Abstract
Objective
This study examined self-reported age of tobacco initiation (cigarette smoking and smokeless tobacco [ST] use) and explored potential sex and generational group influences on tobacco use onset among Alaska Native (AN) adult ever tobacco users.
Methods
Secondary analysis of consolidated data from the Western Alaska Tribal Collaborative for Health (WATCH) study comprised 2800 AN adult ever tobacco users (1490 women, 1310 men; mean age = 39.2 years) from two rural western Alaska regions. ST use data were limited to one region. Logistic regression was used to examine potential sex and generational group (age 18–29, 30–49, ≥50) effects on initiation at ≤13 years of age.
Results
Thirty-seven percent of the sample reported using any tobacco product by age 13 years. Initiation of any ST use by age 13 was greater than for cigarette smoking (52.7% vs. 18.2%), and women were more likely than men to report initiation of any ST use at ≤13 years (52.6% vs. 38.4%). Nearly one-third of ever smokers (31%) initiated in young adulthood (ages 18–29). For ST use, logistic regression analyses revealed significant sex differences (women more likely to initiate by 13 years of age than men) and generational group effects with younger and middle age groups more likely to report initiation ≤13 years compared to the eldest participants. For smoking, no sex differences were observed but the youngest generational group was more likely to report initiation by age 13 compared to the eldest group.
Conclusions
Earlier age of tobacco initiation is found among younger generations of AN people. Findings highlight the need to focus prevention efforts on initiation of smoking in young adulthood and uptake of ST use among girls.
Keywords: Alaska Native, Adolescents, Tobacco, Smoking, Initiation
Highlights
-
•
Younger Alaska Native (AN) adults reported earlier tobacco initiation than older adults.
-
•
Women reported earlier age of smokeless tobacco (ST) initiation than men.
-
•
Almost one third of ever smokers (29%) had initiated in young adulthood (age 18–29).
-
•
Prevention efforts are needed for ST use in AN girls and smoking in young adults.
1. Introduction
A recent representative survey of 13,651 United States (U.S.) adolescents aged 12–17 years indicated that, overall, 13% had ever smoked cigarettes (Kasza et al., 2017). At 21% ever smoked, American Indian and Alaska Native (AI/AN) youth had the highest prevalence of ever smoking compared to all other racial/ethnic groups in this survey. Among Alaskan high school students in 2015, 20% of AN students currently smoked cigarettes compared to 7% among non-Native students (Alaska Department of Health and Social Services [DHSS], 2016). Current use of smokeless tobacco (ST) is also greater among AN students compared to non-Native Alaskan students (25% vs. 6%; DHSS, 2016).
1.1. Public health importance of age of tobacco use onset
Understanding patterns of tobacco use onset is important from a public health perspective (Chassin, Presson, & Macy, 2014; Pierce, White, & Emery, 2012) because tobacco initiation at an earlier age is a risk factor for greater severity of nicotine dependence and difficulty quitting, as well as adverse health consequences (Benowitz, 2010; DiFranza et al., 2000; Hegmann et al., 1993; Lando et al., 1999; Substance Abuse and Mental Health Services Administration [SAMHSA], 2016; Sargent, Gabrielli, Budney, Soneji, & Wills, 2017; Soneji, Sargent, & Tanski, 2016; U.S. Department of Health and Human Services [USDHSS], 2012). Despite extensive work examining patterns of tobacco use onset among adolescents and young adults (Freedman, Nelson, & Feldman, 2012; Johnston, O'Malley, Bachman, & Schulenber, 2013), very little tobacco prevention research has focused on AI/AN people, and most national surveys do not capture tobacco use initiation before 12 years of age (USDHHS, 2012).
1.2. Tobacco use among Alaska Native youth
Some studies suggest that AN people initiate tobacco use, especially ST, at an earlier age compared to the general population (Angstman et al., 2007; Renner et al., 2013; Smith, Ferucci, Dillard, & Lanier, 2010). Based on the 2015 Alaska Youth Risk Behavior Survey, the percentage of Alaskan high school students initiating cigarette smoking before 13 years of age was higher for AN youth than non-Native students (15% vs. 6%; DHSS, 2016). In comparison, 9% of high school students nationally reported trying smoking before 13 years of age (Kann et al., 2014).
In some Alaska regions, ST use, including iqmik, a homemade form of ST, is embedded in cultural practices and considered a healthy alternative to smoking (Hurt et al., 2005; Patten et al., 2009; Renner et al., 2004; Renner et al., 2005; Wolsko, Mohatt, Lardon, & Burket, 2009). While commercial ST and iqmik both contain tobacco, iqmik contains ground ash produced by burning Phellinus igniarius or “punk,” a tree fungus (Renner et al., 2005). Nicotine absorption is greatly enhanced by the punk ash, which increases the pH, thereby increasing the bioavailability of un-ionized nicotine in the product (Renner et al., 2005). Although previous studies document there is no ceremonial use for tobacco in any form among AN people, iqmik is considered a “natural” product. Therefore, many consider its use as healthier than cigarette smoking (Blanchette, Renner, Held, Enoch, & Angstman, 2002; Renner et al., 2004). Angstman et al. (2007) conducted a medical record study in a rural region of Alaska and reported that the proportion of youth who had ever tried iqmik or other ST products was 23% among 6–10 year olds, 42% of 11–14 year olds, and 68% among 15–18 year olds. Similarly, Smith et al. (2010) found that among AN adults who had ever used ST, 22% reported initiation by age 10.
1.3. Study purpose and goals
Greater understanding of when tobacco use initiation is occurring is essential for developing targeted tobacco use prevention programs for AN people. Therefore, the focus of the current study was to describe reported age of tobacco initiation (cigarette smoking and ST use) and to explore potential sex and generational group influences on tobacco use onset among AN adult ever tobacco users. We explored the influence of generational group because it is important for prevention efforts to understand if earlier age of tobacco initiation is occurring in younger generations. Participants resided in two rural western Alaska regions where tobacco use prevalence exceeds that in both Alaska and the U.S. population (Dilley, Peterson, Hiratsuka, & Rohde, 2013).
2. Methods
2.1. Procedures
The study conducted a secondary analysis of consolidated data from the Western Alaska Tribal Collaborative for Health (WATCH) study described by Koller et al. (2013). The data set is comprised of three population-based studies initiated in two adjacent western Alaska regions during 2000–2004: the Genetics of Coronary Artery Disease in Alaska Natives (GOCADAN) study (Howard et al., 2005) based in the Norton Sound region, and the Centers for Alaska Native Health Research (CANHR) (Mohatt et al., 2007) and Education and Research Towards Health (EARTH) (Slattery et al., 2007) studies based in the Yukon-Kuskokwim Delta (Y-K) region. All self-reported tobacco use data were either combined directly or harmonized and redefined to incorporate slight differences in collection methods, questions, and/or response options, as described in Koller et al. (2017). The consolidated data set provides a unique opportunity to study age of tobacco initiation among AN people living in these two rural western Alaska regions.
Approval for this study was granted by the Alaska Area, MedStar Health Research Institute, and the University of Alaska Fairbanks institutional review boards. Tribal approvals were received from the Alaska Native Tribal Health Consortium, Norton Sound Health Corporation, and Yukon-Kuskokwim Health Corporation.
2.2. Sample
The WATCH study consolidated data collected from 3932 participants. WATCH participants who had ever used a tobacco product, either smoking cigarettes and/or use of ST (N = 2800), form the basis of this report.
2.3. Measures
Demographic data obtained by all studies included age, sex, and region of residence. For a sub-set of participants (n = 1189) only, education level in years of school completed was collected. All participants were asked about tobacco use. Those who reported ever having used tobacco were asked to specify tobacco types used, specifically cigarettes and ST (chew or snuff), and age at product initiation (age at which they began using each). Using a standard definition, respondents were asked if they had ever smoked ≥100 cigarettes in their lifetime; those indicating “yes” were considered established smokers and defined as ever smokers (Choi, Gilpin, Farkas, & Pierce, 2001; Pierce, Choi, Gilpin, Farkas, & Merritt, 1996). Because each of the studies specified cigarette smoking (as opposed to cigar, pipe, or other tobacco types) and the exact amount (≥100 cigarettes in a lifetime), we were able to directly combine these study data without altering the definition and preserving data precision. Consistent with other surveys (e.g., Odani, Armour, & Agaku, 2018), we defined ever use of ST as self-reported use of any commercial or homemade ST products. ST data were harmonized to include both commercial and homemade ST products, which varied by communities and regions. In general, while data that are directly combined retain their precision, variables requiring expanded definitions of harmonization become less precise. However, from these data we were able to determine exclusive ever smoking, exclusive ever ST use, and ever use of both tobacco types. Dual ever use was defined as both ever smoker and ever ST user.
For ever use of ST products, the CANHR and EARTH studies (conducted in the Y-K region), asked participants to specify whether ST products were commercially prepared or homemade (i.e., iqmik). Due to inherent differences in composition and regional cultural norms and practices, we analyzed predictors of age of initiation for iqmik and commercial ST separately.
2.4. Data analyses
We used SAS version 9.4 (Cary, North Carolina) to calculate means with standard deviations for continuous variables and frequencies with percentages for categorical data. Similar to other studies (Breslau & Peterson, 1996; Khuder, Dayal, & Mutgi, 1999), we dichotomized age of initiation as less than or equal to 13 years versus >13 years at initiation.
Among ever users of each respective tobacco product, we examined the percentage of the sample initiating tobacco at age ≤13 years stratified by sex, region, and generational group: age 18–29, 30–49, >50 years. Generational groups were based on the age distribution of our sample. We used logistic regression to predict age of smoking initiation using ≤13 years versus >13 years at initiation as the dependent variable and sex, generational group, region and ever use of ST as the independent variables. For ST use (Y-K region only), we used logistic regression to predict age of ST initiation (overall and separately for commercial ST and iqmik use) using ≤13 years versus >13 years at initiation as the dependent variable and sex, generational group, and ever cigarette smoking as the independent variables. Education level was not included as an independent variable because education was only available for a small subset of the sample. Inclusion of education would have resulted in substantially reducing the sample size for analyses, and the close association of education with individuals' locality (i.e., region) could confound the results. Significance was determined at p < 0.05.
3. Results
3.1. Participants
Participants were 2800 (n = 1490 women, n = 1310 men) AN adults who had ever used tobacco residing in the Norton Sound (n = 1036) and Y-K (n = 1764) region. Their mean age was 39.2 years (SD 15.5, range 18–95). By age groups, 936 (33.4%) participants were aged 18–29 years, 1163 (41.5%) were between 30 and 49 years of age, and 701 (25.0%) were aged 50 years or older. Mean years of education (n = 1819) was 10.7 (SD 2.7, range 0–19). Although no significant regional differences were detected on participant sex, participants in Norton Sound differed significantly from those in the Y-K region on age (41.2 vs. 38.0 years; p < 0.001) and years of education (11.7 vs. 9.6; p < 0.001).
Overall, 2157 participants (1033 women, 1124 men) had ever smoked cigarettes, 1371 (785 women, 586 men) had ever used ST, and 955 (424 women, 531 men) were dual ever users.
3.2. Age of initiation of tobacco products
Table 1 displays percentage aged 13 or younger when initating tobacco use by sex, region, and generational group. Overall, 36.7% had initiated any tobacco use by age 13. The proportion initiating tobacco product use by age 13 was higher for women than men for any ST use and any tobacco product use, but lower for cigarette smoking. There is a consistent pattern for generational group with greater proportion of tobacco product initiation ≤age 13 for younger than older age groups. Regional differences are seen for cigarette smoking and any tobacco product use with higher proportion of initiation ≤13 years of age among Y-K adults compared with Norton Sound participants. For example, 48.0% of the Y-K sample used any tobacco product by age 13 years compared with 17.5% in Norton Sound participants. Additional data provided in Supplemental Table S1, Supplemental Table S2, Supplemental Table S3 show the percentage at age of initiation from <5 years to >45 years of age, for any tobacco product, cigarette smoking and ST use respectively.
Table 1.
Percentage 13 years or younger at self-reported age of initiation of tobacco product use by sex, region, and generational group among western Alaska Native adult ever tobacco users: the WATCH study (N = 2800).
| Type of tobacco product ever usedc |
|||||
|---|---|---|---|---|---|
| Any tobaccoa |
Cigarette smokinga |
Any smokelessb |
Commercial chewb |
Iqmikb |
|
| N = 2800 |
N = 2157 |
N = 1371 |
N = 863 |
N = 1110 |
|
| n (%) | n (%) | n (%) | n (%) | n (%) | |
| Overall | |||||
| Total | 1027 (36.7) | 393 (18.2) | 722 (52.7) | 415 (48.1) | 486 (43.8) |
| Women | 599 (40.2) | 185 (17.9) | 464 (59.1) | 263 (54.8) | 309 (47.0) |
| Men | 428 (32.7) | 208 (18.5) | 258 (44.0) | 152 (39.7) | 177 (39.1) |
| Region | |||||
| Norton Sound | 181 (17.5) | 181 (17.5) | – | – | – |
| Y-K Delta | 846 (48.0) | 212 (18.9) | 722 (52.7) | 415 (48.1) | 486 (43.8) |
| Generational age group % ≤13 years | |||||
| 18–29 | 439 (46.9) | 175 (22.7) | 313 (65.2) | 162 (57.5) | 230 (56.7) |
| 30–49 | 429 (36.9) | 138 (16.4) | 321 (54.5) | 216 (52.2) | 184 (41.0) |
| 50+ | 159 (22.7) | 80 (14.7) | 88 (29.1) | 37 (22.2) | 72 (28.2) |
| Women | 599 (40.2) | 185 (17.9) | 464 (59.1) | 263 (54.8) | 309 (47.0) |
| Age 18–29 | 243 (51.3) | 84 (23.4) | 191 (72.4) | 97 (65.1) | 134 (59.0) |
| Age 30–49 | 259 (40.2) | 69 (16.5) | 204 (59.7) | 137 (57.6) | 119 (43.9) |
| Age 50+ | 97 (26.1) | 32 (12.5) | 69 (38.6) | 29 (31.2) | 56 (35.2) |
| Norton Sound | 94 (16.9) | 94 (16.9) | – | – | – |
| Age 18–29 | 36 (23.7) | 36 (23.7) | – | – | – |
| Age 30–49 | 48 (18.5) | 48 (18.5) | – | – | – |
| Age 50+ | 10 (6.9) | 10 (6.9) | – | – | – |
| Y-K Delta | 505 (54.2) | 91 (19.2) | 464 (59.1) | 263 (54.8) | 309 (47.0) |
| Age 18–29 | 207 (64.3) | 48 (23.2) | 191 (72.4) | 97 (65.1) | 134 (59.0) |
| Age 30–49 | 211 (55.0) | 21 (13.3) | 204 (59.7) | 137 (57.6) | 119 (43.9) |
| Age 50+ | 87 (38.5) | 22 (20.0) | 69 (38.6) | 29 (31.2) | 56 (35.2) |
| Men | 428 (32.7) | 208 (18.5) | 258 (44.0) | 152 (39.7) | 177 (39.1) |
| Age 18–29 | 196 (42.4) | 91 (22.1) | 122 (56.5) | 65 (48.9) | 96 (53.6) |
| Age 30–49 | 170 (32.8) | 69 (16.2) | 117 (47.4) | 79 (44.9) | 65 (36.5) |
| Age 50+ | 62 (18.8) | 48 (16.7) | 19 (15.5) | 8 (10.8) | 16 (16.7) |
| Norton Sound | 87 (18.2) | 87 (18.2) | – | – | – |
| Age 18–29 | 30 (22.2) | 30 (22.2) | – | – | – |
| Age 30–49 | 33 (17.0) | 33 (17.0) | – | – | – |
| Age 50+ | 24 (16.1) | 24 (16.1) | – | – | – |
| Y-K Delta | 341 (41.0) | 121 (18.7) | 258 (44.0) | 152 (39.7) | 177 (39.1) |
| Age 18–29 | 166 (50.8) | 61 (22.1) | 122 (56.5) | 65 (48.9) | 96 (53.6) |
| Age 30–49 | 137 (42.2) | 36 (15.6) | 117 (47.4) | 79 (44.9) | 65 (36.5) |
| Age 50+ | 38 (21.1) | 24 (17.3) | 19 (15.5) | 8 (10.8) | 16 (16.7) |
Norton Sound (GOCADAN) and Y-K Delta (CANHR + EARTH) Study Cohorts.
Y-K Delta (CANHR + EARTH) only.
Table values are n (%) reported among ever users of each respective tobacco product (ever use includes former and current users).
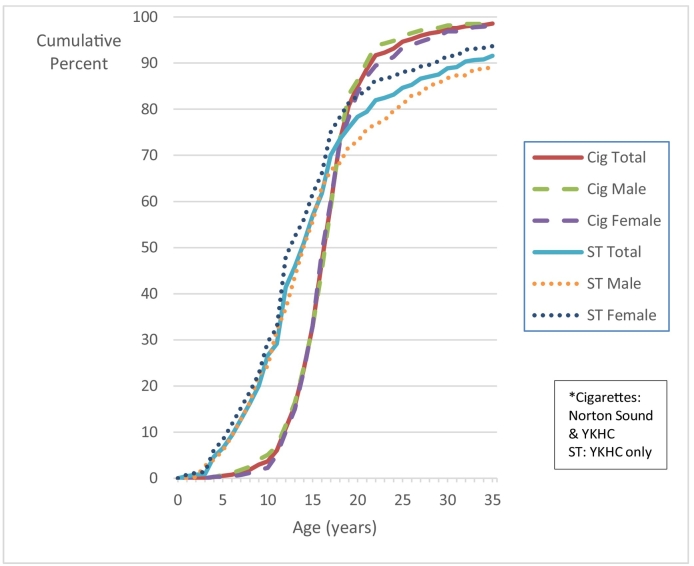
Fig. 1 illustrates the cumulative percentage of initiation of cigarette smoking and use of ST. For both men and women, a greater percentage of ST users initiated early compared to cigarette smokers. For example, only 4% of the sample initiated smoking before age 11 (2% women, 5% men) compared with 28% for ST use (31% women, 24% men). Moreover, 12% smoked before age 13 years (11% women, 13% men) compared to 46% who started using ST (53% women, 38% men) by that age. Sixty-six percent had initiated smoking before 18 years of age (68% women, 65% men); in contrast, 78% had used ST before age 18 years (82% women, 73% men). Thirty-one percent of ever smokers initiated between 18 and 29 years of age in contrast to 14% of those initiating ST use (additional data provided in Supplemental Table S2, Supplemental Table S3).
Fig. 1.
Cumulative percentage of age of initiation of smoking among ever cigarette smokers and of ST use among ever ST users*.
3.3. Predictors of age of tobacco use initiation
3.3.1. Cigarette smoking
Table 2 presents results from the multivariate analysis predicting age of initiation for cigarette smoking at ≤13 years (model 1). No significant sex or regional differences were observed. We observed significant differences between the youngest generation reporting greater likelihood of initiation of smoking by 13 years of age compared to the eldest generation. Adding ever use of ST to the regression model for cigarette smoking initiation did not substantially reduce the observed generational age group effect (model 2).
Table 2.
Logistic regression of sex and generational groups with age of tobacco initiation among western Alaska Native ever tobacco users: WATCH study.a, b
| Cigarette initiation ≤13 years: Y-K and Norton Sound | |||
|---|---|---|---|
| Predictor | OR | 95% CI | P |
| Model 1 (n = 2155) | |||
| Sex (referent = male) | 1.0 | 0.78–1.21 | 0.782 |
| Generational group 18–29 years (ref = 50+ years) | 1.7 | 1.27–2.28 | 0.0004 |
| Generational group 30–49 years (ref = 50+ years) | 1.1 | 0.84–1.54 | 0.399 |
| Region (referent = YK) | 1.0 | 0.78–1.22 | 0.837 |
| Model 2 (n = 2155) | |||
| Sex (referent = male) | 1.0 | 0.78–1.21 | 0.789 |
| Generational group 18–29 years (ref = 50+ years) | 1.7 | 1.29–2.32 | 0.0003 |
| Generational group 30–49 years (ref = 50+ years) | 1.2 | 0.86–1.57 | 0.322 |
| Region (referent = YK) | 0.8 | 0.61–1.06 | 0.118 |
| Smokeless tobacco use (ref = Ever) | 1.4 | 1.05–1.86 | 0.022 |
| Smokeless tobacco initiation ≤13 years: Y-K only | |||
|---|---|---|---|
| Predictor | OR | 95% CI | P |
| Model 3 (n = 1363) | |||
| Sex (referent = male) | 2.0 | 1.59–2.51 | <0.001 |
| Generational group 18–29 years (ref = 50+ years) | 5.0 | 3.61–6.84 | <0.001 |
| Generational group 30–49 years (ref = 50+ years) | 3.0 | 2.25–4.12 | <0.001 |
| Model 4 (n = 1363) | |||
| Sex (referent = male) | 2.1 | 1.64–2.63 | <0.001 |
| Generational group 18–29 years (ref = 50+ years) | 4.8 | 3.50–6.67 | <0.001 |
| Generational group 30–49 years (ref = 50+ years) | 3.0 | 2.25–4.11 | <0.001 |
| Smoker (ref = Ever) | 0.9 | 0.68–1.12 | 0.276 |
| Commercial chew initiation ≤13 years: Y-K only | |||
|---|---|---|---|
| Predictor | OR | 95% CI | P |
| Model 5 (n = 863) | |||
| Sex (referent = male) | 1.9 | 1.47–2.59 | <0.001 |
| Generational group 18–29 years (ref = 50+ years) | 5.0 | 3.23–7.81 | <0.001 |
| Generational group 30–49 years (ref = 50+ years) | 3.9 | 2.58–5.94 | <0.001 |
| Model 6 (n = 863) | |||
| Sex (referent = male) | 2.0 | 1.50–2.73 | <0.001 |
| Generational group 18–29 years (ref = 50+ years) | 4.8 | 3.07–7.58 | <0.001 |
| Generational group 30–49 years (ref = 50+ years) | 3.9 | 2.56–5.89 | <0.001 |
| Smoker (ref = Ever) | 0.9 | 0.64–1.20 | 0.414 |
| Iqmik initiation ≤13 years: Y-K only | |||
|---|---|---|---|
| Predictor | OR | 95% CI | P |
| Model 7 (n = 1102) | |||
| Sex (referent = male) | 1.5 | 1.15–1.90 | 0.003 |
| Generational group 18–29 years (ref = 50+ years) | 3.5 | 2.49–4.91 | <0.001 |
| Generational group 30–49 years (ref = 50+ years) | 1.8 | 1.29–2.51 | 0.001 |
| Model 8 (n = 1102) | |||
| Sex (referent = male) | 1.5 | 1.15–1.96 | 0.003 |
| Generational group 18–29 years (ref = 50+ years) | 3.5 | 2.46–4.89 | <0.001 |
| Generational group 30–49 years (ref = 50+ years) | 1.8 | 1.29–2.51 | 0.001 |
| Smoker (ref = Ever) | 1.0 | 0.73–1.26 | 0.762 |
Logistic regression analysis with age of initiation (dependent variable) for each model based on median split.
Sample for each analysis includes ever users of each respective tobacco product, i.e. for smoking this includes ever cigarette smokers.
3.3.2. Smokeless tobacco use
For Y-K participants only, results are reported for ST use overall and separately for commercial ST and iqmik use (Table 2, models 3–8). Results were consistent across all models with significant sex and generational group differences observed. Women were more likely to initiate ST products by 13 years of age than men. Moreover, both younger (18–29) and middle age (30–49) generational groups were more likely to initiate ST products by age 13 compared to the eldest generation. Adding ever cigarette smoking to the regression models (models 4, 6, and 8) did not reduce observed effects for sex and generational group on ST product initiation.
4. Discussion
From a public health perspective, it is important to investigate patterns of tobacco use initiation for effective message tailoring to the targeted audience (DiFranza et al., 2000; Pierce et al., 2012). Our study contributes to the literature on tobacco use onset among AN people, a disparity group (Blake, Holck, & Provost, 2016; Borrelli, 2010). We found a substantial percentage (31%) of ever cigarette smokers initiated smoking between the ages of 18–29 years. This percentage is slightly higher than observed in a nationally representative sample of adults aged 30–39 who have ever smoked, with 22% reporting initiation between 18 and 29 years of age. It is noteworthy that recent national studies indicate cigarette smoking onset has become more concentrated in the young adult years across sex and racial/ethnic groups (Thompson, Mowery, Tebes, & McKee, 2017). In a large representative sample, smoking onset occurred among 6.3% of young adults aged 18–25 years compared with 1.9% of youth 12–17 years of age; women and racial/ethnic minorities were more likely than men and white participants to initiate smoking in young adulthood (Thompson et al., 2017). Thus, preventing smoking initiation among AN young adults represents an untapped opportunity for tobacco control efforts.
A key finding of our study was the reported onset of ST use at markedly young ages with 28% initiating by age 10 and 46% initiating by 13 years of age. Moreover, 53% of women initiated ST use by age 13 compared to 38% among men. A novel finding is that generational influences for both cigarette smoking and ST use were observed. For cigarette smoking, the youngest (18–29) generational group was almost twice as likely as the eldest group to report initiation by age 13 years. For ST use, risk of initiation by age 13 was greatest in the youngest generational group compared to the eldest, but the middle age group 30–49 also had a higher likelihood of initiation ≤13 years compared to the eldest group. These generational influences are relevant to developing targeted prevention and public health campaign messaging.
Preventing tobacco use or delaying age of when AN children, adolescents, and/or young adults begin using tobacco can reduce the severity of nicotine dependence and tobacco-caused health disparities, as well as enhance the likelihood of successful quitting among those who do become regular smokers (Chassin et al., 2014; DiFranza et al., 2000; Hegmann et al., 1993; Lando et al., 1999; SAMHSA, 2016; Sargent et al., 2017; Soneji et al., 2016; USDHHS, 2012). Broad-based policies and other strategies that focus on prevention of tobacco use may contribute to a reduction in disparities in children's health along with future disparities including high mortality and incidence rates of lung cancer experienced among AN people (Carmack, Schade, Sallison, Provost, & Kelly, 2015; Pierce et al., 2012). The acquired knowledge regarding tobacco use onset from this study can inform policies and be used to identify more effective prevention resources, particularly for girls initiating ST use. Significant youth-focused tobacco control activity (e.g., the youth-targeted anti-smoking truth campaign and the real cost media campaign) introduced in recent decades has contributed to a decline in adolescent smoking onset (Farrelly et al., 2017; Farrelly, Nonnemaker, Davis, & Hussin, 2009; Pierce et al., 2012). Comprehensive programs that focus on modifying pro-tobacco social norms are also effective (Pierce et al., 2012). However, the impact of these types of programs for preventing onset of cigarette and ST use among AN people have not yet been evaluated (Boles et al., 2009). Possible avenues of intervention include targeting pregnant women and women of childbearing age to prevent in utero tobacco exposure (Espy, Fang, Johnson, Stopp, & Wiebe, 2011; Liska, 2014) and prevention efforts aimed at preschool-aged children, such as through Head Start programs. Moreover, regional differences observed in this study suggest development of population-based information pertinent to prevention efforts that are directly applicable and culturally relevant are needed.
4.1. Study strengths
Strengths of our study include the large, population-based sample size of AN persons. The WATCH data set is comprised of several population-based cohort studies all conducted within the same time period. All studies recognized the need for detailed data on tobacco use and initiation. The collection of similar detailed data provided the opportunity to combine or harmonize the data such that an analysis of initiation patterns was possible. Each study was conducted by research teams with longstanding relationships with the respective communities, which contributed to increased response rates and reliability. The extensive data collection on age of initiation, capturing uptake as young as five years old, provided important new information on cigarette smoking initiation along with separate assessment of commercial ST and iqmik initiation that health providers and Tribal leaders can use to inform personal health care decisions and local public policy.
4.2. Study limitations
Certain limitations should be considered when interpreting the findings. One potential weakness is recall bias accounting for generational group findings. As with other surveys (SAMHSA, 2013) ever tobacco users were asked as adults to report on age of initiation. T. P. Johnson and Mott (2001) found that adults provided more accurate reports of smoking onset than adolescents (mean age = 14 years), with an intra-class correlation of 0.85, although reliability estimates decreased with increasing recall intervals. Another report found that “forward telescoping,” defined as temporal displacement of an event whereby people perceive distant events as being more recent than they are, was associated with age, such that older participants reported a later age of smoking initiation than did younger respondents (E. O. Johnson & Schultz, 2005). Our study was limited to assessment of cigarettes, commercial ST, and iqmik. Non-cigarette tobacco products are evolving rapidly, with increasing popularity in the U.S. (Kasza et al., 2017; Odani et al., 2018). However, minimal use of pipe or cigar smoking has been reported in these regions (Renner et al., 2004), and data collection occurred prior to the outspread use of e-cigarettes. Furthermore, investigation of ST use patterns was restricted to the Y-K region, as ST use is not highly prevalent in the Norton Sound region. Collection of data on education level was limited to a substantially smaller subset of participants that closely mirrored region of residence and, therefore, was not included in the logistical analysis. Moreover, although we focused on preventing early initiation of tobacco use, our study did not capture other risk behaviors that are associated with early onset of tobacco use including alcohol use and illicit substances and sexual behavior (Kann et al., 2018). Future studies should account for other psychosocial risk indicators among adolescents.
4.3. Conclusions
Earlier age of tobacco initiation is found among younger generations of AN people. Findings highlight the need to focus prevention efforts on initiation of smoking in young adulthood and uptake of ST use among girls living in the Y-K region.
The following are the supplementary data related to this article.
Percent age of initiation of any tobacco product among western Alaska Native adult ever tobacco users: the WATCH study.⁎
Percent age of cigarette smoking initiation among western Alaska Native adult ever smokers: the WATCH study.⁎
Percent age of smokeless tobacco initiation among Y-K Delta Alaska Native adult ever smokeless tobacco users: the WATCH study.
Role of funding sources
The WATCH study was funded in part by an American Recovery and Reinvestment Act Administrative Supplement to a grant funded by the National Center for Research Resources (NCRR), National Institutes of Health (NIH; grant P20 RR16430). The Center for Alaska Native Health Research (CANHR) was funded through the NCRR COBRE (P20 RR016430 and R01 DK074842) mechanisms. Alaska Education and Research Toward Health (EARTH) was funded by the National Cancer Institute (CA88958 and CA96095). Genetics of Coronary Artery Disease in Alaska Natives (GOCADAN) was funded by the National Heart, Lung, and Blood Institute (U01 HL64244). Additional Federal funding was received from the NCRR and the National Center for Advancing Translational Sciences, NIH, through the Clinical and Translational Science Awards Program, a trademark of the U.S. Department of Health and Human Services, part of the Roadmap Initiative, “Re-Engineering the Clinical Research Enterprise” (Grant # UL1RR031975); the National Institute of Diabetes and Digestive and Kidney Diseases (DK097307); and the Centers of Biomedical Research Excellence (P30GM103325). Funds were also made available by the President of the University of Alaska through unrestricted donations by British Petroleum and ConocoPhillips.
These funding sources had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
Contributors
Authors KRK, GED, JGU, MAA, SEH, and BB designed the parent WATCH study from which data from this report were collected and analyzed. All authors designed and contributed to the writing of the protocol of methods and analyses to examine smoking initiation from data collected in the WATCH study. Authors CAP and CAF conducted literature searches and provided summaries of previous research studies. Authors CAP and KRK wrote the methods section to which all authors then contributed. Author GED conducted the statistical analyses. Author CAP wrote the first draft of the manuscript and all authors contributed to and have approved the final manuscript.
Conflict of interest
All authors declare that they have no conflicts of interest.
Acknowledgements
The authors thank the Alaska Native people who participated in all of the WATCH cohort studies.
References
- Alaska Department of Health and Social Services (DHSS) Alaska tobacco facts 2016. 2016. http://dhss.alaska.gov/dph/Chronic/Documents/Tobacco/PDF/2016_AKTobaccoFacts.pdf Retrieved from:
- Angstman S., Patten C.A., Renner C.C., Simon A., Thomas J.L., Hurt R.D.…Offord K.P. Tobacco and other substance use among Alaska Native youth in western Alaska. American Journal of Health Behavior. 2007;31(3):249–260. doi: 10.5555/ajhb.2007.31.3.249. [DOI] [PubMed] [Google Scholar]
- Benowitz N.L. Nicotine addiction. New England Journal of Medicine. 2010;362(24):2295–2303. doi: 10.1056/NEJMra0809890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blake I., Holck P., Provost E. Alaska Native Epidemiology Center; Anchorage (US): 2016. Alaska Native mortality update: 2009–2013. [Google Scholar]
- Blanchette R., Renner C.C., Held B., Enoch C., Angstman S. The current use of Phellinus igniarius by the Eskimos of Western Alaska. Mycologist. 2002;16(4):142–145. [Google Scholar]
- Boles M., Rohde K., He H., Maher J.E., Stark M.J., Fenaughty A., O'Connor T. Effectiveness of a tobacco quitline in an indigenous population: A comparison between Alaska Native people and other first-time quitline callers who set a quit date. International Journal of Circumpolar Health. 2009;68(2):170–181. doi: 10.3402/ijch.v68i2.18301. [DOI] [PubMed] [Google Scholar]
- Borrelli B. Smoking cessation: Next steps for special populations research and innovative treatments. Journal of Consulting and Clinical Psychology. 2010;78(1):1–12. doi: 10.1037/a0018327. [DOI] [PubMed] [Google Scholar]
- Breslau N., Peterson E.L. Smoking cessation in young adults: Age at initiation of cigarette smoking and other suspected influences. Am Journal Public Health. 1996;86(2):214–220. doi: 10.2105/ajph.86.2.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carmack A.M., Schade T.L., Sallison I., Provost E.M., Kelly J.J. Cancer in Alaska Native people: 1969–2013, the 45-year report. 2015. http://anthctoday.org/epicenter/publications/cancer_report/45_Year_Report_FINAL_Online_Version.pdf Retrieved from:
- Chassin L., Presson C.C., Macy J.T. Adolescent susceptibility to smoking: The importance of an international perspective. The Journal of Adolescent Health. 2014;54(2):119–120. doi: 10.1016/j.jadohealth.2013.11.014. [DOI] [PubMed] [Google Scholar]
- Choi W.S., Gilpin E.A., Farkas A.J., Pierce J.P. Determining the probability of future smoking among adolescents. Addiction. 2001;96(2):313–323. doi: 10.1046/j.1360-0443.2001.96231315.x. [DOI] [PubMed] [Google Scholar]
- DiFranza J.R., Rigotti N.A., McNeill A.D., Ockene J.K., Savageau J.A., St Cyr D., Coleman M. Initial symptoms of nicotine dependence in adolescents. Tobacco Control. 2000;9(3):313–319. doi: 10.1136/tc.9.3.313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dilley J.A., Peterson E., Hiratsuka V.Y., Rohde K. Discovering unique tobacco use patterns among Alaska Native people. International Journal of Circumpolar Health. 2013;72(1):21208. doi: 10.3402/ijch.v72i0.21208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Espy K.A., Fang H., Johnson C., Stopp C., Wiebe S.A. Prenatal tobacco exposure: Developmental outcomes in the neonatal period. Developmental Psychology. 2011;47(1):153–156. doi: 10.1037/a0020724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farrelly M.C., Duke J.C., Nonnemaker J., MacMonegle A.J., Alexander T.N., Zhao X.…Allen J.A. Association between the real cost media campaign and smoking initiation among youths - United States, 2014–2016. MMWR. Morbidity and Mortality Weekly Report. 2017;66(2):47–50. doi: 10.15585/mmwr.mm6602a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farrelly M.C., Nonnemaker J., Davis K.C., Hussin A. The influence of the national truth campaign on smoking initiation. American Journal of Preventive Medicine. 2009;36(5):379–384. doi: 10.1016/j.amepre.2009.01.019. [DOI] [PubMed] [Google Scholar]
- Freedman K.S., Nelson N.M., Feldman L.L. Smoking initiation among young adults in the United States and Canada, 1998–2010: A systematic review. Preventing Chronic Disease. 2012;9:110037. [PMC free article] [PubMed] [Google Scholar]
- Hegmann K.T., Fraser A.M., Keaney R.P., Moser S.E., Nilasena D.S., Sedlars M.…Lyon J.L. The effect of age at smoking initiation on lung cancer risk. Epidemiology. 1993;4(5):444–448. doi: 10.1097/00001648-199309000-00010. [DOI] [PubMed] [Google Scholar]
- Howard B.V., Devereux R.B., Cole S.A., Davidson M., Dyke B., Ebbesson S.O.…Robbins D.C. A genetic and epidemiologic study of cardiovascular disease in Alaska Natives (GOCADAN): Design and methods. International Journal of Circumpolar Health. 2005;64(3):206–221. doi: 10.3402/ijch.v64i3.17985. [DOI] [PubMed] [Google Scholar]
- Hurt R.D., Renner C.C., Patten C.A., Ebbert J.O., Offord K.P., Schroeder D.R.…Moyer T.P. Iqmik—A form of smokeless tobacco used by pregnant Alaska Natives: Nicotine exposure in their neonates. The Journal of Maternal-Fetal & Neonatal Medicine. 2005;17(4):281–289. doi: 10.1080/14767050500123731. [DOI] [PubMed] [Google Scholar]
- Johnson E.O., Schultz L. Forward telescoping bias in reported age of onset: An example from cigarette smoking. International Journal of Methods in Psychiatric Research. 2005;14(3):119–129. doi: 10.1002/mpr.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson T.P., Mott J.A. The reliability of self-reported age of onset of tobacco, alcohol and illicit drug use. Addiction. 2001;96(8):1187–1198. doi: 10.1046/j.1360-0443.2001.968118711.x. [DOI] [PubMed] [Google Scholar]
- Johnston L.D., O'Malley P.M., Bachman J.G., Schulenber J.E. Institute for Social Research, The University of Michigan; Ann Arbor, MI: 2013. Monitoring the future: National results on adolescent drug use: 2012 overview of key findings on adolescent drug use. [Google Scholar]
- Kann L., Kinchen S., Shanklin S.L., Flint K.H., Kawkins J., Harris W.A.…Centers for Disease Control and Prevention (CDC) Youth risk behavior surveillance—United States, 2013. MMWR Suppl. 2014;63(4):1–168. [PubMed] [Google Scholar]
- Kann L., McManus T., Harris W.A., Shanklin S.L., Flint K.H., Queen B.…Ethier K.A. Youth risk behavior surveillance — United States, 2017. MMWR Surveillance Summaries. 2018;67(8):1–114. doi: 10.15585/mmwr.ss6708a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasza K.A., Ambrose B.K., Conway K.P., Borek N., Taylor K., Goniewicz M.L.…Hyland A.J. Tobacco-product use by adults and youths in the United States in 2013 and 2014. The New England Journal of Medicine. 2017;376(4):342–353. doi: 10.1056/NEJMsa1607538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khuder S.A., Dayal H.H., Mutgi A.B. Age at smoking onset and its effect on smoking cessation. Addictive Behaviors. 1999;24(5):673–677. doi: 10.1016/s0306-4603(98)00113-0. [DOI] [PubMed] [Google Scholar]
- Koller K.R., Flanagan C.A., Day G.E., Patten C.A., Umans J.G., Austin M.A.…Boyer B. High tobacco use prevalence with significant regional and sex differences in smokeless tobacco use among Western Alaska Native people: The WATCH study. International Journal of Circumpolar Health. 2017;72(1):1398009. doi: 10.1080/22423982.2017.1398009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koller K.R., Wolfe A.W., Metzger J.S., Austin M.A., Hopkins S.E., Kaufmann C.…Boyer B.B. Utilizing harmonization and common surveillance methods to consolidate 4 cohorts: The Western Alaska Tribal Collaborative for Health (WATCH) study. International Journal of Circumpolar Health. 2013;72(1):20572. doi: 10.3402/ijch.v72i0.20572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lando H.A., Thai D.T., Murray D.M., Robinson L.A., Jeffery R.W., Sherwood N.E., Hennrikus D.J. Age of initiation, smoking patterns, and risk in a population of working adults. Preventive Medicine. 1999;29(6 Pt 1):590–598. doi: 10.1006/pmed.1999.0590. [DOI] [PubMed] [Google Scholar]
- Liska S.R. In utero exposure to Black Bull chewing tobacco and neonatal nicotine withdrawal: A review of the literature. Neonatal Network. 2014;33(1):5–10. doi: 10.1891/0730-0832.33.1.5. [DOI] [PubMed] [Google Scholar]
- Mohatt G.V., Plaetke R., Klejka J., Luick B., Lardon C., Bersamin A.…Center for Alaska Native Health Research The Center for Alaska Native Health Research Study: A community-based participatory research study of obesity and chronic disease-related protective and risk factors. International Journal of Circumpolar Health. 2007;66(1):8–18. doi: 10.3402/ijch.v66i1.18219. [DOI] [PubMed] [Google Scholar]
- Odani S., Armour B.S., Agaku I.T. Racial/ethnic disparities in tobacco product use among middle and high school students — United States, 2014–2017. MMWR. Morbidity and Mortality Weekly Report. 2018;67(34):952–957. doi: 10.15585/mmwr.mm6734a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patten C.A., Enoch C., Renner C.C., Offord K.P., Nevak C., Kelley S.F.…Kaur J.S. Focus groups of Alaska Native adolescent tobacco users: Preferences for tobacco cessation interventions and barriers to participation. Health Education & Behavior. 2009;36(4):711–723. doi: 10.1177/1090198107309456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce J.P., Choi W.S., Gilpin E.A., Farkas A.J., Merritt R.K. Validation of susceptibility as a predictor of which adolescents take up smoking in the United States. Health Psychology. 1996;15(5):355–361. doi: 10.1037//0278-6133.15.5.355. [DOI] [PubMed] [Google Scholar]
- Pierce J.P., White V.M., Emery S.L. What public health strategies are needed to reduce smoking initiation? Tobacco Control. 2012;21(2):258–264. doi: 10.1136/tobaccocontrol-2011-050359. [DOI] [PubMed] [Google Scholar]
- Renner C.C., Enoch C., Patten C.A., Ebbert J.O., Hurt R.D., Moyer T.P., Provost E.M. Iqmik: A form of smokeless tobacco used among Alaska Natives. American Journal of Health Behavior. 2005;29(6):588–594. doi: 10.5555/ajhb.2005.29.6.588. [DOI] [PubMed] [Google Scholar]
- Renner C.C., Lanier A.P., Lindgren B., Jensen J., Patten C.A., Parascandola M.…Hatsukami D.K. Tobacco use among southwestern Alaska Native people. Nicotine & Tobacco Research. 2013;15(2):401–406. doi: 10.1093/ntr/nts137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Renner C.C., Patten C.A., Enoch C., Petraitis J., Offord K.P., Angstman S.…Hurt R.D. Focus groups of Y-K Delta Alaska Natives: Attitudes toward tobacco use and tobacco dependence interventions. Preventive Medicine. 2004;38(4):421–431. doi: 10.1016/j.ypmed.2003.11.005. [DOI] [PubMed] [Google Scholar]
- Sargent J.D., Gabrielli J., Budney A., Soneji S., Wills T.A. Adolescent smoking experimentation as a predictor of daily cigarette smoking. Drug and Alcohol Dependence. 2017;175:55–59. doi: 10.1016/j.drugalcdep.2017.01.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slattery M.L., Schumacher M.C., Lanier A.P., Edwards S., Edwards R., Murtaugh M.A.…Henderson J.A. A prospective cohort of American Indian and Alaska Native people: Study design, methods, and implementation. American Journal of Epidemiology. 2007;166(5):606–615. doi: 10.1093/aje/kwm109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith J.J., Ferucci E.D., Dillard D.A., Lanier A.P. Tobacco use among Alaska Native people in the EARTH study. Nicotine & Tobacco Research. 2010;12(8):839–844. doi: 10.1093/ntr/ntq091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soneji S., Sargent J., Tanski S. Multiple tobacco product use among US adolescents and young adults. Tobacco Control. 2016;25(2):174–180. doi: 10.1136/tobaccocontrol-2014-051638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA) Results from the 2012 National Survey on Drug Use and Health, NSDUH: Detailed tables, 2013. 2013. https://www.samhsa.gov/data/sites/default/files/NSDUHresults2012/NSDUHresults2012.pdf Retrieved from:
- Substance Abuse and Mental Health Services Administration (SAMHSA) Results from the 2015 National Survey on Drug Use and Health, NSDUH: Detailed tables, 2016. 2016. https://www.samhsa.gov/data/sites/default/files/NSDUH-DetTabs-2015/NSDUH-DetTabs-2015/NSDUH-DetTabs-2015.pdf Retrieved from: [PubMed]
- Thompson A.B., Mowery P.D., Tebes J.K., McKee S.A. Time trends in smoking onset by sex and race/ethnicity among adolescents and young adults: Findings from the 2006–2013 National Survey on Drug Use and Health. Nicotine & Tobacco Research. 2017 doi: 10.1093/ntr/ntx010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services (USDHHS) U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; Atlanta, GA: 2012. Preventing tobacco use among youth and young adults: A report of the surgeon general. [Google Scholar]
- Wolsko C., Mohatt G.V., Lardon C., Burket R. Smoking, chewing, and cultural identity: Prevalence and correlates of tobacco use among the Yup'ik—The Center for Alaska Native Health Research (CANHR) study. Cultural Diversity & Ethnic Minority Psychology. 2009;15(2):165–172. doi: 10.1037/a0015323. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Percent age of initiation of any tobacco product among western Alaska Native adult ever tobacco users: the WATCH study.⁎
Percent age of cigarette smoking initiation among western Alaska Native adult ever smokers: the WATCH study.⁎
Percent age of smokeless tobacco initiation among Y-K Delta Alaska Native adult ever smokeless tobacco users: the WATCH study.