Abstract
Alcohol use may have significant negative impacts on individuals’ ability to remain adherent to ART, and may also yield other negative psychosocial, health-related, and behavioral outcomes. In addition, false beliefs about the consequences of mixing alcohol with ART use may cause individuals to avoid taking ART when drinking (alcohol-related ART avoidance). Although research conducted in the US and Europe has reported on alcohol-ART avoidance, the current study presents among the first quantitative evidence of alcohol-related intentional ART nonadherence in South Africa. Patients receiving ART from a community clinic in Cape Town (N =441) completed anonymous surveys of alcohol use, ART adherence, and alcohol-ART avoidance. Results showed that 292 (66%) participants reported current alcohol use; 25% who use alcohol believed that people who drink should stop taking ART when they are drinking and 24% stop their own ART when drinking. Alcohol-ART avoidance mediated the association between alcohol use and ART adherence. Results were robust when controlling for participant age, gender, current care status, and first versus second line ART. We found alcohol-ART avoidance may threaten successful ART in South Africa. Corrective messages that take a harm reduction approach to maximize ART adherence when drinking should be implemented in existing clinical services.
Introduction
The global scale-up of antiretroviral therapy (ART) has brought HIV treatment to nearly 21 million people living with HIV (HIV.gov, 2018), stirring hope of curtailing or perhaps even ending HIV epidemics. Alcohol use is among the many threats to the progress of HIV treatment is alcohol use. Concerns about the risks of alcohol use on health can lead to cessation of drinking after testing HIV positive (Hahn et al., 2016; Hahn et al., 2014), and again at the onset of ART (Santos et al., 2014), often rebounding after a brief time (Hahn et al., 2016). For some patients who continue drinking after starting ART, there may be significant negative effects of alcohol use on adherence, such as through impaired memory (Hendershot, Stoner, Pantalone, & Simoni, 2009). Studies show that even moderate use of alcohol is associated with incomplete ART adherence (Denison et al., 2018; Kim et al., 2017; Veld, Pengpid, Colebunders, Skaal, & Peltzer, 2017) and meta-analyses find that alcohol use is reliably associated with poor ART adherence (Heestermans, Browne, Aitken, Vervoort, & Klipstein-Grobusch, 2016), including in southern Africa (Shubber et al., 2016). The effects of alcohol on unintentional nonadherence, particularly those associated with memory, are often addressed in interventions to improve ART adherence (Simoni, Amico, Pearson, & Malow, 2008; Simoni, Pearson, Pantalone, Marks, & Crepaz, 2006).
Alcohol use can also lead to intentional nonadherence (alcohol-ART avoidance), which is not typically addressed in current interventions. Specifically, beliefs that it is harmful to mix alcohol with ART, referred to as alcohol-ART interactive toxicity beliefs, can motivate individuals to avoid taking ART when drinking alcohol (Kalichman et al., 2015). In Germany, for example, 24% of patients with suboptimal ART adherence state that they skip ART when drinking or using drugs (Boretzki et al., 2017), and in the US as many as one in three people living with HIV who use alcohol and drugs stop taking their medications when drinking (Kalichman et al., 2013; Kalichman et al., 2015; Pellowski, Kalichman, Kalichman, & Cherry, 2016). Alcohol-ART interactive toxicity beliefs may threaten ART adherence in South Africa, a country with the world’s largest ART expansion program (UNAIDS, 2014) and among the highest rates of alcohol consumption (Fritz, Morojele, & Kalichman, 2010).
Similar to the US and Europe, alcohol-related intentional nonadherence has been described in southern Africa. Research in Uganda found that 24% of patients receiving HIV services endorsed the belief that people should stop taking ART when drinking, and 15% indicated that they themselves occasionally stop taking ART in anticipation of using alcohol (Fatch et al., 2017; UNAIDS, 2017). Qualitative studies in South Africa find it is common to fear mixing alcohol with ART (Nkosi, Rich, Kekwaletswe, & Morojele, 2016) and caregivers encourage their HIV positive partners to not take their ART when drinking (Conroy et al., 2017). These studies show that among people who continue drinking after initiating ART, intentional nonadherence may be a source of suboptimal HIV treatment outcomes in southern Africa.
Although alcohol can be associated with ART nonadherence, the degree to which the detrimental effects of alcohol on adherence can be attributed to intentional nonadherence has not yet been studied in South Africa. The current research was undertaken to test the hypothesis that intentional nonadherence, as reflected in behaviors to avoid mixing alcohol with ART, would significantly contribute to the relationship between alcohol use and ART nonadherence. We performed a mediation analysis within a regression framework to test the direct and indirect effects of alcohol use and alcohol-ART avoidance behaviors on ART adherence among people who continue drinking after initiating ART.
Methods
Participants and Setting
The study was conducted in a resource constrained township in Cape Town, South Africa. We collected data at a public health clinic that has an ART dispensary and has instituted the South African national guidelines for shifting primary care tasks in a system of differentiated care. Because of the volume of patients receiving ART, the clinic provides minimal professional services to patients that are defined as stable; specifically, those patients who are HIV viral suppressed, have not been late to pick up their ART refills, and do not have a co-occurring clinical condition such as pregnancy or tuberculosis. Stable patients are administered ART through adherence clubs where they receive 3-month supplies of ART, have their viral load tested infrequently, and receive services from paraprofessionals. In contrast, patients who are not defined as stable (viral unsuppressed, late to pick up ART, have a co-occurring condition) receive their ART monthly, viral load monitored more frequently, and receive services from professional nurses and pharmacists. Instituting differentiated care, including adherence clubs, is intended to maximize the number of patients treated by diverting resources toward those patients in greatest need (Meyer-Rath et al., 2017; Mukumbang, Van Belle, Marchal, & Van Wyk, 2016). Participants in the current study were recruited while waiting for their ART to be dispensed and included persons who were in adherence clubs and not in adherence clubs.
Measures
Measures were collected in an anonymous self-administered survey presented in English and Xhosa, the two languages spoken by nearly all clinic patients. Participants were provided a survey and clipboard and were instructed to read each question and provide their responses. Participants requiring assistance due to literacy concerns (< 5%) were administered the survey in an interview by research staff. Measures included demographic and health characteristics, substance use, ART adherence, alcohol-ART interactive toxicity beliefs, and alcohol-ART avoidance behaviors. All measures were derived from previous studies on alcohol-ART intentional nonadherence and were pilot tested with native speakers for clarity and translation/back translation accuracy (Kalichman et al., 2013; Kalichman et al., 2015).
Demographic and health characteristics.
Participants reported their age, gender, race, level of formal education, and marital status. We also asked participants to indicate their perceived health status on a 4-point rating scale of physical well-being, ranging from 1 = ‘Poor’ to 4 = ‘Excellent’.
Alcohol and other drug use.
The three item Alcohol Use Disorder Identification Test - Consumption scale (AUDIT-C) assessed quantity and frequency of alcohol use (Maisto, Conigliaro, McNeil, Kraemer, & Kelley, 2000). This measure has been validated in South Africa and is recommended for screening for alcohol use in South African clinical settings (Babor, 2001; Parry et al., 2016; Saunders, Aasland, Babor, DeLaFuente, & Grant, 1993). Responses to the three items are summed to score the AUDIT-C. The AUDIT-C was reliable in the current sample, alpha = .89. For other drug use, participants were asked whether they had used cannabis (dagga), methamphetamine (Tik), inhalants, cocaine, or any other recreational drug in the previous month.
ART adherence.
This study used the three item self-report instrument for retrospective adherence (IRA) (Wilson et al., 2014).The items represent the number of days medications were taken over the previous 7 days, the frequency of taking medications as directed, and a self-perception rating of how well medications were taken over the previous week. The items therefore include an estimation of ART adherence. The three items as well as frequencies for responses are shown in the results. We used methods suggested by Wilson et al. to convert scores from each item on a scale of 0 to 100 using linear transformations and calculating the mean to a single adherence score with a range from 0 to 100, interpreted as percent adherence over the past week. Wilson et al. found that the IRA correlates .74 with electronically monitored ART adherence. In the current study the three transformed items created an internally consistent composite, alpha = .73.
Alcohol interactive toxicity beliefs and alcohol-ART avoidance.
We included two items to assess beliefs that people taking ART should not drink alcohol;
“Alcohol and ARV tablets should never be mixed” and “A person should stop taking their ARV tablets if they are drinking alcohol”, responded to on a 3-point scale of 0 = ‘Disagree’, 1 = ‘Somewhat Agree’, and 2 = ‘Agee’. We examined the rates of endorsement as defined by ‘Agree’ responses. To assess alcohol-related intentional nonadherence, participants responded to the item “I skip taking my ARV tablets because I will be drinking alcohol”, 0 = ‘Never’, 1 = ‘Sometimes’, and 2 = ‘Often’.
Data analyses
Descriptive analyses were performed for the entire sample of 441 participants attending the clinic ART dispensary and the model for our primary hypothesis was tested on the 293 participants reporting current alcohol use. For descriptive analyses, participants were grouped on the basis of their current alcohol use; no alcohol use (n = 148) and current alcohol use (n = 293). Descriptive analyses compared participants who were not drinking to those who were drinking alcohol using contingency table X2 tests for categorical variables and independent t-tests for continuous variables. Bivariate associations among variables included in the model were examined with Pearson correlation coefficients.
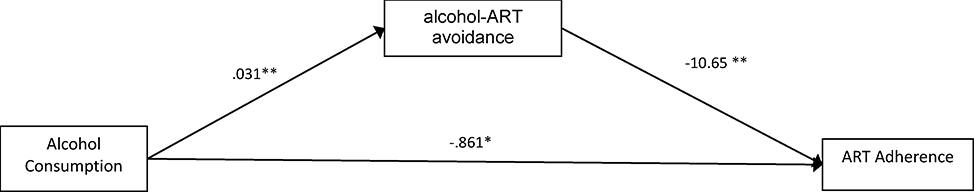
The main analyses tested the mediation model shown in Figure 1 that specifies the associations between alcohol use and ART adherence, mediated by alcohol-ART avoidance. We used the SPSS PROCESS macro for mediation analyses to test direct and indirect effects using bootstrap statistical techniques. The PROCESS macro estimates all paths designated in the model. Specifically, we used Hayes’ Template Model 4 for mediating an x – y relationship (Hayes, 2013). This model tests the effects of the predictor variable (alcohol use) on the mediator variable (alcohol-ART avoidance, representing the a path), the effects of the mediator variable on the outcome (ART adherence, representing the b path), and the effects of the predictor variable on the outcome (the c path). We report the 95% confidence intervals (CI) for the indirect effects of alcohol use on ART adherence through alcohol-ART avoidance estimated from 5,000 bootstrap resamples. We also performed sensitivity analyses by repeating the mediation model with participant’s age, gender, whether currently in an ART adherence club, and first versus second line therapy added as covariates to control for potential confounding. We conducted a post-hoc power analysis entering three model predictors, resulting effect size (R2), an error probability of .05 for a 2-tailed test. The result showed that we had observed power of .99 to detect model effects. There were no missing data for any variables included in the model.
Figure 1.
Mediation model of the effects of alcohol consumption on ART adherence through alcohol-ART avoidance.
Results
We surveyed 463 HIV positive patients, of which 441 (95%) were currently taking ART. Among those taking ART, a total of 293 (66%) participants reported current alcohol use and of those who drink alcohol, 41% drink monthly or less often, 37% 2–4 times a month, and 18% drink 2 or more times per week. In terms of quantity, 39% drink 1–2 drinks on a typical drinking occasion, 33% have 3–4 drinks, 18% have 5–6 drinks, and 7% have 7 or more drinks. Table 1 shows comparisons between the participants reporting no alcohol use and those currently using alcohol. Participants who reported drinking were significantly more likely to be men, unmarried, younger, and were more likely to use cannabis.
Table 1.
Characteristics of HIV positive clinic patients reporting no use and current use of alcohol.
| No Alcohol Use (N=149) | Alcohol Use (N=293) | |||||
|---|---|---|---|---|---|---|
| Characteristic | N | % | N | % | X2 | p |
| Men | 23 | 15 | 75 | 25 | ||
| Women | 126 | 84 | 218 | 75 | 5.9 | .01 |
| Black | 144 | 97 | 284 | 97 | n/a | |
| Age (M,SD) | 36.3 | 9.3 | 34.4 | 7.6 | 2.3 | .01 |
| Education < high school | 92 | 62 | 163 | 56 | ||
| ≥High school | 57 | 38 | 130 | 44 | 1.7 | .19 |
| Currently married | 40 | 27 | 34 | 11 | 16.4 | .01 |
| Physical health | ||||||
| Poor | 11 | 7 | 17 | 6 | ||
| Fair | 23 | 15 | 67 | 23 | ||
| Very good-Excellent | 115 | 78 | 209 | 71 | 3.7 | .15 |
| Cannabis | 7 | 5 | 38 | 13 | 7.3 | .01 |
| Methamphetamine (Tik) | 0 | 4 | 2 | n/a | ||
| Other drugs | 0 | 7 | 2 | n/a | ||
Alcohol use and antiretroviral therapy
Table 2 presents the HIV treatment characteristics of participants who did not and those who did report current alcohol use. There were no differences between the two groups in their taking single-tablet first line ART, frequency of dispensing ART, whether currently in an ART adherence club, and having talked about alcohol use with clinic staff. However, regarding indicators of ART adherence, alcohol drinkers demonstrated poorer adherence. Overall, alcohol drinkers had an estimated 75% ART adherence compared to 87% for nondrinkers, a significant difference. Three out of four participants agreed with the interactive toxicity belief that alcohol and ART should not be mixed and more than one in four agreed that a person should stop taking ART when drinking. Participants who reported no current alcohol use were more likely to endorse the belief that a person should stop taking ART when drinking. Among current alcohol drinkers, nearly one in four stated that they skip taking their ART when drinking.
Table 2.
ART adherence and adherence behaviors among HIV positive clinic patients reporting no use and current use of alcohol.
| No Alcohol Use (N=149) | Alcohol Use (N=293) | |||||
|---|---|---|---|---|---|---|
| Adherence behavior | N | % | N | % | X2 | p |
| Taking single tablet ART | 123 | 83 | 239 | 82 | 0.1 | .77 |
| Dispensed multiple months | 75 | 50 | 138 | 47 | 0.2 | .58 |
| Currently in adherence club | 92 | 62 | 176 | 60 | 0.1 | .86 |
| Discussed drinking while taking ART at clinic | 105 | 71 | 224 | 76 | 1.5 | .21 |
| Adherence | ||||||
| How many days did you miss taking your ART in past week? | ||||||
| 0 | 107 | 73 | 139 | 50 | ||
| 1–2 | 29 | 19 | 92 | 33 | ||
| 3–4 | 7 | 4 | 29 | 10 | ||
| 5–7 | 6 | 4 | 19 | 7 | 25.6 | .01 |
| How good a job have you done taking your ART in the past week? | ||||||
| Very poor | 6 | 4 | 11 | 4 | ||
| Poor | 1 | 1 | 12 | 4 | ||
| Fair | 16 | 11 | 29 | 10 | ||
| Good | 37 | 25 | 89 | 28 | ||
| Very good | 41 | 28 | 69 | 24 | ||
| Excellent | 48 | 32 | 86 | 30 | 5.3 | .37 |
| How often did you take your ART in the past week? | ||||||
| Did not take any | 1 | 1 | 9 | 3 | ||
| Took only a few | 14 | 9 | 21 | 7 | ||
| Took most | 39 | 27 | 93 | 32 | ||
| Every time, never missed | 95 | 64 | 170 | 58 | 6.6 | .15 |
| Total Adherence Score (M, SD) | 86.8 | 22.23 | 75.3 | 23.7 | 4.3 | .01 |
| Alcohol interactive toxicity beliefs | ||||||
| Alcohol and ART should never be mixed. | 112 | 75 | 203 | 70 | 2.4 | .30 |
| A person should stop taking ART when they are drinking alcohol. | 51 | 35 | 72 | 25 | 8.1 | .02 |
| Alcohol-ART avoidance | ||||||
| I Skip my ART tablets because I will be drinking alcohol | ||||||
| Never | 139 | 94 | 220 | 76 | ||
| Sometimes | 9 | 6 | 64 | 22 | ||
| Often | 0 | 5 | 2 | 21.9 | .01 | |
Mediation effects of alcohol-ART avoidance
For participants who were currently drinking alcohol, bivariate correlations among variables included in our regression model showed that alcohol consumption was negatively correlated with ART adherence, r = −.19, p = .01 and alcohol consumption was associated with alcohol-ART avoidance, r = .21, p = .01. Also, alcohol-ART avoidance was associated with ART adherence, r = −.26, p = .01. Results of the regression model predicting ART adherence from alcohol use mediated by alcohol-ART avoidance among participants reporting alcohol use are shown in Figure 1. Results indicated that the complete model was significant in predicting ART adherence, Model F = 20.71, p = .01, accounting for 8.7% of the variance in adherence. For tests of direct effects, results showed that alcohol consumption significantly predicted intentional nonadherence, β = 0.03, se =.006, t = 4.59, p = .01. In addition, alcohol-ART avoidance was significantly negatively related to ART adherence, β = −10.06, se = 2.11, t = 5.03, p = .01. The direct effect of greater alcohol consumption predicting poorer ART adherence was statistically significant, β = −0.861, se = .303, t = 2.83, p = .04. The mediation effect of alcohol-ART avoidance was tested using 5,000 bootstrap resamples and showed a significant indirect effect of alcohol consumption on ART adherence through alcohol-ART avoidance, β = −.32, se = .133, 95%CI −.627 - −.104.
Sensitivity analysis
To test the robustness of our findings, we re-tested the model controlling for four potential confounding variables: participant age, gender, current ART adherence club status, and first versus second line therapy. Results mirrored those reported in the unadjusted model. The model with covariates was significant, F = 12.03, p = .01, accounting for 14.7% of the variance in adherence. All direct effects paths remained significant as did the indirect effect
Discussion
Results showed that two-thirds of people receiving ART in a Cape Town community clinic reported current alcohol use. Alcohol use varied from infrequent and modest drinking to frequent heavy use. Patients who drank were younger, more likely unmarried, and reported recent use of cannabis. These rates of alcohol consumption are themselves concerning because alcohol use has the potential to cause health complications in people living with HIV aside from the effects of alcohol use on adherence (Hahn & Samet, 2010). Consistent with previous research (Hendershot et al. 2009; Kekwaletswe & Morojele, 2014a), we found that participants who drank alcohol had significantly poorer ART adherence. While current ART regimens no longer demand nearly perfect adherence, even the most forgiving ART regimens will not sustain HIV suppression with less than 75% of medications taken (Gordon, Gharibian, Chong, & Chun, 2015; Kimulwo et al., 2017). Previous qualitative research in southern Africa suggested that alcohol-related intentional nonadherence may be common (Fatch et al., 2017), as confirmed in the current study. We found that among participants who were currently drinking alcohol, nearly one in four skips taking their ART when drinking; a similar rate of intentional nonadherence that has been reported in the US and Europe (Boretzki et al., 2017; Kalichman et al., 2012; Kalichman et al., 2009; Kalichman et al., 2013; Kalichman et al., 2015).
We confirmed our primary hypothesis that alcohol-ART avoidance would partially account for the relationship between alcohol consumption and ART nonadherence. While it is not surprising that alcohol-ART avoidance would have a direct effect on ART nonadherence, no previous study has shown that the degree of alcohol-ART avoidance is substantial enough to mediate the association between alcohol use and nonadherence. The results accounted for unintentional nonadherence embedded within the adherence measure. These findings show that alcohol-ART avoidance among alcohol drinkers in South Africa is significant and an essential target for ART adherence interventions.
The current findings should be considered in light of the study limitations. This study relied on self-report measures of alcohol use and ART adherence, both of which are sensitive to social response biases. With respect to alcohol use, it is well-known that self-reported alcohol use tends to be under-reported and therefore under-estimates drinking (Bajunirwe et al., 2014). Our findings therefore should be considered a lower-bound estimate of alcohol use among people living with HIV who are receiving ART in South Africa. For ART adherence, self-report measures have the opposite reporting bias, resulting in over-reporting adherence (Pearson, Simoni, Hoff, Kurth, & Martin, 2007). Thus, our measure of ART adherence should be considered an upper-bound estimate. Our measures were also short in terms of number of items, which may have affected their reliability. We did not have access to clinical records or other reliable medical data concerning health status, particularly HIV viral load. Future research should include clinical data. Our sample was one of convenience and cannot be considered representative of people receiving ART in South Africa. With these limitations in mind, we believe that the current study has implications for addressing alcohol use in ART adherence interventions.
The reliable detrimental effects of alcohol consumption on ART have been answered with interventions focused on reducing alcohol use and efforts to resolve alcohol-related unintentional nonadherence (Kekwaletswe & Morojele, 2014a, 2014b; Parry et al., 2014). One cluster randomized trial, for example, is being conducted at 16 HIV clinics in Zimbabwe using evidence-based treatments grounded in cognitive-behavior therapy and motivational interviewing to reduce alcohol use to improve HIV care engagement and clinical outcomes (Madhombiro et al., 2017). Other trials are testing adherence interventions which include memory aides and medication management skills that can be impaired when drinking (Madhombiro et al., 2017; Peltzer et al., 2012). Studies show that cognitive behavioral interventions for alcohol use are cost-effective in southern Africa (Galarraga et al., 2017). The degree to which existing interventions directly address alcohol-related intentional nonadherence is uncertain. Providers should directly address alcohol-ART interactive toxicity beliefs that motivate alcohol-ART avoidance. Corrective information offered in interventions should avoid reinforcing alcohol use while emphasizing the essential importance of taking ART even when drinking. Existing interventions should assist patients in managing their ART when drinking, including correcting interactive toxicity beliefs and counseling against intentional nonadherence. Interventions aimed toward improving ART adherence will be enhanced by directly addressing alcohol use as a source of intentional as well unintentional nonadherence.
References
- Babor T, Higgins-Biddle J, Saunders J, Monteiro M (2001). The Alcohol Use Disorders Identification Test: Guidelines for use inprimary Care, 2nd Edtion. Geneva, Switzerland: World Health Organization [Google Scholar]
- Bajunirwe F, Haberer JE, Boum Y 2nd, Hunt P, Mocello R, Martin JN, … Hahn JA (2014). Comparison of self-reported alcohol consumption to phosphatidylethanol measurement among HIV-infected patients initiating antiretroviral treatment in southwestern Uganda. PLoS One, 9(12), e113152. doi: 10.1371/journal.pone.0113152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boretzki J, Wolf E, Wiese C, Noe S, Balogh A, Meurer A, … Spinner CD (2017). Highly specific reasons for nonadherence to antiretroviral therapy: results from the German adherence study. Patient Prefer Adherence, 11, 1897–1906. doi: 10.2147/PPA.S141762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conroy AA, McKenna SA, Leddy A, Johnson MO, Ngubane T, Darbes LA, & van Rooyen H (2017). “If She is Drunk, I Don’t Want Her to Take it”: Partner Beliefs and Influence on Use of Alcohol and Antiretroviral Therapy in South African Couples. AIDS Behav, 21(7), 1885–1891. doi: 10.1007/s10461-017-1697-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denison JA, Packer C, Stalter RM, Banda H, Mercer S, Nyambe N, … McCarraher DR (2018). Factors Related to Incomplete Adherence to Antiretroviral Therapy among Adolescents Attending Three HIV Clinics in the Copperbelt, Zambia. AIDS Behav, 22(3), 996–1005. doi: 10.1007/s10461-017-1944-x [DOI] [PubMed] [Google Scholar]
- Fatch R, Emenyonu NI, Muyindike W, Kekibiina A, Woolf-King S, & Hahn JA (2017). Alcohol Interactive Toxicity Beliefs and ART Nonadherence Among HIV-Infected Current Drinkers in Mbarara, Uganda. AIDS Behav, 21(7), 1812–1824. doi: 10.1007/s10461-016-1429-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fritz K, Morojele N, & Kalichman S (2010). Alcohol: the forgotten drug in HIV/AIDS. Lancet, 376(9739), 398–400. doi: 10.1016/S0140-6736(10)60884-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galarraga O, Gao B, Gakinya BN, Klein DA, Wamai RG, Sidle JE, & Papas RK (2017). Task-shifting alcohol interventions for HIV+ persons in Kenya: a cost-benefit analysis. BMC Health Serv Res, 17(1), 239. doi: 10.1186/s12913-017-2169-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon LL, Gharibian D, Chong K, & Chun H (2015). Comparison of HIV Virologic Failure Rates Between Patients with Variable Adherence to Three Antiretroviral Regimen Types. AIDS Patient Care STDS, 29(7), 384–388. doi: 10.1089/apc.2014.0165 [DOI] [PubMed] [Google Scholar]
- Hahn JA, Emenyonu NI, Fatch R, Muyindike WR, Kekiibina A, Carrico AW, … Shiboski S (2016). Declining and rebounding unhealthy alcohol consumption during the first year of HIV care in rural Uganda, using phosphatidylethanol to augment self-report. Addiction, 111(2), 272–279. doi: 10.1111/add.13173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hahn JA, Fatch R, Wanyenze RK, Baveewo S, Kamya MR, Bangsberg DR, & Coates TJ (2014). Decreases in self-reported alcohol consumption following HIV counseling and testing at Mulago Hospital, Kampala, Uganda. BMC Infect Dis, 14, 403. doi: 10.1186/1471-2334-14-403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hahn JA, & Samet JH (2010). Alcohol and HIV disease progression: weighing the evidence. Curr HIV/AIDS Rep, 7(4), 226–233. doi: 10.1007/s11904-010-0060-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF (2013). Model Templates for PROCESS for SPSS and SAS: Guilford Press. [Google Scholar]
- Heestermans T, Browne JL, Aitken SC, Vervoort SC, & Klipstein-Grobusch K (2016). Determinants of adherence to antiretroviral therapy among HIV-positive adults in sub-Saharan Africa: a systematic review. BMJ Glob Health, 1(4), e000125. doi: 10.1136/bmjgh-2016-000125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendershot CS, Stoner SA, Pantalone DW, & Simoni JM (2009). Alcohol use and antiretroviral adherence: review and meta-analysis. J Acquir Immune Defic Syndr, 52(2), 180–202. doi: 10.1097/QAI.0b013e3181b18b6e [DOI] [PMC free article] [PubMed] [Google Scholar]
- HIV.gov. (2018). The Global HIV/AIDS Epidemic. Retrieved from https://www.hiv.gov/hiv-basics/overview/data-and-trends/global-statistics
- Kalichman SC, Amaral CM, White D, Swetsze C, Kalichman MO, Cherry C, & Eaton L (2012). Alcohol and Adherence to Antiretroviral Medications: Interactive Toxicity Beliefs Among People Living With HIV. J Assoc Nurses AIDS Care. doi: 10.1016/j.jana.2011.11.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman SC, Amaral CM, White D, Swetsze C, Pope H, Kalichman MO, … Eaton L (2009). Prevalence and clinical implications of interactive toxicity beliefs regarding mixing alcohol and antiretroviral therapies among people living with HIV/AIDS. AIDS Patient Care STDS, 23(6), 449–454. doi: 10.1089/apc.2008.0184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman SC, Grebler T, Amaral CM, McNerey M, White D, Kalichman MO, … Eaton L (2013). Intentional nonadherence to medications among HIV positive alcohol drinkers: prospective study of interactive toxicity beliefs. J Gen Intern Med, 28(3), 399–405. doi: 10.1007/s11606-012-2231-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman SC, Kalichman MO, Cherry C, Hoyt G, Washington C, Grebler T, … Merely C (2015). Intentional Medication Nonadherence Because of Interactive Toxicity Beliefs Among HIV-Positive Active Drug Users. J Acquir Immune Defic Syndr, 70(5), 503–509. doi: 10.1097/QAI.0000000000000776 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kekwaletswe CT, & Morojele NK (2014a). Alcohol use, antiretroviral therapy adherence, and preferences regarding an alcohol-focused adherence intervention in patients with human immunodeficiency virus. Patient Prefer Adherence, 8, 401–413. doi: 10.2147/PPA.S55547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kekwaletswe CT, & Morojele NK (2014b). Patterns and predictors of antiretroviral therapy use among alcohol drinkers at HIV clinics in Tshwane, South Africa. AIDS Care, 26 Suppl 1, S78–82. doi: 10.1080/09540121.2014.906558 [DOI] [PubMed] [Google Scholar]
- Kim MH, Mazenga AC, Yu X, Ahmed S, Paul ME, Kazembe PN, & Abrams EJ (2017). High self-reported nonadherence to antiretroviral therapy amongst adolescents living with HIV in Malawi: barriers and associated factors. J Int AIDS Soc, 20(1), 21437. doi: 10.7448/IAS.20.1.21437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimulwo MJ, Okendo J, Aman RA, Ogutu BR, Kokwaro GO, Ochieng DJ, … Ochieng W (2017). Plasma nevirapine concentrations predict virological and adherence failure in Kenyan HIV-1 infected patients with extensive antiretroviral treatment exposure. PLoS One, 12(2), e0172960. doi: 10.1371/journal.pone.0172960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madhombiro M, Dube-Marimbe B, Dube M, Chibanda D, Zunza M, Rusakaniko S, … Seedat S (2017). A cluster randomised controlled trial protocol of an adapted intervention for alcohol use disorders in people living with HIV and AIDS: impact on alcohol use, general functional ability, quality of life and adherence to HAART. BMC Psychiatry, 17(1), 44. doi: 10.1186/s12888-017-1208-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maisto SA, Conigliaro J, McNeil M, Kraemer K, & Kelley ME (2000). An empirical investigation of the factor structure of the AUDIT. Psychol Assess, 12(3), 346–353. [DOI] [PubMed] [Google Scholar]
- Meyer-Rath G, Johnson LF, Pillay Y, Blecher M, Brennan AT, Long L, … Rosen S (2017). Changing the South African national antiretroviral therapy guidelines: The role of cost modelling. PLoS One, 12(10), e0186557. doi: 10.1371/journal.pone.0186557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mukumbang FC, Van Belle S, Marchal B, & Van Wyk B (2016). Realist evaluation of the antiretroviral treatment adherence club programme in selected primary healthcare facilities in the metropolitan area of Western Cape Province, South Africa: a study protocol. BMJ Open, 6(4), e009977. doi: 10.1136/bmjopen-2015-009977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nkosi S, Rich EP, Kekwaletswe CT, & Morojele NK (2016). Experiences of alcohol consumption and taking antiretroviral medication among men living with HIV in Tshwane, South Africa. Afr J AIDS Res, 15(4), 367–376. doi: 10.2989/16085906.2016.1255651 [DOI] [PubMed] [Google Scholar]
- Parry CD, Kekwaletswe C, Shuper PA, Nkosi S, Myers BJ, & Morojele NK (2016). Heavy alcohol use in patients on highly active antiretroviral therapy: What responses are needed? S Afr Med J, 106(6), 43–44. doi: 10.7196/SAMJ.2016.v106i6.10639 [DOI] [PubMed] [Google Scholar]
- Parry CD, Morojele NK, Myers BJ, Kekwaletswe CT, Manda SO, Sorsdahl K, … Shuper PA (2014). Efficacy of an alcohol-focused intervention for improving adherence to antiretroviral therapy (ART) and HIV treatment outcomes - a randomised controlled trial protocol. BMC Infect Dis, 14, 500. doi: 10.1186/1471-2334-14-500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson CR, Simoni JM, Hoff P, Kurth AE, & Martin DP (2007). Assessing antiretroviral adherence via electronic drug monitoring and self-report: an examination of key methodological issues. AIDS Behav, 11(2), 161–173. doi: 10.1007/s10461-006-9133-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pellowski JA, Kalichman SC, Kalichman MO, & Cherry C (2016). Alcohol-antiretroviral therapy interactive toxicity beliefs and daily medication adherence and alcohol use among people living with HIV. AIDS Care, 28(8), 963–970. doi: 10.1080/09540121.2016.1154134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peltzer K, Ramlagan S, Jones D, Weiss SM, Fomundam H, & Chanetsa L (2012). Efficacy of a lay health worker led group antiretroviral medication adherence training among nonadherent HIV-positive patients in KwaZulu-Natal, South Africa: results from a randomized trial. SAHARA J, 9(4), 218–226. doi: 10.1080/17290376.2012.745640 [DOI] [PubMed] [Google Scholar]
- Santos GM, Emenyonu NI, Bajunirwe F, Rain Mocello A, Martin JN, Vittinghoff E, … Hahn JA (2014). Self-reported alcohol abstinence associated with ART initiation among HIV-infected persons in rural Uganda. Drug Alcohol Depend, 134, 151–157. doi: 10.1016/j.drugalcdep.2013.09.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, DeLaFuente JR, & Grant M (1993). Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption II. Addictions, 88(6), 791–804. [DOI] [PubMed] [Google Scholar]
- Shubber Z, Mills EJ, Nachega JB, Vreeman R, Freitas M, Bock P, … Ford N (2016). Patient-Reported Barriers to Adherence to Antiretroviral Therapy: A Systematic Review and Meta-Analysis. PLoS Med, 13(11), e1002183. doi: 10.1371/journal.pmed.1002183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simoni JM, Amico KR, Pearson CR, & Malow R (2008). Strategies for promoting adherence to antiretroviral therapy: a review of the literature. Curr Infect Dis Rep, 10(6), 515–521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simoni JM, Pearson CR, Pantalone DW, Marks G, & Crepaz N (2006). Efficacy of interventions in improving highly active antiretroviral therapy adherence and HIV-1 RNA viral load. A meta-analytic review of randomized controlled trials. J Acquir Immune Defic Syndr, 43 Suppl 1, S23–35. doi: 10.1097/01.qai.0000248342.05438.5200126334-200612011-00005 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNAIDS. (2014). 90–90-90: An ambitious treatment target to help end the AIDS epidemic. UNAIDS; Retrieved from http://www.unaids.org/sites/default/files/media_asset/90-90-90_en.pdf [Google Scholar]
- UNAIDS. (2017). Global AIDS monitoring 2017: UNAIDS Data. Retrieved from http://www.unaids.org/sites/default/files/media_asset/20170720_Data_book_2017_en.pdf
- Veld DHI, Pengpid S, Colebunders R, Skaal L, & Peltzer K (2017). High-risk alcohol use and associated socio-demographic, health and psychosocial factors in patients with HIV infection in three primary health care clinics in South Africa. Int J STD AIDS, 28(7), 651–659. doi: 10.1177/0956462416660016 [DOI] [PubMed] [Google Scholar]
- Wilson IB, Fowler FJ Jr., Cosenza CA, Michaud J, Bentkover J, Rana A, … Rogers WH (2014). Cognitive and field testing of a new set of medication adherence self-report items for HIV care. AIDS Behav, 18(12), 2349–2358. doi: 10.1007/s10461-013-0610-1 [DOI] [PMC free article] [PubMed] [Google Scholar]