Abstract
The present study aimed to investigate the expression of methionine sulfoxide reductases B3 (MSRB3) in gastric cancer (GC) and its clinical significance. A total of 90 specimens from patients with GC were collected to evaluate MSRB3 protein expression by immunohistochemical staining. The associations between MSRB3 protein expression, clinicopathological characteristics and prognosis of patients with GC were subsequently investigated. The results demonstrated that MSRB3 protein expression in GC tissues samples was significantly higher compared with that in paired adjacent normal tissues (P=0.017). Among the 90 GC cases, 64 (71.1%) exhibited higher MSRB3 expression. In addition, the diagnostic value of MSRB3 for patients with GC was estimated with a sensitivity of 71.1% and a specificity of 46.7%. However, MSRB3 expression was not associated with clinicopathological characteristics of patients with GC. Kaplan-Meier analysis indicated that patients with high MSRB3 expression had significantly shorter overall survival (OS) times compared with those with low expression (P=0.040). Univariate Cox regression analysis indicated that maximum tumor diameter, depth of invasion, lymph node metastasis, Tumor-Node-Metastasis (TNM) stage and MSRB3 expression were significantly associated with OS time. Multivariate Cox regression analysis indicated that MSRB3 was an independent predicting factor for the OS time of patients with GC (P=0.049). In addition, analysis using The Cancer Genome Atlas (TCGA) database validated these results. Kaplan-Meier analysis revealed that higher MSRB3 mRNA expression was associated with poorer OS time in 442 patients with GC (P=0.004). Univariate analysis of the TCGA data indicated that age, depth of invasion, lymph node metastasis, distant metastasis, TNM stage and MSRB3 expression were significantly associated with OS time; however, sex and histological differentiation were not associated with OS time. Multivariate analysis demonstrated that MSRB3 was an independent prognostic factor in patients with GC (P=0.001). In conclusion, these results demonstrated that MSRB3 expression was upregulated in patients GC, which suggests that MSBR3 may serve as a potential prognostic biomarker.
Keywords: gastric cancer, methionine sulfoxide reductases B3, immunohistochemistry, The Cancer Genome Atlas, prognosis
Introduction
Gastric cancer (GC) is the fourth most common type of cancer and the second most common cause of cancer-associated mortality worldwide (1). In China, the morbidity and mortality rates of GC have gradually increased, which is a major public health concern (2). Although the causes of GC, including environmental and genetic factors (3,4), are commonly known, there are no effective strategies available to prevent its development. The clinical outcome of patients with advanced GC remains poor, despite major advances in treatment strategies, including surgery, radiotherapy and chemotherapy (5). Therefore, it is crucial to identify a sensitive and specific biomarker that could predict GC prognosis and may be used as a target for GC treatment.
Reactive oxygen species (ROS) are involved in cell growth, differentiation, progression and death (6), and include chemically active oxygen-containing atoms or atom groups, including superoxide radical, hydrogen peroxide and hydroxyl radical (7). Low concentrations of ROS are crucial for biological processes, including intracellular signaling and defense against microorganisms (8). In cancer cells, ROS contribute to cancer progression by amplifying genomic instability (9). However, ROS can also induce severe cellular damage, including to cancer cells (10). Both ROS-elevating and ROS-eliminating strategies can therefore be developed to treat cancer eliminate cancer cells. ROS in excess is known to attack DNA (11). The level of oxidative DNA damage is increased in various types of tumor, including melanoma, colorectal and pancreatic cancers, which strongly suggests its involvement in cancer development (12). DNA damage serves a key role in carcinogenesis (13). ROS may be involved in the three stages of carcinogenesis, which are initiation, promotion and progression (14). ROS in excess are normally eliminated by cellular antioxidant defense systems (15), which protect cell against oxidative damage.
Methionine sulfoxide reductase (MSR) in an enzyme that reduces methionine sulfoxide into methionine (16). MSR is considered as an important antioxidant enzyme for cellular ROS scavenging (17). MSRs are commonly identified in various organisms ranging from bacteria to mammals, and are also involved in protein repair and protein function regulation (18). MSRs are evolutionarily conserved. There are two isomers produced during methionine oxidation: Methionine-S-sulfoxide and methionine-R-sulfoxide, which are reduced by MSRA and MSRB, respectively (19). The human MSRA gene is located on chromosome 8 and codes for a protein located in the mitochondria, cytosol and nucleus (20–22). The human genome contains three MSRB genes that code for the proteins, MSRB1, MSRB2 and MSRB3 (23). MSRB1, also termed selenoprotein R, is present in the cytoplasm and nucleus; whereas, MSRB2 is present in the mitochondria. There are two forms of human MSRB3; MSRB3A, which is localized in the endoplasmic reticulum, and MSRB3B, which is localized in the mitochondria. MSRB3A and MSRB3B are generated via alternative first-exon splicing (24).
As an important member of the MSR family, MSRB3 is involved in the response to oxidative stress-induced tissue alteration (25). MSRB3 can prevent oncogene-induced DNA damage (26). This suggests that MSRB3 and cancer may be associated. However, to the best of our knowledge, only a few studies have reported the effects of MSRB3 in cancer cells. Morel et al (26) demonstrated that the expression of MSRB3 promotes malignant transformation of breast stem cells. Kwak et al (17) reported that MSRB3 deficiency leads to breast, lung and liver cancer cell apoptosis. In addition, the functional role of MSRB3 in the protection against oncogene-induced DNA damage may be applicable to a broad range of tumors including breast, lung and colorectal cancers (26). Although MSRB3 is highly expressed in the stomach (27), the role of MSRB3 in GC has not yet been elucidated. Therefore, the study of MSRB3 expression in human GC may provide some indications about its role in GC.
To the best of our knowledge, the expression of MSRB3 in GC and its clinical relevance have not yet been investigated. The present study aimed to investigate the expression of MSRB3 in GC samples and to determine whether MSRB3 may be associated with GC clinical outcomes. In addition, the Cancer Genome Atlas (TCGA) database was used to validate the results.
Materials and methods
Patients and tissue samples
A total of 90 formalin-fixed, paraffin-embedded GC tissues samples and paired adjacent normal tissues (at a distance of 5 cm away from the edge of the cancerous tissue) were collected from the Department of Pathology, Nanjing Drum Tower Hospital Group Suqian People's Hospital (Suqian, China). All samples were pathologically confirmed as GC and were collected from patients who underwent surgical resection between May 2007 and April 2008. The surgical specimens were fixed with 10% formalin at room temperature for 24 h. Formalin-fixed, paraffin-embedded tissue blocks were processed by pathologists in accordance with standard procedures. The sections were stored at room temperature under dry conditions. Patients had not received preoperative radiotherapy, chemotherapy or biotherapy for cancer. The patients consisted of 70 (77.8%) men and 20 (22.2%) women, and the age range was 34–83 years (median, 66 years old). A total of 62 patients succumbed to the disease during the follow-up and the median follow-up time was 38 months. The present study protocol was approved by the Ethics and Research Committees of Nanjing Drum Tower Hospital Group Suqian People's Hospital (Suqian, China) and was conducted in accordance with the principles outlined in The Declaration of Helsinki. Written informed consent was obtained from all patients included in the study. The tissue microarray (TMA) was made in accordance with the standard method (28) using a manual microarray device (Beecher Instruments). The TMA blocks contained complete clinical data, including age, sex, maximum tumor diameter, histological differentiation, depth of invasion, lymph node metastasis, distant metastasis and TNM stage (29).
Data mining
The TCGA database was used to further investigate the association between MSRB3 mRNA expression and the overall survival (OS) time of patients with GC. The TCGA database is a public patient database, which includes high-throughput genome sequencing of >11,000 tumor tissues and matched normal tissues from patients (30). According to parameters defined in previous studies (31,32), the MSRB3 expression and clinical data from the TCGA database were downloaded from the TCGA website (http://cancergenome.nih.gov/). A total of 442 GC samples that contained detailed MSRB3 expression data were available for this analysis. Patients had received no pretreatment and data comprised fully characterized tumors, OS time and complete RNAseq information. The median MSRB3 mRNA level was used as the cut-off value in tumor tissue. According to this level [median, 478.40; interquartile range (IQR), 230.63–1039.47], patients were subdivided into low and high MSRB3 expression groups for further analysis as follows: For the low MSRB3 expression group, the median was 229.36 and the IQR was 156.51–342.33. For the high MSRB3 expression group, the median was 1,035.65 and the IQR was 670.30–1,832.16.
Immunohistochemistry analysis
Some 4-µm-thick sections were cut from TMA blocks. Staining was conducted using the streptavidin-peroxidase method, according to the manufacturer's protocol (Thermo Fisher Scientific, Inc.). Briefly, sections were dewaxed in xylene and rehydrated in increasing ethanol gradients of 100, 95, 90, 85 and 70%. Then samples were boiled at 100°C in citrate buffer for antigen retrieval. Samples were blocked with 5% normal goat serum (cat. no. KL-D1418; Kalang Biologicals) for 30 min at 37°C and incubated with rabbit anti-human MSRB3 polyclonal primary antibody (1:500; cat. no. NBP1-84259; Novus Biologicals; Littleton; CO; USA) overnight at 4°C. Subsequently, samples were washed in PBS and incubated with horseradish peroxidase-conjugated goat anti-rabbit immunoglobulin G (H+L) highly cross-adsorbed secondary antibody (1:1,000; cat. no. A16110; Thermo Fisher Scientific, Inc.) at room temperature for 30 min. The peroxidase reaction was developed by 3,3′-diaminobenzidine staining. Eventually, sections were lightly counterstained with hematoxylin at room temperature for 3 min and mounted on glass slides.
Immunostaining was evaluated by two experienced pathologists using an inverted microscope (IX73; Olympus Corporation; magnification, ×200) in a double-blinded manner. A total of five microscopic fields from representative MSRB3 immune responses were examined. MSRB3 expression was scored based on staining intensity and percentage of positive cells, as previously described (33). Briefly, the percentage of positive cells was scored as 0, 1, 2, 3 or 4 for 5–25, 26–50, 51–75 and 76–100% of positive cells, respectively. The staining intensity was scored as 0, 1, 2 or 3 for a negative, weak, moderate on strong signal, respectively. The immunoreactivity score (IRS) was calculated as follows: IRS=staining percentage × intensity. IRS <6 was considered as low expression and IRS ≥6 was considered as high expression. A total of 64 and 26 cases had high and low expression of MSRB3 in GC tissues, respectively. However, 48 and 42 cases cases had high and low expression of MSRB3 in GC tissues, respectively, in non-cancerous tissues. The diagnostic value of MSRB3 for GC was therefore estimated with a sensitivity of 71.1% [64/(64+26)×100%=71.1%] and a specificity of 46.7% [42/(42+48)×100%=46.7%].
Statistical analysis
All statistical analyses were conducted using SPSS 16.0 software (SPSS Inc.). McNemar's test was used to analyze the difference in MSRB3 expression between different types of tissue. The association between MSRB3 expression and clinicopathological characteristics of patients with GC was analyzed by χ2 test. Kaplan-Meier survival curves were plotted and a log-rank test was used to compare the curves. The Cox's proportional hazards model was used to determine the factors that were significantly associated with OS time. A two-sided P<0.05 was considered to indicate a statistically significant difference.
Results
Aberrant overexpression of MSRB3 in GC tissues and the diagnostic value of MSRB3 in patients with GC
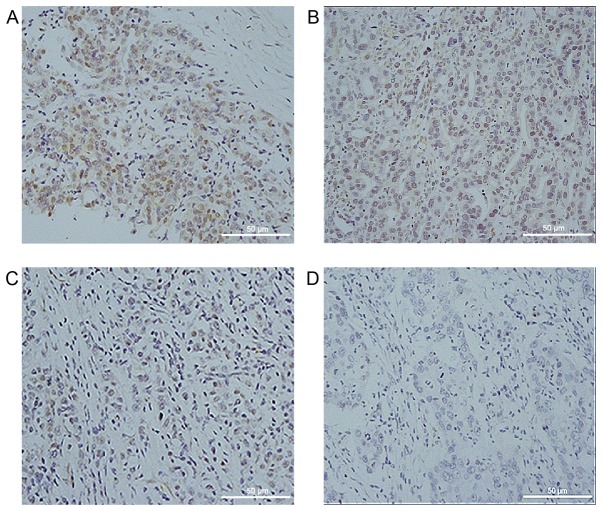
MSRB3 expression was detected by immunohistochemical staining in 90 cases of human GC tissues and paired adjacent normal tissues. As presented in Fig. 1, MSRB3 was localized in the cytoplasm of GC cells. Higher MSRB3 expression levels are presented in Fig. 1A and B, whereas lower expression levels are presented in Fig. 1C and D. Among the 90 GC samples, 64 (71.1%) exhibited a high expression of MSRB3, whereas 48 (53.3%) of the 90 paired adjacent normal tissues presented with a high MSRB3 expression level (Table I). In addition, MSRB3 protein expression was significantly different in GC tissues compared with that in the paired adjacent normal tissues (P=0.017; Table I). The diagnostic value of MSRB3 for GC was estimated with a sensitivity of 71.1% and a specificity of 46.7% (data not shown).
Figure 1.
Immunohistochemical staining of methionine sulfoxide reductases B3. (A) Strong staining; (B) moderate staining; (C) weak staining; (D) absent staining. Magnification, ×200.
Table I.
Methionine sulfoxide reductases B3 expression level in different GC and adjacent normal tissues of patients with GC.
| Adjacent normal tissues | |||
|---|---|---|---|
| GC tissues | High expression | Low expression | Total |
| High expression | 36 | 28 | 64 |
| Low expression | 12 | 14 | 26 |
| Total | 48 | 42 | 90 |
P=0.017 as assessed by McNemar's test. GC, gastric cancer.
Associations between MSRB3 protein expression and clinicopathological characteristics of patients with GC
The associations between MSRB3 expression and the clinicopathological characteristics of patients with GC were investigated. The retrieved data included patient age, sex, maximum tumor diameter, histological differentiation, depth of invasion, lymph node metastasis, distant metastasis and TNM stage. MSRB3 expression levels in the 90 GC samples were not significantly associated with age (P=0.731), sex (P=0.901), maximum tumor diameter (P=0.850), histological differentiation (P=0.972), depth of invasion (P=0.403), lymph node metastasis (P=0.850), distant metastasis (P=0.697) or TNM stage (P=0.745; Table II). The maximum tumor diameter was determined according to the Borrmann classification of cancers (34); this classification identified a diffuse invasion with an unclear boundary in 3 patients. The maximum diameter of tumor for these 3 patients was therefore difficult to determine by pathologists. Therefore, the total number of patients that were evaluated for the maximum tumor diameter was only 87 (Table II).
Table II.
MSRB3 expression and clinical characteristics of 90 patients with gastric cancer.
| MSRB3 expression | ||||
|---|---|---|---|---|
| Variable | Cases, n | Low | High | P-value |
| Age, years | 0.731 | |||
| <65 | 39 | 12 | 27 | |
| ≥65 | 51 | 14 | 37 | |
| Sex | 0.901 | |||
| Female | 20 | 6 | 14 | |
| Male | 70 | 20 | 50 | |
| Maximum tumor diameter, cm | 0.850 | |||
| <5 | 30 | 9 | 21 | |
| ≥5 | 57 | 16 | 41 | |
| Histological differentiation | 0.972 | |||
| Moderate-high | 24 | 7 | 17 | |
| Poor | 66 | 19 | 47 | |
| Depth of invasion | 0.403 | |||
| T1-2 | 11 | 2 | 9 | |
| T3-4 | 79 | 24 | 55 | |
| Lymph node metastasis | 0.850 | |||
| N0 | 23 | 7 | 16 | |
| N+ | 67 | 19 | 48 | |
| Distant metastasis | 0.697 | |||
| M0 | 86 | 24 | 62 | |
| M1 | 4 | 2 | 2 | |
| TNM stage | 0.745 | |||
| I/II | 37 | 10 | 27 | |
| III/IV | 53 | 16 | 37 | |
MSRB3, methionine sulfoxide reductases B3; TNM, Tumor-Node-Metastasis; GC, gastric cancer.
High MSRB3 expression is associated with poor clinical outcomes in patients with GC
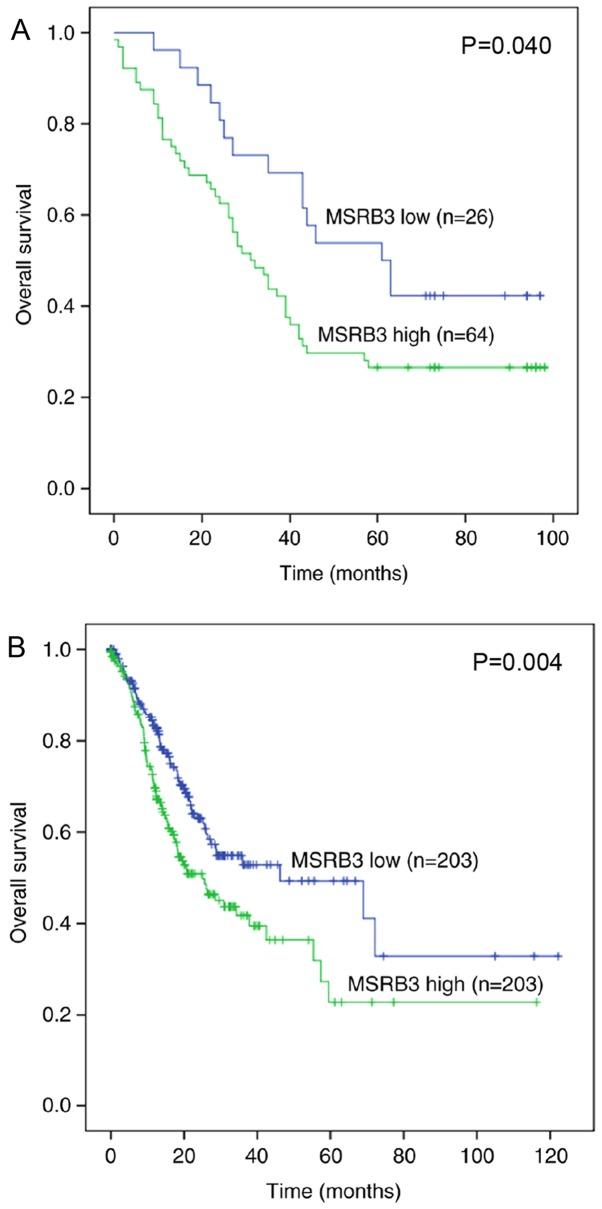
The prognostic value of MSRB3 was evaluated by a Kaplan-Meier survival curve and log-rank test. The Kaplan-Meier analysis demonstrated that patients with higher MSRB3 expression exhibited a poorer prognosis compared with those with lower MSRB3 expression (P=0.040; Fig. 2A). Univariate and multivariate Cox regression analyses were used to compare the effect of MSRB3 expression and other clinicopathological parameters on patient outcome. The univariate analysis suggested that maximum tumor diameter (P=0.002), depth of invasion (P=0.008), lymph node metastasis (P=0.006), TNM stage (P=0.001) and MSRB3 expression (P=0.045) were significantly associated with OS time; however, OS time was not associated with age, sex, histological differentiation or distant metastasis (Table III). Furthermore, multivariate analysis demonstrated that MSRB3 expression was an independent predictor in patients with GC [Hazard ratio (HR), 1.813; 95% confidence interval (CI), 1.001–3.281; P=0.049; Table III].
Figure 2.
Kaplan-Meier survival curves for MSRB3 expression level in patients with GC. (A) OS time curves for patients with GC (n=90) expressing high or low levels of MSRB3. Patients with high MSRB3 expression exhibited a significantly shorter OS time compared with those with low MSRB3 expression (P=0.040). (B) OS time curves for patients with GC (n=442) from The Cancer Genome Atlas database. Patients with high MSRB3 expression level exhibited a significantly shorter OS time compared with patients with low MSRB3 expression level (P=0.004). GC, gastric cancer; MSRB3, methionine sulfoxide reductases B3; OS, overall survival.
Table III.
Univariate and multivariate Cox regression analysis of overall survival time in 90 patients with gastric cancer.
| Univariate analysis | Multivariate analysis | |||||
|---|---|---|---|---|---|---|
| Variable | HR | 95% CI | P-value | HR | 95% CI | P-value |
| Age: <65 vs. ≥65 years | 1.518 | 0.906–2.544 | 0.113 | |||
| Sex: Female vs. male | 0.936 | 0.516–1.698 | 0.827 | |||
| Maximum tumor diameter: <5 vs. ≥5 cm | 2.559 | 1.401–4.677 | 0.002a | 1.818 | 0.986–3.351 | 0.056 |
| Histological differentiation: Moderate-high vs. poor | 1.480 | 0.815–2.687 | 0.198 | |||
| Depth of invasion: T1-2 vs. T3-4 | 6.817 | 1.661–27.980 | 0.008a | 10.038 | 1.329–75.839 | 0.025a |
| Lymph node metastasis: N0 vs. N+ | 2.595 | 1.314–5.122 | 0.006a | 2.167 | 0.793–5.922 | 0.132 |
| Distant metastasis: M0 vs. M1 | 2.251 | 0.809–6.261 | 0.120 | |||
| TNM stage: I/II vs. III/IV | 2.586 | 1.488–4.495 | 0.001a | 1.138 | 0.505–2.564 | 0.756 |
| MSRB3 expression: Low vs. high | 1.817 | 1.013–3.257 | 0.045a | 1.813 | 1.001–3.281 | 0.049a |
P<0.05. CI, confidence interval; GC, gastric cancer; HR, hazard ratio; MSRB3, methionine sulfoxide reductases B3; TNM, Tumor-Node-Metastasis.
To validate the prognostic significance of MSRB3 in a large group of patients with GC, the TCGA database was used to examine the association between MSRB3 mRNA expression and prognosis. A Kaplan-Meier survival curve and log-rank test indicated that high MSRB3 mRNA expression in 442 patients with GC was associated with a poorer OS time (P=0.004; Fig. 2B) compared with a low MSRB3 expression level. Univariate analysis indicated that age (P=0.020), depth of invasion (P=0.003), lymph node metastasis (P<0.001) distant metastasis (P<0.001), TNM stage (P<0.001) and MSRB3 expression (P=0.004) were significantly associated with OS time; however, OS time was not associated with sex or histological differentiation (Table IV). The results from multivariate analysis suggested that MSRB3 may be an independent prognostic factor in patients with GC (HR, 1.755; 95% CI, 1.248–2.466; P=0.001; Table IV).
Table IV.
Univariate and multivariate Cox regression analysis of overall survival time in 442 patients with gastric cancer from The Cancer Genome Atlas database.
| Univariate analysis | Multivariate analysis | |||||
|---|---|---|---|---|---|---|
| Variable | HR | 95% CI | P-value | HR | 95% CI | P-value |
| Age: <65 vs. ≥65 years | 1.451 | 1.061–1.984 | 0.020a | 1.806 | 1.268–2.573 | 0.001 |
| Sex: Female vs. male | 1.094 | 0.797–1.503 | 0.579 | |||
| Histological differentiation: Moderate-high vs. poor | 1.308 | 0.950–1.801 | 0.100 | |||
| Depth of invasion: T1-2 vs. T3-4 | 1.837 | 1.234–2.733 | 0.003a | 1.275 | 0.781–2.083 | 0.331 |
| Lymph node metastasis: N0 vs. N+ | 2.159 | 1.460–3.191 | <0.001a | 1.620 | 0.921–2.851 | 0.094 |
| Distant metastasis: M0 vs. M1 | 2.612 | 1.578–4.323 | <0.001a | 2.313 | 1.282–4.173 | 0.005a |
| TNM stage: I/II vs. III/IV | 2.128 | 1.520–2.981 | <0.001a | 1.242 | 0.731–2.111 | 0.423 |
| MSRB3 mRNA expression: Low vs. high | 1.589 | 1.158–2.180 | 0.004a | 1.755 | 1.248–2.466 | 0.001a |
P<0.05. CI, confidence interval; GC, gastric cancer; HR, hazard ratio; MSRB3, methionine sulfoxide reductases B3; TNM, Tumor-Node-Metastasis.
Discussion
The present study investigated the expression of MSRB3 in GC tissues and its association with the clinicopathological characteristics and prognosis of patients with GC. The results revealed that MSRB3 expression level in GC samples was significantly higher compared with in corresponding normal gastric tissues (P=0.017). The current results also suggested that high MSRB3 expression was associated with a poorer prognosis for patients with GC, which was consistent with the data obtained from the TCGA database. In addition, the expression of MSRB3 was demonstrated to be an independent prognostic factor in patients with GC at the mRNA and protein levels.
MSRB3 is present in the ER and mitochondria of human cells (23), and acts as an antioxidant and protein repair enzyme by specifically catalyzing the reduction of methionine-R-sulfoxide residues in proteins (35). The highest MSRB3 expression levels are observed in the bladder, heart, skeletal muscles, aorta and lung (27). MSRB3 is also highly expressed in the digestive system, including the stomach and intestines (27). Physiologically, MSRB3 is important for mouse and human hearing (36,37), and serves a crucial role in normal cell proliferation (38,39). MSRB3 deficiency causes G1/S cell cycle arrest by regulating the expression of heme oxygenase-1, p21 and p27, thereby inhibiting normal cell proliferation (38,39). In addition, MSRB3 deficiency increases intracellular ROS levels, leading to redox imbalance, and also increases the Bax/Bcl-2 ratio and cytochrome c release from the mitochondria into the cytosol, which results in caspases activation and cell apoptosis (40,41).
The effect of MSRB3 on cancer cells has been previously investigated. Morel et al (26) demonstrated that the expression of MSRB3 enables mammary stem cells to bypass critical anti-tumor barriers by preventing oncogene-induced cellular stress, thereby promoting malignant transformation. Kwak et al (42) further reported that MSRB3 is involved in the regulation of cancer cell proliferation and apoptosis. In addition, MSRB3 deficiency has been demonstrated to lead to breast, lung and liver cancer cell apoptosis (17). These previous findings were consistent with the results from the present study, which demonstrated that increased MSRB3 expression was associated with poor clinical outcomes of patients with GC. Furthermore, TCGA database analysis of MSRB3 mRNA expression validated these results. MSRB3 is understood to serve a crucial role in cell protection (24); notably, the results from the current study suggest that this protective effect may also include the protection of cancer cells.
Based on the results from the present study, low MSRB3 expression was hypothesized to cause GC cell apoptosis, which could lead to better clinical outcomes. A previous study demonstrated that low expression of MSRB3 causes a negative response (cancer cell death), whereas its high expression leads to a positive response (cancer cell proliferation) (42). MSRB3 may also be involved in the apoptosis of GC cells, as it is involved in lung, breast, and liver cancer cells (17). The underlying mechanism of high MSRB3 expression-mediated poor prognosis in patients with GC requires further investigation. Studies on the caspase family may help elucidate the mechanisms involved in MSRB3 downregulation-induced cell death.
MSRB3 expression level was not associated with any clinicopathological parameters of patients with GC, but was significantly associated with OS time. Particularly, high MSRB3 mRNA and protein expression levels were significantly associated with poorer OS time. Since MSRB3 was not associated with clinicopathological characteristics, it was suggested to be an independent prognostic factor. This hypothesis was subsequently verified by Cox regression analysis. Multivariate Cox regression analysis confirmed that MSRB3 expression was a significant independent prognostic factor in patients with GC. This result was further verified by the analysis of 442 GC cases from the TCGA database. Numerous studies have analyzed the clinicopathologic prognostic factors for GC from various countries. Certain controversial factors, including sex, age, tumor diameter and differentiation, depth of invasion, lymph node metastasis, distant metastasis and TNM stage have been considered as independent predictors (43,44). However, no consensus on the optimum predictors was reached. In the present study, besides MSRB3 expression, depth of invasion, age and distant metastasis were considered as independent prognostic factors. TNM stage was excluded from the multivariate analysis. Maximum tumor diameter, depth of invasion, lymph node metastasis, TNM stage and MSRB3 expression were identified to be significantly associated with OS time in the univariate analysis. Subsequently, these five factors were further analyzed by multivariate analysis in order to screen for independent prognostic factors. Since the factor TNM stage is associated with maximum tumor diameter and lymph node metastasis, it was considered not to be an independent factor; therefore, it was excluded from the multivariate analysis. By contrast, MSRB3 expression was revealed to be independent of other factors and may therefore be considered as an independent prognostic factor. These results indicate that MSRB3 may serve an important role in cancer and serve as a prognostic biomarker for GC.
Some limitations to this study should be addressed. Firstly, the present study was a single-center study enrolling limited number of patients. Secondly, the retrospective design covered a period of 10 years and tissue sections from paraffin blocks may exhibit a considerable diminution in antigenicity. Thirdly, many cases were excluded because of neoadjuvant chemotherapy, which would cause collection bias. Eventually, this study only used immunohistochemistry technique, which may cause bias in the results. Further investigation using a multi-center and prospective study and involving additional techniques is necessary to improve the accuracy of the results.
In conclusion, the results from the present study demonstrated that MSRB3 expression was increased in GC tissues and was associated with poorer prognosis in patients with GC. This suggests that MSRB3 may be considered as a potential novel prognostic biomarker for patients with GC and as an effective molecular target for GC treatment. However, further investigation is required to fully elucidate the mechanisms underlying the role of MSRB3 in GC.
Acknowledgements
The authors would like to thank Dr Xiaohong Shi and Dr Xiaoling Jiang (Suqian Hospital Affiliated to Xuzhou Medical University, Xuzhou, China) for evaluating the immunostaining signals.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present study are available from the corresponding author on reasonable request.
Authors' contributions
JWu provided ideas, designed the study, interpreted the data and helped writing and revising the manuscript in a critical way. XM and HH prepared the tissue sections and analyzed the data. JWa and MZ conducted the immunohistochemistry. XM performed the statistical analysis. JWa participated in the analyses of experimental data and of the online public data from The Cancer Genome Atlas. The manuscript was written by XM, and reviewed by JWa and JWu. All authors read and approved the final manuscript.
Ethics approval and consent to participate
The present study was approved by the Ethics and Research Committees of Nanjing Drum Tower Hospital Group Suqian People's Hospital (Suqian, China) and was conducted in accordance with the principles outlined in The Declaration of Helsinki. Written informed consent was provided by the patients and/or guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90. doi: 10.3322/caac.20107. [DOI] [PubMed] [Google Scholar]
- 2.Shen YH, Xie ZB, Yue AM, Wei QD, Zhao HF, Yin HD, Mai W, Zhong XG, Huang SR. Expression level of microRNA-195 in the serum of patients with gastric cancer and its relationship with the clinicopathological staging of the cancer. Eur Rev Med Pharmacol Sci. 2016;20:1283–1287. [PubMed] [Google Scholar]
- 3.Miao R, Guo X, Zhi Q, Shi Y, Li L, Mao X, Zhang L, Li C. VEZT, a novel putative tumor suppressor, suppresses the growth and tumorigenicity of gastric cancer. PLoS One. 2013;8:e74409. doi: 10.1371/journal.pone.0074409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen Y, Pan K, Li S, Xia J, Wang W, Chen J, Zhao J, Lü L, Wang D, Pan Q, et al. Decreased expression of V-set and immunoglobulin domain containing 1 (VSIG1) is associated with poor prognosis in primary gastric cancer. J Surg Oncol. 2012;106:286–293. doi: 10.1002/jso.22150. [DOI] [PubMed] [Google Scholar]
- 5.Lee J, Lim DH, Kim S, Park SH, Park JO, Park YS, Lim HY, Choi MG, Sohn TS, Noh JH, et al. Phase III trial comparing capecitabine plus cisplatin versus capecitabine plus cisplatin with concurrent capecitabine radiotherapy in completely resected gastric cancer with D2 lymph node dissection: The ARTIST trial. J Clin Oncol. 2012;30:268–273. doi: 10.1200/JCO.2011.39.1953. [DOI] [PubMed] [Google Scholar]
- 6.Matés JM, Pérez-Gómez C, Núñez de Castro I. Antioxidant enzymes and human diseases. Clin Biochem. 1999;32:595–603. doi: 10.1016/S0009-9120(99)00075-2. [DOI] [PubMed] [Google Scholar]
- 7.Krause KH. Aging: A revisited theory based on free radicals generated by NOX family NADPH oxidases. Exp Gerontol. 2007;42:256–262. doi: 10.1016/j.exger.2006.10.011. [DOI] [PubMed] [Google Scholar]
- 8.Valko M, Izakovic M, Mazur M, Rhodes CJ, Telser J. Role of oxygen radicals in DNA damage and cancer incidence. Mol Cell Biochem. 2004;266:37–56. doi: 10.1023/B:MCBI.0000049134.69131.89. [DOI] [PubMed] [Google Scholar]
- 9.Schumacker PT. Reactive oxygen species in cancer cells: Live by the sword, die by the sword. Cancer Cell. 2006;10:175–176. doi: 10.1016/j.ccr.2006.08.015. [DOI] [PubMed] [Google Scholar]
- 10.Pelicano H, Carney D, Huang P. ROS stress in cancer cells and therapeutic implications. Drug Resist Updat. 2004;7:97–110. doi: 10.1016/j.drup.2004.01.004. [DOI] [PubMed] [Google Scholar]
- 11.Valko M, Leibfritz D, Moncol J, Cronin MT, Mazur M, Telser J. Free radicals and antioxidants in normal physiological functions and human disease. Int J Biochem Cell Biol. 2007;39:44–84. doi: 10.1016/j.biocel.2006.07.001. [DOI] [PubMed] [Google Scholar]
- 12.Valko M, Rhodes CJ, Moncol J, Izakovic M, Mazur M. Free radicals, metals and antioxidants in oxidative stress-induced cancer. Chem Biol Interact. 2006;160:1–40. doi: 10.1016/j.cbi.2005.12.009. [DOI] [PubMed] [Google Scholar]
- 13.Cooke MS, Evans MD, Dizdaroglu M, Lunec J. Oxidative DNA damage: Mechanisms, mutation, and disease. FASEB J. 2003;17:1195–1214. doi: 10.1096/fj.02-0752rev. [DOI] [PubMed] [Google Scholar]
- 14.Klaunig JE, Kamendulis LM. The role of oxidative stress in carcinogenesis. Annu Rev Pharmacol Toxicol. 2004;44:239–267. doi: 10.1146/annurev.pharmtox.44.101802.121851. [DOI] [PubMed] [Google Scholar]
- 15.Halliwell B. Antioxidants in human health and disease. Annu Rev Nutr. 1996;16:33–50. doi: 10.1146/annurev.nu.16.070196.000341. [DOI] [PubMed] [Google Scholar]
- 16.Kim HY, Gladyshev VN. Methionine sulfoxide reductases: Selenoprotein forms and roles in antioxidant protein repair in mammals. Biochem J. 2007;407:321–329. doi: 10.1042/BJ20070929. [DOI] [PubMed] [Google Scholar]
- 17.Kwak GH, Kim TH, Kim HY. Down-regulation of MsrB3 induces cancer cell apoptosis through reactive oxygen species production and intrinsic mitochondrial pathway activation. Biochem Biophys Res Commun. 2017;483:468–474. doi: 10.1016/j.bbrc.2016.12.120. [DOI] [PubMed] [Google Scholar]
- 18.Kim HY. The methionine sulfoxide reduction system: Selenium utilization and methionine sulfoxide reductase enzymes and their functions. Antioxid Redox Signal. 2013;19:958–969. doi: 10.1089/ars.2012.5081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lim DH, Han JY, Kim JR, Lee YS, Kim HY. Methionine sulfoxide reductase B in the endoplasmic reticulum is critical for stress resistance and aging in Drosophila. Biochem Biophys Res Commun. 2012;419:20–26. doi: 10.1016/j.bbrc.2012.01.099. [DOI] [PubMed] [Google Scholar]
- 20.Kim HY, Gladyshev VN. Role of structural and functional elements of mouse methionine-S-sulfoxide reductase in its subcellular distribution. Biochemistry. 2005;44:8059–8067. doi: 10.1021/bi0501131. [DOI] [PubMed] [Google Scholar]
- 21.Kim G, Cole NB, Lim JC, Zhao H, Levine RL. Dual sites of protein initiation control the localization and myristoylation of methionine sulfoxide reductase A. J Biol Chem. 2010;285:18085–18094. doi: 10.1074/jbc.M110.119701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vougier S, Mary J, Friguet B. Subcellular localization of methionine sulphoxide reductase A (MsrA): Evidence for mitochondrial and cytosolic isoforms in rat liver cells. Biochem J. 2003;373:531–537. doi: 10.1042/bj20030443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kim HY, Gladyshev VN. Methionine sulfoxide reduction in mammals: Characterization of methionine-R-sulfoxide reductases. Mol Biol Cell. 2004;15:1055–1064. doi: 10.1091/mbc.e03-08-0629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kwak GH, Lim DH, Han JY, Lee YS, Kim HY. Methionine sulfoxide reductase B3 protects from endoplasmic reticulum stress in Drosophila and in mammalian cells. Biochem Biophys Res Commun. 2012;420:130–135. doi: 10.1016/j.bbrc.2012.02.128. [DOI] [PubMed] [Google Scholar]
- 25.Zhang C, Jia P, Jia Y, Li Y, Webster KA, Huang X, Achary M, Lemanski SL, Lemanski LF. Anoxia, acidosis, and intergenic interactions selectively regulate methionine sulfoxide reductase transcriptions in mouse embryonic stem cells. J Cell Biochem. 2011;112:98–106. doi: 10.1002/jcb.22876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Morel AP, Ginestier C, Pommier RM, Cabaud O, Ruiz E, Wicinski J, Devouassoux-Shisheboran M, Combaret V, Finetti P, Chassot C, et al. A stemness-related ZEB1-MSRB3 axis governs cellular pliancy and breast cancer genome stability. Nat Med. 2017;23:568–578. doi: 10.1038/nm.4323. [DOI] [PubMed] [Google Scholar]
- 27.Hansel A, Jung S, Hoshi T, Heinemann SH. A second human methionine sulfoxide reductase (hMSRB2) reducing methionine-R-sulfoxide displays a tissue expression pattern distinct from hMSRB1. Redox Rep. 2003;8:384–388. doi: 10.1179/135100003225003429. [DOI] [PubMed] [Google Scholar]
- 28.Oakley GJ, Fuhrer K, Seethala RR. Brachyury, SOX-9, and podoplanin, new markers in the skull base chordoma vs chondrosarcoma differential: A tissue microarray-based comparative analysis. Mod Pathol. 2008;21:1461–1469. doi: 10.1038/modpathol.2008.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Washington K. 7th edition of the AJCC cancer staging manual: Stomach. Ann Surg Oncol. 2010;17:3077–3079. doi: 10.1245/s10434-010-1362-z. [DOI] [PubMed] [Google Scholar]
- 30.Tomczak K, Czerwińska P, Wiznerowicz M. The Cancer Genome Atlas (TCGA): An immeasurable source of knowledge. Contemp Oncol (Pozn) 2015;19:A68–A77. doi: 10.5114/wo.2014.47136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jiang YZ, Yu KD, Zuo WJ, Peng WT, Shao ZM. GATA3 mutations define a unique subtype of luminal-like breast cancer with improved survival. Cancer. 2014;120:1329–1337. doi: 10.1002/cncr.28566. [DOI] [PubMed] [Google Scholar]
- 32.Li Y, Liang L, Dai W, Cai G, Xu Y, Li X, Li Q, Cai S. Prognostic impact of programed cell death-1 (PD-1) and PD-ligand 1 (PD-L1) expression in cancer cells and tumor infiltrating lymphocytes in colorectal cancer. Mol Cancer. 2016;15:55. doi: 10.1186/s12943-016-0539-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ueno H, Jones AM, Wilkinson KH, Jass JR, Talbot IC. Histological categorisation of fibrotic cancer stroma in advanced rectal cancer. Gut. 2004;53:581–586. doi: 10.1136/gut.2003.028365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Espejo Romero H, Navarrete Siancas J. Classification of stomach adenocarcinomas. Rev Gastroenterol Peru. 2003;23:199–212. (In Spanish) [PubMed] [Google Scholar]
- 35.Kwak GH, Kim JR, Kim HY. Expression, subcellular localization, and antioxidant role of mammalian methionine sulfoxide reductases in Saccharomyces cerevisiae. BMB Rep. 2009;42:113–118. doi: 10.5483/BMBRep.2009.42.2.113. [DOI] [PubMed] [Google Scholar]
- 36.Kwon TJ, Cho HJ, Kim UK, Lee E, Oh SK, Bok J, Bae YC, Yi JK, Lee JW, Ryoo ZY, et al. Methionine sulfoxide reductase B3 deficiency causes hearing loss due to stereocilia degeneration and apoptotic cell death in cochlear hair cells. Hum Mol Genet. 2014;23:1591–1601. doi: 10.1093/hmg/ddt549. [DOI] [PubMed] [Google Scholar]
- 37.Ahmed ZM, Yousaf R, Lee BC, Khan SN, Lee S, Lee K, Husnain T, Rehman AU, Bonneux S, Ansar M, et al. Functional null mutations of MSRB3 encoding methionine sulfoxide reductase are associated with human deafness DFNB74. Am J Hum Genet. 2011;88:19–29. doi: 10.1016/j.ajhg.2010.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kwak GH, Kim KY, Kim HY. Methionine sulfoxide reductase B3 deficiency stimulates heme oxygenase-1 expression via ROS-dependent and Nrf2 activation pathways. Biochem Biophys Res Commun. 2016;473:1033–1038. doi: 10.1016/j.bbrc.2016.04.011. [DOI] [PubMed] [Google Scholar]
- 39.Lee E, Kwak GH, Kamble K, Kim HY. Methionine sulfoxide reductase B3 deficiency inhibits cell growth through the activation of p53-p21 and p27 pathways. Arch Biochem Biophys. 2014;547:1–5. doi: 10.1016/j.abb.2014.07.029. [DOI] [PubMed] [Google Scholar]
- 40.Ran Q, Liang H, Gu M, Qi W, Walter CA, Roberts LJ, II, Herman B, Richardson A, Van Remmen H. Transgenic mice overexpressing glutathione peroxidase 4 are protected against oxidative stress-induced apoptosis. J Biol Chem. 2004;279:55137–55146. doi: 10.1074/jbc.M410387200. [DOI] [PubMed] [Google Scholar]
- 41.Torres M. Mitogen-activated protein kinase pathways in redox signaling. Front Biosci. 2003;8:d369–d391. doi: 10.2741/999. [DOI] [PubMed] [Google Scholar]
- 42.Kwak GH, Kim HY. MsrB3 deficiency induces cancer cell apoptosis through p53-independent and ER stress-dependent pathways. Arch Biochem Biophys. 2017;621:1–5. doi: 10.1016/j.abb.2017.04.001. [DOI] [PubMed] [Google Scholar]
- 43.Murakami D, Tsujitani S, Osaki T, Saito H, Katano K, Tatebe S, Ikeguchi M. Expression of phosphorylated Akt (pAkt) in gastric carcinoma predicts prognosis and efficacy of chemotherapy. Gastric Cancer. 2007;10:45–51. doi: 10.1007/s10120-006-0410-7. [DOI] [PubMed] [Google Scholar]
- 44.Yokota T, Ishiyama S, Saito T, Teshima S, Narushima Y, Murata K, Iwamoto K, Yashima R, Yamauchi H, Kikuchi S. Lymph node metastasis as a significant prognostic factor in gastric cancer: A multiple logistic regression analysis. Scand J Gastroenterol. 2004;39:380–384. doi: 10.1080/00365520310008629. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the present study are available from the corresponding author on reasonable request.