Abstract
Objective
To evaluate quality of paediatric endoscopy training of Young members of the European Society for Paediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN).
Methods
An online questionnaire designed by the Young ESPGHAN Committee was sent to 125 Young ESPGHAN members between February 2014 and September 2015. The questionnaire comprised 32 questions addressing some general information of the participants and the structure of their paediatric gastroenterology, hepatology and nutrition programmes; procedural volume and terminal ileal intubation (TII) rate; supervision, assessments, participation in endoscopy courses and simulator training; and satisfaction with endoscopy training and self-perceived competency.
Results
Of 68 participants, 48 (71%) were enrolled in an official training programme. All alumni (n=31) were trained in endoscopy. They completed a median of 200 oesophagogastroduodenoscopies (OGDs) and 75 ileocolonoscopies (ICs) with a TII rate of >90% in 43%. There is a significant difference in numbers of ICs between the TII rate groups >90%, 50%–90% and <50% (median 150 vs 38 vs 55) (p<0.001). 11 alumni (35%) followed the ESPGHAN Syllabus during training. 25 alumni (81%) attended basic skills endoscopy courses and 19 (61%) experienced simulator training. 71% of the alumni were ‘(very) satisfied’ with their diagnostic OGD, while 52% were ‘(very) satisfied’ with their IC training. The alumni felt safe to independently perform OGDs in 84% and ICs in 71% after their training.
Conclusions
Despite reaching the suggested procedural endoscopy volumes, a rather low TII rate of >90% calls for end-of-training certifications based on the achievement of milestones of competency.
Keywords: gastrointesinal endoscopy, paediatric gastroenterology, colonoscopy, diagnostic and therapeutic endoscopy
Introduction
Paediatric gastroenterology, hepatology and nutrition (PGHN) training in Europe takes between 18 and 48 months, and in some countries, PGHN training is not recognised by their government or colleges of physicians.1 In 2014, the European Society for Paediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN) published a training syllabus as an important step towards a European certification and recognition of PGHN specialists with endoscopy as an integral part.1 The ESPGHAN Syllabus suggests 100 oesophagogastroduodenoscopies (OGDs) and 50 ileocolonoscopies (ICs) for certification. However, national training programmes in many countries use their own threshold as a surrogate for competence or none at all. It is acceptable that some endoscopy training and experience can be gained in the adult setting. However, it is of great importance that trainees have sufficient experience in children even below 10 kg.2
The trainees develop their skills by hands-on experience, and their competence is often assessed by subjective judgement and by an arbitrary volume with a variable approach across Europe. Trainees progress at a variable pace and most require more procedures than the 2014 ESPGHAN Syllabus has suggested.3 4 Patient-centred quality and competency-based training have become two important aspects in paediatric endoscopy assessment.5 6 Besides the Gastrointestinal Endoscopy Competency Assessment Tool for paediatric colonoscopy (GiECATKIDS), which is a tool with strong evidence of reliability and validity,7 the Direct Observational Procedure Skill (DOPS) has been developed in the UK and has proven to enhance endoscopy training and thus increase satisfaction of PGHN trainees.4 The DOPS is a valid workplace-based assessment tool that reliably assesses skills and facilitates certification of competence and credentialing of endoscopists.8
The competence thresholds outlined in adult and paediatric OGD and IC guidelines vary widely, and most data for paediatric recommendations are extrapolated from those identified in adult endoscopic studies3 9–11 (table 1).
Table 1.
Suggested procedural volumes of OGDs and ICs in different societies
| Society | OGDs | ICs | Literature |
| ESPGHAN | 100 | 50 | 1 |
| NASPGHAN | 100 | 120 | 3 |
| ASGE | 130 | 275 | 22 |
| ESGE | No suggestion | No suggestion | 14 23 |
ASGE, American Society for Gastrointestinal Endoscopy; ESGE, European Society of Gastrointestinal Endoscopy; ESPGHAN, European Society for Paediatric Gastroenterology, Hepatology and Nutrition; ICs, ileocolonoscopies; NASPGHAN, North American Society for Pediatric Gastroenterology, Hepatology and Nutrition; OGDs, oesophagogastroduodenoscopies.
This is not satisfactory for obvious reasons including but not limited to lower patient numbers, general anaesthesia issues, patient size variability and the different pathologies compared with adult endoscopy.
The aims of this survey were to examine:
The quality of endoscopy training during PGHN training as described by the structure of endoscopy training, procedural volume and terminal ileal intubation (TII) rate, availability of supervision and assessment and possibilities to take part in training courses and simulator training.
The self-perceived competency in performing endoscopy safely and efficiently and the trainees’ readiness to enter practice without direct supervision.
Materials and methods
Study design
An online questionnaire using general available software (SurveyMonkey) was designed by the Young ESPGHAN Committee and sent to 125 Young ESPGHAN members between February 2014 and September 2015. Monthly reminders to fill the questionnaires were sent by email. Inclusion criteria were ESPGHAN membership and less than 10 years experience in PGHN, which is the definition of Young ESPGHAN membership. The questionnaire was approved by the ESPGHAN Endoscopy Working Group. This manuscript was drafted along the ‘Strengthening the Reporting of Observational Studies in Epidemiology’ guideline for reporting observational studies.
Survey
The questionnaire is shown in online supplementary table S1. The questionnaire comprised 32 questions. The first set of questions addressed some general information of the participants (country of training and level of training) and the structure of their PGHN programmes (time devoted to endoscopy and difficulties encountered in the pursuit of their paediatric endoscopy training). The second set of questions investigated procedural volume and TII rate. In a third set of question supervision, assessments, participation in endoscopy courses and simulator training, the use of the ESPGHAN Syllabus as well as accreditation was addressed. A fourth set of questions assessed satisfaction with endoscopy training and their self-perceived readiness to enter practice as an independent endoscopy practitioner.
flgastro-2018-101007supp001.pdf (305.5KB, pdf)
Statistics
Statistical analysis was performed using IBM SPSS Statistics V.23. Data were described using median (IQR), range and percentages. We used the analysis of variance test for continuous variables and the χ2 test for categorical variables. All reported p values are two sided, and p values <0.05 were considered statistically significant.
Results
General information
Seventy-eight participants from 28 countries, of which 20 were countries belonging to ESPGHAN, participated in the survey (response rate 78 out of 125 Young ESPGHAN members (62%)) (table 2).
Table 2.
Participants from ESPGHAN countries that completed the questionnaire
| Country of training | Number of participants | PGHN programme (yes/no) |
Trained in endoscopy (yes/no) | Number finished with training |
| Albania | 2 | 1 yes/1 no | Yes | 2 |
| Austria | 1 | Yes | Yes | 1 |
| Belgium | 3 | 2 yes/1 no | Yes | 1 |
| Croatia | 1 | Yes | Yes | 1 |
| Czech Republic | 1 | Yes | Yes | 0 |
| Denmark | 1 | Yes | Yes | 1 |
| Finland | 2 | Yes | Yes | 1 |
| France | 1 | Yes | Yes | 0 |
| Germany | 9 | Yes | Yes | 7 |
| Greece | 3 | No | Yes | 2 |
| Hungary | 2 | Yes | Yes | 0 |
| Israel | 3 | 2 yes/1 no | Yes | 1 |
| Italy | 5 | No | 1 yes/4 no | 0 |
| Poland | 1 | Yes | Yes | 0 |
| Portugal | 6 | 2 yes/4 no | Yes | 2 |
| Russia | 2 | Yes | No | 0 |
| Spain | 3 | 1 yes/2 no | Yes | 3 |
| Sweden | 3 | No | Yes | 2 |
| Switzerland | 3 | Yes | Yes | 2 |
| UK | 16 | Yes | Yes | 5 |
| 20 countries | 68 participants | 31 finished with training |
ESPGHAN, European Society for Paediatric Gastroenterology, Hepatology and Nutrition; PGHN, paediatric gastroenterology, hepatology and nutrition.
Ten participants had to be excluded from further analysis as they were trained outside of countries belonging to the ESPGHAN. Thirty-seven participants were still in PGHN training, and 31 had finished their training (so-called training alumni). Among all participants, 48 (71%) reported being enrolled in an official PGHN programme leading to a subspecialty certification. The structure and the content of the PGHN training programmes were very heterogeneous even within the same countries. All training alumni were trained in endoscopy, of which 16 (52%) had dedicated their entire time to PGHN and 15 (48%) between 50% and 99%. The alumni ascribed difficulties in accessing endoscopy training to the following: elective duties (n=12; 39%); emergency duties (n=13; 42%); absence of lists, that is, insufficient amount of procedures during a given time (n=13; 42%); and competition with surgical trainees (n=4; 13%). Two alumni (6%) did not wish to train in endoscopy, eight (26%) were partially trained by adult gastroenterologists and one (3%) alumnus was trained by surgeons.
Endoscopic procedures and TII rate
Concerning procedural volume, the training alumni (n=31) had performed a median of 200 OGDs (IQR 150–300) and 75 ICs (IQR 30–150) at the end of their PGHN training (online supplementary table S2). Only 19 (61%) alumni had fulfilled the ESPGHAN criteria (100 OGDs and 50 ICs) by the end of their training (figure 1). The minimal number of procedures needed for certification is 100 upper (IQR 50–100) and 50 lower gastrointestinal (GI) endoscopies (IQR 50–100) in the trainees’ countries of all participants. Three training alumni did not perform any ICs. Thirteen of 28 (46%) training alumni achieved a TII rate of >90%, 13 (46%) had achieved a rate of 50%–90% and 2 (7%) of less than 50%. There is a significant difference in number of colonoscopies between the groups TII rate >90%, 50%–90% and <50% (median 150 vs 38 vs 55) (p<0.001) (figure 2). However, there is no significant difference in the use of the ESPGHAN Syllabus between the three TII rate groups: >90%, 50%–90% and <50% (42% vs 21% vs 50% used the syllabus).
Figure 1.
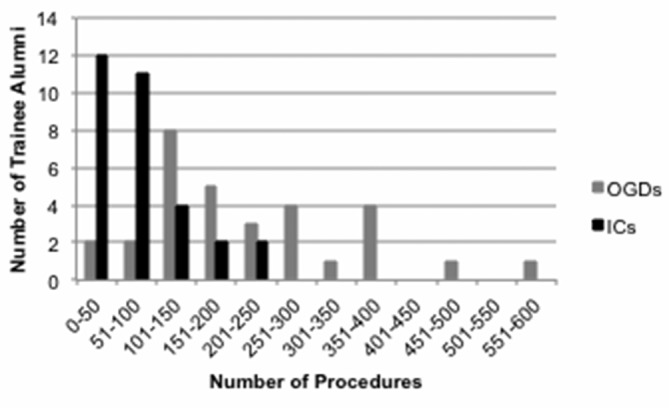
Procedural volume (OGDs and ICs) performed by the trainees (n=31) who finished their PGHN training. ICs, ileocolonoscopies; OGDs, oesophagogastroduodenoscopies; PGHN, paediatric gastroenterology, hepatology and nutrition.
Figure 2.
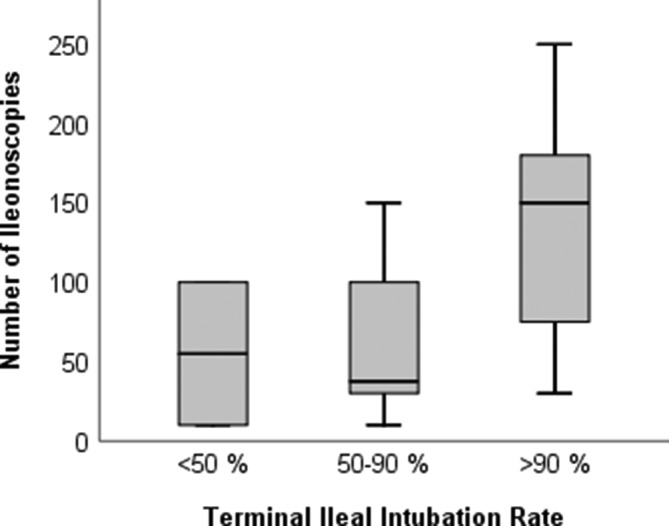
Boxplots with TII rate ((1) >90% (n=13), (2) 50%–90% (n=13), (3)<50% (n=2)) vs number of ICs of the trainees who finished their training. Whiskers depict maximum and minimum number of colonoscopies. ICs, ileocolonoscopies; TII, terminal ileal intubation.
flgastro-2018-101007supp002.pdf (79.7KB, pdf)
Concerning interventional endoscopy, PGHN trainee alumni (n=31) have completed a median of five polypectomies (n=22), three foreign body retrievals (n=19), two PEG insertions (n=19) and three PEG changes (n=19) (online supplementary table S2). Some have also gained experience in video capsule endoscopy (n=9), endoscopic placement of video capsule (n=11), rectal biopsies for Hirschsprung’s disease (n=9), variceal banding ligations (n=14), sclerotherapy of varices (n=6), Bravo probe placements (n=5), balloon dilatations (n=13), stricture dilatations (n=6), ERCP (n=2) and double balloon endoscopy (n=1) (online supplementary table S2).
Supervision, assessment and training in endoscopy
Twenty-four (77%) alumni experienced continuous supervision; 28 (90%) kept an endoscopy logbook, but only 6 (19%) had formal assessments (paper or online) during and 15 (48%) at the end of their training. During training, 11 (35%) alumni followed the ESPGHAN Syllabus.
Twenty-five (81%) training alumni attended basic skills endoscopy courses and 19 (61%) experienced endoscopy simulator training. There were no significant differences in the TII rate in those trainee alumni who underwent simulator training and those who did not. The vast majority of training alumni (n=30 (97%)) wished participation in future ESPGHAN Endoscopy Summer Schools and 31 (100%) would have liked to attend basic endoscopy skills courses. Twenty-one (68%) training alumni would like ESPGHAN to be responsible for the accreditation of Endoscopy Training Centres.
Satisfaction with endoscopy training
Among the training alumni, 10 (32%) were ‘very satisfied’ and 12 (39%) were ‘satisfied’ with the level of their diagnostic upper GI endoscopy training, but only 3 (10%) were ‘very satisfied’ and 13 (42%) were ‘satisfied’ with their IC training. Concerning interventional GI endoscopy training, only three (10%) training alumni were ‘very satisfied’ and four (13%) were ‘satisfied’.
When asked if their endoscopic training would allow them to perform as an independent practitioner at the end of their training, 26 (84%) alumni felt that their upper GI endoscopy training would allow this and 22 (71%) felt that their IC training would do so.
Discussion
The aims of this survey were to examine the quality of endoscopy training during PGHN training and the self-perceived competency in performing endoscopy safely and efficiently and the trainees’ readiness to enter practice without direct supervision.
Key findings
The median procedural volume (200 OGDs (IQR 150–300) and 75 ICs (IQR 30–150)) performed by the PGHN alumni in our survey exceeds the numbers suggested by the ESPGHAN Syllabus with wide variations between the countries. However, a TII rate of >90% was accomplished by only 43% of the alumni, which is low compared with TII rates of 72%–97% reported in the literature.3 5 Fifty per cent admitted to TII rates of only 50%–90% and worryingly 7% admitted to a TII rate of <50%. There is a significant difference in number of colonoscopies between the groups TII rate >90%, 50%–90% and <50% (median 150 vs 38 vs 55) (p<0.001) (figure 2). There exists a remarkable discrepancy between procedural volume and the TII rate. Compared with sister societies, the suggested procedural volume is too low to reach competence (table 1).12 Looking at a recent large study investigating the number of procedures required to achieve competency in colonoscopy, a caecal intubation rate of >90% was reached only after 233 procedures on average.13 Minimal numbers of procedures have shown not to be a reliable quality measure for competence8 11 13–15 (table 1). A move towards a competency-based model is preferable, but until this is widespread, the surrogate ‘procedural volume’ needs to be revised significantly especially for ICs.
Seventy-one per cent of the alumni were ‘(very) satisfied’ with their diagnostic OGD, while 52% were ‘(very) satisfied’ with their IC training. However, the alumni felt safe and competent for OGDs in 84% and for ICs in 71%. There is a gap between the trainees’ satisfaction and their perception of competency suggesting the need for objective markers of competence. The level of ‘dis’-satisfaction indicates an urgent need to improve paediatric endoscopy training in Europe. A competency-based model with objective key performance measures will increase satisfaction of the trainees.
Strengths and weaknesses of our survey
The survey mirrors the important variability of paediatric endoscopy training in ESPGHAN countries, which has been described previously.16 According to previous work, the length of PGHN training in Europe varies between 18 months and 48 months.1 There are countries without subspecialty certification or even without an established PGHN subspecialty programme, and some PGHN programmes do not train in paediatric endoscopy at all (table 2).
The limitations of this survey are that the number of respondents per country was low, and therefore, statistical analysis is not feasible to detect differences between training programmes and countries. This is due to low numbers of PGHN trainees compared with adult gastroenterology trainees, especially in the smaller European countries. The PGHN trainees who are ESPGHAN members were our primary target group, as this group will be preferentially able to participate in ESPGHAN educational events. The procedural volume numbers are self-reported, and hence, there is no control by the respective PGHN training centres. Furthermore, we have no specific information on the patients (below 10 kg body weight; adults). We did not assess the time to complete an IC and did not inquire if the procedure was performed independently or with assistance. Furthermore, we did not assess sedation or patient comfort, which would have a bearing on procedure completion rates.
Implications for the future
There is a need for improved endoscopy training. The accent should shift from procedural volume to procedural assessment of competency. DOPS assessments at the beginning and end of training should be instituted in each European country and policed rigorously as occurs in most adult and in some paediatric endoscopy centres already.17 By filling a log book with self-assessment, the trainee may identify where intensified support and training is needed. Concerning low procedural volumes, the US American PGHN Fellowship Programmes concluded that PGHN trainees should have access to endoscopy hands-on courses and have the opportunity to rotate to adult GI training centres.12 18 Training in an adult endoscopy centre can add to enhancing the learning curve. Therefore, we suggest that cooperation between adult and paediatric endoscopists is valuable and essential in paediatric endoscopy training. Training options include e-learning tools, textbooks, hands-on courses with virtual models, manikins, animal explanted models and also live hands-on intensive patient training courses in dedicated training centres. Endoscopy fellowships will help to allow trainees to receive training in larger paediatric endoscopy training centres.15 19 There is a need for paediatric endoscopy trainers with requisite skills for training, and train-the-trainers workshops are increasingly offered to paediatric endoscopists. Training centres would benefit from a training lead, which can ensure that the trainees receive sufficient protected endoscopy training time to achieve competency, and this should be documented electronically and assessed continuously with objective procedural tools such as the DOPS.7 20 21
Conclusions
We could show that the suggested procedural volume is not sufficient to assess competency in endoscopy. There is a strong discrepancy between feeling competent at the end of training and the achieved competency as assessed by the TII rate. There is a need for improved endoscopy education, and steps have been taken to further this development within Europe under the auspices of ESPGHAN which, we suggest, should become the overarching accreditation body for paediatric endoscopy training in Europe.
Significant of this study.
What is already known on this topic
Training in paediatric endoscopy is very heterogeneous throughout Europe.
National training programmes in many countries use procedural volume as a surrogate for competence in paediatric endoscopy.
What this study adds
Despite exceeding the median procedural volume suggested by the ESPGHAN Syllabus with wide variations between the countries, a terminal ileal intubation (TII) rate of >90% was accomplished by only 43% of the alumni.
There is a gap between the trainees’ satisfaction and their perception of competency, as 71% of the alumni were ‘(very) satisfied’ with their diagnostic oesophagogastroduodenoscopy (OGD) and 52% were ‘(very) satisfied’ with their ileocolonoscopy (IC) training, whereas they felt safe and competent for OGDs in 84% and for ICs in 71%.
How might it impact on clinical practice in the foreseeable future
The accent in endoscopy training should shift from procedural volume to assessment of competency.
In the case of low procedural volumes, trainees should have access to hands-on courses, have the opportunity to rotate to adult gastroenterology training centres and be able to train with e-learning tools.
The results of this survey are a further incentive to homogenise endoscopy training within Europe.
Footnotes
Contributors: IJB, JJ and CT designed the survey; IJB, JJ, NM, HvdD, AE and CT acquired, analysed and interpreted the data; IJB drafted the work; JJ, NM, HvdD, AE, JAD, MT and CT revised the paper critically for important intellectual content; all authors gave final approval of the version to be published and are in agreement to be accountable for all aspects of the work.
Funding: The European Society for Pediatric Gastroenterology, Hepatology and Nutrition.
Competing interests: JAD reports personal fees from Nestlé, Danone, Pharmakern and Abbvie; NM reports personal fees from Nestle; MT reports personal fees from Danone/Nutricia and Movetis, grants from Mead Johnson, Jansen, Nestle, Dubai Arab Paediatric Society, Norgine, Astra-Zeneca, Reckitt-Benckeiser, Movetis and Cook; CT reports personal fees from Abbvie.
Patient consent: Not required.
Ethics approval: The study was reviewed and approved by the University of Cologne Institutional Review Board, Cologne, Germany. A copy of the ethical approval documents is uploaded in PDF format as a supplemental file.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: All data are presented in the manuscript and supplementary material; no additional data are available.
References
- 1. D’Antiga L, Nicastro E, Papadopoulou A, et al. European society for pediatric gastroenterology, hepatology, and nutrition syllabus for subspecialty training: moving towards a European standard. J Pediatr Gastroenterol Nutr 2014;59:417–22. 10.1097/MPG.0000000000000464 [DOI] [PubMed] [Google Scholar]
- 2. BSPGHAN Endoscopy Working Group. JAG paediatric endoscopy certification, version 2.1, 2014. [Google Scholar]
- 3. Leichtner AM, Gillis LA, Gupta S, et al. NASPGHAN guidelines for training in pediatric gastroenterology. J Pediatr Gastroenterol Nutr 2013;56 Suppl 1(Suppl 1):S1–S8. 10.1097/MPG.0b013e31827a78d6 [DOI] [PubMed] [Google Scholar]
- 4. Hinds R, Thomson M. Pediatric ileocolonoscopy training: acquisition of endoscopic skill must be nurtured and objectively assessed within a formalized pediatric framework. J Pediatr Gastroenterol Nutr 2007;45:1–2. 10.1097/MPG.0b013e318054d02d [DOI] [PubMed] [Google Scholar]
- 5. Thomson J, Shah SS. Is Pediatric long-term care the next frontier in infection prevention and control? JAMA Pediatr 2017;171:835 10.1001/jamapediatrics.2017.1752 [DOI] [PubMed] [Google Scholar]
- 6. Dubé C, Rostom A. Acquiring and maintaining competency in gastrointestinal endoscopy. Best Pract Res Clin Gastroenterol 2016;30:339–47. 10.1016/j.bpg.2016.05.004 [DOI] [PubMed] [Google Scholar]
- 7. Walsh CM, Ling SC, Walters TD, et al. Development of the gastrointestinal endoscopy competency assessment tool for pediatric colonoscopy (GiECAT KIDS). J Pediatr Gastroenterol Nutr 2014;59:480–6. 10.1097/MPG.0000000000000358 [DOI] [PubMed] [Google Scholar]
- 8. Barton JR, Corbett S, van der Vleuten CP, et al. The validity and reliability of a Direct Observation of Procedural Skills assessment tool: assessing colonoscopic skills of senior endoscopists. Gastrointest Endosc 2012;75:591–7. 10.1016/j.gie.2011.09.053 [DOI] [PubMed] [Google Scholar]
- 9. Group., B.E.W. JAG Paediatric Endoscopy Certification, version 2.1, 2014. [Google Scholar]
- 10. Patel SG, Keswani R, Elta G, et al. Status of competency-based medical education in endoscopy training: a nationwide survey of US ACGME-Accredited Gastroenterology Training Programs. Am J Gastroenterol 2015;110:956–62. 10.1038/ajg.2015.24 [DOI] [PubMed] [Google Scholar]
- 11. Walsh CM. In-training gastrointestinal endoscopy competency assessment tools: types of tools, validation and impact. Best Pract Res Clin Gastroenterol 2016;30:357–74. 10.1016/j.bpg.2016.04.001 [DOI] [PubMed] [Google Scholar]
- 12. Lerner DG, Li BU, Mamula P, et al. Challenges in meeting fellowship procedural guidelines in pediatric therapeutic endoscopy and liver biopsy. J Pediatr Gastroenterol Nutr 2014;58:27–33. 10.1097/MPG.0000000000000184 [DOI] [PubMed] [Google Scholar]
- 13. Ward ST, Mohammed MA, Walt R, et al. An analysis of the learning curve to achieve competency at colonoscopy using the JETS database. Gut 2014;63:1746–54. 10.1136/gutjnl-2013-305973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Bisschops R, Areia M, Coron E, et al. Performance measures for upper gastrointestinal endoscopy: a European Society of Gastrointestinal Endoscopy (ESGE) Quality Improvement Initiative. Endoscopy 2016;48:843–64. 10.1055/s-0042-113128 [DOI] [PubMed] [Google Scholar]
- 15. Forbes N, Mohamed R, Raman M. Learning curve for endoscopy training: is it all about numbers? Best Pract Res Clin Gastroenterol 2016;30:349–56. 10.1016/j.bpg.2016.04.003 [DOI] [PubMed] [Google Scholar]
- 16. Lentze MJ. Challenge of meeting fellowship procedural guidelines in therapeutic endoscopy and liver biopsy. J Pediatr Gastroenterol Nutr 2014;58:3–4. 10.1097/MPG.0000000000000182 [DOI] [PubMed] [Google Scholar]
- 17. Anderson JT. Assessments and skills improvement for endoscopists. Best Pract Res Clin Gastroenterol 2016;30:453–71. 10.1016/j.bpg.2016.05.005 [DOI] [PubMed] [Google Scholar]
- 18. Kadzielski SM, Winter HS. Novel methods for training future pediatric gastroenterologists. J Pediatr Gastroenterol Nutr 2014;58:2–3. 10.1097/MPG.0000000000000183 [DOI] [PubMed] [Google Scholar]
- 19. Zanchetti DJ, Schueler SA, Jacobson BC, et al. Effective teaching of endoscopy: a qualitative study of the perceptions of gastroenterology fellows and attending gastroenterologists. Gastroenterol Rep 2016;4:125–30. 10.1093/gastro/gow003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Valori RM, Johnston DJ. Leadership and team building in gastrointestinal endoscopy. Best Pract Res Clin Gastroenterol 2016;30:497–509. 10.1016/j.bpg.2016.04.007 [DOI] [PubMed] [Google Scholar]
- 21. James PD, Antonova L, Martel M, et al. Measures of trainee performance in advanced endoscopy: a systematic review. Best Pract Res Clin Gastroenterol 2016;30:421–52. 10.1016/j.bpg.2016.05.003 [DOI] [PubMed] [Google Scholar]
- 22. Faulx AL, Lightdale JR, Acosta RD, et al. Guidelines for privileging, credentialing, and proctoring to perform GI endoscopy. Gastrointest Endosc 2017;85:273–81. 10.1016/j.gie.2016.10.036 [DOI] [PubMed] [Google Scholar]
- 23. Kaminski MF, Thomas-Gibson S, Bugajski M, et al. Performance measures for lower gastrointestinal endoscopy: a European Society of Gastrointestinal Endoscopy (ESGE) quality improvement initiative. Endoscopy 2017;49:378–97. 10.1055/s-0043-103411 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
flgastro-2018-101007supp001.pdf (305.5KB, pdf)
flgastro-2018-101007supp002.pdf (79.7KB, pdf)


