Abstract
Little is known about what differentiates individuals whose drinking patterns escalate into problematic use following the transition out of college compared to those who learn to drink in a way that is consistent with independent adult roles. Patterns of alcohol use and problems during college may pre-sage progression toward problem drinking in adulthood. The present study sought to examine such patterns in an effort to delineate those at greatest risk. Research has not yet elucidated whether, when, and how these groups diverge.
Our results indicate that students who report AUD symptoms one year following graduation reported greater alcohol involvement from the first semester and escalated their involvement with alcohol at a more rapid pace. We observed marked and measurable differences in drinking patterns between those who go on to exhibit AUD symptoms following college, and those who do not. A close inspection of these differences reveals that relatively small absolute differences in alcohol consumption add up to large differences in alcohol related consequences.
Thus, markers of longer-term risk are present early in college, and greater escalation of drinking across college is an indicator that intervention is needed. Brief Motivational Interventions could help students to anticipate some of the challenges ahead as they transition from the college environment, as well as the potential deleterious effects of immoderate alcohol use on making a successful transition into adult roles. In addition to the beginning of college, our findings also point to critical periods during which screening and brief intervention may be optimally timed.
Keywords: College student drinking, Transition out of college, Joinpoint Analysis, Alcohol Use Disorder
For a substantial portion of young adults in the U.S., the years of peak alcohol involvement (ages of 18–24; Dawson, Grant, Stinson & Chou, 2004; Johnston, O’Malley, Bachman, & Schulenberg, 2013) coincide with the college years. The ubiquity of heavy drinking among those in college is well documented, as are the myriad consequences that accompany such drinking (Carter, Brandon & Goldman, 2010; Johnston et al., 2013; Slutske, 2005). These include both acute consequences (e.g., alcohol poisoning, sexual assault, driving under the influence), as well as consequences that extend well beyond the college years (e.g., sexually transmitted diseases, unplanned pregnancies, injury or disability from alcohol-related accidents).
Transitioning out of heavy alcohol involvement.
Though some college students “mature out” of heavy drinking once they leave college, others do not (Verges et al., 2013), and thus are at risk for poor adaptation to adulthood, including continued problem drinking and associated health outcomes (Lee, Chassin, & MacKinnon, 2015; Verges et al., 2013). It has been suggested that patterns of alcohol use and problems during college may pre-sage progression toward problem drinking later in adulthood (Schulenberg & Maggs, 2002). Yet, to date, little is known about what differentiates these two groups. An open question is whether there are specific drinking patterns, identified early in college, which may foretell the evolution into problematic drinking. The objective of the present study was to identify marked and measurable differences in drinking patterns in an effort to delineate those at greatest risk.
The multidimensionality of alcohol involvement.
Researchers have used a variety of strategies to characterize alcohol involvement; however, no one index of alcohol use or problems is considered ideal, as each index has advantages and limitations. Typical drinking can be measured using a simple count of drinks per drinking day to provide an index of a student’s quantity of drinking (Collins, Parks, & Marlatt, 1985; Wood, Read, Palfai, & Stevenson, 2001). Alcohol use can be characterized further by identifying heavy episodic drinking patterns (i.e., 4+/5+ drinks for women/men in a single sitting; “binge” drinking: Wechsler, Dowdall, Davenport, & Rimm, 1995). Binge drinking was first identified as an indicator of problematic alcohol involvement over two decades ago (Wechsler, et al., 1994). Further, more recent findings highlight the utility of examining alcohol consumption that goes beyond the classic “binge” threshold. As such, another way of capturing risky alcohol drinking patterns is to examine these more extreme levels of consumption (Polak & Conner, 2012; Read et al., 2008).
Beyond just amount of alcohol consumed, researchers also have sought to use indices that reflect alcohol intoxication (e.g., Carey & Hustad, 2002). Blood alcohol concentration (BAC) often is used as an event-level indicator of intoxication that controls for biological sex, weight, time spent drinking, and number of standard drinks consumed. Further BAC offers information about impairment, or drunkenness, that may shed light not provided by number of drinks alone. Two dimensions are commonly assessed, typical BAC (tBAC) which evaluates average drunkenness, or Peak BAC (pBAC), which provides insights into student’s maximum drunkenness. The latter of these may be more strongly associated with hazardous alcohol outcomes. Though biological measures of BAC are ideal (Carey & Hustad, 2002; Hustad & Carey, 2005), estimations of BAC based on self-report data dates back to work by Widmark in the 1930s. Data show such estimations are strongly correlated with breath analysis, particularly for BACs below .08, and are valuable indicators of alcohol-impairment (Carey & Hustad, 2002).
Evaluation of the myriad dimensions of alcohol involvement in college must also include patterns of consequences that are experienced. Alcohol-related consequences can range from mild (e.g., being late to class) to severe (e.g., sexual victimization). Previous research has established that while correlated, alcohol use and alcohol related consequences are distinct constructs and as such, are a unique and distinct dimension of college alcohol involvement (Prince, Pearson, Bravo, & Montes, 2018). Further, data show consequences experienced during college may predict later problematic drinking (Davies & Clifford, 2016; Read, Merrill, Kahler, & Strong, 2007; Read, Wardell, & Bachrach, 2013). Many alcohol consequences are normative and may be perceived as desirable among college students (Mallett et al., 2013), but nonetheless denote longer-term risk. The early identification of such consequences and their associations with later AUD symptoms could provide an important marker for preventive interventions.
Modeling Risk.
There are a number of ways to examine longitudinal trends in alcohol use among college students. One approach that has been used successfully to model the clinical course of adults with alcohol use disorder (Prince & Maisto, 2013) is Joinpoint (JP) analysis (JPA; Kim et al., 2000). JPA has a number of advantages in describing longitudinal data. First, JPA was developed by the National Cancer Institute’s Division of Cancer Control & Population Sciences’ Surveillance Research Program specifically to describe outcomes data in a way that is easy to disseminate and interpret by clinicians and interested readers without a strong statistical background. This is accomplished by reducing the longitudinal trends to simple line segments, with slopes and intercepts. Second, JPA identifies how many inflection points are present in longitudinal data, how dramatic the changes are, as well as where (i.e., at what assessment point) the changes occur. This is an advantage over piecewise latent growth curve modeling, which requires researchers to determine a priori where inflection points may lie and/or to manually test a series of piecewise latent growth models to determine the model that best fits the data. Inflection points (e.g., points in the data where the trend goes from increasing to decreasing, or increasing steeply to increasing less steeply) provide insight into critical moments in the course of the data. JPs can be linked to important events in the participant’s life (e.g., developmental milestones, significant events). Third, JPA allows for the comparison of trajectories of multiple groups of individuals. The JP software (https://surveillance.cancer.gov/joinpoint/) allows for tests of parallelism and coincidence, which provide statistical tests of whether two groups change in similar ways across the course of the study. Taken together, JPA is an excellent tool to describe longitudinal changes in alcohol use and related consequences, and to compare those who mature out of heavy/problematic drinking to those who do not.
The present study.
The goal of the current study is to identify differences in patterns of drinking that are associated with longer-term problem drinking. The identification of risky drinking practices and critical moments in the course of college drinking can help to identify which drinking patterns of use and consequences are associated with the greatest impact on drinking outcomes that place young adults at greatest risk for poor long-term adaptation. Understanding the difference between acutely risky drinking and more distal risky drinking can facilitate different intervention actions when delivered to young adults approaching this developmental turning point, with the goal of helping them to successfully meet the developmental demands ahead of them (Maggs, Schulenberg, & Hurrelmann, 1997). JPA is an ideal approach for examining alcohol involvement trajectory differences between individuals who develop AUD symptoms and those who do not following college, because a key feature of JPA is the ability to test for similarities and differences in longitudinal trends across groups.
We were particularly interested in identifying measurable differences in early indicators of alcohol involvement (use, consequences) between those who report AUD symptoms after graduation and those who do not. Further, we were interested to see if any indicators stood out as particularly informative. This study seeks to contrast patterns of during college drinking between those who report AUD symptoms post-graduation and those who did not, by (a) describing longitudinal patterns of alcohol use and related consequences across college and during the first year following graduation, (b) identify critical junctures where these groups diverge or have maximum separation, and (c) identify early patterns of alcohol involvement that were the strongest predictors of later problematic use.
Methods
Participants
Participants (n = 347; n=239 female) were screened and recruited as incoming freshman students from a midsized public university in the northeastern United States. Participants represent 1 of 3 cohorts who were followed for an additional 7 time points from a larger multisite study (N = 997) on college student alcohol use, for many of the students in this cohort (n = 525) the additional assessments spanned the transition out of college (Administrative Supplement: R01DA018993-05S1; see Read et al., 2011; Read et al., 2012). Specifically, participants in the present study are those students who provided data throughout four years of college and the first assessment point (i.e., September of their 5th year of participation) following graduation (i.e., students who did not graduate were not included). Participants completed the survey a total of 19 times including: 6 times in year 1, 4 times in year 2, 4 times in year 3, 4 times in year 4, and 1 time in the Fall following graduation. Participants were either 18 or 19 years old (M = 18.04, SD = .20) at the initial assessment. The majority of participants identified as female (69%) and Caucasian (86%). At wave 19, 28% participants reported symptoms that would meet criteria for an AUD (AUD: n = 96; No AUD: n = 251). Rates were similar for men (32%) and women (24%) regarding AUD symptom ratings (χ2 (1) = 2.44, p = .11).
Procedure
All procedures were approved by the university’s institutional review board. Participants were recruited to participate in a web-based study and all study measures were administered online. To minimize order effects, the online survey was programmed so that measures were administered in random order, clustered within topic area. Also, to minimize underreporting by “skipping out”, surveys were programmed to take approximately the same amount of time to complete, regardless of specific responses. The original study was designed to examine the relation between posttraumatic stress and alcohol use; therefore, there were an equal number of participants who met criteria for posttraumatic stress and those who did not meet criteria (see Read et al., 2011 for details). The current subsample was also balanced with regard to posttraumatic stress status. There were no differences between participants with or without posttraumatic stress on any of the alcohol use variables or alcohol related consequences (ps > .05). Further, those with posttraumatic stress were no more likely to exhibit symptoms of an AUD compared to those without (χ2 (1) = .009, p = .92). All those who were consented into the study were followed for the study duration, regardless of transfer or college attrition status. Rates of college attrition (i.e., “drop out”) were low (<5%; Bachrach & Read, 2012).
Measures
Demographics.
Participants reported demographic information, including biological sex and weight, as part of a general information questionnaire collected at each assessment wave.
Daily Alcohol use.
The Daily Drinking Questionnaire (DDQ; Collins, Parks, & Marlatt, 1985) was administered at every time point to assess typical daily alcohol use. Participants reported the average number of drinks consumed on a typical Monday, Tuesday, … , Sunday in the past 30 days, as well as the number of hours spent drinking on each day of the week during a typical week of drinking in the past month.
Typical quantity.
Participants who reported consuming alcohol were also given a standard drink measurement chart so they could report the typical quantity of alcohol consumption per week in the past month (Wood, Read, Palfai, & Stevenson, 2001). Typical quantity was assessed with a single item “In the PAST MONTH, when you were drinking alcohol, how many drinks did you usually have on any ONE occasion?”. The response options for this item were as follows: 0=Didn’t drink in the past month; 1=Less than 1, or 1 total, 2=2 total, 3=3 total, 4=4 total, 5=5 total, 6=6 total, 7=7 total, 8=8 total, 9=9 or more total.
Estimated Blood Alcohol Concentration (BAC).
Estimated BACs were calculated for each participant on each drinking day. we used the following equation [(c/2)*(GC/w)]-(.02*t), where c=total standard drinks consumed, GC=gender constant (9.0 for women, 7.5 for men), w=weight in pounds and t=total hours spent drinking (Hustad & Carey, 2005).
Estimated Typical Blood Alcohol Concentration (tBAC).
tBAC was calculated by taking the average BAC on drinking days as reported in the DDQ.
Estimated Peak Blood Alcohol Concentration (pBAC).
pBAC was calculated by taking the BAC on the heaviest drinking day during a typical week in the past month.
Percent Binge Drinkers.
Percentage of binge drinkers was calculated by coding those individuals who reported drinking more than the binge threshold as their typical drinking as binge drinkers (i.e., 4+ drinks for females / 5+ drinks for males; Wechsler et al., 1994).
Percent Heavy Binge Drinkers.
Percentage of heavy binge drinkers was calculated using the typical quantity item. Specifically, we followed recommendations by Read et al. (2008) and coded those individuals who reported drinking more than the heavy binge threshold as their typical drinking as heavy binge drinkers (i.e., 6+ drinks for females / 7+ drinks for males).
Alcohol related consequences.
The Young Adult Alcohol Consequences Questionnaire (YAACQ; Read, Kahler, Strong, & Colder, 2006) was used to assess alcohol related consequences in the past month. Response options for the YAACQ are dichotomously scored (yes-no) and includes 48 consequences that range in severity. The YAACQ total score ranges from 0 to 48. The YAACQ has strong psychometric properties and was designed to reduce gender bias (Read et al., 2007).
Alcohol Use Disorder Symptoms.
The presence of alcohol use disorder symptoms (i.e., alcohol abuse, alcohol dependence) was determined using a self-report measure based on DSM-IV-TR criteria and derived from Module J of the Mini-International Neuropsychiatric Interview (MINI; Sheehan et al., 1998). This measure was completed during the Fall of each year (i.e., in waves 1, 7, 11, 15, & 19). Given the change in the conceptualization of an alcohol use disorder from DSM-IV-TR to DSM-V, which no longer separates alcohol abuse and dependence into separate diagnoses, we combined those who reported symptom levels consistent with criteria for abuse and dependence into a broader category to better match the current DSM-V conceptualization of an Alcohol Use Disorder (AUD).
Analysis Plan
In order to describe alcohol use and consequence patterns among college students who did or did not report symptoms consistent with criteria for an AUD following graduation we divided the sample based on AUD symptom counts that indicated AUD status at wave 19 (i.e., September of the 5th year of participation) and only included participants who had graduated college by that time point. The final sample consisted of 347 students out of 525 students total - eliminating 178 students who were followed longitudinally but had not yet graduated or provided incomplete data. Once these groups were established we modeled their alcohol use over time with peak BAC, typical BAC, typical quantity of alcohol consumed on drinking days, percent of participants per group whose typical alcohol use exceeded the threshold for binge drinking (i.e., 4/5+ for females/males), and percent of participants per group whose typical alcohol use exceeded the threshold for heavy binge drinking (i.e., 6/7+ for females/males). In addition to alcohol use, we modeled the number of alcohol related consequences for each group across time.
Joinpoint Analysis.
JPA seeks to identify discrete inflection points in longitudinal data (e.g., when a trend changes from increasing to decreasing) through the use of a permutation test (Kim et al., 2000). The JP Regression Program (http://surveillance.cancer.gov/joinpoint) statistically determines the number of change points through a series of permutation tests such that if one more change point is added the resultant model is not an improvement over a model with one fewer change point (Yu et al., 2007). The permutation test uses a Bonferroni correction to adjust the significance level based on the number of comparisons. If no inflection points are identified, an intercept and slope for the longitudinal data is provided. Slopes equivalent to zero provide evidence for consistency of effects. JPA is appropriate to map longitudinal patterns in alcohol involvement and to identify critical moments when interventions may be ideally timed.
In addition to identifying trends in longitudinal data, JPA provides two comparability tests to assess for similarities across groups. The first is a test of coincidence, which tests if the two JP regression functions are identical (Kim et al., 2004). The second is a test of parallelism, which tests if the functions are parallel. The difference between the tests is that for two functions to be considered coincident they must have the same intercepts and slopes across the domain of the function, whereas to be considered parallel, they need not have the same intercepts. An advantage to JPA when analyzing data from small or unbalanced samples is that trends and group comparisons are modeled from the means and standard errors for each time point allowing for the inclusion of cases with missing data and comparisons of groups of unequal sample sizes.
In the present study, JPA was used to model longitudinal trends in 5 alcohol use indicators and alcohol related consequences separately by AUD status. JPA was used to identify inflection points in longitudinal trajectories across 19 assessment waves and to derive intercepts and slopes for each group. Tests of coincidence and parallelism were conducted to ascertain the degree of similarity between the AUD and no-AUD groups’ trajectories across time.
Effect Size Comparisons.
In order to further examine the magnitude and direction of the differences between groups on all 6 alcohol outcomes effect sizes were calculated. Specifically, for tBAC, pBAC, typical quantity, and alcohol related consequences we calculated independent-samples Cohen’s ds at each wave to provide a standardized measure of the magnitude of the difference between groups at a given time point. Cohen (1988) recommends cutoffs of .2, .5, and .8 for small, medium, and large effects, respectively. We also calculated the average effect size difference and confidence intervals between groups to provide an overall picture of the size of the effect and our degree of confidence in the point estimate. For the binge and heavy binge variables, we used the difference in percent of each group that reported typical drinking levels that met the binge or heavy binge thresholds as our effect size. We also calculated the average difference for each group and a confidence interval around the average difference.
Results
Joinpoint Analyses
Overall summary.
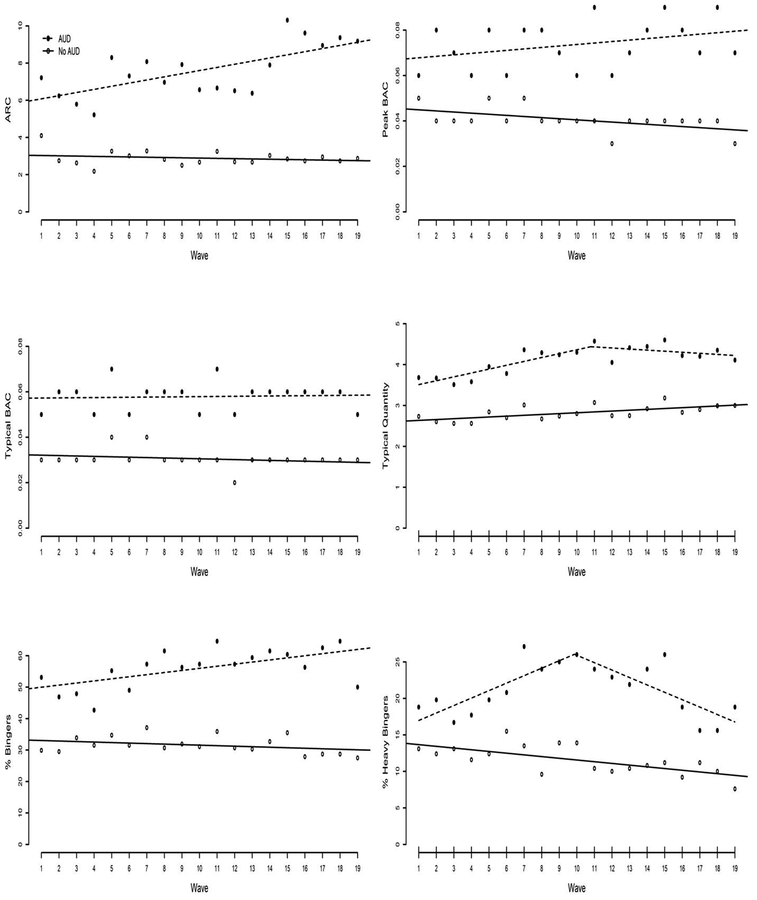
JPAs assessing trends in alcohol outcomes did not identify any discrete change points in the slopes for either group in 4 out of the 6 outcomes. For peak BAC, typical BAC, percent of binge drinkers, and alcohol related consequences, the permutation tests comparing 0 JPs to 4 JPs, 3JPs, 2 JPs, and 1 JP, were all non-significant (ps > .0125). This also held for the trajectory for typical quantity and percent of heavy drinkers in the non-AUD group. The two exceptions were typical quantity and percent of heavy binge drinkers in the AUD group for which the JPA identified 1 JP in each case. Specifically, for typical quantity the permutation test identified a JP at wave 11 for the AUD group, such that typical quantity went from increasing for waves 1 through 11 to remaining stable for waves 12 through 19 (0 JPs vs. 4 JPs: p = .02; 0 JPs vs. 3 JPs: p = .01; 0 JP vs. 2 JPs: p = .01; 1 JP vs. 2 JPs: p = .43). For percent of heavy binge drinkers the permutation test identified a JP at wave 10 for the AUD group, such that the percent of heavy bingers went from increasing for waves 1 through 10 to decreasing for waves 11 through 19 (0 JPs vs. 4 JPs: p = .002; 1 JPs vs. 4 JPs: p = .09; 1 JP vs. 3 JPs: p = .22; 1 JP vs. 2 JPs: p = .42). In addition, as can be seen in Figure 1 panels a through f, the AUD group started higher and remained higher than the non-AUD group on all 6 alcohol outcomes across the 19 assessment waves. The specifics of the JPA for each outcome are provided below.
FIGURE 1:
Changes in alcohol involvement indicators overtime by AUD status.
Note: AUD = self-reported symptoms consistent with an alcohol use disorder; No AUD = self-reported symptoms not consistent with an alcohol use disorder. Peak BAC = estimated peak blood alcohol concentration; typical BAC = estimated typical blood alcohol concentration.
Peak BAC.
The AUD group reported higher pBAC levels compared to the non-AUD group at wave 1 (InterceptAUD = .07, SE = .004, p < .000001; vs. Interceptnon-AUD = 04, SE =.002, p < .000001). In addition, the AUD group significantly increased their pBAC levels across the course of the study (SlopeAUD = .0008, SE = .0004, p = .03), whereas the non-AUD group’s pBAC levels remained stable (Slopenon-AUD = −.0003, SE = .0002, p = .09). Both tests of parallelism and coincidence were rejected (ps < .001), providing evidence that the AUD and non-AUD groups trajectories were substantially different with regard to pBAC levels.
Typical BAC.
The AUD group reported higher tBAC levels compared to the non-AUD group at wave 1 (InterceptAUD = .06, SE = .003, p < .000001; vs. Interceptnon-AUD = 03, SE =.002, p < .000001). In addition, the non-AUD group significantly decreased their tBAC levels across the course of the study (Slopenon-AUD = −.0003, SE = .0001, p = .04), whereas the AUD group’s tBAC levels remained stable (SlopeAUD = .0001, SE = .0002, p = .65). Both tests of parallelism and coincidence were rejected (Parallelism: p = .019, Coincidence: p < .001), providing evidence that tBAC level trajectories were significantly different between groups.
Typical Quantity.
The AUD group reported higher typical quantity levels compared to the non-AUD group at wave 1 (InterceptAUD = 3.43, SE = .13, p < .000001; vs. Interceptnon-AUD = 2.91, SE = .18, p < .000001). In addition, the non-AUD group’s typical quantity remained stable across the course of the study (Slopenon-AUD = −.006, SE = .02, p = .70), whereas the AUD group’s typical quantity initially increased until wave 11 then remained stable until the end of the study (SlopeAUD1 = .09, SE = .02, p = .0008; SlopeAUD2 = −.03, SE = .03, p = .30). Both tests of parallelism and coincidence were rejected (Parallelism: p < .001, Coincidence: p < .001), providing evidence that typical quantity trajectories was significantly different between groups.
Binge.
The AUD group reported a higher percentage of binge drinkers compared to the non-AUD group at wave 1 (InterceptAUD = 49.33, SE = 2.47, p < .000001; vs. Interceptnon-AUD = 33.21, SE = 1.28,p < .000001). In addition, the percent of binge drinkers in the non-AUD group remained stable across the course of the study (Slopenon-AUD = −16, SE = .11, p = .16), whereas the percent of binge drinkers in the AUD group increased across the course of the study (SlopeAUD = .67, SE = .22, p = .007). Both tests of parallelism and coincidence were rejected (Parallelism: p = .019, Coincidence: p < .001), providing evidence that percentage of binge drinkers trajectories were substantially different between groups.
Heavy Binge.
The AUD group reported a higher percentage of heavy bingers compared to the non-AUD group at wave 1 (InterceptAUD1 = 16.06, SE = 1.85, p < .000001; vs. Interceptnon-AUD = 13.81, SE = .72, p < .000001). The percent of heavy bingers in the AUD group increased until wave 10 then decreased until wave 19. The first slope for the AUD group, from waves 1 to 10 was positive (SlopeAUD1 = .99, SE = .33, p = .009). The second slope for the AUD group from waves 11 to 19 was negative (InterceptAUD2 = 36.34, SE = 5.01, p < .000001; SlopeAUD2 = −1.03, SE = .33, p = .007). The non-AUD group decreased the percentage of heavy bingers across the course of the study (Slopenon-AUD = −.23, SE = .06, p = .002). Both tests of parallelism and coincidence were rejected (Parallelism: p = .019, Coincidence: p < .001), providing evidence that the percentage of heavy bingers trajectories was significantly different between groups.
Alcohol Related Consequences.
The AUD group reported higher levels of alcohol related consequences compared to the non-AUD group at wave 1 (InterceptAUD = 5.68, SE = .47, p < .000001; vs. Interceptnon-AUD = 2.91, SE = .18, p < .000001). In addition, the AUD group significantly increased their levels of alcohol related consequences across the course of the study (SlopeAUD = .17, SE = .05, p = .001), whereas the non-AUD group’s levels of alcohol related consequences remained stable (Slopenon-AUD = −.001, SE = .01, p = .70). Both tests of parallelism and coincidence were rejected (ps < .001), providing evidence that levels of alcohol related consequences trajectories were substantially different between the AUD and non-AUD groups.
Effect Size Comparisons
Overall summary.
At every assessment point the AUD group reported higher levels of each alcohol related outcome. Table 1 presents the effect size for difference (i.e., Cohen’s d) between the groups at each wave (calculated as AUD - non-AUD), such that a positive value means that the AUD group had higher levels of that outcome. In addition, the magnitude of the difference between the groups increased across the 19 assessment waves demonstrating a bigger difference in the drinking and consequences patterns at later assessment points. The average effect size for the difference, along with the minimum and maximum differences are also presented in Table 1 for each outcome to summarize the results.
TABLE 1:
Effect Sizes - Cohen’s ds and percent differences for difference between AUD and No AUD groups on alcohol involvement indicators.
| Peak BAC | Typical BAC | Typical Quantity | Percent Binge Drinkers | Percent Heavy Binge Drinkers | Alcohol Related Consequences | |
|---|---|---|---|---|---|---|
| Wave 1 | 0.22 | 0.28 | 0.39 | 23% | 6% | 0.38 |
| Wave 2 | 0.54 | 0.44 | 0.43 | 17% | 7% | 0.50 |
| Wave 3 | 0.44 | 0.44 | 0.37 | 14% | 4% | 0.51 |
| Wave 4 | 0.36 | 0.32 | 0.38 | 11% | 6% | 0.54 |
| Wave 5 | 0.53 | 0.45 | 0.43 | 21% | 7% | 0.59 |
| Wave 6 | 0.36 | 0.30 | 0.41 | 18% | 5% | 0.58 |
| Wave 7 | 0.47 | 0.41 | 0.53 | 20% | 14% | 0.60 |
| Wave 8 | 0.60 | 0.48 | 0.67 | 31% | 14% | 0.53 |
| Wave 9 | 0.47 | 0.45 | 0.58 | 24% | 11% | 0.59 |
| Wave 10 | 0.41 | 0.38 | 0.60 | 26% | 12% | 0.51 |
| Wave 11 | 0.90 | 0.78 | 0.63 | 29% | 14% | 0.49 |
| Wave 12 | 0.68 | 0.48 | 0.54 | 27% | 13% | 0.51 |
| Wave 13 | 0.67 | 0.55 | 0.72 | 29% | 12% | 0.52 |
| Wave 14 | 0.67 | 0.51 | 0.67 | 29% | 13% | 0.55 |
| Wave 15 | 0.77 | 0.61 | 0.67 | 25% | 15% | 0.79 |
| Wave 16 | 0.86 | 0.60 | 0.68 | 28% | 10% | 0.77 |
| Wave 17 | 0.68 | 0.55 | 0.64 | 34% | 4% | 0.65 |
| Wave 18 | 0.95 | 0.67 | 0.70 | 36% | 6% | 0.82 |
| Wave 19 | 0.79 | 0.60 | 0.54 | 23% | 11% | 0.67 |
| Average | ||||||
| daverage | 0.60 | 0.49 | 0.56 | 24% | 10% | 0.58 |
| CI | .69, .51 | .55, .43 | .61, .50 | 13%, 35% | 11%, 8% | .64, .53 |
| Minimum | ||||||
| Wave # | 1 | 1 | 3 | 4 | 3 | 1 |
| dwave# | .22 | .28 | .37 | 11% | 4% | .38 |
| Maximum | ||||||
| Wave # | 18 | 11 | 13 | 18 | 18 | 18 |
| dwave# | .95 | .78 | .72 | 36% | 36% | .82 |
Note: Calculation conducted as AUD - No AUD. Cohen’s d cutoffs .2 = small, .5 = medium, .8 = large. AUD = self-reported symptoms consistent with an alcohol use disorder; No AUD = self-reported symptoms not consistent with an alcohol use disorder. Peak BAC = estimated peak blood alcohol concentration; typical BAC = estimated typical blood alcohol concentration.
Discussion
Despite a large literature documenting heavy drinking and associated problems in college students, surprisingly little research has sought to examine precisely how during-college drinking may be linked to the risk for the later problematic alcohol involvement, or which dimensions of drinking may be most informative for understanding this risk. Further, little is known about specific points in the drinking trajectory that may be best for intervention. Addressing these gaps in the literature was the goal of the present study. Though the heavy drinking and related consequences are relatively normative among college students, findings here suggest that there are marked and measurable differences in these drinking patterns between those who go on to show evidence of more problematic alcohol involvement and those who do not. Importantly, these differences are evident as early as the first year of college. Also notable is that trends in the effect sizes suggest that the differences between the two groups increased across the course of the study. Thus, rather than resolving or leveling off, these patterns and associated risk become greater as time progresses.
Alcohol involvement during college falls on a continuum from abstention to problem use. Yet, our data indicate that although students who develop AUD symptoms and those students who do not are engaging in some of the same behaviors along that continuum, they are in fact on two different trajectories. We described one pattern of drinking behavior that is associated with long-term problem use (AUD symptoms), and another that is not. A close inspection of the differences in the alcohol involvement indices reveals surprisingly small absolute differences. For example, the maximum difference in pBAC is .05, with those in the AUD group reaching pBACs of .09 and those in the non-AUD group reaching pBACs of .04 at the place of greatest divergence. Similarly, the difference in tBAC reaches a maximum of .04 (AUD tBAC = .07; non-AUD = .03), and the maximum difference in typical quantity is 1.66 (AUD typical quantity = 4.41; non-AUD typical quantity = 2.75). These relatively small differences in alcohol consumption add up to large differences in alcohol related consequences. The maximum difference between the groups is 6.63 alcohol related consequences per month (AUD alcohol related consequences = 9.37; non-AUD group alcohol related consequences = 2.74). That translates to more than 1.5 additional consequences per week resulting from less than two drinks more per occasion. Though clinicians and researchers may be aware that heavier drinking begets more consequences, no research to date has provided evidence of the specific magnitude of risk conferred by early heavy drinking. Such information likely will be useful in the context of intervention, as it underscores that relatively small differences in alcohol consumption can make a difference in ways that may be important for the drinker.
The alcohol involvement indices with the biggest effect size differences between those with and without AUD were pBAC, alcohol-related consequences, and percent of binge drinkers. The findings pertaining to binge drinkers is consistent with prior studies (Hasin, Paykin, & Endicott, 2001; Jackson, 2008) showing that this pattern of drinking carries not only acute risk for hazardous outcomes, but longer-term risk as well. Importantly, our findings regarding pBAC add to a growing literature on “high intensity” or “extreme” drinking (Patrick et al., 2013; White et al., 2006), as our results show that especially high levels of alcohol consumption and drunkenness may be not only acutely risky, but may also be associated with the development of alcohol use disorder symptoms further down the road. As such, these patterns may be an especially important focus for efforts at early identification. Also important are the findings pertaining to alcohol consequences. Though such consequences long have been studied as an outcome of high-risk drinking, more recent work has highlighted how these consequences may be used to portend later risk (e.g. Barnett et al., 2006; Mallett et al., 2006; Merrill, Read, & Barnett, 2013). To our knowledge, no studies have examined how alcohol consequences act as a risk marker for post-college drinking outcomes. Our findings point to this as a potentially important warning indicator - one that could be incorporated into feedback-based interventions.
In addition to the absolute magnitude of the differences between the groups, our analyses reveal that as a whole, the non-AUD group tended to decrease or remain stable levels of alcohol involvement across indices, whereas the AUD group tended to increase their involvement or increase sharply then moderate their involvement across the 19 assessment waves. The differences in initial position and slope of the trajectories is what drives the increased separation between the groups. The tests of parallelism and coincidence, provide an objective test of this observation. Specifically, from these tests we can provide evidence that the slopes are in fact statistically different from parallel, and that the initial levels of each index differ to a meaningful degree.
Our joinpoint analyses allowed for examination of whether there were critical points in alcohol involvement trajectories where trends in alcohol use and consequences changed. Overall, out analysis did not identify discrete change points in the slopes for either group in 4 out of the 6 outcomes. This suggests that there was minimal evidence for dramatic breaking points during which drinking changes occur over college and at the transition out of college. This is consistent with a growing literature that suggests that drinking changes in young adulthood generally unfold gradually across time (e.g., Lee et al., 2015; Littlefield et al., 2009) We did find what appeared to be a few periods when changes took place across and even beyond the college years. Specifically, we observed differences between the two groups from the outset (i.e., at wave 1), at wave 10/11 two of our indices demonstrated joinpoints where those who develop AUD symptoms moderated their use, and near the end of the assessment window (i.e. wave 18) tended to be the largest difference between groups. Interestingly, these joinpoints did not appear to coincide with milestones that might be expected to alter drinking behaviors, such as entering the legal drinking age, or college graduation. Again, this pattern of findings suggests that changes in drinking occur slowly, and perhaps in response to a confluence of developmental changes, rather than any single milestone event.
More informative is the way in which our analysis sheds light on how specifically the groups diverged in their alcohol involvement across the five years of study. For example, two important inferences that can be drawn from our models even when examining the alcohol use indices without JPs, are that (1) the AUD and non-AUD groups had different initial levels of alcohol involvement over time, and (2) changed their degree of alcohol involvement at different rates. In short, the AUD group reported greater alcohol involvement from the first assessment and escalated their involvement at a more rapid pace. This suggests that longer-term risk is present early on in college, and presumably, intervention efforts geared toward deterring long-term alcohol use disorder risk may begin for those students who show early evidence of problematic drinking. In particular, greater escalation of drinking across college may serve as a “red flag” that early intervention may be warranted.
There were several limitations of this study that should be borne in mind when considering these findings. The first of these pertain to limitations of the sample. This sample consisted of students from a single university in one region of the United States. As such, these findings may not generalize to other students in other parts of the U.S. or the world. Further, these data cannot speak to maturing out processes in young adults who are not college students or those who remain in college (i.e., did not graduate). Also, the sample had limited demographic heterogeneity, and did not have strong enough representation of ethnic minorities to examine whether these processes may vary according to ethnicity. Related, we had more females than males in the current sample. However, there is no evidence in the extant literature that maturing out patterns differ between men and women, and the measures we used were designed to reduce gender bias, i.e., binge and heavy binge thresholds differ by gender, estimated typical and peak BAC calculations adjust for biological sex, and the consequences scale was designed to reduce gender bias. Second, our operationalization of “binge” and “heavy binge” were well suited to our research goals of characterizing alcohol use over time and comparing AUD and non-AUD groups; however, they are not amenable to inferences based on episodic heavy drinking. Moreover, we did not use a 2-hour time period restriction as part of our binge drinking definition and thus we cannot be certain that drinks were consumed within a 2-hour time period. Finally, the reliance on self-report data may have resulted in retrospective recall bias. Future studies can improve upon the approach used here with methods that allow for real-time data collection, such as ecological momentary assessment. The addition of observer reports could also enhance the reliability of self-report estimates of past drinking behavior.
The objective of this study was to delineate patterns of maturing out, and to determine whether these patterns differ between those who went on to develop AUD symptoms from those who did not. As such, our study was not designed to test mechanisms of maturing out. Thus, we cannot say what it is about these particular drinking behaviors that may lead to risk. Linking patterns that we identified here to specific predictors could be an interesting direction for future research. For example, a nascent literature has begun to examine affective or motivational processes that may account for or portend longer-term problem use (Littlefield et al., 2010; Patrick & Schulenberg, 2011). Therefore, the emergence of coping motivations may be a marker of failure to “mature out” of heavy drinking at this juncture. Other factors that could shed light on the “maturing out” process are specific individual-level characteristics that are associated with alcohol involvement (e.g., sensation seeking, family history), as well as developmental context factors that may influence changes in drinking in young adulthood (e.g., employment, marriage, parenting). As we did not find clear evidence that joinpoints could be readily linked to specific developmental periods or events, it would seem that, rather than looking to single predictors, the field may instead benefit from a broader consideration of multiple changing circumstances that may act in concert to shape drinking changes in young adulthood.
Lastly, though we used self-report of DSM alcohol use disorder symptoms to classify participants and plot trajectories, we did not use a diagnostic assessment of alcohol use disorder. Though self-report of alcohol use and problems has been shown to yield reliable information about these behaviors in young adults and other samples (e.g., Maisto et al., 2008), interview methods remain the gold standard for formulating diagnoses.
Clinical Implications
These findings may have important implications for campus-based counselors, administrators, or interventionists. Though a number of interventions have been developed to prevent problem drinking and related consequences as students transition into the college environment (e.g., Alcohol 101 Plus™, The Century Council, 2003), to our knowledge, there are no such interventions geared toward a successful transition out of college and into the next phase of adulthood. Future work identifying mechanisms of successful transition into adult roles will be important in the formulation of specific recommendations for such interventions were they to be developed. For example, a brief motivational intervention (BMI) might be developed to be administered to students as they approach the end of college. This intervention could help students to anticipate some of the challenges ahead as they transition from the college environment, emphasizing the ways in which current drinking may portend longer-term problems. These interventions could build on current best intervention practices for college drinking (e.g., BASICS; Dimeff, 1999).
Our findings also point to critical periods during which screening may be optimally timed. First, we found that differences between those who do and do not develop alcohol problems post-college are evident early on. This suggests that intervention to prevent long-term risk could be initiated early in college and/or individuals showing evidence of these problems may be prioritized for intervention as they begin to prepare for college graduation. Specifically, our data reveal that initial differences in alcohol use of even 2 drinks per occasion (i.e., 4 drinks vs. 2 drinks per occasion) may be indicative of added risk for going on to develop AUD symptoms. Our findings also suggest that clinicians should monitor the progression of alcohol use, with those whose alcohol use increases more rapidly being at greater risk than for those students whose alcohol use remains stable. Finally, we found that the biggest differences between the groups with regard to problematic drinking. Thus, clinicians should be screening for alcohol related consequences and be aware that students who report even moderate levels of alcohol consumption combined with self-reports of alcohol related consequences will be at greater risk of developing AUD symptoms.
We also identified two additional points of interest that may be of interest for clinicians working with college student drinkers. In the middle of college (waves 10 & 11 in the current study) was a point where heavy drinking students showed signs of moderating their use. This assessment period coincides with a time when the newness of college may have worn off, friendship groups have been established, and engagement in coursework and extracurricular activities may increase or intensify. Any or all of these factors may contribute to a diminution - albeit temporary - in alcohol involvement. Though not necessarily a critical developmental period, our results suggest that that this may be a time of reevaluation for students with regard to their drinking practices. In this critical time, heavy drinking students may be more amenable to receiving an intervention, and it may be possible to help them bring their alcohol use to safer levels. Finally, we saw the biggest discrepancy between groups near the end of the assessment window (i.e., around wave 18). This suggests that it may be easiest to identify those students who are likely to have difficulty with the transition out of college due to alcohol related problems because their alcohol involvement will be more aberrant from their more well-adjusted peers. Interventions targeting the heaviest drinking college students could help ease the transition into adult roles. Clinicians may also recommend more intensive alcohol treatment to these students that extends beyond the college years.
Conclusions.
The current study demonstrated the value of using a multidimensional assessment of alcohol involvement in efforts to understand the clinical course of college drinking, especially as it relates to the development of AUD. We demonstrated that those with AUD after graduation drink differently throughout college compared to those who do not have an AUD after graduation. These results offer insights into the nuances of the differences in alcohol involvement for those who develop AUD and those who do not, and this has implications for screening, brief intervention, and treatment.
Acknowledgements.
This work was supported by the National Institute on Drug Abuse, Grant number R01DA018993 & Administrative Supplement: 3R01DA018993-05S1: Read, PI.
Funding: This work was supported by the National Institute on Drug Abuse, Grant #Z R01DA018993 & Administrative Supplement: 3R01DA018993-05S1: Read, PI. Mark A. Prince is supported by National Institute on Alcohol Abuse and Alcoholism Training Grant T32-AA007583.
Footnotes
Disclosure of potential conflicts of interest: The authors declare that they have no conflicts of interest.
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institution and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent: Informed consent was obtained from all individual study participants.
Contributor Information
Mark A. Prince, Department of Psychology, 1876 Campus Delivery, Colorado State University, Fort Collins, CO 80523;
Jennifer P. Read, University at Buffalo, Department of Psychology, Park Hall, #168, Buffalo, NY 14203.
Craig R. Colder, University at Buffalo, Department of Psychology, Park Hall, #168, Buffalo, NY 14203.
Reference
- Bachrach RL, & Read JP (2012). The role of posttraumatic stress and problem alcohol involvement in university academic performance. Journal of Clinical Psychology, 68, 843–859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett NP, Goldstein AL, Murphy JG, Colby SM, & Monti PM (2006). “I’ll never drink like that again”: Characteristics of alcohol-related incidents and predictors of motivation to change in college students. Journal of Studies on Alcohol, 67, 754–763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey KB, & Hustad JT (2002). Are retrospectively reconstructed blood alcohol concentrations accurate? Preliminary results from a field study. Journal of Studies on Alcohol, 63(6), 762–766. [DOI] [PubMed] [Google Scholar]
- Carter AC, Brandon KO, & Goldman MS (2010). The college and noncollege experience: a review of the factors that influence drinking behavior in young adulthood. Journal of Studies on Alcohol and Drugs, 71, 742–750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J (1988). Statistical power analysis for the behavioral sciences (Vol. 2). Hillsdale, NJ: Lawrence Earlbaum Associates. [Google Scholar]
- Collins RL, Parks GA, & Marlatt GA (1985). Social determinants of alcohol consumption: the effects of social interaction and model status on the self-administration of alcohol. Journal of consulting and clinical psychology, 53, 189–200. [DOI] [PubMed] [Google Scholar]
- Davis CM, & Clifford PR (2016, July 25). Ascertaining the Relationships Between the Trajectories of Specific Categories of Alcohol-Related Negative Consequences and Subsequent Drinking Behavior. Psychology of Addictive Behaviors. Advance online publication. 10.1037/adb0000181. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Grant BF, Stinson FS, & Chou SP (2004). Another look at heavy episodic drinking and alcohol use disorders among college and noncollege youth. Journal of Studies on Alcohol, 65, 477–488. http://www.jsad.com/jsad/articles/65/4797.html [DOI] [PubMed] [Google Scholar]
- Dimeff LA (Ed.). (1999). Brief alcohol screening and intervention for college students (BASICS): A harm reduction approach. Guilford Press. [Google Scholar]
- Hasin D, Paykin A, & Endicott J (2001). Course of DSM-IV Alcohol Dependence in a Community Sample: Effects of Parental History and Binge Drinking. Alcoholism: Clinical and Experimental Research, 25, 411–414. [PubMed] [Google Scholar]
- Hustad JTP, & Carey KB (2005). Using calculations to estimate blood alcohol concentrations for naturally occurring drinking episodes: A validity study. Journal of Studies on Alcohol, 66, 130–138. [DOI] [PubMed] [Google Scholar]
- Jackson KM (2008). Heavy episodic drinking: Determining the predictive utility of five or more drinks. Psychology of Addictive Behaviors, 22, 68–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG, & Schulenberg JE (2013). Monitoring the Future national survey results on drug use, 1975–2011. Volume II: College students and adults ages 19–50. Ann Arbor: Institute for Social Research, The University of Michigan. [Google Scholar]
- Kim HJ, Fay MP, Feuer EJ, Midthune DN, 2000. Permutation tests for joinpoint regression with applications to cancer rates. Stat. Med 19, 335–351 (correction: 2001;20:655). [DOI] [PubMed] [Google Scholar]
- Kim HJ, Fay MP, Yu B, Barrett MJ, and Feuer EJ (2004), Comparability of Segmented Line Regression Models, Biometrics, 1005–1014. [DOI] [PubMed] [Google Scholar]
- Lee MR, Chassin L, & MacKinnon DP (2015). Role transitions and young adult maturing out of heavy drinking: evidence for larger effects of marriage among more severe premarriage problem drinkers. Alcoholism: Clinical and Experimental Research, 39(6), 1064-1074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee MR, Ellingson JM, & Sher KJ (2015). Integrating social-contextual and intrapersonal mechanisms of “maturing out”: Joint influences of familial-role transitions and personality maturation on problem-drinking reductions. Alcoholism: Clinical and Experimental Research, 39(9), 1775–1787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Littlefield AK, Sher KJ, & Wood PK (2009). Is “maturing out” of problematic alcohol involvement related to personality change? Journal of Abnormal Psychology, 118, 360–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maggs JL, Schulenberg J, & Hurrelmann K (1997). Developmental transitions during adolescence: Health promotion implications In Schulenberg J, Maggs JL, & Hurrelmann K (Eds.), Health risks and developmental transitions during adolescence (pp. 522–546). New York, NY, US: Cambridge University Press. [Google Scholar]
- Maisto SA, Conigliaro JC, Gordon AJ, McGinnis KA, & Justice AC (2008). An experimental study of the agreement of self-administration and telephone administration of the Timeline Followback interview. Journal of Studies on Alcohol and Drugs, 69, 468–471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mallett KA, Lee CM, Neighbors C, Larimer ME, & Turrisi R (2006). Do we learn from our mistakes? An examination of the impact of negative alcohol-related consequences on college students’ drinking patterns and perceptions. Journal of Studies on Alcohol, 67, 269–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mallett KA, Varvil-Weld L, Borsari B, Read JP, Neighbors C, & White HR (2013). An update of research examining college student alcohol-related consequences: new perspectives and implications for interventions. Alcoholism: Clinical and Experimental Research, 37(5), 709–716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merrill JE, Read JP, & Barnett NP (2013). The way one thinks affects the way one drinks: Subjective evaluations of alcohol consequences predict subsequent change in drinking behavior. Psychology of Addictive Behaviors, 27, 42–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick ME, & Schulenberg JE (2011). How trajectories of reasons for alcohol use relate to trajectories of binge drinking: National panel data spanning late adolescence to early adulthood. Developmental psychology, 47(2), 311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polak MA, & Conner TS (2012). Impairments in daily functioning after heavy and extreme episodic drinking in university students. Drug and Alcohol Review, 31, 763–769. [DOI] [PubMed] [Google Scholar]
- Prince MA, & Maisto SA (2013). The clinical course of alcohol use disorders: Using joinpoint analysis to aid in interpretation of growth mixture models. Drug and alcohol Dependence, 133(2), 433–439. [DOI] [PubMed] [Google Scholar]
- Prince MA, Pearson MR, Bravo AJ, & Montes KS (2018). A quantification of the alcohol use-consequences association in college student and clinical populations: A large, multi-sample study. The American journal on addictions, 27(2), 116–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Read JP, Beattie M, Chamberlain R, & Merrill JE (2008). Beyond the “Binge” threshold: heavy drinking patterns and their association with alcohol involvement indices in college students. Addictive behaviors, 33(2), 225–234. [DOI] [PubMed] [Google Scholar]
- Read JP, Colder CR, Merrill JE, Ouimette P, White J, & Swartout A (2012). Trauma and posttraumatic stress symptoms predict alcohol and other drug consequence trajectories in the first year of college. Journal of Consulting and Clinical Psychology, 80(3), 426–439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Read JP, Kahler CW, Strong DR, & Colder CR (2006). Development and preliminary validation of the young adult alcohol consequences questionnaire. Journal of studies on alcohol, 67(1), 169–177. [DOI] [PubMed] [Google Scholar]
- Read JP, Merrill JE, Kahler CW, & Strong DR (2007). Predicting functional outcomes among college drinkers: Reliability and predictive validity of the Young Adult Alcohol Consequences Questionnaire. Addictive behaviors, 32, 2597–2610. [DOI] [PubMed] [Google Scholar]
- Read JP, Ouimette P, White J, Colder C, & Farrow S (2011). Rates of DSM-IV-TR trauma exposure and posttraumatic stress disorder among newly matriculated college students. Psychological Trauma: Theory, Research, Practice, and Policy, 3(2), 148–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Read JP, Wardell JD, & Bachrach RL (2013). Drinking consequence types in the first college semester differentially predict drinking the following year. Addictive behaviors, 38, 1464–1471. [DOI] [PubMed] [Google Scholar]
- Schulenberg JE, & Maggs JL (2002). A developmental perspective on alcohol use and heavy drinking during adolescence and the transition to young adulthood. Journal of Studies on Alcohol, Supplement, (14), 54–70. [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, … Dunbar GC (1998). The Mini-International Neuropsychiatric Interview (MINI): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of clinical psychiatry, 59(Suppl 20), 22–33. [PubMed] [Google Scholar]
- Slutske WS (2005). Alcohol use disorders among US college students and their non-college-attending peers. Archives of General Psychiatry, 62, 321–327. [DOI] [PubMed] [Google Scholar]
- Statistical Methodology and Applications Branch and Data Modeling Branch, Surveillance Research Program National Cancer Institute, 2011. Joinpoint Regression Program, Version 3.5. http://surveillance.cancer.gov/joinpoint
- The Century Council (2003). Alcohol 101 Plus [Computer software]. Retrieved from http://www.alcohol101plus.org/home.html.
- Vergés A, Haeny AM, Jackson KM, Bucholz KK, Grant JD, Trull TJ, Wood PK,& Sher KJ (2013). Refining the notion of maturing out: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. American Journal of Public Health, 103, e67–e73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler H, Davenport A, Dowdall G, Moeykens B, & Castillo S (1994). Health and behavioral consequences of binge drinking: A national survey of students at 140 campuses. JAMA, 272, 1672–1677. [PubMed] [Google Scholar]
- Wechsler H, Dowdall GW, Davenport A, & Rimm EB (1995). A gender-specific measure of binge drinking among college students. American journal of public health, 85(7), 982–985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White AM, Kraus CL, & Swartzwelder HS (2006). Many college freshmen drink at levels far beyond the binge threshold. Alcoholism: Clinical and Experimental Research, 30(6), 1006–1010. [DOI] [PubMed] [Google Scholar]
- Wood MD, Read JP, Palfai TP, & Stevenson JF (2001). Social influence processes and college student drinking: the mediational role of alcohol outcome expectancies. Journal of studies on alcohol, 62(1), 32–43. [DOI] [PubMed] [Google Scholar]
- Yu B, Barrett M, Kim H-J, Feuer EJ, 2007. Estimating joinpoints in continuous time scale for multiple change-point models. Comput. Stat. Data. Anal 51, 2420–2427. [Google Scholar]