Abstract
Background:
While liver disease increases surgical risk, it is not accounted for in the Society for Thoracic Surgeons (STS) risk calculator. This study assessed the impact of Model for End-stage Liver Disease (MELD) on outcomes after cardiac surgery and the additional predictive value of MELD in the STS risk model.
Methods:
De-identified records of 21,272 patients were extracted from a regional STS database. Inclusion criteria were any cardiac operation with a risk score available (2011–2016). Exclusion criteria included missing MELD (n=2,895) or preoperative anticoagulation (n=144). Patients were stratified into three categories, MELD <9 (low), MELD 9–15 (moderate), and MELD >15 (high). Univariate and multivariate logistic regression assessed risk-adjusted associations between MELD and operative outcomes.
Results:
Increasing MELD scores were associated with greater comorbid disease, mitral surgery, prior cardiac surgery and higher STS predicted risk of mortality (1.1%, 2.3%, 6.0% by MELD category, p<0.0001). The operative mortality rate increased with increasing MELD score (1.6%, 3.9%, and 8.4%, p<0.0001). By logistic regression, MELD score was an independent predictor of operative mortality (OR 1.03 per MELD score point, p<0.0001) as were the components total bilirubin (OR 1.22 per mg/dL, p=0.002) and INR (OR 1.40 per unit, p<0.0001). Finally, MELD score was independently associated with STS major morbidity, and the component complications renal failure and stroke.
Conclusions:
Increasing MELD score, INR, and bilirubin all independently increase risk of operative mortality. Since high rates of missing data currently limit utilization of MELD, efforts to simplify and improve data collection would help improve future risk models.
Classifications: Liver Disease, Cirrhosis, MELD, Bilirubin, INR, Cardiac Surgery
Current risk assessment tools, such as the Society of Thoracic Surgeons (STS) risk score, and the European System for Cardiac Operative Risk Evaluation, have proven useful in predicting morbidity and mortality in cardiac surgery patients based on demographics, comorbidities, and procedure type.[1, 2] However, the presence of liver disease as a comorbidity is not addressed in these common risk stratification methods. Liver disease has been shown to increase morbidity and mortality in patients undergoing cardiac surgery.[3, 4] While the Model for End-Stage Liver Disease (MELD) was originally used to predict outcomes in patients undergoing transjugular intrahepatic shunts, it has shown useful as a general predictor of survival for patients with severe liver disease.[5] MELD score is calculated through an equation that considers serum bilirubin, creatinine, international normalized ratio (INR), and the need for dialysis.
At baseline, operative patients with liver dysfunction are at high risk due to related sequelae, including decreased toxin clearance, impaired nutritional status, hepatorenal syndrome, infections, and coagulopathies. Numerous studies suggest MELD is predictive of morbidity and mortality in a variety of surgical disciplines outside of cardiac surgery.[6–9] Across surgical populations MELD has been associated with morbidity, mortality and resource utilization. Studies have also assessed MELD-XI which accounts for anticoagulation, which in the transcather aortic valve replacement and tricuspid surgical populations and correlates with survival.[10, 11]
Few analyses evaluate MELD in patients undergoing cardiac surgery and these are largely smaller, single institutional studies.[12] It is reasonable to surmise that the stress of surgery and cardiopulmonary bypass is likely to exacerbate the derangements present in patients with significant liver disease. Yet no large multiinstitutional studies have evaluated the utility of MELD in predicting cardiac surgery outcomes and it is not included in current risk score algorithms. We hypothesized that liver disease and MELD score would be independently associated with morbidity and mortality after cardiac surgery.
PATIENTS AND METHODS
Patient Data
The Virginia Cardiac Services Quality Initiative (VCSQI) is comprised of 19 hospitals and cardiac surgery practices in Virginia and North Carolina region. The methodology for VCSQI clinical and cost data acquisition have been described in detail previously.[13, 14] Briefly, participating hospitals submit STS Adult Cardiac Surgery Database data to VCSQI. The STS clinical data is paired with Uniform Billing-04 files that contain hospital charges. The charges are reclassified by International Classification of Diseases, ninth revision–based revenue codes and converted to estimated costs.
Patient records for all cardiac surgeries from January 1, 2011 through December 31, 2016 (STS data versions 2.73–2.81) were extracted from the Virginia Cardiac Services Quality Initiative (VCSQI) database in a deidentified fashion. Patients were excluded for missing MELD, missing predicted risk of mortality (PROM), or anticoagulation with Coumadin. Standard STS definitions were utilized including operative mortality (30-day or in hospital) and majar morbidity (renal failure, reoperation, stroke, deep sternal wound infection, and prolonged ventilation). Liver disease is defined as a history of hepatitis B, hepatitis C, cirrhosis, portal hypertension, esophageal varices, chronic alcohol abuse or congestive hepatopathy.
Appropriate data use agreements are in place with all participating hospitals. This study was exempt from Institutional Review Board review as the data represents a secondary analysis of a quality database with no Health Insurance Portability and Accountability Act patient identifiers.
Statistical Analysis
Patients were stratified into three categories, MELD <9, MELD 9–15, and MELD >15 for univariate analysis. Categorical variables are represented as counts (percentages) while continuous variables as mean ± standard deviation (SD) or median [IQR as 25th, 75th percentile] depending on normality. Univariate analysis was performed including Chi-Square Test for categorical variables and independent T-Test or Mann Whitney U Test as appropriate. Hierarchical regression modeling calculated the association between MELD and operative outcomes using generalized linear mixed models with random effects of year and hospital. Nested models were utilized starting with the appropriate STS predicted risk score for the outcome of interest and then repeated with MELD, the component variables and liver disease. The utility of the additional covariates were assessed by variable effect size (odds ratio), the change in area under the curve (AUC) for the nested models, and most importantly the net reclassification improvement (NRI).
The NRI is an index measure of how well a new model reclassifies subjects compared to an old model (correct versus incorrect changes in prediction for cases and controls separately).[15] The NRI is a combination of these four proportions with a range from −2 when all patients are incorrectly reclassified to 2 with 100% correct reclassification. The formula is:
In this case a continuous or category free NRI was utilized. While the change in AUC represents a population level assessment of model performance, the NRI assessed the change in risk prediction at the individual level. Further information can be found in the Annals article by Grunkemeier and Jin.[16]
Two sensitivity analyses assessed the impact of MELD on operative mortality in isolated CABG patients and after imputation for all patients with a risk score available. Value for total bilirubin, INR and creatinine were imputated using the mean value stratified on the presence or absence of liver disease. All analyses were performed using SAS Version 9.4 (SAS Institute, Cary, NC) with 0.05 as the significance threshold.
RESULTS
Baseline Patient Characteristics and Operative Variables
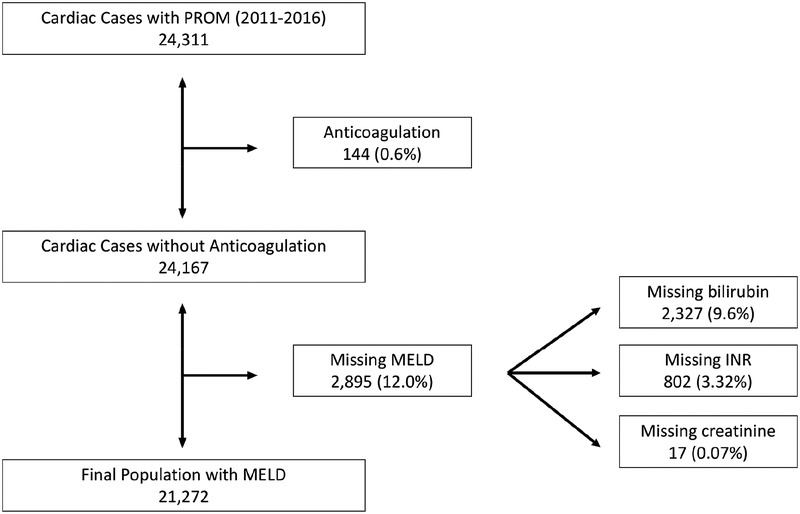
From a potential cohort of 24,311 patients, 144 were excluded for anticoagulation and 2,895 excluded for missing MELD score leaving a final population of 21,272 patients in the study (Figure 1). Of the patients with a missing MELD, 2,327 had a missing bilirubin level, 802 had a missing INR level, and only 17 had a missing creatinine level. Of included patients, the majority of patients had a low MELD score <9 (73%), while 21% had moderately elevated MELD of 9–15 and 5% severely elevated MELD that was >15. Distributions of demographics and comorbidities are represented in Table 1. Patients with a higher MELD tended have greater comorbid disease including diabetes, lung disease and cardiac disease. Renal failure had a greater impact on MELD than liver disease with all dialysis dependent renal failure patients in the high MELD group. While increasing MELD had increasing rates of liver disease, only 7.4% of those with a MELD>15 had documented history of liver disease.
Figure 1.
CONSORT diagram
Table 1.
Preoperative demographics and comorbidities
| MELD <9 | MELD 9–15 | MELD >15 | p-value | |
|---|---|---|---|---|
| Baseline Characteristics | (n=15566) | (n=4542) | (n=1164) | |
| Age (y, median, IQR) | 65 (57–72) | 69 (62–76) | 65 (57–73) | <0.0001 |
| Female | 4905 (31.5%) | 930 (20.5%) | 342 (29.4%) | <0.0001 |
| Chronic lung disease (mod/sev) | 1586 (10.5%) | 624 (14.1%) | 250 (22.1%) | <0.0001 |
| Prior stroke | 1133 (7.3%) | 483 (10.7%) | 174 (15.0%) | <0.0001 |
| Diabetes | 6250 (40.2%) | 2164 (47.7%) | 717 (61.6%) | <0.0001 |
| Dialysis dependent renal failure | 0 (0.0%) | 0 (0.0%) | 593 (51.0%) | <0.0001 |
| Hypertension | 12851 (82.6%) | 4000 (88.1%) | 1080 (92.8%) | <0.0001 |
| Coronary artery disease | 12983 (84.2%) | 3775 (84.1%) | 961 (84.4%) | 0.9838 |
| Heart failure within 2 weeks | 3729 (24.0%) | 1818 (40.1) | 632 (54.4%) | <0.0001 |
| Ejection Fraction (median, IQR) | 55 (50–60) | 55 (40–60) | 50(37–60) | <0.0001 |
| Active endocarditis | 132 (0.9%) | 91 (2.0%) | 69 (6.0%) | <0.0001 |
| STS PROM (%; median, IQR) | 1.8% ± 2.5 | 3.8% ± 4.8 | 9.3% ± 10.2 | <0.0001 |
| Liver disease | 546 (3.5%) | 245 (5.4%) | 90 (7.8%) | <0.0001 |
| MELD (median, IQR) | 7 (6.4–7.5) | 10.6 (9.6–12.0) | 19.7 (17.5–20.8) | <0.0001 |
| Creatinine (median, IQR) | 0.9 (0.8–1.0) | 1.3 (1.1–1.5) | 3.2 (1.9–5.9) | <0.0001 |
| T otal bilirubin (median, IQR) | 0.5 (0.4–0.7) | 0.6 (0.4–0.9) | 0.5 (0.3–0.8) | <0.0001 |
| INR (median, IQR) | 1.0 (1.0–1.1) | 1.1 (1.0–1.2) | 1.1 (1.0–1.4) | <0.0001 |
INR = International Normalized Ratio; MELD = Model for End-stage Liver Disease; PROM = Predicted Risk of Mortality; STS = Society of Thoracic Surgeons
Increasing MELD correlated with higher median STS PROM (1.1% vs 2.3% vs 6%, p<0.0001). The operative characteristics by MELD category are displayed in Table 2. Higher MELD was associated with higher rates of mitral surgery, urgent/emergent and reoperative cases.
Table 2.
Operative characteristics
| MELD <9 | MELD 9–15 | MELD >15 | ||
|---|---|---|---|---|
| Operative Characteristics | (n=15566) | (n=4542) | (n=1164) | p-value |
| Coronary artery bypass | 12475 (80.1%) | 3515 (77.4%) | 890 (76.5%) | <0.0001 |
| Aortic replacement | 3132 (20.1%) | 1059 (23.3%) | 246 (21.1%) | <0.0001 |
| Mitral replacement | 449 (2.9%) | 270 (5.9%) | 117 (10.1%) | <0.0001 |
| Mitral repair | 1047 (6.7%) | 356 (7.8) | 86 (7.4%) | 0.0314 |
| Urgent or emergent | 8042 (51.7%) | 2496 (55.0%) | 723 (62.1%) | <0.0001 |
| Prior cardiac surgery | 676 (4.3%) | 380 (8.4%) | 112 (9.6%) | <0.0001 |
| Cross clamp time (min) | 73 [56–94] | 77 [60–99] | 78 [60–98] | <0.0001 |
| Cardiopulmonary bypass time (min) | 99 [78–126] | 107 [84–136] | 108 [84–140] | <0.0001 |
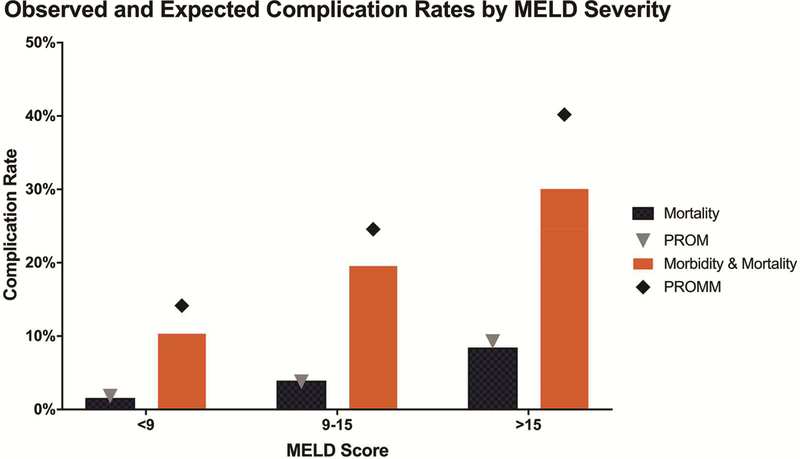
Unadjusted Short-term Outcomes
Higher MELD groups had higher rates of all short-term adverse outcomes measured (Table 3), although potentially confounded by other risk factors. The operative mortality rate reached 8.4% in patients with MELD>15 compared to 1.6% and 3.4% in the other two groups. Similarly, the highest MELD group had more than triple the rate of major morbidity (33%) compared to the lowest MELD group (9%) as seen in Figure 2. This trend of near three fold increase in complication rate for the highest versus lowest MELD group was also true for prolonged ventilation, permanent stroke, renal failure, cardiac arrest, reoperation and transfusion.
Table 3.
Short-term outcomes
| MELD <9 | MELD 9–15 | MELD >15 | ||
|---|---|---|---|---|
| Outcomes | (n=15566) | (n=4542) | (n=1164) | p-value |
| Operative mortality | 246 (1.6%) | 179 (3.9%) | 98 (8.4%) | <0.0001 |
| Major morbidity | 1520 (9.8%) | 833 (18.4%) | 386 (33.2%) | <0.0001 |
| Permanent stroke | 167 (1.1%) | 80 (1.8%) | 28 (2.4%) | <0.0001 |
| Prolonged ventilation | 1114 (7.2%) | 628 (13.8%) | 274 (23.5%) | <0.0001 |
| Dialysis dependent renal failure | 126 (0.8%) | 143 (3.2%) | 90 (7.7%) | <0.0001 |
| Readmission | 1257 (8.5%) | 492 (11.5%) | 171 (16.2%) | <0.0001 |
| Discharge to facility | 2937 (19.2%) | 1364 (31.1%) | 455 (42.1%) | <0.0001 |
| Total cost (mean) | 33898 [26566–47451] | 38655 [29247–57309] | 54414 [36961–81906] | <0.0001 |
| Postoperative LOS (days) | 5 [4–7] | 6 [5–9] | 8 [6–13] | <0.001 |
LOS = Length of Stay
Figure 2.
Rates of mortality or morbidity and mortality by MELD category. Expected rates are displayed as corresponding symbols using STS risk scores.
Risk-adjusted Associations of MELD with Mortality and Morbidity
Hierarchical logistic regression demonstrated continued associations between MELD and some short-term outcomes even after risk-adjustment (Table 4). MELD continued to be a strong independent predictor of operative mortality with an adjusted odds ratio (AOR) of 1.06 per MELD score point after risk adjustment (p<0.0001). Addition of MELD to PROM increased AUC from 0.7869 to 0.7904, and more importantly significantly improved prediction of mortality with an NRI of 0.26 (0.18–0.35), p<0.0001 (Supplemental Table 3). The association between MELD and major morbidity was less strong (AOR 1.01 per MELD score point, p=0.035) and improvement in the model was minimal. MELD was only independently associated with the component complication of renal failure (AOR 1.12 per MELD score point, p<0.0001).
Table 4.
Risk-adjusted associations between MELD and outcomes with nested hierarchical regression models.
| Characteristics | AOR | 95% CI | p-value | AUC Baseline | AUC with MELD |
|---|---|---|---|---|---|
| Operative mortality | 1.06 | (1.04–1.08) | <0.0001 | 0.7869 | 0.7904 |
| Major morbidity | 1.01 | (1.00–1.03) | 0.035 | 0.7485 | 0.7486 |
| Permanent stroke | 1.03 | (0.99–1.06) | 0.126 | 0.6805 | 0.6819 |
| Prolonged ventilation | 1.01 | (0.99–1.02) | 0.295 | 0.7728 | 0.7730 |
| Renal failure | 1.12 | (1.09–1.15) | <0.0001 | 0.8176 | 0.8165 |
| Deep sternal wound infection | 1.06 | (0.95–1.18) | 0.299 | 0.9083 | 0.8989 |
| Reoperation | 1.01 | (0.99–1.03) | 0.648 | 0.6983 | 0.6983 |
AOR = adjusted odds ratio; CI = confident interval; AUC = area under the curve
MELD score was further decomposed into its component variables to determine their individual associations with operative mortality (Table 5). Total bilirubin was strongly associated with mortality (AOR 1.23 per mg/dL, p=0.0008) but only increased the AUC from 0.7869 to 0.7874 and had an NRI of 0.09 (p=0.051). Meanwhile, INR was strongly associated with mortality (AOR 1.40 per unit, p<0.0001), increased the AUC from 0.7869 to 0.7920 with an NRI of 0.12 (p=0.006). Creatinine, already incorporated in PROM, was not independently associated with mortality (p=0.689) with no meaningful change in AUC or NRI.
Table 5.
Risk-adjusted associations between components of MELD and operative mortality with nested hierarchical regression models.
| Characteristics | AOR | 95% CI | p-value | AUC Baseline | AUC Combined |
|---|---|---|---|---|---|
| Total bilirubin | 1.23 | (1.09–1.40) | 0.0008 | 0.7869 | 0.7874 |
| INR | 1.40 | (1.23–1.60) | <0.0001 | 0.7869 | 0.7920 |
| Creatinine | 0.99 | (0.92–1.07) | 0.689 | 0.7869 | 0.7871 |
AOR = adjusted odds ratio; CI = confident interval; AUC = area under the curve
Another method to analyze risk-adjusted outcomes is by using observed to expected ratios. Only the low MELD category was significantly lower than expected (p=0.025) while moderate and severe were not significantly different from expected (p=0.607 and p=0.336). The observed to expected ratios for morbidity and mortality increased with increasing MELD and were significantly lower than expected for all three MELD categories (p <0.0001, p<0.0001, p=0.0003).
Risk-adjusted Associations of liver disease with Mortality and Morbidity
The dichotomous variable liver disease was found to be a strong independent predictor of operative mortality with an AOR 2.08 (1.49–2.91; p<0.0001). There was also a significant improvement in the model as measured by NRI (0.09, p=0.04). Liver disease was associated with major morbidity, AOR 1.36 (1.12–1.66; p=0.002) and its component prolonged ventilation [AOR 1.39 (1.12–1.74); p=0.003]. There were no significant associations between liver disease and permanent stroke [AOR 1.06 (0.60–1.88); p=0.827], renal failure [AOR 1.24 (0.82–1.89); p=0.305], or reoperation [AOR 1.25 (0.93–1.70); p=0.146].
Sensitivity Analyses
A total of 16,533 patients underwent isolated CABG procedures and were not on preoperative anticoagulation. Of these, MELD missing in 2,022 (12.2%) cases for a population of 14,511 patients in the first sensitivity analysis. The complete results are available in Supplemental Table 1. Similar results to the entire cohort were found with MELD (AOR 1.07 per MELD unit), INR (AOR 1.39 per unit) and liver disease (AOR 3.03) all being significant predictors of operative mortality.
Of the 24,167 patients with a risk score available and not on preoperative anticoagulation, a further 93 (0.4%) were excluded for missing liver disease information for a final cohort of 24,074 in the second sensitivity analysis. The results of regression analyses for operative mortality are shown in Supplemental Table 2. MELD (AOR 1.06 per MELD unit), total bilirubin (AOR 1.26 per mg/dL), INR (AOR 1.38 per unit) and liver disease (AOR 2.06) were all significant predictors of operative mortality.
COMMENT
This large multi-institutional analysis of cardiac surgery patients within the Commonwealth of Virginia demonstrates that MELD score correlates with increasing preoperative risk and patient complexity. Not surprisingly therefore, as MELD increases so do postoperative complications. Yet even after risk adjustment, MELD remains a significant independent predictor of operative mortality and improves the performance of the STS risk model. While also a predictor of major morbidity and component complications, the predictive impact is less. Looking at the component variables of MELD, both total bilirubin and INR are significantly associated with mortalilty, with INR the more significant of the two. Finally, even the dichotomous variable of liver disease is an independent predictor of operative mortality and may be a useful addition to current risk models. The addition of these factors significantly improved current operative mortality risk models as assessed by the net reclassification index, with MELD providing the most improvement with an NRI of 0.26.
The majority of cardiac surgical research within this topic has focused on the impact of liver disease and in particular cirrhosis on outcomes. One methodology has been to stratify cirrhotic patients by Child-Turcotte-Pugh classification.[3, 4, 17–22] These smaller institutional studies have clearly demonstrated that worsening liver disease is associated with worse outcomes. However, this methodology is limited by small numbers of severe liver disease patients who undergo cardiac surgery as well as the subjective nature of some components to this scoring system. Another strategy is to simply stratify by presence of any liver disease, which has been shown in the national inpatient sample to dramatically increase rates of mortality and other complications.[23] In this analysis liver disease was a very strong independent predictor of operative mortality with an adjusted odds ratio of 2.08 (p<0.0001). Also consistent with prior results liver disease was independently associated with major morbidity (AOR 1.36, p=0.003).
Risk prediction is severely limited when stratifying patients by presence of liver disease or subjective severity. In comparison, the MELD score uses three simple metrics to quantify the degree of liver dysfunction (INR and bilirubin) and associated renal dysfunction. In fact, studies of tricuspid surgical patients show MELD is highly predictive of mortality.[11, 12] A MELD >15 was associated with a 9 fold higher odds of mortality.[12] Other small studies of cirrhotic patients undergoing coronary and valve operations have mostly found MELD to be a predictor of mortality.[17, 19–22, 24] The utility of MELD goes beyond its objective nature, it does not rely on clinical diagnosis of liver dysfunction. Yet only one single center unadjusted analysis has included patients without a diagnosis of cirrhosis and demonstrated that MELD is predictive of both morbidity and mortality.[25] Our analysis confirms these results in a multi-instutional dataset, but also shows that MELD is predictive over and above the STS risk model. After risk adjustment, each one point increase in MELD is independently associated with a 6% increase in the odds of mortality.
This assessment is likely an underestimation of the impact of MELD as creatinine is contained in both MELD and the STS risk score used for risk-adjustment. Looking more closely at the two remaining components we see that INR is likely more useful than total bilirubin. A one point increase in INR was associated with a 40% increase in the odds of mortality (p<0.0001). The addition of INR to STS PROM improved the model from an AUC of 0.7869 to 0.7920, an even larger improvement than adding MELD or liver disease. While INR significantly improved the model as assessed by NRI, this impact was lower than for MELD as a whole (0.12 versus 0.26). While total bilirubin was also a strong independent predictor of mortalty (AOR 1.23) model improvement by change in AUC and NRI was less than with INR. These results suggest that attempts to use the simplified MELD-XI that excludes INR for patients on anticoagulation are eliminating an important predictor. Another alternative that should be explored would be updating the current STS database to collect sodium levels as well. This would enable calculation of MELD-Na, the current standard used for liver transplantation.[26] As the new score has been scaled to fit MELD this would not require any retroactive changes and would be a simple integration with continued automatic calculation of the total score.
The addition of each of these covariates to the operative mortality risk model results in a small absolute increase in the AUC. However, it is important to remember that risk prediction is improved for only a small number of high risk patients. It is these high risk patients at the extremes of the model were precision breaks down and further refinement of the model should focus. This theory is supported by the NRI, which assessed improvement on an individual level. As payment models change to value based mechanisms, precise risk adjustment in high risk patients will be critical to decreasing hospital based risk.[27] A major limitation of MELD in the STS Adult Cardiac Surgery Database is the high missing rate (12% in this cohort of patients) and this has precluded inclusion in the past. However, this analysis demonstrates the robustness of the relationship between liver disease and operative mortality. Sensitivity analyses using a more homogenous population of isolated CABG patients and using liver disease for imputation both result in similar associations between MELD and operative mortality. Efforts should be made to improve collection of bilirubin levels as well as other variables known to increase risk with high missing rates such as pulmonary hypertension.[28] Other alternatives should also be explored such as including liver disease and INR which have lower missing rates. A final option would be to estimate a normal bilirubin level for patients without liver disease.
This study has certain limitations such as those inherent to all retrospective reviews including the inability to prove causation. The exclusion of patients with MELD score missing may introduce selection bias, however multiple sensitivity analyses confirm the robust associations between MELD and operative mortality. The dataset utilized is also unable to to differentiate causes of liver disease, such as viral hepatopathies versus congestive, which likely have differential effects on complications. Also, the use of MELD is confounded by inclusion of creatinine in STS PROM. Thus the two other components were studied separately. The exclusion of anticoagulated patients limits the generalizability of the study, although this was felt to be necessary as INR is such a strong predictor and the number of patients excluded was low.
Conclusions
Liver disease is an important risk factor in patients undergoing cardiac surgery that is not currently accounted for in risk models. MELD and its components INR and bilirubin are objective assessments of liver function found to be independently associated with mortality and could help improve current STS risk models. Inclusion of MELD in the STS models has not been possible in the past due to a high number of missing values. The robustness of the association demonstrated in the CABG population and through imputation suggest efforts to improve data collection or include alternatives such as INR or liver disease should be considered. While these additions would have limited impact on low-risk patients, the precision of the risk prediction would improve for high risk patients. This is important to help both with clinical decision making as well as adjustment for future payment models.
Supplementary Material
ABBREVIATIONS
- AOR
Adjusted Odds Ratio
- AUC
Area Under the Curve
- CI
Confidence Interval
- INR
International Normalized Ratio
- IQR
Interquartile Range
- LOS
Length of Stay
- MELD
Model for End-stage Liver Disease
- PROM
Predicted Risk of Mortality
- SD
Standard Deviation
- STS
Society of Thoracic Surgeons
- VCSQI
Virginia Cardiac Services Quality Initiative
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Jin R, Furnary AP, Fine SC, Blackstone EH, Grunkemeier GL. Using society of thoracic surgeons risk models for risk-adjusting cardiac surgery results. Ann Thorac Surg 2010;89:677–682. [DOI] [PubMed] [Google Scholar]
- 2.Roques F, Nashef SA, Michel P et al. Risk factors and outcome in european cardiac surgery: Analysis of the euroscore multinational database of 19030 patients. Eur J Cardiothorac Surg 1999;15:816–822; discussion 822–813. [DOI] [PubMed] [Google Scholar]
- 3.An Y, Xiao YB, Zhong QJ. Open-heart surgery in patients with liver cirrhosis. Eur J Cardiothorac Surg 2007;31:1094–1098. [DOI] [PubMed] [Google Scholar]
- 4.Morisaki A, Hosono M, Sasaki Y et al. Risk factor analysis in patients with liver cirrhosis undergoing cardiovascular operations. Ann Thorac Surg 2010;89:811–817. [DOI] [PubMed] [Google Scholar]
- 5.Malinchoc M, Kamath PS, Gordon FD, Peine CJ, Rank J, ter Borg PC. A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts. Hepatology 2000;31:864–871. [DOI] [PubMed] [Google Scholar]
- 6.Hedrick TL, Swenson BR, Friel CM. Model for end-stage liver disease (meld) in predicting postoperative mortality of patients undergoing colorectal surgery. Am Surg 2013;79:347–352. [PubMed] [Google Scholar]
- 7.Krafcik BM, Farber A, Eslami MH et al. The role of model for end-stage liver disease (meld) score in predicting outcomes for lower extremity bypass. J Vasc Surg 2016;64:124–130. [DOI] [PubMed] [Google Scholar]
- 8.Northup PG, Wanamaker RC, Lee VD, Adams RB, Berg CL. Model for end-stage liver disease (meld) predicts nontransplant surgical mortality in patients with cirrhosis. Ann Surg 2005;242:244–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Havens JM, Columbus AB, Olufajo OA, Askari R, Salim A, Christopher KB. Association of model for end-stage liver disease score with mortality in emergency general surgery patients. JAMA Surg 2016;151:e160789. [DOI] [PubMed] [Google Scholar]
- 10.Arai T, Yashima F, Yanagisawa R et al. Prognostic value of liver dysfunction assessed by meld-xi scoring system in patients undergoing transcatheter aortic valve implantation. Int J Cardiol 2017;228:648–653. [DOI] [PubMed] [Google Scholar]
- 11.Tsuda K, Koide M, Kunii Y et al. Simplified model for end-stage liver disease score predicts mortality for tricuspid valve surgery. Interact Cardiovasc Thorac Surg 2013;16:630–635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ailawadi G, Lapar DJ, Swenson BR et al. Model for end-stage liver disease predicts mortality for tricuspid valve surgery. Ann Thorac Surg 2009;87:1460–1467; discussion 1467–1468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Osnabrugge RL, Speir AM, Head SJ et al. Costs for surgical aortic valve replacement according to preoperative risk categories. Ann Thorac Surg 2013;96:500–506. [DOI] [PubMed] [Google Scholar]
- 14.Hawkins RB, Downs EA, Johnston LE et al. Impact of transcatheter technology on surgical aortic valve replacement volume, outcomes, and cost. Ann Thorac Surg 2017;103:1815–1823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pencina MJ, D’Agostino RB Sr., Steyerberg EW. Extensions of net reclassification improvement calculations to measure usefulness of new biomarkers. Stat Med 2011;30:11–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Grunkemeier GL, Jin R. Net reclassification index: Measuring the incremental value of adding a new risk factor to an existing risk model. Ann Thorac Surg 2015;99:388–392. [DOI] [PubMed] [Google Scholar]
- 17.Filsoufi F, Salzberg SP, Rahmanian PB et al. Early and late outcome of cardiac surgery in patients with liver cirrhosis. Liver Transpl 2007;13:990–995. [DOI] [PubMed] [Google Scholar]
- 18.Lopez-Delgado JC, Esteve F, Javierre C et al. Short-term independent mortality risk factors in patients with cirrhosis undergoing cardiac surgery. Interact Cardiovasc Thorac Surg 2013;16:332–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Morimoto N, Okada K, Okita Y. The model for end-stage liver disease (meld) predicts early and late outcomes of cardiovascular operations in patients with liver cirrhosis. Ann Thorac Surg 2013;96:1672–1678. [DOI] [PubMed] [Google Scholar]
- 20.Suman A, Barnes DS, Zein NN, Levinthal GN, Connor JT, Carey WD. Predicting outcome after cardiac surgery in patients with cirrhosis: A comparison of child-pugh and meld scores. Clin Gastroenterol Hepatol 2004;2:719–723. [DOI] [PubMed] [Google Scholar]
- 21.Thielmann M, Mechmet A, Neuhauser M et al. Risk prediction and outcomes in patients with liver cirrhosis undergoing open-heart surgery. Eur J Cardiothorac Surg 2010;38:592–599. [DOI] [PubMed] [Google Scholar]
- 22.Vanhuyse F, Maureira P, Portocarrero E et al. Cardiac surgery in cirrhotic patients: Results and evaluation of risk factors. Eur J Cardiothorac Surg 2012;42:293–299. [DOI] [PubMed] [Google Scholar]
- 23.Araujo L, Dombrovskiy V, Kamran W et al. The effect of preoperative liver dysfunction on cardiac surgery outcomes. J Cardiothorac Surg 2017;12:73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Arif R, Seppelt P, Schwill S et al. Predictive risk factors for patients with cirrhosis undergoing heart surgery. Ann Thorac Surg 2012;94:1947–1952. [DOI] [PubMed] [Google Scholar]
- 25.Murata M, Kato TS, Kuwaki K, Yamamoto T, Dohi S, Amano A. Preoperative hepatic dysfunction could predict postoperative mortality and morbidity in patients undergoing cardiac surgery: Utilization of the meld scoring system. Int J Cardiol 2016;203:682–689. [DOI] [PubMed] [Google Scholar]
- 26.Kim WR, Biggins SW, Kremers WK et al. Hyponatremia and mortality among patients on the liver-transplant waiting list. N Engl J Med 2008;359:1018–1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hawkins RB, Mehaffey JH, Yount KW et al. Coronary artery bypass grafting bundled payment proposal will have significant financial impact on hospitals. J Thorac Cardiovasc Surg 2018;155:182–188. [DOI] [PubMed] [Google Scholar]
- 28.Kennedy JL, LaPar DJ, Kern JA et al. Does the society of thoracic surgeons risk score accurately predict operative mortality for patients with pulmonary hypertension? J Thorac Cardiovasc Surg 2013;146:631–637. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.