05 | 0.35 | 0.25 | 4.23 | 6.33 | 0.72 | 8.06 | 19.33 | 0.37 | 2.96 | 0.11 | 0.22 | 0.53 | 0.54 | 0.14 | 12.66 |
| 10 | Quercetin | 17.89 | 1.12 | 1.56 | 0.73 | 1.13 | 0.78 | 0.86 | 0.80 | 1.89 | 1.37 | 0.86 | 1.21 | 3.52 | 0.66 | 1,00 | 0.67 | 0.69 | 0.81 | 0.92 | 0.64 | 2.46 |
| 11 | Pinobanksin | 18.44 | 7.49 | 7.33 | 3.64 | 8.81 | 3.36 | 5.77 | 5.82 | 2.50 | 8.98 | 2.52 | 8.76 | 23.19 | 2.09 | 2.93 | tr | 1.97 | 3.49 | 5.47 | 1.43 | 24.63 |
| 12 | Naringenin | 18.92 | 1.15 | 1.26 | 0.51 | 0.85 | 1.54 | 1.21 | 1.30 | 1.43 | 0.73 | 1.34 | 0.80 | 1.55 | 0.61 | 0.72 | 1.54 | 1.00 | 1.36 | 1.85 | 0.72 | 0.79 |
| 13 | Apigenin | 19.26 | 3.24 | 3.74 | 1.65 | 3.55 | 2.87 | 2.20 | 2.04 | 3.70 | 3.97 | 3.57 | 4.52 | 6.36 | 1.63 | 2.83 | 3.34 | 1.57 | 2.90 | 2.84 | 2.06 | 4.90 |
| 14 | Kaempferol | 19.44 | 4.40 | 5.30 | 2.03 | 4.70 | 4.65 | 4.74 | 4.53 | 1.80 | 2.84 | 5.02 | 4.28 | 9.80 | 1.85 | 1.98 | 3.83 | 2.05 | 3.78 | 6.24 | 1.54 | 5.65 |
| 15 | Isorhamnetin | 19.72 | 0.81 | 1.40 | 0.39 | 0.48 | 1.50 | 0.19 | 0.15 | 1.09 | 0.94 | 2.98 | 1.61 | 3.21 | 0.37 | 0.87 | 2.73 | 0.31 | 0.67 | 0.60 | 0.70 | 2.20 |
| 16 | Rhamnetin | 20.91 | 0.67 | 0.67 | 0.34 | 0.70 | 0.33 | 0.34 | 0.36 | 0.98 | 0.95 | 0.50 | 0.88 | 2.88 | 0.29 | 0.64 | 0.27 | 0.18 | 0.34 | 0.43 | 0.20 | 1.57 |
| 17 | Caffeic acid prenyl or isoprenyl ester II a | 21.23 | 2.35 | 2.42 | 1.43 | 2.52 | 0.69 | 0.51 | 0.52 | 6.63 | 3.28 | 1.71 | 5.28 | 10.51 | 1.83 | 3.67 | 1.25 | 2.74 | 3.43 | 1.32 | 2.31 | 18.40 |
| 18 | Caffeic acid prenyl or isoprenyl ester III a | 21.33 | 0.87 | 0.67 | 0.47 | 1.12 | 0.49 | 1.06 | 0.74 | 0.13 | 0.32 | 0.54 | 0.65 | 0.99 | 0.41 | 0.47 | 0.18 | 0.58 | 0.81 | 1.13 | 0.62 | 0.43 |
| 19 | Caffeic acid benzyl ester a | 21.64 | 1.69 | 2.27 | 1.35 | 5.45 | 0.50 | 0.60 | 0.58 | 4.02 | 4.29 | 0.95 | 4.61 | 19.62 | 0.86 | 1.73 | 0.27 | 1.06 | 1.26 | 1.45 | 0.76 | 11.53 |
| 20 | Chrysin | 21.93 | 11.08 | 11.13 | 4.64 | 16.30 | 2.73 | 6.90 | 6.26 | 14.23 | 20.34 | 4.38 | 15.66 | 43.00 | 3.34 | 7.45 | 0.58 | 1.78 | 3.82 | 6.69 | 1.74 | 35.76 |
| 21 | Pinocembrin | 22.12 | 58.34 | 53.84 | 24.65 | 72.76 | 29.38 | 53,00 | 52.69 | 47.57 | 60.38 | 28.22 | 48.17 | 167.71 | 15.95 | 23.92 | 2.35 | 11.94 | 24.49 | 49.26 | 14.44 | 164.32 |
| 22 | Sakuranetin | 22.38 | 20.85 | 20.54 | 9.47 | 17.46 | 22.69 | 19.85 | 18.65 | 7.00 | 14.19 | 29.03 | 17.54 | tr | 8.17 | 7.86 | 33.03 | 9.61 | 17.76 | 25.68 | 11.33 | tr |
| 23 | Galangin | 22.43 | 11.24 | 9.25 | 4.03 | 10.35 | 7.91 | 8.08 | 7.44 | 3.27 | 9.23 | 8.61 | 11.57 | 27.29 | 2.65 | 3.72 | 7.25 | 2.47 | 5.84 | 9.35 | 3.90 | 38.39 |
| 24 | Pinobanksin-3-O-acetate c | 22.80 | 23.56 | 25.31 | 18.77 | 33.94 | 17.77 | 18.54 | 17.64 | 54.57 | 35.81 | 22.08 | 41.55 | 41.77 | 23.78 | 38.96 | 10.80 | 37.08 | 35.17 | 24.17 | 29.94 | 78.99 |
| 25 | p-Coumaric acid benzyl ester b | 23.88 | 4.40 | 4.26 | 1.94 | 4.08 | 3.64 | 6.84 | 5.63 | 0.58 | 2.03 | 2.39 | 0.68 | 2.82 | 1.85 | 0.57 | 0.43 | 2.41 | 3.29 | 6.12 | 1.90 | 2.69 |
| 26 | p-Coumaric acid phenethyl ester b | 25.06 | 1.99 | 1.72 | 0.10 | 1.18 | 1.69 | 3.44 | 2.16 | 0.10 | 0.79 | 1.32 | 0.06 | 0.75 | 0.09 | 0.08 | 0.02 | 1.25 | 1.75 | 3.30 | 0.78 | 0.73 |
| 27 | p-Coumaric acid pentyl or isopentyl ester II b | 25.26 | 2.20 | 2.08 | 0.99 | 1.57 | 1.96 | 3.80 | 2.62 | tr | 0.65 | 1.29 | 0.02 | 0.65 | 0.90 | 0.03 | tr | 1.26 | 1.81 | 3.37 | 0.91 | 0.80 |
| 28 | p-Coumaric acid cinnamyl ester b | 26.83 | 10.42 | 10.17 | 4.63 | 8.50 | 7.54 | 16.60 | 12.69 | 1.48 | 4.25 | 6.05 | 0.65 | 5.86 | 6.02 | 1.66 | 0.68 | 5.46 | 8.59 | 9.52 | 4.79 | 3.82 |
| 29 | Pinostrobin | 27.20 | 9.17 | 7.74 | 6.33 | 6.75 | 7.73 | 13.12 | 10.62 | 0.14 | 5.51 | 9.00 | 5.86 | 5.62 | 4.73 | 1.91 | 2.04 | 3.83 | 5.49 | 8.59 | 4.21 | 13.60 |
| Sum | 244.5 | 244.5 | 152.3 | 292.5 | 182.6 | 230.9 | 221.9 | 312.2 | 270.6 | 208.7 | 255.9 | 482.8 | 186.8 | 209.5 | 179.7 | 225.7 | 252.7 | 264.5 | 198.5 | 478.5 | ||
tr—Found in traces; a Calculated as caffeic acid equivalent; b Calculated as p-coumaric acid equivalent; c Calculated as pinobanksin equivalent.
3. Discussion
Since ancient times, propolis, next to herbs, was one of the most important and common agents used for treating infections. The detailed history of using propolis in medicine, as well as discussion of perspectives of its future application, has been recently presented by Silva-Carvalho and coworkers [23]. The results of numerous investigations carried out during the last 40—50 years clearly confirm the high therapeutic (not only antimicrobial) potential of this product. In line with this tendency, we have focused our attention on the antibacterial, primarily anti-staphylococcal, activity of ethanolic extracts of honey bee propolis (EEPs), collected in apiaries located in different regions of Poland. A total of 20 samples were used in the current study. Our previous research revealed the high antifungal potential of Polish propolis [50,51]. The preliminary, screening tests of this study revealed important differences in susceptibility of Gram-positive and Gram-negative bacteria. It is likely a consequence of differences in the cell wall construction of these microorganisms which are also responsible for similar differences of activity of many other agents including antibiotics. In fact, up to the concentration of 4098 µg/mL, no activity was observed against both references strains of Gram-negative pathogenic bacteria: E. coli ATCC 25922 and P. aeruginosa ATCC 27853. The outcome of this study revealed important differences in the activity of different EEPs, against S. aureus, including both reference as well as clinical strains (MIC in the range of concentrations from 32 to 1024 μg/mL).
A similar phenomenon (differences in activity) and comparable level of antistaphylococcal activity have been previously presented by authors who examined the activity of ethanolic extracts of propolis collected in other geographical locations. Brazil is the leader in propolis production and export, with the global market of this product estimated to be approximately 2000 tons [52]. Several independent studies have revealed high efficiency of Brazilian propolis against staphylococci and other important human and animal pathogenic microorganisms. The Regueira group observed high activity of Brazilian red propolis against S. aureus (MIC in the range of concentrations from 64 to >1024 µg/mL) but also against Gram-negative bacteria E. coli (MIC ranged from 128 to 512 µg/mL) and P. aeruginosa (MIC = 512 µg/mL) [53]. Machado and coworkers investigated the antimicrobial potential of three different types of Brazilian propolis: red, brown and green, and ethanolic extracts of the red one were found to be the most active. The MIC of these extracts ranged from 25 to 100 μg/mL for reference strain S. aureus ATCC 25923 and from 100 to 400 μg/mL for S. aureus ATCC 33591. The ethanolic extracts of other products exhibited a bit lower efficacy with MIC values (for S. aureus ATCC 25923) in the ranges 200–800 and 200–400 μg/mL, respectively. The moderate activity against E. coli was also observed with MIC values (for ethanolic extracts) from 400 to 1600 μg/mL. The authors also found that ethanolic extracts of all three propolis types exhibited higher antimicrobial potential in comparison to products obtained with supercritical extraction [54]. In regards to both the antimicrobial potential of different types of Brazilian propolis as well as the activity of extracts obtained with ethanol (classical extraction) or carbon dioxide (supercritical extraction), convergent results have been recently published by Devequi-Nunes and colleagues [55]. The Machado group also reported that much higher concentration is required for obtaining the bactericidal effect (MBC) in comparison to MIC [54], which was also observed in our investigation. This conclusion has been additionally supported by the results of kinetic time-kill assay data reported in this study. Even the most active samples, namely 12 and 20, caused only growth inhibition at MIC concentration and at least 2 × MIC was required for inactivation of the indicator strains. This is an important consideration when propolis is considered as an agent for infection treatments.
Interesting results have been published by Suleman and colleagues [56], who investigated 39 propolis samples collected in South Africa. Most of the ethanolic extracts obtained on the base of these products exhibited higher anti-staphylococcal activity in comparison to three control samples of Brazilan propolis, but also in comparison to Brazilian propolis investigated by other authors (presented above). The MIC value for three most active extracts was 6 μg/mL and two of them exhibited bactericidal activity at this concentration [56]. The authors also observed much lower susceptibility of Gram-negative bacteria (for E.coli MIC ranged from 391 to 1563 μg/mL) and C. albicans (MIC ranged from 98 to 3125 μg/mL), but quite promising activity in the case of another pathogenic yeasts Cryptococcus neoformans (MIC between 49 and 391 μg/mL) [56]. Strong antibacterial activities of propolis samples sourced from three different areas of the Sonoran Desert in northwestern Mexico were confirmed in the research of the Velazquez group [57]. The MIC against S. aureus of the most active sample (coming from Ures) was 100 μg/mL [57]. The extract of the propolis sample collected near Teheran in Iran inhibited the growth of S. aureus ATCC 25923 at a concentration of 250 μg/mL, two times higher concentration was required for bactericidal effect [58]. Similarly, as in our study, some important differences in antibacterial activity were observed within the group of 53 propolis samples collected from different regions of Serbia. The MIC values against S. aureus ATCC 25922 ranged from 0.3 mg/mL (one sample, 0.4 mg/mL for nine samples) to 16.1 mg/mL (one sample) [59]. Comparable antimicrobial efficiency against staphylococci was revealed for two propolis samples harvested in subtropical Eastern Australia. MIC values for these samples were 0.4 and 2.0 mg/mL, but in fact, a bactericidal effect was measured in this study [60]. European propolis samples collected from various geographic origins were investigated by Al-Ani and colleagues. Both antimicrobial properties (MIC against Gram-positive microorganisms ranged from 0.08 mg/mL to 2.5 mg/mL) and antioxidant activity of the investigated products were similar to the EEPs tested in our group [61]. Promising, and mostly convergent to our findings, results regarding the anti-staphylococcal activity of ethanolic extract of Polish propolis (EEPP) against methicillin-sensitive S. aureus (MSSA) and methicillin-resistant S. aureus (MRSA) clinical isolates have been previously published by Wojtyczka and coworkers [62]. However, it should be noted that the authors investigated the propolis from only one location—Kamianna (South Poland). The investigated EEP displayed varying effectiveness against twelve S. aureus strains, with MIC in the range from 0.39 to 0.78 mg/mL, determined by broth microdilution method, and minimal bactericidal concentration (MBC) of the EEP ranged from 0.78 to 3.13 mg/mL [62]. The group of Wojtyczka proved also the high activity of Polish propolis against biofilm forming S. epidermidis strains [63]. Interesting antimicrobial properties of propolis produced in Polish apiaries was also reported by Scheller and coworkers, who observed synergism between EEP and anti-tuberculosis drugs [64]. For comparison of the therapeutic properties of propolis (including antimicrobial potential), it is important to remember that different methods of extraction of active ingredients are used. Woo and colleagues revealed that using 70% ethanol guaranteed optimal conditions for flavonoids extraction from raw propolis [65]. It is in agreement with the general observation that the highest antimicrobial activity is exhibited with extracts obtained using 70% ethanol, which has been also used herein. Also, the time of extraction differs in procedures applied in different studies. For example, Wojtyczka and co-authors continued extraction for 14 days (versus 100 h proposed herein), which also may be the reason of observed differences in the activity of preparations obtained by these authors and in our study.
From a clinical point of view, the most beneficial aspect of propolis is its anti-biofilm activity. In comparison to planktonic cells, only a slightly lower susceptibility of staphylococci growing in the form of biofilm was observed. The differences were much lower when compared to other antimicrobial agents, e.g., antibiotics. In our opinion, the efficacy of the antibiofilm activity is a result of the multitarget mode of action, in comparison to pure agents (antibiotics), which affect one particular component of a bacterial cell. The promising antibiofilm activity of EEPs produced from raw material collected in other geographical regions, e.g., Russia [66], Turkey [67] and Brazil has been also observed in other studies [68]. Promising results have been also presented by Ambi and coworkers. The authors not only reported high activity of Russian propolis against staphylococcal biofilm but also revealed that removing metals from ethanolic extracts of this product significantly reduces cytotoxicity of this product [69]. Our previous investigation confirmed the high activity of the extract of Polish propolis against candidal biofilms, including high efficiency in biofilm eradication from medical devices such as catheters [51].
Interestingly, our study suggests no differences in susceptibility between MSSA (of different resistance profile against five antibiotics) and MRSA strains. It is in agreement with results presented Pepljnjak and Kosalec, who used diffusion and dilution methods for investigation of the antimicrobial potential of propolis samples collected by Croatian beekeepers [70]. These results suggest that EEPs can be considered as a remedy for the treatment of infections caused by staphylococci resistant to different antibiotics. Propolis is also considered as a component of combined therapy with antibiotics. The outcomes of our study revealed a synergistic effect of EEP20 in combination with five commonly used antibiotics. All the antibiotics that demonstrated synergistic effects with propolis had the same mechanism of action—inhibition of the translation process (at different stages). The convergent results, synergism between EEP and antimicrobial drugs that interfere on bacterial protein synthesis have been published by Fernandez Junior [71]. Onlen and coworkers showed the synergistic effect of the combination of EEP with mupirocin using in vivo animal model—rabbits’ nares infections [72] and Krol and coworkers noted that EEP had a marked synergistic effect on the anti-staphylococcal activity of streptomycin and cloxacillin [73]. Interestingly, the group of Al-Ani observed mostly synergistic effects between EEP and antibiotics acting on cell wall synthesis (vancomycin and oxacillin) [61]. No antagonistic effect between EEP20 and any of the tested antibiotics was observed in our study. Synergistic effect of polish EEP with a broad spectrum of antibiotics of different modes of action was reported by Wojtyczka and colleagues, however, a different method (Kirby and Bauer like) was used by the authors [62]. The results presented in Table 3 indicate that using EEP20 in combination with 6 other antibiotics also resulted in some (slight) positive effect. The MIC values for both agents (EEP20 and tested antibiotic) decreased when they were used together and the ΣFIC values for these combinations were only slightly higher than 0.5, which is currently used as a borderline for classification of an interaction of two agents as synergistic in checkerboard method [27]. However, in regards to the guideline proposed previously by other authors e.g., Eliopoulos and Moellering [74] or and Dimkić and coworkers [75], the interaction of two agents with ΣFIC value in the range between 0.5 and 1.0 was classified as additive. Thus, in our opinion, these positive interactions also could be taken into account for combined therapy with using EEP and antibiotics. Synergistic effects of propolis collected in Poland with important antifungal chemotherapeutics, fluconazole, and voriconazole, was demonstrated in our previous publication [51].
The detailed HPLC analysis revealed the importantly different composition of two samples, namely EEP12 and EEP20, which also exhibited the highest anti-staphylococcal activity. These products were characterized by having a high content of flavonoids. The outcomes of many other studies also suggest that these components are crucial for antimicrobial, antioxidant, or even anticancer potential of propolis. On the other hand, important differences in the chemical composition of this product are an important drawback from the point of view of its medical application. As a consequence, propolis is not commonly used in clinical practice. The specific content of propolis collected in different geographical locations varies to a great extent depending on the plant precursors that are available for bees. On this basis only, 13 different types of Brazilian propolis have been identified and characterized [76]. A recent publication by Isidorov and coworkers have demonstrated that the principal plant precursors of propolis from boreal and temperate zones of the European continent are the bud resins of black poplar (Populus nigra L.), downy birch (Betula pubescens Ehrh.) and common aspen (Populus tremula L.) [31]. These authors have also determined taxonomical markers of the resins harvested from these plant origins [77]. The investigated samples contained a variety of compounds, characteristic for different plant sources, e.g., prenyl esters and some flavonoids characteristic for black poplar, glycerides typical for aspen as well as sakuranetin. The compositions of EEP12 and EEP20 were outstanding. Both samples contained considerably higher amounts of caffeic acid and its derivatives, pinostrobin, pinocembrin, chrysin, galangin and other compounds characteristic for the black poplar. The samples EEP12 and EEP20 contained also higher levels of isoferulic acid, in the case of EEP12 the level of isoferulic acid was two times higher than ferulic acid. Additionally, the samples contained just traces of sakuranetin, similar to the black poplar exudate [31,77]. This suggests that most of the samples originate from both black poplar and aspen. On the other hand, the EEP12 and EEP20 may be classified as being derived from black poplar. Such profiles and differences in composition are also consistent with previous findings [39,78]. It is worth to note that the polyphenol composition of black poplar buds themselves may vary [79]. While ‘typical’ black poplar usually contains more flavonoids than free phenolic acids, the concentration of free phenolic acids is higher in cultivar P. nigra ‘Italica’. Its main component is isoferulic acid [31], while other cultivars may contain p-coumaric acid as the main free phenolic acid [78].
4. Materials and Methods
4.1. Chemicals and Drugs
The standard compounds and reagents (all of analytical grade): MTT (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide), DMSO (dimethyl sulfoxide), gallic acid, Na2CO3, 1,1-diphenyl-2-picrylhydrazyl radical (DPPH), Folin-Ciocalteu’s reagent, resazurin, tetracycline, chloramphenicol, kanamycin, acetonitrile (LC-MS grade, gradient grade), formic acid, 4-methoxybenzoic acid, 4-hydroxy-3-methoxycinnamaldehyde, caffeic acid, quercetin, luteolin and pinostrobin PBS were purchased from Merck (Darmstadt, Germany). The standards of 4-hydroxybenzoic acid, p-coumaric acid, ferulic, isoferulic acid, pinobanksin, chrysin, sakuranetin, naringenin, apigenin, kaempferol, isorhamnetin, acacetin and pinocembrin were obtained from Extrasynthese (Genay, France) and galangin from Alfa Aesar, (Haverhill, MA, USA). The antibiotics: ampicillin, oxacillin, teicoplanin, gentamicin, amikacin, fusidic acid, erythromycin, mupirocin, rifampicin, levofloxacin, norfloxacin, linezolid, bacitracin were purchased from Argenda (Poland). Methanol, ethanol, vanillin, benzoic acid, cinnamic acid were purchased from (POCH, Gliwice, Poland). Ultrapure H2O (18.0 MΩ) was obtained with a Milli-Q Advantage A10 system (Millipore, Billerica, MA, USA). The absorbance of the reaction mixture in Folin-Ciocalteu, DPPH assays were measured using a Genesys 20 spectrophotometer (Thermo Scientific, Waltham, MA, USA).
4.2. Bacterial Strains and Media
In the preliminary studies, the antimicrobial activity of ethanol extracts of propolis was tested against five reference strains of bacteria: Staphylococcus aureus ATCC 25923, S. aureus ATCC 29213, S. epidermidis ATCC 12228, Pseudomonas aeruginosa ATCC 27853, and Escherichia coli ATCC 25922. The anti-staphylococcal potential of selected propolis samples was also investigated against sixteen MSSA and five MRSA isolates from patients with different infections (Table 7.). Bacteria were routinely grown on Luria-Bertani Agar (LA, Sigma Aldrich, Schnelldorf, Germany). The Minimum Inhibitory Concentration (MIC) was determined using liquid medium—Mueller-Hinton Broth 2 (MHB2, Sigma Aldrich) and for determination of Minimum Bactericidal Concentrations (MBC) the cells were transferred on the Baird Parker Agar plates (Biomaxima, Lublin, Poland). For biofilm formation TSB liquid medium supplemented with 2.5% of glucose was used.
Table 7.
MSSA and MRSA strains used in this work.
| No. | Number | Material | Ward | Antibiogram 1 |
|---|---|---|---|---|
| 1 | 4471313 | Nasal swab | Intensive care | Pen. – R, Met.– S, Clin.– S, Ery. - S |
| 2 | 4475564 | Nasal swab | Internal | Pen.– R, Met. – S, Clin. – R, Ery. - R |
| 3 | 4476206 | Sputum | Internal | Pen. – R, Met. – S, Clin. – R, Ery. – R |
| 4 | 4475131 | Pus | Internal | Pen. – R, Met. – S, Clin.– R, Ery. – R |
| 5 | 4466686 | Sputum | Surgical | Pen. – R, Met. – S, Clin. – R, Ery. – R |
| 6 | 4467080 | Nasal swab | Internal | Pen. – R, Met. – S, Clin. – S, Ery.– S |
| 7 | 4466380 | Wound | Surgical | Pen.– R, Met. – S, Clin. – S, Ery.– S |
| 8 | 4466896 | Nasal swab | Internal | Pen. – R, Met. – S, Clin. – S, Ery.– S |
| 9 | 4468792 | Pharyngeal swab | Pediatrics | Pen. – R, Met. – S, Clin. – S, Ery. – S |
| 10 | 4468706 | - | - | Pen. – R, Met. – S, Clin. – R, Ery. – R |
| 11 | 4467076 | A swab from the ear | Laryngology | Pen. – R, Met.– S, Clin.– S, Ery.– S |
| 12 | 4468505 | Nasal swab | Internal | Pen. – R, Met. – S, Clin. – R, Ery.– R |
| 13 | 4467526 | Pharyngeal swab | Cardiology | Pen. – R, Met. – S, Clin. – S, Ery.– S |
| 14 | 4467804 | A swab from the skin | Dermatology | Pen. – R, Met. – S, Clin. – S, Ery. – S |
| 15 | 4436126 | A swab from the ear | Laryngology | Pen. – R, Met. – S, Clin. – S, Ery. – S |
| 16 | 4467983 | A swab from the ear | Laryngology | Pen. – R, Met. – S, Clin. – S, Ery. – S |
| 17 | 45300223 | Blood | Pediatrics | Pen – R, Met – R, Clin – R, Ery – R |
| 18 | 9935169 | Wound | Dispensary | Pen.– R, Met. – R, Clin.– R, Ery.– R |
| 19 | 9944662 | Nasal swab | Dermatology | Pen. – R, Met. – R, Clin.– R, Ery. – R |
| 20 | 8007171 | Wound | Laryngology | Pen.– R, Met.– R, Clin. – R, Ery. – R |
| 21 | 9572250 | Wound | Internal | Pen. – R, Met. – R, Clin. – R, Ery. – R |
1 – Identification of bacterial isolates and antibiograms were performed by Laboratory of Clinical Microbiology, University Centre for Laboratory Diagnostics, Medical University of Gdańsk Clinical Centre with Vitek2 Biomerieux system; Pen—Penicillin, Met—Methicillin, Clin—Clindamycin, Ery—Erythromycin, R—resistance, S—sensitive.
4.3. Preparation of Ethanol Extract of Propolis
Twenty crude samples of Apis mellifera propolis were obtained from apiaries located in the various regions of Poland (Figure 4). The samples were kept under dry storage at ambient temperature in the dark until processing. In all cases, 5 g of raw propolis was extracted with 50 mL of 70% ethanol. Extraction was carried out in the dark for 100 h at ambient temperature with gentle agitation. Afterward, the ethanol extract solutions were centrifuged (9000 rpm) and filtered through Millipore filters (0.22 µm). The filtrates were evaporated to dryness at 40 °C using a rotary vacuum evaporator. The obtained resinous substance was weighed and then the working solutions of the extracts were prepared at a concentration of 81.92 mg/mL in 70% ethanol.
Figure 4.
Map of Poland indicating the geographic origin of the propolis samples. The dots (●—Pomerania Province; ●—middle/southern region of Poland) indicate the place where the propolis samples were collected. 1, 2—Rumia, 2015; 3—Kamianna, 2015; 4—Kluczbork, 2015; 5—Czeczewo, 2015; 6, 7, 16—Gdansk, 2015; 8 – Lipsko, 2017; 9—Radom, 2017; 10—Parczew, 2017; 11—Walbrzych, 2017; 12—Pruszcz Gdanski, 2017; 13—Chelm, 2017; 14—Debowy Gaj, 2017; 15, 17, 20—Stezyca, 2017; 18—Jasien, 2017; 19—Szczodrowo, 2017.
4.4. UHPLC-DAD-QqTOF-MS Analysis
UHPLC analyses were performed similarly as described previously [80,81] on Thermo Scientific™ UltiMate™ 3000 system (Thermo Scientific™ Dionex™, Sunnyvale, CA, USA), equipped with an autosampler and DAD detector set at 280, 320 and 360 nm. Spectral data was recorded in the 200–600 nm range. Chromatographic separation was performed on Kinetex® F5 2.6 µm, 100 Å, 150 × 2.1 mm analytical column (Phenomenex, Torrence, CA, USA) thermostated at 35 ± 1°C. Injection volume was set to 1 μL. The mobile phase consisted of 0.1% formic acid solutions in water (solvent A) and acetonitrile (solvent B). The flow rate was set at 0.4 mL/min and the separation was obtained using gradient: 100% of solvent A, decreasing to 91% within 7 min, isocratic for 3 min, decreasing to reach 80% in minute 10.5 and 60% in minute 18.5, isocratic for another 4 min and decreasing to reach 0% in minute 28.5, isocratic until 32 min. Subsequently, it returned to 100% A and the system was stabilized before the next analysis.
UHPLC-DAD-QqTOF-MS was performed in a similar setting and chromatographic conditions, additionally using Compact QqTOF-MS detector (Bruker, Darmstadt, Germany). MS detector was used in ESI negative mode, ion source temperature was set at 100 °C, nebulizer gas pressure was set at 2.0 bar, dry gas flow 0.8 L/min and temperature 210 °C. The capillary voltage was set at 2.20 kV. The collision energy was set at 8.0 eV. Internal calibration was obtained using 10 mM solution of sodium formate clusters. For ESI-MS/MS experiments, collision energy was set at 35 eV and nitrogen was used as collision gas.
Before the analysis, all the extracts were dissolved in ethanol and filtered through CHROMAFIL® 0.2 µm, Ø13mm, H-PTFE membrane syringe filter (Macherey-Nagel, Düren, Germany). Standard compounds were dissolved in ethanol or DMSO-ethanol mixture (1:10) for hardly soluble flavonoids and subsequently diluted in order to obtain calibration curves in the range of concentrations 0.5–200 µg/mL. Amounts of different compounds in the samples were calculated based on the calibration curve of appropriate standard or corresponding parent compound (e.g., amount of pinobanksin-3-O-acetate was expressed as pinobanksin equivalents).
4.5. Measurement of DPPH Radical Scavenging
The antiradical potential of the EEP was measured using DPPH radicals. The 2-fold serial dilutions of EEPs ranging from 0.008 mg/mL to 1.0 mg/mL were prepared in methanol in 96-well microtiter plates. Afterward, the 0.2 mM solution of DPPH was added to the plate at the 1:1 proportion. The mixture was incubated for 30 min in dark, at ambient temperature. Then, the absorbance was measured at 515 nm against a blank using a microplate reader. DPPH solution and methanol was used as a control, while ascorbic acid was used as a reference in comparing to the propolis extract. All measurements were performed in triplicate. The data were expressed as the percentage of DPPH reduction and calculated using the formula below. IC50 values were calculated using GraphPad Prism® 5 (Version 5.01, GraphPad Software, Inc., La Jolla, CA, USA):
4.6. Determination of Total Phenolic Content (TPC) of Propolis
The total content of phenolic compounds was determined using a Folin-Ciocalteu method as described before [82]. The Folin-Ciocalteu reagent in the volume of 0.5 mL was mixed with 100 μL of the EEPs (5 µg/mL in ultrapure water) and after 5 min, 3 mL of 100 g/L solution of Na2CO3 (w/v) was added. Following shaking the mixture was made up to a volume of 10 mL with ultrapure water and incubated for 90 min at ambient temperature. The absorbance at 720 nm was measured against blank in a 10 mm quartz cuvette. Total phenol content was calculated and expressed as milligrams of gallic acid equivalent (GAE) per kilogram, using a calibration curve prepared with a fresh gallic acid standard solution (10–2000 mg/L). All measurements were performed in triplicate.
4.7. Investigation of Antimicrobial Potential of Propolis
The minimum inhibitory concentrations (MICs) were determined by the two-fold broth microdilution method according to the CLSI standard methodology [83]. Bacteria were plated on LB solid medium and incubated overnight at 37 °C. Two to three bacterial colonies were taken directly from the plate and transferred into PBS buffer (pH = 7.4). The bacterial suspension was adjusted to the optical density of OD600 = 0.1 and diluted in MHB2 medium at a ratio of 1:100 v/v to the final cell concentration of approximately 1.0 × 106 CFU/mL. Two-fold serial dilutions of the propolis were prepared with a final dilution rate of 4096, 2048, 1024, 512, 256, 128, 64, 32, 16, 8 μg/mL. An aliquot of 100 μL of inoculum was dispensed to the wells of columns 1–11. Column 11 contained 200 µL of inoculum, and column 12 contained 200 µL of the MHB2 broth only (as control of sterility). The plates were incubated 24 h under static conditions at 37 °C. Because color and solubility of propolis extracts may interfere with growth measurement, the resazurin test was used. After incubation, resazurin (0.015% in PBS buffer) was added to all wells (30 µL), and further incubated for 2 h at 37 °C in the dark. The lowest concentration with no color change (blue resazurin color remained unchanged) was taken as a MIC value. The minimum bactericidal concentrations (MBCs) were assessed by transferring each dilution used for MIC assay on Baird-Parker agar plates using a sterile 48-well microtiter plate replicator. The plates were incubated for 24 h at 37 °C. Concentrations, where no growth of the colonies was observed, were assigned as MBC.
4.8. Kill-Time Assay
Time-kill assay was performed for four propolis samples revealed the highest (EEP20 and EEP12), moderate (EEP6) and weak (EEP8) anti-staphylococcal activity. The suspension of approx. cell density 1.0 × 106 CFU/mL of S. aureus ATCC 25923 was prepared in MHB2 broth supplemented with ethanolic extracts of propolis to the final concentrations equal to MIC, 2 × MIC, 4 × MIC or 8 × MIC and incubated at 37 °C with shaking. Bacterial suspension without propolis addition was used as the untreated control. At predetermined time intervals (0, 1, 2, 4, 6, 8 and 24 h) samples were taken, serially diluted in PBS buffer (from 10−1 to 10−7) and spotted (10 µL) onto a Baird-Parker agar plate. After 24 h of incubation, the plates were enumerated. Bactericidal activity was determined if a greater then 3 log10-fold decrease in the number of survivors was noted.
4.9. Biofilm Formation in 96-Well Microtiter Plate
The assay for biofilm cultivation was performed according to the procedure described previously with slight modifications [84]. The suspensions of approx. cell density 1-5 × 108 CFU/mL of S. aureus ATCC 25923 and S. aureus ATCC 29213 were diluted 1:100 (v/v) in TSB medium supplemented with 2.5% of glucose. Two hundred microliters of the cell suspensions were placed into the wells of columns 1–7 of vertically set plates. Negative controls were performed with a sterile medium placed in the wells of column 8. The plates were incubated for 24 h at 37 °C without shaking in order to allow bacteria to attach.
4.10. MBEC Assay
The Minimum Biofilm Eradication Concentration (MBEC) assay was carried out as described previously. The medium was removed and the biofilm was gently washed with 200 μL of sterile PBS. The 2-fold serial dilutions of propolis in MHB2 medium ranging from 2048 to 128 µg/mL were added to the wells and incubated for 24 h at 37 °C. The assay was performed for six propolis samples: EEP12 and EEP20—the most active against planktonic cells, EEP4 and EEP6—classified as samples of medium activity against planktonic cells and two samples that exhibited low activity—EEP3 and EEP8. The MBEC50 values were taken as the lowest concentration of propolis that caused eradication of at least 50% of living cells in comparison to the cells growing in the untreated control—measured as comparison of ability of living cells to the biotransformation of MTT (3-(4,5-dimethyl-2-thiazolyl)-2,5-diphenyl-2H-tetrazolium bromide) to insoluble in water violet formazan crystals [85]. The MTT assay was performed as described previously [85,86]. Briefly, after the biofilm formation (according to the procedure presented above) the inoculum was removed and the wells of microplate were washed with 200 μL of sterile PBS buffer. Subsequently, 150 μL of PBS and 50 μL of MTT solution (0.3% in PBS) were added to the wells and mixed. Following 2 h incubation at 37 °C in the dark, the MTT solution was replaced with 200 μL of DMSO for dissolving of formed formazan crystals. The optical density of the obtained solutions was measured at 540 nm using a Victor3 microtiter reader (Perkin Elmer, Waltham, MA, USA).
4.11. Checkerboard Dilution Test
The checkerboard test was used to evaluate the antimicrobial effect of propolis and different antibiotics in combination. Two samples of propolis (EEP12 and EEP20) with the highest antimicrobial activity and sixteen antibiotics were tested. Two-fold dilutions of propolis extracts were prepared along the ordinate in a 96-well plate. Then, previously prepared two-fold dilutions of antibiotic were distributed along the abscissa. Final concentrations of both antibiotic and propolis range from at least MIC to 1/32 MIC. Afterward, each microtiter well was inoculated with a bacterial inoculum of 1.0 × 106 CFU/mL in a volume equal to the volume of diluted antimicrobial solution (final cell concentration in each well was 5.0 × 105 CFU/mL), and the plates were incubated at 37 °C for 24 h under static conditions. After incubation, resazurin (0.015% in PBS buffer) was added to all wells (30 µL), and further incubated for 2 h at 37 °C in the dark. The change of color from blue to pink indicated the growth of bacteria. Fractional inhibitory concentration index (ΣFIC) was calculated for each well as follow:
ΣFICs were interpreter according to the model suggested by Odds [27]. A synergistic effect was observed when ΣFIC ≤ 0.5; an indifferent effect when 0.5 < ΣFIC < 4 and an antagonistic effect when ΣFIC ≥ 4.
4.12. Data Analysis
All experiments in this study were completed in triplicate and data was expressed as the means ± SD.
5. Conclusions
Our research revealed that propolis produced in Polish apiaries exhibits considerable anti-staphylococcal activity. The ethanolic extracts of this natural product effectively eliminate biofilm as well as planktonic cells of S. aureus. However, some important differences in the antimicrobial efficiency of the products were observed. The HPLC analysis revealed that two products that exhibited the highest antibacterial potential were characterized by having a high content of flavonoids, which suggests that these compounds are crucial for antimicrobial activity of Polish propolis. From a clinical point of view especially important was observed the synergistic effect of EEPs with antibiotics that affect protein synthesis in bacterial cells. Another, important health beneficial property of investigated samples of propolis was high antioxidant potential.
Acknowledgments
The authors are grateful to the members of The Society of Beekeepers in Gdansk for their help in preparing collection of the propolis samples. We are also grateful to the company IGO PHU Maria Borowik from Lublin for the propolis samples delivered for our research. The authors thank Marek Bronk from Laboratory of Clinical Microbiology, University Centre for Laboratory Diagnostics, Medical University of Gdańsk Clinical Centre for providing MRSA and MSSA clinical isolates. The authors are also grateful for Michael Wink from Heidelberg University for hosting Katarzyna Grecka for a 3-month fellowship.
Author Contributions
K.G.: (1) investigation of antimicrobial activity of EEPs (including synergism and tests with bacteria growing in the form of biofilm); (2) investigation antioxidant activity and determination of total phenolic content; (3) preparing tables, pictures and revision of the text of manuscript. P.M.K.: (1) partnership in determination of antioxidant properties; (2) determination of chemical composition of the EEPs tested; (3) revision of the manuscript. P.O.: (1) determination of chemical composition of the EEPs tested; (3) revision of the manuscript. R.W.W.: (1) consultations of idea of the research, discussion of obtained results and proposed conclusions; (2) revision of the manuscript. J.G.: (1) technical support. P.S.: principal investigator, head of the project, (1) partnership in research aiming in antimicrobial activity of EEPs and their antioxidant properties; (2) preparing the text of the manuscript.
Funding
The researches were financed by the [Grant no 2015/18/E/NZ6/00700] from the “National Science Centre, Poland”.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Sample Availability: Samples of the compounds are not available from the authors.
References
- 1.Seleem D., Pardi V., Murata R.M. Review of flavonoids: A diverse group of natural compounds with anti-Candida albicans activity in vitro. Arch. Oral Biol. 2017;76:76–83. doi: 10.1016/j.archoralbio.2016.08.030. [DOI] [PubMed] [Google Scholar]
- 2.Ngoc Thi Vu B., J Jafari A., Aardema M., Kieu Thi Tran H., Ngoc Thi Nguyen D., Tuyet Dao T., Vu Nguyen T., Khanh Tran T., Kim Thi Nguyen C., Fox A., et al. Population structure of colonizing and invasive Staphylococcus aureus strains in northern Vietnam. J. Med. Microbiol. 2016;65:298–305. doi: 10.1099/jmm.0.000220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Van Belkum A., Melles D.C., Nouwen J., van Leeuwen W.B., van Wamel W., Vos M.C., Wertheim H.F., Verbrugh H.A. Co-evolutionary aspects of human colonisation and infection by Staphylococcus aureus. Infect. Genet. Evol. 2009;9:32–47. doi: 10.1016/j.meegid.2008.09.012. [DOI] [PubMed] [Google Scholar]
- 4.Nascimento J.S., Ceotto H., Nascimento S.B., Giambiagi-Demarval M., Santos K.R., Bastos M.C. Bacteriocins as alternative agents for control of multiresistant staphylococcal strains. Lett. Appl. Microbiol. 2006;42:215–221. doi: 10.1111/j.1472-765X.2005.01832.x. [DOI] [PubMed] [Google Scholar]
- 5.Okuda K., Zendo T., Sugimoto S., Iwase T., Tajima A., Yamada S., Sonomoto K., Mizunoe Y. Effects of bacteriocins on methicillin-resistant Staphylococcus aureus biofilm. Antimicrob. Agents Chemother. 2013;57:5572–5579. doi: 10.1128/AAC.00888-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sulakvelidze A., Alavidze Z., Morris J.G., Jr. Bacteriophage therapy. Antimicrob. Agents Chemother. 2001;45:649–659. doi: 10.1128/AAC.45.3.649-659.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Matsuzaki S., Yasuda M., Nishikawa H., Kuroda M., Ujihara T., Shuin T., Shen Y., Jin Z., Fujimoto S., Nasimuzzaman M.D., et al. Experimental protection of mice against lethal Staphylococcus aureus infection by novel bacteriophage phi MR11. J. Infect. Dis. 2003;187:613–624. doi: 10.1086/374001. [DOI] [PubMed] [Google Scholar]
- 8.Szweda P., Schielmann M., Kotlowski R., Gorczyca G., Zalewska M., Milewski S. Peptidoglycan hydrolases-potential weapons against Staphylococcus aureus. Appl. Microbiol. Biotechnol. 2012;96:1157–1174. doi: 10.1007/s00253-012-4484-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kurek A., Grudniak A.M., Kraczkiewicz-Dowjat A., Wolska K.I. New antibacterial therapeutics and strategies. Pol. J Microbiol. 2011;60:3–12. [PubMed] [Google Scholar]
- 10.Solórzano-Santos F., Miranda-Novales M.G. Essential oils from aromatic herbs as antimicrobial agents. Curr. Opin. Biotechnol. 2012;23:136–141. doi: 10.1016/j.copbio.2011.08.005. [DOI] [PubMed] [Google Scholar]
- 11.Szweda P., Kot B. Bee products and essential oils as alternative agents for treatment of infections caused by S. aureus. In: Enany S., Alexander L.E.C., editors. Frontiers in Staphylococcus aureus. IntechOpen; London, UK: [DOI] [Google Scholar]
- 12.Szweda P., Zalewska M., Pilch J., Kot B., Milewski S. Essential oils as potential anti-staphylococcal agents. Acta Vet. Beograd. 2018;68:95–107. doi: 10.2478/acve-2018-0008. [DOI] [Google Scholar]
- 13.Kang J., Dietz M.J., Hughes K., Xing M., Li B. Silver nanoparticles present high intracellular and extracellular killing against Staphylococcus aureus. J. Antimicrob. Chemother. 2019:dkz053. doi: 10.1093/jac/dkz053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Betts J.W., Abdul Momin H.F., Phee L.M., Wareham D.W. Comparative activity of tedizolid and glycopeptide combination therapies for the treatment of Staphylococcus aureus infections: An in vitro and in vivo evaluation against strains with reduced susceptibility to glycopeptides. J. Med. Microbiol. 2018;67:265–271. doi: 10.1099/jmm.0.000671. [DOI] [PubMed] [Google Scholar]
- 15.Leijtens B., Elbers J.B.W., Sturm P.D., Kullberg B.J., Schreurs B.W. Clindamycin-rifampin combination therapy for staphylococcal periprosthetic joint infections: A retrospective observational study. BMC Infect. Dis. 2017;17:321. doi: 10.1186/s12879-017-2429-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fu X.J., Fang Y., Yao M. Antimicrobial photodynamic therapy for methicillin-resistant Staphylococcus aureus infection. Biomed. Res. Int. 2013:159157. doi: 10.1155/2013/159157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Almeida P.P., Pereira Í.S., Rodrigues K.B., Leal L.S., Marques A.S., Rosa L.P., da Silva F.C., da Silva R.A.A. Photodynamic therapy controls of Staphylococcus aureus intradermal infection in mice. Lasers Med. Sci. 2017;32:1337–1342. doi: 10.1007/s10103-017-2247-1. [DOI] [PubMed] [Google Scholar]
- 18.Giersing B.K., Dastgheyb S.S., Modjarrad K., Moorthy V. Status of vaccine research and development of vaccines for Staphylococcus aureus. Vaccine. 2016;34:2962–2966. doi: 10.1016/j.vaccine.2016.03.110. [DOI] [PubMed] [Google Scholar]
- 19.Haghighat S., Siadat S.D., Sorkhabadi S.M.R., Sepahi A.A., Mahdavi M. A novel recombinant vaccine candidate comprising PBP2a and autolysin against Methicillin Resistant Staphylococcus aureus confers protection in the experimental mice. Mol. Immunol. 2017;91:1–7. doi: 10.1016/j.molimm.2017.08.013. [DOI] [PubMed] [Google Scholar]
- 20.Chang B.C., Wang S.J. The newly filed patent applications for vaccines against Staphylococcus aureus. Hum. Vaccin. Immunother. 2017;13:2637–2638. doi: 10.1080/21645515.2017.1361577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Szweda P. Honey Analysis. IntechOpen; London, UK: 2017. Antimicrobial activity of honey. [DOI] [Google Scholar]
- 22.Simone-Finstrom M., Spivak M. Propolis and bee health: The natural history and significance of resin use by honey bees. Apidologie. 2010;41:295–311. doi: 10.1051/apido/2010016. [DOI] [Google Scholar]
- 23.Silva-Carvalho R., Baltazar F., Almeida-Aguiar C. Propolis: A complex natural product with a plethora of biological activities that can be explored for drug development. Evid. based Complement. Alternat. Med. 2015:206439. doi: 10.1155/2015/206439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Burdock G.A. Review of the biological properties and toxicity of bee propolis. Food Chem. Toxicol. 1998;36:347–363. doi: 10.1016/S0278-6915(97)00145-2. [DOI] [PubMed] [Google Scholar]
- 25.Dobrowolski J.W., Vohora S.B., Sharma K., Shah S.A., Naqvi S.A.H., Dandiya P.C. Antibacterial, antifungal, antiamoebic, antiinflammatory and antipyretic studies on propolis bee products. J. Ethnopharmacol. 1991;35:77–82. doi: 10.1016/0378-8741(91)90135-Z. [DOI] [PubMed] [Google Scholar]
- 26.Marcucci M.C. Propolis: Chemical composition, biological properties and therapeutic activity. Apidologie. 1995;26:83–99. doi: 10.1051/apido:19950202. [DOI] [Google Scholar]
- 27.Odds F.C. Synergy, antagonism, and what the chequerboard puts between them. J. Antimicrob. Chemother. 2003;52:1. doi: 10.1093/jac/dkg301. [DOI] [PubMed] [Google Scholar]
- 28.Archer N.K., Mazaitis M.J., Costerton J.W., Leid J.G., Powers M.E., Shirtliff M.E. Staphylococcus aureus biofilms: Properties, regulation and roles in human disease. Virulence. 2011;2:445–459. doi: 10.4161/viru.2.5.17724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Donlan R.M., Costerton J.W. Biofilms: Survival mechanisms of clinically relevant microorganisms. Clin. Microbiol. Rev. 2002;15:167–193. doi: 10.1128/CMR.15.2.167-193.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Metlin Scripps Center for Metabolomics and Mass Spectrometry (Metlin) La Jolla, USA The Scripps Research Institute. [(accessed on 28 August 2018)]; Available online: https://metlin.scripps.edu/index.php.
- 31.Isidorov V.A., Szczepaniak L., Bakier S. Rapid gc/ms determination of botanical precursors of Eurasian propolis. Food Chem. 2014;142:101–106. doi: 10.1016/j.foodchem.2013.07.032. [DOI] [PubMed] [Google Scholar]
- 32.Shi H., Yang H., Zhang X., Yu L.L. Identification and quantification of phytochemical composition and anti-inflammatory and radical scavenging properties of methanolic extracts of chinese propolis. J. Agric. Food Chem. 2012;60:12403–12410. doi: 10.1021/jf3042775. [DOI] [PubMed] [Google Scholar]
- 33.Pellati F., Orlandinia G., Pinetti D., Benvenutia S. HPLC-DAD and HPLC-ESI-MS/MS methods for metabolite profiling of propolis extracts. J. Pharm. Biomed. Anal. 2011;55:934–948. doi: 10.1016/j.jpba.2011.03.024. [DOI] [PubMed] [Google Scholar]
- 34.Shi H., Yang H., Zhang X., Sheng Y., Huang H., Yu L. Isolation and characterization of five glycerol esters from Wuhan propolis and their potential anti-inflammatory properties. J. Agric. Food Chem. 2012;60:10041–10047. doi: 10.1021/jf302601m. [DOI] [PubMed] [Google Scholar]
- 35.Trudić B., Anđelković B., Orlović S., Tešević V., Pilipović A., Cvetković M., Stanković J. HPLC/MS-TOF analysis of surface resins from three poplar clones grown in Serbia. South-East Eur. For. 2016;7:129–133. doi: 10.15177/seefor.16-12. [DOI] [Google Scholar]
- 36.Wishart Research Group HMDB: The Human Metabolome Database. University of Alberta, Edmonton, Canada, Wishart Lab. [(accessed on 30 August 2018)]; Available online: www.hmdb.ca.
- 37.Ristivojević P., Trifković J., Gašić U., Andrić F., Nedić N., Tešić Ž., Milojković-Opsenica D. Ultrahigh-performance liquid chromatography and mass spectrometry (UHPLC-LTQ/Orbitrap/MS/MS) study of phenolic profile of Serbian poplar type propolis. Phytochem. Anal. 2015;26:127–136. doi: 10.1002/pca.2544. [DOI] [PubMed] [Google Scholar]
- 38.Popova M., Giannopoulou E., Skalicka-Woźniak K., Graikou K., Widelski J., Bankova V., Kalofonos H., Sivolapenko G., Gaweł-Bęben K., Antosiewicz B., et al. Characterization and biological evaluation of propolis from Poland. Molecules. 2017:22. doi: 10.3390/molecules22071159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ristivojević P., Trifković J., Andrić F., Milojković-Opsenica D. Poplar-type propolis: Chemical composition, botanical origin and biological activity. Nat. Prod. Commun. 2015;11:1869–1876. doi: 10.1177/1934578X1501001117. [DOI] [PubMed] [Google Scholar]
- 40.Lee I., Han M., Kim D., Yun B. Phenylpropanoid acid esters from Korean propolis and their antioxidant activities. Bioorg. Med. Chem. Lett. 2014;24:3503–3505. doi: 10.1016/j.bmcl.2014.05.065. [DOI] [PubMed] [Google Scholar]
- 41.Justesen U. Negative atmospheric pressure chemical ionisation low-energy collision activation mass spectrometry for the characterisation of flavonoids in extracts of fresh herbs. J. Chromatogr. A. 2000;902:369–379. doi: 10.1016/S0021-9673(00)00861-X. [DOI] [PubMed] [Google Scholar]
- 42.Bertrams J., Müller B.M., Kunz N., Kammerer D.R., Stintzing F.C. Phenolic compounds as marker compounds for botanical origin determination of German propolis samples based on TLC and TLC-MS. J. Appl. Bot. Food Qual. 2013;86:143–153. [Google Scholar]
- 43.Greenaway W., Wollenweber E., Scaysbrook T., Whatley F.R. Esters of caffeic acid with aliphatic alcohols in bud exudate of Populus nigra. Z. Naturforsch. C. 1988;43:795–798. doi: 10.1515/znc-1988-11-1201. [DOI] [Google Scholar]
- 44.Justen U. Collision-induced fragmentation of deprotonated methoxylated flavonoids, obtained by electrospray ionization mass spectrometry. J. Mass Spectrom. 2001;36:169–178. doi: 10.1002/jms.118. [DOI] [PubMed] [Google Scholar]
- 45.Medana C., Carbone F., Aigotti R., Appendino G., Baiocchi C. Selective analysis of phenolic compounds in propolis by HPLC-MS/MS. Phytochem. Anal. 2008;19:32–39. doi: 10.1002/pca.1010. [DOI] [PubMed] [Google Scholar]
- 46.Gardana C., Scaglianti M., Pietta P., Simonetti P. Analysis of the polyphenolic fraction of propolis from different sources by liquid chromatography–tandem mass spectrometry. J. Pharm. Biomed. Anal. 2007;45:390–399. doi: 10.1016/j.jpba.2007.06.022. [DOI] [PubMed] [Google Scholar]
- 47.Isidorov V.A., Brzozowska M., Czyżewska U., Glinka L. Gas chromatographic investigation of phenylpropenoid glycerides from aspen (Populus tremula L.) buds. J. Chromatogr. A. 2008;1198–1199:196–201. doi: 10.1016/j.chroma.2008.05.038. [DOI] [PubMed] [Google Scholar]
- 48.Greenaway W., Whatley F.R. Bud exudate composition of Populus tremuloides. Can. J. Bot. 1991;69:2291–2295. [Google Scholar]
- 49.Kečkeš S., Gašić U., Veličković T.Ć., Milojković-Opsenica D., Natić M., Tešić Ž. The determination of phenolic profiles of Serbian unifloral honeys using ultra-high-performance liquid chromatography/high resolution accurate mass spectrometry. Food Chem. 2013;138:32–40. doi: 10.1016/j.foodchem.2012.10.025. [DOI] [PubMed] [Google Scholar]
- 50.Szweda P., Gucwa K., Kurzyk E., Romanowska E., Dzierżanowska-Fangrat K., Zielińska Jurek A., Kuś P.M., Milewski S. Essential oils, silver nanoparticles and propolis as alternative agents against fluconazole resistant Candida albicans, Candida glabrata and Candida krusei clinical isolates. Indian J. Microbiol. 2015;55:175–183. doi: 10.1007/s12088-014-0508-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Gucwa K., Kusznierewicz B., Milewski S., Van Dijck P., Szweda P. Antifungal activity and synergism with azoles of Polish propolis. Pathogens. 2018;7:56. doi: 10.3390/pathogens7020056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. [(accessed on 29 April 2019)]; Available online: https://www.whatech.com/market-research/materials-chemicals/125806-world-propolis-industry-trends-share-size-2021-forecast-report.
- 53.Regueira M.S., Neto Tintino S.R., da Silva A.R.P., Costa M.D.S., Boligon A.A., Matias E.F.F., de Queiroz Balbino V., Menezes I.R.A., Melo Coutinho H.D. Seasonal variation of Brazilian red propolis: Antibacterial activity, synergistic effect and phytochemical screening. Food. Chem. Toxicol. 2017;107:572–580. doi: 10.1016/j.fct.2017.03.052. [DOI] [PubMed] [Google Scholar]
- 54.Machado B.A., Silva R.P., Barreto Gde A., Costa S.S., Silva D.F., Brandão H.N., Rocha J.L., Dellagostin O.A., Henriques J.A., Umsza-Guez M.A., et al. Chemical composition and biological activity of extracts obtained by supercritical extraction and ethanolic extraction of brown, green and red propolis derived from different geographic regions in Brazil. PLoS ONE. 2016;11:e0145954. doi: 10.1371/journal.pone.0145954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Devequi-Nunes D., Machado B.A.S., Barreto G.A., Rebouças Silva J., da Silva D.F., da Rocha J.L.C., Brandão H.N., Borges V.M., Umsza-Guez M.A. Chemical characterization and biological activity of six different extracts of propolis through conventional methods and supercritical extraction. PLoS ONE. 2018;13:e0207676. doi: 10.1371/journal.pone.0207676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Suleman T., van Vuuren S., Sandasi M., Viljoen A.M. Antimicrobial activity and chemometric modelling of South African propolis. J. Appl. Microbiol. 2015;119:981–990. doi: 10.1111/jam.12906. [DOI] [PubMed] [Google Scholar]
- 57.Velazquez C., Navarro M., Acosta A., Angulo A., Dominguez Z., Robles R., Robles-Zepeda R., Lugo E., Goycoolea F.M., Velazquez E.F., et al. Antibacterial and free-radical scavenging activities of Sonoran propolis. J. Appl. Microbiol. 2007;103:1747–1756. doi: 10.1111/j.1365-2672.2007.03409.x. [DOI] [PubMed] [Google Scholar]
- 58.Jafarzadeh Kashi T.S., Kasra Kermanshahi R., Erfan M., Vahid Dastjerdi E., Rezaei Y., Tabatabaei F.S. Evaluating the in-vitro antibacterial effect of Iranian propolis on oral microorganisms. Iran. J. Pharm. Res. 2011;10:363–368. [PMC free article] [PubMed] [Google Scholar]
- 59.Ristivojević P., Dimkić I., Trifković J., Berić T., Vovk I., Milojković-Opsenica D., Stanković S. Antimicrobial activity of serbian propolis evaluated by means of MIC, HPTLC, bioautography and chemometrics. PLoS ONE. 2016;11:e0157097. doi: 10.1371/journal.pone.0157097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Massaro C.F., Simpson J.B., Powell D., Brooks P. Chemical composition and antimicrobial activity of honeybee (Apis mellifera ligustica) propolis from subtropical eastern Australia. Naturwissenschaften. 2015;102:68. doi: 10.1007/s00114-015-1318-z. [DOI] [PubMed] [Google Scholar]
- 61.Al-Ani I., Zimmermann S., Reichling J., Wink M. Antimicrobial activities of European propolis collected from various geographic origins alone and in combination with antibiotics. Medicines. 2018;5:E2. doi: 10.3390/medicines5010002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wojtyczka R.D., Dziedzic A., Idzik D., Kępa M., Kubina R., Kabała-Dzik A., Smoleń-Dzirba J., Stojko J., Sajewicz M., Wąsik T.J. Susceptibility of Staphylococcus aureus clinical isolates to propolis extract alone or in combination with antimicrobial drugs. Molecules. 2013;18:9623–9640. doi: 10.3390/molecules18089623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wojtyczka R.D., Kępa M., Idzik D., Kubina R., Kabała-Dzik A., Dziedzic A., Wąsik T.J. In vitro antimicrobial activity of ethanolic extract of Polish propolis against biofilm forming Staphylococcus epidermidis Strains. Evid. Based. Complement. Alternat. Med. 2013;2013:590703. doi: 10.1155/2013/590703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Scheller S., Dworniczak S., Waldemar-Klimmek K., Rajca M., Tomczyk A., Shani J. Synergism between ethanolic extract of propolis (EEP) and anti-tuberculosis drugs on growth of mycobacteria. Zeitschrift für Naturforschung C. 1999;54:549–553. doi: 10.1515/znc-1999-7-814. [DOI] [PubMed] [Google Scholar]
- 65.Woo S.S., Hong I.P., Han S.M. Extraction properties with of propolis with ethanol concentration. J. Apicul. 2015;30:211–216. doi: 10.17519/apiculture.2015.09.30.3.211. [DOI] [Google Scholar]
- 66.Bryan J., Redden P., Traba C. The mechanism of action of Russian propolis ethanol extracts against two antibiotic-resistant biofilm-forming bacteria. Lett. Appl. Microbiol. 2016;62:192–198. doi: 10.1111/lam.12532. [DOI] [PubMed] [Google Scholar]
- 67.Akca A.E., Akca G., Topçu F.T., Macit E., Pikdöken L., Özgen I.Ş. The comparative evaluation of the antimicrobial effect of propolis with chlorhexidine against oral pathogens: An in vitro study. Biomed. Res. Int. 2016;2016:3627463. doi: 10.1155/2016/3627463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.de Oliveira Dembogurski D.S., Silva Trentin D., Boaretto A.G., Rigo G.V., da Silva R.C., Tasca T., Macedo A.J., Carollo C.A., Silva D.B. Brown propolis-metabolomic innovative approach to determine compounds capable of killing Staphylococcus aureus biofilm and Trichomonas vaginalis. Food. Res. Int. 2018;111:661–673. doi: 10.1016/j.foodres.2018.05.033. [DOI] [PubMed] [Google Scholar]
- 69.Ambi A., Bryan J., Borbon K., Centeno D., Liu T., Chen T.P., Cattabiani T., Traba C. Are Russian propolis ethanol extracts the future for the prevention of medical and biomedical implant contaminations? Phytomedicine. 2017;30:50–58. doi: 10.1016/j.phymed.2017.03.006. [DOI] [PubMed] [Google Scholar]
- 70.Pepeljnjak S., Kosalec I. Galangin expresses bactericidal activity against multiple-resistant bacteria: MRSA, Enterococcus spp. and Pseudomonas aeruginosa. FEMS Microbiol. Lett. 2004;240:111–116. doi: 10.1016/j.femsle.2004.09.018. [DOI] [PubMed] [Google Scholar]
- 71.Fernandes Júnior A., Balestrin E.C., Betoni J.E., Orsi Rde O., da Cunha Mde L., Montelli A.C. Propolis: Anti-Staphylococcus aureus activity and synergism with antimicrobial drugs. Mem. Inst. Oswaldo. Cruz. 2005;100:563–566. doi: 10.1590/S0074-02762005000500018. [DOI] [PubMed] [Google Scholar]
- 72.Onlen Y., Duran N., Atik E., Savas L., Altug E., Yakan S., Aslantas O. Antibacterial activity of propolis against MRSA and synergism with topical mupirocin. J. Altern. Complement. Med. 2007;13:713–718. doi: 10.1089/acm.2007.7021. [DOI] [PubMed] [Google Scholar]
- 73.Krol W., Scheller S., Shani J., Pietsz G., Czuba Z. Synergistic effect of ethanolic extract of propolis and antibiotics on the growth of Staphylococcus aureus. Arzneimittelforschung. 1993;43:607–609. [PubMed] [Google Scholar]
- 74.Eliopoulos G.M., Moellering R.C., Jr. Antimicrobial combinations. In: Lorian V., editor. Antibiotics in Laboratory MedicineLorian. 4th ed. Wolters Kluwer|Williams & Wilkins Co.; Philadelphia, PA, USA: 1996. pp. 330–396. [Google Scholar]
- 75.Dimkić I., Ristivojević P., Janakiev T., Berić T., Trifković J., Milojković-Opsenica D., Stanković S. Phenolic profiles and antimicrobial activity of various plant resins as potential botanical sources of Serbian propolis. Ind. Crop. Prod. 2016;94:856–871. doi: 10.1016/j.indcrop.2016.09.065. [DOI] [Google Scholar]
- 76.Park Y.K., Alencar S.M., Aguiar C.L. Botanical origin and chemical composition of Brazilian propolis. J. Agric. Food. Chem. 2002;50:2502–2506. doi: 10.1021/jf011432b. [DOI] [PubMed] [Google Scholar]
- 77.Isidorov V.A., Bakier S., Pirożnikow E., Zambrzycka M., Swiecicka I. Selective behaviour of honeybees in acquiring European propolis plant precursors. J. Chem. Ecol. 2016;42:475–485. doi: 10.1007/s10886-016-0708-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Okińczyc P., Szumny A., Szperlik J., Kulma A., Franiczek R., Żbikowska B., Krzyżanowska B., Sroka Z. Profile of polyphenolic and essential oil composition of Polish propolis, black poplar and aspens buds. Molecules. 2018;23:E1262. doi: 10.3390/molecules23061262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Ristivojević P., Dimkić I., Guzelmeric E., Trifković J., Knežević M., Berić T., Yesilada E., Milojković-Opsenica D., Stanković S. Profiling of Turkish propolis subtypes: Comparative evaluation of their phytochemical compositions, antioxidant and antimicrobial activities. LWTFood Sci. Technol. 2018;95:367–379. [Google Scholar]
- 80.A Kuś P.M., Jerković I., Jakovljević M., Jokić S. Extraction of bioactive phenolics from black poplar (Populus nigra L.) buds by supercritical CO2 and its optimization by response surface methodology. J. Pharm. Biomed. Anal. 2018;152:128–136. doi: 10.1016/j.jpba.2018.01.046. [DOI] [PubMed] [Google Scholar]
- 81.B Kuś P.M., Okińczyc P., Jakovljević M., Jokić S., Jerković I. Development of supercritical CO2 extraction of bioactive phytochemicals from black poplar (Populus nigra L.) buds followed by GC–MS and UHPLC-DAD-QqTOF-MS. J. Pharm. Biomed. Anal. 2018;158:15–27. doi: 10.1016/j.jpba.2018.05.041. [DOI] [PubMed] [Google Scholar]
- 82.Kuś P., Congiu F., Teper D., Sroka Z., Jerkovi C.I., Tuberoso C.I.G. Antioxidant activity, color characteristics, total phenol content and general HPLC fingerprints of six Polish unifloral honey types. LWT Food Sci. Technol. 2013;55:124–130. doi: 10.1016/j.lwt.2013.09.016. [DOI] [Google Scholar]
- 83.CLSI . Performance Standards for Antimicrobial Susceptibility Testing; Seventeenth Informational Supplement. Clinical Laboratory Standard Institute; Wayne, PA, USA: 2007. CLSI document M100–S17. [Google Scholar]
- 84.Grecka K., Kuś P.M., Worobo R.W., Szweda P. Study of the anti-staphylococcal potential of honeys produced in Northern Poland. Molecules. 2018;23:E260. doi: 10.3390/molecules23020260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Kairo S.K., Bedwell J., Tyler P.C., Carter A., Corbel M.J. Development of a tetrazolium salt assay for rapid determination of viability of BCG vaccines. Vaccine. 1999;17:2423–2428. doi: 10.1016/S0264-410X(99)00023-7. [DOI] [PubMed] [Google Scholar]
- 86.Walencka E., Sadowska B., Rozalska S., Hryniewicz W., Rozalska B. Lysostaphin as a potential therapeutic agent for staphylococcal biofilm eradication. Pol. J. Microbiol. 2005;54:191–200. [PubMed] [Google Scholar]