Abstract
The Joint Advisory Group on Gastrointestinal Endoscopy (JAG) was initially established in 1994 to standardise endoscopy training across specialties. Over the last two decades, the position of JAG has evolved to meet its current role of quality assuring all aspects of endoscopy in the UK to provide the highest quality, patient-centred care. Drivers such as changes to healthcare agenda, national audits, advances in research and technology and the advent of population-based cancer screening have underpinned this shift in priority. Over this period, JAG has spearheaded various quality assurance initiatives with support from national stakeholders. These have led to the achievement of notable milestones in endoscopy quality assurance, particularly in the three major areas of: (1) endoscopy training, (2) accreditation of endoscopy services (including the Global Rating Scale), and (3) accreditation of screening endoscopists. These developments have changed the landscape of UK practice, serving as a model to promote excellence in endoscopy. This review provides a summary of JAG initiatives and assesses the impact of JAG on training and endoscopy services within the UK and beyond.
Keywords: gastrointesinal endoscopy, health service research, diagnostic and therapeutic endoscopy
Introduction
The role of Joint Advisory Group on Gastrointestinal Endoscopy (JAG) in quality assurance (QA)
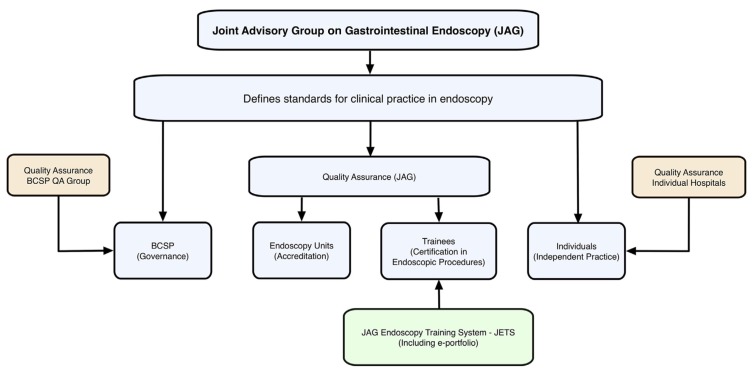
QA is the process of monitoring and assessing a product, service or process to ensure that it is of sufficient quality.1 In the 1990s, the expansion and multidisciplinary nature of endoscopy led to calls for a unified advisory body to quality assure endoscopy training.2 Thus, the JAG was established in 1994 under the auspices of the Academy of Royal Medical Colleges with committee members from the Royal Colleges of Physicians, Royal Colleges of Surgeons, Royal Colleges of Radiologists and Royal Colleges of General Practitioners. Although the initial focus was on standardising training between specialties, the role of JAG has progressively evolved to meet its current vision of quality assuring all aspects of endoscopy to provide the highest quality, patient-centred care. Over the last two decades, drivers such as changes to healthcare agenda, national audits, advances in research and technology and the advent of population-based cancer screening have been key in this shift in priority.3 Over this period, JAG has spearheaded various QA initiatives with support from other national stakeholders including the Department of Health (DoH), British Society of Gastroenterology (BSG), Association of Coloproctology of Great Britain and Ireland (ACPGBI), Association of Upper GI Surgeons and Specialist Advisory Committees (SACs). These have led to the achievement of notable milestones in endoscopy QA (table 1), establishing its role in the three major areas of: (1) training, (2) accreditation of services and (3) accreditation of screening endoscopists (figure 1). These developments have changed the landscape of endoscopy practice in the UK and serve as a model to promote excellence in endoscopy. This review provides a summary of JAG initiatives and assesses the impact of JAG on training and endoscopy services within the UK and beyond.
Table 1.
Timeline of JAG achievements and corresponding drivers
| Year | JAG milestone | Driver(s) |
| 1994 | JAG established. | |
| 1999 | First JAG position statement: ‘Recommendations for training in GI endoscopy’. | |
| 2002 | First JAG committee meeting. | |
| 2003 | Development of endoscopy modernisation England – NHS endoscopy toolkit. | DoH support |
| 2004 | GRS piloted – part of NEP, aligned with JAG. | DoH support |
| ‘Guidelines for training, appraisal and assessment of trainees in GI endoscopy and for the Assessment of units for Registration and Re-Registration’. Endoscopy curriculum. DOPS in formative and summative assessment. |
NCEPOD ‘Scoping Our Practice’ 1st National Colonoscopy Audit |
|
| Early preparation for JAG QA visits. | DoH support | |
| 2005 | National endoscopy training programme established. | DoH support, SACs |
| Endoscopy GRS handover to JAG to underpin accreditation. | ||
| Bowel Cancer Screening Programme (BCSP). | ||
| 2006 | Endoscopy service accreditation commenced to coincide with BCSP. | |
| 2007 | BSG Quality and Safety Indicators for Endoscopy document released. | |
| 2008 | Gastrointestinal Endoscopy for Nurses programme commenced. | NEP |
| 2009 | Formal handover of NEP work and all outputs to JAG. | |
| Release of JETS e-Portfolio. | ||
| National Nurse Endoscopist project linked to training centres. | DoH support | |
| GRS introduced for private providers. | ||
| 2011 | JAG GRS released for use in New Zealand and Ireland. | |
| Electronic e-certification (diagnostic upper GI endoscopy, flexible sigmoidoscopy and colonoscopy). | 2nd National Colonoscopy Audit, Full BCSP Roll-out. |
|
| First DOPyS. | ||
| 2013 | National Endoscopy Database project started. | |
| JAG formally take on administration and governance of BCSP accreditation from Public Health England. | ||
| Best Practice Tariff for JAG-accredited units. | DoH support | |
| BCSP Bowel Scope accreditation started. | ||
| 2016 | Updated Global Rating Scale census and JAG accreditation standards released. | |
| Updated DOPS forms and trainee certification criteria released. | ||
| 2017 | JAG Research Group formed. |
BCSP, Bowel Cancer Screening Programme; BSG, British Society of Gastroenterology; DoH, Department of Health; DOPS, direct observation of procedural skills; DOPyS, direct observation of polypectomy skills; GRS, Global Rating Scale; JAG, Joint Advisory Group on Gastrointestinal Endoscopy; JETS, JAG Endoscopy Training System; QA, quality assurance; NCEPOD, National Confidential Enquiry into Patient Outcome and Death; NEP, National Endoscopy Programme; SAC, Specialist Advisory Committee.
Figure 1.
The role of JAG.12 Courtesy of Dr John Anderson. BCSP, Bowel Cancer Screening Programme.
Training
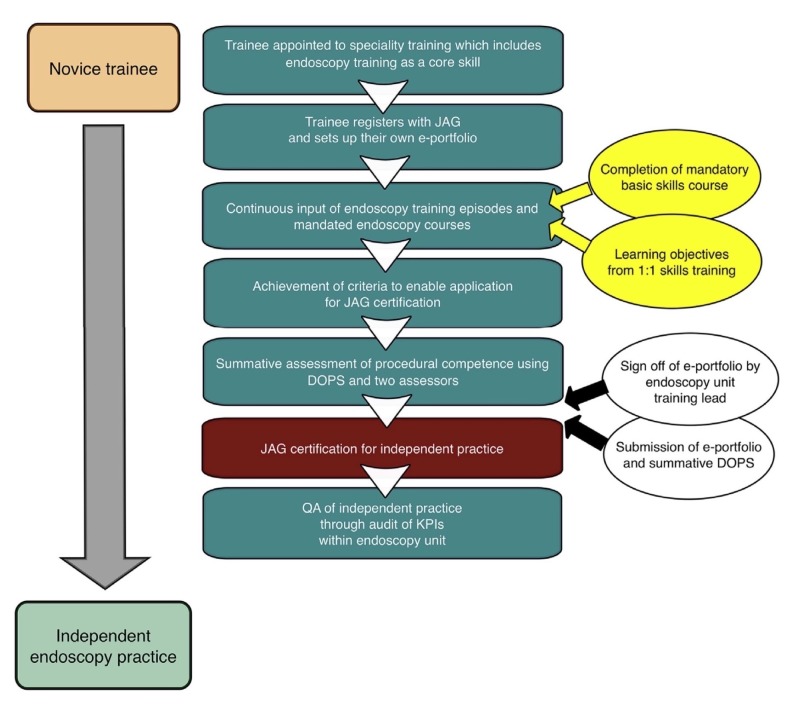
The unacceptable standards of practice reported in the 1999 UK colonoscopy audit,4 in anticipation of national bowel cancer screening, raised questions over workforce competence. This catalysed a review of endoscopy training, which identified clear needs for defining standards for competent practice, methods for assessing competence and a structured endoscopy curriculum. In response, these elements were covered in a seminal 2004 JAG document,5 which also called for training units to have shared responsibility in ensuring trainee competence. The concept of certification was proposed, which relied on trainee adoption of a ‘JAG logbook of experience’, engagement in summative assessment and supervisor sign-off.5 Direct observation of procedural skills (DOPS) and direct observation of procedural polypectomy skills (DOPyS) were introduced to standardise assessment, and highly focused courses were developed for trainees and trainers. JAG-approved basic upper and lower GI endoscopy courses became compulsory for certification, while specific training-the-trainer courses evolved to improve training standards at base hospitals. The guideline formed the foundations for quality assurance of training (QA-T) and service accreditation (described below).
In 2009, the JAG Endoscopy Training System (JETS) was launched. It had four main purposes: (1) an electronic record of trainee procedural experience and assessment, (2) a portal for accessing training courses, (3) to provide evidence of trainees meeting JAG standards of competence and (4) to provide feedback to trainers and training course organisers.1 6 JETS enabled trainee competence to be monitored and determined centrally, paving the way for e-certification, which began in 2011 for upper and lower gastrointestinal (GI) endoscopy (figure 2). By January 2017, JETS had been adopted in >250 UK training centres, with 2857 instances of e-certification awarded.7 JAG training courses are now regularly delivered in 28 UK centres, comprising 10 types of basic skills courses, 9 skills improvement courses and 4 endoscopy trainer courses.8 JAG have also supported non-medical endoscopists and endoscopy nurses via the GI Endoscopy for Nurses programme.
Figure 2.
JAG trainee certification pathway.12 Courtesy of Dr John Anderson. DOPS, direct observation of procedural skills; JAG, Joint Advisory Group on Gastrointestinal Endoscopy; KPIs, key performance indicators; QA, quality assurance.
Accreditation of services
Shortly after publication of the national colonoscopy audit,4 the 2004 National Confidential Enquiry into Patient Outcome and Death (NCEPOD) report: ‘Scoping our Practice’ also highlighted shortfalls in quality of care.9 The expectation for individual endoscopy units to meet quality standards of care led to centralised accreditation of endoscopy units being proposed in the 2004 JAG position statement.10 The Global Rating Scale (GRS) was developed in 2004 as a quality improvement tool for endoscopy units to self-assess against a number of measures associated with high-quality and safe patient-centred care.11 The GRS assesses patient experience within four domains (table 2), each with corresponding items. Items are scored A–D, with level B indicating attainment of minimum requirements, with level A being an aspirational target for high performing services. To be accredited, units are required to achieve at least level B in all GRS domains and provide substantiating evidence. Service standards are inspected through a peer-review site visit by trained JAG assessors. During the site visit, the unit environment is also assessed to evaluate privacy, dignity and safe decontamination practices. Once awarded, accreditation is renewed annually, with services required to provide interim evidence of eligibility via the annual report card.
Table 2.
The four GRS domains and their corresponding items
| Domains | Clinical quality | Quality of the patient experience | Workforce | Training of endoscopists |
| Items |
|
|
|
|
By 2005, service accreditation achieved national roll-out and became required for services wishing to contribute to bowel cancer screening in England. A JAG subcommittee, now known as the Endoscopy Services Quality Assurance Group, administers and regulates the data collected. In 2013, the Best Practice Tariff was commissioned by the DoH in England, thereby enabling higher rates of reimbursement for accredited units. Additionally, service accreditation become a prerequisite for Trusts to receive trainees in endoscopy,12 further incentivising units to participate in the QA process.
Today, the GRS has evolved into a web-based tool for unit-level quality improvement (figure 3). The GRS is in place in 485 UK units, with 228 units (47%) achieving full JAG accreditation in August 2017.11
Figure 3.
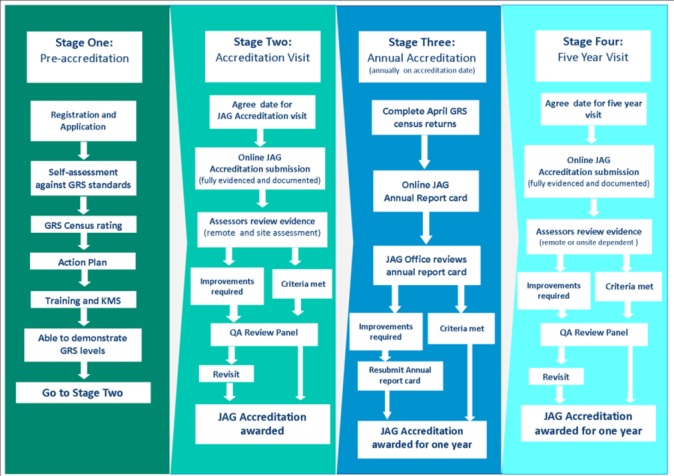
JAG unit accreditation pathway. GRS, Global Rating Scale; JAG, Joint Advisory Group on Gastrointestinal Endoscopy; KMS, Knowledge Management System; QA, quality assurance.
Accreditation of screening endoscopists
The Bowel Cancer Screening Programme (BCSP) operates on the observation that population-based endoscopic screening reduces colorectal cancer (CRC) incidence and mortality.13 In England, the BCSP commenced roll-out in 2006 for colonoscopy and 2013 for flexible sigmoidoscopy (Bowel Scope) screening. At the outset of screening, the Screening Assessment and Accreditation System (SAAS) was launched to quality assure the endoscopists within BCSP.4 In order to achieve accreditation, endoscopists are required to provide evidence of locally verified key performance indicators (KPIs), complete knowledge-based assessments and demonstrate competence in summative assessment (figure 4).
Figure 4.
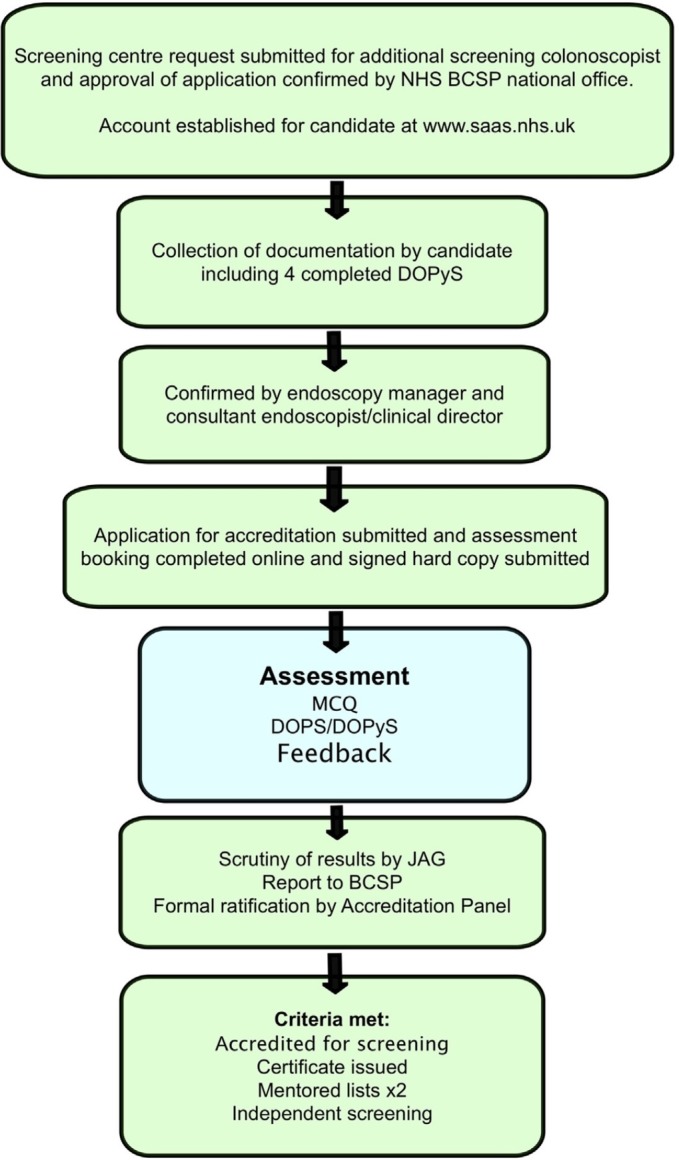
BCSP accreditation pathway.12 Courtesy of Dr John Anderson. BCSP, Bowel Cancer Screening Programme; DOPS, direct observation of procedural skills; DOPyS, direct observation of polypectomy skills; JAG, Joint Advisory Group on Gastrointestinal Endoscopy; MCQ, Multiple Choice Questionnaire; NHS, National Health Service.
Aims
The primary aim of this review was to amalgamate published evidence supporting the impact of JAG on quality of care (ie, patient outcomes), services or training in endoscopy. Secondary aims included assessing the impact of JAG on (1) service implementation and (2) research, where JAG tools were integral to the design.
Methods
Search strategy
In order to assess the impact of JAG, a comprehensive literature search was conducted in July 2017 through Embase, Ovid and PubMed to identify relevant publications and conferences abstracts over the last 10 years. The search strategy involved the combination of the following terms: (‘Joint Advisory Group’ or ‘JAG’ or ‘Global Rating Scale’ or ‘JETS e-portfolio’ or ‘DOPS’ or ‘DOPyS’ or ‘bowel screening’) AND (‘endoscopy’ or ‘colonoscopy’ or ‘polypectomy’ or ‘accreditation’). Studies were limited to those in English, with accompanying abstracts, and those published after January 2007.
Inclusion and exclusion criteria
To enable summation of the literature search results, thematic analysis was used to summarise suitable publications into the following categories: (A) quality of care, for example, KPIs related to patient outcomes such as caecal intubation rate (CIR); (b) quality of service provision, for example, waiting times; and (C) quality of training, for example, trainee performance/satisfaction
For each category, studies were subdivided based on: (A) impact; and (B) implementation: these may demonstrate impact, but specifically include studies where JAG tools/recommendations have resulted in quality improvement of patient or trainee-centred services.
For duplicate abstracts, either the full paper was referenced or the earliest instance was selected.
Data extraction
Data from eligible articles were extracted into tables to summarise the literature review. Column headings included: (A) first author, (B) year of publication (full papers marked with an asterisk), (C) country, (D) JAG division (ie, training/service accreditation/SAAS), (E) study design, (F) outcomes, (G) results/conclusion and (H) impact of JAG.
Results
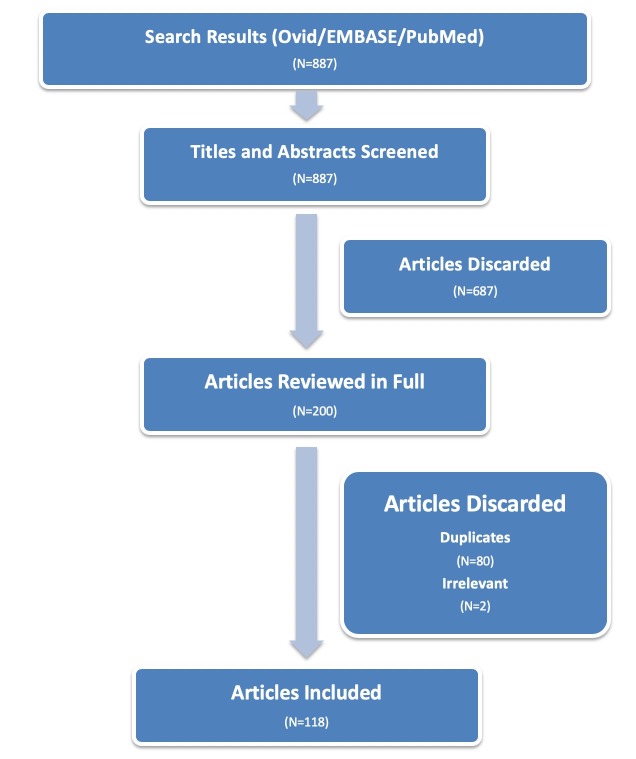
The search strategy yielded 887 results from full publications and conference proceedings. After removing 687 inappropriate results, 80 duplicate and 2 irrelevant studies, 118 publications (43 papers and 75 conference abstracts) were reviewed (figure 5). These were categorised according to the impact of JAG.
Figure 5.
Results from the literature search.
Impact on quality of care
Thirty-four studies were identified that related to quality of care (online supplementary appendix table 1),14–47 with 31 relating to impact and three on implementation.
flgastro-2018-100969supp001.docx (79.9KB, docx)
Key performance indicators
Evidence of variable practice between endoscopists has led to renewed focus on KPIs, which may be used as a surrogate marker for quality and safety in endoscopy. These may assess direct (eg, complication rates) or indirect effects on patient outcomes, for example, endoscopist’s adenoma detection rates as a surrogate for lower post colonoscopy CRC rates and mortality,48 longer colonoscopy withdrawal times correlating with adenoma detection rate (ADR)49 and higher CIR with reduced discomfort and sedation use.50 As such, audits involving KPIs allow services to safeguard patient outcomes and benchmark performance.
From the literature review, 20 studies identified were audits of JAG standards, which are aligned with BSG recommendations. Fifteen were based on colonoscopy KPIs, four on endoscopic retrograde cholangiopancreatography (ERCP)16 20 38 39 and two on gastroscopy.15 37 Quality measures of published audits mainly comprised procedural completion rates14 16 21–23 28 29 33 34 38 39 and complications15 16 20 and also included comfort scores,37 45 gastric ulcer follow-up,31 42 antibiotic concordance in percutaneous endoscopic gastrostomy (PEG),18 quality of bowel preparation22 51 and colonic biopsies for diarrhoea.41 Seven studies pertained to Bowel Cancer Screening (SAAS), reporting higher quality of care in accredited endoscopists compared with non-accredited counterparts in terms of CIR,19 27 43 52polyp detection rates (PDR),17 19 43 ADRs,19 27 43 adherence to tattoo placement17 25 and polyp retrieval rate.43
National improvements in patient outcomes
Several national studies have attributed improvements in care to JAG. In the second UK colonoscopy audit (n=20 085) performed in 2011,30 Gavin et al reported significant improvements in KPIs since the previous audit (table 3), including improvements in CIR from 76.9% in 1999 to 92.3% in 2011. The authors credited improved performance to advances in quality of training and service accreditation. Similar findings were reproduced in a retrospective comparison of colonoscopy KPIs between 2004 and 2012.32 Valori et al36 studied a composite measure coined the performance indicator of colonic intubation (PICI) which incorporated CIR with safe sedation use (midazolam <2 mg) and acceptable (mild–moderate) discomfort scores. On multivariate analysis, endoscopy performed within a JAG-accredited unit was an independent predictor of PICI (OR 1.26; 95% CI 1.16 to 1.35) and higher levels of JAG training were also associated with PICI. Britton et al35 observed that in the UK, there was a lower postcolonoscopy colorectal carcinoma incidence compared with other countries. The authors suggested that advances in quality, driven by JAG and BCSP, may have contributed towards this finding.
Table 3.
Comparisons in colonoscopy KPIs between the two national colonoscopy audits
Evidence of implementation processes
Three studies described implementation processes related to quality of care. Dewi et al introduced root-cause analyses of perforations following screening colonoscopy, whereby suboptimal management was addressed with individual feedback and training.46 Thompson et al assessed the robustness of the 90% CIR standard by factoring in the conversion of intended colonoscopy procedures to sigmoidoscopy.47 Conversion to flexible sigmoidoscopy (FS) occurred in 4.7%, with the majority lacking valid reasons, which artificially boosted CIR. Falvey et al presented data regarding implementation of nurse-assisted reporting of comfort scores,45 which was associated with significantly higher discomfort than endoscopist-reported scores. This enabled outlier performance to be identified and has since been adopted routinely as a QA measure.
Recently, two national recommendations have been released in partnership with JAG. These include the use of Buscopan in endoscopy procedures and the minimal and aspirational standards for colonoscopy practice and quality of service across the UK.44 53
Impact on quality of service
Thirty-one studies (online supplementary appendix table 2) were relevant to the impact of JAG on quality of endoscopy services.2 54–83 Twenty-two were relevant to implementation of service, with the majority being GRS based.
Impact of the GRS
An overview of JAG unit accreditation has been described in detail by Stebbing,2 who also reported improvements in quality of service. Valori et al64 expanded on the national impact of the GRS by demonstrating a reduction in patients waiting >6 weeks for endoscopy from >250 000 in 2004 to <2000 in 2008. The components of the GRS have since been validated from a patient perspective.57 Moreover, from a survey involving endoscopy staff ranging from administrative to nursing roles, >75% of staff felt that JAG recommendations had improved quality of service and care.60
Other service evaluations
Service evaluations were reported in several UK studies. Challand et al54 combined quality of care (CIR) and cost-effectiveness of a service (points per list) and found that this composite endpoint was met in 30% of endoscopists, with higher rates in trainer endoscopists and those with higher volumes. One study audited procedures that were overdue for surveillance,61 reporting high rates of procedures requested at inappropriate intervals and implemented vetting procedures to rationalise surveillance requests. Another reported implementation of a propofol-based service to meet increasing service demand.72 Two studies reported success with unit accreditation in the novel settings of community-based endoscopy76 and within the independent sector,63 both complemented by positive patient satisfaction. Three studies provided evidence to support the role of accreditation/GRS in paediatric services.70 82 83 Implementation of strategies to improve patient outcomes within BCSP have also been presented.68 71 77
Impact on services abroad
Use of the GRS is not restricted to the UK. The JAG International subcommittee responds to international interest in JAG tools/services and facilitates implementation processes in those countries. The international impact of JAG is summarised in table 4. Adoption of the GRS has been described in studies from Ireland,78 Canada,66 73 79 the Netherlands,69 84 New Zealand,85 Iraq75 and Malawi80 following collaborative efforts with JAG International, which has been successfully used to benchmark quality of service and identify areas for improvement. In a service development initiative supported by BSG and JAG International in Malawi, Nyahoda et al80 presented their experience of implementing a GI bleeding service, and Geraghty et al86 described how a training network was established in three Malawian hospitals using JAG-based training, DOPS assessments, development of a local faculty and the application of a modified GRS for service evaluation. A similar international collaboration led to the introduction of a GRS in Iraq.75 Carpentier et al provided evidence of test–retest reliability of the Canadian GRS (GRS-C), modified from the UK version, with evidence of quality improvement.79 Use of the GRS-C has been reviewed in a 2013 publication,74 which outlined its use in 39 Canadian units. Herein, 35% achieved improvements in 8/12 domains over a 2-year cycle, with 15% reporting improvements in wait times. GRS has also been referenced in international research, including the development of a novel comfort score55 and the assessment of patient derived indicators of quality of care.56
Table 4.
International use and involvement of JAG services (based on JAG International Committee minutes from July 2016) – courtesy of JAG office
| Nation | Level of interaction with JAG |
| Australia |
|
| Canada |
|
| Hong Kong |
|
| Iraq |
|
| Ireland |
|
| Malawi |
|
| Netherlands |
|
| New Zealand |
|
| Norway |
|
| Poland |
|
| Portugal |
|
| Saudi Arabia |
|
| Singapore |
|
| South Africa |
|
| Spain |
|
| USA |
|
EUS, Endoscopic Ultrasound; ERCP, endoscopic retrograde cholangiopancreatography; DOPS, direct observation of procedural skills; GIN, GI Endoscopy for Nurses; GRS, Global Rating Scale; JAG, Joint Advisory Group on Gastrointestinal Endoscopy.
Impact on quality of training
Fifty-three articles relevant to the impact of JAG on training were identified (online supplementary appendix table 3),1 6 7 12 86–130 of which 29 assessed impact and 24 described training-related implementation. Two in-depth reviews of the role of JAG in endoscopy training are provided by Dunckley1 and Anderson.1 12 The majority of studies relate to QA of training.
Trainee outcomes
Haycock et al surveyed changes in quality of training between 2002 and 2007 and reported significant improvements in standards of teaching, reduced trainee complication rates and increased trainee satisfaction, correlating with JAG’s impact.88 89 Dharmasiri et al93 reported high rates of trainee satisfaction with the e-certification system. Other surveys at regional and national levels have exposed disparities in training satisfaction by specialty87 95 103 107 and training region.101 105 In the recently published 2016 BSG trainees survey,130 85% were satisfied with the level of supervision during endoscopy training, with 12.5% reporting no access to regular training lists. Conflicting on-call commitments,130 competition for and absence of training lists are cited as contributory factors,95 104 130 despite the training domain of the GRS, which places onus on individual units to ensure sufficient training opportunities. To overcome these challenges, several studies have evaluated innovative approaches to improve trainee exposure. Walker et al115 described the successful implementation of a dedicated training e-booking system, which improved the uptake of dedicated training lists from 18% in 2007 to 61% in 2010. Similarly, by implementing generic training lists, Lamb et al117 reported increases in mean training lists from 7.8 to 13.6 lists per quarter, which was associated with improvements in trainee KPIs and DOPS counts.
Upskilling interventions
Two studies reported improvements in endoscopist KPIs after attendance on a JAG-based course. Hussain et al131 evaluated the performance of four certified endoscopists before and after attendance at a JAG-certified advanced colonoscopy course, specifying improvements in polyp retrieval and biopsy practice for chronic diarrhoea, although improvements in CIR (88%–93%) and minimal–mild discomfort scores (71%–82%) were not statistically significant. In an international study involving JAG faculty members, Kaminski et al132 identified endoscopy leaders from 40 Polish bowel cancer screening centres with suboptimal ADR and randomised them to a Train-Colonoscopy-Leaders (TCL) programme with a 2-day hands-on component or feedback only. The study analysed 24 582 colonoscopies performed by 38 leaders and 56 617 colonoscopies performed by 138 endoscopists at participating centres. The TCL arm had larger improvement in ADR than the feedback group in both early (OR 1.61; p<0.001) and late (OR 1.35; p=0.004) postintervention phases.
Non-medical endoscopists
In the UK, non-medical (nurse) endoscopists benefit from the flexibility of dedicated immersion training without competing medical and on-call commitments. The Health Education England sponsored clinical endoscopist programme has led to 31/40 non-medical endoscopists (78%) achieving gastroscopy or sigmoidoscopy certification within a 7-month timeframe.123 133 In a randomised trial from Hong Kong, non-medical endoscopists trained according to the JAG curriculum had superior ADR during screening colonoscopies compared with medical endoscopists (43.8% vs 32.7%). The authors concluded that proper training, that is, completion of well-established training programmes such as JAG, may equip nurses with the competencies for screening colonoscopy.134
Competency-based certification
Effective training is key for competent unsupervised practice. The success of JETS implementation has been well characterised.6 7 114 116 The robustness of endoscopy certification has been evidenced by precertification KPIs during training102 and postcertification KPIs of independently performing specialty trainees.7 24 Based on a 2011 analysis of JETS entries, 28% of specialist trainee procedures were logged as service lists.92 Hence, supporting trainees to achieve certification enables effective contribution to an endoscopy service.
Competency assessment tools
The role of DOPS and DOPyS as competence-assessment tools have been evaluated since their introduction in 2004.5 DOPS were first assessed in the context of BCSP, which showed validity and reliability.120 In order to standardise polypectomy assessment, DOPyS were developed,118 validated118 119 and integrated into colonoscopy certification criteria in 2011, with subsequent improvements in trainee polypectomy exposure and standards.129 This has provided a much-needed framework for polypectomy assessment. A recent survey involving 610 colonoscopists from 19 countries unearthed significant variation in polypectomy training internationally.113 Only 4 of the 19 countries, including UK, had specific guidelines for polypectomy training and competency assessment. The impact of the post-July 2016 changes to DOPS has also been published. Implementation of novel DOPS for GI bleeding121 and percutaneous endoscopic gastrostomy (PEG) have been described.135 The endoscopic non-technical skills (ENTSs) domain introduced into new DOPS/DOPyS has also been validated.126 The changes in DOPS scoring from a performance-based to supervision-based scale have improved the quality and validity of assessment tools.127 From a research perspective, DOPS and DOPyS have been integral to studies which appraise the impact of practical and simulator based training,96 99 100 106 108 110 112 136–138 thereby contributing to current understanding of optimal training methods in endoscopy. Similarly, interrogation of the JETS e-portfolio has enabled learning curve analyses for competence in gastroscopy,111 colonoscopy98 and polypectomy,109 which inform trainees, trainers and SACs regarding length of training and variation in learning curves.
Direction of training
Several publications provide insights into the future direction of training. As gastroscopy certification does not ensure competence in managing GI bleeding, certification specific for endotherapy has been proposed.128 130 In response to trainee dissatisfaction regarding exposure to training,130 139 the JAG QA-T committee has outlined strategic measures,130 including placing further increasing emphasis on GRS to improve unit-level training delivery and appraisal of measures to reduce time to competency.130 A trial roll-out of accelerated training to specialty trainees has been effective and well received.122 ‘Immersion training’, where blocks of time are dedicated to endoscopy alone, is being considered.130 These approaches may be paired with new e-learning tools to accelerate development of non-technical competencies such as lesion recognition.124 However, the single innovation likely to have greatest impact on training is the impending National Endoscopy Database (NED).125 NED has been designed to autopopulate KPIs from endoscopy reporting systems directly into future iterations of JETS and allow benchmarking of trainee learning curves nationwide.
Discussion
Summary
This literature review provides evidence that supports the impact of JAG on quality of care, service and training in UK endoscopy over the last decade. The majority demonstrate a positive impact of JAG. Of note, comparisons of performance metrics between the two national colonoscopy audits4 30 and the fall in national waiting times64 are testament to advances in quality at both endoscopist and unit levels.
The promotion of the QA framework has underpinned the success of JAG. QA in endoscopy is reliant on: (1) definition of quality standards, (2) measuring quality by comparing against quality standards, (3) methods for improving quality and (4) providing incentives for participation.1 Continuous audit and quality improvement is integral to the QA process and is supported by the centralised JAG infrastructure of JETS, GRS and SAAS. Importantly, a substantial proportion of publications (42%) in this review reported process implementation. Thus, it is encouraging that our review has uncovered the breadth of innovative approaches undertaken to accomplish and surpass minimum JAG standards.
Moreover, the international impact of JAG has also been recognised through involvement with at least 16 countries (table 4), with further involvement facilitated by international affiliations at individual institutions. Although the use of JAG tools, for example, DOPS, DOPyS and GRS, have supported research abroad, these have also benefited from international validation.
Strengths and limitations
This literature search was designed to be an objective and comprehensive summary of publications related to JAG. As the majority of publications were in abstract form, one limitation of this review is the lack of methodological rigour for selecting studies. The majority were retrospective, with only two abstracts excluded due to poor quality. However, some of these retrospective studies are well designed and have included patient numbers in excess of 100 000 (online supplementary appendix table 1). We acknowledge that there is crossover between JAG quality standards with other national guidelines. As some standards are ubiquitously recommended in guidelines, for example, CIR and ADR, it would not be appropriate to solely attribute these to the impact of JAG. Hence, the search strategy was limited to JAG-relevant terms and some studies may not have been captured. Next, search results were arbitrarily categorised into groupings of impact on care, services and training, which was intended to demonstrate outcomes on patients, units and trainees, respectively. We acknowledge there may be considerable overlap between the search results. This was also true for the subgrouping of studies according to impact and/or implementation. The relative lack of implementation-based data on patient outcomes (3/34 studies) may either indicate potential difficulties for units to implement change, which is a well-recognised barrier, or reflect publication bias, whereby unsuccessful interventions may be withheld. Sharing examples of successful (and failed) implementation measures are necessary to drive quality improvement, a strategy jointly promoted by JAG and the BSG Endoscopy Quality Improvement Project.
Future directions
In addition to future initiatives described above, upcoming agenda include a review of existing certification pathways to ensure these remain current, evidence based and supported by competency-based milestones. Plans to introduce certification in additional modalities of GI bleed haemostasis, ERCP, endoscopic ultrasound (EUS) and capsule endoscopy are also underway, supplemented with procedure-specific curricula, e-learning and JAG-approved courses. The demand for a JETS-like platform for endoscopy nurses to record competencies has prompted the development of JETS Workforce, an e-portfolio platform specific for endoscopy nurses for documenting assisting competencies that could be used to support revalidation. Pressures faced by endoscopy units,140 notwithstanding the imminent plans to introduce faecal immunochemical testing141 and lower the bowel cancer screening age to 50 years,142 are likely to instigate a review of workforce requirements, with emphasis on recruitment and upskilling of existing Bowel Scope practitioners towards BCSP colonoscopy accreditation.
NED, which is hosted by JAG, went live in April 2018. The vision of NED is to autopopulate performance metrics of individual endoscopists to centrally benchmark performance, summate unit-level data pertaining to the Clinical Quality domain of the GRS and import trainee metrics directly into JETS. This will eliminate data entry bias and allow for reliable and detailed assessment of endoscopy performance and service activity. The NED promises a data-rich platform for research on endoscopy-based metrics. This is likely to boost the research impact of JAG and will further extend JAG’s influence as an international model for facilitating endoscopy QA.
Finally, in recognition that errors in endoscopy are common and under-reported,143 JAG has announced a 5-year strategy to Improve Safety and Reduce Error in Endoscopy,144 145 which aims to improve training and the practice of error reporting, learning from error and implement system-level approaches for safety and performance improvement. This workstream will use the GRS and NED infrastructures and complement JAG’s aspirations to improve communication with endoscopy services to disseminate learning and support services in the UK, and in renewing commitments for placing patient safety and clinical quality at the forefront of endoscopy practice.
Conclusion
The UK experience shows that it is possible to achieve a transformation in quality, safety, patient experience and training with a strategic, centrally led, and modestly resourced approach.
Acknowledgments
In addition to the authors listed, we wish to acknowledge the following who have been instrumental in developing JAG’s role in UK endoscopy: Roland Valori and Debbie Johnston, previous chairs of JAG: Tony Morris, Kelvin Palmer; chairs of the QA groups: John O’Donohue, Neil Haslam; chairs of BCSA panel: John Anderson, Brian McKaig. We also wish to acknowledge the substantial contributions of Roger Leicester, staff at the JAG office, all JAG assessors and faculty of training courses.
Footnotes
Twitter: Dr Keith Siau: @drkeithsiau; Dr Siwan Thomas-Gibson: @SiwanTG; JAG Endoscopy: @JAG_Endoscopy
Contributors: KS performed the literature review and produced the initial draft. RB provided historical insight in the development of JAG. JAG section headings were cowritten by the leads of JAG subdivisions (MF: JAG International; NH: Quality Assurance of Training; JTG: Endoscopy Services Quality Assurance Group; PD: JETS lead). JRB and JS are previous chairs of JAG and confirmed the accuracy of the manuscript. ST-G holds the current chair of JAG, initially commissioned the review and is the article guarantor. All authors provided critical review and helped to shape the final version of the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: All authors have either held a position on JAG or worked on behalf of JAG
Patient consent: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Dunckley P, Elta G. Quality assurance of training. Best Pract Res Clin Gastroenterol 2011;25:397–407. 10.1016/j.bpg.2011.05.010 [DOI] [PubMed] [Google Scholar]
- 2. Stebbing JF. Quality assurance of endoscopy units. Best Pract Res Clin Gastroenterol 2011;25:361–70. 10.1016/j.bpg.2011.05.004 [DOI] [PubMed] [Google Scholar]
- 3. Valori R. Quality improvements in endoscopy in England. Techniques in Gastrointestinal Endoscopy 2012;14:63–72. 10.1016/j.tgie.2011.11.001 [DOI] [Google Scholar]
- 4. Bowles CJ, Leicester R, Romaya C, et al. A prospective study of colonoscopy practice in the UK today: are we adequately prepared for national colorectal cancer screening tomorrow? Gut 2004;53:277–83. 10.1136/gut.2003.016436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. JAG, 2004. Guidelines for the training, appraisal and assessment of trainees in gastrointestinal endoscopy and for the assessment of units for registration and re-registration. http://www.bsg.org.uk/pdf_word_docs/jag_recommendations_2004.pdf (cited 10 Aug 2017).
- 6. Mehta T, Dowler K, McKaig BC, et al. Development and roll out of the JETS e-portfolio: a web based electronic portfolio for endoscopists. Frontline Gastroenterol 2011;2:35–42. 10.1136/fg.2010.003269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Siau K, Anderson J, Beales I, et al. PTU-013 Trends in certification for gastrointestinal endoscopy and variations between trainee specialties: results from the UK JETS database. Gut 2017;66(Suppl 2):A57. [Google Scholar]
- 8. JETS, 2012. Course finder. https://www.jets.nhs.uk/FindCourseHome.aspx (cited 10 Aug 2017).
- 9. Cullinane M, Gray AJG, Hargraves CMK, et al. , 2004. Scoping our practice: the 2004 report of the confidential enquiry into patient outcome and death. http://www.ncepod.org.uk/2004report/ (cited 10 Aug 2017).
- 10. JAG, 2015. Joint Advisory Group on Gastrointestinal Endoscopy (JAG) accreditation standards for endoscopy services. https://www.thejag.org.uk/downloads/Accreditation/JAG%20accreditation%20standards%20for%20endoscopy%20services.pdf (cited 10 Aug 2017).
- 11. JAG. JAG accreditation. https://www.jagaccreditation.org (cited 10 Aug 2017).
- 12. Anderson JT. Assessments and skills improvement for endoscopists. Best Pract Res Clin Gastroenterol 2016;30:453–71. 10.1016/j.bpg.2016.05.005 [DOI] [PubMed] [Google Scholar]
- 13. Hewitson P, Glasziou P, Irwig L, et al. Screening for colorectal cancer using the faecal occult blood test, Hemoccult. Cochrane Database Syst Rev 2007:CD001216 10.1002/14651858.CD001216.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Dhayatker V, Tutton M. Colonoscopy preparation should be tailored to the patient. Colorectal Disease 2009;11:45. [Google Scholar]
- 15. Moore AR, Ormerod C, Mcmahon M, et al. 891c: Emergency readmission following elective endoscopy: audit of 29,868 day case procedures performed at four teaching hospitals in Northwest England. Gastrointestinal Endoscopy 2010;71:AB137 10.1016/j.gie.2010.03.125 [DOI] [Google Scholar]
- 16. Chatterjee S, Rees C, Dwarakanath AD, et al. Endoscopic retrograde cholangio-pancreatography practice in district general hospitals in North East England: a Northern Regional Endoscopy Group (NREG) study. J R Coll Physicians Edinb 2011;41:109–13. 10.4997/JRCPE.2011.221 [DOI] [PubMed] [Google Scholar]
- 17. Gavin D, Sidwell A, Scott M, et al. Endoscopic tattoo practice at a district general hospital. Gut 2011;60(Suppl 1):A128 10.1136/gut.2011.239301.271 [DOI] [Google Scholar]
- 18. Kurien M, Westaby D, Romaya C, et al. National survey evaluating service provision for percutaneous endoscopic gastrostomy within the UK. Scand J Gastroenterol 2011;46:1519–24. 10.3109/00365521.2011.619278 [DOI] [PubMed] [Google Scholar]
- 19. Horner R, Baranowski E, Raman S, et al. Quality assurance in colonoscopy – numbers not speciality? An audit of 10 026 colonoscopies. Colorectal Disease 2011;13:1–14. [Google Scholar]
- 20. Bodger K, Bowering K, Sarkar S, et al. All-cause mortality after first ERCP in England: clinically guided analysis of hospital episode statistics with linkage to registry of death. Gastrointest Endosc 2011;74:825–33. 10.1016/j.gie.2011.06.007 [DOI] [PubMed] [Google Scholar]
- 21. Leyden JE, Doherty GA, Hanley A, et al. Quality of colonoscopy performance among gastroenterology and surgical trainees: a need for common training standards for all trainees? Endoscopy 2011;43:935–40. 10.1055/s-0030-1256633 [DOI] [PubMed] [Google Scholar]
- 22. Butt S, Lygoe S, Defoe H, et al. Tu1481 Photographic documentation of caecal intubation: how good is it? Gastrointestinal Endoscopy 2011;73:AB423 10.1016/j.gie.2011.03.973 [DOI] [Google Scholar]
- 23. Verma AM, McGrath N, Bennett P, et al. A multi-centre audit of 16,064 colonoscopies looking at caecal intubation rates, over a 2-year period. Non-GI operators and those doing. Gut 2012;61:A150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Nayagam S, Selvapatt N, Auguste JL, et al. OC-138 Quality of colonoscopic procedures among independently practising gastroenterology trainees in a NW London cohort: are they reaching national standards? Gut 2012;61:A59.3–A60. 10.1136/gutjnl-2012-302514a.138 [DOI] [Google Scholar]
- 25. Travers H, Shirazi T, Mansfield S. PMO-223 Tattooing of suspicious colonic lesions at colonoscopy: is adherence to local protocol better if identified through the Bowel Cancer Screening Programme? Gut 2012;61:A165 10.1136/gutjnl-2012-302514b.223 [DOI] [Google Scholar]
- 26. Butt S, Defoe H, Besherdas K. PWE-200 The impact of bowel preparation on other colonoscopy quality indicators. Gut 2012;61(Suppl_2):A378. [Google Scholar]
- 27. Bhangu A, Bowley DM, Horner R, et al. Volume and accreditation, but not specialty, affect quality standards in colonoscopy. Br J Surg 2012;99:1436–44. 10.1002/bjs.8866 [DOI] [PubMed] [Google Scholar]
- 28. Kong C, Young AN, Benson K, et al. OC-048 Colonoscopy: what is the number required to maintain competency? – a retrospective audit. Gut 2013;62(Suppl 1):A21 10.1136/gutjnl-2013-304907.047 [DOI] [Google Scholar]
- 29. Verma AM, Mcgrath N, Dixon A, et al. Tu1323 gender differences - analysis of 6704 colonoscopies over 5 years reveals lower caecal intubation rates in female patients. Gastrointestinal Endoscopy 2013;77(5):AB499 10.1016/j.gie.2013.03.804 [DOI] [Google Scholar]
- 30. Gavin DR, Valori RM, Anderson JT, et al. The national colonoscopy audit: a nationwide assessment of the quality and safety of colonoscopy in the UK. Gut 2013;62:242–9. 10.1136/gutjnl-2011-301848 [DOI] [PubMed] [Google Scholar]
- 31. McGlacken-Byrne S, Lahiff C, MacMathuna P, et al. A review of gastric ulcer follow-up practices in a tertiary care gastroenterology service. Gut 2013;62:A40 10.1136/gutjnl-2013-305143.97 [DOI] [Google Scholar]
- 32. El Menabawey TM, O’Donohue J, Srirajaskanthan R. PWE-065 Colonoscopy performance in a district general hospital. has the standardisation of training standardised performance? Gut 2014;63(Suppl 1):A152 10.1136/gutjnl-2014-307263.325 [DOI] [Google Scholar]
- 33. Verma AM, Dixon AD, Chilton AP. Correlation of caecal intubation rate to volume: colonoscopists should undertake at least 120 procedures per year. Frontline Gastroenterol 2014;5:156–60. 10.1136/flgastro-2013-100395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Lee HY, Gashau W, Willert R. PWE-041 Management of large colonic polyps in a Bowel Cancer Screening Programme. Gut 2014;63(Suppl 1):A140 10.1136/gutjnl-2014-307263.301 [DOI] [Google Scholar]
- 35. Britton J, Chan L, Allan K, et al. Post-colonoscopy colorectal cancer in the United Kingdom: a double-center experience. American Journal of Gastroenterology 2014;109:S608. [Google Scholar]
- 36. Valori RM, Damery S, Gavin DR, et al. A new composite measure of colonoscopy: the Performance Indicator of Colonic Intubation (PICI). Endoscopy 2018;50:40–51. 10.1055/s-0043-115897 [DOI] [PubMed] [Google Scholar]
- 37. Rafferty H, Hutchinson J, Ansari S, et al. PWE-040 Comfort scoring for endoscopic procedures: who is right – the endoscopist, the nurse or the patient? Gut 2014;63(Suppl 1):A139 10.1136/gutjnl-2014-307263.300 [DOI] [Google Scholar]
- 38. Cretu I, Kelleher B, Stewart S, et al. Audit of ERCP key performance indicators in a high volume interventional/biliary endoscopy centre. Irish Journal of Medical Science 2015;184(Suppl 1):S99. [Google Scholar]
- 39. Sheppard D, Craddock S, Warner B, et al. PTH-007 ERCP cannulation success benchmarking: implications for certification and validation. Gut 2014;63:A210 10.1136/gutjnl-2014-307263.453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Davies J, Mills S. Assessment of accuracy in predicting site of colorectal cancer at endoscopy. International Journal of Surgery 2013;11:621 10.1016/j.ijsu.2013.06.184 [DOI] [Google Scholar]
- 41. Easaw J, Bennett A, Leslie F, et al. Routine colonosopic biopsies-should practice change? United European Gastroenterology Journal 2015;3(Suppl 1):A420. [Google Scholar]
- 42. Aslam NS, Ingram RJM, Mandal A. PTH-035 Does repeat gastroscopy for gastric ulceration have an impact on cancer detection and mortality across Lincolnshire? Gut 2016;65(Suppl 1):A235 10.1136/gutjnl-2016-312388.440 [DOI] [Google Scholar]
- 43. Ahmed S, Naumann DN, Karandikar S. Differences in screening vs non-screening colonoscopy: scope for improvement? Colorectal Dis 2016;18:903–9. 10.1111/codi.13291 [DOI] [PubMed] [Google Scholar]
- 44. Rees CJ, Thomas Gibson S, Rutter MD, et al. UK key performance indicators and quality assurance standards for colonoscopy. Gut 2016;65:1923–9. 10.1136/gutjnl-2016-312044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Falvey J, King C, Dixit A, et al. Comfort during colonoscopy: do nurses tell us more? Gut 2009;58(Suppl 1):A1.19307448 [Google Scholar]
- 46. Dewi F, Heard H, Davies M, et al. PWE-316 Incidence and management of iatrogenic perforations in the welsh bowel screening programme. Gut 2015;64(Suppl 1):A349 10.1136/gutjnl-2015-309861.762 [DOI] [Google Scholar]
- 47. Thompson C, Ismail T, Radley S, et al. Conversion of colonoscopy to flexible sigmoidoscopy: an unintended consequence of quality measurement in endoscopy. Frontline Gastroenterol 2016;7:202–6. 10.1136/flgastro-2015-100626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Corley DA, Jensen CD, Marks AR, et al. Adenoma detection rate and risk of colorectal cancer and death. N Engl J Med 2014;370:1298–306. 10.1056/NEJMoa1309086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Vavricka SR, Sulz MC, Degen L, et al. Monitoring colonoscopy withdrawal time significantly improves the adenoma detection rate and the performance of endoscopists. Endoscopy 2016;48:256–62. 10.1055/s-0035-1569674 [DOI] [PubMed] [Google Scholar]
- 50. Ekkelenkamp VE, Dowler K, Valori RM, et al. Patient comfort and quality in colonoscopy. World J Gastroenterol 2013;19:2355–61. 10.3748/wjg.v19.i15.2355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Butt SK, Defoe H, Besherdas K. The impact of bowel preparation on other colonoscopy quality indicators. Gut 2012;61:A378. [Google Scholar]
- 52. Verma AM, McGrath N, Bennett P, et al. PMO-187 A multi-centre audit of 16064 colonoscopies looking at caecal intubation rates, over a 2-year period. Gut 2012;61:A150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Lee T, Anderson J, Thomas-Gibson S, et al. Use of intravenous hyoscine butylbromide (Buscopan) during gastrointestinal endoscopy. Frontline Gastroenterol 2018;9 10.1136/flgastro-2017-100877 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Challand CP, Bullen N, Wu E, et al. How do you measure performance as a colonoscopist? Colorectal Dis 2011;13:939–43. 10.1111/j.1463-1318.2010.02344.x [DOI] [PubMed] [Google Scholar]
- 55. Rostom A, Ross ED, Dubé C, et al. Development and validation of a nurse-assessed patient comfort score for colonoscopy. Gastrointest Endosc 2013;77:255–61. 10.1016/j.gie.2012.10.003 [DOI] [PubMed] [Google Scholar]
- 56. Sewitch MJ, Dubé C, Brien S, et al. Patient-identified quality indicators for colonoscopy services. Can J Gastroenterol 2013;27:25–32. 10.1155/2013/574956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Williams T, Ross A, Stirling C, et al. Validation of the global rating scale for endoscopy. Scott Med J 2013;58:20–1. 10.1177/0036933012474587 [DOI] [PubMed] [Google Scholar]
- 58. Boereboom C, Lund J, Watson N. A descriptive longitudinal assessment of the endoscopy requirements of 183 consecutive consultant colorectal surgeon posts. Colorectal Disease 2014;16:202–3. [Google Scholar]
- 59. O’Brien C, Walsh K. An audit of GI endoscopic follow up in Sligo regional hospital. Irish Journal of Medical Science 2014;183(Suppl 1):S137. [Google Scholar]
- 60. Mahmood T, Aung KYI. A study of gap analysis between perception of the Joint Advisory Group (JAG) and staff members of endoscopy unit regarding quality of care in UK. Journal of Gastrointestinal & Digestive System 2015;5:319. [Google Scholar]
- 61. Kilmartin DM, Khan T, Walsh K. An audit of GI endoscopic surveillance in sligo regional hospital. Irish Journal of Medical Science 2015;184(Suppl 1):S323. [Google Scholar]
- 62. Valliani T, Dowler K, Dunckley P. OC-021 Flexible sigmoidoscopy completion rates. Time to change certification criteria? Gut 2015;59(Suppl 1):A9. [Google Scholar]
- 63. Caronia S, Murkin A, Ludford H. A year in the life of an Independent Sector Treatment Centre (ISTC): the endoscopy service at St Mary’s NHS treatment centre. Gut 2009;58(Suppl 1):A1.19307448 [Google Scholar]
- 64. Valori RM, Barton R, Johnston DK. The English national endoscopy quality assurance programme: quality of care improves as waits decline. Gastrointestinal Endoscopy 2009;69:AB221 10.1016/j.gie.2009.03.523 [DOI] [Google Scholar]
- 65. Shah R, Chan D, Dewar D. Audit of clinical indication for recall endoscopy in 974 patients. Gut 2009;58(S1). [Google Scholar]
- 66. de Jonge V, Sint Nicolaas J, Lalor EA, et al. A prospective audit of patient experiences in colonoscopy using the Global Rating Scale: a cohort of 1,187 patients. Can J Gastroenterol 2010;24:607–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Sint Nicolaas J, de Jonge V, ter Borg F, et al. Evaluation of a quality assurance program for endoscopy services in the Netherlands. Gastroenterology 2011;140:S-558–S-559. 10.1016/S0016-5085(11)62312-3 [DOI] [Google Scholar]
- 68. Coleman L, Fretwell I. * NHS bowel cancer screening programme in england. Gut 2011;60(Suppl 1):A250 10.1136/gut.2011.239301.531 [DOI] [Google Scholar]
- 69. Sint Nicolaas J, de Jonge V, Korfage IJ, et al. Benchmarking patient experiences in colonoscopy using the Global Rating Scale. Endoscopy 2012;44:462–72. 10.1055/s-0031-1291663 [DOI] [PubMed] [Google Scholar]
- 70. Muhammed R, Thomson M, McGrogan P, et al. The provision of paediatric gastrointestinal endoscopy services in the United Kingdom. Frontline Gastroenterol 2012;3:263–6. 10.1136/flgastro-2012-100209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Kyte R. PMO-001 The role of the specialist screening practitioner within the Bowel Screening Wales programme. Gut 2012;61(Suppl 2):A73 10.1136/gutjnl-2012-302514b.1 [DOI] [Google Scholar]
- 72. Rogers D, Robinson R, Shah S. PMO-211 Propofol sedation for colonoscopy: a single centre’s experience. Gut 2012;61(Suppl 2):A160 10.1136/gutjnl-2012-302514b.211 [DOI] [Google Scholar]
- 73. MacIntosh D, Dubé C, Hollingworth R, et al. The endoscopy Global Rating Scale-Canada: development and implementation of a quality improvement tool. Can J Gastroenterol 2013;27:74–82. 10.1155/2013/165804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Dubé C. Use of the endoscopy global rating scale by endoscopy services in Canada. Canadian Journal of Gastroenterology 2013;27:684–5. 10.1155/2013/485040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Hawkes N, Al-Rubaiy L, Hawkes B, et al. PTH-046 Benchmarking endoscopy services In Iraq – results of a national survey. Gut 2014;63:A229 10.1136/gutjnl-2014-307263.492 [DOI] [Google Scholar]
- 76. Hitchen A, Kompo B, Phillips P, et al. OC-040 community-based endoscopy in a car park. fantasy or reality? Gut 2014;63(Suppl 1):A19–A20. 10.1136/gutjnl-2014-307263.40 [DOI] [Google Scholar]
- 77. Hawkes N, Heard H, Dolwani S. PWE-050 development of a performance management framework For Bsw Colonoscopists. Gut 2014;63(Suppl 1):A144–A145. 10.1136/gutjnl-2014-307263.310 [DOI] [Google Scholar]
- 78. El Ouali S, Sharara N, Carpentier SM, et al. Mo1079 patient perspectives on their colonoscopy experience and impact on the global rating scale - the adult McGill Experience. Gastroenterology 2015;148:S-599 10.1016/S0016-5085(15)32024-2 [DOI] [Google Scholar]
- 79. Carpentier S, Sharara N, Barkun AN, et al. Pilot validation study: canadian global rating scale for colonoscopy services. Can J Gastroenterol Hepatol 2016;2016:1–7. 10.1155/2016/6982739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Nyahoda R, Uledi S, Kibrete W, et al. PTH-134 Setting Up An Endoscopy Unit in Northern Malawi. Gut 2016;65(Suppl 1):A286 10.1136/gutjnl-2016-312388.537 [DOI] [Google Scholar]
- 81. Rossos P, Xenodemetropoulos T, Lane K, et al. A80 The snare project: closing the loop on synoptic endoscopic reporting and skills assessment - program and abstracts from the canadian digestive diseases week 2016. Canadian Journal of Gastroenterology and Hepatology 2016;2016:51. [Google Scholar]
- 82. Narula P, Broughton R, Bremner R, et al. Development of a paediatric endoscopy global rating scale: Results of a national pilot. Journal of Pediatric Gastroenterology and Nutrition 2017;64:25–6. [DOI] [PubMed] [Google Scholar]
- 83. Jwy W, Thomson M, Campbell D, et al. G189(P) Development of an annual endoscopy audit plan using measures in the P-GRS(paediatric global rating scale for endoscopy) in a tertiary paediatric endoscopy service to facilitate quality improvement. Archives of Disease in Childhood 2017;102(Suppl 1):A76. [Google Scholar]
- 84. Sint Nicolaas J, Jonge de V, de Man RA, et al. The global rating scale in clinical practice: a comprehensive quality assurance programme for endoscopy departments. Digestive and Liver Disease 2012;44:919–924. [DOI] [PubMed] [Google Scholar]
- 85. Livesey A, Esplin J, 2015. Report prepared for the Ministry of Health: Governance of endoscopy quality and related initiatives - report for stakeholder feedback. https://www.surgeons.org/media/21905792/2015-06-05_rpt_governance_of_endoscopy_quality_and_related_initiatives_report_for_sta.pdf (cited 21 Aug 2017).
- 86. Geraghty J, Kankwatira A, Feeney M, et al. OC-028 developing sustainable GI endoscopy training in Malawi. Gut 2012;61(Suppl 2):A12 10.1136/gutjnl-2012-302514a.28 [DOI] [Google Scholar]
- 87. Cornish J, Horwood J, Maw A. Attaining JAG endoscopy competency during higher surgical training - The trainees experience. Colorectal Disease 2010;12:42. [Google Scholar]
- 88. Haycock AV, Flanagan P, Ignjatovic A, et al. Endoscopy training in 2008: Results from the TiG/BSG national training survey. Gut 2009;58(S1). [Google Scholar]
- 89. Haycock AV, Patel JH, Tekkis PP, et al. Evaluating changes in gastrointestinal endoscopy training over 5 years: closing the audit loop. Eur J Gastroenterol Hepatol 2010;22:368–73. 10.1097/MEG.0b013e32832adfac [DOI] [PubMed] [Google Scholar]
- 90. Kelly NM, Moorehead J, Tham T. Is the ’driving test' a robust quality indicator of colonoscopy performance? World J Gastrointest Endosc 2010;2:112–20. 10.4253/wjge.v2.i4.112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Samji S, Dowler K, Valori R, et al. Analysis of trainer feedback from the JETS E-portfolio. Gut 2011;60(Suppl 1):A123–A124. 10.1136/gut.2011.239301.261 [DOI] [Google Scholar]
- 92. Griffiths LP, Dowler K, Valori R, et al. UK endoscopy trainees provide a significant quantity of service delivery. Gut 2011;60:A120 10.1136/gut.2011.239301.254 [DOI] [Google Scholar]
- 93. Dharmasiri S, Wells C, Flexer L, et al. PTU-266 Trainee satisfaction with JAG e-certification. Gut 2012;61:A295 10.1136/gutjnl-2012-302514c.266 [DOI] [Google Scholar]
- 94. Macdougall L, Corbett S, Welfare M, et al. PTU-007 Evaluating endoscopy trainers; how reliable are peer evaluators? Gut 2013;62(Suppl 1):A44 10.1136/gutjnl-2013-304907.100 [DOI] [Google Scholar]
- 95. Hammond JS, Watson NFS, Lund JN, et al. Surgical endoscopy training: the Joint Advisory Group on gastrointestinal endoscopy national review. Frontline Gastroenterol 2013;4:20–4. 10.1136/flgastro-2012-100242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Ansell J, Hurley J, Horwood J, et al. The WIMAT colonoscopy suitcase is a valid simulator for polypectomy training. Surgical Endoscopy and Other Interventional Techniques 2013;27:S340. [Google Scholar]
- 97. Hawkes N, McDonald J. PTU-011 Identifying The Learning Needs Of Bsw Colonoscopists Using An Active Learning Diary During Screening Lists. Gut 2014;63(Suppl 1):A42 10.1136/gutjnl-2014-307263.85 [DOI] [Google Scholar]
- 98. Ward ST, Mohammed MA, Walt R, et al. An analysis of the learning curve to achieve competency at colonoscopy using the JETS database. Gut 2014;63:1746–54. 10.1136/gutjnl-2013-305973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Ansell J, Hurley JJ, Horwood J, et al. Can endoscopists accurately self-assess performance during simulated colonoscopic polypectomy? A prospective, cross-sectional study. Am J Surg 2014;207:32–8. 10.1016/j.amjsurg.2013.05.019 [DOI] [PubMed] [Google Scholar]
- 100. Ansell J, Hurley JJ, Horwood J, et al. The Welsh Institute for Minimal Access Therapy colonoscopy suitcase has construct and concurrent validity for colonoscopic polypectomy skills training: a prospective, cross-sectional study. Gastrointest Endosc 2014;79:490–7. 10.1016/j.gie.2013.08.003 [DOI] [PubMed] [Google Scholar]
- 101. Beejooa G, Prasad N, Shields P. PTU-005 Factors influencing the quality of colonoscopy training in the North West Deanery. Gut 2014;63(Suppl 1):A39 10.1136/gutjnl-2014-307263.79 [DOI] [Google Scholar]
- 102. Ewing I, Lim J, Bryce K, et al. PTU-008 Dedicated colonoscopy training lists improve trainee completion rates to match a consultant benchmark. Gut 2014;63:A40–A41. 10.1136/gutjnl-2014-307263.82 [DOI] [Google Scholar]
- 103. Jones RP, Stylianides NA, Robertson AG, et al. National survey on endoscopy training in the UK. The Annals of The Royal College of Surgeons of England 2015;97:386–9. 10.1308/003588415X14181254790400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Chadwick G, Budihal S. PTU-050 Is current UK colonoscopy training fit for purpose? – results of the 2014 BSG training survey. Gut 2015;64(Suppl 1):A81 10.1136/gutjnl-2015-309861.165 [DOI] [Google Scholar]
- 105. Bhatt S, Ambrose T, Dunckley P, et al. PWE-440 Trainee endoscopic procedures by deanery and grade in the United Kingdom: September 2013 – August 2014. have we improved? Gut 2015;64:A403 10.1136/gutjnl-2015-309861.886 [DOI] [Google Scholar]
- 106. Axe K, Hawkes E, Turner J, et al. PWE-432 Learning curve for upper GI endoscopy – qualitative assessment of developmental phases of novice trainees. Gut 2015;64(Suppl 1):A399–A400. 10.1136/gutjnl-2015-309861.878 [DOI] [Google Scholar]
- 107. Everett S, Welman T, Younis J, et al. A survey of the delivery of endoscopy training amongst higher surgical trainees. Int J Surg 2015;23:S101–S102. 10.1016/j.ijsu.2015.07.473 [DOI] [Google Scholar]
- 108. Amadio JM, Walsh CM, Scaffidi MA, et al. Su1553 Can novice endoscopists accurately self-assess performance during their initial clinical colonoscopies? A prospective, cross-sectional study. Gastrointest Endosc 2015;81:AB325 10.1016/j.gie.2015.03.1450 [DOI] [Google Scholar]
- 109. Rajendran A, Thomas-Gibson S, Bassett P, et al. PTH-116 Time to achieve competency in lower gastrointestinal polypectomy in the United Kingdom, a retrospective analysis. Gut 2016;65(Suppl 1):A276–A277. 10.1136/gutjnl-2016-312388.519 [DOI] [Google Scholar]
- 110. van Doorn SC, Bastiaansen BAJ, Thomas-Gibson S, et al. Polypectomy skills of gastroenterology fellows: can we improve them? Endosc Int Open 2016;04:E182–E89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Ward ST, Hancox A, Mohammed MA, et al. The learning curve to achieve satisfactory completion rates in upper GI endoscopy: an analysis of a national training database. Gut 2017;66:1022–33. 10.1136/gutjnl-2015-310443 [DOI] [PubMed] [Google Scholar]
- 112. Grover SC, Scaffidi MA, Khan R, et al. Progressive learning in endoscopy simulation training improves clinical performance: a blinded randomized trial. Gastrointest Endosc 2017;86:881–9. 10.1016/j.gie.2017.03.1529 [DOI] [PubMed] [Google Scholar]
- 113. Patel K, Rajendran A, Faiz O, et al. An international survey of polypectomy training and assessment. Endosc Int Open 2017;5:E190–E197. 10.1055/s-0042-119949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Sinha A, Dowler K, Valori R, et al. National uptake of JETS E-portfolio. Gut 2011;60(Suppl 1):A124 10.1136/gut.2011.239301.262 [DOI] [Google Scholar]
- 115. Walker NAF, McNair A, Beale A, et al. E-booking system for endoscopy training lists enhances their utilisation. Gut 2011;60(Suppl 1):A51 10.1136/gut.2011.239301.100 [DOI] [Google Scholar]
- 116. Mehta T, Dowler K, McKaig B, et al. PTH-018 Results on the national uptake of the JETS e-Portfolio. Gut 2010;59(Suppl 1):A129–A130. 10.1136/gut.2009.209023e [DOI] [Google Scholar]
- 117. Lamb CA, Singh JN, Eltringham M, et al. Generic medical and surgical endoscopy training lists can improve the number of opportunities for training in colonoscopy. Gut 2011;60(Suppl 1):A121 10.1136/gut.2011.239301.256 [DOI] [Google Scholar]
- 118. Gupta S, Anderson J, Bhandari P, et al. Development and validation of a novel method for assessing competency in polypectomy: direct observation of polypectomy skills. Gastrointest Endosc 2011;73:1232–9. 10.1016/j.gie.2011.01.069 [DOI] [PubMed] [Google Scholar]
- 119. Gupta S, Bassett P, Man R, et al. Validation of a novel method for assessing competency in polypectomy. Gastrointest Endosc 2012;75:568–75. 10.1016/j.gie.2011.09.028 [DOI] [PubMed] [Google Scholar]
- 120. Barton JR, Corbett S, van der Vleuten CP, et al. The validity and reliability of a Direct Observation of Procedural Skills assessment tool: assessing colonoscopic skills of senior endoscopists. Gastrointest Endosc 2012;75:591–7. 10.1016/j.gie.2011.09.053 [DOI] [PubMed] [Google Scholar]
- 121. China L, Johnson GJ. Su1594 A novel training and assessment tool for the endoscopic management of Upper GI Bleeding (UGIB). Gastrointest Endosc 2014;79:AB333 10.1016/j.gie.2014.02.338 [DOI] [Google Scholar]
- 122. Hawkes N, Turner J, Hurley J, et al. Accelerated training in upper GI endoscopy-an analysis of SPRINT programme outcomes. United European Gastroenterology Journal 2015;3(Suppl 1):A368–A369. [Google Scholar]
- 123. Watson H, Hibberts F. PWE-427 The development of a national nurse / non-medical endoscopist course. Gut 2015;64:A397 10.1136/gutjnl-2015-309861.873 [DOI] [Google Scholar]
- 124. Axe K, Hawkes E, Turner J, et al. PWE-433 A qualitative assessment of cognitive framework development in novice endoscopists: implications for programmed lesion recognition training. Gut 2015;64(Suppl 1):A400 10.1136/gutjnl-2015-309861.879 [DOI] [Google Scholar]
- 125. Lee TJW, Macdougall L, Broughton R, et al. PTH-044 The National Endoscopy Database (NED) Project. Gut 2016;65(Suppl 1):A240. [Google Scholar]
- 126. Siau K, Dunckley P, Anderson J, et al. PTU-009 Competency of endoscopic non-technical skills (ENTS) during endoscopy training. Gut 2017;66(Suppl 2):A54. [Google Scholar]
- 127. Siau K, Dunckley P, Valori R, et al. Changes in scoring of Direct Observation of Procedural Skills (DOPS) forms and the impact on competence assessment. Endoscopy 2018;50:770–8. 10.1055/a-0576-6667 [DOI] [PubMed] [Google Scholar]
- 128. Siau K, Dunckley P, Anderson J, et al. PTU-010 Exposure to endotherapy for upper gastrointestinal bleeding at the point of gastroscopy certification – is it sufficient? Gut 2017;66(Suppl 2):A55. [Google Scholar]
- 129. Patel K, Faiz O, Rutter M, et al. The impact of the introduction of formalised polypectomy assessment on training in the UK. Frontline Gastroenterol 2017;8:104–9. 10.1136/flgastro-2016-100718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Biswas S, Alrubaiy L, China L, et al. Trends in UK endoscopy training in the BSG trainees' national survey and strategic planning for the future. Frontline Gastroenterol 2018;9 10.1136/flgastro-2017-100848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. Hussain Z, Reynolds K, Smales S, et al. Colonoscopy quality and safety indicators: 356. Colorectal Dis 2011;13:57. [Google Scholar]
- 132. Kaminski MF, Anderson J, Valori R, et al. Leadership training to improve adenoma detection rate in screening colonoscopy: a randomised trial. Gut 2016;65:616–24. 10.1136/gutjnl-2014-307503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133. Office for Public Management, 2017. Accelerated non-medical endoscopist training programme: report to health education England. http://www.opm.co.uk/wp-content/uploads/2017/06/OPM_NME-Year-1-Evaluation-Report-Final.pdf (cited 18 Oct 2017).
- 134. Hui AJ, Lau JY, Lam PP, Ppy L, et al. Comparison of colonoscopic performance between medical and nurse endoscopists: a non-inferiority randomised controlled study in Asia. Gut 2015;64:1058–62. 10.1136/gutjnl-2013-306293 [DOI] [PubMed] [Google Scholar]
- 135. Bonnington S, Wells CW. Su1566 Development of a DOPS assessment tool for Percutaneous Endoscopic Gastrostomy (PEG) Insertion. Gastrointest Endosc 2015;81:AB332 10.1016/j.gie.2015.03.1463 [DOI] [Google Scholar]
- 136. Thomas-Gibson S, Bassett P, Suzuki N, et al. Intensive training over 5 days improves colonoscopy skills long-term. Endoscopy 2007;39:818–24. 10.1055/s-2007-966763 [DOI] [PubMed] [Google Scholar]
- 137. Ansell J, Hurley J, Horwood J, et al. Colonoscopists can accurately self-assess their performance when using the wimat colonoscopy suitcase polypectomy trainer. Surgical Endoscopy and Other Interventional Techniques 2013;27:S340. [Google Scholar]
- 138. Grover SC, Garg A, Scaffidi MA, et al. Impact of a simulation training curriculum on technical and nontechnical skills in colonoscopy: a randomized trial. Gastrointest Endosc 2015;82:1072–9. 10.1016/j.gie.2015.04.008 [DOI] [PubMed] [Google Scholar]
- 139. Greenaway D, 2013. Shape of training. http://www.shapeoftraining.co.uk/static/documents/content/Shape_of_training_FINAL_Report.pdf_53977887.pdf (cited 18 Oct 2017).
- 140. Shenbagaraj L, Thomas-Gibson S, Stebbing J, et al. Endoscopy in 2017: a national survey of practice in the UK. Frontline Gastroenterol 2018:flgastro-2018-100970 10.1136/flgastro-2018-100970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141. Murphy J, Halloran S, Gray A. Cost-effectiveness of the faecal immunochemical test at a range of positivity thresholds compared with the guaiac faecal occult blood test in the NHS Bowel Cancer Screening Programme in England. BMJ Open 2017;7:e017186 10.1136/bmjopen-2017-017186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142. Public Health England, 2018. Bowel screening to start at 50. https://www.gov.uk/government/news/bowel-screening-to-start-at-50 (cited 17 Sep 2018).
- 143. Matharoo M, Haycock A, Sevdalis N, et al. A prospective study of patient safety incidents in gastrointestinal endoscopy. Endosc Int Open 2017;5:E83–E89. 10.1055/s-0042-117219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144. JAG, 2018. Joint Advisory Group for GI Endoscopy (JAG) Improving Safety and Reducing Error in Endoscopy (ISREE) Implementation strategy https://www.thejag.org.uk/Downloads/General/180801-Improving%20Safety%20and%20Reducing%20Error%20in%20Endoscopy%20(ISREE)%20Implementation%20strategy%20v1.0.pdf
- 145. Thomas-Gibson S, Matharoo M, Siau K, et al. PTH-044 Improving safety and reducing error in endoscopy (ISREE) – a JAG initiative. Gut 2018;67(Suppl 1):A34. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
flgastro-2018-100969supp001.docx (79.9KB, docx)