Abstract
Background
Perception of chronic illness and a positive outlook improve recovery, and yoga can improve wellbeing. This study aimed to compare perception, mental wellbeing, and quality of life in yoga-experienced compared with yoga-naïve patients with chronic illness and to determine whether the duration of yoga practice in the yoga-experienced group had any correlation with the perception of illness, mental wellbeing, and quality of life.
Material/Methods
A cross-sectional comparative study recruited 419 patients with chronic non-communicable disease. Yoga-experienced patients (n=150) (mean age, 41.9±13.6 years) and yoga-naïve patients (n=269) (mean age, 41.2±12.6 years) were assessed for the perception of their illness, mental wellbeing, and quality of life using the Warwick-Edinburgh mental wellbeing scale (WEMWBS) and the World Health Organization quality of life (WHOQOL-BREF) self-reporting questionnaire.
Results
The yoga-experienced group had significantly increased mental wellbeing, personal control as a dimension of their perception of illness, and psychological and environmental quality of life compared with the yoga-naïve group (all, p<0.05), when comparisons were made using the Mann-Whitney U test. The duration of yoga practised in months was positively-correlated with mental wellbeing and different aspects of quality of life. There was a negative correlation with the perception of illness suggesting that the illness was perceived to be less severe (all, p<0.05) when correlations were made using Spearman’s rank correlation coefficient.
Conclusions
In patients with chronic illness, yoga improved mental wellbeing, aspects of quality of life, and resulted in a positive perception of illness.
MeSH Keywords: Chronic Disease, Cross-Sectional Studies, Perception, Quality of Life, Yoga
Background
The perception of chronic illness by patients has several consequences that can affect wellbeing and quality of life [1]. In chronically ill patients, perception of illness influences self-management behaviors and quality of life, and patients who have a negative perception of their illness also have impaired health [2]. A negative perception of illness, especially negative emotional reactions, perceived consequences, concerns about the illness, and identifying strongly with the illness are significantly associated with high levels of emotional distress, an impaired response to the consequences of illness and low quality of life [2]. A negative perception of illness impacts negatively on quality of life and wellbeing for patients and a positive perception of chronic illness can improve quality of life and wellbeing [2].
Subjective wellbeing and positive emotions are associated with improved immune function and immune defense to common infections [3]. Therefore, a sense of wellbeing is important in disease prevention, and subjective mental wellbeing also favorably influences overall health and recovery from an illness [4]. Mental wellbeing is associated with positive health behaviors such as a healthy diet, engaging in physical activity, and a lower incidence of smoking [5,6]. People with good health generally have a sense of wellbeing. However, the findings from a previously published study reported that 38% of individuals with poor health had high levels of wellbeing, whereas 18% of individuals with good health had low levels of wellbeing [7]. In a dissertation from Ohio State University [8], correlation analysis showed that patient perception of illness was associated with differences in their mental wellbeing and quality of life. Quality of life is often defined ambiguously but may be defined in terms of the subjective and objective domains involved [9].
In 2003, Pollard and Lee [10] described wellbeing as complex and multifaceted, and hence difficult to define. While the quality of life and wellbeing are often used interchangeably, they are not the same [11]. Subjective wellbeing is mainly concerned with the respondent’s internal judgments of wellbeing, whereas the quality of life is assessed based on subjective wellbeing as well as social indicators of the quality of life. Therefore, quality of life indicates how illness impacts most aspects of a patient’s life. Mental wellbeing indicates how a patient feels when all factors are considered.
In 2014, Henriques, Kleinman, and Asselin provided a comprehensive definition of wellbeing as, ‘happiness with the worthiness to be happy’ [12]. This definition was based on a detailed review of previous theories and the presentation of a nested model for wellbeing, which has four domains [12]. These domains include firstly, the subjective domain or the phenomenological experience of happiness, or misery as an inverted view, and satisfaction, or the possible inverted view, dissatisfaction [12]. Second, the biological and psychological aspects of health and functioning [12]. The third domain is the material and social environment [12]. The fourth domain consists of values and ideology, which include ethics, morals and the individual’s world view [12]. An inverted view of the nested model can provide insights about how a change in any of the four domains, subjective experience, health, environment, and values/ideology from what is generally considered to be positive to negative could correspondingly influence health, and if continued, could lead to maladaptation and disease.
Yoga is a mind-body practice that positively impacts health [13]. A systematic review of ten randomized controlled trials compared the effectiveness of yoga with conventional care for patients with chronic illnesses including heart disease, stroke and chronic obstructive pulmonary disease (COPD) [14]. The quality of life was assessed using the Cochrane risk of bias tool and included 431 people, with a mean age of 56±8 years. Compared with conventional care, yoga significantly improved health-related quality of life and exercise capacity [14]. Apart from the studies of quality of life in patients, mental wellbeing was found to improve wellbeing in 118 healthy primary school teachers after fifteen days of an intensive residential yoga [15].
Currently, there have been few studies that have evaluated the quality of life and mental wellbeing concerning the perception of illness in patients with chronic illness that have compared patients who have experience of yoga with those who are naïve to yoga. Therefore, this study aimed to compare illness perception, mental wellbeing, and quality of life in yoga-experienced compared with yoga-naïve patients with chronic illness. This study also sought to determine whether the duration of yoga in the yoga-experienced group had any correlation with the perception of illness, mental wellbeing, and quality of life.
Material and Methods
Design of the study
This study was approved by the Local Ethics Committee (approval number: PRF/16/0020). Participation in the study was voluntary and there was no patient remuneration for participation in the study. Signed informed consent was obtained from all study participants. The study design was a cross-sectional single assessment with assessments performed using standard appropriate questionnaires. Data were collected for five months, from April 2017 to August 2017.
Study participants
A total of 468 patients with chronic illness aged between 18–74 years (mean age, 41.4±12.9 years) participated in the study. At the time of enrollment in the study all participants filled in a social-demographic data form. This included two questions related to the duration of yoga. The first question was close-ended: ‘Do you practice yoga?’ (yes/no). The second question was open-ended: ‘Since when have you been practicing any form of yoga regularly?’ Based on the responses, 150 participants (mean age, 41.9±13.6 years) were considered as the yoga-experienced group, with at least one month of experience of yoga practice (mean experience, 50.9±73.3 months). In the yoga-naïve group, there were 269 participants (mean age, 41.2±12.6 years) who reported no experience of yoga practice. The participants were patients from the outpatient department in a yoga and Ayurveda hospital located in the north of India.
Inclusion and exclusion criteria
Patients who were diagnosed with chronic non-communicable diseases (NCDs) and those who completed their questionnaires were included in the study. The exclusion criteria were infectious diseases and diseases that could have a fatal outcome during the study, such as malignancy, and 49 participants were excluded for these reasons (Figure 1). With the sample size in the yoga-experienced group (n=92) and the Cohen’s d=0.34, the power was 0.75 for a=0.05 calculated using G*Power software version 3.1 from the difference in the quality of life scores between the two groups [16]. Baseline characteristics of both the yoga-experienced group and the yoga-naïve group are shown in Table 1. Disease classification was based on the International Classification of Diseases, 10th edition (ICD-10) (Table 2) [17].
Figure 1.
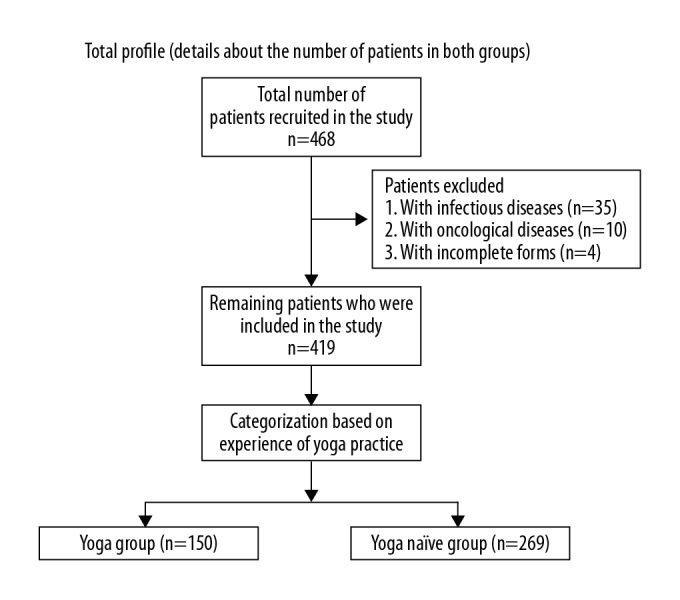
Flowchart of the study design, including details about the number of participants in the yoga-experienced and yoga-naïve patient groups.
Table 1.
Baseline characteristics of the yoga-experienced and yoga-naïve groups.
| S. No. | Baseline characteristics | Yoga-experienced (n=150) | Yoga-naïve (n=269) | |
|---|---|---|---|---|
| 1 | Average age of the group (mean ±SD) | 41.86±13.57 | 41.16±12.57 | |
| 1.1 | Gender mean ±SD | Male (M) | 41.79±13.59 | 41.16±12.59 |
| Female (F) | 41.79±13.59 | 41.13±12.54 | ||
| 2 | Gender | |||
| 2.1 | M: F (n) | 90: 60 | 155: 114 | |
| 2.2 | M: F (%) | 60.0: 40.0 | 57.6: 42.4 | |
| 3 | Education, n (%) | |||
| 3.1 | <10 years | 27 (18.0) | 52 (19.3) | |
| 3.2 | 10 years | 9 (6.0) | 26 (9.7) | |
| 3.3 | >10 years | 114 (76.0) | 191 (71.0) | |
| 4 | Socioeconomic (level based on income per month in INR), n (%) | |||
| 4.1 | 5000 to 16000 | 50 (33.3) | 109 (40.5) | |
| 4.2 | 17000 to 40000 | 42 (28.0) | 56 (20.8) | |
| 4.3 | 41000 to 85000 | 22 (14.7) | 30 (11.2) | |
| 4.4 | 85000 and above | 13 (8.7) | 11 (4.1) | |
| 4.5 | No details | 23 (15.3) | 63 (23.4) | |
| 5 | Occupation, n (%) | |||
| 5.1 | Business | 26 (17.3) | 50 (18.6) | |
| 5.2 | Agriculture | 13 (8.7) | 30 (11.2) | |
| 5.3 | House holder | 56 (37.3) | 118 (43.9) | |
| 5.4 | Professionals | 55 (36.7) | 71 (26.4) | |
| 6 | Marital status, n (%) | |||
| 6.1 | Married | 117 (78.0) | 219 (81.4) | |
| 6.2 | Unmarried | 30 (20.0) | 40 (14.9) | |
| 6.3 | Widow/widower | 2 (1.3) | 9 (3.3) | |
| 6.4 | Separated/divorced | 1 (0.7) | 1 (0.4) | |
| 7 | Use of intoxicants/stimulants, n (%) | |||
| 7.1 | Alcohol | |||
| 7.1.1 | Yes | 13 (8.7) | 21 (7.8) | |
| 7.1.2 | No | 137 (91.3) | 248 (92.2) | |
| 7.2 | Tobacco | |||
| 7.2.1 | Yes | 16 (10.1) | 25 (9.3) | |
| 7.2.2 | No | 134 (89.3) | 244 (90.7) | |
| 8 | Yoga experience (months) (mean ±SD) | 50.87±73.31 | Not applicable | |
There were no significant differences for all comparisons (p>0.05) using the chi-squared (χ2) test.
Table 2.
Classification of diseases according to the International Classification of Diseases 10th edition (ICD-10) [17] of the yoga-experienced group and yoga-naïve group.
| S. No. | Description of the disease | Disease codes | Yoga-experienced (n=150) | Yoga-naïve (n=269) |
|---|---|---|---|---|
| 1 | Disease of blood and blood forming organs and certain disorders involving the immune mechanism; n (%) | D50-D89 | 1 (0.7) | 3 (1.1) |
| 2 | Endocrine nutritional and metabolic diseases; n (%) | E00-E89 | 16 (10.7) | 28 (10.4) |
| 3 | Mental, behaviour and neurodevelopmental disorder; n (%) | F01-F99 | 4 (2.7) | 3 (1.1) |
| 4 | Disease of the nervous system; n (%) | G00-G99 | 14 (9.3) | 19 (7.1) |
| 5 | Disease of the eye and adnexa; n (%) | H00-H59 | 5 (3.3) | 4 (1.5) |
| 6 | Disease of the ear and mastoid process; n (%) | H60-H95 | 2 (1.3) | 1 (0.4) |
| 7 | Disease of the circulatory system; n (%) | I00-I99 | 5 (3.3) | 12 (4.5) |
| 8 | Disease of the respiratory system; n (%) | J00-J99 | 7 (4.7) | 12 (4.5) |
| 9 | Disease of the digestive system; n (%) | K00-K95 | 25 (16.7) | 33 (12.3) |
| 10 | Disease of the skin and subcutaneous tissue | L00-L99 | 10 (6.7) | 19 (7.1) |
| 11 | Disease of the musculoskeletal system and connective tissue; n (%) | M00-M99 | 34 (22.8) | 77 (28.6) |
| 12 | Disease of the genitourinary system; n (%) | N00-N99 | 14 (9.4) | 28 (10.4) |
| 13 | Symptoms, signs abnormal clinical and laboratory findings, not elsewhere classified; n (%) | R00-R99 | 12 (8.1) | 24 (8.9) |
| 14 | Injury, poisoning and certain others; n (%) | S00-T88 | 1 (0.7) | 6 (2.2) |
The chi-squared (χ2) test showed no significant difference (p>0.05) between the numbers in the yoga-experienced group and the yoga-naïve group in different disease categories.
Assessment of perception of illness
The level of perception of illness (POI), mental wellbeing, and quality of life were assessed using three different questionnaires. Perception of illness was assessed using the brief illness perception questionnaire (BIPQ) which is a nine-item scale designed for rapid assessment of perception of illness (POI) and was particularly helpful in this patient population [18]. The BIPQ questionnaire has been standardized for use in an Indian population and included test-retest reliability (r) ranging from 0.42–0.75, and predictive validity (r) ranging from 0.30–0.43 for an Indian population [18,19]. The BIPQ questionnaire used an 11-point response scale that varies between 0–10 and assessed cognitive POI, emotional POI, comprehension POI, and causal perception of illness. Out of a total of nine items, five of the items assessed patients’ cognitive perception of illness, including consequences (item 1), timeline (item 2), personal control (item 3), treatment control (item 4), and identity (item 5). Two of the items assessed the emotional perception of illness and included concern (item 6) and emotions (item 8). One item assessed comprehension about the illness (item 7). Assessment of the perceived causes was based on an open-ended response question, which asked patients to list the three most important causes of their illness (item 9).
Assessment of perception of mental wellbeing
Mental wellbeing was evaluated using the Warwick-Edinburgh mental wellbeing scale (WEMWBS) [20]. This scale showed Cronbach’s α score of 0.89, test-retest reliability of 0.83, criterion validity of 0.43–0.77, and construct validity of 0.87–0.91 [20]. The WEMWBS has been validated in Asian populations from China and Pakistan, with an internal consistency of 0.88–0.94, test-retest validity of 0.86–0.95, and construct validity of 0.64 [21,22]. While China and Pakistan are culturally different from India, there are many sociocultural aspects that influence mental wellbeing that are similar. The WEMWBS has been previously used in Indian populations [15,23]. The WEMWBS is a fourteen-item scale that asks people to describe their experience of feelings and thoughts over the last two weeks with five possible options as their response: 1, never; 2, rarely; 3, sometimes; 4, often; and 5, very often.
Assessment of quality of life
Quality of life (QoL) was assessed using the WHO quality of life BREF (WHOQOL-BREF), which is a useful tool to assess the changes during the course of treatment of an individual [24]. This scale has previously been standardized for use in an Indian population earlier and has shown internal consistency (Cronbach’s α=0.87), content validity (0.50–0.77), and predictive validity (0.44–0.63) [25,26]. WHOQOL-BREF consists of 26 items with five possible responses, including: 1, not at all; 2, not much; 3, moderately; 4, a great deal; and 5, completely. Out of the 26-items, question 1 assessed prediction about the overall perception of quality of life, question 2 was used to assess the overall perception of health, and the remaining 24 questions assess four domains on quality of life, physical, psychological, social and environmental.
The initial aim of the study was to assess the perception of illness in relation to mental wellbeing, with a possible provision to add a quality of life questionnaire at a further stage if participants were willing. The WHOQOL-BREF self-reporting questionnaire was used when it was clear that participants had time to answer the questionnaire fully. Therefore, WHOQOL-BREF responses were not obtained from all participants. The results presented of QoL were for the yoga-experienced group (n=92) and the yoga-naïve group (n=178) (Figure 1).
Data extraction
All questionnaires were anonymously scored by an evaluator who was unaware of the patients’ diagnosis and their group allocation to the yoga-experienced group or the yoga-naïve group. The group mean ± standard deviation (SD) scores were calculated. For perception of illness, each item of the scale was given a weighted score of 0–10. A standard method was used to score the data [18]. The overall score represents the degree to which the illness is perceived as threatening. A higher score indicated that the patient viewed their illness as particularly severe. For mental wellbeing, each item of the scale was given a weighted score of 1–5, and a standard method was used to score the data [20]. Higher scores are positively correlated with a higher level of mental wellbeing. For the quality of life, each item was scored between 1–5. Questions 3, 4, and 26 were reverse-scored and the remaining questions were scored directly, with a higher score indicating a higher QoL. The mean scores of items within each domain were used to calculate the domain scores in the four domains, physical, psychological, social, and environmental, which indicated an individual’s perception of their QoL in each domain, respectively, with higher scores indicating a higher quality of life [24].
Statistical analysis
Data were analyzed using SPSS version 24.0. Three types of analysis were performed for background and patient demographics, comparisons between yoga-experienced and yoga-naïve groups, and correlation analysis. At baseline, the data included scores for mental wellbeing, quality of life, and perception of illness, which were tested for a normal distribution using the Shapiro-Wilk test. In all cases, the data were not normally distributed, the data were analyzed for equal or comparable variance using Levene’s test for equality of variance. There was inequality of variance of the data between the yoga-experienced and yoga-naïve groups, and the chi-squared (χ2) test was used to compare the sociodemographic characteristics and different categories of diseases based on the ICD-10 categories. A Mann-Whitney U test was performed to compare mental wellbeing, dimensions of perception of illness, and quality of life between the yoga-experienced and the yoga-naïve groups. Spearman’s rank correlation coefficient was used to determine the correlation between yoga experience in months with mental wellbeing, dimensions of perception of illness, and quality of life in the yoga-experienced group. For all comparisons and statistical analysis, the α-value was pre-set as 0.05.
Results
Background patient demographics
The yoga-experienced group (n=150) and the yoga-naïve group (n=269) showed no significant differences in the following variables at baseline: gender, number of years of education, and socioeconomic level, based on a standard categorization [27], occupation, marital status, consumption of alcohol, and consumption of nicotine in any form, with the chi-squared (χ2) test result of p>0.05 in all cases. The details of the baseline characteristics of both groups are shown in Table 1. The participants were also categorized at baseline using the International Classification of Diseases, 10th edition (ICD-10) [17]. The number of patients in the yoga-experienced and yoga-naïve groups in the 14 categories of disease showed no significant difference, with the chi-squared (χ2) test result being p>0.05 in all cases.
Comparisons between yoga-experienced and yoga-naïve groups
The yoga-experienced group (n=150) had significantly higher scores compared with the yoga-naïve group (n=269) in mental wellbeing (Mann–Whitney U test; p<0.05). The yoga-experienced group (n=92) and yoga-naïve group (n=178) differed significantly in the three dimensions of quality of life, based on the World Health Organization quality of life (WHOQOL-BREF) self-reporting questionnaire. The yoga-experienced group had a significantly better psychological quality of life (p<0.05), environmental quality of life (p<0.05), and total quality of life (p<0.05; one-tailed level). In the perception of illness questionnaire, there was one significant difference between the yoga-experienced group and the yoga-naïve group (n=269), which was in personal control which was significantly better in the yoga-experienced group (p<0.05; one-tailed) (Table 3). In all the comparisons described above the levels of significance were low and Cohen’s d-values were small, which was a limitation in the interpretation of the findings.
Table 3.
Comparison between the yoga-experienced and yoga-naïve patients for mental wellbeing, perception of illness, and quality of life using Mann-Whitney U test.
| S. No, | Variables | Yoga-experienced (n=150) | Yoga-naïve (n=269) | z-Value | p-Value |
|---|---|---|---|---|---|
| 1 | Mental wellbeing | 49.99±11.65 | 47.54±11.63* | 1.99 | 0.05 |
| 2 | Brief perception of illness | 43.59±11.49 | 45.03±11.28 | 1.26 | 0.21 |
| 2.1 | Consequences | 6.99±2.56 | 7.00±2.86 | 0.53 | 0.59 |
| 2.2 | Timeline | 5.53±2.82 | 5.86±3.08 | 1.28 | 0.20 |
| 2.3 | Personal control | 4.51±2.52 | 5.03±2.80# | 1.87 | 0.06 |
| 2.4 | Treatment control | 3.47±2.55 | 3.68±2.82 | 0.54 | 0.59 |
| 2.5 | Identity | 6.42±2.43 | 6.15±2.65 | 1.13 | 0.26 |
| 2.6 | Concern | 7.37±2.99 | 7.74±2.85 | 1.52 | 0.13 |
| 2.7 | Coherence | 2.39±2.48 | 2.73±2.76 | 0.99 | 0.32 |
| 2.8 | Emotional representation | 6.92±2.84 | 6.85±3.02 | 0.04 | 0.97 |
| 2.9 | Cognitive | 26.91±7.59 | 27.71±7.88 | 1.19 | 0.24 |
| 3 | Emotional | 14.29±5.23 | 14.59±5.22 | 0.75 | 0.45 |
| 4 | WHOQOL-BREF | Yoga-experienced (n=92) | Yoga-naïve (n=178) | ||
| 4.1 | Overall perception of quality of life | 3.33±1.04 | 3.27±1.02 | 0.33 | 0.74 |
| 4.2 | Overall perception of their health | 2.99±2.20 | 2.75±1.05 | 0.37 | 0.62 |
| 4.3 | Physical health | 21.97±5.17 | 21.92±4.76 | 0.35 | 0.81 |
| 4.4 | Psychological | 19.09±5.08 | 17.77±4.47* | 2.11 | 0.05 |
| 4.5 | Social relationship | 10.55±3.00 | 10.19±2.76 | 1.06 | 0.24 |
| 4.6 | Environmental | 26.27±6.10 | 24.27±5.81* | 2.43 | 0.02 |
| 4.7 | Total quality of life | 84.20±17.13 | 80.16±16.02# | 1.89 | 0.07 |
p<0.05 at two tailed level,
p<0.05 at one tailed level, level of significance between the groups; Mann-Whitney U test for non-parametric data.
WHOQOL-BREF – the World Health Organization quality of life self-reporting questionnaire.
Correlations
The yoga-experienced group (n=150) showed a positive correlation between the duration of yoga experience in months and the mental wellbeing scores (rs=0.214; p<0.01). The quality of life was positively correlated with the duration of yoga experience for the three dimensions of quality of life (n=92), psychological (rs=0.91; p<0.05; one-tailed), environmental (rs=0.206; p<0.05), and total quality of life (rs=0.79; p<0.05; one-tailed). The perception of illness was negatively correlated with duration of yoga experience in months (n=150) for five aspects that included, overall perception of illness (rs=0.241; p<0.01), consequences (rs=0.201; p<0.05), timeline (rs=0.206; p<0.05), level of concern (rs=0.168; p<0.05), and cognitive perception (rs=0.248; p<0.01) (Table 4).
Table 4.
Correlation of mental wellbeing, quality of life, and perception of illness with experience of yoga practice in months in the yoga-experienced group.
| S. No. | Variables | Yoga experience | |
|---|---|---|---|
| rs-Value | p-Value | ||
| 1 | Mental wellbeing | 0.21** | 0.01 |
| 2 | Brief perception of illness | −0.24** | <0.01 |
| 2.1 | Consequences | −0.20* | 0.01 |
| 2.2 | Timeline | −0.21* | 0.01 |
| 2.3 | Personal control | −0.12 | 0.16 |
| 2.4 | Treatment control | −0.11 | 0.17 |
| 2.5 | Identity | −0.05 | 0.54 |
| 2.6 | Concerned | −0.17* | 0.04 |
| 2.7 | Coherence | −0.08 | 0.32 |
| 2.8 | Emotional representation | −0.03 | 0.73 |
| 2.9 | Cognitive | −0.25** | <0.01 |
| 3 | Emotional | −0.12 | 0.13 |
| 4 | WHOQOL-BREF | ||
| 4.1 | Overall perception of quality of life | 0.15 | 0.15 |
| 4.2 | Overall perception of their health | 0.01 | 0.91 |
| 4.3 | Physical health | 0.14 | 0.19 |
| 4.4 | Psychological | 0.19# | 0.07 |
| 4.5 | Social relationship | 0.01 | 0.99 |
| 4.6 | Environmental | 0.21* | 0.04 |
| 4.7 | Total quality of life | 0.79# | 0.07 |
p<0.05 at two tailed level;
p<0.01 at two tailed level;
p<0.05 at one tailed level; level of significance based on Spearman’s rank correlation coefficient.
WHOQOL-BREF – the World Health Organization quality of life self-reporting questionnaire.
Discussion
The findings of this study showed that patients with chronic illness who practiced yoga had significantly increased self-reported scores for total mental wellbeing and psychological and environmental aspects of the quality of life when compared with patients who were naïve to yoga. The patients in the present study all had chronic illnesses which were non-communicable and not expected to be fatal.
Yoga influences the mental state in different ways. Yoga has an effect on voluntary breath regulation, or pranayama, which is an important part of the practice of yoga [28]. Breathing in an involuntary activity but it can be controlled voluntarily and bridges volition and those functions considered to be chiefly involuntary. In the text of the Hatha Yoga Pradipika from around 300 A.D., in chapter II, verse 2.a the yoga text states that, ‘through steadying the breath, control over the mind is achieved’ [29].
There are several pranayama practices including those in which the breathing becomes slow and the depth of breathing increases [30]. One way in which breath regulation might result in physiological changes is through the close association between breathing and the vagus nerve. While the role of the vagus nerve in cardiac sinus arrhythmia and the stress response are well known, there are other more complex effects of vagal activity that influence the psycho-physiological regulation of physical and mental health. The neurovisceral integration model has been proposed to improve understanding in the integration of the brain-body integration and emphasizes the role of the vagus in adapting to the environment [31]. The polyvagal theory [32] describes a neural circuit which regulates behavioral flexibility in response to environmental changes as well as social bonding.
Both the neurovisceral integration model and the polyvagal theory might influence mental wellbeing. A further model, the Genomics Environmental vagus Nerve social Interaction Allostatic regulation Longevity (GENIAL) model considers the vagus nerve as a method to regulate multisystem pathways that can influence psychological factors, social ties, and regulate physiological or behavioral change [33]. Therefore, increased levels of overall mental wellbeing, psychological wellbeing, and environmental wellbeing in patients who practiced yoga compared with patients who were naïve to yoga, may be explained by the activation of the vagal nerve and associated with yoga modulated breathing. Modulation of breathing as slow, deep, and regular is a part of all yoga practices such as yoga postures and yoga meditation and is not restricted to yoga breathing techniques or pranayamas.
A hypothetical association between the practice of yoga and the benefits obtained has been provided in a literature review which focused on a school-based yoga intervention [34]. Yoga practice, which included yoga postures, breathing techniques, relaxation, and meditation were believed to impact mind-body awareness, self-regulation, and physical fitness, with all three factors being interconnected [34]. These three factors were considered as responsible for the positive effects of yoga on behavior, the mental state, physical health, cognitive performance, relationships and the quality of life [34].
In the present study, the findings showed that the perception of illness significantly varied in the single dimension of personal control between patients who practiced yoga versus those who were yoga-naïve, although the degree of significance was weak (p<0.05, one-tailed). This finding might be explained by the validity of the brief illness perception questionnaire (BIPQ) for personal control and its association with self-sufficiency [17,35]. One of the aims of the practice of yoga is to empower a person to be self-sufficient and functionally effective [13]. In a previously published study that included patients with diabetes, blood sugar control was positively associated with personal control [35]. These findings support that when a patient has better personal control of their illness, their ability to manage their chronic illness independently can be improved. Also, the practice of yoga has been shown to improve awareness [36] and interoception or the sense of the internal state of the body [37], which could increase the feeling of being personally involved in the healing process and hence feeling a sense of control. In the Yoga Sutras of Patanjali, chapter II, verse 9, the practice of yoga is supposed to reduce fear, including the fear of death, or abhinivesha [38]. However, in the present study, there was no attempt to measure interoception, fear, or feelings of empowerment, which mean that their role can only be speculated.
In 2008, Deci and Ryan developed a theory to explain the factors that motivate people to grow and achieve fulfillment, which is also relevant to feelings of personal control [39]. Special emphasis was placed on intrinsic motivation, or internal sources of motivation, such as competence, connection or feeling related to other people, and a sense of autonomy or being in control of their own goals [39]. Intrinsic motivation and self-determination are considered to be comparable in the continuum of self-motivation, as people who have high levels of self-determination and have the belief that their behaviors can influence outcomes which are important to their life [39]. Such people are usually highly self-motivated and are good at setting goals and working with a sense of purpose, and their behaviors are directed towards realizing their goals and attempting to achieve the outcome they desire [39].
The perception of illness also could influence the choice of medical care. In a previously reported study conducted in Mexico [40], patients were considered to have three options for treatment, including conventional treatment from physicians, surgeons, and paramedical professionals, self-care that included treatment by close relatives and people associated with the patients, and lay-care that included contacting traditional healers, and other alternative treatments [40]. The findings showed that if patients perceived their illness as threatening or severe, they would contact conventional practitioners, depending on factors such as their economic status and access to conventional health providers [40]. In the present study, both the yoga-experienced group and the yoga-naïve group of patients were seeking treatment at an outpatient department of a yoga and Ayurveda hospital. The two groups did not differ in their socioeconomic status or level of education. Therefore, it may be assumed that the selection of treatment was an informed choice. However, it would be important to have further details about why the patients selected this treatment, and if this was their first choice or if they had already consulted a physician for traditional treatment.
Mental wellbeing, social interaction, and the way in which a person responds to their environment are also influenced by other physiological changes that impact brain function. Oxytocin is a nine amino acid peptide secreted by the hypothalamus, which can positively impact socio-emotional cues facilitating interpersonal trust and positive social interaction [41]. A previously published study demonstrated that the practice of yoga for one month increased plasma oxytocin levels by 7.2 pg/ml, whereas a control group showed no significant change [42]. The effects of the vagus and neurochemical changes are two examples of psychophysiological changes that could explain the benefits seen in patients who practiced yoga. However, in the absence of quantitative methods of evaluation, these psychophysiological effects require further study.
In this study, correlations for the yoga-experienced group were performed between the duration of experience of yoga in months and the dimensions of mental wellbeing, quality of life, and perception of illness. There was a significant positive correlation between the duration of the practice of yoga and mental wellbeing, perception of quality of life, psychological aspects of quality of life, quality of life related to the environment, and total quality of life. There may be many ways in which the practice of yoga may positively influence mental wellbeing, especially in relation to the environment and the ways a person perceives their quality of life.
Mental wellbeing includes hedonic and eudemonic aspects of wellbeing [43]. The hedonic aspects include happiness and subjective wellbeing, while positive functioning is a eudemonic aspect. The mental wellbeing scale used in this study assessed both aspects of mental wellbeing. The hedonic elements include happiness, joy, and contentment. In yoga, contentment is a necessary prerequisite to practice yoga postures (asanas), yoga breathing (pranayama) and meditation, or santosha [28]. It has been traditionally described that through the practice of yoga, a person reaches the state of physical and mental balance or homeostasis, which leads to perfect bliss or ananda [44]. These examples from traditional texts can be correlated with scientific findings based on contemporary research [45,46]. The eudemonic elements of wellbeing are psychological functioning, autonomy, a sense of purpose in life, and a positive relationship with others, and yoga increases the sense of self-sufficiency and independence. The practice of yoga also increases emotional resilience [47] and self-esteem [48], which could contribute to increased feelings of autonomy.
In the present study, the duration of the practice of yoga was negatively correlated with the way the patients perceived their illness, the consequences of the illness, and the timeline or course. As described above, yoga enhances positive feelings and increases self-sufficiency, which could possibly give patients a more positive view of their illness. Also, yoga is known to reduce anxiety [49]. Anxiety in patients who are chronically ill is often related to the way they perceive the outcome or consequences of being ill, as well as the timeline or course of the illness. It is possible that the positive mental attitude and reduced anxiety levels due to yoga helped patients with chronic illness to perceive their outcome and course of the illness as less threatening.
Worldwide, the burden of chronic non-communicable illnesses continues to increase, due to an increasing proportion of elderly patients and unhealthy lifestyles [50]. The findings of the present study showed that patients with chronic illness who practiced yoga had a more positive mental state with better mental wellbeing and a greater sense of being in control of their illness when compared with yoga-naïve patients. Also, mental wellbeing, quality of life, and a positive perception of their illness were significantly greater in yoga-experienced patients who had a long experience of yoga.
This study had several limitations. In some cases, there were inadequate details about the type of yoga, such as the yoga school, the name of the specific yoga practices, and the intensity and the frequency of yoga. Also, this study relied entirely on questionnaires without other forms of assessment to understand the underlying mechanisms of the effects. The levels of significance in all cases were low (p<0.05) and Cohen’s d values were small. Despite these limitations, the results suggest that yoga is a useful intervention in patients with non-communicable chronic illness, and can improve mental state, the way patients perceive their illness, and their overall quality of life.
Conclusions
A cross-sectional study compared yoga-experienced and yoga-naïve patients with chronic illness in terms of mental wellbeing, quality of life, and perception of their illness. Both groups included patients attending a yoga and Ayurveda outpatient department for treatment of chronic non-communicable illnesses without fatal outcome. The yoga-experienced group had significantly better mental wellbeing, psychological quality of life, environmental quality of life and total quality of life when compared with the yoga-naïve group. In their perception of illness, the yoga-experienced group had better personal control than the yoga-naïve patients suggesting that they felt more in control of their illness. The levels of mental wellbeing, aspects of quality of life and dimensions of perception of illness were significantly correlated with the duration of yoga in months suggesting that a longer duration of yoga experience improved mental wellbeing, quality of life and the way persons perceive their illness. The way in which an illness is perceived can impact the outcome in several ways. In patients who perceive their illness as severe and that they have little control over the illness this would negatively influence their recovery. However, patients who are optimistic about their illness might have a better chance of improvement. Illness perception can also influence patient choice of medical care, as patients who perceive their illness as life-threatening may be more likely to seek conventional medical care, whereas those who perceive their illness as chronic may choose complementary and alternative methods of treatment. Therefore, the findings of this study suggest the importance of evaluating mental wellbeing, overall quality of life, and the way illness is perceived, in patients with chronic non-communicable diseases.
Footnotes
Source of support: Patanjali Research Foundation (Trust), Haridwar, India
Conflict of interest
None.
References
- 1.Petrie KJ, Jago LA, Devcich DA. The role of illness perceptions in patients with medical conditions. Curr Opin Psychiatry. 2007;20:163–67. doi: 10.1097/YCO.0b013e328014a871. [DOI] [PubMed] [Google Scholar]
- 2.Wu H, Zhao X, Fritzsche K, et al. Negative illness perceptions associated with low mental and physical health status in general hospital outpatients in China. Psychol Health Med. 2014;19:273–85. doi: 10.1080/13548506.2013.802358. [DOI] [PubMed] [Google Scholar]
- 3.Cohen S, Doyle WJ, Turner RB, et al. Emotional style and susceptibility to the common cold. Psychosom Med. 2003;65:652–57. doi: 10.1097/01.psy.0000077508.57784.da. [DOI] [PubMed] [Google Scholar]
- 4.De Neve JE, Diener E, Tay L, Xuereb C. The objective benefits of subjective wellbeing. In: Helliwell J, Layard R, Sachs J, editors. World Happiness Report 2013. New York: UN Sustainable Development Solutions Network; 2013. [Google Scholar]
- 5.Department of Health (DoH) UK. Why it matters to health policy. Health is the top thing people say matters to their wellbeing. DoH UK; 2014. Wellbeing. Available from [URL]: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/277566/Narrative__January_2014_.pdf. [Google Scholar]
- 6.Chanfreau J, Lloyd C, Byron C, et al. Predicting wellbeing. NatCen Social Research that works for society. 2013. Available from [URL]: https://www.natcen.ac.uk/media/205352/predictors-of-wellbeing.pdf.
- 7.Beaumont J, Thomas J. Office for National Statistics (ONS) Measuring National Well-being. Oct 1, 2015. Available from [URL]: https://www.ons.gov.uk/peoplepopulationandcommunity/wellbeing/articles/measuringnationalwellbeing/2015-10-01.
- 8.Long RN. Doctoral dissertation. The Ohio State University US; 2013. Illness perceptions, quality of life, and psychological functioning in patients with chronic obstructive pulmonary disease and their caregivers. Available from [URL]: https://etd.ohiolink.edu/!etd.send_file?accession=osu1384728914&disposition=inline. [Google Scholar]
- 9.Farquhar M. Definitions of quality of life: A taxonomy. J Adv Nurs. 1995;22:502–9. doi: 10.1046/j.1365-2648.1995.22030502.x. [DOI] [PubMed] [Google Scholar]
- 10.Pollard EL, Lee PD. Child wellbeing: A systematic review of the literature. Soc Indic Res. 2003;61:59–78. [Google Scholar]
- 11.Christoph B, Noll HH. Subjective wellbeing in the European Union during the 90’s. Soc Indic Res. 2003;64:521–46. [Google Scholar]
- 12.Henriques G, Kleinman K, Asselin C. The nested model of well-being: A unified approach. Rev Gen Psychol. 2014;18:7–18. [Google Scholar]
- 13.Woodyard C. Exploring the therapeutic effects of yoga and its ability to increase quality of life. Int J Yoga. 2011;4:49–54. doi: 10.4103/0973-6131.85485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Desveaux L, Lee A, Goldstein R, Brooks D. Yoga in the management of chronic disease: A systematic review and meta-analysis. Med Care. 2015;53:653–61. doi: 10.1097/MLR.0000000000000372. [DOI] [PubMed] [Google Scholar]
- 15.Telles S, Gupta RK, Bhardwaj AK, et al. Increased mental wellbeing and reduced state anxiety in teachers after participation in a residential yoga program. Med Sci Monit Basic Res. 2018;24:105–12. doi: 10.12659/MSMBR.909200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Erdfelder E, Faul F, Buchner A. GPOWER: A general power analysis program. Behav Res Methods Instrum Comput. 1996;28:1–11. [Google Scholar]
- 17.WHO ICD-10 Version. 2016. Available from [URL]: https://icd.who.int/browse10/2016/en.
- 18.Broadbent E, Petrie KJ, Main J, Weinman J. The brief illness perception questionnaire. J Psychosom Res. 2006;60:631–37. doi: 10.1016/j.jpsychores.2005.10.020. [DOI] [PubMed] [Google Scholar]
- 19.Basu S, Poole J. The brief illness perception questionnaire. Occup Med. 2016;66:419–20. doi: 10.1093/occmed/kqv203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tennant R, Hiller L, Fishwick R, et al. The Warwick-Edinburgh mental wellbeing scale (WEMWBS): Development and UK validation. Health Qual Life Outcomes. 2007;5:63–76. doi: 10.1186/1477-7525-5-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Waqas A, Ahmad W, Haddad M, et al. Measuring the well-being of health care professionals in the Punjab: A psychometric evaluation of the Warwick-Edinburgh mental wellbeing scale in a Pakistani population. Peer J. 2015;3:e1264. doi: 10.7717/peerj.1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Taggart F, Friede T, Weich S, et al. Cross cultural evaluation of the Warwick-Edinburgh mental well-being scale (WEMWBS) – a mixed methods study. Health Qual Life Outcomes. 2013;11:27. doi: 10.1186/1477-7525-11-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vaingankar JA, Abdin E, Chong SA, et al. Psychometric properties of the short Warwick-Edinburgh mental well-being scale (SWEMWBS) in service users with schizophrenia, depression and anxiety spectrum disorders. Health Qual Life Outcomes. 2017;15:153. doi: 10.1186/s12955-017-0728-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.World Health Organization. The World Health Organization Quality of Life (WHOQOL)-BREF. 2004. Available from [URL]: https://www.who.int/substance_abuse/research_tools/en/english_whoqol.pdf.
- 25.Agnihotri K, Awasthi S, Chandra H, et al. Validation of WHO QOL-BREF instrument in Indian adolescents. Indian J Pediatr. 2010;77:381–86. doi: 10.1007/s12098-010-0041-1. [DOI] [PubMed] [Google Scholar]
- 26.Meena UK, Sen RK, Behera P, et al. WHOQOL-BREF Hindi questionnaire: Quality of life assessment in acetabular fracture patients. Indian J Orthop. 2015;49:323–28. doi: 10.4103/0019-5413.156206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Reserve Bank of India. Financial Inclusion. 2008. Available from [URL]: https://www.rbi.org.in/scripts/publicationsview.aspx?id=10494.
- 28.Ramdev S. Yoga: Its philosophy and practice. Haridwar (India): Divya Prakashan; 2007. [Google Scholar]
- 29.Muktibodhananda S. Hatha yoga pradipika: Light on hatha yoga. 2nd ed. Bihar (India): Yoga Publication Trust; 2002. [Google Scholar]
- 30.Telles S, Raghavendra BR. Neurophysiological changes in meditation correlated with descriptions from the ancient texts. Biofeedback. 2011;39:56–59. [Google Scholar]
- 31.Thayer JF, Lane RD. A model of neurovisceral integration in emotion regulation and dysregulation. J Affect Disord. 2000;61:201–16. doi: 10.1016/s0165-0327(00)00338-4. [DOI] [PubMed] [Google Scholar]
- 32.Porges SW. The Polyvagal Theory: Neurophysiological foundations of emotions, attachment, communication, and self-regulation. 1st ed. New York: WW Norton; 2011. [Google Scholar]
- 33.Kemp AH. Mechanisms underpinning the link between emotion, physical health, and longevity. Front Psychol. 2017;8:1338. doi: 10.3389/fpsyg.2017.01338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Butzer B, Bury D, Telles S, Khalsa SBS. Implementing yoga within the school curriculum: A scientific rationale for improving social-emotional learning and positive student outcomes. J Child Serv. 2016;11:3–24. [Google Scholar]
- 35.Griva K, Myers LB, Newman S. Illness perceptions and self-efficacy beliefs in adolescents and young adults with insulin dependent diabetes mellitus. Psychol Health. 2000;15:733–50. [Google Scholar]
- 36.Dittmann KA, Freedman MR. Body awareness, eating attitudes, and spiritual beliefs of women practicing yoga. Eat Disord. 2009;17:273–92. doi: 10.1080/10640260902991111. [DOI] [PubMed] [Google Scholar]
- 37.Impett EA, Daubenmier JJ, Hirschman AL. Minding the body: Yoga, embodiment, and well-being. Sex Res Social Policy. 2006;3:39–48. [Google Scholar]
- 38.Bharti SV. Yoga Sutras of Patanjali with the exposition of Vyasa. 1st ed. Delhi (India): Motilal Banarsidass Publisher Limited; 2001. [Google Scholar]
- 39.Deci EL, Ryan RM. Facilitating optimal motivation and psychological wellbeing across life’s domains. Can Psychol. 2008;49:14–23. [Google Scholar]
- 40.Leyva-Flores R, Kageyama ML, Erviti-Erice J. How people respond to illness in Mexico: self-care or medical care? Health Policy. 2001;57:15–26. doi: 10.1016/s0168-8510(00)00136-6. [DOI] [PubMed] [Google Scholar]
- 41.Behere RV, Raghunandan V, Venkatasubramanian G, et al. TRENDS – A tool for recognition of emotions in neuropsychiatric disorders. Indian J Psychol Med. 2008;30:2. [Google Scholar]
- 42.Jayaram N, Varambally S, Behere RV, et al. Effect of yoga therapy on plasma oxytocin and facial emotion recognition deficits in patients of schizophrenia. Indian J Psychiatry. 2013;55:S409–13. doi: 10.4103/0019-5545.116318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Clarke A, Friede T, Putz R, et al. Warwick-Edinburgh mental well-being scale (WEMWBS): Validated for teenage school students in England and Scotland. A mixed methods assessment. BMC Public Health. 2011;11:487. doi: 10.1186/1471-2458-11-487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Shivaram M. Ananda an Experience. Mysore (India): Kavyalaya Prakashana; 1954. [Google Scholar]
- 45.Katariya M. Laughter yoga: Daily laughter practices for health and happiness. Penguin Random House India Private Limited; 2018. [Google Scholar]
- 46.Gupta RK, Singh S, Singh N. Does yoga influence happiness and mental balance: A comparison between yoga practitioners and non-yoga practitioners. OJMR. 2016;2:1–5. [Google Scholar]
- 47.Hartfiel N, Havenhand J, Khalsa SB, et al. The effectiveness of yoga for the improvement of well-being and resilience to stress in the workplace. Scand J Work Environ Health. 2011;37:70–76. doi: 10.5271/sjweh.2916. [DOI] [PubMed] [Google Scholar]
- 48.Telles S, Singh N, Bhardwaj AK, et al. Effect of yoga or physical exercise on physical, cognitive and emotional measures in children: A randomized controlled trial. Child Adolesc Psychiatry Ment Health. 2013;7:37. doi: 10.1186/1753-2000-7-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Telles S, Pathak S, Kumar A, et al. Influence of intensity and duration of yoga on anxiety and depression scores associated with chronic illness. Ann Med Health Sci Res. 2015;5:260–65. doi: 10.4103/2141-9248.160182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Karmee N, Satapathy SP, Tripathy RM. Association between socio-demographic characteristics and preventable lifestyle related risk factors of non-communicable diseases among adolescents: A school-based study in Berhampur Odisha. Int J Community Med Public Health. 2017;4:2905–11. [Google Scholar]


