Abstract
Drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome is a potentially life-threatening drug-induced reaction. Though the most common clinical manifestations are eosinophilia, fever, rash, and lymphadenopathy, patients can also present with severe organ dysfunction. The pathogenesis of DRESS syndrome is only currently partially understood, though it is known that DRESS syndrome is commonly associated with infection or viral reactivation; specifically, human herpes viruses 6 and 7 and Epstein-Barr virus have been implicated in the pathogenesis. We present the first case of DRESS syndrome in the context of serology-proven influenza virus.
Keywords: DRESS syndrome, drug-induced hypersensitivity syndrome, eosinophilia, influenza, sulfasalazine
Drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome is an uncommon drug reaction associated with eosinophilia, fever, skin eruptions, and lymphadenopathy. Prior research on the pathogenesis of DRESS syndrome has implicated viral infection or reactivation and toxic metabolite accumulation paired with their subsequent immunological reactions.1,2 However, a more comprehensive understanding is still required in order to improve clinical diagnosis and management. We report the first case of DRESS syndrome associated with positive serology for influenza virus in hopes of contributing to the understanding of this syndrome and its pathogenesis.
CASE DESCRIPTION
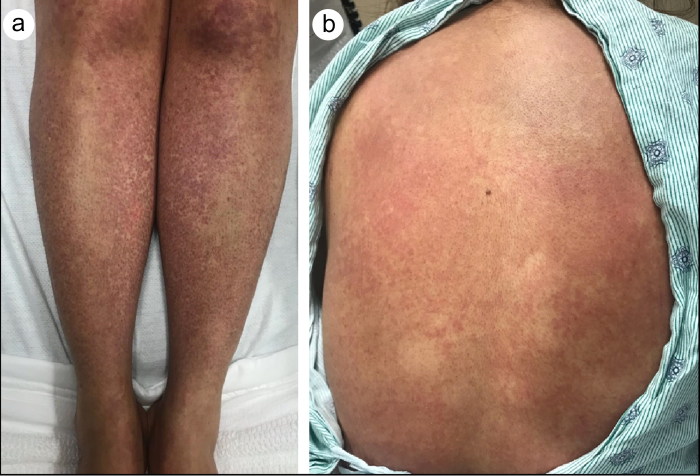
A 35-year-old woman with a history of rheumatoid arthritis was admitted after developing a new, diffuse rash over 10 days after starting sulfasalazine 6 weeks prior. The pruritic eruption first appeared on her right wrist and quickly proceeded to involve the majority of her body, including the palms, soles, and face. Concomitantly, she developed painful cervical lymphadenopathy, mild mucositis, and abdominal pain. Physical examination demonstrated widespread erythematous macules affecting the face, palms, soles, abdomen, back, and upper and lower extremities (Figure 1); the eyes, conjunctiva, and lips were unaffected. Notably, she developed a maximum temperature of 103°F.
Figure 1.
(a) Multiple dark red to brick brown macules and patches on the knees and anterior legs. (b) Erythematous macules coalescing into patches on the back.
Laboratory testing demonstrated positive influenza A and B antigens, transaminitis, and eosinophilia (1.26 × 109/L); blood cultures and serological testing for Rickettsia rickettsii, human immunodeficiency virus, and hepatitis A, B, and C were negative. Epstein-Barr virus (EBV) serology was consistent with past infection. A punch biopsy revealed a lymphocytic perivascular infiltrate in the dermis, with prominent extravasation of red blood cells; fibrinoid necrosis was not appreciated. Given the clinical constellation (with a RegiSCAR score of 4), treatment was started with 60 mg methylprednisolone intravenously twice a day, resulting in improvement over the course of a week. She was subsequently switched to oral prednisone (to be tapered over 6 weeks) and discharged for outpatient management.
DISCUSSION
DRESS is a life-threatening adverse medication effect that has been associated with numerous drugs, such as anticonvulsants, allopurinol, and sulfonamides.1 DRESS syndrome is unique in that the cutaneous eruption manifests 3 to 8 weeks after initial drug administration, whereas other drug-related reactions occur within 1 to 2 weeks.1
One postulated explanation for the latency period is the time necessary for toxic metabolite accumulation. For example, anticonvulsant-related DRESS has been linked to an inherited epoxide hydrolase deficiency, leading to increased arylamine reactive intermediates from aromatic anticonvulsant breakdown.1 Similarly, sulfonamide-associated DRESS has been associated with slow acetylator phenotypes, an important component of phase II detoxification.3 Elevated drug metabolites are believed to drive cell death and delayed T-cell activation, leading to release of cytokines, including interleukin-5, and thus triggering peripheral eosinophilia.2
Viral infection or reactivation (most commonly, human herpes virus [HHV] 6 and 7 and EBV) has also been implicated in the pathogenesis. To our knowledge, this is the first reported case of DRESS syndrome in the context of serology-proven influenza virus; two cases of DRESS after influenza vaccination do exist.4,5
Reactivation of HHV subtypes (most often HHV-6, HHV-7, EBV, and cytomegalovirus) has been implicated in driving DRESS via viral T-cell expansion and drug-antigen cross-reactivity.1,6 Disease progression beyond drug cessation and potential visceral involvement after initial resolution support this theory.6 It is plausible that the drug causes antiviral T cells to cross-react with alloantigens.1 In an analysis of peripheral blood T cells (CD4 and CD8) in 40 patients with DRESS secondary to allopurinol, sulfonamides, and carbamazepine, over 70% of patients demonstrated EBV, HHV6, or HHV7 reactivation.7 CD8 activation was present in all patients in locations such as the skin, liver, and lungs, and tumor necrosis factor-α and interferon-γ levels correlated with the degree of visceral involvement.7 Notably, nearly half of activated T cells recognized EBV epitopes, and drug administration triggered viral production in previously EBV-transformed B cells.7 Therefore, drug-related viral reactivation and the ensuing immune response to viral epitopes could explain how multi-organ symptoms occur long after drug discontinuation.
A number of factors—drug, viral, and genetic—appear to drive this unique syndrome, of which our understanding continues to evolve. We hope that our reporting of this novel presentation of DRESS in the context of influenza virus can shed light on a potential new dimension of the puzzle.
References
- 1.Cho YT, Yang CW, Chu CY. Drug reaction with eosinophilia and systemic symptoms (DRESS): an interplay among drugs, viruses, and immune system. IJMS. 2017;18:E1243. doi: 10.3390/ijms18061243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Choudhary S, McLeod M, Torchia D, et al. . Drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome. J Clin Aesthet Dermatol. 2013;6(6):31–37. [PMC free article] [PubMed] [Google Scholar]
- 3.Michel F, Navellou JC, Ferraud D, et al. . DRESS syndrome in a patient on sulfasalazine for rheumatoid arthritis. Joint Bone Spine. 2005;72:82–85. doi: 10.1016/j.jbspin.2004.06.002.. [DOI] [PubMed] [Google Scholar]
- 4.Hewitt N, Levinson M, Stephenson G. Drug reaction with eosinophilia and systemic symptoms associated with H1N1 vaccination. Intern Med J. 2012;42:1365–1366. doi: 10.1111/imj.12012. [DOI] [PubMed] [Google Scholar]
- 5.Solak B, Dikicier BS, Kara RO, et al. . DRESS syndrome potentially induced by allopurinol and triggered by influenza vaccine. BMJ Case Rep. 2016;2016:bcr2016214563. doi: 10.1136/bcr-2016-214563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shiohara T, Inaoka M, Kano Y. Drug-induced hypersensitivity syndrome (DIHS): a reaction induced by a complex interplay among herpesviruses and antiviral and antidrug immune responses. Allergol Int. 2006;55:1–8. [DOI] [PubMed] [Google Scholar]
- 7.Picard D, Janela B, Descamps V, et al. . Drug reaction with eosinophilia and systemic symptoms (DRESS): a multiorgan antiviral T cell response. Sci Transl Med. 2010;2(46):46ra62. doi: 10.1126/scitranslmed.3001116. [DOI] [PubMed] [Google Scholar]