Abstract
Introduction
Adolescent substance use is a major public health concern since it enhances adolescent morbidity and mortality, affecting adulthood health and well-being. Although current evidence shows a high risk for substance use among transgender populations, to date, few studies evaluate substance use among transgender youth.
Method
Brazilian transgender youth (ages between 16 and 25 years old) answered an online questionnaire measuring demographics, substance use and modifiable factors associated with drug use to deal with general stress, gender-related stress, and recreational use.
Results
Cannabis was the most frequent substance used among transgender youth (20.88%; CI 95% 23.71–36.19), whereas 11.45% (CI 95% 11.38–21.47) of volunteers disclosed use of pain medication, such as codeine, and 5.05% (CI 95% 3.71–10.78) revealed use of sedatives and tranquilizers in the last 30 days. ADH medication (not prescribed), as well as cocaine and other drugs (such as antihistamines and Hookah), was also reported by 2.36% (CI 95% 0.92–5.84), 2.69% (CI 95% 1.24–6.49) and 4.04% (CI 95% 2.61–8.98) of transgender youth.
Conclusion
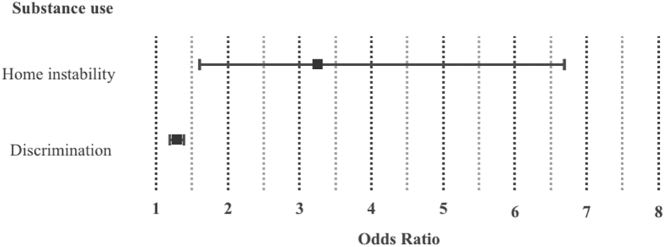
A logistic regression model showed that discrimination and home instability were the primary determinants of vulnerable to substance use among youth. Therefore, the harm reduction strategies must affect the social and physical aspects of transgender youth lives.
Keywords: Transgender youth, Young transgender men, Young transgender women, Gender diverse youth, Substance use, Drug use, Minority stress theory
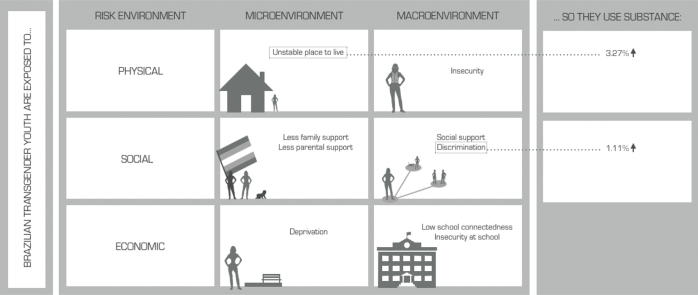
Graphical abstract
Highlights
-
•
Around 60% of Brazilian transgender youth reported using Cannabis.
-
•
One-third of Brazilian transgender youth utilized pain medications.
-
•
Tranquilizers, cocaine and ADHD medications were utilized by 14.1%, 8.1% and 7.1% of youth.
-
•
Discrimination and home instability were the primary determinants of substance harm among youth.
Substance use among adolescents is a major public health concern since it enhances adolescent morbidity and mortality, affecting adulthood health and well-being. Furthermore, early age of initial use increases the chances of addiction later in life (Grant, Stinson, & Harford, 2001), impairs decision making (Dom, Sabbe, Hulstijn, & Van Den Brink, 2005), and increases HIV exposure (Solorio, Swendeman, & Rotheram-Borus, 2003). Bearing in mind the adverse social, physical and emotional costs that substance use during adolescence causes, it is of great importance to identify groups, such as transgender youth, that are especially vulnerable to substance use, as well as further explore modifiable factors associated to substance use. Transgender adolescents and young adults endure many challenges related to stigma and discrimination: from subtle (such as barriers to access health care (Costa et al., 2016)) to explicit aggressions (i.e., homicide (Balzer, Hutta, Adrián, & Hyndal, 2012)). Furthermore, they report more frequent episodes of psychological distress, self-harm, depression symptoms, and suicide both ideation and attempts when compared to their cisgender peers (Veale et al., 2015). As exposition to discrimination (Clark, Salas-wright, Vaughn, & Whitfiled, 2015; Reisner, Greytak, Parsons, & Ybarra, 2014), mental health symptoms also have been associated to substance use among adolescents (Lai, Cleary, Sitharthan, & Hunt, 2015). Therefore, it is crucial to further explore substance use among transgender youth.
Although current evidence shows a high risk for substance use among transgender populations, to date, few studies evaluate substance use among transgender youth (Day, Fish, Perez-Brumer, Hatzenbuehler, & Russell, 2017; Reisner et al., 2015). Accordingly, a statewide cross-sectional sample of California middle and high schools evaluated, between 2013 and 2015, 335 transgender and 31.737 cisgender aged 16 to 25 years and verified that the lifetime prevalence of cannabis and multiple drugs use was 2.5 times higher for transgender youth. These findings were consistent with other studies (Garofalo, Deleon, Osmer, Doll, & Harper, 2006). Concerning specifically other drugs use prevalence among transgender youth, such as nonmedical use of prescription pain medication, inhalants, diet pills, Attention Deficit Hyperactivity Disorder (ADHD) medication, and cold medicine, there is exclusively one research available (De Pedro, Gilreath, Jackson, & Esqueda, 2017). De Pedro et al. (2017) performed a secondary data analysis from 2013 to 2015 California Healthy Kids Survey and verified that transgender students were about three times more likely to use cocaine, methamphetamine, inhalant drugs, and prescription pain medication when compared to cisgender peers.
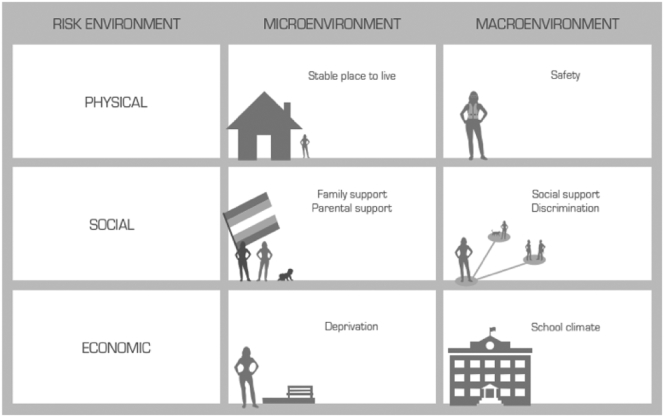
Nevertheless, transgender youth are not ipso facto “risky” populations (Gilbert, Pass, Keuroghlian, Green, & Reisner, 2018). “Risk environment” framework shows drug harm as result of social situations and, thus, changes the main responsibility, as well as the focus of harm-reducing actions, from individual to social perspective (Editorial, 2009). A “risk environment” comprises physical, social, economic and policy aspects that interact in micro and macro environmental levels, creating a place where harm has more chances to occur. Besides describing types of environment (physical, social, economic, policy) and levels of environment influence (micro and macro), “risk environment” framework also includes mechanisms of environment influence (susceptibility and vulnerability). Susceptibility refers to factors that determine the rate at which an epidemic is propagated, whereas vulnerability describes characteristics of a social or economic entity that make it more likely to present a particularly increased morbidity and mortality associated with disease (Barnett, Whiteside, Khodakevich, & Kruglov, 2000). Transgender youth are especially susceptible and vulnerable to substance use due to physical, social, economic and policy factors. Accordingly, a 2013 meta-analysis – that evaluated 12 studies assessing substance use among LGB youth (from 12 to 25 years old) – verified that the strongest risk factors for drug use were victimization, lack of supportive environments, psychological stress, negative disclosure reactions, and housing status (Goldbach & Gibbs, 2015; Goldbach, Tanner-Smith, Bagwell, & Dunlap, 2014). In addition, hostile school environments (Tharp-Taylor, Haviland, & D'Amico, 2009) and gender minority social stress (Reisner et al., 2015) contribute to substance use among LGBT youth. Substance use among transgender youth may be especially deleterious since they face difficulties to access health services (Costa et al., 2016; Reisner et al., 2015) and to mobilize network support when necessary (Seibel et al., 2018). Thus, “risk environment” plays a vital role in substance use among transgender youth. See Fig. 1.
Fig. 1.
Risk environments. A “risk environment” plays an important role in substance use among transgender youth. Physical (such as having a stable place to live and feeling safe around the city) as well as social (family, parental and social support) and economic (deprivation and school climate) aspects were assessed in the present study.
Adolescents and young adults use substances for many reasons, including recreational and social motives as well as to cope with stress. Different justifications usually mean diverse drug types and patterns of use (Boys, Marsden, Griffiths, Stillwell, & Strang, 1999; Hyman & Sinha, 2009). For example, cope with stress is one of the main reasons to use cannabis and utilizing cannabis to deal with stress is more frequent among heavier users (Hyman & Sinha, 2009).
Transgender youth endure stressful situations. According to Minority Stress Theory (Meyer, 2003), belonging to a minority group increases experiences of prejudice, expectations of prejudice, concealment of one's minority status, and internalization of social stigma. Meyer suggested three main processes by which LGB persons suffer minority stress (Meyer, 1995). First, environmental events, such as verbal harassment and physical assault, resulting from the LGB minority status. Second, the constant anticipation for external events to occur, causing LGB to avoid specific situations. Third, internalized homophobia. These three processes result in poorer health outcomes. The Minority Stress Model was previously applied for transgender persons (Hendricks & Testa, 2012) and substance abuse was studied as a mental health outcome of experiencing chronic stress (Reisner et al., 2014). Brazil has one of the highest transgender homicide numbers in the world (Balzer et al., 2012) and, in addition to explicit violence, transgender individuals still encounter barriers motivated by direct or indirect discrimination to access basic services (Costa et al., 2018).
Therefore, the present study aims to evaluate the impact of a “risk environment” on substance use specifically to deal with gender and general stress-related situations among Brazilian transgender youth.
1. Methods
From February to April 2018, an online Facebook announcement was displayed for users of Facebook who indicated the following characteristics in their profiles: live in Brazil; ages between 16 and 25 years old; and “liked” pages on Facebook and joined groups or events related to transsexuality, transgender and gender diverse individuals and the LGBT movement. Facebook statistics indicated that the advertisement had 45,741 impressions (number of times the advertisement was shown on the site), with 627 advertisement clicks. The click rate was calculated dividing the total measured clicks by the total measured advertisement impressions. It indicated that 1.37% of the impressions drove individuals to the main page of the study.
1.1. Inclusion criteria
The inclusion criteria were 1) identifying as transgender women, transgender men or gender diverse youth, 2) ages between 16 and 25 years old, 3) living in Brazil, and 4) answered all questions concerning drug use.
1.2. Measures
The survey was modeled after the TransYouth CAN! Project (see http://transyouthcan.ca/). TransYouth CAN! is a 9-clinical 2-year cohort study that will document sociodemographic and health-related characteristics of Canadian transgender youth and their parents or caregivers. The procedure for cross-cultural adaptation of the instrument for Brazilian populations was based on Borsa, Damásio, and Bandeira (2012) (Borsa et al., 2012), according to the following steps: (1) contextual equivalence and review by expert committee; (2) translation; (3) evaluation by the target audience; and (4) evaluation by the original authors of the instrument. For this study, the survey was adapted for use in the Brazilian population by a group of health practitioners who worked in gender and sexuality diversity and who were assessed by Brazilian transgender and gender diverse community members.
The Brazilian version of TransYouth CAN! questionnaire was grouped into 14 categories: (1) about you; (2) gender experiences; (3) accessing gender affirming care; (4) your live situation; (5) your social world; (6) school experiences; (7) your family; (8) community, support and discrimination; (9) relationships, romance and intimacy; (10) your health and well-being; (11) substance use; (12) your mental well-being; (13) taking care of yourself; and (14) sharing your thoughts.
1.2.1. Gender identity
Gender identity was assessed by the two questions method (Sausa, Sevelius, Keatley, Iñiguez, & Reyes, 2009). The first question concerns the gender assigned at birth and the second question focus on how the participants describe their gender identity. Participants were included if they reported a gender different from the one assigned to them at birth (Bauer, Braimoh, Scheim, & Dharma, 2017). Based on their self-reported gender identity, participants were re-categorized as young transgender women, young transgender men, and gender diverse youth. Young transgender women were those who were assigned as male at birth but identified as women, transgender women or travestis. Young transgender men were those who were assigned as female at birth but identified as men or transgender men. Finally, gender diverse youth were those who identified with a gender identity outside the binaries (male and female), such as queer, non- binary, a-gender, etc.
1.2.2. Substance use
Adapted from TransYouth CAN! survey, participants answered whether, in the last 30 days, they had used any substance, including cannabis and medications that were not prescribed. If they reported use of substances, they were invited to fulfill a list containing all substances utilized in the last 30 days. Among them, cannabis, mushrooms, spice, sizzurp, adrenochromes, poppers or nitrites, crack, cocaine, crystal meth, PCP, ketamine, GHB, LSD, opium, heroin, ecstasy, bath salts, fentanyl, other pain medication (besides fentanyl), sedatives or tranquilizers that were not prescribed, ADHD medication that were not prescribed, huffing gas or other solvents, and other drugs. Finally, they were inquired if the use of substance was to alleviate gender-related stress or general stress, and recreational use.
1.2.3. Physical aspects
Participants responded “Do you feel like you have a stable place to live?” with “yes” or “no” options. Furthermore, volunteers answered whether they feel safe in their neighborhood, in their home, and in public transportation during day and night using a five levels Likert scale from “totally insecure” to “completely secure”.
1.2.4. Social aspects
The Self-Report Family Inventory evaluates families through five domains: health or competence, conflict, cohesion, leadership, and emotional expressiveness (Beavers & Hampson, 2000; Goodrich, Selig, & Trahan, 2012). It is composed of 36 items answered with a five items Likert-type scale. In particular, the health or competence subscale comprises 19 items that encompass family affection, parental coalitions, problem-solving abilities, autonomy and individuality, optimistic versus pessimistic views, and acceptance of family members. The conflict subscale includes 12 items involving overt versus covert arguing. The cohesion subscale is composed of five items that focus on aspects associated with family togetherness and satisfaction with, for example, time spent together. The leadership subscale consists of three items concerning parental leadership. Finally, the emotional expressiveness subscale comprises six items involving expressions of caring and closeness. The inventory exhibited a satisfactory internal consistency with Cronbach alphas varying from 0.84 to 0.93 and test–retest reliabilities of 0.85 or better (Beavers & Hampson, 2000; Beavers, Hampson, & Hulgus, 1985).
Parental support for gender identity also was part of TransYouth CAN! survey. It evaluated parental support by inquiring “in general, how supportive of your gender identity or expression is your mother?” and “in general, how supportive of your gender identity or expression is your father?”. A four-item Likert-type scale, varying from “not at all supportive” to “very supportive”, was used for both questions.
The MOS Social Support Survey is composed of four domains (Sherbourne & Stewart, 1991): emotional or informational support, tangible support, affectionate support, and positive social interaction. All questions were answered with a five-items Likert-type scale. The emotional or informational support subscale included eight questions concerning having someone to talk and share personal problems. The tangible support subscale encompasses four questions about actually having help in case of a disease. The affectionate support subscale is composed of three items involving having someone that shows love and makes them feel wanted. Finally, the positive social interaction subscale includes three items concerning having someone to share happy moments. The MOS social support survey internal consistency reliability was good with Cronbach alpha coefficients varying from 0.86 to 0.92 (Sherbourne & Stewart, 1991).
The discrimination scale was developed by TransYouth CAN! Team. It is composed of nine questions evaluating previous experiences of discrimination, for example, “because of who you are, have you been called names or heard/saw your identity used as an insult?”. A four-point Likert-type scale was used to answer each question, and it ranged from “never” to “yes, many times in the past year”.
1.2.5. Economic aspects
The Deprivation Scale was developed by TransYouth CAN! Team in order to verify transgender youth access to basic needs. It is composed of five questions each one with a five-point Likert scale from “never” to “always”. For example, “in the last 12 months, how often did you have access to school supplies (like a school bag, notebooks, pencils, etc.) if and when you need them?”
The School Connectedness is composed of five statements that can be answered with a four-point Likert-type scale ranging from “strongly agree” to “strongly disagree”. For example, “I am happy to be at this school” and “the teachers at this school treat students fairly” (Mcneely, Nonnemaker, & Blum, 2002). The safety at school items were adapted from the Trans Youth Survey and BC Adolescent Health Survey by TransYouth CAN! Team (Veale et al., 2015). It contains seven questions concerning school places were the youth may or may not feel safe, such as, “while at school, how often do you feel safe in your classroom?”. The sentences are answered with a five-point Likert-type scale ranging from “never” to “always”.
1.3. Statistical analysis
SPSS software version 18.0 was used for data management and statistical analyses. Exclusively participants who answered the questions concerning substance use in the last month were included in the statistical analysis. First, respectively for categorical and continuous variables Pearson chi-square and ANOVA tests were applied to compare young transgender men, young transgender women and gender diverse youth' general characteristics and the substance used. Second, Pearson chi-square and ANOVA tests were applied to compare respectively categorical and continuous sociodemographic characteristics, substance used and modifiable factors variables among three groups: transgender youth who use substance to deal with gender-related stress, who use substance exclusively to deal with general stress and who use substance exclusively with recreational intention. Tukey's honestly significant difference (HSD) post hoc test was applied after the ANOVA test. Since the same volunteer could report drug use for more than one reason, all the participants that selected gender-related stress were categorized in the first group independently of using substance to also deal with general stress or to have fun. Finally, a multinomial logistic regression model was performed to assess the impact of each modifiable factor that presented p < .05 in Pearson chi-square or ANOVA tests when comparing the three groups of substance use (to deal with gender-related stress, exclusively to deal with general stress and only with recreational purpose).
2. Results
2.1. General characteristics and substance use among young transgender men, young transgender women and gender diverse youth
As shown in Table 1, participants have an average of 18.61 (95% CI 18.27–18.95) years. Young transgender women (19.83 years; 18.96–20.71) were older than young transgender men (18.32 years; 95% CI 17.83–18.08) and gender diverse youth (18.24 years; 17.70–18.78) (p = .001); the gender identity groups did present statistically significant differences when comparing, through Pearson chi-square and ANOVA tests, other characteristics. Briefly, the sample was mainly composed by Caucasian (62.03%; CI 95% 54.46–69.59) transgender men (46.97%; CI 95% 40.02–53.92) who live in cities (76.81%; CI 95% 71.06–82.56) from Southeast Brazil (44.78%; CI 95% 37.90–51.65).
Table 1.
General characteristics of young transgender men and women and gender diverse youth.
| Variables | Total |
Young transgender men |
Young transgender women |
Gender diverse youth |
p | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | 95% CI | Mean | SD | 95% CI | Mean | SD | 95% CI | Mean | SD | 95% CI | ||
| Age | 18.61 | 2.47 | 18.27–18.95 | 18.32 | 2.38 | 17.83–18.08 | 19.83 | 2.80 | 18.96–20.71 | 18.24 | 2.14 | 17.70–18.78 | .001a, b |
| N | % | 95% CI | N | % | 95% CI | N | % | 95% CI | N | % | 95% CI | ||
| Ethnicity | 158 | 71 | 38 | 49 | .305c | ||||||||
| White | 98 | 62.03 | 54.46-69.59 | 48 | 67.61 | 56.72–78.49 | 20 | 52.63 | 36.76–68.51 | 30 | 61.22 | 47.58–74.87 | |
| Non-white | 60 | 37.97 | 30.41–45.54 | 23 | 32.39 | 21.51–43.28 | 18 | 47.37 | 31.49–63.24 | 19 | 38.78 | 25.13–52.42 | |
| School | 207 | 97 | 44 | 66 | .364c | ||||||||
| Studying | 130 | 62.80 | 56.22–69.39 | 63 | 64.95 | 55.45–74.44 | 30 | 68.18 | 54.42–81.94 | 37 | 56.06 | 44.09–68.03 | |
| Not studying | 77 | 37.20 | 30.61–43.78 | 34 | 35.05 | 25.56–44.55 | 14 | 31.82 | 18.06–45.58 | 29 | 43.94 | 31.97–55.91 | |
| Local of residence | 207 | 97 | 44 | 66 | |||||||||
| City | 159 | 76.81 | 71.06–82.56 | 69 | 71.13 | 62.12–80.15 | 39 | 88.64 | 79.26–98.01 | 51 | 77.27 | 67.16–87.38 | .312c |
| Suburb | 37 | 17.87 | 12.66–23.09 | 20 | 20.62 | 12.57–28.70 | 4 | 9.09 | 0.60–17.59 | 13 | 19.70 | 10.10–29.29 | |
| Rural area | 6 | 2.90 | 0.61–5.18 | 4 | 4.12 | 0.17–8.08 | 1 | 2.27 | 2.13–6.67 | 1 | 1.52 | 1.40–4.46 | |
| Do not know | 5 | 2.42 | 0.32–4.51 | 4 | 4.12 | 0.17–8.08 | 0 | 0.00 | 0.00–0.00 | 1 | 1.52 | 1.40–4.46 | |
| Brazil region | 201 | 93 | 43 | 65 | .765c | ||||||||
| North | 9 | 4.48 | 1.62–7.34 | 5 | 5.38 | 0.79–9.96 | 2 | 4.65 | 1.64–10.95 | 2 | 3.08 | 1.12–7.27 | |
| Northeast | 25 | 12.44 | 7.88–17.00 | 10 | 10.75 | 4.467–17.05 | 6 | 13.95 | 3.60–24.31 | 9 | 13.85 | 5.45–22.24 | |
| Central-West | 15 | 7.46 | 3.83–11.10 | 4 | 4.30 | 0.18–8.42 | 4 | 9.30 | 0.62–17.98 | 7 | 10.77 | 3.23–18.30 | |
| Southeast | 90 | 44.78 | 37.90–51.65 | 41 | 44.09 | 34.00–54.18 | 18 | 41.86 | 27.12–56.61 | 31 | 47.69 | 35.55–59.83 | |
| South | 62 | 30.85 | 24.46–37.23 | 33 | 35.48 | 25.76–45.21 | 13 | 30.23 | 16.51–43.96 | 16 | 24.62 | 14.14–35.09 | |
Note. Sample size varied according to the question because participants had the possibility to skip sections of the survey. Bold = p < .05.
ANOVA test.
According to Turkey posthoc test, the differences were between young transgender women and young transgender men, as well as between transgender women and gender diverse youth.
Chi-square test.
The substance use did not vary significantly among gender identity groups. As shown in Table 2, cannabis was the most frequent substance used among transgender youth: 20.88% (CI 95% 23.71–36.19) of participants, and 63.9% of transgender youth who reported drug use, confessed use of cannabis it in the previous month. Considering the total sample, 11.45% (CI 95% 11.38–21.47) of volunteers disclosed the use of pain medication, such as codeine, whereas 5.05% (CI 95% 3.71–10.78) revealed the use of sedatives and tranquilizers in the last 30 days. ADH medication (not prescribed), as well as cocaine and other drugs (such as antihistamines and Hookah), was also reported by 2.36% (CI 95% 0.92–5.84), 2.69% (CI 95% 1.24–6.49) and 4.04% (CI 95% 2.61–8.98) of transgender youth.
Table 2.
Substance use by gender identity.
| Substances | Total |
Young transgender men |
Young transgender women |
Gender diverse youth |
p | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 207 |
97 |
44 |
66 |
||||||||||
| N | % | 95% CI | N | % | 95% CI | N | % | 95% CI | N | % | 95% CI | ||
| Cannabis | 62 | 20.88 | 23.71–36.19 | 31 | 31.96 | 22.68–41.24 | 13 | 29.55 | 16.06–43.03 | 18 | 27.27 | 16.53–38.02 | .812b |
| Mushrooms | 1 | 0.34 | 0.46-1.43 | 1 | 1.03 | 0.98–3.04 | 0 | 0.00 | 0.00–0.00 | 0 | 0.00 | 0.00–0.00 | .566b |
| Cocaine | 8 | 2.69 | 1.24-6.49 | 4 | 4.12 | 0.17–8.08 | 2 | 4.55 | 1.61–10.70 | 2 | 3.03 | 1.11–7.17 | .907b |
| LSD | 5 | 1.68 | 0.32-4.51 | 4 | 4.12 | 0.17–8.08 | 0 | 0.00 | 0.00–0.00 | 1 | 1.52 | 1.43–4.46 | .284b |
| Fentanyl | 1 | 0.34 | 0.46-1.43 | 0 | 0.00 | 0.00–0.00 | 1 | 2.27 | 2.13–6.68 | 0 | 0.00 | 0.00–0.00 | .155b |
| Other pain medication besides fentanyl | 34 | 11.45 | 11.38–21.47 | 15 | 15.46 | 8.27–22.66 | 4 | 9.09 | 0.60–17.59 | 15 | 22.73 | 12.62–32.84 | .157b |
| Sedatives or tranquilizers | 15 | 5.05 | 3.71–10.78 | 8 | 8.25 | 2.77–13.72 | 3 | 6.82 | 0.63–14.27 | 4 | 6.06 | 0.30–11.82 | .863b |
| ADHD medicationsa | 7 | 2.36 | 0.92–5.84 | 4 | 4.12 | 0.17–8.08 | 1 | 2.27 | 2.13–6.68 | 2 | 3.03 | 1.11–7.17 | .838b |
| Huffing gas and other solvents | 2 | 0.67 | 0.37–2.30 | 0 | 0.00 | 0.00–0.00 | 0 | 0.00 | 0.00–0.00 | 2 | 3.03 | 1.11–7.17 | .116b |
| Other drugs | 12 | 4.04 | 2.61–8.98 | 5 | 5.15 | 0.75–9.55 | 4 | 9.09 | 0.60–17.59 | 3 | 4.55 | 0.48–9.57 | .566b |
Note. Sample size varied according to the question because participants had the possibility to skip sections of the survey.
That were not prescribed.
Chi-square test.
2.2. General characteristics and reasons to use substances among transgender youth
As shown in Table 3, general characteristics did not differ among transgender youth who used substances to deal with gender-related stress, to endure general stress, to “have fun” and who did not report substance use.
Table 3.
General characteristics of transgender youth separated by reason to use substance.
| Variables | Substance use to… |
Did not report substance use |
p |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| … deal with gender-related stress |
... deal with general stress |
... recreational purposes |
|||||||||||
| 53 |
21 |
36 |
|||||||||||
| Mean | SD | 95% CI | Mean | SD | 95% CI | Mean | SD | 95% CI | Mean | SD | 95% CI | ||
| Age | 18.32 | 2.30 | 17.69–18.96 | 18.71 | 2.88 | 17.40–20.03 | 18.94 | 2.65 | 18.05–19.84 | 18.64 | 2.47 | 18.10–1918 | .708a |
| N | % | 95% CI | N | % | 95% CI | N | % | 95% CI | N | % | 95% CI | ||
| Gender identity | 54 | 100.00 | – | 21 | 100.00 | – | 37 | 100.00 | 86 | 100.00 | .717a | ||
| Young transgender men | 24 | 44.44 | 31.19–57.70 | 10 | 47.62 | 26.26–68.98 | 18 | 48.65 | 32.54–64.75 | 41 | 47.67 | 37.12–58.23 | |
| Young transgender women | 16 | 29.63 | 17.45–41.81 | 3 | 14.29 | 0.68–29.25 | 7 | 18.92 | 6.30–31.54 | 16 | 18.60 | 10.38–26.83 | |
| Gender diverse youth | 14 | 25.93 | 14.24–37.61 | 8 | 38.10 | 17.33–58.87 | 12 | 32.43 | 17.35–47.52 | 29 | 33.72 | 23.73–43.71 | |
| Ethnicity | 41 | 100.00 | 64.52–87.33 | 18 | 100.00 | – | 35 | 100.00 | – | 61 | 100.00 | – | .554a |
| White | 24 | 58.54 | 43.46-73.62 | 10 | 55.56 | 32.60–78.51 | 20 | 57.14 | 40.75–73.54 | 42 | 68.85 | 57.23–80.47 | |
| Non-white | 17 | 41.46 | 26.38–56.54 | 8 | 44.44 | 21.49–67.40 | 15 | 42.86 | 26.46–59.25 | 19 | 31.15 | 19.53–42.77 | |
| School | 54 | 100.00 | – | 22 | 100.00 | – | 37 | 100.00 | – | 87 | 100.00 | – | .211a |
| Studying | 36 | 66.67 | 54.09-79.24 | 11 | 50.00 | 29.11–70.89 | 20 | 54.05 | 38.00–70.11 | 60 | 68.97 | 59.24–78.69 | |
| Not studying | 18 | 33.33 | 20.76–45.91 | 11 | 50.00 | 29.11–70.89 | 17 | 45.95 | 29.89–62.00 | 27 | 31.03 | 21.31–40.76 | |
| Local of residence | 54 | 100.00 | – | 22 | 100.00 | – | 37 | – | 87 | 100.00 | – | .051a | |
| City | 42 | 77.78 | 66.69-88.87 | 17 | 77.27 | 59.76–94.78 | 35 | 94.59 | 87.31–101.88 | 60 | 68.97 | 59.24–78.69 | |
| Suburb | 11 | 20.37 | 9.63–31.11 | 3 | 13.64 | 0.70–27.98 | 1 | 2.70 | 2.52–7.93 | 20 | 22.99 | 14.15–31.83 | |
| Rural area | 1 | 1.85 | 1.74–5.45 | 0 | 0.00 | 0–0 | 1 | 2.70 | 2.52–7.93 | 4 | 4.60 | 0.20–9.00 | |
| Do not know | 0 | 0.00 | 0–0 | 2 | 9.09 | 2.92–21.10 | 0 | 0.00 | 0–0 | 3 | 3.45 | 0.39–7.28 | |
| Brazil region | 51 | 100.00 | – | 22 | 100.00 | – | 36 | 100.00 | – | 85 | 100.00 | – | .411a |
| North | 4 | 7.84 | 0.46-15.22 | 3 | 13.64 | 0.70–27.98 | 0 | 0.00 | 0.00–0.00 | 2 | 2.35 | 0.87–5.58 | |
| Northeast | 3 | 5.88 | 0.57–12.34 | 4 | 18.18 | 2.06–34.30 | 4 | 11.11 | 0.85–21.38 | 12 | 14.12 | 6.72–21.52 | |
| Central-West | 5 | 9.80 | 1.64–17.97 | 1 | 4.55 | 4.16–13.25 | 3 | 8.33 | 0.70–17.36 | 6 | 7.06 | 1.61–12.50 | |
| Southeast | 25 | 49.02 | 35.30–62.74 | 9 | 40.91 | 20.36–61.45 | 18 | 50.00 | 33.67–66.33 | 36 | 42.35 | 31.85–52.86 | |
| South | 14 | 27.45 | 15.20–39.70 | 5 | 22.73 | 5.22–40.24 | 11 | 30.56 | 15.51–45.60 | 29 | 34.12 | 24.04–44.20 | |
Note. Sample size varied according to the question because participants had the possibility to skip sections of the survey. Bold = p < .05.
Chi-square test.
Table 4 summarizes the drug used according to the justification (to deal with gender-related stress, to endure general stress, and to “have fun”). The only substance that differed significantly among groups was sedatives (p = .021): tranquilizers were mainly utilized by transgender youth to deal with gender-related stress (22.22% vs. 9.09% and 2.70%).
Table 4.
Substances that transgender youth reported use according to justification.
| Substance | Substance use to… |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| … deal with gender-related stress |
... deal with general stress |
... recreational purposes |
p | |||||||
| 54 |
22 |
37 |
||||||||
| N | % | 95% CI | N | % | 95% CI | N | % | 95% CI | ||
| Cannabis | 31 | 57.41 | 48.290–66.52 | 15 | 68.18 | 48.72–87.64 | 17 | 45.95 | 29.89–62.00 | .237a |
| Mushrooms | 0 | 0.00 | 0-0 | 1 | 4.55 | 4.16–13.25 | 0 | 0.00 | 0.00–0.00 | .124a |
| Cocaine | 3 | 5.56 | 1.33-9.78 | 3 | 13.64 | 0.70–27.98 | 2 | 5.41 | 1.88–12.69 | .409a |
| LSD | 3 | 5.56 | 1.33-9.78 | 2 | 9.09 | 2.92–21.10 | 0 | 0.00 | 0–0 | .222a |
| Fentanyl | 0 | 0.00 | 0.00–0.00 | 0 | 0.00 | 0.00–0.00 | 1 | 2.70 | 2.52–7.93 | .355a |
| Other pain medication besides fentanyl | 13 | 24.07 | 16.19–31.96 | 6 | 27.27 | 8.66–45.88 | 15 | 40.54 | 24.72–56.36 | .231a |
| Sedatives or tranquilizers | 12 | 22.22 | 14.56–29.89 | 2 | 9.09 | 2.92–21.10 | 1 | 2.70 | 2.52–7.93 | .021a |
| ADHD medicationsa | 6 | 11.11 | 5.32–16.91 | 0 | 0.00 | 0–0 | 1 | 2.70 | 2.52–7.93 | .107a |
| Huffing gas and other solvents | 1 | 1.85 | 0.63–4.34 | 1 | 4.55 | 4.16–13.25 | 0 | 0.00 | 0–0 | .440a |
| Other drugs | 5 | 9.26 | 3.91–14.60 | 3 | 13.64 | 0.70–27.98 | 4 | 10.81 | 0.81–20.82 | .853a |
Note. Sample size varied according to the question because participants had the possibility to skip sections of the survey. Bold = p < .05.
Chi-square test.
Cannabis was the preferred drug independently of the reason: 57.41% (CI 95% 48.290–66.52) and 68.18% (CI 95% 48.72–87.64) of transgender youth who use drugs revealed utilizing cannabis to deal with gender-related and general stress respectively, whereas 45.95% (CI 95% 29.89–62.00) of transgender youth reported Cannabis recreational use. The second most prevalent substance reported was pain medications: 24.07% (95% CI 16.19–31.96) and 27.27% (CI 95% 8.66–45.88) of transgender youth disclosed use to face gender-related and general stress respectively, while 40.54% (CI 95% 24.72–56.36) revealed recreational use.
2.3. Modifiable factors and substance use among transgender youth
As described in Table 5, the modified factors were divided into three main groups: physical, social and economic aspects. All the aspects differed significantly among transgender youth who used substances to deal with gender-related stress, to endure general stress, to “have fun” and who did not report substance use.
Table 5.
Modifiable factors and substance use among transgender youth.
| Modifiable factors | Total |
Substance use to… |
Did not report substance use |
p | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| … deal with gender-related stress |
... deal with general stress |
... recreational purposes |
||||||||||||||
| 200 |
54 |
22 |
37 |
87 |
||||||||||||
| N | % | 95% CI | N | % | 95% CI | N | % | 95% CI | N | % | 95% CI | N | % | 95% CI | ||
| Physical aspects | ||||||||||||||||
| Have a stable place to live (no) | 90 | 45 | 38.11–51.89 | 36 | 66.67 | 54.09–79.24 | 9 | 40.91 | 20.36–61.45 | 12.00 | 32.43 | 17.35–47.52 | 33.00 | 37.93 | 27.74–48.12 | .002a |
| Mean | SD | 95% CI | Mean | SD | 95% CI | Mean | SD | 95% CI | Mean | SD | 95% CI | Mean | SD | 95% CI | ||
| Feel safe around the city | 10.53 | 4.39 | 9.91–11.15 | 9.12 | 4.49 | 7.88–10.35 | 12.31 | 4.12 | 10.48–14.13 | 11.18 | 4.27 | 9.75–12.60 | 10.68 | 4.25 | 9.75–11.61 | .018b |
| Social aspects | – | – | – | – | ||||||||||||
| Social support scale | 64.34 | 20.03 | 61.48–67.19 | 59.61 | 18.63 | 54.52–64.69 | 68.14 | 16.41 | 60.46–75.82 | 62.82 | 20.82 | 55.77–69.86 | 67.22 | 21.01 | 62.58–71.87 | .131b |
| Discrimination scale | 26.62 | 6.62 | 25.67–27.56 | 30.63 | 5.53 | 29.09–32.17 | 24.60 | 6.54 | 21.54–27.66 | 26.23 | 6.83 | 23.88–28.57 | 24.78 | 6.16 | 23.44–26.11 | .000b |
| Self-report family inventory | – | – | – | – | ||||||||||||
| Health and competence | 49.87 | 16.18 | 46.74–53.00 | 52.76 | 20.66 | 44.23–61.29 | 48.38 | 16.54 | 38.39–58.38 | 46.59 | 14.29 | 39.24–53.93 | 49.92 | 14.29 | 45.86–53.98 | .664b |
| Conflict | 31.79 | 11.89 | 29.46–34.13 | 33.88 | 11.04 | 29.32–38.44 | 30.00 | 13.77 | 22.38–37.62 | 34.93 | 12.89 | 27.79–42.07 | 30.26 | 11.39 | 26.91–33.60 | .405b |
| Cohesion | 11.04 | 3.89 | 10.39–11.69 | 10.92 | 3.96 | 9.64–12.21 | 11.20 | 4.18 | 8.89–13.51 | 10.40 | 4.01 | 8.74–12.06 | 11.35 | 3.77 | 10.38–12.32 | .776b |
| Expressiveness | 11.52 | 4.41 | 10.80–12.24 | 12.30 | 4.29 | 10.87–13.73 | 10.39 | 4.95 | 7.93–12.85 | 11.92 | 4.17 | 10.20–13.64 | 11.24 | 4.42 | 10.15–12.33 | .427b |
| Leadership | 8.30 | 3.21 | 7.77–8.82 | 7.90 | 3.45 | 6.78–9.02 | 8.18 | 3.70 | 6.28–10.08 | 8.71 | 3.86 | 7.08–10.34 | 8.42 | 2.69 | 7.75–9.08 | .779b |
| Parental support for gender identity | – | – | – | – | – | |||||||||||
| Mother (no support) | 97.00 | 48.50 | 41.57–55.43 | 35.00 | 64.81 | 52.08–77.55 | 10.00 | 45.45 | 24.65–66.26 | 14.00 | 37.84 | 22.21–53.46 | 38.00 | 43.68 | 33.26–54.10 | .120a |
| Father (no support) | 122.00 | 61.00 | 54.24–67.76 | 39.00 | 72.22 | 60.28–84.17 | 11.00 | 50.00 | 29.10–70.89 | 19.00 | 51.35 | 35.25–67.46 | 53.00 | 60.92 | 50.67–71.17 | .440a |
| Economic aspects | – | – | – | – | – | |||||||||||
| School climate | – | – | – | – | – | |||||||||||
| School connectedness | 11.16 | 3.90 | 10.57–11.75 | 12.34 | 4.15 | 11.13–13.56 | 12.00 | 4.16 | 9.78–14.22 | 9.85 | 4.01 | 8.38–11.32 | 10.78 | 3.44 | 9.99–11.57 | .024b |
| School security | 20.57 | 9.86 | 19.13–22.00 | 17.02 | 8.74 | 14.51–19.53 | 23.89 | 11.27 | 18.46–29.33 | 22.71 | 8.55 | 19.62–25.79 | 21.07 | 10.16 | 18.86–23.27 | .016b |
| Deprivation scale | 21.50 | 3.80 | 20.95–22.05 | 20.46 | 4.22 | 19.26–21.66 | 21.53 | 2.86 | 20.15–22.90 | 21.58 | 3.89 | 20.27–22.90 | 22.09 | 3.60 | 21.29–22.88 | .126b |
Note. Sample size varied according to the question because participants had the possibility to skip sections of the survey. Bold = p < .05.
Chi-square test.
ANOVA test.
Concerning physical aspects, not having a stable place to live was related to higher substance use to face gender-related stress (66.67%; CI 95% 54.09–79.24) than to endure general stress (40.91%; CI 95% 20.36–61.45), recreational use (32.43%; CI 95% 17.35–47.52) and not reporting drugs use (37.93%; CI 95% 27.74–48.12) (χ2(3) = 14.509; p = .002). Furthermore, unsafety around the city was associated with using more substance to deal with general stress than to endure gender-related stress (F(3,190) = 3.456, p = .018).
In relation to social aspects, modifiable factors concerning social structure were associated with an increase in drug use. In particular, experiencing discrimination was associated with higher substance use to deal with gender-related stress when compared to endure general stress, to recreational use and to not report drug use (F(3,187) = 10.604, p = .000).
Considering economic aspects, less school connectedness was associated with drug use to deal with gender-related when compared to recreational use (F(3,165) = 3.222, p = .024). Feeling unsafe at school, as well as feeling secure around the city, was associated with substance use to deal with gender-related stress when compared to substance use to endure general stress and to “have fun” (F(3,180) = 3.552, p = .016).
After a multinomial logistic regression (controlled by home instability, insecurity, school climate, and discrimination), exclusively experiencing discrimination and home instability remained associated with using substance to deal with gender-related stress. As described in Fig. 2 and Table 6, having suffered discrimination enhanced 1.183 (95% CI 1.10–1.27 p = .001) the odds of using substance, whereas having an unstable home increased 3.270 (95% CI 1.60–6.67 p = .009) the odds of using substance.
Fig. 2.
Multivariable logistic regression analyses.
Table 6.
Multinomial logistic regression including modifiable factors with p < .05.
| Modifiable factors | Substance use to… |
|||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| …deal with gender-related stress |
…deal with general stress |
…recreational purposes |
||||||||||||||||
| p | OR | 95% CI | p | aOR | 95% CI | p | OR | 95% CI | p | aOR | 95% CI | p | OR | 95% CI | p | aOR | 95% CI | |
| Physical aspects | ||||||||||||||||||
| Have a stable place to live (no) | .001 | 3.270 | 1.60–6.67 | .009 | 3.225 | 1.34–7.76 | .798 | 1.133 | 0.434–2.94 | .694 | 1.287 | 0.37–4.52 | .561 | 0.785 | 0.35–1.77 | .658 | 0.798 | 0.29–2.17 |
| Feel safe around the city | .042 | 0.918 | 0.84–1.00 | .420 | 1.050 | 0.93–1.18 | .119 | 1.093 | 0.98–1.22 | .169 | 1.123 | 0.95–1.32 | .560 | 1.027 | 0.94–1.12 | .573 | 1.038 | 0.91–1.18 |
| Social aspects | ||||||||||||||||||
| Discrimination scale | .000 | 1.183 | 1.10–1.27 | .001 | 1.145 | 1.06–1.24 | .913 | 0.996 | 0.92–1.07 | .950 | 1.003 | 0.91–1.11 | .269 | 1.035 | 0.97–1.10 | .391 | 1.033 | 0.96–1.11 |
| Economic aspects | ||||||||||||||||||
| School climate | ||||||||||||||||||
| School connectedness | .033 | 1.110 | 1.01–1.22 | .705 | 1.025 | 0.90–1.17 | .245 | 1.086 | 0.94–1.25 | .143 | 1.133 | 0.96–1.34 | .239 | 0.931 | 0.83–1.05 | .622 | 0.965 | 0.83–1.11 |
| School security | .023 | 0.957 | 0.92–0.99 | .296 | 0.969 | 0.91–1.03 | .248 | 1.032 | 0.98–1.09 | .510 | 1.027 | 0.95–1.11 | .411 | 1.018 | 0.98–1.06 | .740 | 0.990 | 0.93–1.05 |
Note. Bold = p < .05.
3. Discussion
To date, this is the first study to describe substance use among Brazilian transgender youth, including young transgender women, young transgender men, and gender diverse youth. Worldwide, it innovates when considering particularities in drug use specifically to endure gender-related and general stress situations in contrast to recreative substance use. It also stands out for assessing the impact of a “risk environment” on drug harm among transgender youth: experiencing discrimination and home instability were associated with using substance to deal with gender-related stress.
Cannabis was the preferred drug among participants who reported substance use in this research, independently of justification. High level of cannabis use was also shown in a 3-year prospective study that evaluated 230 US transgender women aged 19 to 59 years. After alcohol (48.4% to 60.4%), cannabis use was reported by 29.1% to 40.0% participants. Higher odds of alcohol, cannabis and cocaine use (three to four times) were linked to higher levels of physical and psychological gender abuse (Nuttbrock, Bockting, Rosenblum, Hwahng, & Mason, 2014). Another study involving US transgender women (adolescents and mostly adults) showed that cannabis was consumed by 81% of the 38% subjects who used drugs in the past 12 months (Denson et al., 2017).
A multinomial logistic regression model showed that the primary determinants of substance harm among Brazilian transgender youth are physical (home instability) and social (discrimination). Considering physical aspects, in a very plausible response to an unsafe environment, Brazilian transgender youth reported feeling unsafe in their neighborhoods, their homes, and public transportation during both day and night. The ones that felt less safe used more substance specifically to cope with gender-related stress. A US study that evaluated perceptions of safety using a similar methodology verified that transgender students exhibited a higher history of violent experiences and lower perceptions of safety when compared to their peers (Messman & Leslie, 2018). The same study showed that transgender students report significantly more use of illicit substance and non-prescription substances (Messman & Leslie, 2018). Feeling unsafe is surely much aggravated among transgender youth that experienced homelessness. In a convenience sample of 51 US ethnic-minority young transgender women (aged from 16 to 25 years), 18% reported homelessness; although no association analysis was performed, around 70% of the total sample revealed the previous use of cannabis and other drugs (Garofalo et al., 2006). Transgender youth who experienced homelessness have indeed a particularly high rate of substance use (Cochran, Stewart, Ginzler, & Cauce, 2002) as reported in the present research.
Regarding social issues, the present study showed that previous experiences of discrimination were significantly associated with substance use to deal with gender-related stress. This finding is in accordance with the literature. For example, experiences of discrimination in health care services and the use of substances as a coping mechanism were reported by 28% of 2578 participants in a study involving transgender men and transmasculine individuals (binary and non-binary) from US (Reisner et al., 2015). Accordingly, 26.3% of 5612 US transgender women reported alcohol and drugs use to cope with gender abuse (Klein & Golub, 2016), and discrimination based on gender identity was associated to the non-medical use of prescription drugs by 155 US transgender adults (Benotsch et al., 2013).
The present study presents four main limitations. First, even though it is the first study to evaluate substance abuse among Brazilian transgender youth, adolescents and young adults from outside Southern Brazil are underrepresented. Also, the sample is not population-based, preventing prevalence analysis. Second, this sample is composed mostly of white transgender youth able to access the internet and, thus, more marginalized groups may not have had the opportunity to fulfill the online questionnaire. Third, assessing the amount and the frequency of each substance utilized would provide determinant information concerning use patterns; however, these questions were not included in the survey. Finally, the cross-sectional design hampers causality inferences.
Finally, bearing in mind that a “risky” environment was associated with higher odds of substance use, the harm reduction strategies must affect the social and physical aspects of transgender youth lives. For example, US LGBT youth attending schools with a gay-straight alliance reported reduced risk for use cocaine, hallucinogens, cannabis, non-prescribed ADHD medication and pain medication (Heck et al., 2014). They also presented lower odds of past year discrimination, as well as suicidal thoughts and attempts (Saewyc, Konishi, Rose, & Homma, 2016). A not so easily achievable harm reduction strategy is housing (Thornton et al., 2016). Homelessness transgender youth endure unique adversities: from difficulty to be accepted in shelters to physical and sexual victimization (Quintana, Rosenthal, & Krehely, 2010). Although these challenges are well reported, strategies to actually facilitated transgender youth lives are understudied and often unaddressed.
Declaration of interest
None.
Detailed disclosures
None.
Role of the funding source
Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) and Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) provided financial support through scholarships.
Ethical considerations
The project was approved by the Ethical Committee and Research Commission of Universidade Federal do Rio Grande do Sul Psychology Institute (14,221,513.4.0000.5334). Volunteers were informed about the research objectives, and the inexistence of direct benefices for joining the survey, before signing the consent. Confidentiality and anonymity were assured, as well as the possibility to withdraw at any time.
Acknowledgments
We thank the Health Equity and Epidemiology Research Group (HEER) for multiple, and very useful, insights. We also thank TransYouth CAN! Team for sharing their survey. We also acknowledge CNPq and CAPES for provide financial support through scholarships.
References
- Balzer C., Hutta J.S., Adrián T., Hyndal P. Transgender Europe. 2012. Transrespect versus transphobia worldwide: A comparative review of the human-rights situation of gender-variant/trans people.https://transrespect.org/wp-content/uploads/2015/08/TvT_research-report.pdf Berlin. Retrieved from. [Google Scholar]
- Barnett T., Whiteside A., Khodakevich L., Kruglov Y. The HIV/AIDS epidemic in Ukraine: Its potential social and economic impact. Social Science & Medicine. 2000;51(9):1387–1403. doi: 10.1016/s0277-9536(00)00104-0. [DOI] [PubMed] [Google Scholar]
- Bauer G.R., Braimoh J., Scheim A.I., Dharma C. Transgender-inclusive measures of sex/gender for population surveys: Mixed-methods evaluation and recommendations. PLoS One. 2017;12(5):1–28. doi: 10.1371/journal.pone.0178043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beavers R., Hampson R.B. 22(2) The Association for Family Therapy; 2000. The Beavers systems model of family functioning; pp. 128–143. [Google Scholar]
- Beavers W.R., Hampson R.B., Hulgus Y.F. Commentary: The Beavers systems approach to family assessment. Family Process. 1985;24(3):398–405. [Google Scholar]
- Benotsch E.G., Zimmerman R., Cathers L., McNulty S., Pierce J., Heck T.…Snipes D. Non-medical use of prescription drugs, polysubstance use, and mental health in transgender adults. Drug and Alcohol Dependence. 2013;132(1–2):391–394. doi: 10.1016/j.drugalcdep.2013.02.027. [DOI] [PubMed] [Google Scholar]
- Borsa J.C., Damásio B.F., Bandeira D.R. Cross-cultural adaptation and validation of psychological instruments: Some considerations. Paidéia (Ribeirão Preto) 2012;22(53):423–432. [Google Scholar]
- Boys A., Marsden J., Griffiths P., Stillwell G., Strang J. Substance use among young people: The relationship between perceived functions and intentions. Addiction. 1999;94(7):1043–1050. doi: 10.1046/j.1360-0443.1999.94710439.x. [DOI] [PubMed] [Google Scholar]
- Clark T.T., Salas-wright C.P., Vaughn M.G., Whitfiled K.E. Everyday discrimination and mood and substance use disorders: A latent profile analysis with African Americans and Caribbean Blacks. Addictive Behaviors. 2015;40:119–125. doi: 10.1016/j.addbeh.2014.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cochran B.N., Stewart A.J., Ginzler J.A., Cauce A.M. Challenges faced by homeless sexual minorities: Comparison of gay, lesbian, bisexual, and transgender homeless adolescents with their heterosexual counterparts. American Journal of Public Health. 2002;92(5):773–777. doi: 10.2105/ajph.92.5.773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costa A.B., da Rosa Filho H.T., Pase P.F., Fontanari A.M.V., Catelan R.F., Mueller A.…Koller S.H. Healthcare needs of and access barriers for brazilian transgender and gender diverse people. Journal of Immigrant and Minority Health. 2016;0(0):1–9. doi: 10.1007/s10903-016-0527-7. [DOI] [PubMed] [Google Scholar]
- Costa A.B., Fontanari A.M.V., Catelan R.F., Schwarz K., Stucky J.L., da Rosa Filho H.T.…Koller S.H. HIV-related healthcare needs and access barriers for Brazilian transgender and gender diverse people. AIDS and Behavior. 2018;22(8):2534–2542. doi: 10.1007/s10461-017-2021-1. [DOI] [PubMed] [Google Scholar]
- Day J.K., Fish J.N., Perez-Brumer A., Hatzenbuehler M.L., Russell S.T. Transgender youth substance use disparities: Results from a population-based sample. Journal of Adolescent Health. 2017;61(6):729–735. doi: 10.1016/j.jadohealth.2017.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Pedro K.T., Gilreath T.D., Jackson C., Esqueda M.C. Substance use among transgender students in California public middle and high schools. Journal of School Health. 2017;87(5):303–309. doi: 10.1111/josh.12499. [DOI] [PubMed] [Google Scholar]
- Denson D.J., Padgett P.M., Pitts N., Paz-Bailey G., Bingham T., Carlos J.A.…Finlayson T. Health care use and HIV-related behaviors of black and Latina transgender women in 3 US metropolitan areas: Results from the transgender HIV behavioral survey. Journal of Acquired Immune Deficiency Syndromes. 2017;75(3):268–275. doi: 10.1097/QAI.0000000000001402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dom G., Sabbe B., Hulstijn W., van Den Brink W. Substance use disorders and the orbitofrontal cortex. British Journal of Psychiatry. 2005;187(03):209–220. doi: 10.1192/bjp.187.3.209. [DOI] [PubMed] [Google Scholar]
- Editorial Risk environments and drug harms: A social science for harm reduction approach. International Journal of Drug Policy. 2009;20(3):193–201. doi: 10.1016/j.drugpo.2008.10.003. [DOI] [PubMed] [Google Scholar]
- Garofalo R., Deleon J., Osmer E., Doll M., Harper G.W. Overlooked, misunderstood and at-risk: Exploring the lives and HIV risk of ethnic minority male-to-female transgender youth. Journal of Adolescent Health. 2006;38(3):230–236. doi: 10.1016/j.jadohealth.2005.03.023. [DOI] [PubMed] [Google Scholar]
- Gilbert P.A., Pass L.E., Keuroghlian A.S., Green T.K., Reisner S.L. Alcohol research with transgender populations: A systematic review and recommendations to strengthen future studies. Drug and Alcohol Dependence. 2018;186(1):138–146. doi: 10.1016/j.drugalcdep.2018.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldbach J.T., Gibbs J. Strategies employed by sexual minority adolescents to cope with minority stress. Psychology of Sexual Orientation and Gender Diversity. 2015;2(3):297–306. doi: 10.1037/sgd0000124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldbach J.T., Tanner-Smith E.E., Bagwell M., Dunlap S. Minority stress and substance use in sexual minority adolescents: A meta-analysis. Prevention Science. 2014;15(3):350–363. doi: 10.1007/s11121-013-0393-7. [DOI] [PubMed] [Google Scholar]
- Goodrich K.M., Selig J.P., Trahan D.P. The self-report family inventory: An exploratory factor analysis. Measurement and Evaluation in Counseling and Development. 2012;45(4):245–256. [Google Scholar]
- Grant B.F., Stinson F.S., Harford T.C. Age at onset of alcohol use and DSM-IV alcohol abuse and dependence: A 12-year follow-up. Journal of Substance Abuse. 2001;13(4):493–504. doi: 10.1016/s0899-3289(01)00096-7. [DOI] [PubMed] [Google Scholar]
- Heck N.C., Livingston N.A., Flentje A., Oost K., Stewart B.T., Cochran B.N. Reducing risk for illicit drug use and prescription drug misuse: High school gay-straight alliances and lesbian, gay, bisexual, and transgender youth. Addictive Behaviors. 2014;39(4):824–828. doi: 10.1016/j.addbeh.2014.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendricks M.L., Testa R.J. A conceptual framework for clinical work with transgender and gender nonconforming clients: An adaptation of the minority stress model. Professional Psychology: Research and Practice. 2012;43(5):460–467. [Google Scholar]
- Hyman S.M., Sinha R. Stress-related factors in cannabis use and misuse: Implications for prevention and treatment. Journal of Substance Abuse Treatment. 2009;36(4):400–413. doi: 10.1016/j.jsat.2008.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein A., Golub S.A. Family rejection as a predictor of suicide attempts and substance misuse among transgender and gender nonconforming adults. LGBT Health. 2016;3(3):193–199. doi: 10.1089/lgbt.2015.0111. [DOI] [PubMed] [Google Scholar]
- Lai H.M.X., Cleary M., Sitharthan T., Hunt G.E. Prevalence of comorbid substance use, anxiety and mood disorders in epidemiological surveys, 1990–2014: A systematic review and meta-analysis. Drug and Alcohol Dependence. 2015;154:1–13. doi: 10.1016/j.drugalcdep.2015.05.031. [DOI] [PubMed] [Google Scholar]
- Mcneely C.A., Nonnemaker J.M., Blum R.W. Promoting school connectedness: Evidence from the national longitudinal study of adolescent health. Journal of School Health. 2002;72(4):138–146. doi: 10.1111/j.1746-1561.2002.tb06533.x. [DOI] [PubMed] [Google Scholar]
- Messman J.B., Leslie L.A. Transgender college students: Academic resilience and striving to cope in the face of marginalized health. Journal of American College Health. 2018:1–13. doi: 10.1080/07448481.2018.1465060. [DOI] [PubMed] [Google Scholar]
- Meyer I.H. Minority stress and mental-health in gay men. Journal of Health and Social Behavior. 1995;36(1):38–56. [PubMed] [Google Scholar]
- Meyer I.H. Prejudice as stress: Conceptual and measurement problems. American Journal of Public Health. 2003;93(2):262–265. doi: 10.2105/ajph.93.2.262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nuttbrock L., Bockting W., Rosenblum A., Hwahng S., Mason M. Gender abuse, depressive symptoms, and substance use among transgender women: A 3-year prospective study. American Journal of Public Health. 2014;104(11):2199–2206. doi: 10.2105/AJPH.2014.302106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quintana N.S., Rosenthal J., Krehely J. Center for American Progress; Washington, DC: 2010. On the streets: The federal response to gay and transgender homeless youth.https://www.americanprogress.org/issues/lgbt/reports/2010/06/21/7983/on-the-streets/ Retrieved from. [Google Scholar]
- Reisner S.L., Greytak E.A., Parsons J.T., Ybarra M.L. Gender minority social stress in adolescence: Disparities in adolescent bullying and substance use by gender identity. Journal of Sex Research. 2014:37–41. doi: 10.1080/00224499.2014.886321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reisner S.L., Pardo S.T., Gamarel K.E., Hughto J.M.W., Pardee D.J., Keo-Meier C.L. Substance use to cope with stigma in healthcare. LGBT Health. 2015;2(4):324–332. doi: 10.1089/lgbt.2015.0001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saewyc E.M., Konishi C., Rose H.A., Homma Y. School-based strategies to reduce suicidal ideation, suicide attempts, and discrimination among sexual minority and heterosexual adolescents in Western Canada. International Journal of Child, Youth and Family Studies. 2016;5(1):1–23. doi: 10.18357/ijcyfs.saewyce.512014. (26793284) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sausa L.A., Sevelius J., Keatley J., Iñiguez J.R., Reyes M. University of California; San Francisco: 2009. Policy recommendations for inclusive data collection of trans people in HIV prevention, care & services.http://transhealth.ucsf.edu/pdf/data-recommendation.pdf Retrieved from. [Google Scholar]
- Seibel B.L., de Brito Silva B., Fontanari A.M.V., Catelan R.F., Bercht A.M., Stucky J.L.…Costa A.B. The impact of the parental support on risk factors in the process of gender affirmation of transgender and gender diverse people. Frontiers in Psychology. 2018;9(3):1–9. doi: 10.3389/fpsyg.2018.00399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherbourne C.D., Stewart A.L. The MOS social support survey. Social Science & Medicine. 1991;32(6):705–714. doi: 10.1016/0277-9536(91)90150-b. 2035047 [DOI] [PubMed] [Google Scholar]
- Solorio R., Swendeman D., Rotheram-Borus M.J. Risk among young gay and bisexual men living with HIV. AIDS Education and Prevention. 2003;15(1):80–89. doi: 10.1521/aeap.15.1.5.80.23610. 12630601 [DOI] [PubMed] [Google Scholar]
- Tharp-Taylor S., Haviland A., D'Amico E.J. Victimization from mental and physical bullying and substance use in early adolescence. Addictive Behaviors. 2009;34(6–7):561–567. doi: 10.1016/j.addbeh.2009.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thornton R.L.J., Glover C.M., Cené C.W., Glik D.C., Henderson J.A., Williams D.R.…Williams D.R. Evaluating strategies for reducing health disparities by addressing the social determinants of health. Health Affairs. 2016;35(8):1416–1423. doi: 10.1377/hlthaff.2015.1357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veale J., Saewyc E., Frohard-Dourlent H., Dobson S., Clark B., Canadian Trans Youth Health, S. R. G Being safe, being me: Results of the Canadian trans youth health survey. 2015. https://saravyc.sites.olt.ubc.ca/files/2015/05/SARAVYC_Trans-Youth-Health-Report_EN_Final_Web2.pdf Retrieved from.