Abstract
Objective:
The present study assessed whether adding a telephone care management protocol to usual aftercare improved the outcomes of veterans in the year after they discharged from residential treatment for posttraumatic stress disorder (PTSD).
Method:
In a multisite randomized controlled trial, 837 veterans entering residential PTSD treatment were assigned to receive either standard outpatient aftercare (n = 425) or standard aftercare plus biweekly telephone monitoring and support in the first 3 months after discharge (n = 412). PTSD, violence, substance use, depression, and quality of life were assessed using self-report questionnaires at intake, discharge, and 4 month and 12 months post-discharge. Treatment utilization was determined from VA administrative data.
Results:
Telephone case monitors reached 86% of intervention participants (n = 355), providing an average 4.5 out of 6 planned telephone calls. Participants in the telephone care and control conditions showed similar outcomes on all clinical measures. Time to rehospitalization did not differ by condition. In contrast with prior studies reporting poor treatment attendance in this population, participants in both arms of this study completed a mental health visit an average of once every 10 days in the year after discharge. Many participants had continuing problems despite high utilization of outpatient care.
Conclusions:
Telephone care management had little incremental value in a context where patients were already high utilizers of mental health services. Telephone care management could potentially be beneficial in other settings where patients experience greater barriers to engaging with outpatient mental health care after discharge from inpatient treatment.
Keywords: Stress disorders, post-traumatic, veterans, patient compliance, telemedicine, patient care management
Helping patients maintain functioning after discharge from inpatient care presents a continuing challenge (1–4). The U.S. Department of Veterans Affairs (VA) provides its most intensive treatment for posttraumatic stress disorder (PTSD) in residential rehabilitation programs (5). The structure of these programs varies, but most combine pharmacotherapy, psychotherapy to teach coping skills, and opportunities to practice these skills in a therapeutic milieu. Some programs also offer evidence-based psychotherapies such as cognitive processing therapy or EMDR for patients who are deemed appropriate candidates. Average length of stay varies by program from 15 to 90 days (5). Veterans treated in residential PTSD programs often have co-occurring problems including depression, anger, and interpersonal difficulties (6,7). Most have prior histories of substance misuse, although veterans are often required to be abstinent from substances when they enter residential PTSD treatment (8,9).
Several studies in the 1990s challenged the effectiveness of lengthy inpatient treatment programs for PTSD and questioned whether gains were adequately maintained after discharge (10,11). Many veterans continue to have difficulties after discharge from residential treatment. In one program, 12% of patients relapsed to heavy drinking, 9% relapsed to illicit drug use, and 48% reported aggressive behavior within four months of discharge (11). Other studies reported that 10% of veterans who discharged from residential PTSD treatment programs were rehospitalized within four months and 21% were rehospitalized within a year (1,12).
Improving veterans’ outpatient treatment attendance and medication compliance after discharge from intensive PTSD treatment could potentially enhance their functioning and reduce rehospitalization. Dropout from outpatient mental health treatment is a common problem in the general population (13,14) and among veterans (15,16). Previous reports indicated that over one-quarter of veterans discharging from VA residential PTSD treatment programs did not complete an outpatient treatment visit in the first 30 days after discharge (1,17). Poor compliance with medications might also contribute to poor outcomes (18,19). One study found that only one-third of veterans who were prescribed antidepressants during residential PTSD treatment consistently refilled them after discharge (10).
Prior studies in patients with psychiatric disorders have shown that monitoring and support via telephone can improve rates of initial entry into MH treatment (20,21), enhance medication compliance (19,22), and reduce rehospitalization (23). Telephone-based care management has been shown to improve depression and alcohol outcomes for patients treated in primary care (24–26). Telephone-based continuing care has reduced relapse to substance use after discharge from intensive addiction treatment (27,28). A quasi-experimental pilot study confirmed that providing three months of biweekly telephone support to veterans after discharge from residential PTSD treatment was feasible, acceptable to patients, and reduced time from discharge to completion of a first outpatient visit (17).
The present study tested whether augmenting usual aftercare with biweekly telephone monitoring and support would improve veterans’ outcomes after discharge from residential PTSD treatment. Our primary hypotheses were that veterans randomized to the telephone care condition would have less severe PTSD symptoms, less aggressive behavior and fewer alcohol and drug use problems at 4 and 12 months post-discharge than would those receiving treatment as usual (TAU). Our secondary hypotheses were that participants getting telephone care would have longer time to re-hospitalization, less depression, and better quality of life at 4 and 12 months post-discharge than would those getting TAU.
The tertiary goal of the study was to assess whether the clinical effects of telephone case monitoring were mediated by improved engagement in outpatient care. We expected that participants in the telephone case monitoring condition would have fewer days between discharge and attending a first outpatient mental health appointment, would complete more mental health visits in the year after discharge, and would have higher medication possession ratios (i.e., more days with completed refills of antidepressants) than those getting TAU. We further anticipated that improved treatment engagement would mediate observed differences in outcomes between study conditions. Additional exploratory analyses examined whether the effects of telephone care management were moderated by risk factors for poor treatment engagement identified in prior studies (29,30). We anticipated intervention effects would be strongest among patients who previously had fewer treatment visits, lived further away from care, had lower therapeutic alliance with their outpatient provider, and/or who had lower treatment expectancies.
Method
Study procedures were overseen by institutional review boards at each study site. All participants gave written consent to participate.
Subjects
A total of 837 veterans were recruited from consecutive admissions to five VA residential PTSD treatment programs within two weeks of admission. Participants’ length of stay in these programs ranged from 15 to 149 days. Median length of stay varied by program from 26 to 64 days. Patients were excluded if cognitive impairment precluded their giving informed consent, if they discharged from treatment in less than 15 days, or if they transferred from residential treatment directly to another inpatient treatment program. Active duty military personnel were excluded because they receive their aftercare outside the VA system.
Measures
Participants completed self-report measures of their functioning at intake, at discharge from residential treatment (PTSD and depression only), and roughly four months and 12 months after discharge. Aggressive behavior was assessed using a six-item index (range 0 to 6) adapted from the Conflict Tactics Scale (31), which expands on a four-item index widely used with VA patients (7,9). Alcohol and drug use problems were assessed with the composite scores from the self-report version of the Addiction Severity Index (ASI; 32,33). PTSD symptoms were assessed with the PTSD Checklist (PCL; 34). Depression symptoms were evaluated with the Center for Epidemiological Studies Scale (CES-D; 35). Subjective quality of life was assessed with a scale developed for the Veterans Affairs Military Stress Treatment Assessment study (36).
Re-hospitalizations in a psychiatric or substance use bed section and mental health and substance use outpatient treatment visits in the year after discharge were determined from the National Patient Care Database. For patients prescribed antidepressants, medication possession ratios (days supply of medications divided by total days) were determined from the National Data Extracts for Pharmacy Database following procedures used by Lockwood et al. (12)
Mental health and substance abuse treatments visits in the prior year and distance from patients’ homes to the nearest VA clinic or Vet Center were determined from VA administrative data. Therapeutic alliance with participants’ main outpatient mental health provider was determined using the short version (WAI-S) of the patient form of the Working Alliance Inventory (WAI; 37). Treatment expectancies were assessed using a procedure developed by Battle and colleagues (38).
Procedure
Participants were recruited between October 2006 and December 2009 from all subsequent admissions to five residential treatment programs for PTSD. Participants were recruited within two weeks of admission to residential treatment. Referring clinicians invited patients to meet with a research assistant who then explained the study and obtained consent. Of 1,025 eligible subjects, 837 (82%) agreed to participate. Randomization was done centrally by someone blind to participants’ treatment histories, using Efron randomization (39) stratified within site, gender, and whether participants had served in the recent wars in Iraq or Afghanistan. Baseline data were collected when patients were consented into the study. Discharge self-report measures were collected in the 14 days prior to discharge or by mail shortly after discharge. Surveys at four and 12 months post-discharge were obtained by mail with mail and telephone follow-up using the Dillman method (40).
Treatment
Participants in the treatment as usual arm received standard referral to their outpatient counselors and/or psychiatrists. Participants in the telephone care management arm received standard referrals plus biweekly telephone monitoring and support during their first 3 months after discharge. The telephone monitoring intervention was delivered from a centralized call center by twelve clinical psychology graduate students supervised by four clinical psychologists. Telephone monitors normally contacted patients every two weeks. If participants were unavailable on the first call attempt, the telephone monitor left a message and toll-free call-back number, and made two additional contact attempts on different days of the week at different times of day. After three unsuccessful call attempts, participants were not re-contacted until their next scheduled call. If the given phone number was no longer in service or the participant was no longer at that number, we obtained the participants’ new telephone number from a family member or friend whom the participant had provided as a contact.
When monitors reached the participant, they followed a scripted protocol to briefly assess the participants’ outpatient treatment attendance, medication compliance, symptom severity and coping (PTSD, depression, anger, and coping each assessed on 1–10 Likert scale), substance use, suicidality, and risk for violence (17). Participants were verbally reinforced for positive behaviors. Participants who had a problem in any given area would get interventions to address that issue, including problem-solving support or brief motivation enhancement. For example, if participants reported becoming verbally aggressive, the monitor asked them whether this had caused any problems (negative consequences) and whether they were satisfied with how they had handled their anger. If participants were satisfied, the monitor briefly reiterated the negative consequences mentioned by the participants and moved on. If participants felt they handled the argument badly, the monitor asked the participant to generate some alternative things they could have done and encouraged them to discuss this concern with their outpatient provider. If participants were at risk of harming themselves or others, monitors immediately alerted their supervisor and the participants’ outpatient provider.
Statistical Analysis
Analyses were conducted on an intent-to-treat basis, using multiple imputation to address potential bias introduced by missing data (41,42). All analyses were conducted using R version 2.9.2 (43) and multiple imputations were completed with the R MICE library (44). Our sample size provided 90% power to detect small (d = .20) effects of condition on outcomes. To address our primary and secondary hypotheses , we assessed the effect of condition on clinical outcomes at 4 and 12 months post-discharge using regression models that included the effects of condition, site, and condition x site, while controlling for baseline scores on the outcome measure and time from intake to 4-month follow-up. Analyses of PTSD and depression outcomes controlled for scores at both intake to (baseline 1) and discharge from residential treatment (baseline 2). Analyses for all other outcomes included only the intake baseline as a covariate. The effects of condition on time to rehospitalization was assessed using Cox regression including the effects of condition, site, and condition x site.
To address our tertiary hypotheses, time to first outpatient visit was assessed using the same Cox regression model as for rehospitalization. Regression models were used to test the effects of condition, site, and condition x site on (log-transformed) number of mental health treatment visits completed in the year after discharge and medication possession ratios. Additional meditational analyses would be conducted if there were significant differences by condition in both outcomes and treatment engagement. Exploratory regression analyses tested whether there were significant interactions between each of our five moderators and treatment condition in predicting violence, alcohol problems and drug problems at four months post-discharge, antidepressant medication possession ratios, and mental health/addiction treatment visits in the year after discharge.
Results
Characteristics of study participants are shown in Table 1. There were no significant differences in demographic or baseline clinical characteristics of participants in the two treatment conditions. Participants’ progression through the study is depicted in Figure 1. Of 925 consented participants, 6 dropped out prior to randomization and 82 were disenrolled because they discharged within 14 days or discharged directly to another inpatient program. The remaining 837 participants were randomized to intervention (n = 412) or control (n = 425) conditions.
Table 1:
Participant Characteristics by Treatment Condition
| Telephone Care (n = 408 to 412) |
TAU Control (n = 417 to 425) |
|||||
|---|---|---|---|---|---|---|
| n | % | n | % | Chi- square |
df | |
| Female (n = 837) | 357 | 13.3 | 368 | 13.4 | 0.00 | 1 |
| OEF/OIF veteran (n = 837) | 114 | 27.7 | 114 | 26.8 | 0.08 | 1 |
| Marital status (n = 818) | 2.09 | 3 | ||||
| Married | 167 | 41.3 | 186 | 44.9 | ||
| Divorced/separated | 167 | 41.3 | 153 | 37.0 | ||
| Widowed | 12 | 23.0 | 10 | 2.4 | ||
| Never married | 58 | 14.4 | 65 | 15.7 | ||
| Race/Ethnicity (n = 819) | 4.54 | 7 | ||||
| Caucasian | 263 | 64.8 | 256 | 62.0 | ||
| African-American | 87 | 21.4 | 93 | 22.5 | ||
| Asian-American | 2 | 0.5 | 0 | 0.0 | ||
| Native American | 11 | 2.7 | 8 | 1.9 | ||
| Pacific Islander | 2 | 0.5 | 2 | 0.5 | ||
| Latino ethnicity | 19 | 4.7 | 26 | 6.3 | ||
| Other | 22 | 5.4 | 28 | 6.8 | ||
| Co-occurring diagnoses (n = 837) | ||||||
| Depression | 328 | 79.6 | 349 | 82.1 | 0.85 | |
| Anxiety (other than PTSD) | 123 | 29.9 | 135 | 31.8 | 0.36 | 1 |
| Substance use disorder | 224 | 54.4 | 240 | 56.5 | 0.37 | 1 |
| Schizophrenia | 20 | 4.9 | 18 | 4.2 | 0.18 | 1 |
| Bipolar disorder | 49 | 11.9 | 58 | 13.6 | 0.58 | 1 |
| Service connected disability (n = 837) | 285 | 69.2 | 282 | 66.4 | 0.50 | 1 |
| Mean | SE | Mean | SE | t | df | |
| Age (n = 837) | 50.2 | 0.62 | 49.9 | 0.86 | 0.53 | 835 |
| Working alliance (n = 825) | 63.9 | 0.73 | 64.5 | 1.1 | −0.40 | 823 |
| Treatment expectancies (n = 825) | 3.2 | 0.1 | 3.1 | 0.1 | 0.62 | 823 |
| Length of stay in residential program (n = 837) | 47.0 | 1.2 | 45.9 | 1.7 | 0.63 | 835 |
| Outpatient MH visits in prior year (n = 829) | 35.0 | 2.1 | 38.6 | 2.9 | −1.24 | 827 |
Note: no significant differences by condition. Working alliance scores ranged from 12 to 84, with higher scores indicating stronger alliance with their outpatient provider. Treatment expectancies scores ranged from −5 to +5, with more positive scores indicating greater expectation that treatment could improve their presenting problems.
Figure 1.
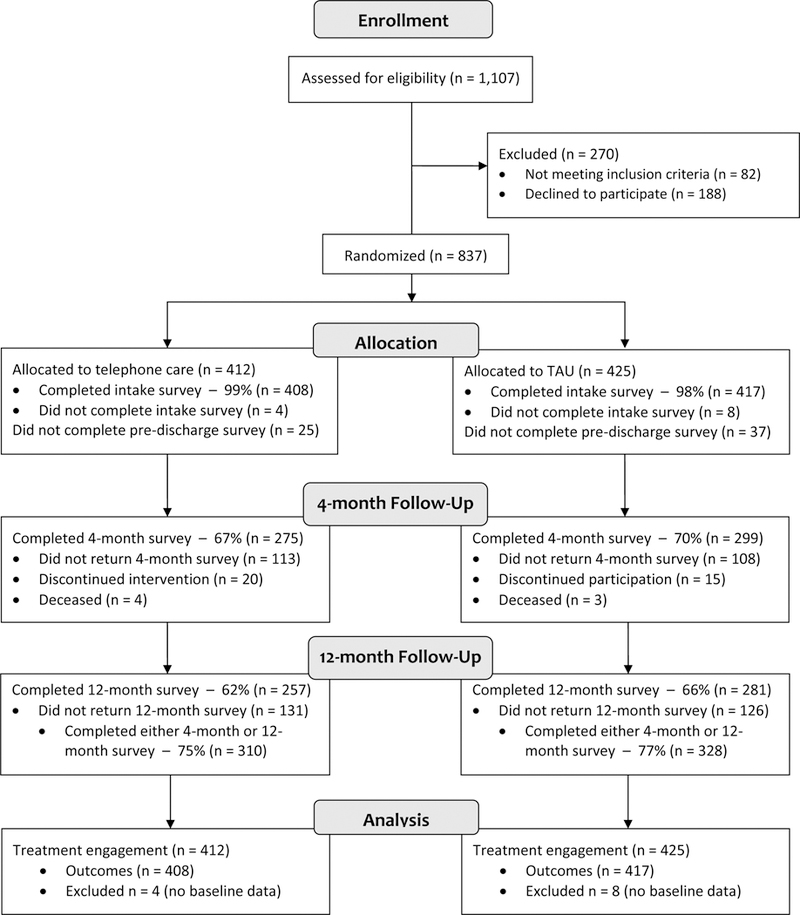
Flow of participants through the trial
Telephone case monitors successfully reached and completed at least one call with 86% of participants (n = 355) in the intervention condition. Patients contacted by phone completed an average of 4.5 +/−1.6 out of 6 planned calls. Call length ranged from 2 to 113 minutes, with an average of 16.4 +/−10.8 minutes. Approximately 16% of all completed calls identified an emergent issue that required phone or email follow up to patients’ outpatient mental health providers. Serious suicidal ideation was reported in 6% of the calls, homicidal ideations in 6% of the calls, and heavy alcohol or drug use was reported in 5% of all calls. Telephone case monitors also informed outpatient mental health providers when participants reported an increase 3 or more points in PTSD, depression, or anger symptoms.
Our study hypotheses are shown graphically in Figure 2. Our primary and secondary hypotheses, that telephone case monitoring would improve clinical outcomes and extend to hospitalization were not supported. There were no differences in aggressive behavior, alcohol problems, or drug problems at either 4 months or 1 year post-discharge between patients randomized to telephone care management and to usual care (see Table 2). PTSD, depression, and subjective quality of life outcomes did not differ by condition. Time to rehospitalization for psychiatric or substance use problems was similar in both conditions, with 11% (n = 46) of intervention and 13% (n = 55) of control participants rehospitalized within a year of discharge.
Figure 2:
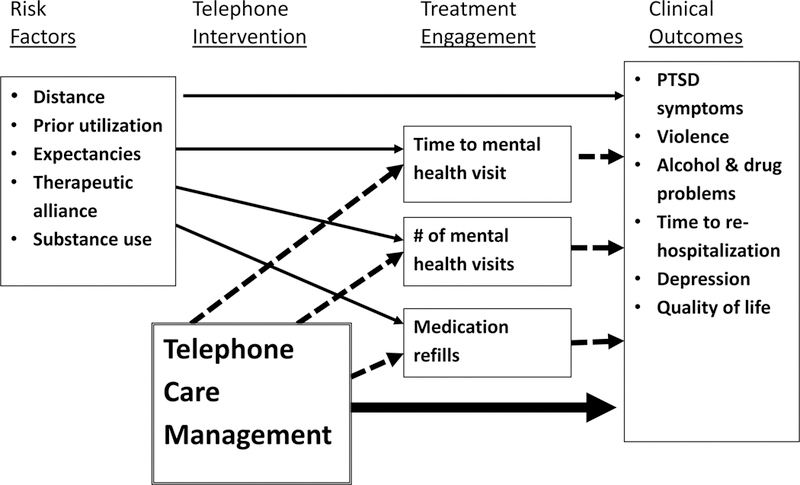
Telephone care management logic model
Table 2.
Clinical Outcomes by Treatment Condition
| Baseline 1 (intake) | Baseline 2 (discharge) | 4 Month Follow Up | 12 Month Follow Up | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Telephone | Control | Telephone | Control | Telephone | Control | ES | Telephone | Control | ES | |||||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | d | Mean | SD | Mean | SD | d | |
| PCL | 67.9 | 11.0 | 67.2 | 11.4 | 60.4 | 14.4 | 59.7 | 14.3 | 63.8 | 12.9 | 63.3 | 12.7 | .04 | 63.9 | 13.0 | 63.4 | 12.5 | .04 |
| CES-D | 41.2 | 9.4 | 40.2 | 9.8 | 31.8 | 11.5 | 32.1 | 11.3 | 37.7 | 10.1 | 37.2 | 10.8 | .06 | 38.0 | 10.1 | 38.4 | 10.4 | −.03 |
| Alcohol | .10 | .14 | .15 | .18 | -- | -- | -- | -- | .15 | .18 | .16 | .18 | -.03 | .15 | .19 | .17 | .19 | −.09 |
| Drugs | .03 | .05 | .03 | .06 | -- | -- | -- | -- | .04 | .07 | .05 | .07 | −.05 | .05 | .09 | .05 | .08 | −.03 |
| Aggression | 3.4 | 2.1 | 3.5 | 2.1 | -- | -- | -- | -- | 2.9 | 2.1 | 3.0 | 2.1 | −.08 | 3.0 | 2.2 | 3.1 | 2.2 | −.05 |
| Quality of life | 3.1 | 1.0 | 3.2 | 1.0 | -- | -- | -- | -- | 3.2 | 1.1 | 3.2 | 1.1 | −.03 | 3.3 | 1.1 | 3.3 | 1.1 | .00 |
Note: Telephone = treatment as usual plus telephone case monitoring. Control = treatment as usual. PCL = PTSD Checklist; scores range from 17 to 85, with higher scores indicating worse symptoms. CES-D = Center for Epidemiological Studies Depression Scale; scores range from 0 to 60, with higher scores indicating more severe depression. ASI Alcohol = Addiction Severity Index alcohol composite score; scores range for 0 to 1, with higher scores indicating more alcohol-related problems. ASI Drug = Addiction Severity Index drug composite score; scores range for 0 to 1, with higher scores indicating more drug-related problems. Aggression = 6-item index of aggression behavior derived from the Conflict Tactics Scale; scores range from 0 to 6, with higher scores indicating more types of aggressive behavior. Quality of Life = 10-item quality of life subscale of the Veterans Affairs Military Stress Treatment Assessment; scores range from 1 to 7 with higher scores indicating greater satisfaction. There were no significant differences by condition in outcomes at either 4-month or 12-month follow-up after controlling for the effects of baseline scores, site, and days from discharge to follow-up.
Our tertiary hypotheses, that our intervention would improve engagement in care were also not supported (see Figure 2). Time to first outpatient visit was similar in both arms, with 86% (n = 354) of intervention participants and 87% (n = 370) of controls completing a mental health visit within 30 days of discharge. Patients in the telephone condition completed an average of 37.8 +/− 46.6 in-person mental health or addiction treatment visits in the year after discharge, similar to the 34.4 +/− 39.9 visits completed by controls. The only difference in utilization was for telephone visits in the first 90 days after discharge (not including those delivered as part of the study): intervention participants had an average of 3.2 +/− 4.1 telephone visits with mental health providers compared to 1.3 +/− 2.8 received by controls, t = 8.0, df 1,831, p < .001. This reflected providers checking on their patients after telephone case monitors informed them that their patient was experiencing problems. Among the 758 participants prescribed antidepressants, mean medication possession ratios were similar for those in the intervention, 0.60 +/− 0.26 and TAU conditions, 0.62 +/− 0.27. Finally, our exploratory analyses showed that the effects of telephone care on clinical outcomes and treatment engagement were not moderated by prior use of mental health care, distance from clinic, therapeutic alliance, treatment expectancies, or substance use problems.
Discussion
Why did telephone care management fail to improve veterans’ outcomes compared to care as usual after discharge from residential treatment? We were able to successfully deliver the intervention. Three-quarters of intervention participants received at least 3 of the 6 intended telephone calls. This is comparable to the number of contacts provided in other successful trials of telephone interventions (21,22). Many patients and their clinicians said that they appreciated the calls and thought they were helpful. Nonetheless, the intervention did not improve patients’ functioning.
Our intervention model was based on the assumption that poor compliance with aftercare contributed to veterans’ problems after discharge (Figure 2). This assumption was incorrect. In contrast with prior reports (1,17), over 85% of participants completed a mental health visit within 30 days of discharge; most were seen within a week of discharge. Rather than having poor treatment attendance, veterans in this study were high utilizers of outpatient care, attending an average of one mental health appointment every 10 days in the year after discharge. In this context, there was little incremental value in providing an additional telephone contact every 14 days.
Our null findings contrast with prior studies in which telephone care management improved outcomes of patients in primary care, addiction, and psychiatric aftercare programs (23,24,26,28). In these studies, patients saw their providers infrequently and telephone care management represented a substantial increase in patient contact. That was not the case in the present study. It is therefore unclear whether telephone support can be an effective tool for improving post-discharge outcomes in other settings where there is limited aftercare (2).
Our treatment utilization findings likely reflect VA efforts to improve continuity of care in the years since our pilot study was conducted. Between fiscal years 2000 and 2009, the proportion of PTSD patients completing an outpatient visit within 30 days after discharge from VA inpatient mental health care rose from 68% to 78% (5,45). During that same period, rates of rehospitalization within six months of discharge from residential PTSD treatment declined from 29% to 24%.
However, continuity of care does not ensure good clinical outcomes (1). Many veterans in the present study had continuing problems despite receiving large doses of residential and outpatient care. There are undoubtedly selection factors, with more chronically impaired individuals being the most likely to be referred for residential PTSD treatment. Over 95% of patient in VA residential treatment either receive or are seeking disability pensions for PTSD (46,47). It has often been suggested that reliance on pension compensation could potentially reduce veterans’ response to PTSD treatment; however there has yet to be strong empirical evidence confirming this contention (47,48).
Our findings also raise questions about whether we are providing the right mix of services for chronic PTSD patients. Not all residential treatment programs, especially those with shorter lengths of stay, included evidence-based psychotherapies that directly target PTSD symptoms. Providing these treatments can enhance patient outcomes (49).
Patients showed little mean improvement in PTSD symptoms between 4-month and 12-month follow-up assessments despite receiving a large dose of aftercare. It is likely that many of these treatment contacts provided case management or supportive care rather than active psychotherapy (50). There may be more efficient and effective ways of providing continuing care. Scheduling frequent in-person appointments to monitor patient safety may be less necessary now that the VA has a 24-hour crisis counseling hotline. Some supportive services currently delivered during clinic visits could be provided via brief telephone contacts, peer-led support groups, or internet or mobile phone technologies (51,52). These alternative approaches could free up more of clinicians’ time for delivering evidence-based psychotherapies that can have a greater impact on veterans functioning (53).
The authors are unaware of any significant unintended effects or harms of this telephone intervention. Five (1.2%) participants asked to discontinue calls due to distress and 4 (1.0%) due to concerns about confidentiality. As noted above, this study was limited to patients who sought intensive residential treatment in VA health care system, where aftercare was readily available. Telephone case monitoring might function differently in other treatment environments.
Conclusions
Augmenting usual care with biweekly telephone care management support in the first three months after discharge failed to improve veterans’ clinical outcomes in the year after residential PTSD treatment. This is likely due to the fact that patients were already high utilizers of outpatient care, receiving an average of one visit every 10 days in the year after discharge. Many veterans had continuing difficulties in functioning despite receiving a large dose of care. This suggests a need for more effective and efficient ways of providing continuing support to veterans living with severe and chronic PTSD.
References
- 1.Greenberg GA, Rosenheck RA, Fontana A: Continuity of care and clinical effectiveness: Treatment of posttraumatic stress disorder in the Department of Veteran Affairs. The Journal of Behavioral Health Services & Research 30:202–214, 2003 [DOI] [PubMed] [Google Scholar]
- 2.Mistiaen P, Poot E: Telephone follow-up, initiated by a hospital-based health professional, for postdischarge problems in patients discharged from hospital to home. Cochrane Database of Systematic Reviews 18:CD004510, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ilgen MA, Hu KU, Moos RH, McKellar J: Continuing care after inpatient psychiatric treatment for patients with psychiatric and substance use disorders. Psychiatric Services 59:982–988, 2008 [DOI] [PubMed] [Google Scholar]
- 4.Steffen S, Kosters M, Becker T, Puschner B: Discharge planning in mental health care: A systematic review of the recent literature. Acta Psychiatrica Scandinavica 120:1–9, 2009 [DOI] [PubMed] [Google Scholar]
- 5.Desai R, Spencer H, Gray S, Pilver C: The Long Journey Home XVIII Treatment of posttraumatic stress disorder in the Department of Veterans Affairs: Fiscal year 2009 Service Delivery and Performance. West Haven, CT: Northeast Program Evaluation Center, 2010 [Google Scholar]
- 6.McFall M, Fontana A, Raskind M, Rosenheck R: Analysis of violent behavior in Vietnam combat veteran psychiatric inpatients with posttraumatic stress disorder. Journal of Traumatic Stress 12:501–517, 1999 [DOI] [PubMed] [Google Scholar]
- 7.Fontana A, Rosenheck R: Treatment-seeking veterans of Iraq and Afghanistan: Comparison with veterans of previous wars. Journal of Nervous and Mental Disease 196:513–521, 2008 [DOI] [PubMed] [Google Scholar]
- 8.Rosen CS, Murphy RT, Chow HC, et al. : PTSD patients’ readiness to change alcohol and anger problems. Psychotherapy 38:233–244, 2001 [Google Scholar]
- 9.Hartl TL, Rosen CS, Drescher KD, et al. : Predicting high-risk behaviors in combat veterans with posttraumatic stress disorder. Journal of Nervous and Mental Disease 193:464–472, 2005 [DOI] [PubMed] [Google Scholar]
- 10.Fontana A, Rosenheck R. Effectiveness and cost of the inpatient treatment of posttraumatic stress disorder: comparison of three models of treatment. American Journal of Psychiatry 154: 758–65, 1997. [DOI] [PubMed] [Google Scholar]
- 11.Rosenheck R, Fontana A. Impact of efforts to reduce inpatient costs on clinical effectiveness: treatment of posttraumatic stress disorder in the Department of Veterans Affairs. Medical Care 39: 168–80, 2001. [DOI] [PubMed] [Google Scholar]
- 12.Lockwood A, Steinke DT, Botts SR: Medication adherence and its effects on relapse among patients discharged from a Veterans Affairs Posttraumatic Stress Disorder treatment program. Annals of Pharmacotherapy 43:1227–1232, 2009 [DOI] [PubMed] [Google Scholar]
- 13.Olfson M, Mojtabai R, Sampson NA, et al. : Dropout from outpatient mental health care in the United States. Psychiatric Services 60:898–907, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Simon GE, Ludman EJ: Predictors of early dropout from psychotherapy for depression in community practice. Psychiatric Services 61:684–689, 2010 [DOI] [PubMed] [Google Scholar]
- 15.Harpaz-Rotem I, Rosenheck RA: Serving those who served: Retention of newly returning veterans from Iraq and Afghanistan in mental health treatment. Psychiatric Services 62:22–27, 2010 [DOI] [PubMed] [Google Scholar]
- 16.Lu MW, Duckart JP, O’Malley JP, et al. : Correlates of utilization of PTSD specialty treatment among recently diagnosed veterans at the VA. Psychiatric Services 62:943–949, 2011 [DOI] [PubMed] [Google Scholar]
- 17.Rosen CS, DiLandro C, Corwin KN, et al. : Telephone monitoring and support for veterans with chronic posttraumatic stress disorder: A pilot study. Community Mental Health Journal 42:501–508, 2006 [DOI] [PubMed] [Google Scholar]
- 18.Fortney JC, Pyne JM, Edlund MJ, et al. : Relationship between antidepressant medication possession and treatment response. General Hospital Psychiatry 32:377–379, 2010 [DOI] [PubMed] [Google Scholar]
- 19.Chong WW, Aslani P, Chen TF: Effectiveness of interventions to improve antidepressant medication adherence: A systematic review. International Journal of Clinical Practice 65:954–975, 2011 [DOI] [PubMed] [Google Scholar]
- 20.Zanjani F, Miller B, Turiano N, et al. : Effectiveness of telephone based referral care management, a brief intervention to improve psychiatric treatment engagement. Psychiatric Services 59:776–781, 2008 [DOI] [PubMed] [Google Scholar]
- 21.Seal K, Abadjian L, McCamish N, Shi Y, Tarasovsky G, Weingardt K. A randomized controlled trial of telephone motivational interviewing to enhance mental health treatment engagement in Iraq and Afghanistan veterans. General Hospital Psychiatry, in press. [DOI] [PubMed] [Google Scholar]
- 22.Cook PH, Emiliozzi S, Waters C et al. : Effects of telephone counseling on antipsychotic adherence and emergency department utilization. The American Journal of Managed Care 14:841–846, 2008 [PubMed] [Google Scholar]
- 23.Taylor CE, LoPiccolo CJ, Eisdorfer C, et al. : Reducing rehospitalization with telephonic targeted care management in a managed health care plan. Psychiatric Services 56:652–654, 2005 [DOI] [PubMed] [Google Scholar]
- 24.Oslin DW, Sayers S, Ross J, et al. : Disease management for depression and at-risk drinking via telephone in an older population of veterans. Psychosomatic Medicine 65:931–937, 2003 [DOI] [PubMed] [Google Scholar]
- 25.Williams JW, Gerrity M, Holsinger T, et al. : Systematic review of multifaceted interventions to improve depression care. General Hospital Psychiatry 29:91–116, 2007 [DOI] [PubMed] [Google Scholar]
- 26.Gensichen J, von Korff M, Peitz M, et al. : Case management for depression by health care assistants in small primary care practices: A cluster randomized trial. Annals of Internal Medicine 151:369–378, 2009 [DOI] [PubMed] [Google Scholar]
- 27.McKay JR, Lynch KG, Shepard DS, et al. : The effectiveness of telephone-based continuing care in the clinical management of alcohol and cocaine use disorders: 12 month outcomes. Journal of Consulting and Clinical Psychology 72:967–979, 2004 [DOI] [PubMed] [Google Scholar]
- 28.Godley MD, Coleman-Cowger VH, Titus JC, et al. : A randomized controlled trial of telephone continuing care. Journal of Substance Abuse Treatment 38:74–82, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dew SE, Bickman L: Participant expectancies about therapy. Mental Health Services Research 7:21–33, 2005 [DOI] [PubMed] [Google Scholar]
- 30.Pfeiffer PN, Glass J, Austin K, et al. : Impact of distance and facility of initial diagnosis on depression treatment. Health Services Research 46:768–786, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Straus M: Measuring intra family conflict and violence: The Conflict Tactics Scale. Journal of Marriage and the Family 41:75–188, 1979 [Google Scholar]
- 32.McLellan AT, Kushner H, Metzger D, et al. : The fifth edition of the Addiction Severity Index. Journal of Substance Abuse Treatment 9:199–213, 1992 [DOI] [PubMed] [Google Scholar]
- 33.Rosen CS, Henson BR, Finney JW, Moos RH: Consistency of self-administered and interview-based Addiction Severity Index composite scores. Addiction 95:419–425, 2000 [DOI] [PubMed] [Google Scholar]
- 34.Weathers FW, Litz BT, Herman DS, et al. : The PTSD Checklist (PCL): Reliability, validity, and diagnostic utility. Proceedings of the 9th Annual Meeting of the International Society of Traumatic Stress Studies Chicago, IL: ISTSS, 1993 [Google Scholar]
- 35.Radloff LS: The CES-D scale: A self report depression scale for research in the general population. Applied Psychological Measurement 1:385–401, 1977 [Google Scholar]
- 36.Fontana A, Ruzek JI, McFall M, & Rosenheck R The Veterans Affairs Military Stress Treatment Assessment (VAMSTA): A descriptive and monitoring instrument for the treatment of PTSD and comorbid disorders. West Haven, CT: Northeast Program Evaluation Center, 2006 [Google Scholar]
- 37.Horvath AO, Greenberg LS: Development and validation of the Working Alliance Inventory. Journal of Counseling Psychology 36:223–233, 1989 [Google Scholar]
- 38.Battle CC, Imber SD, Hoehn-Saric R, et al. : Target complaints as criteria of improvement. American Journal of Psychotherapy 20:184–192, 1996 [DOI] [PubMed] [Google Scholar]
- 39.Efron B: Forcing a sequential experiment to be balanced. Biometrika 58:403–417, 1971 [Google Scholar]
- 40.Dillman DA (1978) Mail and Telephone Surveys: The Total Design Method. New York: Wiley. [Google Scholar]
- 41.Rubin DB: Inference and missing data. Biometrika 63:581–592, 1976 [Google Scholar]
- 42.Schafer JL, Graham JW Missing data: Our view of the state of the art. Psychological Methods 7:147–177, 2002 [PubMed] [Google Scholar]
- 43.R Development Core Team: R: A language and environment for statistical computing. Vienna, Austria, R Foundation for Statistical Computing, 2009. [Google Scholar]
- 44.Van Buuren S, Oudshoorn CGM. Multivariate Imputation by Chained Equations. R package version 1.14, 2005. [Google Scholar]
- 45.Fontana A, Rosenheck R, Spencer H, Gray S: The Long Journey Home IX Treatment of posttraumatic stress disorder in the Department of Veterans Affairs: Fiscal year 2000 service delivery and performance. West Haven, CT: Northeast Program Evaluation Center, 2001 [Google Scholar]
- 46.Fontana A, Rosenheck R. Effects of compensation-seeking on treatment outcomes among veterans with posttraumatic stress disorder. Journal of Nervous and Mental Disease 186: 223–230, 1998 [DOI] [PubMed] [Google Scholar]
- 47.Belsher BE, Tiet QQ, Garvert, DW, Rosen CS. Compensation and treatment: Disability benefits and outcomes for veterans engaged in residential PTSD treatment. Journal of Traumatic Stress, in press. [DOI] [PubMed] [Google Scholar]
- 48.Laffaye C, Rosen CS, Schnurr PP.Friedman MJ. Does compensation status influence treatment participation and course of recovery from posttraumatic stress disorder? Military Medicine 172:1039–1045, 2007 [DOI] [PubMed] [Google Scholar]
- 49.Alvarez J, McLean CL, Harris AH et al. : The comparative effectiveness of Cognitive Processing Therapy for male Veterans treated in a VHA posttraumatic stress disorder residential rehabilitation program. Journal of Consulting and Clinical Psychology 79: 590–9, 2011 [DOI] [PubMed] [Google Scholar]
- 50.Shiner B, D’Avolio LW, Nguyen TM, et al. : Automated classification of psychotherapy note text: Implications for quality assessment in PTSD care. Journal of Evaluation in Clinical Practice, in press [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Jain S: The role of paraprofessionals in providing treatment for posttraumatic stress disorder in low-resource communities. The Journal of the American Medical Association 304:571–572, 2010 [DOI] [PubMed] [Google Scholar]
- 52.Cucciare MA, Weingardt KR, Humphreys K: How internet technology can improve the quality of care for substance use disorders. Current Drug Abuse Reviews 2:256–262, 2009 [DOI] [PubMed] [Google Scholar]
- 53.Karlin BE, Ruzek JI, Chard KM, et al. : Dissemination of evidence-based psychological treatments for posttraumatic stress disorder in the Veterans Health Administration. Journal of Traumatic Stress 23:663–673, 2010 [DOI] [PubMed] [Google Scholar]


