Abstract
A 34-year-old woman entered the emergency room with abdominal pain in the right upper quadrant. Computed tomography scan showed a nutmeg liver suspected for increased venous pressure by thrombosis of the liver veins, Budd-Chiari malformation, or right-sided heart failure. Interestingly, the diagnosis was pelvic inflammatory disease complicated by the Fitz-Hugh-Curtis syndrome (FHCS).
Pelvic inflammatory disease resulted from an ascended infection by Chlamydia trachomatis. FHCS was caused by perihepatitis defined as inflammation of the peritoneal capsule of the liver. Fast diagnosis and treatment is crucial. Therefore, we report a case of FHCS characterized by a nutmeg liver on computed tomography.
Keywords: Fitz-Hugh-Curtis syndrome, Perihepatitis, Hepatomegaly, Nutmeg liver, Pelvic Inflammatory disease, Chlamydia trachomatis
Abbreviations: FHCS, Fitz-Hugh-Curtis syndrome; GP, general practitioner; IUD, intrauterine device; PID, pelvic inflammatory disease
Case report
A 34-year-old female presented at our emergency room with right upper quadrant abdominal pain for 5 days and painful respiration. Her history reports 2 normal vaginal births (3 and 5 years ago), abdominal wall surgery, and a recent knee operation. She was a nonsmoker and drank 2 units alcohol a week. Social anamnesis reports a high socioeconomic status, a fulltime job, and a marriage for 14 years. A month ago, the general practitioner tried to place an intrauterine device for contraception, but was unsuccessful. She was treated for possible cystitis with nitrofurantoin for 4 days prior to her presenting symptoms.
The pain was sharp and progressive since the first day, aggravated by respiration and coughing. There were no complaints of nausea, vomiting, dysuria, and defecation. Before starting the oral contraceptive, she had a regular cycle of 28 days with a menstrual period of 5 days. There was no irregular blood loss or dyspareunia.
The patient was hemodynamically stable with a blood pressure of RR130/97 mm Hg, temperature of 37.7°C, and a pulse of 74 beats/min. During physical exam abdominal palpation was extremely painful, in particular at the level of the right upper quadrant. Hepatomegaly was diagnosed clinically by percussion. There were no signs of splenomegaly.
On the first day of presentation, laboratory data suggested an inflammatory process. An X-ray of the chest showed normal lungs, an elevated position of the diaphragm, and minimal free fluid. An ultrasound of the upper abdomen showed hepatomegaly resulting in a displaced pancreas. The diagnosis hepatitis was considered, although liver function tests were normal. She was admitted to the Department of Gastroenterology.
On the second day, laboratory results showed an increased level of D-dimers (920 μg/L). The patient was also experiencing chest pain, while breathing therefore a computed tomography (CT) pulmonary angiography was performed to exclude pulmonary vein embolism. No abnormalities were seen on this CT pulmonary angiography. A second ultrasound was made because symptoms worsened. No new features were found on the ultrasound. The gynecologist was consulted and examined the patient. The vaginal ultrasound showed a normal uterus and adnexal regions. A vaginal swab was performed to test for by Chlamydia trachomatis and Neisseria gonorrhoeae. Further imaging was not indicated at that time as the abdominal pain has reduced. The patient was discharged with instructions to seek medical advice if symptoms worsened.
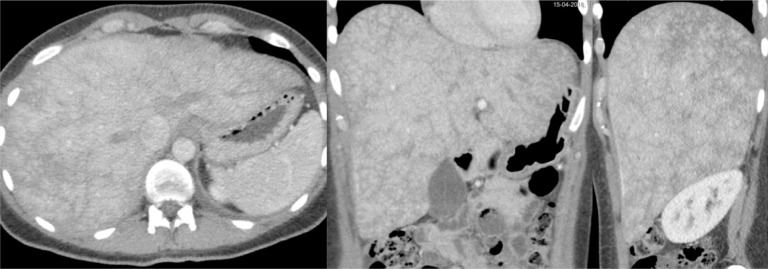
She returned on day 4 because of the severe progressive pain in the right upper quadrant. A contrast-enhanced CT scan of the abdomen was performed because of the continuous increased infection parameters (C-reactive protein 65 mg/mL), fever of 38.6°C, and the lack of a diagnosis. The previously diagnosed hepatomegaly was confirmed. Second, it demonstrated reversible intrahepatic parenchymal attenuation differences, also called a nutmeg liver. A nutmeg appearance of the liver is due to hepatic venous congestion. Contrast is prevented from diffusing through the liver in a normal manner, which results in a reticular or mosaic pattern of contrast enhancement in the early portal venous phase. This specific finding is highly suspicious for increased venous pressure by thrombosis of the liver veins, Budd-Chiari syndrome, or right-sided heart failure (Fig. 1).
Fig. 1.
Contrast-enhanced CT scan of the enlarged liver in axial, coronal, and sagittal dimension (right to left) demonstrates hepatic parenchymal attenuation differences, also called a “nutmeg liver.”
Interestingly, laboratory findings showed an increased level of N-terminal pro b-type natriuretic peptide of 238 pg/mL suspected for right-sided heart failure. The cardiologist was consulted. An electrocardiogram was conducted and no signs of heart failure were found.
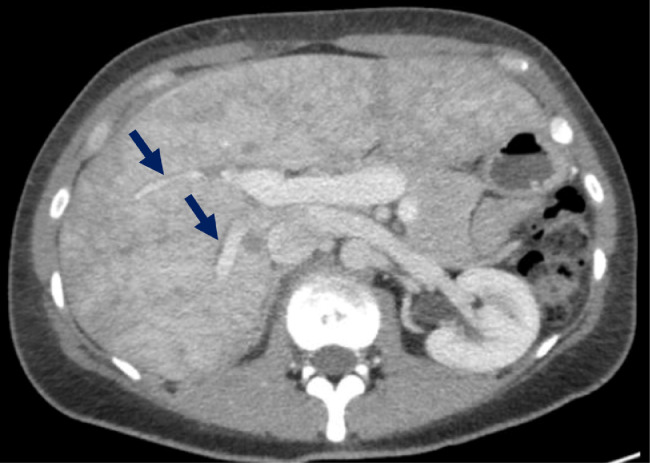
Reevaluation of the CT scan revealed enhancement of the hepatic capsule of the left lobe (Fig. 2). This specific finding is suggestive of Fitz-Hugh-Curtis syndrome (FHCS), which is a complication of more advanced pelvic inflammatory disease (PID). Additionally, pelvic fat inflammation and free fluid was present.
Fig. 2.
Early phase contrast-enhanced CT scan of the liver showing hyperintense enhancement of the anterior hepatic capsule of the right lobe.
A positive test for C trachomatis was found later as a causative organism for PID complicated by the FHCS. Doxycycline 100 mg was directly subscribed twice a day for 14 days. The patient was discharged and 6 weeks later she was seen in a good clinical condition at the outpatient department.
Discussion
A Chlamydia infection is associated with a wide spectrum of upper genital tract pathologies, ranging from asymptomatic endometritis to symptomatic salpingitis, tubo-ovarian abscess, peritonitis, and long-term sequelae such as infertility, ectopic pregnancy, and chronic pelvic pain [1], [2], [3], [4].
FHCS is characterized by acute perihepatitis secondarily to PID and classically presents with sudden onset of sharp right upper quadrant abdominal pain [5]. C trachomatis and N gonorrhoeae infections are usually responsible for FHCS, although 30%-40% of cases are polymicrobial [6]. The inflammation mechanism of the peritoneal capsule of the liver is believed to result from ascending infection from the pelvic cavity. Bacteria spread by means of direct extension along the right paracolic gutter or through the lymphatic system, causing inflammation of the right upper quadrant peritoneal surfaces of the liver.
Irritation of the hepatic capsule or peritoneum by the accumulated inflammatory exudates causes the sharp right upper quadrant abdominal pain. This pain is aggravated with deep respiration or coughing as a result of negative pressure during respiratory movements. Other related symptoms are nausea, vomiting, fever, and malaise. Fever, lower abdominal pain, and changed vaginal discharge are often seen in patients with PID and/or FHCS.
FHCS can be misdiagnosed as it may present like many other disorders including pulmonary embolism, pneumonia, cholecystitis, renal colic, and perforated ulcer [5]. When a patient presents with nonspecific symptoms only, the diagnosis is even more difficult.
In retrospect, uncertainty in the diagnostic process combined with the severe abdominal pain of the patient resulted in overutilization of medical studies. Importantly, the overuse of diagnostic imaging leaded to an increase in the number of diagnostic errors and resulted in high costs. The CT finding of the nutmeg liver was suspicious for other diseases diverging from the correct final diagnosis. FHCS is not in the differential diagnosis of this specific imaging finding. Therefore, we will discuss these imaging findings in further detail.
CT findings of early PID are typically subtle in the female reproductive tract. Often the only findings are fluid in the pouch of Douglas and pelvic fat inflammation. As the infection progresses, CT features of PID include fluid filled fallopian tubes with thick walls and enlarged ovaries with a heterogeneous or partly cystic appearance [7] (Fig. 3). A tubo-ovarian abscess represents a more advanced stage of PID.
Fig. 3.
Contrast-enhanced CT scan of the pelvis, which demonstrates enhanced and thickened fallopian tubes suspected for salpingitis. Additionally, the ovaries are enlarged, inflamed, and have a cystic appearance due to early oophoritis. Moreover, pelvic fat inflammation and free fluid is seen.
CT findings of perihepatitis with PID are relatively well described [8]. However, these studies focus on the specific finding of the liver capsule, also known as Glisson's capsule. They report capsular enhancement along the surface of the liver, most commonly seen on the right-anterior hepatic surface [9]. The mechanism of capsular enhancement seen on early-phase images is thought to be due to increased blood flow at the inflamed hepatic capsule. On the contrary, capsular enhancement seen on delayed images may reflect early capsular fibrosis [10]. In our case, hepatic capsular enhancement on early phase images with normalization of the capsule on the delayed images reflects the acute presentation or early phase of FHCS.
Only 1 case report describes the finding of transient hepatic attenuation difference due to hepatic venous outflow obstruction [11]. This can be categorized into 3 categories according to the level of obstruction: (1) at the level of sinusoids and terminal venules, (2) from hepatic veins to the superior end of inferior vena cava, and (3) venous obstruction at the level of the heart. Hepatic venous outflow obstruction is usually caused by hepatic veno-occlusive disease after hematopoietic stem cell transplantation, Budd-Chiari syndrome, or cardiovascular condition leading to an increased central venous pressure [11]. However, in our case, these diagnoses were unlikely because there was no history of transplant, there were no signs of increased central venous pressure and ultrasound showed flow in the portal vein.
The CT of the abdomen in our case showed hepatomegaly and multiple hypodense periportal halos around the patent portal veins consistent with periportal edema (Fig. 4). Although the portal vein did not appear to be compromised in our case, hepatic venous outflow obstruction was believed to be due to the inflammatory process. The pathophysiology is probably perihepatic and capsular inflammation that may have progressed to periportal infiltration of inflammatory cells. Dilated lymphatics and lymphedema on CT scans have been described in both intrahepatic and extrahepatic diseases [12]. The inflammatory process leads to the formation of periportal edema. There is fluid accumulation or dilatation of lymphatics in the loose areolar tissue around the portal triads or subsegmental portal venous branches. This may cause partial hepatic venous outflow obstruction by narrowing the hepatic veins, which induces congestion at the level of the sinusoids. Local inflammation is a less-common cause of transient hepatic attenuation differences; this however can cause decreased parenchymal attenuation of the liver parenchyma.
Fig. 4.
A zone of low attenuation around the central portal veins is seen, which indicates that there is periportal edema present, also referred to as periportal halo sign.
Therefore, the finding of a nutmeg liver in our case was believed to be due to the inflammation of the periportal regions secondary to the perihepatic and capsular inflammatory process. The CT finding of transient hepatic perfusion abnormalities in patients with FHCS can be referred to as the Budd-Chiari phenomenon [11]. Additionally, we found hepatomegaly on ultrasound and CT imaging. Hepatomegaly without elevated liver function tests is a nonspecific sign and has multiple causes including infection, fat infiltration, hepatic vein occlusion, and hepatic congestion.
Conclusion
In summary, severe abdominal pain in the right upper quadrant in a woman of reproductive age should raise suspicion for progressive PID known as the FHCS. Timely diagnosis and treatment, especially to retain fertility, is important.
Characteristic findings on CT scan regarding to the liver are hepatomegaly, intraparenchymal reversible dynamic perfusion abnormalities and capsular enhancement. We report a case of FHCS and the Budd-Chiari phenomenon. This impressive CT presentation shows a nutmeg liver appearance, which was believed to be due to local inflammation of the periportal regions secondary to the perihepatic and capsular inflammatory process. Hopefully, this case allows for accurate and prompt diagnosis in future cases.
Footnotes
Competing Interests: No grant or financial support was used for this case report. No author had any financial interest in the subject matter discussed in the submitted manuscript. No conflict of interest needs to be disclosed. All authors state that this study complies with the Declaration of Helsinki.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.radcr.2019.04.008.
Appendix. Supplementary materials
References
- 1.Mishori R., McClaskey E.L., WinklerPrins V.J. Chlamydia trachomatis infections: screening, diagnosis, and management. Am Fam Physician. 2012;86(12):1127–1132. [PubMed] [Google Scholar]
- 2.Wiesenfeld H.C., Hillier S.L., Krohn M.A., Amortegui A.J., Heine R.P., Landers D.V. Lower genital tract infection and endometritis: insight into subclinical pelvic inflammatory disease. Obstet Gynecol. 2002;100(3):456–463. doi: 10.1016/s0029-7844(02)02118-x. [DOI] [PubMed] [Google Scholar]
- 3.Kobayashi Y., Takeuchi H., Kitade M., Kikuchi I., Sato Y., Kinoshita K. Pathological study of Fitz-Hugh-Curtis syndrome evaluated from fallopian tube damage. J Obstet Gynaecol Res. 2006;32(3):280–285. doi: 10.1111/j.1447-0756.2006.00399.x. [DOI] [PubMed] [Google Scholar]
- 4.Paavonen J., Eggert-Kruse W. Chlamydia trachomatis: impact on human reproduction. Hum Reprod Update. 1999;5(5):433–447. doi: 10.1093/humupd/5.5.433. [DOI] [PubMed] [Google Scholar]
- 5.Peter N.G., Clark L.R., Jaeger J.R. Fitz-Hugh-Curtis syndrome: a diagnosis to consider in women with right upper quadrant pain. Cleve Clin J Med. 2004;71:233–239. doi: 10.3949/ccjm.71.3.233. [DOI] [PubMed] [Google Scholar]
- 6.Hyun J.J., Kim J.Y., Bak Y.-T., Lee C.H., Choi S.Y. Education and imaging. Gastrointestinal: Fitz-Hugh–Curtis syndrome. J Gastroenterol Hepatol. 2006;21(9):1493. doi: 10.1111/j.1440-1746.2006.04632.x. [DOI] [PubMed] [Google Scholar]
- 7.Sam J.W., Jacobs J.E., Birnbaum B.A. Spectrum of CT findings in acute pyogenic pelvic inflammatory disease. Radiographics. 2002;22(6):1327–1334. doi: 10.1148/rg.226025062. [DOI] [PubMed] [Google Scholar]
- 8.Kim J.Y., Kim Y., Jeong W.K., Song S.Y., Cho O.K. Perihepatitis with pelvic inflammatory disease (PID) on MDCT: characteristic findings and relevance to PID. Abdom Imaging. 2009;34(6):737–742. doi: 10.1007/s00261-008-9472-9. [DOI] [PubMed] [Google Scholar]
- 9.Kim S., Kim T.U., Lee J.W., Lee T.H., Lee S.H., Jeon TY. The perihepatic space: comprehensive anatomy and CT features of pathologic conditions. Radiographics. 2007;27(1):129–143. doi: 10.1148/rg.271065050. [DOI] [PubMed] [Google Scholar]
- 10.Pickhardt P.J., Fleishman M.J., Fisher A.J. Fitz-Hugh-Curtis syndrome: multidetector CT findings of transient hepatic attenuation difference and gallbladder wall thickening. Am J Roentgenol. 2003;180(6):1605–1606. doi: 10.2214/ajr.180.6.1801605. [DOI] [PubMed] [Google Scholar]
- 11.Wells M.L., Fenstad E.R., Poterucha J.T. Imaging findings of congestive hepatopathy. RadioGraphics. 2016;36:1024–1037. doi: 10.1148/rg.2016150207. [DOI] [PubMed] [Google Scholar]
- 12.Karcaaltincaba M., Haliloglu M., Akpinar E., Akata D., Ozmen M., Ariyurek M. Multidetector CT and MRI findings in periportal space pathologies. Eur J Radiol. 2007;61(1):3–10. doi: 10.1016/j.ejrad.2006.11.009. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.