Abstract
Background
Traffic noise can induce chronic stress reactions and thereby elevate the risk of cardiovascular disease. The responsible pathophysiological mechanisms are as yet unclear.
Methods
This review is based on publications retrieved by a selective search in PubMed for epidemiological and experimental studies (2007–2018) on the relation between noise and the risk of cardiovascular disease. The search terms were “noise AND cardiovascular effects” and “noise cardiovascular effects.”
Results
Epidemiological studies have shown that noise caused by air, road, and rail traffic has a dose-dependent association with elevated cardiovascular morbidity and mortality. A current meta-analysis commissioned by the World Health Organization concludes that road-traffic noise elevates the incidence of coronary heart disease by 8% per 10 dB(A) increase starting at 50 dB(A) (95% confidence interval [1,01; 1,15]). Traffic noise at night causes fragmentation of sleep, elevation of stress hormone levels, and oxidative stress. These factors can promote the development of vascular dysfunction (endothelial dysfunction) and high blood pressure, which, in turn, elevate the cardiovascular risk.
Conclusion
Traffic noise, and air-traffic noise in particular, is an important cardiovascular risk factor that has not been sufficiently studied to date. Preventive measures are needed to protect the population from the harmful effects of noise on health.
The Nobel Prize laureate Robert Koch is said to have predicted as early as 1910 that “One day man will have to fight noise as fiercely as plague and cholera” (1). The spectrum of disease has changed greatly over the past few decades, with the result that nontransmissible chronic illnesses such as cardiovascular disorders make up a considerable part of the global disease burden (2). Although research efforts in recent years have focussed primarily on classic risk factors such as high blood pressure, smoking, and diabetes mellitus, recently published results point to the influence of environmental factors such as noise in the development of cardiovascular disease (3). Insights from epidemiological studies show that exposure to traffic noise (from aircraft, road vehicles, and trains) is associated with increased cardiovascular morbidity and mortality (4, 5). In Europe, traffic noise is responsible for 18 000 premature deaths, 1.7 million cases of hypertension, and 80 000 hospitalizations each year (6). The World Health Organization (WHO) has stated that the following years of healthy life are lost annually in Western Europe (7):
61 000 due to ischemic heart disease
45 000 due to cognitive impairments in childhood
903 000 due to sleep disturbance
22 000 due to tinnitus
654 000 due to noise annoyance.
Altogether, illness induced by traffic noise results in over 1 million disability-adjusted life years (DALYs; i.e. loss of healthy life years) annually in Western Europe. Research into the effects of noise has made significant advances in recent years, particularly with regard to the pathophysiological mechanisms involved in the development of traffic noise–induced cardiovascular disease. A review of the recent literature has thus become necessary.
Methods
We carried out a selective survey of the epidemiological and experimental studies added to the PubMed database in the period 2007–2018. The search terms were “noise AND cardiovascular effects” and “noise cardiovascular effects.” We included large primary studies and systematic meta-analyses.
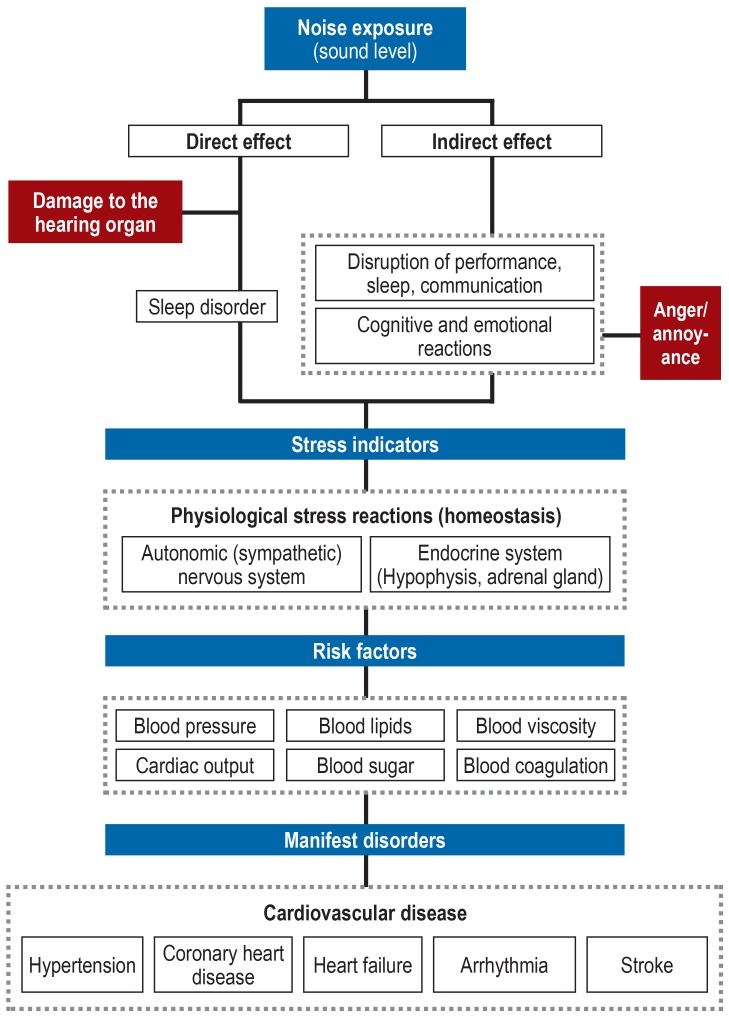
Noise effects model
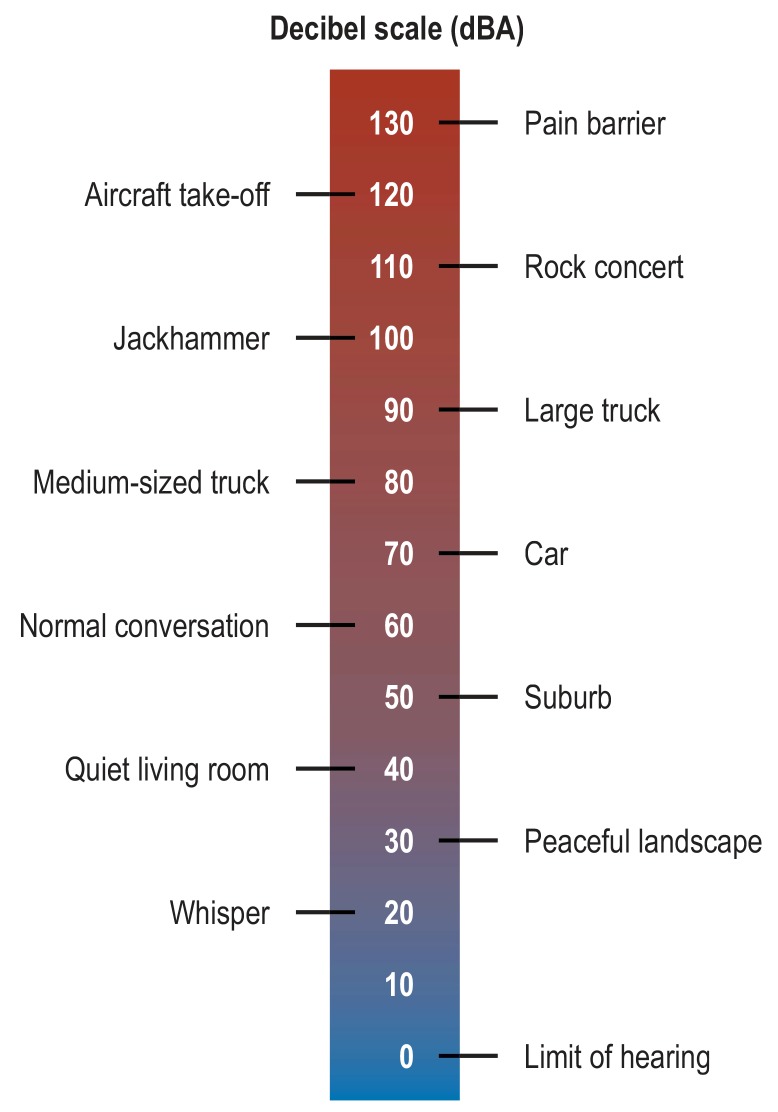
The definition of noise is sound perceived as annoying. Noise has an objectively (physically) quantifiable dimension in the shape of sound levels or decibels (dB[A]) (figure 1) and a subjective (psychological) dimension determined by the listener’s individual assessment of the sound source (8). According to Babisch’s noise effects model (9), apart from the direct auditory effects of noise on the organism (damage to the acoustic apparatus by very loud sounds), noise’s non-auditory effects are primarily responsible for triggering a stress cascade (figure 2). Long-term or short-term environmental noise can cause stress reactions/noise annoyance reactions, mediated by disturbances of sleep, communication, and activity together with the associated cognitive and emotional reactions. These affect the autonomic (sympathetic) and endocrine systems (e.g., elevated catecholamine and cortisone concentrations) and may as a result lead to changes in lipd metabolism, glucose metabolism, and blood pressure regulation that then contribute to an increased risk of cardiovascular illness. The noise-related stress is attributed an intermediary role in the development of noise-induced cardiovascular disease, i.e., the effects of noise on health are determined partly by the extent to which the listener perceives the noise as annoying (10). Data from the large, population-based Gutenberg Health Study (N = 15 010 persons resident in Mainz and the Mainz–Bingen region) show that the noise-related stress reaction to various sources of noise during the day and while sleeping at night, including aircraft (odds ratio [OR] 1.09, 95% confidence interval [1.05; 1.13]), road traffic (OR 1.15 [1.08; 1.22]), and rail traffic (OR 1.13 [1.04; 1.22] at night and per one point increase in noise annoyance) is associated dose-dependently with an increased risk of atrial fibrillation (11). Moreover, in the context of this study it was shown that the risk of depression (prevalence ratio [PR] 1.97 [1.62; 2.39]) and anxiety disorder (PR 2.14 [1.71; 2.67]), comparing no noise annoyance with extreme noise annoyance, rose with increasing total noise annoyance, which in turn may impact negatively on the cardiovascular system (11, 12). However, here only the subjectively assessed noise annoyance was documented, not the objective noise exposure (sound levels).
Figure 1.
Examples of sound levels from various sources. The dB(A) scale is a logarithmic scale, so that an increase/decrease of 3 dB(A) means doubling/halving of the sound level. An increase/decrease of 10 dB(A) is perceived as doubling/halving of loudness. In circumstances of long-term exposure to over 55 dB(A) weighted day–evening–night levels (Lden), with an increment of 5 dB(A) for the evening and 10 dB(A) for the night, the risk of cardiovascular disease rises (13, 20). (Modified from Münzel et al. [39]. Reproduced with the permission of the publisher. Copyright © 2017, Oxford University Press)
Figure 2.
The noise effect model of Babisch et al. (9) adjusted according to Münzel et al. (4). Both persistent and acute exposure to noise leads to increased development of cardiovascular risk factors (raised blood pressure, increases in blood lipids and blood sugar, greater cardiac output, increased blood viscosity, and activation of blood coagulation), mediated by mental and physiological stress reactions. In the long term, this leads in turn to the clinical manifestation of cardiovascular diseases such as hypertension, coronary heart disease, heart failure, arrhythmia, and stroke. (Modified from Münzel et al. [4]. Reproduced with the permission of the publisher. Copyright © 2014, Oxford University Press)
Epidemiological evidence of the association between noise and cardiovascular disease
Because of the recent increase in traffic, scientific evaluation of the health-related effects of noise is receiving increasing attention. Epidemiological research into the impact of noise has increased considerably in both quantity and quality in recent years. Methods for calculation/standardization of noise exposure have improved, larger populations have been studied, and there has been better correction for confounding variables. Furthermore, phenomena such as habituation, sensitization, conditioning, and exhaustion are adequately represented by the reproduction of daily living conditions in epidemiological studies. The most powerful studies are on the topics of coronary heart disease, myocardial infarction, stroke, and hypertension (etable).
eTable. Selected primary studies on the association between noise and cardiovascular endpoints.
|
First author, year |
Exposure |
Study design, location |
Overall population and endpoint (selected) |
Control variables | Results (selected) |
| O. Hahad, 2018 (11) |
Noise from various sources (including aircraft, road traffic, and rail traffic) during the day and while sleeping at night | Cross-sectional, data from the Gutenberg Health Study, Germany | N = 15 010, 35–74 years, AF diagnosis or diagnosis from study ECG |
Age, sex, SES, shift work, depression, medication intake, diabetes, hypertension, smoking, obesity, dyslipidemia, family history of MI/stroke | OR per 1-point increase in exposure during sleeping hours Aircraft noise: 1.09 [95% CI: 1.05; 1.13] Road traffic noise: 1.15 [95% CI: 1.08; 1.22] Rail traffic noise: 1.13 [95% CI: 1.04; 1.22] |
| N. Roswall, 2017 (17) |
Road traffic noise (L den) |
Longitudinal, data from the Diet, Cancer and Health study, Denmark | N = 50 744, 50–64 years, incidental MI |
Age, sex, smoking, alcohol, fruit and vegetable consumption, exercise, education, SES, calendar year, rail traffic noise, NO2 | HR per IQR Lden Road traffic noise: 1.12 [95% CI: 1.03; 1.21] |
| J. Selander, 2009 (18) |
Road traffic noise (L Aeq,24h) |
Population-based case–control study, Sweden | N = 5452 (2 246 cases, 3 206 controls), 45–70 years, MI diagnosis |
Age, sex, smoking, physical inactivity, diabetes, NO2, noise exposure in the workplace | OR LAeq,24h <50 vs. ≥ 50 db(a): 1.12 [95% ci: 0.95; 1.33] After exclusion of persons with hearing loss or noise exposure from other sources: 1.38 [95% CI: 1.11; 1.71] |
| H. Heritier, 2017 (19) |
Road traffic, rail traffic, and aircraft noise (L den) |
Longitudinal, data from the Swiss National Cohort study, Switzerland | N = 4 415 206, 30 years, Mortality due to MI |
Sex, SES, relationship status, NO2, native language, nationality | HR per 10 dB(A) Lden Road traffic noise: 1.038 [95% CI: 1.019; 1.058] Rail traffic noise: 1.018 [95% CI: 1.004; 1.031] Aircraft noise: 1.026 [95% CI: 1.004; 1.048] |
| M. Sørensen, 2012 (20) |
Road traffic noise (L den) |
Longitudinal, data from the Diet, Cancer and Health study, Denmark |
N = 57 053, 50–64 years, incidental MI |
Age, sex, smoking, fruit and vegetable consumption, education, alcohol, BMI, exercise, calendar year, rail traffic and aircraft noise, NOx | IRR per 10 dB(A) Lden At time of diagnosis: 1.12 [95% CI: 1.02; 1.22] L den 5 years before diagnosis: 1.12 [95% CI: 1.02; 1.23] |
| M. Sørensen, 2011 (21) |
Road traffic noise (L den) |
Longitudinal, data from the Diet, Cancer and Health study, Denmark |
N = 57 053, 50–64 years, hospitalization due to incidental stroke |
Smoking, fruit and vegetable consumption, coffee consumption, alcohol, BMI, exercise, education, income, rail traffic and aircraft noise, NOx | IRR per 10 dB(A) Lden: 1.14 [95% CI 1.03; 1.25] 1.02 [95% CI: 0.91; 1.14] for persons <64.5 years 1.27 [95% CI: 1.13; 1.43] for persons ≥ 64.5 years |
| AL. Hansell, 2013 (22) |
Aircraft noise (L Aeq,16h, L night) |
Longitudinal, small area study, England | N = 3.6 million, hospitalization due to incidental stroke |
Age, sex, ethnicity, deprivation, smoking | Significant linear association between hospitalization and LAeq,16h/ Lnight RR L night > 55 vs. ≤ 50 dB(A): 1.29 [95% CI: 1.14; 1.46] |
| Halonen, 2015 (23) |
Road traffic noise (L Aeq,16h, L night) |
Longitudinal, small area study, England | N = 8.6 million, ≥ 25 and ≥ 75 years, hospitalization due to incidental stroke |
Age, sex, deprivation, ethnicity, smoking, PM2.5,topographical structure of neighborhood | RR LAeq,16h >60 vs. <55 db(a): 1.05 [95% CI: 1.02; 1.09] for persons ≥ 25–74 years RR L night 55–60 vs. <55 db(a): 1.05 [95% CI: 1.01; 1.09] for persons ≥ 75 years |
| Eriksson, 2007 (25) |
Aircraft noise (L Amax) |
Longitudinal, data from the Stockholm Diabetes Preventive Program, Sweden |
N = 2754 men, 35–56 years, incidental hypertension |
Age, BMI | RR LAmax <70 vs. ≥ 70 db(a): 1.20 [95% CI: 1.03; 1.40] After exclusion of persons with tobacco consumption before blood pressure measurement: 1.32 [95% CI: 1.12; 1.55] |
| Dimakopoulou, 2017 (26) |
Aircraft noise (L night, L Aeq,16h) Road traffic noise (L Aeq,24h) |
Longitudinal, data from the HYENA study, Greece | N = 420, 45–70 years, incidental hypertension |
Sex, age, smoking, BMI, education, exercise, alcohol, salt consumption |
OR per 10 dB(A) Lnight Aircraft noise: 2.63 [95% CI: 1.21; 5.71] OR per 10 dB(A) L Aeq,16h Aircraft noise: 1.46 [95% CI: 0.89; 2.39] OR per 10 dB(A) L Aeq,24h Road traffic noise: 1.18 [95% CI: 0.92; 1.52] |
| Fuks, 2017 (27) |
Road traffic noise (L den) |
Longitudinal, data from the ESCAPE study, Norway, Sweden, Denmark, Germany, Spain | N = 41 072, 47–71 years (mean), incidental hypertension |
Age, sex, education, working situation, BMI, smoking, alcohol, exercise, family history of hypertension, SES | RR per 10 dB(A) Lden Self-reported hypertension: 1.03 [95% CI: 0.99; 1.07] Measured hypertension: 0.99 [95% CI: 0.94; 1.04] |
| Seidler, 2016 (28) |
Aircraft, road traffic, and rail traffic noise (L Aeq,24h) |
Population-based case–control study, data from the NORAH study, Germany | N = 854 366 (19 632 cases, 834 734 controls), 40 years, MI diagnosis |
Age, sex, social status,education, occupation | OR per 10 dB(A) LAeq,24h Aircraft noise: 0.993 [95% CI: 0.966; 1.020] Road traffic noise: 1.028 [95% CI: 1.012; 1.045] Rail traffic noise: 1.023 [95% CI: 1.005; 1.042] |
| Seidler, 2016 (29) |
Aircraft, road traffic, and rail traffic noise (L Aeq,24h) |
Population-based case–control study, data from the NORAH study, Germany | N = 758 857 (104 145 cases, 654 172 controls), 40 years, diagnosis of heart failure or hypertensive heart disease |
Age, sex, social status,education, occupation | OR per 10 dB(A) LAeq,24h Aircraft noise: 1.016 [95% CI: 1.003; 1.030] Road traffic noise: 1.024 [95% CI: 1.016; 1.032] Rail traffic noise: 1.031 [95% CI: 1.022; 1.041] |
| Zeeb, 2017 (30) |
Aircraft, road traffic, and rail traffic noise (L Aeq,24h) |
Population-based case–control study, data from the NORAH study, Germany | N = 493 168 (137 577 cases, 355 591 controls), 40 years, newly diagnosed hypertension |
Age, sex, SES, education, occupation | OR per 10 dB(A) LAeq,24h Aircraft noise: 0.997 [95% CI: 0.985; 1.010] Road traffic noise: 1.003 [95% CI: 0.995; 1.011] Rail traffic noise: 1.003 [95% CI 0.994; 1.011] |
Epidemiological primary studies were selected for this tabular presentation.
AF, atrial fibrillation; BMI; body mass index; CI, confidence interval; HR, hazard ratio; IQR, interquartile range; IRR, incidence rate ratio;
L den weighted day (7 a.m. to 7 p.m.)–evening (7 to 11 p.m.)–night (11 p.m. to 7 a.m.) sound level over a 24-h period, with an increment of 5 dB(A) for the evening and 10 dB(A) for the night;
L night noise level at night (11 p.m. to 7 a.m.);
L Aeq,24/16h Unw eighted level over a period of 24 h or 16 h (usually 7 a.m. to 11 p.m.);
L Amax maximum level over a certain period
MI, myocardial infarction; NO2, nitrogen dioxide; NOx, nitrogen oxides; OR, odds ratio; PM2.5, particulate matter with diameter less than 2.5 µm; SES, socioeconomic status
Coronary heart disease
Three meta-analyses have shown that traffic noise leads to a significant increase in coronary heart disease (13– 15). The meta-analysis published by Vienneau et al. in 2015 covered studies on the link between noise from aircraft and road traffic and the incidence of coronary heart disease (13). For traffic noise, they found a pooled relative risk (RR) of 1.06 [1.03; 1.09] starting at 50 dB(A) and per increase of 10 dB(A) Lden (weighted day [7 a.m. to 7 p.m.]—evening [7 to 11 p.m.]—night [11 p.m. to 7 a.m.] noise level over a period of 24 h, with an increment of 5 dB[A] added for the evening period and 10 dB[A] for the night). This effect persisted after correction for airborne toxins (mostly nitrogen oxides [NOX] or nitrogen dioxide [NO2], documented in a subgroup of studies) and exclusion of studies with no data on smoking behavior. The meta-analysis by Babisch came to a similar conclusion, with RR 1.08 [1.04; 1.13]—starting at 52 dB(A) and per increase of 10 dB(A) Lden road traffic noise (weighted day–night level for a period of 24 h, with an increment of 10 dB[A] added for the night) (14). In a WHO study published in 2018, the investigators analyzed longitudinal studies and found that road traffic noise, starting at 50 dB(A) and per increase of 10 dB(A), raised the incidence of coronary heart disease by 8% [1.01; 1.15] (15).
Because increasing traffic not only represents a noise problem but also leads to greater emission of air pollutants, it is necessary to ascertain the independent effects of these two variables. Despite the high correlation of the two parameters, the assumption is that noise and air pollutants have independent negative impacts on the cardiovascular system (16).
Myocardial infarction
Cohort studies that controlled for air pollutants, socioeconomic status, and lifestyle factors identified a significant association between road traffic noise and the occurrence of myocardial infarctions (17, 18). The data from a large Danish cohort (N = 50 744) showed that exposure to road traffic noise (10-year mean), independent of the air NO2 concentration, was associated with a hazard ratio (HR) of 1.12 [1.03; 1.21] per interquartile range Lden (17). The findings were similar in a Swedish cohort (OR 1.38 [1.11; 1.71] for road traffic noise = 50 vs. <50 dB(A) LAeq,24h [unweighted 24-h level] after exclusion of persons with hearing loss or exposure to other sources of noise (18).
In a nationwide cohort study in Switzerland (N = 4 415 206), the authors investigated the influence of noise from aircraft, road traffic, and rail traffic on cardiovascular mortality (19). The strongest associations were observed for death from myocardial infarction, with an HR of 1.038 [1.019; 1.058] for road traffic noise, 1.018 [1.004; 1.031] for noise from rail traffic, and 1.026 [1.004; 1.048] for aircraft noise, starting at 30 dB(A) (for rail traffic and aircraft noise) or 35 dB(A) (for road traffic) and per increase of 10 dB(A) Lden with correction for air concentrations of NO2.
Analysis of a Danish cohort (N = 57 053) showed that road traffic noise, starting at 42 dB(A) (N = 57 053) and per increase of 10 dB(A) Lden, increases the incidence of myocardial infarction by 12% (incidence rate ratio [IRR] [1.02; 1.22]) independent of air NOX concentration, smoking behavior, education, and style of nutrition (20).
Stroke
In a large cohort study (N = 57 053), Sørensen et al. found that, starting at 55 dB(A) and per increase of 10 dB(A) Lden, road traffic noise increases the risk of stroke by 14% (IRR [1,03; 1,25]), independent of air NOX concentration, smoking behavior, style of nutrition, and alcohol consumption (21). However, this association was not observed in younger persons (<64.5 years) (IRR 1.02 [0.91; 1.14]). A large study including 3.6 million inhabitants of the area around Heathrow Airport near London, UK demonstrated that aircraft noise, after controlling for age, sex, and lifestyle factors, was dose-dependently associated with increased hospitalization due to stroke both during the day (LAeq,16h, level over a period of 16 h, 7 a.m. to 11 p.m.) and at night (Lnight, from 11 p.m. to 7 a.m.). The risk of hospitalization was greater for aircraft noise at night (RR 1.29 [1.14; 1.46]) than during the day (RR 1.24 [1.08; 1.43]) when comparing high and low noise exposure (night: >55 vs. = 50 dB[A]; day: >63 vs. = 51 dB[A]) (22). The results for stroke-related mortality in this study were similar even after taking account of particulates (PM10, particle diameter less than 10 µm). This pattern of findings suggests that particularly aircraft noise at night is associated with greater stress on the cardiovascular system. Another study carried out in London, this time including 8.6 million members of the population, revealed that after controlling for particulate pollution (PM2.5), road traffic noise (>60 vs. <55 dB[A]) during the day (LAeq,16h) was associated with an elevated risk of stroke-related hospitalization in persons aged = 25–74 years (RR 1.05 [1.02; 1.09]) and in those = 75 (RR 1.09 [1.04; 1.14]) (23). Moreover, road traffic noise (>60 vs. <55 dB[A]) during the day was significantly associated with overall mortality (RR 1.04 [1.00; 1.07]), although the association with cardiovascular mortality did not attain significance (RR 1.03 [0.98; 1.07]).
Hypertension
A meta-analysis of 24 studies by van Kempen and Babisch revealed that road traffic noise is associated with an elevated risk of the occurrence of high blood pressure (OR 1.034 [1.011; 1.056], starting at 45 dB(A) and per increase of 5 dB(A) LAeq,16h ) (24). This analysis was restricted to cross-sectional studies, so the power of any conclusions about the causal role of noise is limited. However, large prospective studies have demonstrated that both aircraft noise and road traffic noise exposure are associated with an increased risk of hypertension (25– 27), with stronger effects for aircraft noise at night (OR 2.63 [1.21; 5.71] per increase of 10 dB(A) Lnight) than for road traffic noise (RR 1.03 [0.99; 1.07] per increase of 10 dB(A) Lden) (27).
Other endpoints
The investigators involved in the NORAH study (Noise-Related Annoyance, Cognition, and Health) of persons resident in the Rhine–Main region (in and around Darmstadt, Mainz, and Worms) found that traffic noise was associated with an increased risk of heart failure or hypertensive heart disease (greatest increase in risk, of 3.1% for rail traffic noise per increase of 10 dB(A) LAeq,24h [2.2; 4.1%]) and of myocardial infarction (greatest increase in risk, of 2.8% for road traffic noise per increase of 10 dB[A] LAeq,24h [1.2; 4.5%]) (28, 29). Analyses of the risk of hypertension, however, showed no significant associations with noise exposure from aircraft, road traffic, or rail traffic, although it must be pointed out that the study suffered from methodological deficiencies in blood pressure measurement and limited inclusion of confounding factors (30).
In addition, a Danish prospective study (N = 57 053) showed that road traffic noise is associated with an increased incidence of atrial fibrillation (IRR: 1.06 [1.00; 1.12] starting at 40 dB(A) and per increase of 10 dB(A) Lden); however, this effect was not independent of the air concentration of NOX or NO2 (after controlling for NOX, IRR: 1.04 [0.96; 1.11]; after controlling for NO2, IRR: 1.01 [0.94; 1.09]) (31).
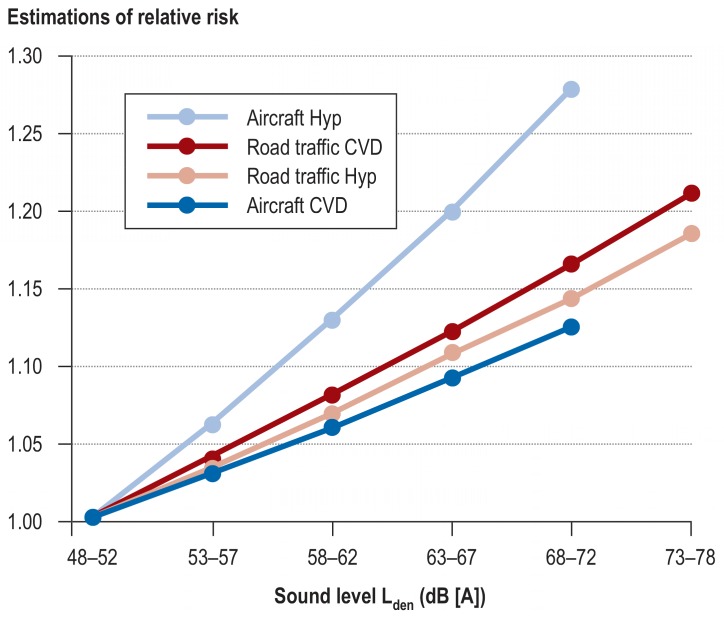
In conclusion, it can be stated that large studies of high methodological quality that controlled for airborne pollutants, lifestyle factors, and other important confounding factors were able to demonstrate a systematic association of exposure to traffic noise with the risk of cardiovascular disease (figure 3).
Figure 3.
Dose–response relationships for noise and cardiovascular disease. Lden is the weighted day–evening–night sound level, with an increment of 5 dB(A) for the evening and 10 dB(A) for the night. CVD, cardiovascular disease; Hyp, hypertension. (Modified from Münzel et al. [4]. Reproduced with the permission of the publisher. Copyright © 2014, Oxford University Press)
Noise-induced pathophysiological effects on the cardiovascular system
The pathophysiological mechanisms by which noise causes more cardiovascular illness have not yet been fully elucidated and are a topic of ongoing research (box). The assumption is that long-term noise leads to stress reactions or noise annoyance reactions, which in turn, via activation of the sympathetic nervous system and increased excretion of stress hormones (5, 9), favors the development of oxidative stress and inflammatory processes, resulting in disruption of vascular and endothelial function (32– 34). As well as the emergence of endothelial dysfunction and the associated negative impact on blood pressure regulation, the noise-related development of further risk factors such as elevated blood pressure, rises in blood lipids and blood sugar, increased cardiac output, raised blood viscosity, and activation of blood coagulation leads to a higher risk of cardiovascular disease (4).
BOX. Noise-related endothelial dysfunction.
Only a small number of studies have explicitly explored the association between noise and endothelial function. In two recent studies, Schmidt et al. demonstrated that simulated aircraft noise at night (30 or 60 flights overhead, peak noise level 60 dB[A], mean level 43 or 46 dB[A]) led to deterioration of vascular function (measured as flow-mediated vasodilation), elevated levels of stress hormone (epinephrine), and lower sleep quality both in healthy probands and in patients with coronary heart disease (32, 33). In two recently published animal studies in mice, the investigators uncovered, for the first time, the molecular mechanisms of noise-induced vascular function disorder (35, 36). Münzel et al. showed that simulated aircraft noise (recorded previously and played over a loudspeaker system) led within 4 days to a marked increase in the stress hormone concentration, elevated blood pressure, alteration of gene expression in the vascular wall, and disturbance of vascular function that was attributable particularly to increased formation of free radicals and thus oxidative stress (35). The authors identified two radical-forming enzymes that played a crucial part in induction of the vascular function disorders: nicotinamide adenine dinucleotide phosphate oxidase (NADPH oxidase) and nitric oxide synthase (NOS). The noise-related dysregulation of these factors facilitated the formation of reactive oxygen species, which led directly to decreased vascular bioavailability of nitric oxide (NO), resulting in deterioration of endothelial function. A follow-up study by Kröller-Schön et al. went on to demonstrate that the vascular injuries are accompanied by cerebral changes. Notably, these were found after exposure of the mice to noise in their sleeping phase, but not during the waking phase (36). A newly published WHO meta-analysis shows that traffic noise significantly increases the risk of sleep disorders, to the point where noise-induced reduction and fragmentation of sleeping time may represent an important factor in the mediation of cardiovascular disease (37). Findings from the SAPALDIA study (Swiss Cohort Study on Air Pollution and Lung and Heart Diseases in Adults) also showed that the frequency of traffic noise events, especially during the night, is associated with increased arterial stiffness, an important marker of vascular dysfunction (38).
Summary and conclusion
Epidemiological studies have shown that noise from aircraft, road traffic, and rail traffic represents a significant risk factor for the development of cardiovascular disease. The research involved in these studies has identified important pathophysiological factors that will enable development of drug treatment strategies to minimize the harmful effects of noise on the human organism. Particularly on the basis of the new WHO noise guidelines (3), which, in summary, state an RR of 1.08 [1.01; 1.15] for the occurrence of coronary heart disease, starting at 50 dB(A) and per increase of 10 dB(A) Lden in connection with recommendations for much lower mean noise levels during the day and at night (aircraft noise: 45 dB[A] Lden and 40 dB[A] Lnight; road traffic: 53 dB[A] Lden and 45 dB[A] Lnight; rail traffic: 54 dB[A] Lden and 44 dB[A] Lnight), it is urgently necessary to introduce measures for adequate protection of the population from the negative health effects of environmental noise.
Limitations
Our goal in writing this article was to give a selective overview of the most important recent research findings, reviewing systematic analyses and large cohort studies in the light of our own experience. This approach entails limitations, particularly due to the selective inclusion of primary studies and meta-analyses that vary with regard to quality of results, controlling for confounding factors, operationalization of endpoints, and statistical methods, making it difficult to compare their findings. Nevertheless, overall the results of the studies presented here reinforce the contention that noise significantly increases the occurrence of cardiovascular disease.
Key Messages.
Epidemiological studies show that traffic noise raises the risk of cardiovascular diseases such as hypertension, coronary heart disease, myocardial infarction, heart failure, and stroke.
Sustained noise causes stress reactions that bring about activation of the autonomic and endocrine system, resulting per se in increased formation of cardiovascular risk factors.
At the pathophysiological level, particularly traffic noise at night causes oxidative stress and inflammatory processes in the brain, which in turn impact negatively on the vascular system and result in endothelial dysfunction and hypertension.
Traffic noise is an important new risk factor for cardiovascular illness.
Effective preventive measures are needed to protect the population from the negative health effects of noise.
Acknowledgments
Translated from the original German by David Roseveare
Footnotes
Conflict of interest statement
Prof. Daiber coordinated third-party funding for a research project from the Boehringer-Ingelheim Foundation and the Mainzer Herz Foundation.
The remaining authors declare that no conflict of interest exists.
References
- 1.Bull HP. Was sagt die medizinische Wissenschaft zur Geräuschbelästigung? Ausgabe vom 11. Januar 1963. www.zeit.de/1963/02/was-sagt-die-medizinische-wissenschaft-zur-geraeuschbelaestigung (last accessed on 14 January 2019) [Google Scholar]
- 2.Cohen AJ, Brauer M, Burnett R, et al. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the Global Burden of Diseases Study 2015. Lancet. 2017;389:1907–1918. doi: 10.1016/S0140-6736(17)30505-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO. Environmental noise guidelines for the European Region (2018) www.euro.who.int/en/publications/abstracts/environmental-noise-guidelines-for-the-european-region-2018 (last accessed on 14 January 2019) [Google Scholar]
- 4.Munzel T, Gori T, Babisch W, Basner M. Cardiovascular effects of environmental noise exposure. Eur Heart J. 2014;35:829–836. doi: 10.1093/eurheartj/ehu030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Babisch W. Cardiovascular effects of noise. Noise Health. 2011;13:201–204. doi: 10.4103/1463-1741.80148. [DOI] [PubMed] [Google Scholar]
- 6.European Topic Centre on Air Pollution and Climate Change Mitigation (ETC/ACM) Health impact assessment for noise in Europe 2014. https://acm.eionet.europa.eu/reports/docs/ETCACM_TP_2014_9_HIA-noise_europe.pdf (last accessed on 14 January 2019) [Google Scholar]
- 7.WHO. Burden of disease from environmental noise Quantification of healthy life years lost in Europe 2011. www.euro.who.int/__data/assets/pdf_file/0008/136466/e94888.pdf (last accessed on 14 January 2019) [Google Scholar]
- 8.Basner M, Babisch W, Davis A, et al. Auditory and non-auditory effects of noise on health. Lancet. 2014;383:1325–1332. doi: 10.1016/S0140-6736(13)61613-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Babisch W. Stress hormones in the research on cardiovascular effects of noise. Noise Health. 2003;5:1–11. [PubMed] [Google Scholar]
- 10.Babisch W, Pershagen G, Selander J, et al. Noise annoyance—a modifier of the association between noise level and cardiovascular health? Sci Total Environ. 2013:452–453. doi: 10.1016/j.scitotenv.2013.02.034. 50-7. [DOI] [PubMed] [Google Scholar]
- 11.Hahad O, Beutel M, Gori T, et al. Annoyance to different noise sources is associated with atrial fibrillation in the Gutenberg Health Study. Int J Cardiol. 2018;264:79–84. doi: 10.1016/j.ijcard.2018.03.126. [DOI] [PubMed] [Google Scholar]
- 12.Beutel ME, Junger C, Klein EM, et al. Noise annoyance is associated with depression and anxiety in the general population—the contribution of aircraft noise. PLoS One. 2016;11 doi: 10.1371/journal.pone.0155357. e0155357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vienneau D, Schindler C, Perez L, Probst-Hensch N, Roosli M. The relationship between transportation noise exposure and ischemic heart disease: a meta-analysis. Environ Res. 2015;138:372–380. doi: 10.1016/j.envres.2015.02.023. [DOI] [PubMed] [Google Scholar]
- 14.Babisch W. Updated exposure-response relationship between road traffic noise and coronary heart diseases: a meta-analysis. Noise Health. 2014;16:1–9. doi: 10.4103/1463-1741.127847. [DOI] [PubMed] [Google Scholar]
- 15.Kempen EV, Casas M, Pershagen G, Foraster M. WHO Environmental noise guidelines for the European region: a systematic review on environmental noise and cardiovascular and metabolic effects: a summary. Int J Environ Res Public Health. 2018;15 doi: 10.3390/ijerph15020379. pii: E379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stansfeld SA. Noise effects on health in the context of air pollution exposure. Int J Environ Res Public Health. 2015;12:12735–12760. doi: 10.3390/ijerph121012735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Roswall N, Raaschou-Nielsen O, Ketzel M, et al. Long-term residential road traffic noise and NO2 exposure in relation to risk of incident myocardial infarction—a danish cohort study. Environ Res. 2017;156:80–86. doi: 10.1016/j.envres.2017.03.019. [DOI] [PubMed] [Google Scholar]
- 18.Selander J, Nilsson ME, Bluhm G, et al. Long-term exposure to road traffic noise and myocardial infarction. Epidemiology. 2009;20:272–279. doi: 10.1097/EDE.0b013e31819463bd. [DOI] [PubMed] [Google Scholar]
- 19.Heritier H, Vienneau D, Foraster M, et al. Transportation noise exposure and cardiovascular mortality: a nationwide cohort study from Switzerland. Eur J Epidemiol. 2017;32:307–315. doi: 10.1007/s10654-017-0234-2. [DOI] [PubMed] [Google Scholar]
- 20.Sørensen M, Andersen ZJ, Nordsborg RB, et al. Road traffic noise and incident myocardial infarction: a prospective cohort study. PLoS One. 2012;7 doi: 10.1371/journal.pone.0039283. e39283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sørensen M, Hvidberg M, Andersen ZJ, et al. Road traffic noise and stroke: a prospective cohort study. Eur Heart J. 2011;32:737–744. doi: 10.1093/eurheartj/ehq466. [DOI] [PubMed] [Google Scholar]
- 22.Hansell AL, Blangiardo M, Fortunato L, et al. Aircraft noise and cardiovascular disease near Heathrow airport in London: small area study. BMJ. 2013;347 doi: 10.1136/bmj.f5432. f5432. [DOI] [PubMed] [Google Scholar]
- 23.Halonen JI, Hansell AL, Gulliver J, et al. Road traffic noise is associated with increased cardiovascular morbidity and mortality and all-cause mortality in London. Eur Heart J. 2015;36:2653–2661. doi: 10.1093/eurheartj/ehv216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.van Kempen E, Babisch W. The quantitative relationship between road traffic noise and hypertension: a meta-analysis. J Hypertens. 2012;30:1075–1086. doi: 10.1097/HJH.0b013e328352ac54. [DOI] [PubMed] [Google Scholar]
- 25.Eriksson C, Rosenlund M, Pershagen G, Hilding A, Ostenson CG, Bluhm G. Aircraft noise and incidence of hypertension. Epidemiology. 2007;18:716–721. doi: 10.1097/EDE.0b013e3181567e77. [DOI] [PubMed] [Google Scholar]
- 26.Dimakopoulou K, Koutentakis K, Papageorgiou I, et al. Is aircraft noise exposure associated with cardiovascular disease and hypertension? Results from a cohort study in Athens, Greece. Occup Environ Med. 2017;74:830–837. doi: 10.1136/oemed-2016-104180. [DOI] [PubMed] [Google Scholar]
- 27.Fuks KB, Weinmayr G, Basagana X, et al. Long-term exposure to ambient air pollution and traffic noise and incident hypertension in seven cohorts of the European study of cohorts for air pollution effects (ESCAPE) Eur Heart J. 2017;38:983–990. doi: 10.1093/eurheartj/ehw413. [DOI] [PubMed] [Google Scholar]
- 28.Seidler A, Wagner M, Schuber Mt, et al. Myocardial infarction risk due to aircraft, road and rail traffic noise—results of a case-control study based on secondary data. Dtsch Arztebl Int. 2016;113:407–414. doi: 10.3238/arztebl.2016.0407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Seidler A, Wagner M, Schubert M, et al. Aircraft, road and railway traffic noise as risk factors for heart failure and hypertensive heart disease—a case-control study based on secondary data. Int J Hyg Environ Health. 2016;219:749–758. doi: 10.1016/j.ijheh.2016.09.012. [DOI] [PubMed] [Google Scholar]
- 30.Zeeb H, Hegewald J, Schubert M, et al. Traffic noise and hypertension—results from a large case-control study. Environ Res. 2017;157:110–117. doi: 10.1016/j.envres.2017.05.019. [DOI] [PubMed] [Google Scholar]
- 31.Monrad M, Sajadieh A, Christensen JS, et al. Residential exposure to traffic noise and risk of incident atrial fibrillation: a cohort study. Environ Int. 2016:92–93. doi: 10.1016/j.envint.2016.04.039. 457-63. [DOI] [PubMed] [Google Scholar]
- 32.Schmidt F, Kolle K, Kreuder K, et al. Nighttime aircraft noise impairs endothelial function and increases blood pressure in patients with or at high risk for coronary artery disease. Clin Res Cardiol. 2015;104:23–30. doi: 10.1007/s00392-014-0751-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schmidt FP, Basner M, Kroger G, et al. Effect of nighttime aircraft noise exposure on endothelial function and stress hormone release in healthy adults. Eur Heart J. 2013;34:3508. doi: 10.1093/eurheartj/eht269. 14a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Charakida M, Deanfield JE. Nighttime aircraft noise exposure: flying towards arterial disease. Eur Heart J. 2013;34:3472–3474. doi: 10.1093/eurheartj/eht339. [DOI] [PubMed] [Google Scholar]
- 35.Munzel T, Daiber A, Steven S, et al. Effects of noise on vascular function, oxidative stress, and inflammation: mechanistic insight from studies in mice. Eur Heart J. 2017;38:2838–2849. doi: 10.1093/eurheartj/ehx081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kröller-Schön S, Daiber A, Steven S, et al. Crucial role for Nox2 and sleep deprivation in aircraft noise-induced vascular and cerebral oxidative stress, inflammation, and gene regulation. Eur Heart J. 2018;39:3528–3539. doi: 10.1093/eurheartj/ehy333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Basner M, McGuire S. WHO environmental noise guidelines for the European region: a systematic review on environmental noise and effects on sleep. Int J Environ Res Public Health. 2018;15 doi: 10.3390/ijerph15030519. pii: E519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Foraster M, Eze IC, Schaffner E, et al. Exposure to road, railway, and aircraft noise and arterial stiffness in the SAPALDIA Study: Annual average noise levels and temporal noise characteristics. Environ Health Perspect. 2017;125 doi: 10.1289/EHP1136. 097004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Munzel T, Sorensen M, Gori T, et al. Environmental stressors and cardio-metabolic disease: part I-epidemiologic evidence supporting a role for noise and air pollution and effects of mitigation strategies. Eur Heart J. 2017;38:550–556. doi: 10.1093/eurheartj/ehw269. [DOI] [PubMed] [Google Scholar]