Abstract
Foreign body ingestion is a common reason for visiting the emergency room. Foreign bodies can lodge anywhere in the upper aerodigestive tract and can sometimes be difficult to extract. Wire bristles that dislodge from grill-cleaning wire brushes and which are then accidentally swallowed can be particularly challenging to remove due to their small size, propensity to become embedded, and their ability to migrate through tissues. This case reveals the speed with which wire bristle foreign bodies can migrate through tissues and exemplifies the need to obtain computerized tomography evaluations in close proximity to any planned attempt to remove them.
Keywords: Otolaryngology, surgery, gastroenterology/hepatology, wire bristle, pharyngeal foreign body
Introduction
Grill-cleaning wire brush bristles represent an uncommon perpetrator of accidental ingestion, which have gained more awareness in the past decade. These objects dislodge from the brush after a cleaning and adhere to food cooked on the grill. Patients who ingest wire bristles present with pain while eating, as the sharp and malleable bristles lodge into the oral mucosa or into distal parts of the aerodigestive tract.
Diagnosing ingested wire bristles can be challenging due to the non-specific symptoms of throat pain, swelling, dysphagia, and odynophagia. A systematic review by Mortensen highlighted how visualization and diagnosis require multiple imaging modalities and procedures. They reported that initial imaging with lateral neck radiography or evaluation with flexible laryngoscopy was falsely negative in 30% and 47%, respectively.1 Plain radiographs might be sufficient in children with suspected coin ingestion but computerized tomography (CT) has been shown to have the highest sensitivity when attempting to diagnose small metallic foreign bodies such as wire bristles.1–3 However, diagnosing a wire bristle foreign body is only half the battle, as extraction of this foreign body can be equally challenging.
The case
A 63-year-old woman presented to an emergency room with dysphagia and throat pain for 2 h following an episode of sharp pain while eating a hot dog at a barbecue. No foreign bodies were visualized on physical exam, and an esophagoscopy was negative. As there was no evidence of a foreign body found, she was discharged home without further treatment.
The patient’s dysphagia worsened, and she presented back to the emergency department seven days later. A non-contrast neck CT revealed a curvilinear metallic object embedded within the soft tissue of the left posterior oropharynx (Figure 1). Fiberoptic laryngoscopy revealed no evidence of foreign body. She was taken to the operating room for direct laryngoscopy and an abscess in the left tonsil was discovered, and several of the tonsillar crypts were explored without evidence of the wire. Several real-time x-rays were obtained without evidence of a targetable object to remove. Following this, a repeat non-contrast CT was obtained, which revealed a curvilinear calcification within the left lateral pharyngeal wall. This was interpreted as a tortuous calcified left internal carotid artery and soft tissue fullness of the left lateral pharyngeal wall below the base of the tongue. She presented for follow up 1 month later with a persistent sore throat and incessant throat clearing but no dysphagia. Repeat laryngoscopy revealed a swollen pharynx and tonsillar swelling but no foreign bodies.
Figure 1.
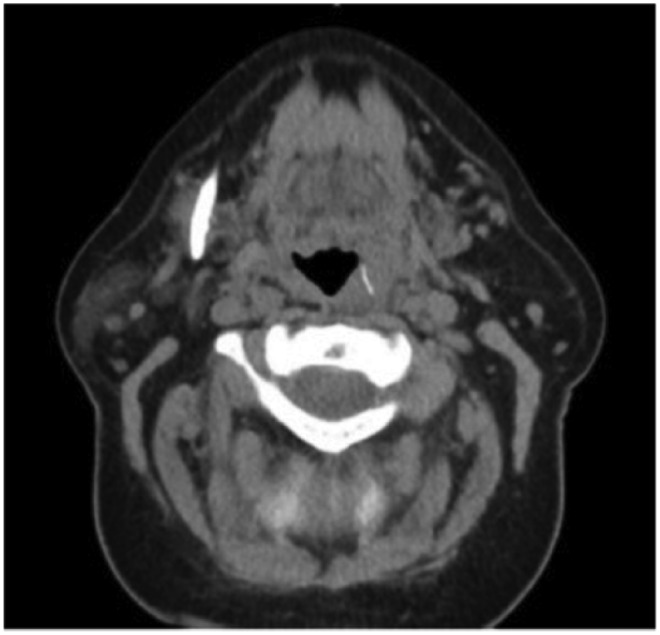
An axial non-contrast CT scan demonstrating the radiopaque foreign body lodged within left palatine tonsil soft tissue.
Due to continued discomfort, she presented to the University of Michigan Otolaryngology-HNS Department for a second opinion. Her presentation was concerning for a persistent foreign body. Another CT without contrast was obtained and the previously identified linear hyperdensity in the left palatine tonsil had migrated into the right retro-hypopharyngeal region (Figure 2(a) and (b)). A plan was developed with the patient to perform a trans cervical approach to removal due to the foreign body’s lateral location and proximity to the carotid artery. Given the migration of the foreign body, a repeat CT with contrast was obtained immediately prior to removal and once again showed migration to a midline position of the retropharynx anterior to C2C3 level (Figure 3). This resulted in a change in the operative plan to a transoral approach. Once general anesthesia was induced, palpation revealed a thin linear area of firmness in the posterior pharynx at the level just above the tip of the epiglottis. The foreign body was successfully removed through an intraoral incision and retropharyngeal dissection deep to the constrictor muscle with complete resolution of her symptoms (Figure 4).
Figure 2.
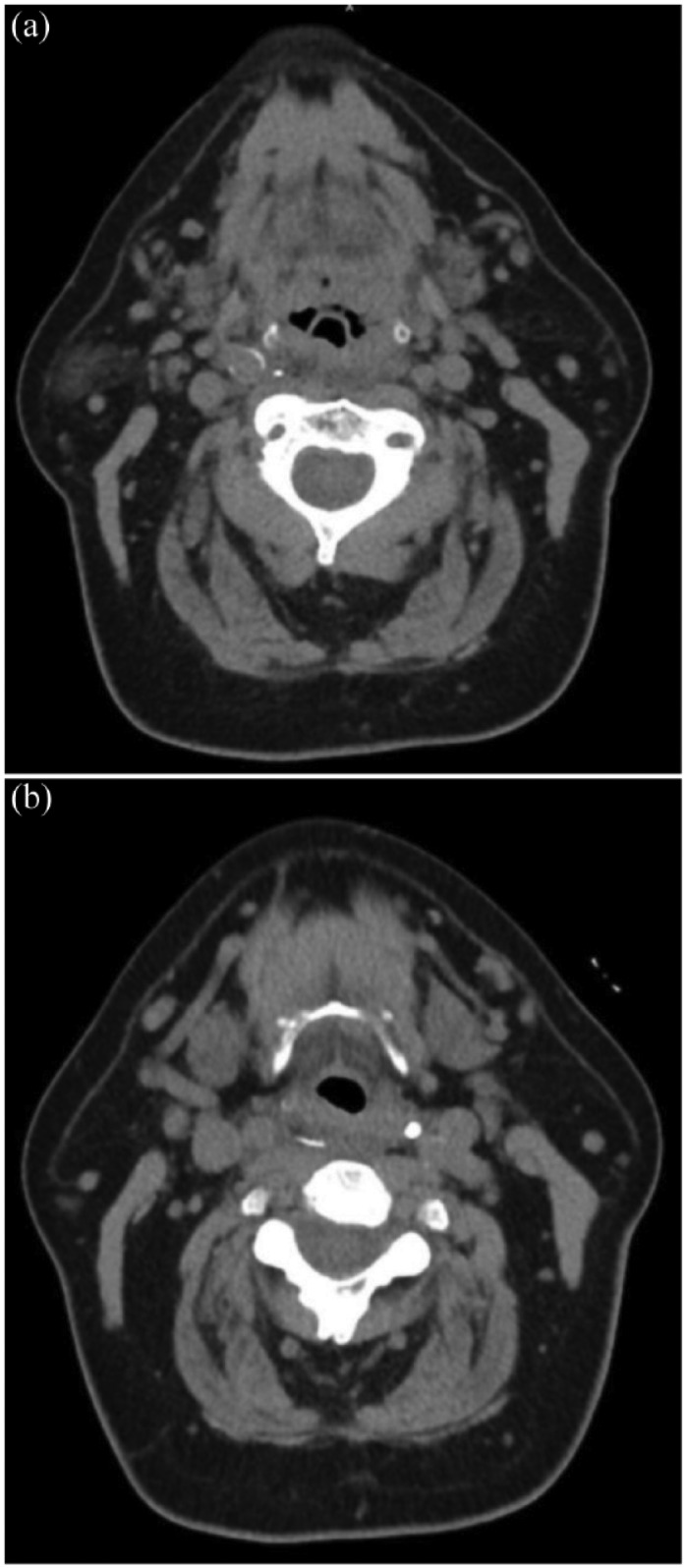
(a) An axial cut on a non-contrast CT scan showing the wire bristle located medially to the right carotid artery (demonstrated by rim calcifications). (b) An axial cut just caudal to the prior image showing the medial extent of the wire in the retropharyngeal plane.
Figure 3.
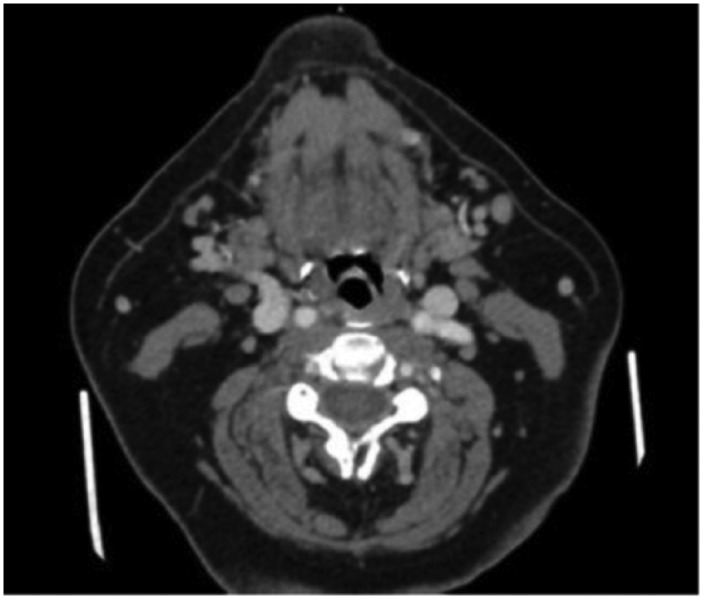
An axial CT scan with contrast showing the radiopaque foreign body in the midline retropharyngeal space in a horizontal orientation.
Figure 4.
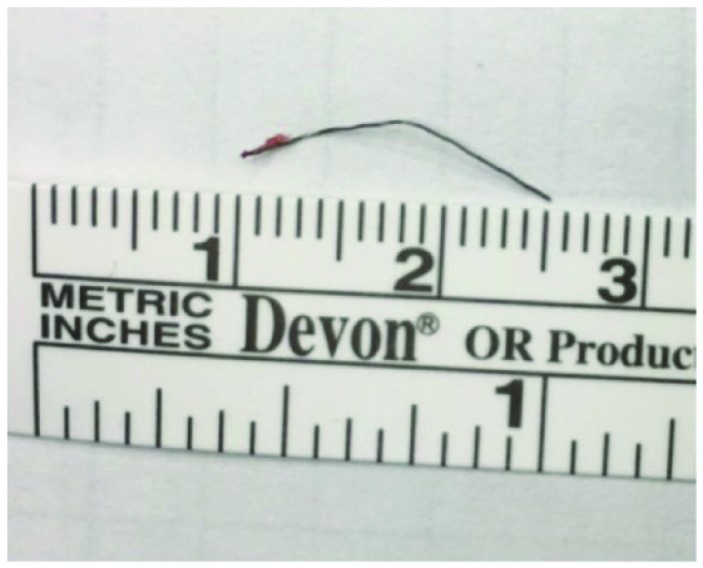
Image of wire bristle following removal.
Discussion
Grill-cleaning wire brush bristles are infrequently identified foreign bodies associated with 1698 emergency room visits from 2002–2014 but less than 35 published case reports.1,2 The first report of an ingested wire bristle was in a 19-year-old patient who suffered from eventual esophageal perforation due to foreign body ingestion in 1952.3 Subsequent cases have included pediatric and adult patients and noted that ingested bristles were commonly located in the base of the tongue, esophagus, palatine tonsils, parapharyngeal space, vallecula, and in the gastrointestinal tract.1,4–13
Non-specific patient symptoms, small size, and easy migration make diagnosis and management of ingested wire bristles challenging. For patients with persistent globus, dysphagia, or odynophagia, it is important to maintain a high index of suspicion even with negative endoscopic examinations. The American Medical Association, Centers for Disease Control and Prevention, and Health Canada have all issued warnings regarding the risks of grill bristle ingestion; we support further investigation of the public health risk and possible greater restrictions or a ban on wire bristle grill brushes. We also suggest considering alternative grill-cleaning products, such as a grill stone or scraper, aluminum foil, or liquid grill cleaners to avoid the unintentional ingestion of the wire bristles.9,13
Wong et al.5 published an algorithm for diagnosis and removal of suspected brush bristle ingestions, including a physical examination and flexible fiberoptic laryngoscopy. If a foreign body is visualized and accessible, bedside endoscopic extraction with local anesthetic spray should be undertaken. If negative, a non-contrast CT scan is preferred over an x-ray because of its greater sensitivity.
In our case report, the patient’s wire bristle was not visualized on esophagoscopy or fiberoptic laryngoscopy. Diagnosis was initially established with a non-contrast CT, but migration of the wire led to failed endoscopic removal. The proximity of the bristle to the carotid artery led to a misdiagnosis by non-contrast CT, months of further symptoms, and delayed removal.
Different modalities have been used to retrieve the bristles including esophagoscopy,6 suspension microscopic laryngoscopy,6 partial tonsillectomy with coblation,11 and intraoperative C-arm fluoroscopy.7 Regardless of the retrieval modality, close to 40% of first attempts at removing the bristle have been unsuccessful and close to 22% have required open neck exploration to remove the foreign bodies.1 Harlor et al.10 and Mortensen et al.1 have suggested the use of contrasted imaging to localize bristles that have migrated, especially those close to vascular structures in the head and neck. We also believe that a contrasted CT with 1–2 mm cuts better highlights anatomy and is more suited for operative planning.
Conclusion
Wire brush bristles can easily adhere to food after a barbecue grill is cleaned and may dislodge into the oral mucosa or distal parts of the upper aerodigestive tract. Symptoms of persistent globus sensation, dysphagia, or odynophagia should be investigated for an ingested wire bristle, especially in the context of recent barbecue use. Physical examination, esophagoscopy, or flexible laryngoscopy is often negative. Non-contrasted CT is helpful in establishing the diagnosis. However, CT imaging with contrast is more suited for precise localization and operative planning, especially when the bristles are located near important vasculature in the head and neck. Depending on the precise location of the bristle brush, different modalities including endoscopic removal might be effective.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: Ethical approval to report this case was obtained from University of Michigan IRB - HUM00161403.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Written informed consent was obtained from the patient(s) for their anonymized information to be published in this article.
ORCID iD: Mark EP Prince  https://orcid.org/0000-0002-1120-9008
https://orcid.org/0000-0002-1120-9008
References
- 1. Mortensen M, Samara G, Regenbogen E. Grill-cleaning wire brush bristle ingestion: case series and review of the literature. Ann Otol Rhinol Laryngol 2018; 127(10): 698–702. [DOI] [PubMed] [Google Scholar]
- 2. Grand DJ, Cloutier DR, Beland MD, et al. Inadvertent ingestion of wire bristles from a grill cleaning brush: radiologic detection of unsuspected foreign bodies. Am J Roentgenol 2012; 198(4): 836–839. [DOI] [PubMed] [Google Scholar]
- 3. Pinto A, Brunese L, Daniele S, et al. Role of computed tomography in the assessment of intraorbital foreign bodies. Semin Ultrasound CT MR 2012; 33(5): 392–395. [DOI] [PubMed] [Google Scholar]
- 4. Zafar AM, Chiang FL, Fazal Z, et al. Grill-cleaning wire brush bristle ingestion: two cases and review of literature with focus on diagnostic approach. Am J Med 2016; 129(7): e61–e63. [DOI] [PubMed] [Google Scholar]
- 5. Wong S, Brook C, Grillone G. Management of wire brush bristle ingestion: review of literature and presentation of an algorithm. Ann Otol Rhinol Laryngol 2016; 125(2): 160–164. [DOI] [PubMed] [Google Scholar]
- 6. Baugh TP, Hadley JB, Chang CW. Epidemiology of wire-bristle grill brush injury in the United States, 2002-2014. Otolaryngol Head Neck Surg 2016; 154(4): 645–649. [DOI] [PubMed] [Google Scholar]
- 7. Naunheim MR, Dedmon MM, Mori MC, et al. Removal of a wire brush bristle from the hypopharynx using suspension, microscope, and fluoroscopy. Case Rep Otolaryngol 2015; 2015: e925873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. McMullen CP, Frank DK, Smith LP. Backyard hazard: a case series of ingested grill brush bristles and a novel approach to extraction. Am J Otolaryngol 2012; 33(6): 731–734. [DOI] [PubMed] [Google Scholar]
- 9. Ballenger J, Bennet R, Dorsey J. Perforation of esophagus by a wire bristle and its removal. Q Bull Northwest Univ Med Sch 1952; 26(4): 309–311. [PMC free article] [PubMed] [Google Scholar]
- 10. Harlor EJ, Lindemann TL, Kennedy TL. Outdoor grilling hazard:wire bristle esophageal foreign body-a report of six cases. Laryngoscope 2012; 122(10): 2216–2218. [DOI] [PubMed] [Google Scholar]
- 11. Campisi P, Stewart C, Forte V. Penetrating esophageal injury by ingestion of a wire bristle. J Pediatr Surg 2005; 40(10): e15–e16. [DOI] [PubMed] [Google Scholar]
- 12. Boon M, Pribitkin E, Spiegel J, et al. Lingual abscess from a grill cleaning brush bristle. Laryngoscope 2009; 119(1): 79–81. [DOI] [PubMed] [Google Scholar]
- 13. Dolce A. How to clean your grill without a grill brush. The Daily Meal, 2012, http://www.thedailymeal.com/how-clean-yourgrillwithout-grill-brush


