Abstract
Purpose
The medical morbidity and mortality associated with neck of femur fractures is well-documented, whereas there is limited data for patient-reported outcomes. The aim of this study was to characterize the impact of neck of femur fractures on activities of daily living and patient-reported health-related quality of life.
Methods
Design and participants: Multicentric prospective cohort study. Consecutive sample patients with fragility hip fracture over 50 years old admitted in 48 hospitals in Spain.
Outcomes: daily living activity function (Barthel Index) and health-related quality of life (EQ-5D) pre-fracture, admission to hospital and at 1- and 4-month follow-up post-fracture.
Statistics: Barthel and EQ-5D over time are described as mean (SD) and median (interquartile range).
Results
A total of 997 patients were recruited at baseline with 4-month outcomes available for, and 856 patients (89.5%). Barthel Index fell from 78.77 (23.75) at baseline to 43.62 (19.86) on admission to hospital with the fracture. Scores partially recovered to 54.89 (25.40) and 64.09 (21.35) at 1- and 4-month post-fracture, respectively. EQ-5D fell from a median of 0.75 (0.47–0.91) to − 0.01 (− 0.03 to 0.51) on admission. Partial recovery was observed again to (0.51 (− 0.06 to 0.67)) and (0.60 (0.10 to 0.80)) at 1- and 4-month post-fracture, respectively.
Conclusions
Hip fracture results in a large decline in the ability to perform activities of daily living and patient-reported health-related quality of life with only partial recovery amongst survivors 4-month post-fracture.
Keywords: Fragility hip fracture, Osteoporosis, Registries, Quality of life
Introduction
A total of 620,000 hip fractures were sustained in the European Union in 2010.Osteoporotic hip fractures are associated with significant morbidity, mortality and societal costs [1]. Fragility fractures of any site had an estimated economic burden of € 37 billion and accounted for almost 1.2 million quality-adjusted life years in that same year [2].
It is estimated that between 2020 and 2050, the number of hip fractures worldwide will increase to more than 2 billion cases [3]. This will represent a large socioeconomic burden [4, 5].
Despite the increasing socioeconomic burden, there is a scarcity of data on the impact of hip fracture to patients in terms of patient-reported outcomes and activities of daily living. Particularly, there is no previous reports to our knowledge of both in a same cohort in Spain. This is important for a comprehensive assessment of the burden of hip fractures in the Spanish population.
The aim of this study is to determine the association between proximal femur fragility fractures and patient-reported health-related quality of life and activities of daily living during the 4-month following fracture.
Methods
Study design and setting
Multi-centre prospective observational cohort study in 48 hospitals in Spain
Eligibility criteria
Details on sampling strategies, data collection and follow-up have been reported elsewhere [6]. One thousand consecutive men or women aged ≥ 50 years old with a diagnosis of a fragility femur fracture were recruited. Consent was obtained from patient or principal carer and/or legal representative of the patient.
Measurements
Data was collected during consultations on admission and at 1-month and 4-month follow-up appointments. Phone consultations were conducted for the 1 month and 4 months when face-to-face visits were not possible. Baseline (pre-fracture) measures were collected on admission to hospital-based on patient recollection of their previous activity and health status.
Outcome measures were Barthel Index (ability to perform activities of daily living) [7]) and EQ-5D-3L (global health-related quality of life [8]). Barthel scores range from 0 to 100, with lower scores indicating more disability. EQ-5D-3L measures five dimensions (mobility, self-care, usual activities, pain and anxiety/depression) and a global visual analogue scale (VAS). Utility indices were derived from EQ-5D-3L using Spanish national preference tables [9]. These range from 0 (death) or even negative values (worse than death) to 1 (full health).
Statistical analyses
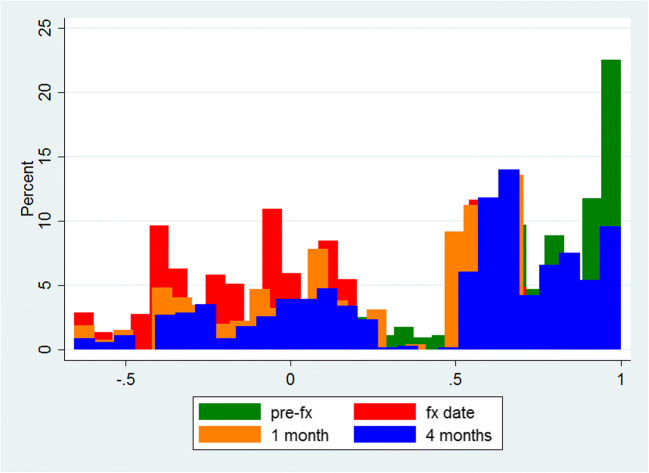
Barthel EQ-5D-3L is expressed as mean (standard deviation) and as median (interquartile range) (Table 1). Change in utility indices over time is plotted as a histogram (Fig. 1).
Table 1.
Change in health-related quality of life at the time of a femur fracture, and in the following 1 and 4 months of follow-up
| Change in EQ-5D-3L utility at index admission | Change in EQ-5D-3L from index admission to 1 month | Change in EQ-5D-3L from 1 to 4 months of follow-up | |
|---|---|---|---|
| Mean (sd) | − 0.57 (0.43) | 0.23 (0.40) | 0.37 (0.43) |
| Median (IQR) | − 0.56 (− 0.90 to − 0.28) | 0.16 (0.0 to 0.50) | 0.34 (0.09 to 0.70) |
*Positive values are equivalent to improvement/recovery; negative values mean worsening
Fig. 1.
Histogram of EQ-5D-3L utility indices at baseline (pre-fx), at admission for a femur fracture (fx date), and at 1 and 4 months of follow-up
Results
Baseline outcome data was available for 997 patients, of whom 856 (85.9%) completed 4 months of follow-up. Of the 141 without follow-up data, 99 (9.9%) have died, and 42 (4.2%) were lost to follow-up. Detailed patient characteristics have been previously reported [6]. Complete data on baseline and 1- and 4-month Barthel and EQ-5D-3L were collected for 824/856 (96.3%) and 746/856 (90.2%) participants respectively.
On average, overall health-related quality of life dropped by 57% at the time of fracture, to then recover by 23% in the first month and by a total 37% at 4-month post-admission.
Discussion
Our study demonstrates a significant fall in both EQ-5D and the Barthel Index on sustaining a proximal femoral fracture, and this falls only partial recovers at 4-week follow-up. Barthel Index, assessing the ability to perform activities of daily living fell from 79 to 44% immediately after sustaining the fracture, with a recovery to 64% function 4-month post-fracture. The impact on patient quality of life is even more striking: participants started with 75% of full health which fell to 0% of full health ‘like dead’ immediately after the fracture. Partial recovery was again seen in the following 4 months, increasing to a 60% full health.
Our results are similar to those found in similar cohort from the UK [10], Norway [11] and Portugal [5]. In those, the authors reported a gradual recovery up to 1 year in terms of quality of life. These findings are also comparable to those obtained from a smaller Spanish cohort [12]. As in our study, improvement in quality of life seemed to be mirrored by functional recovery in these previous studies. Other studies [13, 14] including the UK (WHiTE) study [15] have also shown similar deterioration in functional status [16].
Our study has limitations. Our findings are only representative of the subjects who survived, as almost 10% of the study participants died within 4 months, and it is possible that their function and health status were worse at baseline and post-fracture. In addition, recall bias is possible in the determination of pre-fracture (baseline) health status, as this was recorded during the index hospital admission.
This analysis also has strengths. First, the prospective nature of data collection and the fact that the information was recorded by trained clinician/s and/or nurses give high validity to our findings. Secondly, we have low attrition, with < 5% loss to follow-up at 4-month post-fracture. Finally, our participants were recruited from a representative sample of hospitals around the country.
In conclusion, we report a sustained detriment of proximal femoral fractures on the ability of a patient to perform activities of daily living and their health-related quality of life. These data should be used to estimate the socioeconomic burden of osteoporosis-related fractures and to inform the planning of care for these patients.
Funding information
This work has been sponsored by an unrestricted grant of AMGEN to the Hospital del Mar Institute of Medical Investigation (IMIM).
Compliance with ethical standards
Conflicts of interest
ADP is advisor or speaker for Amgen/UCB, Roche, Gilead, EchoLight and Lilly. Institutional grant EchoLight and Kiowa-Kirin and Shareholder Active Life Sci. DPA’s research group has received unrestricted research grants from Servier, Amgen and UCB; and speaker and consultancy fees from Amgen and UCB. All other authors report no conflict of interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Pedersen AB, Ehrenstein V, Szépligeti SK, Lunde A, Lagerros YT, Westerlund A, Tell GS, Sørensen HT. Thirty-five–year trends in first-time hospitalization for hip fracture, 1-year mortality, and the prognostic impact of comorbidity: a Danish nationwide cohort study, 1980–2014. Epidemiology. 2017;28(6):898–905. doi: 10.1097/EDE.0000000000000729. [DOI] [PubMed] [Google Scholar]
- 2.Svedbom A, Hernlund E, Ivergård M, Compston J, Cooper C, Stenmark J, et al. Osteoporosis in the European Union: a compendium of country-specific reports. Arch Osteoporos. 2013;8(1–2):137. doi: 10.1007/s11657-013-0137-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cooper C, Campion G, Melton LJ., 3rd Hip fractures in the elderly: a world-wide projection. Osteoporos Int. 1992;2(6):285–289. doi: 10.1007/BF01623184. [DOI] [PubMed] [Google Scholar]
- 4.Borgström F, Lekander I, Ivergård M, Ström O, Svedbom A, Alekna V, Bianchi ML, Clark P, Curiel MD, Dimai HP, Jürisson M, Kallikorm R, Lesnyak O, McCloskey E, Nassonov E, Sanders KM, Silverman S, Tamulaitiene M, Thomas T, Tosteson ANA, Jönsson B, Kanis JA. The international costs and utilities related to osteoporotic fractures study (ICUROS)—quality of life during the first 4 months after fracture. Osteoporos Int. 2013;24(3):811–823. doi: 10.1007/s00198-012-2240-2. [DOI] [PubMed] [Google Scholar]
- 5.Marques A, Lourenço Ó, da Silva J. The burden of osteoporotic hip fractures in Portugal: costs, health related quality of life and mortality. Osteoporos Int. 2015;26(11):2623–2630. doi: 10.1007/s00198-015-3171-5. [DOI] [PubMed] [Google Scholar]
- 6.Prieto-Alhambra D, Reyes C, Sainz MS, González-Macías J, Delgado LG, Bouzón CA, Gañan SM, Miedes DM, Vaquero-Cervino E, Bardaji MFB, Herrando LE, Baztán FB, Ferrer BL, Perez-Coto I, Bueno GA, Mora-Fernandez J, Doñate TE, Blasco JMI, Aguado-Maestro I, Sáez-López P, Doménech MS, Climent-Peris V, Rodríguez ÁD, Sardiñas HK, Gómez ÓT, Serra JT, Caeiro-Rey JR, Cano IA, Carsi MB, Etxebarria-Foronda I, Hernández JDA, Solis JR, Suau OT, Nogués X, Herrera A, Díez-Perez A. In-hospital care, complications, and 4-month mortality following a hip or proximal femur fracture: the Spanish registry of osteoporotic femur fractures prospective cohort study. Arch Osteoporos. 2018;13(1):96. doi: 10.1007/s11657-018-0515-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Collin C, Wade D, Davies S, Horne V (1988) The Barthel ADL Index: a reliability study. Disability and rehabilitation 10(2):61–63 [DOI] [PubMed]
- 8.EuroQol G (1990) EuroQol--a new facility for the measurement of health-related quality of life. Health policy 16(3):199 [DOI] [PubMed]
- 9.Badia X, Roset M, Herdman M, Kind P. A comparison of United Kingdom and Spanish general population time trade-off values for EQ-5D health states. Med Decis Mak. 2001;21(1):7–16. doi: 10.1177/0272989X0102100102. [DOI] [PubMed] [Google Scholar]
- 10.Griffin X, Parsons N, Achten J, Fernandez M, Costa M. Recovery of health-related quality of life in a United Kingdom hip fracture population: the Warwick hip trauma evaluation-a prospective cohort study. Bone Joint J. 2015;97(3):372–382. doi: 10.1302/0301-620X.97B3.35738. [DOI] [PubMed] [Google Scholar]
- 11.Gjertsen J-E, Baste V, Fevang JM, Furnes O, Engesæter LB. Quality of life following hip fractures: results from the Norwegian hip fracture register. BMC Musculoskelet Disord. 2016;17(1):265. doi: 10.1186/s12891-016-1111-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Caeiro JR, Bartra A, Mesa-Ramos M, Etxebarría Í, Montejo J, Carpintero P, et al. Burden of first osteoporotic hip fracture in Spain: a prospective, 12-month, observational study. Calcif Tissue Int. 2017;100(1):29–39. doi: 10.1007/s00223-016-0193-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ruths S, Baste V, Bakken MS, Engesæter LB, Lie SA, Haugland S. Municipal resources and patient outcomes through the first year after a hip fracture. BMC Health Serv Res. 2017;17(1):144. doi: 10.1186/s12913-017-2087-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vergara I, Vrotsou K, Orive M, Gonzalez N, Garcia S, Quintana JM. Factors related to functional prognosis in elderly patients after accidental hip fractures: a prospective cohort study. BMC Geriatr. 2014;14(1):124. doi: 10.1186/1471-2318-14-124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Costa ML, Griffin XL, Achten J, Metcalfe D, Judge A, Pinedo-Villanueva R, Parsons N. World hip trauma evaluation (WHiTE): framework for embedded comprehensive cohort studies. BMJ Open. 2016;6(10):e011679. doi: 10.1136/bmjopen-2016-011679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moerman S, Vochteloo AJ, Tuinebreijer WE, Maier AB, Mathijssen NM, Nelissen RG. Factors associated with the course of health-related quality of life after a hip fracture. Arch Orthop Trauma Surg. 2016;136(7):935–943. doi: 10.1007/s00402-016-2474-0. [DOI] [PubMed] [Google Scholar]