Abstract
We present an uncommon case of a patient presenting at the emergency department for severe vomiting, persisting for at least 12 hours, without nausea or abdominal pain. She initially referred vomiting food eaten several hours earlier and eventually a single episode of haematemesis with emission of a small amount of red blood and clots. She also reported the occurrence of acute dysphagia for solid food. The patient underwent oesophagogastroduodenoscopy (OGD), which showed that the lumen was almost completely narrowed by a submucosal bluish bulging from midoesophagus (19 cm from the incisors) to the cardia (located at 35 cm from the incisors). She therefore underwent chest CT showing a 15 cm long intramural oesophageal haematoma. Although the combination of vomiting and haematemesis is usually associated with Mallory-Weiss syndrome, in which a prompt OGD has a key role in the patient management, when these symptoms are associated with acute dysphagia, a possible intramural haematoma might be suspected. In this case, chest CT should take precedence, because it allows a quick and complete diagnostic appraisal. However, in this setting, although OGD can directly show typical findings (bluish swelling mucosa with or without a superficial tears), it might increase the risk of oesophageal haematoma rupture and intraluminal bleeding.
Keywords: gastrointestinal haemorrhage, dysphagia, oesophageal disease
Question
Introduction
A 70-year-old woman presented at the emergency department for severe vomiting persisting for at least 12 hours without nausea or abdominal pain. She initially referred vomiting food eaten several hours earlier and eventually a single episode of haematemesis with emission of a small amount of red blood and clots. She also reported the occurrence of acute dysphagia for solid food.
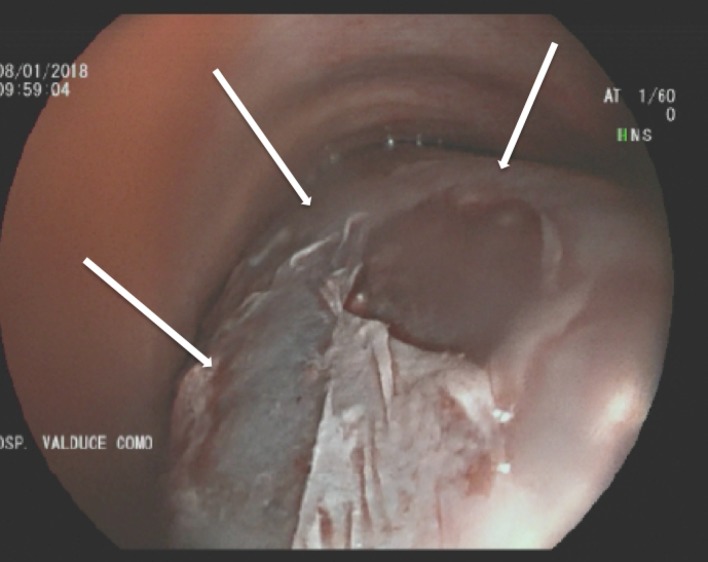
Her medical history was unremarkable; she was taking atenolol for mild hypertension and no other drugs. At admission, she was haemodinamically stable, and physical examination was normal. At digital rectal examination, there was no evidence of melena. Lab tests documented a mild anaemia (Hb 101 g/L) and a slight increase in the white cell count (11870/mm3). Platelets count and routine coagulation assay, including international normalised ratio and partial thromboplastin time, were normal. The patient underwent oesophagogastroduodenoscopy (OGD); some traces of fresh blood and small blood clots were seen in the proximal oesophagus; the lumen was almost completely narrowed by a submucosal bluish bulging (figure 1) from midoesophagus (19 cm from the incisors) to the cardia (located at 35 cm from the incisors); stomach and duodenum were normal.
Figure 1.
Oesophagogastroduodenoscopy performed at time of admission: the esophageal lumen is almost completely narrowed by a submucosal bluish bulging (white arrows).
Question
What is the most likely endoscopic diagnosis?
Answer
The patient underwent chest CT showing a 15 cm long intramural haematoma (IOH) (figure 2). The patient kept fasting and treated conservatively with parenteral nutrition and intravenous fluids, and the dysphagia quickly improved. Seven days later, the patient underwent first CT, followed by OGD. The OGD showed a shallow superficial ulcer, which covered half of the oesophageal circumference, from 19 cm to 33 cm from the incisors (figure 3); within this area, a deep ulcer (figure 4) was detected. The CT confirmed the OGD findings. A complete re-epithelialisation of the entire area covered by the haematoma was seen at OGD performed 3 weeks later (figure 5).
Figure 2.
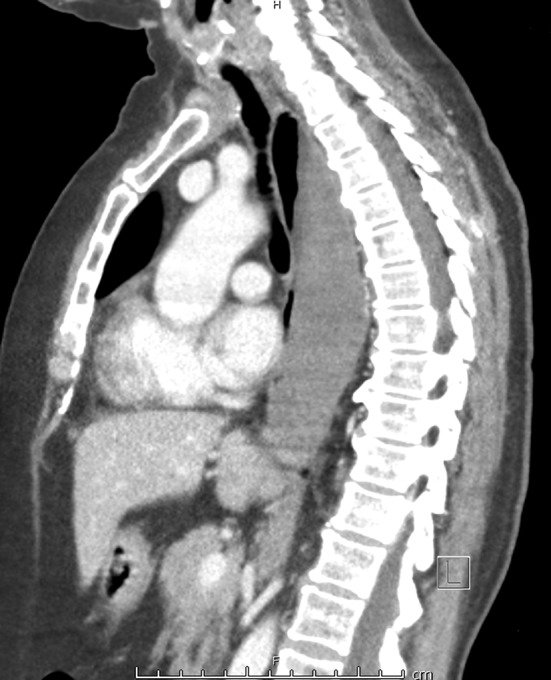
Chest CT performed at time of admission (sagittal view) showing the esophageal hematoma (radiodensity 65 Hunsfield units) narrowing the oesophageal lumen.
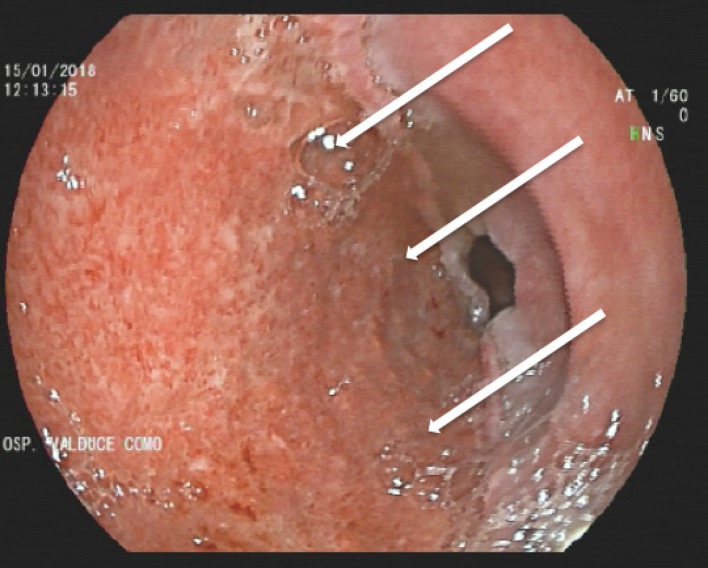
Figure 3.
Oesophagogastroduodenoscopy performed 7 days after admission showing half of the oesophageal circumference covered by a shallow superficial ulcer with granulation tissue (white arrows demarcate the distal border of the ulcer).
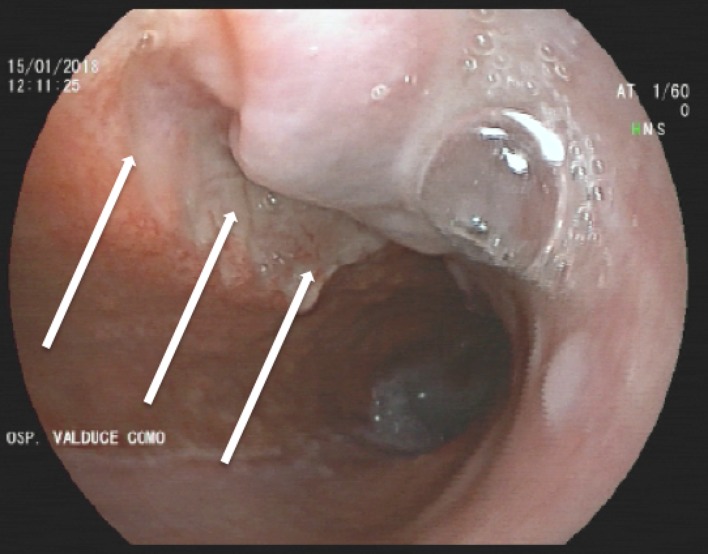
Figure 4.
Oesophagogastroduodenoscopy performed 7 days after admission: within the ulcerated area depicted in figure 3, a deep ulcer (white arrows), covered by fibrin and without bleeding stigmata, was detected.
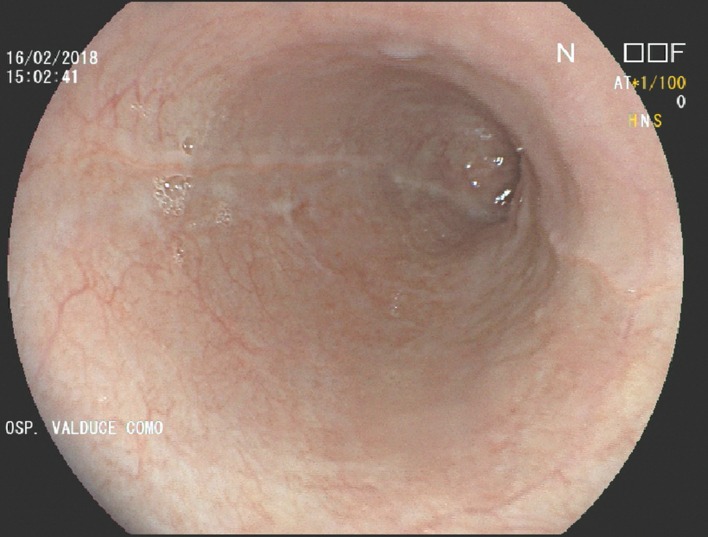
Figure 5.
Oesophagogastroduodenoscopy performed 4 weeks after admission showing complete re-epithelialisation of the entire area covered by the haematoma.
In patients with persisting retching referring the presence of red blood and/or clots in the vomit, Mallory-Weiss syndrome is the most common diagnosis.1 Nevertheless, when persisting vomiting is associated with acute severe dysphagia, the occurrence of an IOH might be suspected mainly in elderly patients, in those receiving anticoagulant or antiplatelet therapy or after foreign body ingestion, nasogastric tube insertion or transoesophageal echocardiogram examination.2–4 When an IOH is suspected, CT should be the first diagnostic test, as the OGD might increase the risk of IOH rupture and potentially life-threatening intraluminal bleeding. We prudentially suggest performing first CT even in the follow-up to confirm the oesophageal patency and the absence of local complications (eg, tamponed perforation), before undertaking OGD to evaluate the mucosal healing.
Footnotes
Contributors: GM, GI, AM, FR and GS performed diagnostic procedures. GM and EE drafted the paper; all authors revised and approved the final manuscript.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Michel L, Serrano A, Malt RA, et al. Evolution of diagnostic and therapeutic patterns over two decades. Ann Surg 1980;192:716–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Mathew G, Bhimji SS. Esophageal Hematoma. StatPearls. Treasure Island (FL): StatPearls Publishing, 2017. [Google Scholar]
- 3. Disney BR, Preece SA, Ishaq S. Intramural esophageal hematoma: an unusual cause of acute chest pain. Endoscopy 2014;46:E607–8. 10.1055/s-0034-1390712 [DOI] [PubMed] [Google Scholar]
- 4. Concannon ES, Khan F, O’Hanrahan T. Spontaneous intramural oesophageal haematoma: an unusual cause of chest pain. BMJ Case Rep 2011;2011:bcr0920114837 10.1136/bcr.09.2011.4837 [DOI] [PMC free article] [PubMed] [Google Scholar]