Abstract
Objective:
Many combat veterans struggle with Posttraumatic Stress Disorder (PTSD) and hazardous alcohol use and are hesitant to engage in behavioral health services. Combining peer support with an eHealth intervention may overcome many barriers to care. This pilot study investigated the feasibility of adding peer support to a web-based cognitive behavior therapy (CBT) targeting PTSD symptoms and hazardous drinking, called Thinking Forward.
Method:
Thirty primary care patients with PTSD and hazardous alcohol use were randomized to receive Thinking Forward with or without peer support. Participants were assessed at pre-treatment, post-treatment and 24-week follow-up. Feasibility was analyzed with descriptive statistics. Preliminary outcomes were analyzed with multilevel modeling and effect sizes are presented.
Results:
Peer support specialists can be feasibly trained to support the Thinking Forward intervention with good fidelity. Both participants and peers reported good satisfaction with the protocol; although peers discussed a mismatch between the philosophies of peer support and diagnostically-focused CBT. All participants experienced significant improvements in PTSD, quality of life, resiliency, and coping from pre-to-post treatment, with no differences between conditions. Pre-treatment patient activation predicted outcomes regardless of whether participants received peer support.
Conclusions and Implications for Practice:
Peer support interventions to facilitate eHealth programs should strive to be consistent with the person-centered, recovery orientation of peer support, explicitly focus on patient activation, and consider characteristics of the patients, such as their level of problem recognition and willingness to engage in traditional behavioral health modalities.
Keywords: Peer Support, ehealth, primary care- mental health integration, PTSD, hazardous alcohol use
Veterans who fought in recent wars in Iraq and Afghanistan have high rates of Posttraumatic Stress Disorder (PTSD) and hazardous alcohol use. Co-occurring PTSD and hazardous drinking is related to negative outcomes, including relationship concerns, depression, functional health impairments, and aggression (Blow et al., 2013; McDevitt‐Murphy et al., 2010; Owens et al., 2014). Several evidence-based PTSD and substance use disorder treatments are available (VA/DOD, 2017; VA/DOD, 2015). However, engagement and retention in these treatments are significant problems. For example, among Veterans with a new diagnosis of PTSD, only 34% initiate psychotherapy and only 9% receive eight or more sessions (Mott, Hundt, Sansgiry, Mignogna, & Cully, 2014). Only 4% of Veterans who screen positive for hazardous alcohol use receive any substance use treatment within one year (Glass et al., 2010). Given the high potential for negative outcomes and poor treatment engagement among Veterans with PTSD and hazardous alcohol use, novel strategies for engaging Veterans in treatment are warranted.
Peer support services are a recovery-oriented and patient-centered approach being implemented within the Veterans Health Administration (VHA) to engage Veterans in care. Peer support is when an individual is trained to use his or her own lived experience with mental health recovery to help others. Research demonstrates that adding peers to existing clinical services is associated with improved treatment engagement, motivation for treatment, social functioning, and quality of life (Chinman et al., 2014). The few studies that have evaluated peer support services specifically for substance use showed positive findings (e.g., reduced relapse rates, increased treatment retention, and increased treatment satisfaction) (Bassuk, Hanson, Greene, Richard, & Laudet, 2016; Reif et al., 2014). Preliminary research supports the feasibility of two peer outreach programs for Veterans to increase treatment engagement in PTSD services (Jain, Hernandez, & Lindley, 2014; Joseph, Hernandez, & Jain, 2015). Qualitative feedback from Veterans with PTSD suggests that peer support can be used to increase PTSD treatment initiation and retention, increase social support, and normalize symptoms (Hundt, Robinson, Arney, Stanley, & Cully, 2015). To date, no published research has focused on delivering peer support to individuals with co-occurring PTSD and hazardous alcohol use.
There is a growing movement to increase the reach of peer support beyond traditional mental health settings to new settings, such as primary care (Daaleman & Fisher, 2015; Swarbrick, Tunner, Miller, Werner, & Tiegreen, 2016). Peer services helping patients manage physical health concerns are effective, especially when they focus on peer navigation and supporting self-management interventions (Cabassa, Camacho, Vélez-Grau, & Stefancic, 2017). In line with VHA’s commitment to providing mental health services within primary care (Kearney, Post, Zeiss, Goldstein, & Dundon, 2011), a 2014 Executive Order assigned peer support specialists to 25 VHA primary care clinics and the implementation of these peers into primary care is being evaluated (Chinman et al., 2017). However, very little is known about what peer services may be most helpful for primary care patients with mental health and substance use concerns. Research investigating the efficacy of peer-delivered programs in primary care is needed.
Peer support is also being extended to facilitate engagement and retention in technology-based or eHealth interventions. While eHealth interventions generally broaden reach of behavioral health services, evidence suggests that users may be unlikely to follow-through on engagement with these services (Mohr, Burns, Schueller, Clarke, & Klinkman., 2013). Adding human support is one of the strategies that has been proposed for addressing this concern (Mohr, Cuijpers, & Lehman, 2011). In fact, one research group that examined a variety of disorders, found that, although self-help interventions can be efficacious, therapist-assisted eHealth treatments demonstrate better treatment outcomes (Newman, Szkodny, Llera, & Przeworski, 2011a, 2011b). Research has also investigated the combination of peer support and web-based therapies for depression and bipolar disorders. These approaches appear highly feasible and show evidence of better treatment adherence, but their efficacy to reduce symptoms warrants further study (Nelson, Abraham, Walters, Pfeiffer, & Valenstein, 2014; Proudfoot et al., 2012).
The parent trial for the current project was a test of a 12-week self-guided, structured web-based intervention, Thinking Forward, for Iraq/ Afghanistan War Veterans with PTSD and hazardous substance use enrolled in VHA primary care (Acosta et al., 2017; Possemato et al., 2015). Veterans were randomized to either receive Thinking Forward or primary care treatment as usual (TAU). Veterans who received Thinking Forward demonstrated significantly larger decreases in heavy drinking compared to those in TAU. The reduction in drinking was mediated by increased social support, self-efficacy, and hope for the future. Veterans in both conditions reported reductions in PTSD severity and improvement in quality of life (Acosta et al., 2017). Qualitative analysis of feedback among Thinking Forward participants indicated that Veterans would have liked more interpersonal contact and support from a healthcare provider or other Veterans with similar experiences while completing the program. These results, coupled with the previously reviewed literature on peer support, led us to develop and preliminarily test a program that combines peer support with Thinking Forward with the goals of increasing patients’ engagement in the web-based treatment and boosting patient outcomes in the areas of hazardous alcohol use, PTSD severity, and quality of life.
The primary aim of this pilot study was to evaluate the feasibility of adding peer support to Thinking Forward. To fully describe our pilot data we also present outcome measure means at pre-treatment and post-treatment and follow-up, the results of significance testing, and effect sizes. We hypothesized that Veterans receiving Peer-Supported Thinking Forward would demonstrate increases in treatment engagement and quality of life, and reduced problematic symptoms compared to veterans who had access to Thinking Forward without peer support.
Method
Participants.
To be included in the study, participants had to be VHA primary care patients and Iraq/ Afghanistan War Veterans. Participants also needed hazardous alcohol use and to have either diagnostic-level PTSD or subthreshold PTSD (criterion A traumatic stressor plus 1 re-experiencing B symptom plus 3 avoidance C symptoms OR 2 arousal D symptoms) from DSM-IV criteria (Schnurr, Lunney, Sengupta, & Spiro, 2005). Patients were excluded if they were enrolled in psychotherapy in the previous two months; had a change in any psychiatric medications in the last two months; or had a current plan or intent to harm themselves.
Procedures.
Veterans were referred by primary care providers. Referred patients were sent a letter, then contacted by study staff via phone and invited to come to the VA for a baseline interview. At the baseline interview, informed consent was obtained and eligibility was assessed. Eligible participants were randomly assigned to Self-Managed Thinking Forward or Peer-Supported Thinking Forward. Permuted-blocks randomized participants based on whether they met DSM-IV criteria for a current substance use disorder and diagnostic vs. subthreshold PTSD. Participants were assessed at pre-treatment, post-treatment and 24 week follow-up. Participants were compensated for the time they spent completing assessments at a rate of $25/ hour. Participants were not compensated for completing treatment modules or attending peer support sessions. The pilot trial was registered at ClinicalTrials.gov (NCT0261183) and was approved by the local VHA institutional review board.
Measures.
Three measures assessed eligibility and baseline health status. The Clinical Administered PTSD Scale (CAPS) assessed the 17 core symptoms of PTSD as defined in the DSM-IV in an interview format (Blake et al., 1995). The CAPS is reliable and has excellent diagnostic utility. This measure verified the presence of a criterion A traumatic event and documented rates of full and subthreshold PTSD. The CAPS was used instead of the newer CAPS-5, to keep all assessments the same between the parent trial and the current pilot trial to allow direct comparison. All interviewers were trained and supervised by a licensed psychologist. The Alcohol Use Disorders Identification Test (AUDIT) (Babor, Higgins-Biddle, Saunders, & Monteiro, 2001) screened for hazardous alcohol use at baseline. Patients had to score 8 or higher for men and 7 or higher for women to be eligible. The AUDIT is reliable, valid, and had acceptable internal consistency in this study (α=.75). The MINI International Neuropsychiatric Interview (MINI) assessed for DSM-IV substance use disorders and was administered in a computerized, self-report format. The MINI has comparable validity to well-established structured clinical interviews (Sheehan, 2004).
Three measures assessed the primary study outcomes and were administered at each time point. The Timeline Follow-Back (TLFB) interview assessed self-reported substance use using calendars to record daily alcohol use in standardized drink quantities for the previous 90 days at baseline and since the last assessment at follow-ups. Primary outcomes derived were drinking days and heavy drinking days. The TLFB has good test-retest reliability and high content, criterion, and construct validity across multiple related measures (Sobell & Sobell, 2000). The PTSD Checklist- Military (PCL-M) asked respondents to self-report how much they have been bothered by 17 PTSD symptoms in the past month on a 5-point scale. The PCL-M is reliable, valid (Weathers & Ford, 1996), and had good internal consistency in this study (α=.76). The total score was the primary PTSD outcome. The WHOQOL-BREF measured quality of life (QOL) with 26-items assessing the broad domains of physical health, psychological health, social relationships, and environmental factors (Murphy, Herrman, Hawthorne, Pinzone, & Evert, 2000). This measure is reliable, valid, and has good internal consistency in this study (α=.85). The psychological and social domain scores were the QOL outcome measures.
Other self-report measures administered include the Patient Activation Measure for Mental Health (PAM-MH) which assessed patients’ knowledge about mental health, beliefs about illness and healthcare, and self-efficacy to initiate and receive care. It has good test-retest reliability and strong concurrent validity (Green et al., 2010). The 23-item Coping Strategies Scale (CSS) (Litt, Kadden, Cooney, & Kabela, 2003) assessed change processes and skills taught in coping skills treatment, such as problem solving and resisting urges to use substances. This measure has good predictive validity, as total coping skills has been found to be related to reduced drinking (Litt et al., 2003) and good internal consistency reliability in this sample (.87). The Connor-Davidson Resilience Scale (CD-RISC) measured resiliency, with 25-items. The scale has high test-retest reliability, convergent validity, and discriminant validity (Connor & Davidson, 2003). Internal consistency reliability in this sample was good at .88. The Peer Support Feedback Questionnaire was developed for the current project and administered at post-treatment. The Patient version incorporated the 8-items from the Client Satisfaction Questionnaire (CSQ), which assessed the participant’s perception of the value of services. The CSQ has good test-retest reliability and higher satisfaction is correlated to more service use and positive clinical outcomes (Attkisson & Zwick, 1982). The Patient and Peer versions both asked respondents to rate how helpful specific components of peer support were, select optimal frequency of visits, rate if the treatment was flexible to patient needs, and provide open-ended feedback on what they like least and most about the treatment. The Peer version also inquired about ease of delivery.
Intervention.
Self-Managed Thinking Forward participants had access to Thinking Forward which consisted of 24 brief (20-minute) online modules. Participants were asked to complete two modules per week. During the baseline research session, staff ensured that participants knew how to access the content. Research staff did not provide any support for completing the modules but did contact participants who were not regularly completing modules with reminder calls. Modules were self-guided and topics included “The Connection Between PTSD and Substance Use”, “Motivational Enhancement”, “Relaxation”, “Identifying, Evaluating and Challenging Automatic Thoughts”, “Functional Analyses of Substance Use”, and “Substance Use Refusal Skills”. Modules included interactive exercises and veteran stories that illustrate common symptoms and healthy coping strategies. (See Possemato et al. (2015) and Acosta et al. (2017) for detailed descriptions of the web-based program).
Peer-Supported Thinking Forward participants had access to the Thinking Forward online content and were assigned a peer support specialist. The first peer support meeting was in-person, with subsequent meetings delivered either in-person or by phone, depending on patient preference. Peers were asked to meet with participants weekly for about 20 minutes for the 12 weeks of treatment. However, consistent with typical peer support services, session length and frequency was flexible to be responsive to patient needs.
Peer services were guided by the Thinking Forward Peer Support Guide created by study authors. Primary components of the Guide included: 1) introducing Thinking Forward and teaching basic skills on how to access and use the program, 2) discussing the peer’s own recovery story as appropriate, 3) inviting participants to discuss their challenges and changes they would like to make in their lives and to set obtainable and measurable recovery goals, 4) discussing how specific modules can help patients’ specific problems (i.e., personalize Thinking Forward for the Veteran), 5) encouraging module completion and practicing skills along with other healthy behaviors, as directed by the patient’s interests and goals, 6) engaging patients in discussions about Thinking Forward content and helping them apply it to their lives (the Guide includes scripted discussion questions for each module to guide the peer in these discussions), and 7) facilitating engagement in additional mental health and substance use services following completion of 12 weeks of Thinking Forward, as needed, depending on patient symptoms and concerns. The Guide also includes simple session checklists to ensure peers have covered important topics.
Two VA certified peer support specialists served as peers in this study. One peer typically provided services in primary care and one typically provided services in the PTSD and substance use clinics. Prior to the study, peers received 13 hours of study-specific training over 10 weeks in addition to navigating through all the Thinking Forward online content. Training focused on reviewing major content areas of the online material and the Guide and role-playing session content. Peers received weekly group supervision and session recordings were reviewed for fidelity by their supervisor using a fidelity checklist created for this study. Four session components were evaluated on a three-point scale. The highest rating for each component is described here: 1) General Check-in was conducted with a targeted follow-up, 2) Discussed personalized Recovery Goals by setting an obtainable and measureable goal or having an in depth discussion of progress achieving goals including barriers/ facilitators, 3) Tailored Thinking Forward Content to the Veteran’s concerns and experiences navigating the modules, and 4) Developed a tailored Action Plan including how to apply skills learned in Thinking Forward to achieve recovery goals.
Analyses.
Feasibility was assessed with several metrics recommended by Leon, Davis, and Kraemer (2011) using descriptive statistics. A general inductive method was used to organize and interpret the small amount of qualitative data collected on participant and peer surveys (Thomas, 2006). Quotes were chosen to reflect the breadth and depth of qualitative feedback provided. This study was not adequately powered to detect between group differences in outcomes. However, in order to fully describe our pilot data we present outcome measure means at each assessment point, the results of significance testing, and effect sizes. Multi-level models (MLM) investigated changes in patient outcomes from pre to post treatment. Specifically, piecewise linear models were used to track data patterns that initially improved at a higher rate but then leveled out as the study period progressed (Neter, Wasserman, & Kutner, 1990). Scatter and mean plots, and the Bayesian Information Criterion were used to access and compare model fit (Schwartz & Gideon, 1978). Cohen’s d effect sizes with 95% confidence intervals were estimated for pre to post changes in the Peer Support condition and between group changes. In MLM, participants are not removed from the analysis for missing values and unbiased parameter estimates are provided for data missing at random (Diggle, Liang, & Zeger, 1991). Participants with missing data were compared to those without missing data on baseline characteristics using t-tests. No meaningful differences were found, supporting a missing at random assumption.
Results
Socio-demographic and clinical characteristics of participants (N=30) are in Table 1. The sample was mostly male and White with an average age of 39 years old. Figure 1 details the flow of the forty patients screened in-person. Thirty participants were recruited over 11 months, averaging 2.7 eligible participants per month. Intervention retention was 93% for Peer Support and 73% for Self-Managed. Assessment retention was 60% for Peer Support and 73% for Self-Managed. Randomization assignment was unrelated to average number of completed modules (t= .18, p=.86) (Peer Support mean= 11.13 (7.76), mode= 8, 24, Self-Managed mean= 10.60 (8.07), mode= 0) and assessment retention (Figure 1, X2= .60, p=.44). Peer Support participants attended an average of 5.63 peer sessions (SD=3.59, range= 2–13). Peer sessions were an average of 46.90 minutes long (SD=15.73, range=22–67 minutes) and 71% were completed in-person (29% via phone). Peer sessions were rated for fidelity to the Peer Guide. On average, peers scored 5.77 points (SD= 1.59, range 3–8). Peers averaged higher ratings for discussing how to apply Thinking Forward content and lowest for conducting a targeted check-in at the beginning of each session. Optional items on the fidelity checklist that were commonly endorsed include peer self-disclosure and encouragement of healthy behaviors.
Table 1.
Socio-demographic and Clinical Characteristics of Participants (N=30)
| Characteristic | n (%) | mean (SD) |
|---|---|---|
| Male | 28 (93) | |
| White Race | 24 (80) | |
| Age | 39 years (9) | |
| Married | 17 (57) | |
| Education post High School | 17 (57) | |
| Average Family Income | $59,000 ($34,000) | |
| Served in Army | 22 (73) | |
| Diagnostic-level PTSD | 18 (60) | |
| Current Alcohol Use Disorder | 12 (40) | |
| Current Substance Use Disorder (other than alcohol) |
0 (0) | |
Figure 1:
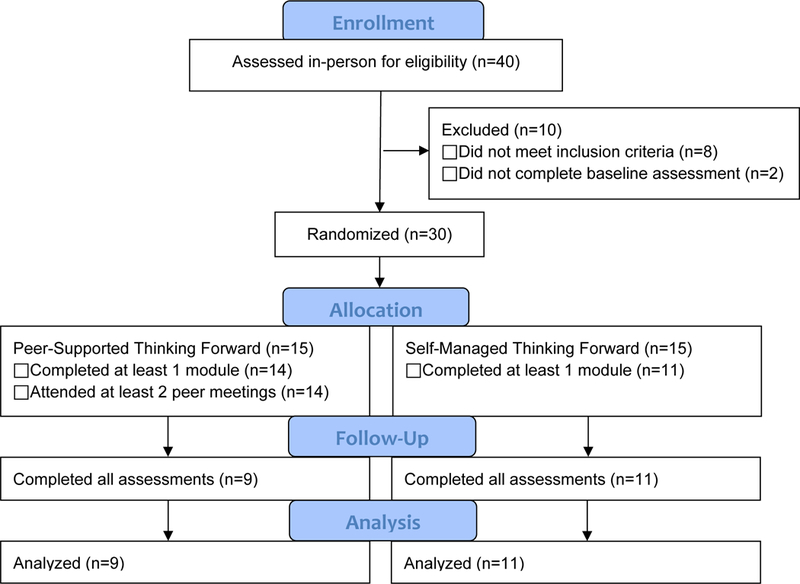
Consort Flow Diagram
Figure 2 provides a summary of participant and peer feedback on Peer-Supported Thinking Forward. Overall satisfaction was good for both participants and peers. Components rated as most helpful by participants and peers were discussing how to apply module content in real life and setting personal life goals. In open-ended responses, participants reported liking being accountable to their peer and feeling genuinely care for. Peers liked reaching veterans who did not typically come in for mental health treatment; however, they also reported that sometimes they were not “meeting the veterans where they were at” in their recovery process. One peer reported that he preferred to “plant a seed and let it grow” rather than encourage rapid acquisition of coping skills. Peers also discussed how the content was more diagnostically focused than they preferred and they typically take their lead from patients on what is discussed, rather then it being predetermined by a structured program. Participants and peers thought that sessions should be weekly and liked the flexibility of being able to engage by phone. Peers reported that the service was easy to deliver.
Figure 2:
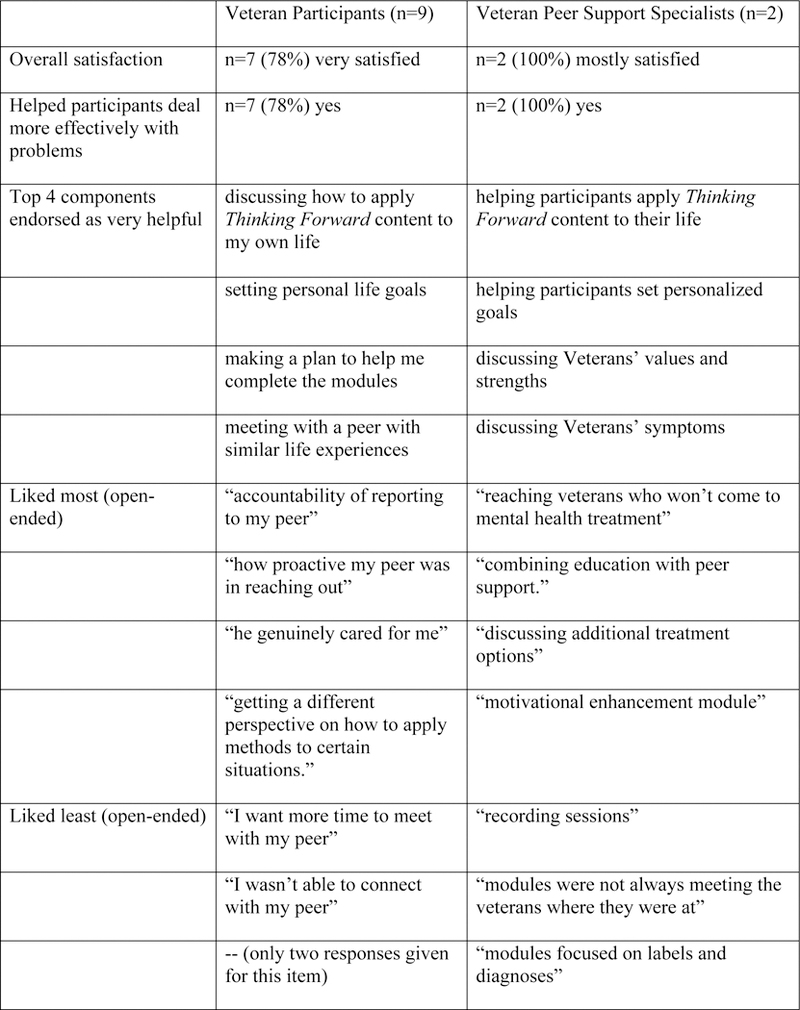
Summary of Participant and Peer Intervention Feedback
At baseline, participants did not statistically differ on PTSD severity, number of drinking or heavy drinking days, quality of life domain scores, patient activation, or any other clinical variable. Table 2 displays means and standard deviations of each outcome measure at baseline, post-treatment (12 weeks) and follow-up (24 weeks), and results from MLM significance tests for both within group and between group changes. Peer Support participants experienced statistically significant improvements in PTSD severity (medium effect), psychological quality of life (large effect), social quality of life (medium effect), resiliency (medium effect), and coping (large effect) from pre to post-treatment. No significant differences were observed for alcohol use outcomes. No between group differences were observed and all between group effect sizes were small except coping, which has a medium effect size.
Table 2:
Means and Between and Within-Groups Effects for Study Outcomes
| Peer Support | Self-Managed | Pre to Post-treatment |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Within Peer Support Between Groups | ||||||||||
| Week 0 |
Week 12 | Week 24 | Week 0 |
Week 12 | Week 24 | effect size (95% CI) |
Sign. test | effect size (95% CI) |
Sign. test | |
| Measure | M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | Cohen’s d | ʈ | Cohen’s d | ʈ |
| PTSD severity | 48.2 (11.62) | 41.78 (14.90) | 40.31 (12.10) | 51.87 (9.01) | 43.16 (13.42) | 41.64 (12.18) | .55(0, 1.09) | 2.80* | .22(−.50, .93) | -.70 |
| Drinking days | 12.60 (8.10) | 11.17(7.58) | 9.73 (7.21) | 13.30 (8.7) | 10.77 (8.52) | 8.24 (7.48) | .18(−.34, .69) | 1.51 | .13(−.59, .84) | .68 |
| Heavy Drinking Days | 6.71 (9.36) | 5.74 (9.11) | 4.77 (9.15) | 6.43 (7.89) | 3.99 (7.01) | 1.55 (3.79) | .10(−.41, .61) | 1.49 | .17(−.55, .89) | 1.20 |
| Psych Quality of Life | 47.76 (19.39) | 63.45 (27.62) | 65.21 (27.32) | 43.78 (16.42) | 53.42 (20.10) | 54.67 (19.83) | .81(.21, 1.39) | 4.04* | .34(−.39, 1.06) | 1.15 |
| Social Quality of Life | 46.91 (45.47) | 57.68 (27.38) | 68.45 (28.93) | 45.67 (18.43) | 53.72 (26.50) | 61.76 (20.30) | .45(−.09, .97) | 3.66* | .13(−.59, .84) | .69 |
| Resiliency | 64.13 (14.20) | 71.34 (18.77) | 75.37 (14.84) | 62.47 (15.21) | 67.81 (13.87) | 70.70 (10.20) | -.51(−.04, 1.04) | 3.36* | .13(−.59, .84) | .62 |
| Coping | 1.08 (.40) | 1.63 (.65) | 1.68 (.85) | 1.44 (.49) | 1.78 (.67) | 1.76 (.56) | 1.38(.65, 2.08) | 5.10* | .49(−.24, 1.21) | 1.46 |
| Activation | 59.31 (13.03) | 63.23 (15.99) | 67.14 (17.31) | 57.47(12.45) | 60.99 (14.34) | 64.50 (13.94) | .30(−.22, .81) | 1.58 | .03(−.68, .75) | .12 |
Note:
p ≤ .05.
Based on the peer feedback that this intervention was not “meeting patients where they were at” we conducted post-hoc analyses exploring if baseline level of patient activation predicted changes in PTSD and drinking. The PAM categorized participants into four levels based on their reported activation. Participants in levels 1 (e.g., person sees value in taking an active role) and 2 (e.g., person has knowledge to take action) were combined to form the low activation group (n=12). Participants in levels 3 (e.g., person taking action) and 4 (e.g., person staying the course under stress) were combined to form the high activation group (n=17). High activation participants reported a significantly larger decrease (−12.54 [8.25]) in PTSD severity from pre to post treatment than low activation participants (+1.83 [6.88]) (t=3.62, p=.003). High activation participants had a significantly larger reduction in drinking days per month (−3.58 [7.07]) from pre to post treatment, than low activation participants (+1.80 [2.80]), (t=2.43, p=.026). This pattern of results was similar for Peer-Supported and Self-Managed participants when analyzed separately, indicating that patients who were activated to make changes made improvements, regardless of whether they received peer support.
Discussion
Results from this pilot study indicated that Peer-Supported Thinking Forward can be feasibility delivered and is associated with good patient and peer satisfaction. This study had good rates of recruitment, enrollment, intervention retention, but had lower than desired assessment retention within the Peer Support condition. Participants in both conditions completed an average of eleven Thinking Forward modules. This is higher than the average of nine modules completed in the parent study (Acosta et al., 2017). This finding is contrary to our hypothesis that peer support would increase use of the modules. However, means in small samples can be highly variable, so we also report the modal number of modules completed (Self-Management= 0 modules, Peer Support= 8 and 24 modules) to indicate that the pattern of results for number of modules completed were different between the two conditions.
Participants demonstrated good engagement in peer support sessions, with an average attendance of five sessions per participant. This number of sessions mirrors the number of appointments mental health providers in primary care typically offer, indicating that the scope of this intervention may be a good fit for primary care. Interestingly, both peers and participants thought sessions should be weekly, though few participants attended weekly sessions. The key to interpreting this set of results is likely that peers and participants want the ability to meet weekly and the flexibility to meet less often, depending on the needs of the patient. This coincides with peers’ and participants’ appreciation of having the flexibility to meet by phone or in-person.
All but one participant in the Peer Support condition provided very positive feedback. Our two peers also reported good satisfaction with the protocol. There was considerable overlap between the components of the intervention that peers and participants found most valuable, including setting personalized goals and discussing how to apply skills learned via Thinking Forward to their daily lives. Other components seem to have been valued differently by peers and participants. For instance, peers saw the discussion of the participants’ values and strengths as very helpful to participants, while participants saw being accountable to their peers as very helpful. Taken together, these results describe some potential active components of Peer-Supported Thinking Forward (e.g., goal setting, applying skills to daily life, values-driven action, accountability). These components are highly consistent with Supportive Accountability, a model of how human support can enhance the effectiveness of eHealth interventions (Mohr, Cuijpers, & Lehman, 2011). Within this model, the human must be viewed as trustworthy, benevolent, and knowledgeable, and work collaboratively with the participant to set clear expectations.
Peers demonstrated good fidelity to the Peer-Supported Thinking Forward Guide. This is an important finding, as the peers said that following more structured interventions was new to them and was not their preferred way of working with patients. Peer feedback at the end of the study indicated that the peers came to see the benefits of a structured approach (e.g., they were able to provide more psychoeducation and teach more coping skills to the participants), while still having concerns that the content was not a good fit for some participants’ readiness to change. Primary care patients who are not seeking behavioral health treatment often have low problem recognition and our peers thought that language about “readjustment” would have been better received than labeling specific behavioral problems as “symptoms” and “diagnoses.” Peers appreciated the motivation enhancement module and may have been more satisfied with Thinking Forward if the motivational enhancement strategies were incorporated throughout the online content.
There is a potential mismatch between the philosophies of peer support and CBT interventions. Most peer certification training programs emphasize person-centered approaches that resist diagnostic labels and instead let the patient take the lead in developing both the focus of the session and the approach to be used (Chinman et al., 2016; Solomon, 2004). In contrast, Thinking Forward, like most CBT approaches, starts from the perspective that the patient has a problem (PTSD and hazardous alcohol use) that needs to be addressed by 1) learning more about the problem and 2) learning specific skills to decrease symptoms (e.g., relaxation, cognitive restructuring, functional analysis of alcohol use). Therefore, these findings likely indicate that peers can deliver semi-structured services, however the services should be consistent with the philosophy of peer support and prior peer support training. The peers in our study may have benefited from further training in how CBT can meet patient needs. Guidance on how to train peers to support low-intensity CBT is available (Lawn et al., 2010).
Within group analyses of Peer Support participants demonstrate significant improvements in PTSD severity, quality of life, resiliency, and coping with medium to large effect sizes. This is a clear indication that this approach was helpful for participants. Contrary to our hypotheses, there is no indication that peer support boosted the effect of Thinking Forward on PTSD or drinking outcomes. Rather, it appears the benefits of peer support were more generalized. This could be attributable to the holistic focus of peer support services and is evidenced by the largest between group effect size being found for coping (d= .49). However, between group effect sizes must be interpreted with caution given the wide confidence intervals reported in Table 2.
Our post-hoc analyses indicate that patient activation was a robust predictor of treatment gain regardless of whether participants received peer support. It is disappointing that peer support did not increase patient activation in the way we measured it. Future development and refinement of peer support interventions to support eHealth programs may benefit from more focus on building patients’ confidence to manage their mental health concerns. This could be done by enabling patients to experience health care “successes” such as effectively using a coping strategy or effectively seeking healthcare when needed. Future research should investigate what measures of engagement and activation are most sensitive to the effects of peer support. Our measure of activation, the PAM-MH, emphasizes the ability to participate as an effective member of the mental health care team (Green et al., 2010). Given the emphasis on peer support in patient-centered care and meeting Veterans at their respective level of recovery, measures more sensitive to motivation or readiness to change inspired by the Transtheoretical model (Prochaska & Velicer, 1997) or Self-Determination theory (Ng et al., 2012) should be investigated.
This pilot study has several notable limitations. The scope of this study in terms of number of peers delivering the intervention as well as patient sample size was very small. Therefore it is unknown how much peer and patient feedback, as well as patient clinical outcomes, would generalize to other samples. Attrition from the Peer Support condition may have positively skewed the patient satisfaction results. Also, the frequent reminder calls from research staff to complete modules made our Self-Managed condition non-representative of true self-management.
Despite these limitations, several important conclusions emerge from this study. Peer support can be feasibly combined with eHealth interventions for primary care veterans with PTSD and hazardous alcohol use. Peers can be trained to deliver semi-structured interventions to support eHealth programs with good fidelity. Primary care patients can benefit from peer-supported eHealth services, especially in the areas of quality of life and coping. Future development and refinement of peer support protocols to facilitate the use of eHealth interventions or to be delivered in primary care settings should be consistent with the philosophy of peer support. For instance, Whole Health Coaching (Simmons & Wolever, 2013) and Motivational Enhancement (Mastroleo, Magill, Barnett, & Borsari, 2014) are two approaches that may be appropriate for peer delivery with primary care patients who have lower problem recognition and less interest in engaging in traditional mental health interventions. As peer support specialists begin delivering services in more and more new settings, research should continue to investigate what types of services are most appropriate given the relevant background and skill sets that peers possess and the needs of patients within that setting.
Impact:
Peer support specialists can provide high fidelity support for an eHealth program focused on PTSD and hazardous alcohol use and this support is associated with high patient satisfaction. Further development of peer support services to facilitate eHealth programs should strive to be consistent with the person-centered, recovery orientation of peer support and explicitly focus on patient activation.
Acknowledgements of support:
This research was supported by a pilot award from the VA Center for Integrated Healthcare as well as the National Institutes of Health (grant numbers R01AA020181 and P30DA029926). The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
Footnotes
Conflict of Interest Statement: One of the investigators, Dr. Marsch, is affiliated with the business that developed the web-based psychosocial intervention platform that was used in the study. This relationship is extensively managed by Dr. Marsch and her academic institution.
Contributor Information
Kyle Possemato, VA Center for Integrated Healthcare, Syracuse VA Medical Center.
Emily M. Johnson, VA Center for Integrated Healthcare, Syracuse VA Medical Center
J. Bronte Emery, VA Center for Integrated Healthcare, Syracuse VA Medical Center.
Michael Wade, VA Center for Integrated Healthcare, Syracuse VA Medical Center.
Michelle C. Acosta, National Development Research Institutes
Lisa A. Marsch, Dartmouth College
Andrew Rosenblum, National Development Research Institutes, VA Center for Integrated Healthcare, Syracuse VA Medical Center.
Stephen A. Maisto, National Development Research Institutes, VA Center for Integrated Healthcare, Syracuse VA Medical Center
References
- Acosta MC, Possemato K, Maisto SA, Marsch LA, Barrie K, Lantinga L, Rosenblum A (2017). Web-delivered CBT reduces heavy drinking in OEF-OIF veterans in primary care with symptomatic substance use and PTSD. Behavior Therapy, 48(2), 262–276. doi: 10.1016/j.beth.2016.09.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Attkisson CC, & Zwick R (1982). The client satisfaction questionnaire. Psychometric properties and correlations with service utilization and psychotherapy outcome. Eval Program Plann, 5(3), 233–237. [DOI] [PubMed] [Google Scholar]
- Babor TF, Higgins-Biddle JC, Saunders JB, & Monteiro MG (2001). Audit. The Alcohol Use Disorders Identification Test (AUDIT): Guidelines for use in primary care. [Google Scholar]
- Bassuk EL, Hanson J, Greene RN, Richard M, & Laudet A (2016). Peer-delivered recovery support services for addictions in the United States: A systematic review. Journal of Substance Abuse Treatment, 63, 1–9. doi: 10.1016/j.jsat.2016.01.003 [DOI] [PubMed] [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, & Keane TM (1995). The development of a Clinician-Administered PTSD Scale. Journal of Traumatic Stress, 8(1), 75–90. [DOI] [PubMed] [Google Scholar]
- Blow AJ, Gorman L, Ganoczy D, Kees M, Kashy DA, Valenstein M, Chermack S (2013). Hazardous drinking and family functioning in National Guard veterans and spouses postdeployment. Journal of Family Psychology, 27(2), 303. doi: 10.1037/a0031881 [DOI] [PubMed] [Google Scholar]
- Cabassa LJ, Camacho D, Vélez-Grau CM, & Stefancic A (2017). Peer-based health interventions for people with serious mental illness: a systematic literature review. Journal of Psychiatric Research, 84, 80–89. doi: 10.1016/j/jpsychires.2016.09.021 [DOI] [PubMed] [Google Scholar]
- Chinman M, Daniels K, Smith J, McCarthy S, Medoff D, Peeples A, & Goldberg R (2017). Provision of peer specialist services in VA patient aligned care teams: protocol for testing a cluster randomized implementation trial. Implement Sci, 12(1), 57. doi: 10.1186/s13012-017-0587-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chinman M, George P, Dougherty RH, Daniels AS, Ghose SS, Swift A, & Delphin-Rittmon ME (2014). Peer support services for individuals with serious mental illnesses: Assessing the evidence. Psychiatric Services, 65(4), 429–441. doi: 10.1176/appi.ps.201300244 [DOI] [PubMed] [Google Scholar]
- Chinman M, McCarthy S, Mitchell-Miland C, Daniels K, Youk A, & Edelen M (2016). Early stages of development of a peer specialist fidelity measure. Psychiatric Rehabilitation Journal, 39(3), 256. doi: 10.1037/prj0000209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connor KM, & Davidson JR (2003). Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC). Depression and Anxiety, 18(2), 76–82. doi: 10.1002/da.10113 [DOI] [PubMed] [Google Scholar]
- Daaleman TP, & Fisher EB (2015). Enriching patient-centered medical homes through peer support. The Annals of Family Medicine, 13(Suppl 1), S73–S78. doi: 10.1370/afm.1761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diggle PJ, Liang KY, and Zeger SL (1991). Analysis of Longitudinal Data. Oxford Science Publications, Oxford. [Google Scholar]
- Glass JE, Perron BE, Ilgen MA, Chermack ST, Ratliff S, & Zivin K (2010). Prevalence and correlates of specialty substance use disorder treatment for Department of Veterans Affairs Healthcare System patients with high alcohol consumption. Drug and Alcohol Dependence, 112(1), 150–155. doi: 10.1016/j.drugalcdep.2010.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green CA, Perrin NA, Polen MR, Leo MC, Hibbard JH, & Tusler M (2010). Development of the Patient Activation Measure for mental health. Administration and Policy in Mental Health and Mental Health Services Research, 37(4), 327–333. doi: 10.1007/s10488-009-0239-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hundt NE, Robinson A, Arney J, Stanley MA, & Cully JA (2015). Veterans’ perspectives on benefits and drawbacks of peer support for posttraumatic stress disorder. Military Medicine, 180(8), 851–856. doi: 10.7205/MILMED-D-14-00536 [DOI] [PubMed] [Google Scholar]
- Jain S, Hernandez JM, & Lindley SE (2014). Peer support program for veterans in rural areas. Psychiatric Services, 65(9), 1177–1177. doi: 10.1176/appi.ps.650704 [DOI] [PubMed] [Google Scholar]
- Joseph KM, Hernandez JM, & Jain S (2015). Peer support telephone outreach intervention for veterans with PTSD. Psychiatric Services, 66(9), 1001–1001. doi: 10.1176/appi.ps.660903 [DOI] [PubMed] [Google Scholar]
- Kearney LK, Post EP, Zeiss A, Goldstein MG, & Dundon M (2011). The role of mental and behavioral health in the application of the patient-centered medical home in the Department of Veterans Affairs. Transl Behav Med, 1(4), 624–628. doi: 10.1007/s13142-011-0093-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawn S, Smith A, Hunter K, Smith J, Hirst N, Nanai M, Neate K (2010). Training peers to provide low intensity CBT support: The value of personal experience. In: Oxford guide to low intensity CBT interventions Bennett-Levy, J. et al. (Ed); Publisher: Oxford University Press, 437–443. [Google Scholar]
- Leon AC, Davis LL, & Kraemer HC (2011). The role and interpretation of pilot studies in clinical research. J Psychiatr Res, 45(5), 626–629. doi: 10.1016/j.jpsychires.2010.10.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Litt MD, Kadden RM, Cooney NL, & Kabela E (2003). Coping skills and treatment outcomes in cognitive-behavioral and interactional group therapy for alcoholism. Journal of Consulting and Clinical Psychology, 71(1), 118–128. [DOI] [PubMed] [Google Scholar]
- Mastroleo NR, Magill M, Barnett NP, & Borsari B (2014). A pilot study of two supervision approaches for peer-led alcohol interventions with mandated college students. J Stud Alcohol Drugs, 75(3), 458–466. doi: 0.15288/jsad.2014.75.458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDevitt‐Murphy ME, Williams JL, Bracken KL, Fields JA, Monahan CJ, & Murphy JG (2010). PTSD symptoms, hazardous drinking, and health functioning among US OEF and OIF veterans presenting to primary care. Journal of Traumatic Stress, 23(1), 108–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohr DC, Burns MN, Schueller SM, Clarke G, & Klinkman M (2013). Behavioral intervention technologies: evidence review and recommendations for future research in mental health. General Hospital Psychiatry, 35(4), 332–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohr DC, Cuijpers P, & Lehman K (2011). Supportive accountability: a model for providing human support to enhance adherence to eHealth interventions. J Med Internet Res, 13(1), e30. doi: 10.2196/jmir.1602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mott JM, Hundt NE, Sansgiry S, Mignogna J, & Cully JA (2014). Changes in psychotherapy utilization among veterans with depression, anxiety, and PTSD. Psychiatric Services, 65(1), 106–112. doi: 10.1176/appi.ps.201300056 [DOI] [PubMed] [Google Scholar]
- Murphy B, Herrman H, Hawthorne G, Pinzone T, & Evert H (2000). Australian WHOQoL instruments: User’s manual and interpretation guide. Melbourne, Australia: Australian WHOQOL Field Study Centre. [Google Scholar]
- Nelson CB, Abraham KM, Walters H, Pfeiffer PN, & Valenstein M (2014). Integration of peer support and computer-based CBT for veterans with depression. Computers in Human Behavior, 31, 57–64. doi: 10.1016/j.chb.2013.10.012 [DOI] [Google Scholar]
- Neter J, Wasserman W, Kutner M (1990) Applied Linear Statistical Models. (3rd edition), CRC Press: New York: pgs 370–378. [Google Scholar]
- Newman MG, Szkodny LE, Llera SJ, & Przeworski A (2011a). A review of technology-assisted self-help and minimal contact therapies for anxiety and depression: is human contact necessary for therapeutic efficacy? Clinical Psychology Review, 31(1), 89–103. doi: 10.1016/j.cpr.2010.09.008 [DOI] [PubMed] [Google Scholar]
- Newman MG, Szkodny LE, Llera SJ, & Przeworski A (2011b). A review of technology-assisted self-help and minimal contact therapies for drug and alcohol abuse and smoking addiction: is human contact necessary for therapeutic efficacy? Clinical Psychology Review, 31(1), 178–186. doi: 10.1016/j.cpr.2010.10.002 [DOI] [PubMed] [Google Scholar]
- Ng JY, Ntoumanis N, Thøgersen-Ntoumani C, Deci EL, Ryan RM, Duda JL, & Williams GC (2012). Self-determination theory applied to health contexts: A meta-analysis. Perspectives on Psychological Science, 7(4), 325–340. [DOI] [PubMed] [Google Scholar]
- Owens GP, Held P, Blackburn L, Auerbach JS, Clark AA, Herrera CJ, Stuart GL (2014). Differences in relationship conflict, attachment, and depression in treatment-seeking veterans with hazardous substance use, PTSD, or PTSD and hazardous substance use. Journal of Interpersonal Violence, 29(7), 1318–1337. doi: 10.1177/0886260513506274 [DOI] [PubMed] [Google Scholar]
- Possemato K, Acosta MC, Fuentes J, Lantinga LJ, Marsch LA, Maisto SA, Rosenblum A (2015). A web-based self-management program for recent combat veterans with PTSD and substance misuse: Program development and veteran feedback. Cogn Behav Pract, 22(3), 345–358. doi: 10.1016/j.cbpra.2014.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prochaska JO, & Velicer WF (1997). The transtheoretical model of health behavior change. American Journal of Health Promotion, 12(1), 38–48. doi: 10.4278/0890-1171-12.1.38 [DOI] [PubMed] [Google Scholar]
- Proudfoot J, Parker G, Manicavasagar V, Hadzi-Pavlovic D, Whitton A, Nicholas J, Burckhardt R (2012). Effects of adjunctive peer support on perceptions of illness control and understanding in an online psychoeducation program for bipolar disorder: a randomised controlled trial. Journal of Affective Disorders, 142(1), 98–105. doi: 10.1016/j.jad.2012.04.007 [DOI] [PubMed] [Google Scholar]
- Reif S, Braude L, Lyman DR, Dougherty RH, Daniels AS, Ghose SS, Delphin-Rittmon ME (2014). Peer recovery support for individuals with substance use disorders: Assessing the evidence. Psychiatric Services, 65(7), 853–861. doi: 10.1176/appi.ps.201400047 [DOI] [PubMed] [Google Scholar]
- Schnurr PP, Lunney CA, Sengupta A, & Spiro A 3rd. (2005). A longitudinal study of retirement in older male veterans. Journal of Consulting and Clinical Psychology, 73(3), 561–566. doi: 10.1037/0022-006X.73.3.561 [DOI] [PubMed] [Google Scholar]
- Schwarz GE (1978). Estimating the dimension of a model. Annals of Statistics, 6 (2): 461–464. doi: 10.1214/aos/1176344136 [DOI] [Google Scholar]
- Sheehan D, Janavs J, Baker R, Harnett-Sheehan K, Knapp E, Sheehan M (2004). The MINI International Neuropsychiatric Interview. [Google Scholar]
- Simmons LA, & Wolever RQ (2013). Integrative health coaching and motivational interviewing: synergistic approaches to behavior change in healthcare. Global Advances in Health and Medicine, 2(4), 28–35. doi: 10.1001/jama.289.16.2083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell LC, & Sobell MB (2000). Alcohol Timeline Followback (TLFB) In I. A. P. A. (ed.) (Ed.), Handbook of Psychiatric Measures (pp. 477–479). Washington, DC: American Psychiatric Association. [Google Scholar]
- Solomon P (2004). Peer support/peer provided services underlying processes, benefits, and critical ingredients. Psychiatric Rehabilitation Journal, 27(4), 392. doi: 10.2975/27.2004.392.401 [DOI] [PubMed] [Google Scholar]
- Swarbrick M, Tunner TP, Miller DW, Werner P, & Tiegreen WW (2016). Promoting health and wellness through peer-delivered services: Three innovative state examples. Psychiatric Rehabilitation Journal, 39(3), 204–210. doi: 10.1037/prj0000205 [DOI] [PubMed] [Google Scholar]
- Thomas DR (2006). A general inductive approach for analyzing qualitative evaluation data. American Journal of Evaluation, 27(2), 237–246. doi: 10.1177/1098214005283748 [DOI] [Google Scholar]
- VA/DOD Clinical Practice Guideline for the Management of Posttraumatic Stress Disorder and Acute Stress Disorder. (2017) Retrieved from https://www.healthquality.va.gov/guidelines/MH/ptsd/VADoDPTSDCPGFinal082917.pdf.
- VA/DoD Clinical Practice Guideline for the Management of Substance Use Disorders. (2015). Retrieved from https://www.healthquality.va.gov/guidelines/MH/sud/VADoDSUDCPGRevised22216.pdf.
- Weathers FW, & Ford J (1996). Psychometric review of the PTSD checklist In Stamm BH (Ed.), Measurement of Stress, Trauma, and Adaptation. Lutherville, MD: Sidran Press. [Google Scholar]


