Abstract
Background
The primary goal of this study was to create a frequency map of a series of surgically treated both-column fractures and to explore its implications on surgical management.
Methods
We used a consecutive series of 71 both-column fractures to create 3-dimensional reconstruction images, which were superimposed and oriented to fit a model hemipelvis template by aligning specific pelvis landmarks. Fracture lines were identified and traced to create a fracture map of both-column fractures. Then the possible clinical implications of fracture line map were explored.
Results
Fracture location is closely related to the distribution of fracture line. Of 71 fractures that met the criteria for inclusion, we found the most common pattern demonstrated by coexisting fracture lines. The anterior column was involved by 66% of the fractures extending obliquely from the anterior superior spine to the ischial spine, while 62% of the fractures involved the anterior column extending approximately vertically from the iliac crest to the acetabular roof. Additionally, 39% of the fractures involved the posterior column traversing posterior wall. Furthermore, the high fracture line intensity (n = 65, 92%) formed a Y-shaped pattern, which highlighted the consistency of the patterns.
Conclusions
Surgically treated both-column fractures display very common patterns. The most common pattern is the low anterior column fracture in nearly two thirds of cases, the high anterior column fracture in three fifths of cases and the posterior column fracture with posterior wall involvement in nearly two fifths of cases. These study results may help surgeons to yield insight relevant to surgical approaches, reduction, fixation strategies and even implant design for both-column fractures.
Keywords: Acetabulum, Fracture, Both-column, Mapping, Computed tomography
Background
Both-column fractures typically result from high energy trauma, which are complex injuries with technically demanding fracture patterns. In these fractures, the posterior column is usually detached and displaced, possibly with a posterior wall fracture [1]. A secondary fracture line from the posterior column can detach a fragment of the posterior wall that results in the loss of some articular cartilage [2]. If a posterior wall fracture affects the stability of the hip joint in all positions, surgeons often recommend open reduction and internal fixation of the fragment.
In our clinical practice, we have found that associated both-column fractures are frequently associated with posterior wall fractures. However, when posterior wall fractures affect the clinical outcome of both-column fractures, the best way to manage such injuries has not been clearly defined. Many classification systems for acetabular fractures have been established, which may sometimes differ from clinical data sets of actual fracture patterns. A full understanding of the fracture patterns is helpful to develop appropriate surgical strategies. It has been reported that three-dimensional computed tomography (3DCT) reconstruction technology can better understand the three-dimensional structure of acetabular fractures and be used as a guide for surgical planning [3, 4]. The purpose of this study was to analyze 3DCT data from a cohort of patients with a both-column fractures to create a frequency map by superimposing tracked fracture patterns, and to further explore its significance for surgical treatment.
Methods
Subjects
At our level I trauma center, a search in the administrative database showed three hundred and seventy two patients with acetabular or pelvic fractures were admitted into the trauma department from January 2009 to January 2018. Inclusion criteria were (1) age of 18 years or older, (2) acute both-column fracture, (3) complete radiographic assessment including X-ray and CT scan. Exclusion criteria included: (1) anatomical details obscured by artifacts, (2) severe comminuted fractures which were difficult to determine fracture lines; (3) poor quality CT data or lack of complete radiographic images. 301 patients were excluded. The remaining 71 patients were analyzed in this study. All radiographs, CT scan and surgical reports were evaluated by two authors to establish the diagnosis.
This study was approved by the Ethics Committee and Institutional Review Board of West China Hospital. All investigations were conducted in conformity with ethical principles of research. The ethics committee waived the need for consent and patients provided verbal consent to participate in the study.
Fracture mapping
Referring to the mapping method that Cole et al. [5] and Armitage et al. [6] described, we modified the fracture mapping methodology [7] and applied a similar method to the study of both-column fractures. The digitally imaged files (DICOM) were loaded into 3D Slicer (version 4.7.0; Boston, MA, USA), in which three-dimensional computed tomography reconstructions of hemipelvis were created through proper cropping and rotation. Selection of a 3DCT view was based on sufficient evaluation of all images available. These views that allowed the best visualization of the fracture line in the plane (mainly the back of the acetabular posterior column) represented by the standard hemipelvis were collected for each patient. All CT scans for 3D reconstruction had a slide thickness between 0.62 mm and 1.25 mm.
Then these views were imported into Macromedia Fireworks MX software (Macromedia Inc., San Francisco, CA, USA) to overlap and orient fracture patterns onto a template hemipelvis image. Proper rotation and normalization were guided by aligning specific pelvic landmarks: greater sciatic notch, ischial spine and ischial tuberosity. Once proper anatomical alignment was obtained, fracture lines were identified and were traced on the back of the pelvis (Fig. 1). At the process, lines of each hemipelvis case were graphically superimposed to create a compilation of fracture lines on a standard template of an intact left hemipelvis as a representation of the osseous anatomy. The overlap of all major fracture lines resulted in the creation of a both-column fracture map on the rear surface of the pelvis (Fig. 2b). For back views of right hemipelvis, the images were flipped horizontally to obtain corresponding mirror images. Also, the variability in the size and shape of posterior column was standardized with a 4 × 4 cells grid oriented to the posterior border of the posterior column (greater sciatic notch). All mapping was performed under the guidance of a single resident with a background in computer graphics, and all fracture line interpretations were verified by a trauma fellow and a fellowship-trained trauma surgeon.
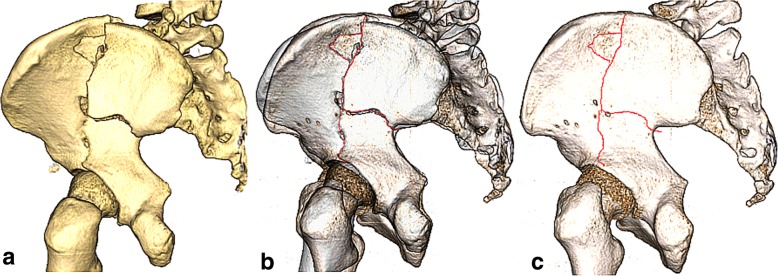
Fig. 1.
A series of images showing the progression of the mapping of the fractures, starting with (a) a computed tomography image, (b) fracture line drawn onto the matched standard template, and (c) ending with fracture line mapped on the standard template
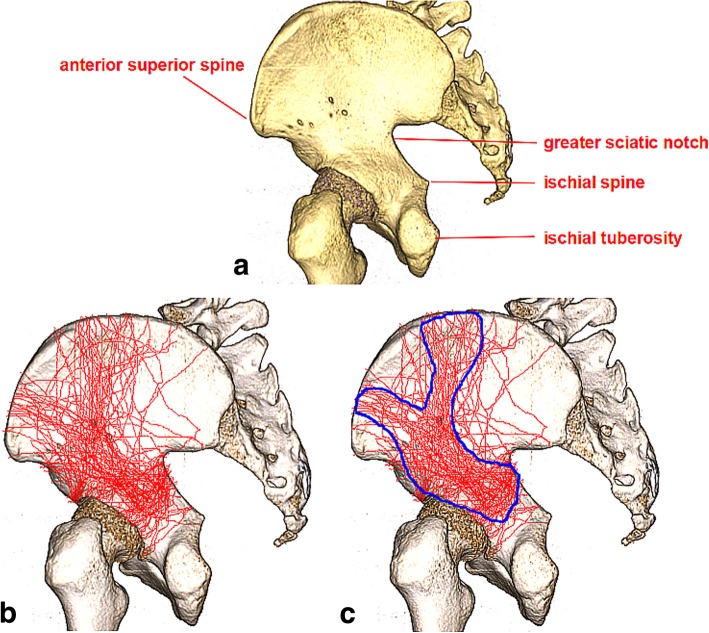
Fig. 2.
a Hemipelvis anatomy. b This picture shows the fracture lines of all 71 superimposed fractures. c This picture illustrates the “corridors” in which nearly 92 % of the major fracture lines occurred
In addition, zones were defined on the basis of pelvic anatomy and/or key muscular origins and insertions (Fig. 2a). Based on the definitions of relevant zones, all fractures were analyzed with respect to acetabular involvement. With qualitative and quantitative assessment of fracture map, the direction of the fracture line was further determined.
Radiographic evaluation and data analysis
Quality of reduction was estimated on anteroposterior (AP) pelvis and Judet views that taken immediately after surgery by Matta’s criteria [8]: anatomical (0–1 mm displacement), imperfect (2–3 mm displacement), and poor (> 3 mm displacement) results. The analysis of the fracture maps was descriptive. Patient characteristics were summarized with frequencies and percentages for categorical variables and with means and standard deviations for continuous variables. The fracture maps were assessed for recurrent patterns of fracture lines and zones of comminution.
Results
A total of 71 patients met the inclusion criteria, among which were 43 male patients and 28 female patients, with an average age of 41 years. All patients underwent surgery. The most common injury mechanism was fall from height (Table 1). Most both-column fractures (56%) were managed through combined Ilioinguinal and Kocher-Langenbeck (IL + KL) approaches in our study. According to the reduction categories described by Matta, we achieved anatomical reduction in 45 patients (63%), imperfect reduction in fourteen (20%), and poor reduction in twelve (17%). All data were detailed in Tables 2.
Table 1.
Patient demographics
| Variable | All patients (n = 71) |
|---|---|
| Mean age (SD),year | 41 (14) |
| Sex, n (%) | |
| Male | 43 (61) |
| Female | 28 (39) |
| Side of injury, n (%) | |
| Right | 36 (51) |
| Left | 35 (49) |
| Injury mechanism, n (%) | |
| Motor vehicle collision | 26 (37) |
| Fall from height | 42 (59) |
| others | 3 (4) |
| Total | 71 (100) |
Table 2.
Surgical approaches and reduction quality
| Variable | Results |
|---|---|
| Surgical approaches, n (%) | |
| IL | 8 (11) |
| KL | 10 (14) |
| P | 3 (4) |
| S | 3 (4) |
| IL + KL | 40 (56) |
| S + KL | 4 (6) |
| S + IF | 2 (3) |
| S + IF+KL | 1 (2) |
| Reduction status, n (%) | |
| Anatomical | 45 (63) |
| Imperfect | 14 (20) |
| Poor | 12 (17) |
IL Ilioinguinal, KL Kocher-Langenbeck, P Pararectus, S Stoppa, IL + KL Ilioinguinal and Kocher-Langenbeck, S + KL Stoppa and Kocher-Langenbeck, S + IF Stoppa and Iliac Fossa, S + IF+KL Stoppa and Iliac Fossa combined with Kocher-Langenbeck
Consistent fracture lines were identified and deemed major fracture lines by critically reviewing all these images. Clearly, most of major fracture lines entered in three directions as if to replicate a Y-shaped pattern (Fig. 2c). Three corridors, making up the “Y”, can be created to reflect the location of nearly 92 % of all major fracture lines, which further highlighted the consistency of the pattern.
From Fig. 2b, we were able to find the main fracture lines of both-column fractures. For the convenience of understanding, the fracture line from the point (near the anterior superior spine) between the anterior superior spine and the iliac tuberosity towards the ischial spine was defined as A, that from the iliac crest to the acetabular roof was defined as B, that traversed posterior wall was defined as C (Fig. 3). A and B constituted the main fracture lines of the anterior column in the both-column fractures, while C constituted the main fracture line of the posterior column. Apparently, A can be regarded as low anterior column fracture, while B can be regarded as high anterior column fracture. At the same time, we also found a part of the fractures from the lower part of the anterior superior spine into the anterior column, which can also be considered as low anterior column fractures (Fig. 2b).
Fig. 3.
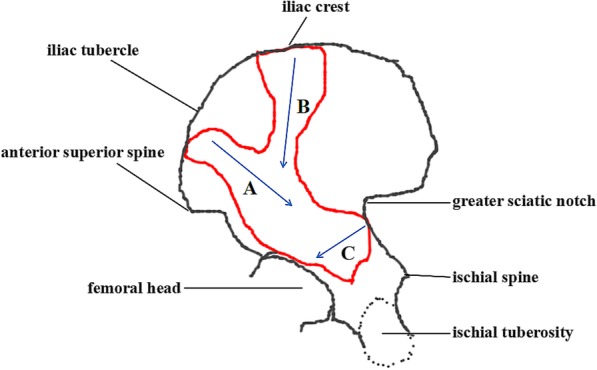
This image shows the area with high incidence of fractures (red line area) and main fracture lines (blue arrow marked with A, B and C)
According to the above definition, we found that of seventy one both-column fractures, forty four cases (62%) had high anterior column fractures, 47 cases (66%) had low anterior column fractures, twenty-eight cases (39%) had posterior column fractures involving the posterior wall (Fig. 4), and forty-two cases (59%) had posterior column fractures without posterior wall involvement. One case had posterior column fracture involving the sacroiliac joint. In addition, it should be noted that multiple major fracture lines can occur in the same case.
Fig. 4.
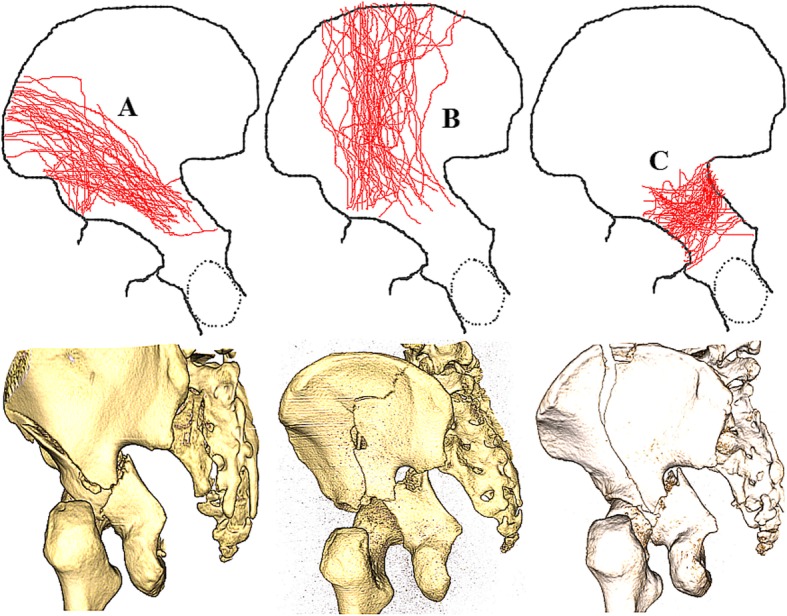
Maps of three major fracture lines marked with a, b and c. Representative three-dimensional computed tomography images of each group are presented for illustrative purposes
Discussion
Both-column fractures, characterised by lines developing on multiple planes, are the most complex of all acetabular fractures [9–13]. The detachment of the entire weight-bearing articular surface from the sacroiliac joint is truly pathognomonic of this injury [9–11]. This injury is often caused by lateral direct impact, which is accompanied by central dislocation of the femoral head. In the treatment of such fracture, the specific injury of the acetabular wall, especially the posterior wall, must be defined, as it can affect the surgical approach and prognosis. In addition, we should also consider secondary congruence that might have impact on the indication for surgery. This state would allow hip joint contact stresses to be evenly distributed throughout the articular surfaces. The long-term results after nonoperative management of both-column fractures is better than other fracture patterns that affect the weight-bearing surface of the acetabulum [14–16].
There are various classification schemes for acetabular fractures [14, 17–22], but the Judet-Letournel classification system remains the most widely accepted [14, 17]. The both-column fracture maps can also be helpful to better understand the existing classification system. The OTA/AO classification system [18] divides acetabular fractures into three categories (group A, group B and group C), each of which includes three subcategories (1, 2, and 3). Pierannunzii et al. [23] classified both-column fractures into two subcategories (type I and II) based on the fracture line morphology (T- or Y-sharped). In our study, the both-column fractures of fracture line A and C were consistent with C2 and type I, those of fracture line B and C were consistent with C1 and type II, and those of the posterior column fractures involving the sacroiliac joints were consistent with C3. In addition, the fracture maps in this study revealed common fracture patterns in the anterior and posterior columns of both-column. The incidence of low anterior column fracture was slightly higher than that of high anterior column fracture.
The choice of surgical approach depends on a variety of factors that include the type of fracture, the direction of fracture displacement, whether accompanied by posterior wall fracture, the conditions of soft tissue and surgeon’s individual preference. The Ilioinguinal approach has been found to be effective in the management of both-column fractures. The specific procedure is that the anterior column fracture is directly reduced through this approach and the posterior column fracture is indirectly reduced, but the premise is that the posterior column fracture is only an isolated large fragment [2, 15]. A single conventional anterior approach is not a good way to deal with posterior wall fractures when double column fractures are combined with posterior wall fractures. Surgical indications for fixation of posterior wall fractures include hip instability, marginal impaction of the articular surface, and intra-articular fragments [24]. Because of the involvement of the posterior wall, some authors recommend the simultaneous addition of Kocher-Langenbeck approach or two-staged procedures for both-column fractures [25, 26]. However, extensile approaches have been reported to be associated with higher rates of complications [25–28]. To optimize treatment and reduce complications, it has been necessary to use limited exposures and understand the common fracture patterns in both-column fractures. Our understanding is that low anterior column fracture (fracture line A in the study) can be reduced and fixed through Stoppa approach, while high anterior column fracture (fracture line B in the study) can be treated through Ilioinguinal approach or combined Stoppa and iliac fossa approach (Fig. 5).
Fig. 5.
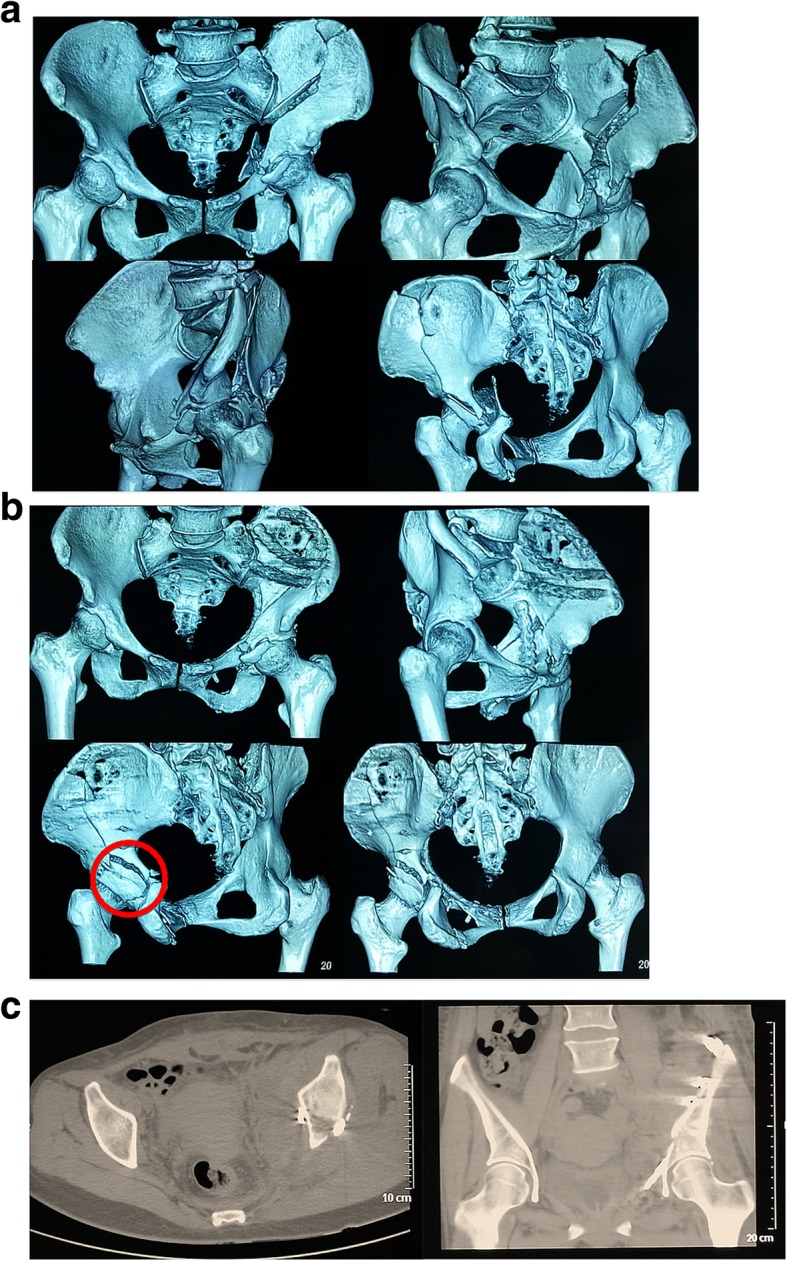
Images for a 45-year-old patient due to a traffic accident. a Preoperative computed tomography scans showed a both-column acetabular fracture including high anterior column fracture (fracture line B in the study) and posterior column fracture (fracture line C in the study). b high anterior column fracture (fracture line B in the study) was treated through the Stoppa and iliac fossa approach and sequential Kocher-Langenbeck approach was added because of the displaced posterior-wall fragment (red circle). c Postoperative coronal and axial CT scans at the level of the acetabular dome presenting anatomic reduction
In this study, we identified a Y-shape region with a high incidence of comminution composed of three major fracture lines; these included (1) the fracture line from the point near the anterior superior spine towards the ischial spine, (2) that from the iliac crest to the acetabular roof, and (3) that traversed posterior wall. Furthermore, in the cases of both-column fractures we studied, posterior wall fractures tended to be concomitant. The most common pattern was a fracture line traversing posterior wall.
These results can facilitate the identification of critical locations at which to access displaced fractures. Surgeons can apply our study results to guide the placement of implants for optimal screw purchase and internal fixation. Additionally, we can also combine anatomical parameters of the pelvis with the main fracture lines to design a novel internal fixation device, which is the focus of further research in the future.
Our study has several limitations. First, it was a retrospective review of prospectively gathered data for a small number of patients. Second, our analysis did not take potential variability in anatomy and injury mechanism into account. Third, some hemipelvis images did not match the hemipelvis model perfectly. Finally, fracture lines drawn on the hemipelvis model could slightly differ from true fracture morphology.
Conclusions
In conclusion, the fracture maps of both-column fractures derived from 3D CT can aid in guiding the treatment of such complex fractures, in terms of surgical approaches, preoperative planning, and implant strategy.
Acknowledgements
Not applicable.
Funding
Not applicable.
Availability of data and materials
This article only includes summarized data from this study. Anonymized datasets (CT) are available from the corresponding author on reasonable request.
Abbreviations
- 3DCT
Three-dimensional computed tomography
- AP
Anteroposterior
- CT
Computed Tomography
- DICOM
Digital Imaging and Communications in Medicine
- IL
Ilioinguinal
- KL
Kocher-Langenbeck
Authors’ contributions
YY designed this study and analyzed the data and was a major contributor in writing and revising. ZC was a major contributor in conception and design and revising. FY was a major contributor in conception and design and revising it critically. YY made contributions in data collecting and drafting. All authors read and approved the final manuscript.
Ethics approval and consent to participate
Before the study began, we had carefully consulted the Ethics Committee and Institutional Review Board of West China Hospital. They suggested that this study did not involve special interventions for patients and we should conduct this study in compliance with the Helsinki Declaration and Inform patients fully of the purpose of the study. So, all data was fully anonymised at-source with researchers having access to fully anonymised data only. Given the anonymous nature of the data, the ethics committee waived any requirement for patient informed consent. Nevertheless, patients were informed of the purpose of the study at the start of the study, and all patients were willing to participate in the study and agreed verbally.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Yun Yang, Email: xgz123yy@163.com.
Chang Zou, Email: ciciboylove@163.com.
Yue Fang, Email: fangyue1968@163.com.
References
- 1.Tile M. Describing the injury: classification of acetabular fractures. In: Tile M, Helfet D, Kellam J, editors. Fractures of the pelvis and acetabulum. 3. Baltimore, MD: Lippincott Williams & Wilkins; 2003. pp. 427–475. [Google Scholar]
- 2.Larson CB. Fracture dislocations of the hip. Clin Orthop Relat Res. 1973;92:147–154. doi: 10.1097/00003086-197305000-00013. [DOI] [PubMed] [Google Scholar]
- 3.Scott WJ, Fishman EK, Magid D. Acetabular fractures: optimal imaging. Radiology. 1987;165(2):537–539. doi: 10.1148/radiology.165.2.3659379. [DOI] [PubMed] [Google Scholar]
- 4.Garrett J, Halvorson J, Carroll E, Webb LX. Value of 3-D CT in classifying acetabular fractures during orthopedic residency training. Orthopedics. 2012;35(5):e615–e620. doi: 10.3928/01477447-20120426-12. [DOI] [PubMed] [Google Scholar]
- 5.Cole PA, Mehrle RK, Bhandari M, Zlowodzki M. The pilon map: fracture lines and comminution zones in OTA/AO type 43C3 pilon fractures. J Orthop Trauma. 2013;27(7):e152–e156. doi: 10.1097/BOT.0b013e318288a7e9. [DOI] [PubMed] [Google Scholar]
- 6.Armitage BM, Wijdicks CA, Tarkin IS, Schroder LK, Marek DJ, Zlowodzki M, et al. Mapping of scapular fractures with three-dimensional computed tomography. J Bone Joint Surg Am. 2009;91(9):2222–2228. doi: 10.2106/JBJS.H.00881. [DOI] [PubMed] [Google Scholar]
- 7.Yang Y, Yi M, Zou C, Yan ZK, Yan XA, Fang Y. Mapping of 238 quadrilateral plate fractures with three-dimensional computed tomography. Injury. 2018;49(7):1307–1312. doi: 10.1016/j.injury.2018.05.026. [DOI] [PubMed] [Google Scholar]
- 8.Matta JM. Operative treatment of acetabular fractures through the ilioinguinal approach: a 10-year perspective. J Orthop Trauma. 1994;20(Suppl 1):S20–S29. [PubMed] [Google Scholar]
- 9.Chen KN, Wang G, Cao LG, Zhang MC. Differences of percutaneous retrograde screw fixation of anterior column acetabular fractures between male and female: a study of 164 virtual three-dimensional models. Injury. 2009;40(10):1067–1072. doi: 10.1016/j.injury.2009.01.014. [DOI] [PubMed] [Google Scholar]
- 10.Moroni A, Caja VL, Sabato C, Zinghi G. Surgical treatment of both-column fractures by staged combined ilioinguinal and Kocher-Langenbeck approaches. Injury. 1995;26(4):219–224. doi: 10.1016/0020-1383(95)00007-V. [DOI] [PubMed] [Google Scholar]
- 11.Giannoudis PV, Grotz MR, Papakostidis C, Dinopoulos H. Operative treatment of displaced fractures of the acetabulum. A meta-analysis J Bone Joint Surg Br. 2005;87(1):2–9. doi: 10.1302/0301-620X.87B1.15605. [DOI] [PubMed] [Google Scholar]
- 12.Giannoudis PV, Tzioupis CC, Pape HC, Roberts CS. Percutaneous fixation of the pelvic ring: an update. J Bone Joint Surg Br. 2007;89(2):145–154. doi: 10.1302/0301-620X.89B2.18551. [DOI] [PubMed] [Google Scholar]
- 13.Chuckpaiwong B, Suwanwong P, Harnroongroj T. Roof-arc angle and weightbearing area of the acetabulum. Injury. 2009;40(10):1064–1066. doi: 10.1016/j.injury.2009.01.016. [DOI] [PubMed] [Google Scholar]
- 14.Letournel E. Acetabulum fractures: classification and management. Clin Orthop Relat Res. 1980;(151):81–106. [PubMed]
- 15.Letournel E, Judet R. Fractures of the acetabulum. 2. New York: Springer-Verlag; 1993. [Google Scholar]
- 16.Tornetta P., III Nonoperative management of acetabular fractures: the use of dynamic stress views. J Bone Joint Surg Br. 1999;81(1):67–70. doi: 10.1302/0301-620X.81B1.8805. [DOI] [PubMed] [Google Scholar]
- 17.Judet R, Judet J, Letournel E. Fractures of the acetabulum: classification and surgical approaches for open reduction. Preliminary Report J Bone Joint Surg Am. 1964;46:1615–1646. doi: 10.2106/00004623-196446080-00001. [DOI] [PubMed] [Google Scholar]
- 18.Marsh JL, Slongo TF, Agel J, Broderick JS, Creevey W, DeCoster TA, et al. Fracture and dislocation classification compendium-2007: Orthopaedic trauma association classification, database and outcomes committee. J Orthop Trauma. 2007;21(suppl 10):S1–S133. doi: 10.1097/00005131-200711101-00001. [DOI] [PubMed] [Google Scholar]
- 19.Harris JH, Jr, Lee JS, Coupe KJ, Trotscher T. Acetabular fractures revisited: part 1, redefinition of the Letournel anterior column. AJR Am J Roentgenol. 2004;182(6):1363–1366. doi: 10.2214/ajr.182.6.1821363. [DOI] [PubMed] [Google Scholar]
- 20.Harris JH, Jr, Coupe KJ, Lee JS, Trotscher T. Acetabular fractures revisited: part 2, a new CT-based classification. AJR Am J Roentgenol. 2004;182(6):1367–1375. doi: 10.2214/ajr.182.6.1821367. [DOI] [PubMed] [Google Scholar]
- 21.Durkee NJ, Jacobson J, Jamadar D, Karunakar MA, Morag Y, Hayes C. Classification of common acetabular fractures: radiographic and CT appearances. AJR Am J Roentgenol. 2006;187(4):915–925. doi: 10.2214/AJR.05.1269. [DOI] [PubMed] [Google Scholar]
- 22.Scheinfeld MH, Dym AA, Spektor M, Avery LL, Dym RJ, Amanatullah DF. Acetabular fractures: what radiologists should know and how 3D CT can aid classification. Radiographics. 2015;35(2):555–577. doi: 10.1148/rg.352140098. [DOI] [PubMed] [Google Scholar]
- 23.Pierannunzii L, Fischer F, Tagliabue L, Calori GM, d'Imporzano M. Acetabular both-column fractures: essentials of operative management. Injury. 2010;41(11):1145–1149. doi: 10.1016/j.injury.2010.08.011. [DOI] [PubMed] [Google Scholar]
- 24.Olson SA, Matta JM. Fractures of the acetabulum, hip dislocations, and femoral head fractures. In: Chapman MW, editor. Chapman’s orthopaedic surgery. 3rd ed. Philadelphia: Lippincott Williams & Wikins; 2001. p. 587–616.
- 25.Harris AM, Althausen P, Kellam JF, Bosse MJ. Simultaneous anterior and posterior approaches for complex acetabular fractures. J Orthop Trauma. 2008;22:494–497. doi: 10.1097/BOT.0b013e3181830d2a. [DOI] [PubMed] [Google Scholar]
- 26.Guerado E, Cano JR, Cruz E. Simultaneous ilioinguinal and Kocher-Langenbeck approaches for the treatment of complex acetabular fractures. Hip Int. 2010;20(Suppl 7):S2–S10. doi: 10.1177/11207000100200s702. [DOI] [PubMed] [Google Scholar]
- 27.Routt ML, Jr, Swiontkowski MF. Operative treatment of complex acetabular fractures. Combined anterior and posterior exposures during the same procedure. J Bone Joint Surg Am. 1990;72(6):897–904. doi: 10.2106/00004623-199072060-00016. [DOI] [PubMed] [Google Scholar]
- 28.Min BW, Lee KJ, Jung JW, Kim GW, Song KS, Bae KC, et al. Outcomes are equivalent for two-column acetabular fractures either with or without posterior-wall fractures. Arch Orthop Trauma Surg. 2018;138:1223–1234. doi: 10.1007/s00402-018-2953-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
This article only includes summarized data from this study. Anonymized datasets (CT) are available from the corresponding author on reasonable request.