Abstract
Background
Idiopathic systemic capillary leak syndrome (ISCLS), is a rare disorder characterized by recurrent attacks of varying severity of hypovolemic shock and generalized edema in association with hemoconcentration and hypoalbuminemia in the absence of albuminuria. The chronic form of ISCLS is extremely rare with only a few cases reported in the literature.
Case presentation
Here we report the case of a young woman who developed chronic ISCLS characterized by massive, generalized and persistent edema. The work up confirmed the presence of monoclonal gammopathy. She was treated with several agents with no response.
Conclusion
Chronic ISCLS is a very rare disease of unknown etiology and results in devastating complications. The medical community should be aware of this disease with the hope that targeted therapy will become available in the future.
Keywords: Capillary leak syndrome, Clarkson disease
Case
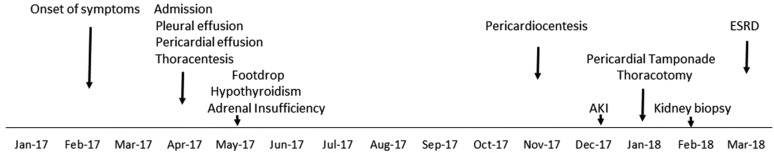
A 23-year-old female patient who is known to have type 1 diabetes mellitus since the age of 12 years. Her blood sugar had been poorly controlled. She was transferred to our hospital from another institution in April, 2017 for evaluation of anasarca. Two months prior to her admission she started developing generalized body swelling with no associated arthritis, arthralgia or hair loss. There was no family history of similar illness. Her weight was 140 kg. Her weight prior to her illness was around 70 kg. Her exam was significant for massive anasarca involving all extremities, abdominal wall and back. She developed bilateral pleural effusions and pericardial effusion with tamponade. She later on developed bilateral foot drop, adrenal insufficiency, hypothyroidism, acute kidney injury and end stage renal disease (ESRD) (Fig. 1).
Fig. 1.
Timeline of clinical events. AKI acute kidney injury, ESRD end stage renal disease
Laboratory tests
Admission hemoglobin was 13.7 (12.0–16.0) gm/dL. The white blood cell count with differential and platelet counts were normal. Renal function and liver function were normal. Urinalysis showed no proteinuria. Random urine creatinine was 199 mg/dL and urinary sodium was 8 mmol/L. B-type natriuretic peptide: 18. Serum albumin was 3.1 (3.4–4.7) g/dL. Thyroid stimulating hormone was 5.18 (0.35–4.94) μIU/mL, free T4: 0.93 (0.68–2.53) ng/dL and free T3: 1.62 (1.71–3.71) pg/mL. The chest X-ray showed bilateral pleural effusions. The echocardiogram showed normal ejection fraction greater than 55% and a large pericardial effusion with impending tamponade. The pleural fluid analysis showed: LDH: 65 U/L, total protein: 2.7 g/dL (simultaneous serum sample: protein 5.2 (6.3–7.9) g/dL, LDH: 133 (120–246) U/L. The anti-nuclear antibodies were positive at 1:80 with speckled pattern. The anti-double-stranded deoxyribonucleic acid (DNA) was negative. The antibodies to extractable nuclear antigens were all negative. C-reactive protein was 0.8, and erythrocytes sedimentation rate was 8 mm/hr. C3:91 (9–180), C4:23 (10–40) mg/dL and total serum complements (CH50) were 45 (30–75) U/mL. Hepatitis B, C and HIV serologies were negative. Tissue glutaminase IgA antibodies were < 1.2 U/mL (normal < 4.0 U/mL). Serum protein electrophoresis showed: total protein 4.9 (6.3–7.9) g/dL, albumin: 2.2 (3.4–4.7) g/dL, alpha-1 globulin: 0.2 (0.1–0.3) g/dL, alpha-2 globulin: 0.9 (0.6–1.0) g/dL, beta-globulin: 0.6 (0.7–1.2) g/dL, gamma-globulin: 1.0 (0.6–1.6) g/dL, albumin/globulin ratio: 0.84. The serum immunofixation showed small monoclonal IgG kappa within the gamma fraction. Kappa and lambda free light chains were 5.54 and 1.80 mg/dL respectively. The Kappa/lambda ratio was 3.08. Total IgG: 936 (767–1590) mg/dL, the IgG subclasses: IgG1: 704 (341–894) mg/dL, IgG2: 66 (171–632) mg/dL, IgG3: 20.9 (18.4–106) mg/dL, IgG4: < 0.3 (2.4–121) mg/dL. C1 esterase inhibitor level was 33 (19–37) mg/dL. Total vitamin D was 5.0 (25–80) ng/mL. Abdominal fat biopsy was negative for amyloid deposition by Congo red stain.
Hospital course
She required thoracentesis repeatedly to treat the persistent pleural effusion. She also required pericardiocentesis. She was tried on multiple medications that have been shown in earlier case reports to be effective in treating capillary leak syndrome including: high dose systemic corticosteroids, several doses of intravenous immunoglobulins (IVIG) followed by monthly administration for 6 months (2 gm/kg body weight), intravenous Theophylline, Terbutaline, Bevacizumab (two doses 2 weeks apart), intravenous methylene blue, and Thalidomide for 4 months. She did not respond to any of these modalities (Table 1).
Table 1.
Therapeutic agents used during the course of illness
| Agent | Dose | Duration | Response |
|---|---|---|---|
| Methyl-prednisone | 500 mg/day | Several doses | No |
| IVIG | 2 gm/kg | Several doses followed by monthly for 6 months | No |
| Intravenous theophylline | 5 mg/kg followed by 0.4 mg/kg/h | 2 days | No |
| Terbutaline | 5 mg three times/day | 14 days | No |
| Bevacizumab | 5 mg/kg | 2 doses 2 weeks apart | No |
| Intravenous methylene blue | 2 mg/kg | One dose | No |
| Thalidomide | 200 mg daily | 4 months | No |
IVIG intravenous immunoglobulins
She had developed recurrent episodes of sepsis related to central line infection and pneumonia and required transfer to the intensive care unit on multiple occasions. She also developed pericardial tamponade and required thoracotomy, pericardial drainage and creation of a large pericardial window. As a result of the septic episodes and the cardiac procedure, she developed acute kidney injury and was started on continuous renal replacement therapy and later was switched to intermittent hemodialysis. After 6 weeks on dialysis, a kidney biopsy was performed and showed acute tubular necrosis with regenerating renal tubules. She however did not recover and became dialysis dependent requiring daily dialysis in an attempt to control the edema. After 24 months of continuous hospitalization with frequent transfers to the step down unit and intensive care unit, she still has massive edema mainly in the lower extremities requiring daily dialysis, is bedbound, and has bilateral foot drop. She has suffered from immobilization hypercalcemia, bone fractures and decubitus ulcerations.
Discussion
The patient represents a rare case of severe and chronic ISCLS where she developed massive and persistent generalized edema in addition to bilateral pleural effusion and pericardial effusion. The initial laboratory values were normal except for the presence of monoclonal gammopathy.
The classic systemic capillary leak syndrome is a rare disease of reversible plasma extravasation and vascular collapse accompanied by hemoconcentration and hypoalbuminemia [1, 2]. The first description of the syndrome was by Clarkson et al. who described a case of a 32-year-old woman who experienced “a strange cyclical illness in which she intermittently had a sudden massive movement of plasma from her vascular bed [3]. Typically, patients experience the development of massive edema and shock after a nonspecific prodrome of weakness, fatigue, and myalgias. They may develop ischemia-induced organ failure, rhabdomyolysis, compartment syndromes, and venous thromboembolism. These manifestations may rapidly resolve and patients may experience recurrent and intermittent attacks with spontaneous recovery. Less than 500 cases have been reported in the literature since the initial description by Clarkson et al. [4]. On the other hand the chronic form of ISCLS is extremely rare with only a few cases reported in the literature [5–8]. Unlike the classic form of ISCLS, chronic ISCLS is characterized by persistent edema with no signs of recovery and may be responsive to treatment with systemic steroids and IVIG [5, 7]. Similar to our case, monoclonal gammopathy is classically found in both forms of ISCLS. ISCLS is a life-threatening disorder that carries a high mortality rate. The pathogenesis is poorly understood and is believed to be a manifestation of transient endothelial dysfunction due to endothelial contraction, apoptosis, injury, or a combination of these factors [1]. Exaggerated microvascular endothelial responses to surges of otherwise routinely encountered inflammatory mediators have been also suggested [4]. Certain cytokines were found to be elevated in acute ISCLS sera compared to baseline or sera from healthy controls, including CXCL10, CCL2, IL-1β, IL-6, IL-8, IL-12 and tumor necrosis factor α (TNFα) [9].
In severe forms, patients may develop persistent and chronic edema with no sign of recovery. Our patient represents this type of chronic ISCLS where she developed severe and persistent generalized edema and showed no response to any of the modalities that had been previously tried. She also developed hypothyroidism and adrenal insufficiency which may be related to extravasational loss of hormones and their serum binding proteins [10].
The diagnosis of ISCLS is made clinically after excluding conditions that may have a similar presentation such as sepsis, anaphylaxis and angioedema. There is no established treatment for ISCLS and management is mainly supportive directed towards correction of intravascular volume depletion, maintaining organ perfusion, and avoiding severe metabolic acidosis. Crystalloids and or protein containing solutions may be used to maintain hemodynamic stability. Caution must be exercised as excessive fluid administration may lead to worsening edema and development of compartment syndrome. Different modalities have been tried to treat this devastating illness with some success in case reports and case series including vascular endothelial growth factor (VEGF), TNFα, Theophylline, IVIG, Terbutaline and Thalidomide [11–20].
In conclusion, we have described a case of severe chronic ISCLS that has not responded to any modality of treatment. The patient ended up with devastating complications. The medical community should be aware of this disease with the hope that targeted therapy will become available in the future.
Acknowledgements
The authors thank Dr. Kirk Druey from National Institute of Allergy and Infectious Diseases, National Institutes of Health, Bethesda, Maryland for reviewing and commenting on the case. Opinions expressed in this article are those of the authors and not necessarily of Johns Hopkins Aramco Healthcare (JHAH). Therapeutic agents used in this case were all off-label.
Abbreviations
- ISCLS
idiopathic systemic capillary leak syndrome
- DNA
deoxyribonucleic acid
- IVIG
intravenous immunoglobulins
- VEGF
vascular endothelial growth factor
- IL
interleukin
Authors’ contributions
AMA provided care to the patient, made the diagnosis of ISCLS and did the writing of the manuscript. AHK collected data and helped in caring for the patient. MAET provided medical care to the patient. All authors read and approved the final manuscript.
Funding
None.
Availability of data and materials
Not applicable.
Ethics approval and consent to participate
An informed consent was obtained from the patient prior to publication.
Consent for publication
Approval to publish this case report was obtained by the Institutional Review Board at JHAH.
Competing interests
The authors declare that they no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Ahmed M. Alkhunaizi, Phone: 966-13-870-7794, Email: aalkhunaizi@gmail.com
Abdullah H. Kabbani, Email: abdullah_kabbani@hotmail.co.uk
Mohamed A. ElTigani, Email: mohamed.eltigani@jhah.com
References
- 1.Druey KM, Greipp PR. Narrative review: the systemic capillary leak syndrome. Ann Intern Med. 2010;153(2):90–98. doi: 10.7326/0003-4819-153-2-201007200-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kapoor P, Greipp PT, Schaefer EW, Mandrekar SJ, Kamal AH, Gonzalez-Paz NC, et al. Idiopathic systemic capillary leak syndrome (Clarkson’s disease): the Mayo clinic experience. Mayo Clin Proc. 2010;85(10):905–912. doi: 10.4065/mcp.2010.0159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Clarkson B, Thompson D, Horwith M, Luckey EH. Cyclical edema and shock due to increased capillary permeability. Am J Med. 1960;29:193–216. doi: 10.1016/0002-9343(60)90018-8. [DOI] [PubMed] [Google Scholar]
- 4.Druey KM, Parikh SM. Idiopathic systemic capillary leak syndrome (Clarkson disease) J Allergy Clin Immunol. 2017;140(3):663–670. doi: 10.1016/j.jaci.2016.10.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Airaghi L, Montori D, Santambrogio L, Miadonna A, Tedeschi A. Chronic systemic capillary leak syndrome. Report of a case and review of the literature. J Intern Med. 2000;247(6):731–735. doi: 10.1046/j.1365-2796.2000.00693.x. [DOI] [PubMed] [Google Scholar]
- 6.Bajwa R, Starr J, Daily K. Gemcitabine-induced chronic systemic capillary leak syndrome. BMJ Case Rep. 2017 doi: 10.1136/bcr-2017-221068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mullane R, Langewisch E, Florescu M, Plumb T. Chronic systemic capillary leak syndrome treatment with intravenous immune globulin: case report and review of the literature. Clin Nephrol. 2019;91(1):59–63. doi: 10.5414/CN109467. [DOI] [PubMed] [Google Scholar]
- 8.Baron D, Mayo A, Kluger Y. Gemcitabine-induced chronic systemic capillary leak syndrome: a life-threatening disease. Clin Oncol (R Coll Radiol) 2006;18(1):90–91. doi: 10.1016/j.clon.2005.09.003. [DOI] [PubMed] [Google Scholar]
- 9.Xie Z, Chan E, Yin Y, Ghosh CC, Wisch L, Nelson C, et al. Inflammatory markers of the systemic capillary leak syndrome (Clarkson Disease) J Clin Cell Immunol. 2014;5:1000213. doi: 10.4172/2155-9899.1000213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Then C, Ritzel K, Seibold C, Mann JF, Reincke M. Multiglandular hormone deficiency in a patient with systemic capillary leak syndrome. Case Rep Med. 2015;2015:958283. doi: 10.1155/2015/958283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dowden AM, Rullo OJ, Aziz N, Fasano MB, Chatila T, Ballas ZK. Idiopathic systemic capillary leak syndrome: novel therapy for acute attacks. J Allergy Clin Immunol. 2009;124(5):1111–1113. doi: 10.1016/j.jaci.2009.06.043. [DOI] [PubMed] [Google Scholar]
- 12.Gousseff M, Arnaud L, Lambert M, Hot A, Hamidou M, Duhaut P, et al. The systemic capillary leak syndrome: a case series of 28 patients from a European registry. Ann Intern Med. 2011;154(7):464–471. doi: 10.7326/0003-4819-154-7-201104050-00004. [DOI] [PubMed] [Google Scholar]
- 13.Hajare KR, Patil P, Bansode J. Idiopathic systemic capillary leak syndrome. Indian J Crit Care Med. 2018;22(5):369–371. doi: 10.4103/ijccm.IJCCM_464_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lambert M, Launay D, Hachulla E, Morell-Dubois S, Soland V, Queyrel V, et al. High-dose intravenous immunoglobulins dramatically reverse systemic capillary leak syndrome. Crit Care Med. 2008;36(7):2184–2187. doi: 10.1097/CCM.0b013e31817d7c71. [DOI] [PubMed] [Google Scholar]
- 15.de Chambrun PM, Gousseff M, Mauhin W, Lega JC, Lambert M, Riviere S, et al. Intravenous immunoglobulins improve survival in monoclonal gammopathy-associated systemic capillary-leak syndrome. Am J Med. 2017;130(10):1219. doi: 10.1016/j.amjmed.2017.05.023. [DOI] [PubMed] [Google Scholar]
- 16.Pratesi A, Valoti P, Baldasseroni S, Marchionni N, Tarantini F. Sudden cardiac arrest in a 73-year-old woman caused by systemic capillary leak syndrome. Intern Emerg Med. 2016;11(5):719–720. doi: 10.1007/s11739-016-1449-z. [DOI] [PubMed] [Google Scholar]
- 17.Staak JO, Glossmann J-P, Esser JM, Diehl V, Mietz H, Josting A. Thalidomide for systemic capillary leak syndrome. Am J Med. 2003;115(4):332–334. doi: 10.1016/S0002-9343(03)00349-8. [DOI] [PubMed] [Google Scholar]
- 18.Tahirkheli NK, Greipp PR. Treatment of the systemic capillary leak syndrome with terbutaline and theophylline. A case series. Ann Intern Med. 1999;130(11):905–909. doi: 10.7326/0003-4819-130-11-199906010-00015. [DOI] [PubMed] [Google Scholar]
- 19.Yabe H, Yabe M, Koike T, Shimizu T, Morimoto T, Kato S. Rapid improvement of life-threatening capillary leak syndrome after stem cell transplantation by bevacizumab. Blood. 2010;115(13):2723–2724. doi: 10.1182/blood-2009-11-247056. [DOI] [PubMed] [Google Scholar]
- 20.Umbrello M, Gardinali M, Ottolina D, Zanforlin G, Iapichino G. Systemic capillary leak syndrome: is methylene blue the silver bullet? Case Rep Crit Care. 2014;2014:141670. doi: 10.1155/2014/141670. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.