Abstract
Background
There have been many individual studies on the question whether aircraft noise is a risk factor for stroke, but until now there has not been any summary of the current state of the evidence of adequately high methodological quality.
Methods
In a systematic review and meta-analysis (PROSPERO registry number CRD42013006004), we evaluated the relation between address-based aircraft noise exposure and the incidence of stroke. A systematic literature search was performed in the MEDLINE, EMBASE, and BIOSIS databases including publications up to August 2017. Two of the authors, working independently of each other, screened the titles, abstracts, and full texts for eligible articles and evaluated the quality of the included studies on a three-level scale. The change of risk per 10 dB increase in the weighted mean aircraft noise level (LDEN) was calculated. LDEN is a noise level indicator with additional weighting of evening and nighttime noise.
Results
Of the nine studies that met the inclusion criteria, seven were suitable for inclusion in the meta-analysis. The result of the meta-analysis indicated a relative stroke risk of 1.013 (95% confidence interval, [0.998; 1.028]) per 10 dB increase in LDEN, corresponding with an estimated 1.3% increase in the risk of stroke for each additional 10 dB of aircraft noise. The underlying studies were of poor to medium quality. The analyses of the studies included adjustments for various combinations of confounders, including age, sex, ethnicity, and socioeconomic status.
Conclusion
The present meta-analysis indicates that aircraft noise increases the risk of stroke, even if the overall finding just fails to reach statistical significance. The differing measures of exposure in the included studies, the lack of differentiation between ischemic and hemorrhagic stroke, and the lack of consideration of maximum noise levels are all factors that may have led to a marked underestimation of the risk of stroke.
The health effects of noise are a highly relevant problem for the population. The World Health Organization (WHO) estimates that in the European Union and Western Europe the number of healthy life years lost due to environmental noise exceeds one million (disability-adjusted life years, DALYs) (1). Environmental noise-related sleep disturbances are presumably the greatest problem with more than 900 000 DALYs; the WHO report estimates that noise-related ischemic heart disease accounts for 61 000 DALYs. The WHO report does not provide a corresponding estimate for cerebrovascular events. Furthermore, the various individual sources of noise are not considered separately in the WHO report.
The German Federal Environmental Agency set as an average target to reduce noise pollution to 55 dB during the day and 45 dB during nighttime to prevent considerable annoyance (e1). Based on noise mapping information (e2), 8.7 million people in Germany are exposed to road noise of day–evening–night noise levels (LDEN) of more than 55 dB. For 6.4 million people, an LDEN of 55 dB is exceeded by rail traffic and for 0.8 million by air traffic. According to a representative survey from 2016 (e3), 76% of the German population feels disturbed or annoyed by road noise, and the same applies to 44% and 34% for aircraft noise and rail traffic noise, respectively.
Pathophysiologically, the cardiovascular effects of noise have been attributed to an activation of the autonomous nervous system with subsequent release of stress hormones (norepinephrine, epinephrine, cortisol); most of the supporting data are from experimental studies. These neuroendocrinological mechanisms can trigger or promote abnormal processes, such as increases in blood pressure and insulin resistance (e4). Disturbed sleep at night with subsequent daytime sleepiness and impaired regenerative processes may be of special importance in chronic stress reactions caused by noise pollution (e5, e6). While a causal relationship between noise and cardiovascular morbidity appears biologically plausible, it remains unclear whether the postulated effects can cause a measurable increase in stroke incidence that is also potentially detectable at the population level.
There is no current systematic review of the evidence on the relationship between aircraft noise and stroke incidence available at present. The design and methodological quality of the available individual studies are as heterogeneous as their results. Both cohort studies (for example [2]) and cross-sectional studies (for example [3]) have been reported. Some studies evaluate noise exposure as a continuous variable, other studies as a categorical variable with various intervals and cut-offs. In some studies, the endpoints were recorded as ICD-coded (ICD, International Classification of Diseases and Related Health Problems) hospital diagnoses or deaths determined by physicians (for example [4, 5]), while other studies rely solely on patient-reported information (for example [3]). Reviewing the individual studies identified mostly statistically non-significant risk estimates. The aim of this systematic review is to present the currently available evidence on the aircraft noise-related stroke risk.
Methods
Research question and inclusion criteria
This systematic review addresses the question whether noise due to civil air traffic or the perceived annoyance caused by it has an effect on the risk of fatal or non-fatal stroke (cerebrovascular accident) in humans. The research question was operationalized by means of a detailed a priori specification of the population, exposure and assessed endpoints. The inclusion and exclusion criteria are detailed in Table 1.
Table 1. Inclusion and exclusion criteria.
| Category | Inclusion criteria | Exclusion criteria |
| Population | General population (children and adults, male and female) | Vocationally exposed persons; self-selected persons (who offer to participate in the study of their own accord, e.g. volunteers, recruitment via newspaper ads, etc.) |
| Exposure | Environmental aircraft noise, annoyance by environmental aircraft noise | Noise from industrial activities, road traffic, rail traffic, neighborhood; exclusively military aircraft noise |
| Endpoints | Overall project*: ● non-auditory health problems and diseases ● effects on human health (incidence/prevalence) ● mixed and non-diagnosis-specific health endpoints (e.g. health problems in general) ● stress (e.g. Lewis Child Stress Scale, stress hormone measurement) | Auditory noise effects (e.g. hearing loss, tinnitus) |
| Subproject*: fatal and nonfatal cerebrovascular accident (stroke) | ||
| Study design/ publication | Cohort studies, case-control studies, cross-sectional studies, ecological studies | Reviews, editorials, letters to the editor |
* The study is part of a large review project, evaluating effects of aircraft noise on a broad spectrum of non-auditory endpoints and diseases. The results for the endpoint “stroke“ are the subject of this article.
Search strategy
We performed a systematic electronic literature search in the MEDLINE (publications from 1947), EMBASE (publications from 1974) and BIOSIS (publications from 1969) bibliographic databases up to 31 August 2017, and complemented this with a manual search. Only original studies with an available abstract were included. No language limitations were imposed. With regard to study design, the search included cohort studies, case-control studies, cross-sectional studies, and ecological studies.
For the database search, the search strategy was adapted to the respective database, and is shown in eBox 1. In addition, a manual search was conducted in references of included publications, narrative reviews and key publications, as well as an online search using the citation-tracking function of the Google Scholar search engine (6, 7).
eBOX 1. Search strategy in MEDLINE (via PubMed).
((Noise[tw] OR noise[MH]) AND (aircraft OR jet OR flight OR “air traffic”)) AND (Epidemiologic Studies[MH] OR Odds Ratio [MH] OR observational stud*[tw] OR cohort stud*[tw] OR cohort analy*[tw] OR follow up stud*[tw] OR prospective stud* OR incidence stud*[tw] OR Longitudinal[tw] OR Case control[tw] OR Case-control[tw] OR Retrospective stud*[tw] OR cross-sectional stud*[tw] OR prevalence stud*[tw] OR ecological stud*[tw] OR correlation analys*[tw] OR incidence OR prevalence) NOT (letter[tw] OR editorial[tw] OR comment [tw]) NOT ((animals[Mesh:noexp]) NOT (humans[Mesh])) AND (“1“[PDat] : “2017/08/31“[PDat])
Literature screening
The screening of the titles, abstracts and full-text articles of the publications identified was performed by two authors independently of each other (VMW, AS); in case of diverging judgment, a third person (UE) was consulted. The reasons for excluding full-text articles were documented for each publication not included.
Data extraction
The data of the included studies were entered into an extraction table created a priori. The authors responsible for screening the literature (VMW, AS) performed the data extraction. Differences were discussed in consensus conferences. In case of incomplete data, the authors of the corresponding publication were contacted and asked to provide additional information.
Quality evaluation
The study quality was also assessed by two authors (VMW, AS) independently of each other, using an instrument which had been developed based on SIGN (Scottish Intercollegiate Guidelines Network 2004) and CASP (Critical Appraisal Skills Program 2004/2006) and which had been successfully used in several earlier reviews (among others in [8–13]). The instrument was adapted to the aircraft noise topic. The assessment included a summary quality rating on a three-step scale (++, +, -). In cases where the potential effect of methodological weaknesses on the core results of the study appeared to be significant, the respective studies were classified as “of low methodological quality (-)”.
Data synthesis and statistical analysis
In preparation of the quantitative analysis, data were processed and converted. This included, among others, transformation of noise metrics of all studies included in the meta-analysis to the average noise level LDEN. LDEN is the weighted day-evening-night level with an extra 5 dB being added to noise in the evening hours and 10 dB to the nighttime hours. For the transformation, the conversion rules of the WHO working paper by Brink (14) were used. These rules are based on aircraft noise measurements. An overview of the noise metrics and their definitions in provided in eTable 1.
eTable 1. Noise metrics and their definitions*1.
| Abbreviation | Definition |
| dB | Logarithmic scale for sound pressure levels |
| Leq | Average value of an energy-equivalent continuous sound level over a period of time |
| LAeq | A-weighted Leq |
| LDay | LAeq for daytime hours (usually 7:00 am – 7:00 pm)*2 for all day periods of a year |
| LEvening | LAeq for evening hours (usually 7:00 pm – 11:00 pm)*2 for all evening hours of a year |
| LNight | LAeq for nighttime hours (usually 11:00 pm – 7:00 am)*2 for all nighttime hours of a year |
| LDN | All 24 h LAeq periods of a year with additional 10 dB for nighttime noise annoyance (usually from 11:00 pm –7:00 am)*2 |
| LDEN | All 24 h LAeq periods of a year with additional 5 dB for evening hours (8:00 pm – 10:00 pm or 7:00 pm – 11:00 pm)*2 and additional 10 dB for nighttime hours (10:00 pm – 6:00 am or from 11:00 pm – 7:00 am)*2 |
| NAT6 | Maximum level which is exceeded six times above 50 dB without upper limit during the night (from 10:00 pm – 6:00 am). At the same time, the 24 h continuous sound level is below 40 dB. |
*1 adapted according to directive 2002/49/EC
(European Parliament and European Council, 2002)
*2 In Germany, normal sleeping hours are defined in the respective federal states immission control legislation and usually encompasses the period from 10:00 pm – 6:00 am. Therefore, German studies (e.g. NORAH study) sometimes deviate from the periods for L Day /L Evening /L Night listed in eTable 1 and instead use the periods stipulated in the legislation.
The statistical software Stata (version 14.1) was used to determine the potential dose-response relationships from the studies’ results and for the meta-analysis conducted using the random-effects model.
In the core analysis, the linear change of the effect estimate with each increase in the LDEN noise level by 10 dB was assessed. For this, the data of the studies with continuous exposure measurements—after transformation to LDEN, if necessary—were directly integrated into the model. In studies with categorical noise intervals and various corresponding risk estimates, the change in risk for each 10 dB increase in aircraft noise levels was first calculated using the Stata function glst (method of generalized least squares [16]). For this, the risk estimates reported in the studies were allocated to the mean dB of the respective exposure category. If it was not possible to specify the covariance matrix, the Stata vwls procedure was used instead. Next, the studies were pooled using a random-effects model (Stata metan [15]).
In order to assess the impact of individual studies on the pooled effect estimate, a sensitivity analysis was conducted excluding one study at a time from the meta-analysis (leave-one-out method) (17).
Further details on the methodology are provided in eBox 2.
eBOX 2. Supplementary methodology information.
• General
This review was performed according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement (e7).
The study protocol was published in advance in the International Prospective Register of Systematic Reviews (PROSPERO) under the registration number CRD42013006004 (e8).
• Data synthesis and statistical analysis
Similar to the approach taken in other meta-analyses (e.g. [e9]), the various effect estimates (risk ratio [RR], standardized mortality ratio [SMR], hazard ratio [HR], odds ratio [OR]) of the individual studies were altogether regarded as estimates of the risk ratio. They were included unchanged in the creation of an aggregated risk estimate. Since stroke is a comparatively rare event on the population level (incidence far below 10%), it was possible to interpret odds ratios as risk ratios (e10) and include them in the meta-analysis.
In order to be able to perform a quantitative meta-analysis, the various exposure measures of the individual studies had first to be transformed, using conversion formulas, to the exposure measure LDEN, i.e. to a weighted average level which adds a “penalty” for the evening and especially night hours, based on the assumption that during these times the negative effect of noise is particularly strong. Such “penalties” are normally specified in directives. The directive 2002/49/EC of the European Parliament and of the Council, for example, defines the noise measure LDEN and prescribe for evening hours a “penalty” of 5 dB and night hours a penalty of 10 dB. Thus, the definition of LDEN combines the objectively measured aircraft noise with the subjective component of perceived annoyance (penalties for evening and night hours). Pathophysiologically, these “penalties” are justified in particular by the disturbance of sleep architecture which has also been discussed as a risk factor for stroke (e11). On the other hand, when data from studies using different exposure measures are transformed into LDEN for the sake of pooling and comparability, this inevitably means that information is lost: The conversion formulas cannot adequately reflect the peculiarities of an aircraft noise-exposed area (e.g., the existence of a ban on night flights or the number of flights in the evening and morning “shoulder” hours).
Furthermore, the precision of exposure identification varies between the studies included in this review with the magnitude of the noise map resolutions (e.g. 10 × 10 m grid in the study by Hansell et al. [4] vs. spatial resolution of 250 × 250 m in the HYENA study [3]) and how the noise data were linked to the population (e.g. very rough—and thus susceptible to bias—postcode-based allocation in the studies by Correia et al. [18] and Gan et al. [23]). In addition, exposure allocation based on place of residence is associated with considerable uncertainty with regard to the actual exposure, because especially during the day a large proportion of the population is not at home. These exposure-related uncertainties typically apply equally to persons with and without health effects. This so-called non-differential bias tends to result in conservative bias—i.e. an underestimation—of aircraft noise-related stroke risks.
Our meta-analysis is based on the assumption of a linear change of the risk of disease with increasing aircraft noise. This basic assumption is grounded on previous studies on cardiovascular aircraft noise risks (e.g. [e12, e13]). However, in the large NORAH study it was not possible to adequately match the association between aircraft noise and risk of stroke with a linear model (33, 35). Consequently, at this point it is not yet supported by conclusive scientific evidence that a linear model best describes the exposure-risk relationship between aircraft noise and the occurrence of stroke.
In particular, it is conceivable that there is a lower noise level threshold which has to be exceeded before the risk starts to increase. Here it should be noted that most of the individual studies de-facto introduced such a lower threshold by setting a “starting point”; however, the starting points of the various studies range between 0 and 45 dB. For comparison: 40–65 dB correspond to the usual sounds at home (e.g. a fridge: 40–43 dB) and a normal conversation (approx. 55–65 dB). Consequently, the question of a lower threshold cannot be answered by means of meta-analysis. Similarly, a starting point which is set too high in an individual study can result in biased risk estimates if risks of disease are already present at noise levels below the starting point. Thus, the different starting points of the individual studies would lead to underestimating rather than overestimating the pooled stroke risk.
Results
Study selection
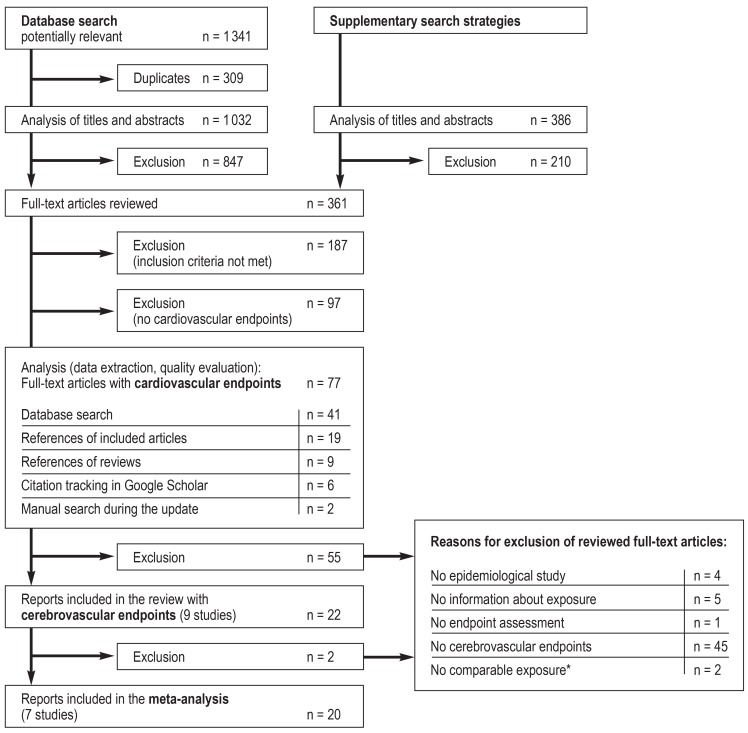
The flowchart (eFigure) shows the literature selection process. Twenty-two publications (2– 5, 18– 34, e14), containing data of altogether 9 studies, met the inclusion criteria. The extracted study data with the characteristics of the included studies/publications are listed in eTable 2.
eFigure.
Flowchart of the selection process (based on the PRISMA Statement [e7])
*The exposure information in the studies by Wiens (27) and Evrard (19) differs considerably from the exposure information of the remaining studies and thus were not included in the meta-analysis: Wiens (27) only collected data on perceived annoyance, but not aircraft noise levels;
Evrard (19) did not perform any individual, address-based estimation of the aircraft noise.
PRISMA, preferred reporting items for systematic reviews and meta-analyses
Results of the individual included studies
The results of the included individual studies are summarized in Table 2. For studies with categorical measurements of aircraft noise, the risk estimates are allocated to their corresponding intervals; for studies with continuous exposure data, reference intervals are reported in dB. The described noise metrics and effect estimates are the original data and have not yet been converted.
Table 2. Exposure parameters and endpoints of included studies.
|
First author, publication year (additional associated publications) |
Exposure metrics |
Categorical or continuous exposure reporting*1 (range) |
Effect estimates, endpoint data collection |
Confounders considered |
Value |
95% confidence interval |
| Correia et al., 2013 (18) | LDN*2 | per 10 dB (≥ 45 – 71.59 dB) |
RR, ICD-coded hospital admissions for stroke | Age, sex, ethnicity | 1.039*3 | [0.995; 1.084]*3 |
| Evrard et al., 2015 (19) | LDENAEI*2 | per 10 dB (≥ 42.0 – 46.1 dB) |
MRR, ICD-coded stroke mortality rate | Adjusted on municipal level for sex, age, population density, lung cancer mortality, and a deprivation index*4 | 1.08*4 | [0.97; 1.21]*4 |
| Frerichs et al.,1980 (20– 22) | LDay (17.5 hours)*2 | 45 – 50 dB | SMR, ICD-coded cerebrovascular deaths | Age, sex, ethnicity | 1.06*5 | [0.86; 1.29]*5 |
| 90 dB | 0.92*5 | [0.71; 1.17]*5 | ||||
| Gan et al., 2012 (23) | LDEN*2 | not exposed | RR, ICD-coded stroke mortality | Age, sex, neighborhood, socioeconomic status, and comorbidity (diabetes, COPD, hypertensive heart disease) | 1.00*3 | [1.00; 1.00]*3 |
| 0.01 – 21.3 dB | 1.30*3 | [1.11; 1.53]*3 | ||||
| 21.4 – 35.2 dB | 1.29*3 | [1.10; 1.51]*3 | ||||
| 35.3 – 44.4 dB | 1.07*3 | [0.90; 1.26]*3 | ||||
| 44.5 – 71.0 dB | 1.16*3 | [0.98; 1.36]*3 | ||||
| Hansell et al., 2013 (4) | LDay (7–23 hrs)*2 | ≤ 51 dB | RR, ICD-coded hospital admissions for stroke | Age, sex, ethnicity, deprivation (Carstairs index), lung cancer (ecological variables) | 1.00 | [1.00; 1.00] |
| >51 – 54 dB | 1.03 | [0.98; 1.09] | ||||
| >54 – 57 dB | 1.04 | [0.98; 1.12] | ||||
| >57 – 60 dB | 1.04 | [0.95; 1.14] | ||||
| >60 – 63 dB | 1.10 | [0.96; 1.25] | ||||
| >63 dB | 1.24 | [1.08; 1.43] | ||||
| LNight (23–7 hrs)*2 | ≤ 50 dB | 1.00*4 | [1.00; 1.00]*4 | |||
| >50–55 dB | 0.99*4 | [0.92; 1.07]*4 | ||||
| >55 dB | 1.29*4 | [1.14; 1.46]*4 | ||||
| Héritier et al., 2017 (2, 5) | LDEN*2 | per 10 dB (≥ 30 dB) | HR, ICD-coded stroke mortality | Sex, neighborhood index of socioeconomic status, marital status, education level, first language, nationality, and NO2 exposure | 1.013 | [0.993; 1.033] |
| Floud et al., 2013 (HYENA study: [3, 24–31, e14]) |
LAeq, 16 hours*2 | per 10 dB (<35 – 76 db) | OR, self-reporting of a physician’s stroke diagnosis | Age, sex, ethnicity, education level, body mass index; additionally assessed but not included in the final regression (≤ 10% change in exposure coefficient): alcohol consumption, exercise, smoking | 1.08 | [0.82; 1.41] |
| LNight*2 | per 10 dB (<30 – 70 db) | 1.18 | [0.89; 1.56] | |||
| Seidler et al., 2016 (NORAH study: [32, 33]) |
LDEN*2 | <40 db | ICD-10-coded hospital diagnosis of stroke | Age, sex, education level, job title (if available) and local proportion of persons receiving unemployment benefits | 1.0*3 | [1.00; 1.00]*3 |
| ≥ 40 to <45 db | 1.04*3 | [1.01; 1.08]*3 | ||||
| ≥ 45 to <50 db | 0.99*3 | [0.96; 1.03]*3 | ||||
| ≥ 50 to <55 db | 1.03*3 | [0.98; 1.08]*3 | ||||
| ≥ 55 to <60 db | 0.99*3 | [0.93; 1.06]*3 | ||||
| ≥ 60 dB | 0.86*3 | [0.76; 0.97]*3 | ||||
| Wiens. 1995 (34) | Annoyance | Little, moderately annoyed | POR, self-reporting of a physician’s stroke diagnosis | None | 0.94*4 | [0.44; 2.04]*4 |
| Rather, very annoyed | 0.66*4 | [0.66; 1.49]*4 |
*1 All aircraft noise information is based on calculated exterior noise levels which were established using noise maps. Personalized interior noise measurements were not included in any of the studies.
*2 L Aeq : A-weighted average of an energy-equivalent continuous sound level over a period of time (A-weighting: in noise research typically the A filter is used which adjusts for deep and high frequencies, as these are perceived as less loud);
L Day : L Aeq for the day (usually 7:00 am – 7:00 pm) for all day periods of a year; L Night : L Aeq for the night (usually from 11:00 pm – 7:00 am) for all night periods of a year; L DN : all 24 h L Aeq periods of a year with additional 10 dB for nighttime noise annoyance (usually from 11:00 pm – 7:00 am) ; L DEN : all 24h L Aeq periods of a year with additional 5 dB for the evening hours (8:00 pm – 10.00 pm or 7:00 pm – 11:00 pm) and additional 10 dB for nighttime hours (10:00 pm – 6:00 am or from 11:00 pm 7:00 am) ; L DEN AEI: see L DEN , but in addition weighted average exposure on municipal level
*3 Additional data from correspondence with study authors
*4 Data extraction of cerebrovascular events, but these data were not suitable for meta-analysis
*5 Self-calculated as described by Ulm, 1990 (e15)
COPD: chronic obstructive pulmonary disease; HR: hazard ratio; ICD: International Classification of Diseases and Related Health Problems; MRR: mortality rate ratio; OR: odds ratio, POR: prevalence odds ratio; RR: risk ratio, SMR: standardized mortality ratio
The included studies apply a cohort approach (2, 4, 20, 23), a case-control approach (32), a cross-sectional design (3, 18, 34) or an ecological design with case-control approach (19). The majority of the studies are secondary data analyses (2, 4, 18– 20, 23, 32). The observation periods studied vary between two (20) and eight (2) years. With the exception of the study by Wiens (34), data of women and men are evaluated in the studies. The included age groups are very heterogeneous between the individual studies. Frequently, the lower limit is set at 30 to 45 years (2, 3, 23, 32, 34), presumably because the endpoint “stroke“ would only be very sporadically observed in younger age groups.
Synthesis of the results
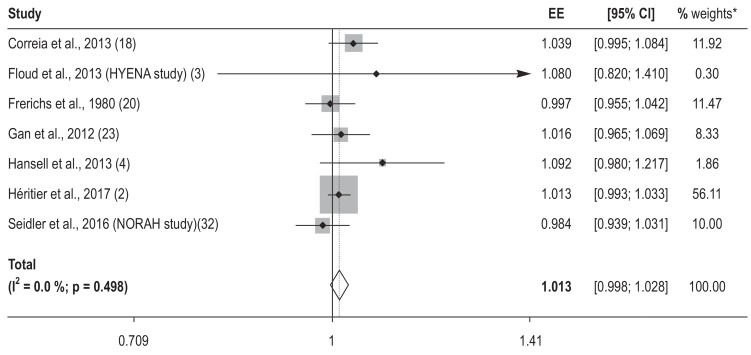
Seven of the 9 included studies (with 20 related publications) were included in the meta-analysis. The meta-analysis yielded a relative stroke risk of 1.013 (95% confidence interval [0.998; 1.028]) with each increase in the noise level LDEN by 10 dB. This corresponds to a risk increase of 1.3% with each 10 dB increase. Formally, the significance level is not reached. However, the result is so close to the significance threshold that an actual effect seems likely. The results of the core analysis are shown in the Figure. With a heterogeneity measure I2 of 0%, no formal indication of heterogeneity of the included studies was found.
Figure.
Forest plot with the included risk estimates of the individual studies per increase in aircraft noise-related LDEN by 10 dB and the pooled risk estimate (overall). With calculation of the fixed-effects model instead of the random-effects model, no change in the effect estimates and no relevant change in the width of the confidence intervals were found.
* The weights are from the random-effects analysis.
EE: effect estimate, CI: confidence interval; LDEN: noise level with all 24h LAeq periods of a year with additional 5 dB for the evening hours (8:00 pm–10:00 pm or 7:00 pm–11:00 pm) and additional 10 dB for nighttime hours (10:00 pm–6:00 am or from 11:00 pm–7:00 am)
In the leave-one-out sensitivity analysis, pooled effect estimates between 1.010 and 1.016 were found, corresponding to a risk increase of 1.0 to 1.6% with each 10 dB increase in the aircraft noise level LDEN (table 3). Only when excluding the largest study, the NORAH study on health risks (35), a statistically significant risk increase of 1.6% with each increase in LDEN by 10 dB (risk ratio [RR] = 1.016; [1.001; 1.032]) was found. This applies to studies with good quality ratings as well as for studies rated as low-quality studies in our review. Separate analysis of the cohort studies also found no substantially different effect estimate. The NORAH study on health risks reported no positive association between average 24-hour sound levels and the diagnosis of stroke; however, this study shows a statistically significant increased stroke risk of 7% when nighttime maximal levels exceed 50 dB (NAT6) and average 24-hour noise levels are below 40 dB (odds ratio [OR]: 1.07; [1.02; 1.13]).
Table 3. Results of the leave-one-out analysis.
|
Study left out (first author, year of publication) |
RR | 95% confidence interval |
| Correia et al., 2013 (18) | 1.0097 | [0.9940; 1.0258] |
| Frerichs et al.,1980 (20– 22) | 1.0152 | [0.9994; 1.0313] |
| Gan et al., 2012 (23) | 1.0130 | [0.9957; 1.0306] |
| Hansell et al., 2013 (4) | 1.0118 | [0.9968; 1.0270] |
| Héritier et al., 2017 (2, 5) | 1.0137 | [0.9901; 1.0378] |
| HYENA study (3, 24– 31, e14) | 1.0130 | [0.9975; 1.0288] |
| NORAH study on health risks (32, 33) | 1.0165 | [1.0007; 1.0324] |
RR: risk ratio
Further information about the results is provided in eBox 3.
eBOX 3. Supplementary information about the results.
• Results of the individual included studies:
The research question of our review comprised, besides the effects of measurable noise exposure, the effects of noise-related annoyance. However, this question could not be answered, because the aspect of annoyance was evaluated in one study only (36).
The majority of exposure data used in the individual studies were address-specific average noise levels (in some cases limited to certain times of the day/night or to noise levels weighted according to the time of the day). One study described the exposure in an ecological way by using the LDENAEI measure (LDENAEI: weighted average exposure to aircraft noise on the municipal level) (19). In its core analysis, the NORAH Study on health risks reported the effect estimates for maximum nighttime levels above 50 dB separately (at 24-hour continuous noise levels below 40 dB) (33). Only the study by Wiens (34) used noise-related annoyance as the exposure variable.
The spectrum of endpoint data collection ranges from self-reported information (3, 34) to ICD-coded medical or hospital diagnoses (4, 18, 32) to death-certificate diagnoses (2, 19, 20, 23).
All studies took age and sex as confounders into account. However, the analyzed studies differ with regard to the number and selection of additional confounders considered.
Three studies modeled the exposure-effect relationship continuously (2, 3, 18) using 10 dB increments, while the remaining studies reported the effect estimates based on noise intervals of variable size. The reported effect estimates include risk ratio (4, 18, 23), hazard ratio (2), odds ratio (3, 32, 34), mortality rate ratio (19), and standardized mortality rates (20).
Since almost all of the included studies were publicly funded, this source of bias is unlikely. Only one study (32) received indirect mixed funding with a small portion stemming from the aviation industry (11.4%) and otherwise mainly public funding; for a second study (20), funding information was unavailable.
• Quality of the included studies:
Four studies (2, 4, 23, 32) were of adequate quality (rating: +). The methodological quality of the remaining 5 studies (3, 18– 20, 34) was inadequate (rating: -). None of the included studies reached the highest of the 3 quality rating levels (rating: ++). Further information about the methodological strengths and weaknesses of the individual studies is provided in the data extraction table (eTable 2).
Discussion
Our systematic review with meta-analysis found a statistically nonsignificant increase in stroke risk of 1.3% with each increase of the weighted aircraft noise level LDEN by 10 dB. If the largest study (the NORAH study) is excluded, this association is statistically significant.
Strengths and limitations
Special features of this review include the a priori defined and published procedure and the comprehensive systematic search of the literature.
A literature search update for the period from September 2017 to November 2018 performed in the PubMed database yielded 35 hits. These were screened by 2 authors (VMW, AS) independently of each other. No new publications meeting the inclusion criteria were identified in the process.
It is generally possible that confounding and temporality could have biased the risk estimation. The 3 methodologically sound cohort studies included (2, 4, 23) found risk increases between 1.3% (2) and 9.2% (4) with each 10 dB increase in aircraft noise level. Thus, it seems to be rather unlikely that the risk was underestimated due to the above mentioned methodological aspects. The—in comparison to the pooled risk estimates of all studies—equal or higher risk estimates of the methodologically sound cohort studies also suggest that no relevant publication bias was present. Another important limitation is that the actual exposure of the subjects can deviate from the exposure assumed in the studies because the latter is based on the place of residence, but presumably many study participants spend much of their time elsewhere.
A large proportion of the studies is based on collections of secondary data which may harbor a higher risk of systematic bias, because these data were not collected directly from the subjects and not generated for research purposes. On the other hand, analyses of secondary data can counteract various biases: Selection mechanisms affecting the recruitment of research participants (selection bias) are usually negligible and recall bias can generally be avoided.
Comparison with the results of other studies
The meta-analysis of a Bulgarian working group (e16), investigating the association between various types of traffic noise and stroke has several issues related to the selection of the included studies. Among other things, the results of Gan et al. (23) were only analyzed collectively in the “mixed noise” category. Depending on the model used, this meta-analysis arrived at a risk estimate of 1.04 or 1.05 for each 10 dB increase in noise levels.
The meta-analysis published by Vienneau et al. (36) included 4 aircraft noise studies with stroke as the endpoint (4, 5, 18, 23). However, the aircraft-noise risk estimates were not reported separately from the risk estimates for other types of traffic noise. The Swiss working group found a pooled overall effect estimate of 1.014 ([0.96; 1.066]) with each increase in LDEN by 10 dB. This result is very close to the result of our meta-analysis.
The 2018 WHO review on the association between traffic noise and cardiovascular disease (37, 38) reported a pooled risk estimate with each increase in LDEN by 10 dB for the stroke risk due to aircraft noise for:
prevalence studies of 1.02 ([0.80; 1.28]),
incidence studies of 1.05 ([0.96; 1.15]),
mortality studies of 1.07 ([0.98; 1.17]).
However, the search period is limited to January 2000 until August 2015 and thus does not include older (for example, Frerichs et al. [20]) and, most importantly, newer analyses (for example, the NORAH study on health risks [32]).
The systematic review by Vienneau et al. (36, e12) and the WHO review (37, 38) allow a comparison between the traffic noise–related risk estimates for the “stroke” outcome with the corresponding risk estimates for the “ischemic heart disease” outcome. In both systematic reviews, the risk estimates for stroke are considerably lower compared to those for ischemic heart disease. At least to some extent, this could be explained by the fact that the diagnosis “stroke” includes both the ischemic and the hemorrhagic stroke. These two types of stroke can differ in their etiology (e17, e18). Thus, the separate analyses of the NORAH study on health risks indicated potential differences with regard to the traffic noise–related risks between hemorrhagic and ischemic stroke (e19).
Overall, our systematic review with meta-analysis provided evidence in support of an association between aircraft noise and the occurrence of stroke. Although the risk increase did not reach statistical significance when all identified studies were included in the analysis, the NORAH study on health risks—with the lowest risk estimates of all included studies—indicated that stroke risks may not be adequately described based solely on average sound levels. Accordingly, the NORAH study showed an association between the diagnosis of stroke and maximum aircraft noise levels at night. In recent years/decades, night flight restrictions, or even bans on night flights, have been introduced at many airports. A comparatively lower proportion of night flights in the NORAH study on health risks compared to several older studies may explain why the increased stroke risks observed with maximum nighttime aircraft noise levels are not apparent with the weighted average sound levels. Consequently, future studies on stroke risks associated with aircraft noise should not be limited to average sound levels, but should also take maximum nighttime levels into account.
Even if all uncertainties are taken into account, significantly less strokes are caused by aircraft noise compared to unhealthy lifestyle patterns. Based on the INTERSTROKE study by O´Donnell et al. (39), approximately 39% of strokes can be attributed to hypertension and 36% to being overweight. Even if all people were exposed to very high levels of aircraft noise (60 dB), less than 3% of all strokes could be attributed to aircraft noise, based on a 1.3% risk increase with every 10 dB increase in aircraft noise (the lifetime prevalence of stroke is 2,9% [40]).
Although the cerebrovascular accidents which could be prevented by noise-reducing measures only account for a comparatively small proportion of all strokes, the authors of this review believe that traffic noise-related health risks are important for the health of the population. Unlike the exposure to lifestyle factors, it is hardly possible for individuals to change their exposure to traffic noise. Consequently, effective noise reduction is a social responsibility.
Conclusion
All in all, our systematic review with meta-analysis indicates that there is an association between aircraft noise and the occurrence of stroke. Especially differences between the individual studies and in some cases inaccurate exposure estimations, the lack of differentiation between ischemic and hemorrhagic stroke, as well as the failure to take into account maximum levels could have resulted in a significant underestimation of the stroke risk. Given the large number of individuals exposed to environmental noise and the high prevalence of stroke in the population, more studies with improved methodology should be conducted. This would further strengthen the scientific evidence that serves as the foundation for effective noise protection—and thus effective health protection—of the population.
Key Messages.
With each increase of the noise level LDEN by 10 dB, a statistically nonsignificant increase in stroke risk by 1.3% is found.
One of the uncertainties with regard to the actual exposure of included subjects is that noise levels were measured at the place of residence, but study participants may have spent much of their time elsewhere.
There is a need for further scientific studies evaluating whether linear models can provide an optimum description of the exposure-risk relationship between aircraft noise and the occurrence of stroke.
Due to the specific characteristics of aircraft noise, future studies on the stroke risk associated with aircraft noise should also take maximum noise levels into account.
Acknowledgments
Translated from the original German by Ralf Thoene, MD.
Acknowledgement
Our special thanks go to our librarian Soja Nazarov for her continuous technical support and her unceasing efforts in searching and retrieving documents. We also wish to thank Prof. Jochen Schmitt, one of the original initiators of this review. We would furthermore like to express our heartfelt thanks to all study authors who answered to our request for additional information to their publications and so supported us: Prof. Michael Brauer (23), Dr. Andrew Correia (18), Prof. Wenqi Gan (23), Dr. Rebecca Ghosh (4), Dr. Hind Sbihi (23), Prof. Martin Röösli (2), and the team of the NORAH study on health risks (32).
Footnotes
Conflict of interest statement Prof. Seidler received reimbursement of congress fee and travel expenses for the “International Conference Active Noise Protection“ as well as study support (third party funding) from the State of Hesse (Umwelt- und Nachbarschaftshaus GmbH) and the German Federal Environment Agency. He received lecture fees from the Klinik Henningsdorf, the University of Mainz (Robert-Müller lecture) and the Lärmkontor GmbH.
The remaining authors declare no conflicts of interest.
Financial support
This review was financed by the Institute and Policlinic for Occupational and Social Medicine (IPAS), Faculty of Medicine Carl Gustav Carus, Technical University of Dresden, Germany, without additional external funding.
References
- 1.WHO. WHO Regional Office for Europe. Copenhagen: 2011. Burden of disease from environmental noise - quantification of healthy life years lost in Europe. [Google Scholar]
- 2.Héritier H, Vienneau D, Foraster M, et al. Transportation noise exposure and cardiovascular mortality: a nationwide cohort study from Switzerland. Eur J Epidemiol. 2017;32:307–315. doi: 10.1007/s10654-017-0234-2. [DOI] [PubMed] [Google Scholar]
- 3.Floud S, Blangiardo M, Clark C, et al. Exposure to aircraft and road traffic noise and associations with heart disease and stroke in six European countries: a cross-sectional study. Environ Health. 2013;12 doi: 10.1186/1476-069X-12-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hansell AL, Blangiardo M, Fortunato L, et al. Aircraft noise and cardiovascular disease near Heathrow airport in London: small area study. BMJ. 2013;347 doi: 10.1136/bmj.f5432. [DOI] [PubMed] [Google Scholar]
- 5.Huss A, Spoerri A, Egger M, et al. Aircraft noise, air pollution, and mortality from myocardial infarction. Epidemiology. 2010;21:829–836. doi: 10.1097/EDE.0b013e3181f4e634. [DOI] [PubMed] [Google Scholar]
- 6.Giles J. Science in the web age: start your engines. Nature. 2005;438:554–555. doi: 10.1038/438554a. [DOI] [PubMed] [Google Scholar]
- 7.Bakkalbasi N, Bauer K, Glover J, Wang L. Three options for citation tracking: Google Scholar, Scopus and Web of Science. Biomed Digit Libr. 2006;3 doi: 10.1186/1742-5581-3-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Seidler A, Euler U, Muller-Quernheim J, et al. Systematic review: Progression of beryllium sensitization to chronic beryllium disease. Occup Med (Lond) 2012;62:506–513. doi: 10.1093/occmed/kqs069. [DOI] [PubMed] [Google Scholar]
- 9.Seidler A, Jähnichen S, Hegewald J, et al. Systematic review and quantification of respiratory cancer risk for occupational exposure to hexavalent chromium. Int Arch Occup Environ Health. 2013;86:943–955. doi: 10.1007/s00420-012-0822-0. [DOI] [PubMed] [Google Scholar]
- 10.Seidler A, Thinschmidt M, Deckert S, et al. The role of psychosocial working conditions on burnout and its core component emotional exhaustion—a systematic review. J Occup Med Toxicol. 2014;9 doi: 10.1186/1745-6673-9-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wagner M, Bolm-Audorff U, Hegewald J, et al. Occupational polycyclic aromatic hydrocarbon exposure and risk of larynx cancer: a systematic review and meta-analysis. Occup Environ Med. 2015;72:226–233. doi: 10.1136/oemed-2014-102317. [DOI] [PubMed] [Google Scholar]
- 12.Seidler A, Steputat A, Drössler S, et al. Determinanten und Auswirkungen von Informationsüberflutung am Arbeitsplatz. Zentralblatt für Arbeitsmedizin, Arbeitsschutz und Ergonomie. 2018;68:12–26. [Google Scholar]
- 13.Thinschmidt M, Deckert S, Then F, et al. Dresden Bundesanstalt für Arbeitsschutz und Arbeitsmedizin. Dortmund, Berlin: 2014. Systematischer Review: Der Einfluss arbeitsbedingter psychosozialer Belastungsfaktoren auf die Entstehung psychischer Beeinträchtigungen und Erkrankungen; 189 pp. [Google Scholar]
- 14.Brink M. Federal Office for the Environment. Bern: 2015. Conversion of transportation noise exposure metrics Leq24h, LDay, LEvening, Ldn, and Lden to LNight WHO Environmental Noise Guidelines for the European Region; 9 pp. [Google Scholar]
- 15.Harris R, Bradburn M, Deeks J, Harbord R, Altman D, Sterne J. Metan: fixed-and random-effects meta-analysis. Stata J. 2008;8:3–28. [Google Scholar]
- 16.Orsini N, Bellocco R, Greenland S. Generalized least squares for trend estimation of summarized dose-response data. Stata J. 2006;6:40–57. [Google Scholar]
- 17.Higgins JP. Commentary: Heterogeneity in meta-analysis should be expected and appropriately quantified. Int J Epidemiol. 2008;37:1158–1160. doi: 10.1093/ije/dyn204. [DOI] [PubMed] [Google Scholar]
- 18.Correia AW, Peters JL, Levy JI, Melly S, Dominici F. Residential exposure to aircraft noise and hospital admissions for cardiovascular diseases: multi-airport retrospective study. BMJ. 2013;347 doi: 10.1136/bmj.f5561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Evrard AS, Bouaoun L, Champelovier P, Lambert J, Laumon B. Does exposure to aircraft noise increase the mortality from cardiovascular disease in the population living in the vicinity of airports? Results of an ecological study in France. Noise Health. 2015;17:328–336. doi: 10.4103/1463-1741.165058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Frerichs RR, Beeman BL, Coulson AH. Los Angeles airport noise and mortality—faulty analysis and public policy. Am J Public Health. 1980;70:357–362. doi: 10.2105/ajph.70.4.357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Meecham WC, Shaw NA. Increase in mortality rates due to aircraft noise. Schriftenreihe des Vereins fur Wasser-, Boden- und Lufthygiene. 1993;88:428–441. [PubMed] [Google Scholar]
- 22.Meecham WC, Shaw N. Effects of jet noise on mortality rates. Br J Audiol. 1979;13:77–80. doi: 10.3109/03005367909078881. [DOI] [PubMed] [Google Scholar]
- 23.Gan WQ, Davies HW, Koehoorn M, Brauer M. Association of long-term exposure to community noise and traffic-related air pollution with coronary heart disease mortality. Am J Epidemiol. 2012;175:898–906. doi: 10.1093/aje/kwr424. [DOI] [PubMed] [Google Scholar]
- 24.Floud S, Vigna-Taglianti F, Hansell A, et al. Medication use in relation to noise from aircraft and road traffic in six European countries: results of the HYENA study. Occup Environ Med. 2011;68:518–524. doi: 10.1136/oem.2010.058586. [DOI] [PubMed] [Google Scholar]
- 25.Jarup L, Babisch W, Houthuijs D, et al. Hypertension and exposure to noise near airports: the HYENA study. Environ Health Perspect. 2008;116:329–333. doi: 10.1289/ehp.10775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jarup L, Babisch W, Houthuijs D, et al. Acute and long-term effect on blood pressure of exposure to noise near airports-The HYENA study. INTER-NOISE and NOISE-CON Congress and Conference Proceedings: Institute of Noise Control Engineering. 2008:562–578. [Google Scholar]
- 27.Babisch W, Houthuijs D, Pershagen G, et al. INTER-NOISE and NOISE-CON Congress and Conference Proceedings. Istanbul, Turkey: 2007. Association between noise annoyance and high blood pressure Preliminary results from the HYENA study. [Google Scholar]
- 28.Babisch W, Swart W, Houthuijs D, et al. Exposure modifiers of the relationships of transportation noise with high blood pressure and noise annoyance. J Acoust Soc Am. 2012;132:3788–3808. doi: 10.1121/1.4764881. [DOI] [PubMed] [Google Scholar]
- 29.Babisch W, Pershagen G, Selander J, et al. Noise annoyance—a modifier of the association between noise level and cardiovascular health? Sci Total Environ. 2013;452:50–57. doi: 10.1016/j.scitotenv.2013.02.034. [DOI] [PubMed] [Google Scholar]
- 30.Dimakopoulou K, Koutentakis K, Papageorgiou I, et al. Is aircraft noise exposure associated with cardiovascular disease and hypertension? Results from a cohort study in Athens, Greece. Occup Environ Med. 2017 doi: 10.1136/oemed-2016-104180. [DOI] [PubMed] [Google Scholar]
- 31.Jarup L, Dudley ML, Babisch W, et al. Hypertension and Exposure to Noise near Airports (HYENA): study design and noise exposure assessment. Environ Health Perspect. 2005;113:1473–1478. doi: 10.1289/ehp.8037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Seidler A, Wagner M, Schubert M, Dröge P, Hegewald J. Band 6: Sekundärdatenbasierte Fallkontrollstudie mit vertiefender Befragung. Verkehrslärmwirkungen im Flughafenumfeld. Kelsterbach: Gemeinnützige Umwelthaus GmbH. 2016 [Google Scholar]
- 33.Seidler AL, Hegewald J, Schubert M, et al. The effect of aircraft, road, and railway traffic noise on stroke—results of a case-control study based on secondary data. Noise Health. 2018;20:152–161. doi: 10.4103/nah.NAH_7_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wiens D. Verkehrslärm und kardiovaskuläres Risiko Eine Fall-Kontrollstudie in Berlin (West) Institut für Wasser-, Boden- und Lufthygiene des Bundesgesundheitsamtes. 1995 [Google Scholar]
- 35.Seidler A, Wagner M, Schuber M, et al. Myocardial infarction risk due to aircraft, road and rail traffic noise—results of a case-control study based on secondary data. Dtsch Arztebl Int. 2016;113:407–414. doi: 10.3238/arztebl.2016.0407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vienneau D, Perez L, Schindler C, et al. Years of life lost and morbidity cases attributable to transportation noise and air pollution: A comparative health risk assessment for Switzerland in 2010. Int J Hyg Environ Health. 2015;218:514–521. doi: 10.1016/j.ijheh.2015.05.003. [DOI] [PubMed] [Google Scholar]
- 37.van Kempen E, Casas M, Pershagen G, Foraster M. WHO Environmental noise guidelines for the European region: a systematic review on environmental noise and cardiovascular and metabolic effects: a summary. Int J Environ Res Public Health. 2018;15 doi: 10.3390/ijerph15020379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.van Kempen E, Casas M, Pershagen G, Foraster M. Cardiovascular and metabolic effects of environmental noise: systematic evidence review in the framework of the development of the WHO environmental noise guidelines for the European region. Bilthoven, The Netherlands: National Institute for Public Health and the Environment. 2017 [Google Scholar]
- 39.O‘Donnell MJ, Chin SL, Rangarajan S, et al. Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (INTERSTROKE): a case-control study. Lancet. 2016;388:761–775. doi: 10.1016/S0140-6736(16)30506-2. [DOI] [PubMed] [Google Scholar]
- 40.Busch MA, Schienkiewitz A, Nowossadeck E, Gosswald A. [Prevalence of stroke in adults aged 40 to 79 years in Germany: results of the German Health Interview and Examination Survey for Adults (DEGS1)] Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2013;56:656–660. doi: 10.1007/s00103-012-1659-0. [DOI] [PubMed] [Google Scholar]
- E1.Umweltbundesamt. Belästigung durch Verkehrslärm. www.umweltbundesamt.de/themen/verkehr-laerm/verkehrslaerm#textpart-1 (last accessed on 18 December 2018) [Google Scholar]
- E2.Umweltbundesamt. Belastung der Bevölkerung durch Umgebungslärm. www.umweltbundesamt.de/daten/umwelt-gesundheit/belastung-der-bevoelkerung-durch-umgebungslaerm (last accessed on 18 December 2018) [Google Scholar]
- E3.Umweltbundsamt. Umweltbewusstsein in Deutschland 2016 - Ergebnisse einer repräsentativen Bevölkerungsumfrage. Berlin/Dessau-Roßlau. Umweltbundesamt. 2017 [Google Scholar]
- E4.Münzel T, Gori T, Babisch W, Basner M. Cardiovascular effects of environmental noise exposure. Eur Heart J. 2014;35:829–836. doi: 10.1093/eurheartj/ehu030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E5.Halonen JI, Vahtera J, Stansfeld S, et al. Associations between nighttime traffic noise and sleep: the Finnish public sector study. Environ Health Perspect. 2012;120:1391–1396. doi: 10.1289/ehp.1205026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E6.Badran M, Yassin BA, Fox N, Laher I, Ayas N. Epidemiology of sleep disturbances and cardiovascular consequences. Can J Cardiol. 2015;31:873–879. doi: 10.1016/j.cjca.2015.03.011. [DOI] [PubMed] [Google Scholar]
- E7.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA Statement. Ann Intern Med. 2009;151:264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- E8.Seidler A, Weihofen V, Wagner M, et al. Systematic review: environmental aircraft noise and non-auditory health complaints and diseases PROSPERO. University of York. International prospective register of systematic reviews. 2013 [Google Scholar]
- E9.Roerecke M, Rehm J. Chronic heavy drinking and ischaemic heart disease: a systematic review and meta-analysis. Open Heart. 2014;1 doi: 10.1136/openhrt-2014-000135. e000135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E10.Pearce N. Effect measures in prevalence studies. Environ Health Perspect. 2004;112:1047–1050. doi: 10.1289/ehp.6927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E11.Koo DL, Nam H, Thomas RJ, Yun CH. Sleep disturbances as a risk factor for stroke. J Stroke. 2018;20:12–32. doi: 10.5853/jos.2017.02887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E12.Vienneau D, Schindler C, Perez L, Probst-Hensch N, Roosli M. The relationship between transportation noise exposure and ischemic heart disease: a meta-analysis. Environ Res. 2015;138:372–380. doi: 10.1016/j.envres.2015.02.023. [DOI] [PubMed] [Google Scholar]
- E13.Seidler A, Wagner M, Schubert M, et al. Aircraft, road and railway traffic noise as risk factors for heart failure and hypertensive heart disease-a case-control study based on secondary data. Int J Hyg Environ Health. 2016;219:749–758. doi: 10.1016/j.ijheh.2016.09.012. [DOI] [PubMed] [Google Scholar]
- E14.Babisch W, Houthuijis D, Kwekkeboom J, et al. HYENA-Hypertension and exposure to noise near airports A European study on health effects of aircraft noise. INTER-NOISE and NOISE-CON Congress and Conference Proceedings. Institute of Noise Control Engineering. 2005:1376–1385. [Google Scholar]
- E15.Ulm K. A simple method to calculate the confidence interval of a standardized mortality ratio (SMR) Am J Epidemiol. 1990;131:373–375. doi: 10.1093/oxfordjournals.aje.a115507. [DOI] [PubMed] [Google Scholar]
- E16.Dzhambov AM, Dimitrova DD. Exposure-response relationship between traffic noise and the risk of stroke: a systematic review with meta-analysis. Arh Hig Rada Toksikol. 2016;67:136–151. doi: 10.1515/aiht-2016-67-2751. [DOI] [PubMed] [Google Scholar]
- E17.O‘Donnell MJ, Xavier D, Liu L, et al. Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): a case-control study. Lancet. 2010;376:112–123. doi: 10.1016/S0140-6736(10)60834-3. [DOI] [PubMed] [Google Scholar]
- E18.Blomstrand A, Blomstrand C, Ariai N, Bengtsson C, Bjorkelund C. Stroke incidence and association with risk factors in women: a 32-year follow-up of the Prospective Population Study of Women in Gothenburg. BMJ Open. 2014;4 doi: 10.1136/bmjopen-2014-005173. e005173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E19.Seidler A, Steputat A, Drössler S, et al. Determinanten und Auswirkungen von Informationsüberflutung am Arbeitsplatz. Zentralblatt für Arbeitsmedizin, Arbeitsschutz und Ergonomie. 2018;68:12–26. [Google Scholar]