Abstract
Hypotension, poor peripheral perfusion, and tachycardia are the most common presenting signs of hemorrhagic shock. Many patients fail to show initial signs of tachycardia and paradoxically present with bradycardia. An 81-year-old man presenting with lower gastrointestinal bleed showed initial vital signs significant for tachycardia and normal blood pressure. After resuscitation with fluids and blood products, his heart rate stabilized to between 64 and 86 bpm. It later dropped to 30 bpm, which improved after administration of atropine. The patient soon experienced two episodes of hematochezia. The paradoxical bradycardia proved to be a false reassurance that the hemorrhage had resolved. Identification of paradoxical bradycardia is important in suspecting ongoing gastrointestinal hemorrhage.
Keywords: Bradycardia, hemorrhagic shock, paradoxical bradycardia, relative bradycardia
Relative bradycardia is defined as a heart rate (HR) <90 bpm in the setting of hemorrhage, and paradoxical bradycardia is the phenomenon with HR <60 bpm.1 Paradoxical bradycardia poses a diagnostic dilemma, because most clinicians are unaware of this finding, leading to delayed intervention. Paradoxical bradycardia is usually described in the setting of recent surgeries or trauma. We report a unique case of paradoxical bradycardia in a patient presenting with acute gastrointestinal bleed.
CASE DESCRIPTION
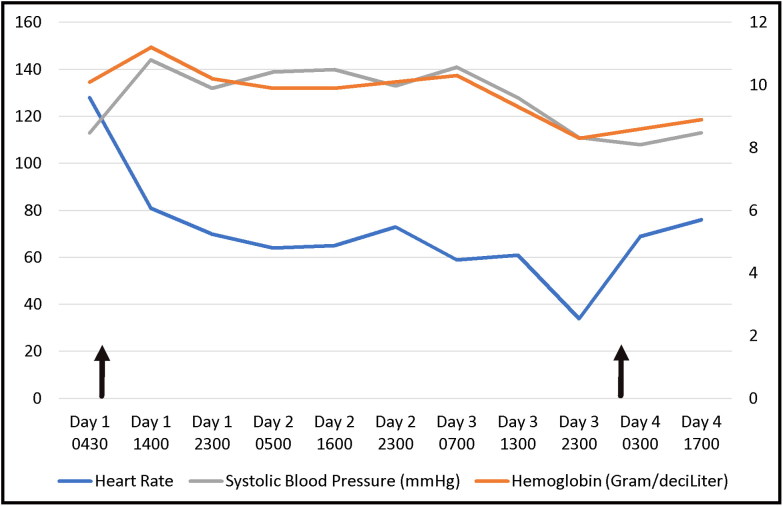
An 81-year-old man with prior diverticulosis and chronic deep vein thrombosis on warfarin presented with lower gastrointestinal hemorrhage. His blood pressure was 113/74 mm Hg with initial HR of 128 bpm. Initial international normalized ratio was 2.6, which decreased to 1.11 with vitamin K and fresh frozen plasma. The patient received two units of packed red blood cells at an outside facility prior to transfer, and his hemoglobin at the time of admission was 10.1 g/dL. After further resuscitation with fluids and blood products, his HR remained 64 to 86 bpm. A tagged red blood cell scan done on day 2 of admission was negative for acute hemorrhage. On day 3 of hospitalization, his HR decreased to 50 to 60 bpm, and an electrocardiogram showed sinus bradycardia. HR later declined further to the 30s, requiring atropine. Shortly afterward, the patient experienced two episodes of hematochezia, with an acute hemoglobin drop from 10.3 g/dL to 8.3 g/dL (Figure 1).
Figure 1.
Hemoglobin vs systolic blood pressure and heart rate. The first arrow indicates initial blood transfusion on presentation. The second arrow indicates the time of the second bleeding event, with blood transfusion administered shortly after. Times are approximate.
Multiple electrocardiograms disclosed no conduction delays or heart block. Results of a transthoracic echocardiogram, basic metabolic panel, and thyroid-stimulating hormone level were unremarkable. The patient’s HR remained stable after blood transfusion and volume resuscitation. He refused further intervention with endoscopy.
DISCUSSION
Most reported cases of paradoxical bradycardia are related to trauma, surgery, or retroperitoneal hemorrhage. The classic clinical schema for hemorrhagic shock is hypotension, poor peripheral perfusion, and tachycardia. The accurate response after significant volume loss is biphasic: initial tachycardia followed by bradycardia.2 Furthermore, up to 28% of patients do not manifest initial tachycardia but present with either relative or paradoxical bradycardia, as was the case for our patient.3
Paradoxical bradycardia is theorized to be mediated by the parasympathetic system. Afferent branches of the vagus and glossopharyngeal nerves located in the aortic arch detect a drop in pulse pressure during the initial phase of hemorrhage (10% to 15% blood loss).2 Activation of the baroreceptors causes a withdrawal of the efferent vagal activity, increasing the HR.2 Once the blood loss reaches 20% to 25%, efferent branches of the vagal nerve activity increases, which slows the HR to allow the ventricle increased time for filling.2
It is not known why some patients fail to display the initial tachycardic phase.3 Barriot and Riou did a retrospective chart review on patients who presented to an emergency department in hemorrhagic shock and found that those with paradoxical bradycardia (7%) were more likely to have massive, rapid bleeds.4 This may be the reason why our patient showed paradoxical bradycardia during his second hemorrhagic episode; another possibility is that his initial resuscitation efforts were not aggressive enough, causing his repeat hemorrhage to take him to the threshold where the neurohormonal reflex favors bradycardia.
Atropine was administered, because our patient complained of dizziness when his HR dropped to 30 bpm. In Barriot and Riou’s study, atropine was used in two patients, causing premature ventricular contractions in both patients and ventricular fibrillation in one of the patients.4 Repeat hemorrhage was not suspected until the hematochezia was witnessed and atropine was administered. In retrospect, aggressive fluid resuscitation should have been employed. This further underlines the importance of recognizing paradoxical bradycardia.
It is important to eliminate other causes of bradycardia. An electrocardiogram should be obtained to exclude bradyarrhythmias. A thorough medication review must be completed with emphasis on beta-blockers, nondihydropyridine calcium channel blockers, clonidine, and digoxin.5 Our patient was on timolol eye drops, which have been shown to cause bradycardia. This usually occurs during the first 6 months of introduction and in those with underlying cardiac disease.6 Stroke, hypothyroidism, acute myocardial infarction, and electrolyte abnormalities must be ruled out as well.5
References
- 1.Demetriades D, Chan LS, Bhasin P, et al. . Relative bradycardia in patients with traumatic hypotension. J Trauma. 1998;45(3):534–539. [DOI] [PubMed] [Google Scholar]
- 2.Little RA, Kirkman E, Driscoll P, Hanson J, Mackway-Jones K. Preventable deaths after injury: why are the traditional ‘vital’ signs poor indicators of blood loss? J Accid Emerg Med. 1995;12(1):1–14. doi: 10.1136/emj.12.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thomas I, Dixon J. Bradycardia in acute haemorrhage. BMJ. 2004; 328(7437):451–453. doi: 10.1136/bmj.328.7437.451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barriot P, Riou B. Hemorrhagic shock with paradoxical bradycardia. Intensive Care Med. 1987;13(3):203–207. [DOI] [PubMed] [Google Scholar]
- 5.Mangrum JM, DiMarco JP. The evaluation and management of bradycardia. N Engl J Med. 2000;342(10):703–709. doi: 10.1056/NEJM200003093421006. [DOI] [PubMed] [Google Scholar]
- 6.Pratt NL, Ramsay EN, Kalisch Ellett LM, et al. . Association between ophthalmic timolol and hospitalisation for bradycardia. J Ophthalmol. 2015;2015:567387. doi: 10.1155/2015/567387. [DOI] [PMC free article] [PubMed] [Google Scholar]