Abstract
Study design:
A retrospective cohort study.
Objective:
To investigate factors influencing the incidence of moderate to severe postoperative axial neck pain following cervical laminoplasty.
Methods:
We reviewed 125 patients with cervical myelopathy who underwent double-door laminoplasty. The primary outcomes were the Numerical Rating Scale score (NRS score, 0-10) for neck pain, the Short Form 36 (SF-36) Health Survey score (Physical and Mental Component Summary scores [PCS and MCS, respectively]), and satisfaction. Imaging parameters on plain radiographs and magnetic resonance imaging were also evaluated. Patients with moderate to severe postoperative neck pain (NRS ≥ 5) were compared with those with no or mild neck pain (NRS ≤ 4).
Results:
One hundred and three patients (82%) with complete data were eligible for inclusion. There were 67 men and 36 women, with a mean age of 65 years (32-89 years). Twenty-five patients (23%) had moderate to severe postoperative axial pain (NRS ≥ 5) and were compared with the other 78 patients (NRS ≤ 4), which revealed several predictive factors, including female sex, the presence of preoperative neck pain, low postoperative PCS, low preoperative and postoperative MCS, and satisfaction with the treatment. Multivariable logistic regression analysis revealed that the postoperative MCS (P = .002) was a risk factor for postoperative neck pain, although the preoperative MCS did not reach statistical significance (P = .06).
Conclusions:
Patients with a low mental state, possibly before surgery, are at a high risk for postoperative axial neck pain. None of the imaging parameters were statistically different.
Keywords: mental component score, physical component score, complication, cervical myelopathy, satisfaction, neck pain
Introduction
Cervical laminoplasty is one of the established procedures for the treatment of cervical compression myelopathy, and relatively good surgical results have been reported in terms of neurological improvement.1,2 However, postoperative axial neck pain has been reported as a complication after cervical laminoplasty.3-9 Because postoperative axial pain will affect a patient’s satisfaction and health-related quality of life,10-12 surgeons should consider the preoperative risk factors and anticipate this surgery-related complication.
The reported incidence of axial neck pain after cervical laminoplasty ranges from 5.1% to 61.5%.3,5,6,13-15 Many researchers have examined factors as causes of axial pain after cervical laminoplasty and have identified the involvement of age, sex, radiological assessment, and preoperative neck pain, although some of these factors are controversial. Few reports have investigated the involvement of both physical or mental outcome scores and imaging evaluations. It is reasonable to speculate that the mental state of patients can modify the degree of pain in general. Therefore, postoperative axial pain after cervical laminoplasty can be expected to occur according to the degree of mental health of patients.
One possible problem in investigating the causes of neck pain is that the definitions of pain intensity and distribution are vague and differ among studies. We consider this as a reason for the inconsistency in results with regard to the occurrence of postoperative axial neck pain. Indeed, few previous reports involved quantitative evaluation using a visual analog scale or numerical rating scale reported by patients. Moreover, the term “neck” in the past reports was obscure with regard to the inclusion of scapular and shoulder lesions, possibly representing the involvement of radiculopathy.
The present study aimed to investigate factors influencing postoperative axial neck pain in patients with cervical myelopathy undergoing double-door laminoplasty. To eliminate confusion, we defined neck pain with the exclusion of the scapular and shoulder area using an illustration of each part of the body.
Materials and Methods
The study protocols were approved by the institutional review board of our institution. This is a retrospective cohort study of 125 patients with cervical compression myelopathy who underwent double-door laminoplasty between 2004 and 2011 and replied to a questionnaire on patient-reported outcomes preoperatively. The primary outcomes were the Numerical Rating Scale score (NRS score, 0-10) for neck pain (Figure 1) and the Short Form 36 (SF-36) Health Survey score (Physical and Mental Component Summary scores [PCS and MCS, respectively]). Postoperative axial pain was defined as an NRS score ≥5, as we aimed to select patients with moderate to severe neck pain.16 Satisfaction was evaluated based on a 7-point scale as follows: very satisfied, satisfied, slightly satisfied, neither satisfied nor dissatisfied, slightly dissatisfied, dissatisfied, and very dissatisfied. Patients were divided into 2 groups: satisfied (very satisfied, satisfied, slightly satisfied) and dissatisfied (neither satisfied nor dissatisfied, slightly dissatisfied, dissatisfied, very dissatisfied). Radiological parameters included the Cobb angle between the C2 and C7 vertebras in cervical lateral radiographs (C2-C7 Cobb angle), range of motion between C2 and C7, C7 slope, and the presence of spondylolisthesis (>3.5 mm). Magnetic resonance imaging (MRI) evaluation included the presence or absence of intramedullary signal changes and the maximum spinal cord compression (MSCC). The degree of cervical spinal cord compression was evaluated using midsagittal T2-weighted MRI, as described previously, by comparing the sagittal diameter of the spinal cord at the maximum compression level with that of C1 and C7 (MSCC).17 A higher MSCC indicates that the patient has severe cervical spinal cord compression.
Figure 1.
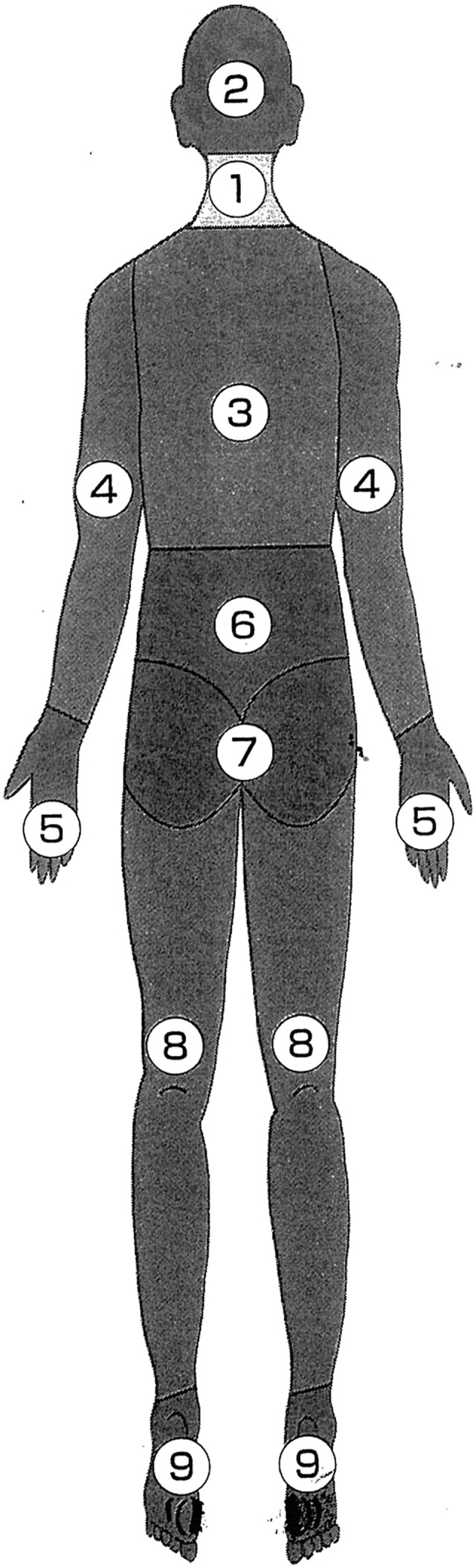
Each area was defined as the diagram. “Neck” was defined as the area labeled No. 1.
Statistical Analysis
The Mann-Whitney U test was used for nonparametric data, and the χ2 test was used for categorical variables. Propensity score adjustment was performed, and it preserved statistical power by reducing covariates into a single variable. For example, when the adjusted effect of postoperative axial pain was evaluated, the propensity score was obtained through a binary logistic regression that provided the predicted probability of having postoperative axial pain as a function of the other candidate risk factors. For continuous variables, a proportional odds logistic regression model was used to derive the propensity score. The propensity score was separately computed for each candidate risk factor and was then used as a covariate in the model evaluating the adjusted effect of each factor. Locally weighted scatterplot smoothing was used to assess the association between fluoroquinolone exposure and fluoroquinolone-resistant tuberculosis. The statistical package SAS 9.4 (SAS Institute, Inc, Cary, NC) was used for all analyses. All P values were 2-sided, and a P value of <.05 was considered statistically significant.
Results
One hundred and three patients (82%) with complete data were eligible for inclusion. There were 67 men and 36 women, and the mean patient age was 65 years (range = 32-89 years). The mean follow-up period was 24 months (range = 12-60 months; Table 1). Twenty-five patients (23%) had moderate to severe axial neck pain (NRS score ≥5), whereas 78 patients did not (NRS score ≤4). These groups of patients were compared (Table 2). The proportion of female patients and the average score of preoperative neck pain were significantly higher among patients with postoperative axial neck pain than among those without postoperative axial pain. Furthermore, both the preoperative and postoperative PCS and MCS of SF-36 were worse among patients with postoperative axial neck pain than among those without postoperative axial neck pain, although only the preoperative PCS did not reach statistical significance. The surgical levels included C7 in 89% of the patients, and this did not affect the incidence of postoperative neck pain. Only 11 patients (44%) were satisfied with the surgical treatment in those with postoperative neck pain, whereas 57 patients (73%) were satisfied in those without postoperative neck pain (P = .001). None of the imaging parameters was statistically different between the 2 groups. Multivariable logistic regression analysis revealed that the postoperative MCS (odds ratio = 1.11) was a risk factor associated with postoperative neck pain (Table 3).
Table 1.
Demographic Data of Patients (N = 103).
| Age (year) | 65 (range = 32-89) |
| Sex (male/female) | 67/36 |
| Follow-up (months) | 24 (range = 12-60) |
| CSM/OPLL | 59/44 |
Abbreviations: CSM, cervical spondylotic myelopathy; OPLL, ossification of the posterior longitudinal ligament.
Table 2.
Comparison Between Patients With (NRS ≥5) and Without (NRS ≤4) Postoperative Axial Pain Groups.
| No Pain (N = 78) | Axial Pain (N = 25) | ||||||
|---|---|---|---|---|---|---|---|
| Average | SD | Average | SD | P a | |||
| Age | 63.9 | 11.8 | 65.8 | 10.7 | .48 | ||
| Sexb | Male/female | 55/23 | 12/13 | .04 | |||
| Follow-up | 24.1 | 8.7 | 25 | 11.9 | .72 | ||
| CSM/OPLLb | 41/37 | 18/7 | .11 | ||||
| Involvement of C7b | 70/8 | 21/4 | .83 | ||||
| Neck pain | Pre | 1.4 | 2.4 | 3.6 | 2.5 | <.0001 | |
| Post | 1.0 | 1.4 | 6.3 | 1.3 | <.0001 | ||
| SF-36 | PCS | Pre | 23.4 | 19.3 | 16.0 | 15.4 | .09 |
| Post | 35.2 | 17.5 | 20.5 | 16.4 | .001 | ||
| MCS | Pre | 50.9 | 11.5 | 42.7 | 8.5 | .003 | |
| Post | 52.8 | 9.6 | 43.3 | 9.1 | <.0001 | ||
| Radiographic measurements | |||||||
| C2/7 Cobb | Pre | 9.3 | 9.8 | 9.8 | 7.9 | .81 | |
| Post | 9.5 | 11.8 | 7.6 | 11.3 | .48 | ||
| ROM | Pre | 39.7 | 15.2 | 37.1 | 16.0 | .60 | |
| Post | 25.7 | 12.3 | 23.7 | 12.1 | .47 | ||
| C7 slope | Pre | 26.2 | 8.9 | 26.6 | 8.7 | .81 | |
| Post | 26.4 | 9.6 | 24.8 | 9.3 | .46 | ||
| Slip (yes/no)b | Pre | 66/10 | 22/3 | 1.00 | |||
| MRI measurements | |||||||
| MSCC | Pre | 45.8 | 18.0 | 40.9 | 12.8 | .26 | |
| T2 high (yes/no)b | Pre | 68/10 | 20/5 | .51 | |||
Abbreviations: NRS, Numerical Rating Scale; CSM, cervical spondylotic myelopathy; OPLL, ossification of the posterior longitudinal ligament; PCS, Physical Component Summary; MCS, Mental Component Summary; ROM, range of motion; MRI, magnetic resonance imaging; MSCC, maximum spinal cord compression; Pre, preoperative; Post, postoperative.
a Significant values (P < .05) are shown in boldface.
b Number of patients.
Table 3.
Risk Factors for Postoperative Axial Neck Pain (≥5): Multivariable Logistic Regression Analysis.
| OR | 95% CI | P | |
|---|---|---|---|
| Sex (female) | 1.02 | 0.25-3.73 | .97 |
| Pre neck pain (≥5) | 2.04 | 0.50-8.12 | .24 |
| Pre MCS | 1.06 | 1.00-1.13 | .06 |
| Post PCS | 1.01 | 0.96-1.05 | .77 |
| Post MCS | 1.11 | 1.04-1.20 | .002 |
Abbreviations: OR, odds ratio; CI, confidence interval; MCS, Mental Component Summary; PCS, Physical Component Summary; Pre, preoperative; Post, postoperative.
Discussion
We sought to clarify the factors influencing postoperative axial neck pain and found several predictive factors, including female sex, preoperative neck pain, and low MCS and PCS scores of SF-36. In particular, multivariable analysis revealed that mental factors may increase the risk of postoperative axial neck pain, although the preoperative MCS did not reach statistical significance. On the other hand, none of the radiographic parameters significantly affected the degree of postoperative axial neck pain.
Patients with postoperative neck pain could have 2 patterns. These involve one with preoperative neck pain and the other without preoperative neck pain. Our results showed that the mean preoperative pain intensity scores were higher in patients with postoperative axial neck pain. The causes of neck pain may involve several factors,18 such as discs,19,20 facet joints or posterior rami,21,22 muscles,14,23 posture,24 and radiculopathy.25 Of the various factors, spondylotic changes in the cervical spine may be the main cause of preoperative and postoperative neck pain. It is reasonable to speculate that some of these factors will influence the degree of postoperative neck pain, irrespective of newly developed, laminoplasty-related neck pain. Patients with postoperative neck pain may complain of preexisting neck pain before surgery. Indeed, in our series, no patients with cervical myelopathy underwent anterior or posterior fixation surgery even if preoperative neck pain was noted. It would be reasonable to speculate that some of these patients would have had less neck pain postoperatively if they had undergone fixation surgery. However, the existence of preoperative neck pain was insignificant after adjustment in multivariable analysis, indicating that this factor was not critical. Nevertheless, surgeons should be aware that patients with preoperative neck pain are more likely to complain of postoperative neck pain, regardless of the actual cause of neck pain. In patients with cervical myelopathy who have severe neck pain fixation surgery may be beneficial and may help reduce the pain.
This study showed the possible involvement of mental factors in the occurrence of postoperative axial neck pain even after adjustment for the presence of preoperative neck pain. It is reasonable to consider that patients with low mental scores have a lower threshold for pain. Indeed, it is well known that lower back pain is closely related to psychological problems.26 Previous reports have indicated the possible involvement of mental factors in the occurrence of neck pain,27 although they may not be as common in neck pain as in lower back pain. A relationship between a victim’s feeling and long-lasting neck pain after a traffic accident has been reported.28 Therefore, we speculate that patients who complained of postoperative axial neck pain in this study were susceptible to pain. On the other hand, we cannot exclude the possibility that postoperative pain affected MCS because only postoperative MCS significantly affected the incidence of postoperative axial neck pain in multivariable analysis. However, as preoperative MCS tended to be associated with the incidence of postoperative axial neck pain (P = .06), even after multivariable analysis, we believe that patients with a low mental state before surgery are at a high risk for postoperative axial neck pain. Detailed tools for detecting mental problems, such as Hospital Anxiety and Depression Scale,29 may be more effective in investigating the relationship between mental state and postoperative axial neck pain.In this study, we did not find any relationship between imaging parameters and postoperative axial neck pain. This finding is consistent with the findings of previous reports. Although the range of motion significantly decreased after surgery, the degree of postoperative neck pain was not influenced. On the other hand, several studies have shown that posterior muscle atrophy may be related to postoperative axial neck pain.30 The influence of the posterior paravertebral muscles is further supported by the fact that several less-invasive techniques have succeeded in reducing the incidence of postoperative axial pain, suggesting the importance of maintaining supporting structures.9,15,31-37 Because our procedure was not a muscle-preserving approach, the intensity of postoperative neck pain may have been high. We speculate that the incidence of postoperative axial neck pain can be reduced by utilizing a less-invasive, muscle-preserving method. A further study will be necessary to clarify this speculation.
The present study has several limitations. First, the design was retrospective and the follow-up period was not consistent, ranging from 12 to 60 months. Second, the number of patients was limited and therefore the results could be biased. Third, there are other confounding factors that were not investigated in this study, such as the degree of muscle dissection or duration of surgery, the intensity of postoperative physiotherapy, medications used for analgesia, and the duration of preoperative neck pain and neurological symptoms. Finally, the results may differ according to the cutoff value of the neck pain, although we believe that our definition of postoperative axial pain was adequate because patients’ satisfaction was significantly influenced. The limitations may impair the capacity of broad generalization of this study, and a future prospective study will be necessary to solve these problems.
Nevertheless, we believe that mental problems are related to postoperative complaints of axial neck pain, and patients with a low mental state, possibly before surgery, are at a high risk for postoperative axial neck pain. We believe that our findings will help surgeons predict and deal with postoperative neck pain following cervical laminoplasty.
Footnotes
Authors’ Note: The article does not contain information about medical device(s)/drug(s). The study approval was given by the institutional review board of the Clinical Research Support Center of the University of Tokyo Hospital. Portions of this work were presented in poster form in the Cervical Spine Research Society (CSRS) meeting in 2016.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Dr Riew reports personal fees from Biomet, Medtronic; other support from Nexgen, Amedica, Vertiflex, Benvenue, Spinal Kinetics, Spineology, Expanding Orthopedics, Osprey, Paradigm Spine, PSD; other support from Biomet, Medtronic; personal fees from Zeiss Teaching Webinar; other support from AO Spine; personal fees from AO Spine; other support from Advanced Medical, outside the submitted work. Dr Tanaka has received honoraria from Amgen Inc, Asahi Kasei Pharma Corporation, Amgen Astellas BioPharma K.K., Kyocera Medical Corporation, Daiichi Sankyo Company, Limited, Teijin Pharma Limited, Eli Lilly Japan K.K., Pfizer Japan Inc; endowments from Astellas Pharma Inc, Ayumi Pharmaceutical Corporation, BristolMyers Squibb, Pfizer Japan Inc, Daiichi Sankyo Company Limited, Chugai Pharmaceutical Co, Ltd; and grants from The Japan Agency for Medical Research and Development (AMED), Japan Society for the Promotion of Science (JSPS)/Grant-in-Aid for Scientific Research (A), and the Japan Society for the Promotion of Science (JSPS)/Grant-in-Aid for Exploratory Research. Dr Oshima, Dr Matsubayashi, Dr Taniguchi, Dr Hayakawa, Dr Fukushima, Dr Oichi, and Dr Oka have no conflicts of interest to disclose.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Seichi A, Takeshita K, Ohishi I, et al. Long-term results of double-door laminoplasty for cervical stenotic myelopathy. Spine (Phila Pa 1976). 2001;26:479–487. [DOI] [PubMed] [Google Scholar]
- 2. Oshima Y, Miyoshi K, Mikami Y, Nakamoto H, Tanaka S. Long-term outcomes of cervical laminoplasty in the elderly. Biomed Res Int. 2015;2015:713952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hosono N, Yonenobu K, Ono K. Neck and shoulder pain after laminoplasty. A noticeable complication. Spine (Phila Pa 1976). 1996;21:1969–1973. [DOI] [PubMed] [Google Scholar]
- 4. Moon MS. Neck and shoulder pain after laminoplasty. Spine (Phila Pa 1976). 1997;22:1674–1676. [DOI] [PubMed] [Google Scholar]
- 5. Wang SJ, Jiang SD, Jiang LS, Dai LY. Axial pain after posterior cervical spine surgery: a systematic review. Eur Spine J. 2011;20:185–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kawaguchi Y, Matsui H, Ishihara H, Gejo R, Yoshino O. Axial symptoms after en bloc cervical laminoplasty. J Spinal Disord. 1999;12:392–395. [PubMed] [Google Scholar]
- 7. Nurboja B, Kachramanoglou C, Choi D. Cervical laminectomy vs laminoplasty: is there a difference in outcome and postoperative pain? Neurosurgery. 2012;70:965–970. [DOI] [PubMed] [Google Scholar]
- 8. Hosono N, Sakaura H, Mukai Y, Fujii R, Yoshikawa H. C3-6 laminoplasty takes over C3-7 laminoplasty with significantly lower incidence of axial neck pain. Eur Spine J. 2006;15:1375–1379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sakaura H, Hosono N, Mukai Y, Fujimori T, Iwasaki M, Yoshikawa H. Preservation of muscles attached to the C2 and C7 spinous processes rather than subaxial deep extensors reduces adverse effects after cervical laminoplasty. Spine (Phila Pa 1976). 2010;35:E782–E786. [DOI] [PubMed] [Google Scholar]
- 10. Ohya J, Oshima Y, Oka H, et al. Patient satisfaction with posterior decompression surgery for cervical ossification of the posterior longitudinal ligament: prognostic radiographic factors and patient-reported outcomes for the effectiveness of surgical treatment. World Neurosurg. 2016;96:272–279. [DOI] [PubMed] [Google Scholar]
- 11. Ohya J, Oshima Y, Takeshita K, et al. Patient satisfaction with double-door laminoplasty for cervical compression myelopathy. J Orthop Sci. 2015;20:64–70. [DOI] [PubMed] [Google Scholar]
- 12. Neo M, Fujibayashi S, Takemoto M, Nakamura T. Clinical results of and patient satisfaction with cervical laminoplasty for considerable cord compression with only slight myelopathy. Eur Spine J. 2012;21:340–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Duetzmann S, Cole T, Ratliff JK. Cervical laminoplasty developments and trends, 2003-2013: a systematic review. J Neurosurg Spine. 2015;23:24–34. [DOI] [PubMed] [Google Scholar]
- 14. Kim JY, Kwag KI. Clinical effects of deep cervical flexor muscle activation in patients with chronic neck pain. J Phys Ther Sci. 2016;28:269–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Riew KD, Raich AL, Dettori JR, Heller JG. Neck pain following cervical laminoplasty: does preservation of the C2 muscle attachments and/or C7 matter? Evid Based Spine Care J. 2013;4:42–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Jensen MP, Chen C, Brugger AM. Interpretation of visual analog scale ratings and change scores: a reanalysis of two clinical trials of postoperative pain. J Pain. 2003;4:407–414. [DOI] [PubMed] [Google Scholar]
- 17. Rao SC, Fehlings MG. The optimal radiologic method for assessing spinal canal compromise and cord compression in patients with cervical spinal cord injury. Part I: an evidence-based analysis of the published literature. Spine (Phila Pa 1976). 1999;24:598–604. [DOI] [PubMed] [Google Scholar]
- 18. Carragee EJ, Hurwitz EL, Cheng I, et al. ; Bone and Joint Decade 2000-2010 Task Force on Neck Pain and its Associated Disorders. Treatment of neck pain: injections and surgical interventions: results of the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and its Associated Disorders. Spine (Phila Pa 1976). 2008;33(4 suppl):S153–S169. [DOI] [PubMed] [Google Scholar]
- 19. Slipman CW, Plastaras C, Patel R, et al. Provocative cervical discography symptom mapping. Spine J. 2005;5:381–388. [DOI] [PubMed] [Google Scholar]
- 20. Malik KM, Cohen SP, Walega DR, Benzon HT. Diagnostic criteria and treatment of discogenic pain: a systematic review of recent clinical literature. Spine J. 2013;13:1675–1689. [DOI] [PubMed] [Google Scholar]
- 21. Falco FJ, Erhart S, Wargo BW, et al. Systematic review of diagnostic utility and therapeutic effectiveness of cervical facet joint interventions. Pain Physician. 2009;12:323–344. [PubMed] [Google Scholar]
- 22. Falco FJ, Manchikanti L, Datta S, et al. Systematic review of the therapeutic effectiveness of cervical facet joint interventions: an update. Pain Physician. 2012;15:E839–E868. [PubMed] [Google Scholar]
- 23. Iqbal ZA, Rajan R, Khan SA, Alghadir AH. Effect of deep cervical flexor muscles training using pressure biofeedback on pain and disability of school teachers with neck pain. J Phys Ther Sci. 2013;25:657–661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Gupta BD, Aggarwal S, Gupta B, Gupta M, Gupta N. Effect of deep cervical flexor training vs conventional isometric training on forward head posture, pain, Neck Disability Index in dentists suffering from chronic neck pain. J Clin Diagn Res. 2013;7:2261–2264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Tanaka Y, Kokubun S, Sato T, Ozawa H. Cervical roots as origin of pain in the neck or scapular regions. Spine (Phila Pa 1976). 2006;31:E568–E573. [DOI] [PubMed] [Google Scholar]
- 26. Geneen LJ, Moore RA, Clarke C, Martin D, Colvin LA, Smith BH. Physical activity and exercise for chronic pain in adults: an overview of Cochrane Reviews. Cochrane Database Syst Rev. 2017;(1):CD011279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hogg-Johnson S, van der Velde G, Carroll LJ, et al. ; Bone and Joint Decade 2000-2010 Task Force on Neck Pain and its Associated Disorders. The burden and determinants of neck pain in the general population: results of the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and its Associated Disorders. Spine (Phila Pa 1976). 2008;33(4 suppl):S39–S51. [DOI] [PubMed] [Google Scholar]
- 28. Oka H, Matsudaira K, Fujii T, et al. Risk factors for prolonged treatment of whiplash-associated disorders. PLoS One. 2015;10:e0132191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–370. [DOI] [PubMed] [Google Scholar]
- 30. Fujibayashi S, Neo M, Yoshida M, Miyata M, Takemoto M, Nakamura T. Neck muscle strength before and after cervical laminoplasty: relation to axial symptoms. J Spinal Disord Tech. 2010;23:197–202. [DOI] [PubMed] [Google Scholar]
- 31. Benglis DM, Guest JD, Wang MY. Clinical feasibility of minimally invasive cervical laminoplasty. Neurosurg Focus. 2008;25:E3. [DOI] [PubMed] [Google Scholar]
- 32. Hosono N, Sakaura H, Mukai Y, Ishii T, Yoshikawa H. En bloc laminoplasty without dissection of paraspinal muscles. J Neurosurg Spine. 2005;3:29–33. [DOI] [PubMed] [Google Scholar]
- 33. Ono A, Tonosaki Y, Yokoyama T, et al. Surgical anatomy of the nuchal muscles in the posterior cervicothoracic junction: significance of the preservation of the C7 spinous process in cervical laminoplasty. Spine (Phila Pa 1976). 2008;33:E349–E354. [DOI] [PubMed] [Google Scholar]
- 34. Oshima Y, Takeshita K, Inanami H, et al. Cervical microendoscopic interlaminar decompression through a midline approach in patients with cervical myelopathy: a technical note. J Neurol Surg A Cent Eur Neurosurg. 2014;75:474–478. [DOI] [PubMed] [Google Scholar]
- 35. Shiraishi T. Skip laminectomy—a new treatment for cervical spondylotic myelopathy, preserving bilateral muscular attachments to the spinous processes: a preliminary report. Spine J. 2002;2:108–115. [DOI] [PubMed] [Google Scholar]
- 36. Shiraishi T, Fukuda K, Yato Y, Nakamura M, Ikegami T. Results of skip laminectomy-minimum 2-year follow-up study compared with open-door laminoplasty. Spine (Phila Pa 1976). 2003;28:2667–2672. [DOI] [PubMed] [Google Scholar]
- 37. Yukawa Y, Kato F, Ito K, et al. Laminoplasty and skip laminectomy for cervical compressive myelopathy: range of motion, postoperative neck pain, and surgical outcomes in a randomized prospective study. Spine (Phila Pa 1976). 2007;32:1980–1985. [DOI] [PubMed] [Google Scholar]


