Abstract
Objectives
Cocaine use is increasing and many cocaine users engage in polysubstance use. Within polysubstance use, relationships among use of individual substances are necessarily complex. To address this complexity, we used latent class analysis (LCA) to identify patterns of polysubstance use among lifetime cocaine users and examine associations among these patterns, demographics, and risk profiles.
Methods
Members of HealthStreet, an ongoing community engagement program, were asked about lifetime and past 30-day use of cocaine, alcohol, tobacco, marijuana, and prescription medications, mental health conditions, recent Emergency Department (ED) visits and demographics. LCA was used to identify classes of past 30-day polysubstance use among individuals who endorsed lifetime cocaine use. Multinomial logistic regression identified factors associated with these classes.
Results
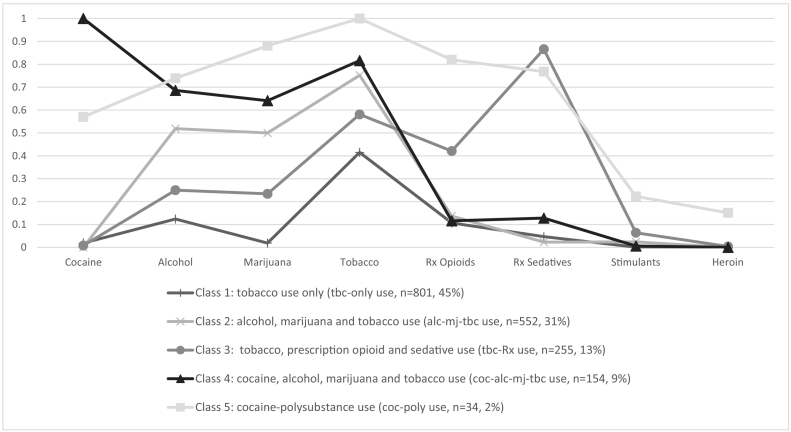
Among 1797 lifetime cocaine users, a five-class LCA model was identified: 1) past 30-day tobacco use only (45%), 2) past 30-day alcohol, marijuana and tobacco use (31%), 3) past 30-day tobacco, prescription opioid and sedative use (13%), 4) past 30-day cocaine, alcohol, marijuana and tobacco use (9%), 5) past 30-day cocaine and multiple polysubstance use (2%). Demographics, ED visits and mental health conditions were associated with class membership.
Conclusions
Approximately 11% of lifetime cocaine users used cocaine in the past 30 days with two different concurrent substance use patterns. Prescription medication (opioids and sedatives) and complex polysubstance use patterns were stronger indicators of negative outcomes than current cocaine use. Cocaine was not used frequently with other stimulants. In addition to polysubstance use, prescription medication use should be targeted for intervention among lifetime cocaine users.
Highlights
-
•
Among 1,797 lifetime cocaine users, a five-class LCA model was identified.
-
•
Approximately 11% of lifetime cocaine users used cocaine in the past 30 days with two different polysubstance use patterns.
-
•
Opioid and sedative use and complex polysubstance use patterns were strong indicators of negative outcomes.
-
•
Cocaine was not used frequently with other stimulants.
1. Introduction
Cocaine is one of the most prevalent illicit drugs used in the United States (US). Approximately 1.5 million individuals in the US aged 12 or older report past 30-day cocaine use (NIDA, 2015). Recent evidence shows increased problematic cocaine use since 2011. According to the National Survey on Drug Use and Health (NSDUH), the prevalence of past year cocaine use increased by 20% from 2011 to 2015, and according to the Centers for Disease Control and Prevention (CDC) cocaine-related death also increased in the same period (John & Wu, 2017). Evidence shows that this trend may increase even further with greater cocaine production in Columbia, the major source of cocaine in the US (The Office of National Drug Control Policy (ONDCP), n.d.). In addition to national studies, it is important to examine data within a community setting specifically among a community sample in Florida where a similar increase in cocaine-related deaths was observed from 2.8% in 2012 to 8.6% in 2016, an increase of over 200% (Florida Drug-Related Outcomes Surveillance and Tracking System, 2003–2016). Though national studies provide an overview of prevalence rates, community data provide information on burdens of substance use within specific geographic regions and are valuable for the design and implementation of local interventions to address community needs.
Previous studies have shown that cocaine users concurrently use other substances frequently, including alcohol (Blow et al., 2011; Borders & Booth, 2013; Evans-Polce, Lanza, & Maggs, 2016; Hedden, Malcolm, & Latimer, 2009; Liu, Williamson, Setlow, Cottler, & Knackstedt, 2018), tobacco (Winhusen et al., 2013), marijuana (Gonçalves & Nappo, 2015; Liu et al., 2018), heroin (Leeman, Sun, Bogart, Beseler, & Sofuoglu, 2016; Ojha, Sigdel, Meyer-Thompson, Oechsler, & Verthein, 2014; Oviedo-Joekes et al., 2015), and prescription medications (Al-Tayyib, Rice, Rhoades, & Riggs, 2014; Chen et al., 2014; Evans-Polce et al., 2016; Herman-Stahl, Krebs, Kroutil, & Heller, 2006; Winhusen et al., 2013). Polysubstance users have been found to have a higher risk of overdose, emergency department (ED) visits, violence, accidental injury (Macdonald et al., 2014), traffic accidents (De Boni et al., 2014), and lower addiction treatment effectiveness (Evans et al., 2015; Hou, Zhan, Zheng, Zhan, & Zheng, 2014; Liu et al., 2018) compared to mono-substance users. Polysubstance use has also been associated with worse physical health (Quek et al., 2013; White et al., 2013), lower quality of life (Kelly et al., 2017) and higher rates of mental health conditions, such as anxiety, depression, social phobia, and personality disorders (Agrawal, Lynskey, Madden, Bucholz, & Heath, 2007; Chen et al., 2014; Evans et al., 2015; Kelly et al., 2017; Leeman et al., 2016; Quek et al., 2013; White et al., 2013). Studies examining cocaine-polysubstance use mainly focus on the comparison between individuals who used cocaine only and individuals who used cocaine plus one other substance. However, patterns of polysubstance with more than two substances are typically ignored (Gonçalves & Nappo, 2015; Hedden et al., 2009; Leeman et al., 2016; Winhusen et al., 2013). It is crucial to understand more about the complex patterns of polysubstance use, because a high degree of complexity is inherent in polysubstance use and we need to begin to account for its complexity in research. Latent class analysis (LCA) is a statistical method that can be used to identify homogenous subgroups within a heterogeneous population based on similarity of response patterns (Lubke & Muthén, 2005). This method has been used in previous studies to examine substance use patterns (Blow et al., 2011; Chen et al., 2014; Scherer, Harrell, & Romano, 2015; Shiu-Yee et al., 2018). However, to our knowledge, LCA has not been used to examine polysubstance use patterns specifically among cocaine users.
We employed LCA to understand current (past 30-day) polysubstance use patterns among individuals who reported cocaine use in their lifetime. In addition, substance users' demographic characteristics (e.g., age) can be used to identify high-risk populations for targeted interventions. ED visits and mental health conditions also contribute to cocaine users' risk profile. Therefore, association of polysubstance use patterns with demographics, ED visits, and mental health conditions were assessed.
2. Methods
A total of 9717 community members were recruited from September 2011 to December 2017 through HealthStreet, an ongoing community engagement program. The purpose of HealthStreet is to assess community needs and link community members to medical and social services and eligible research studies. Therefore, traditional under-represented populations such as females, blacks, and people who are unemployed were over-sampled. This study was approved by the University of Florida Institutional Review Board and informed consent was obtained from each participant. After consenting, participants were asked by community health workers about their socio-demographics, recent ED visits, mental health conditions, and past 30-day and lifetime substance use. Before interviews, participants were assured of the confidentiality of the data by explaining protections available under the certificate of NIH confidentiality issued for the study. Substance use measurements included: cocaine, alcohol, tobacco, marijuana, prescription opioids, prescription sedatives, prescription stimulants, heroin, and speed/amphetamines. Lifetime cocaine use was elicited by: “Have you ever used cocaine or crack?” Respondents who answered “yes” were considered lifetime cocaine users and were included as the sample for the current analysis. If a participant reported ever using a substance, the question, “Have you used [substance name] in the last 30 days” was asked. Past 30-day substance use status was assessed in the same way for all substances except alcohol. At-risk alcohol use in the past-30 days was measured with respect to whether participants had more than [4 drinks (for males)/3 drinks (for females)] in a single day. Prescription stimulants and speed/amphetamines were combined as other stimulants in the current analyses. Age, sex, race (black, white, or other), marital status (single or married), employment (employed or unemployed) and educational attainment (high school or below, or above high school) were also measured. Recent ED visits were elicited as: “How many times have you been to the ER in the last 6 months for your own injury, illness, or condition?” Answers were dichotomized into “yes” for at least one visit or “no” for zero visits. Mental health status for anxiety, depression and bipolar disorder was elicited as “Have you ever been told you had, or have you ever had a problem with [condition]?” with “yes” or “no” responses.
2.1. Data analysis
LCA was conducted among lifetime cocaine users to identify patterns of past 30-day polysubstance use. Starting with one-class, a series of models with increasing number of classes were fit. The best number of classes was determined based on Bayesian information criterion (BIC), sample size adjusted BIC (SSABIC), Akaike information criterion (AIC), entropy, Lo-Mendel-Rubin likelihood ratio test (LMR-LRT) (Lo, Mendell, & Rubin, 2001), bootstrap likelihood ratio test (BLRT) and the interpretability of the model. A smaller value for BIC, SSABIC, and AIC indicated better model fit (Lanza, Collins, Lemmon, & Schafer, 2007). Entropy was a measure of the classification accuracy of placing participants into classes based on their model-based posterior probabilities and higher entropy values reflected better classification (Celeux & Soromenho, 1996). The LMR-LRT and BLRT examined the overall fit between the current model and a model with k-1 classes; a p-value smaller than 0.05 indicated that the current model was significantly better than k-1 class model in terms of model fit (Nylund, Asparouhov, & Muthén, 2007). P-values from the LMR-LRT and BLRT were consistent and only the results from the LMR-LRT are reported in the table.
After the optimal number of classes was determined, participants were assigned to the class in which they had the highest probability of membership. The Mantel Haenszel Chi-square test was used to test differences between the latent classes on demographic characteristics, having a recent ED visit, and mental health conditions. Multivariate logistic regression was used to further explore these associations and the largest LCA class was used as the reference group. P-value <0.05 was considered statistically significant. The LCA was performed in M-Plus 7 and the rest of the analyses were performed in SAS 9.4.
3. Results
3.1. Study participants
Among the 9717 community members aged 18–83 who were recruited through HealthStreet, 1797 (18.5%) individuals reported lifetime cocaine use and among them, 183 (10.2%) reported past 30-day (current) cocaine use. The mean age of all lifetime cocaine users was 48.3, older than the mean age of the total HealthStreet cohort which was 44.4. Black was the largest racial group of HealthStreet members and of lifetime cocaine users. Most of the HealthStreet members were single or not married (78.9%), unemployed (65.2%), and with their highest education levels equal to or below high school (58.4%). These proportions were even higher among lifetime cocaine users. Demographics are shown in Table 1.
Table 1.
Descriptive statistics of the sample.
| Total HealthStreet sample, n = 9717 |
Lifetime cocaine users, n = 1797 |
||||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| Age | 44.4 | 16.6 | 48.3 | 12.3 | |
| n | % | n | % | ||
| Gender | Male | 3944 | 40.6 | 988 | 55.3 |
| Race | Black | 5754 | 56.1 | 871 | 48.6 |
| White | 3302 | 33.9 | 808 | 45.0 | |
| Other | 681 | 7 | 115 | 6.4 | |
| Marital status | Single | 7681 | 78.9 | 1516 | 84.5 |
| Employment | Unemployed | 6310 | 65.2 | 1353 | 78.8 |
| Education | High school or below | 5673 | 58.4 | 1149 | 64.2 |
| Past 30-day cocaine use | 183 | 1.9 | 183 | 10.2 | |
3.2. Model fit and selection
LCA was conducted among the 1797 individuals who reported lifetime cocaine use. Model fit statistics and brief class descriptions for 1 to 6-class solutions are shown in Table 2. Although the AIC (11,508.66) and the BIC (11,750.36) of the five-class solution was slightly higher than the AIC and the BIC of the four-class solution, the LMR-LRT showed the five-class solution to be a better fit to the data than the four-class solution. The entropy of the five-class solution was the highest among all tested solutions and 9% higher than the four-class solution. In addition, the five-class solution identified a subgroup of cocaine users who were using six different substances including cocaine in the same 30-day period, which the four class-solution did not identify. Although the number of people who were categorized into that class was small, this class represents a high-risk cocaine polysubstance use pattern that we believe to be important to identify. A smaller class size has been seen in past literature (Evans-Polce et al., 2016; Schwartz, Wetzler, Swanson, & Sung, 2010; Trenz et al., 2013). Incorporating all of this information, we chose the five-class solution.
Table 2.
Fit statistics from 1 to 6-class models.
| Class | Likelihood | AIC | BIC | SSABIC | Entropy | p-Value (LMR-LRT) | Class description |
|---|---|---|---|---|---|---|---|
| 1 | −5974.22 | 11,964.45 | 12,008.4 | 11,982.98 | NA | NA | The one class model featured tobacco, alcohol and marijuana use. |
| 2 | −5799.27 | 11,632.53 | 11,725.92 | 11,671.91 | 0.501 | <0.0001 | 33% featured tobacco, alcohol and marijuana use; 67% featured tobacco only use. |
| 3 | −5745.15 | 11,542.3 | 11,685.13 | 11,602.53 | 0.598 | 0.0503 | 10% featured Rx sedative, Rx opioid and tobacco use; 55% featured tobacco only use; 34% featured tobacco, alcohol and marijuana use. |
| 4 | −5718.8 | 11,507.6 | 11,699.87 | 11,588.68 | 0.602 | 0.0192 | Similar to the four class model. An additional class featured cocaine, alcohol, marijuana, and tobacco use was identified. |
| 5 | −5710.33 | 11,508.66 | 11,750.36 | 11,610.58 | 0.692 | 0.0347 | See Fig. 1 |
| 6 | −5706.74 | 11,519.48 | 11,810.63 | 11,642.25 | 0.613 | 0.4617 | The six class model had three classes featured cocaine use, but the Prob. of using alcohol, marijuana, tobacco, Rx sedative, and Rx opioid varies. |
3.3. Class description
Results of the LCA are depicted in Fig. 1 as the conditional probability of using different drugs in the past-30 days given class membership.
Fig. 1.
Current substance use patterns among individuals who used cocaine in their lifetime (n = 1797).
Class 1 included 801 (45%) of the lifetime cocaine users. It had nearly no probability of current cocaine use, but moderate probability (42%) of current tobacco use and low probability of other substance use. This class was summarized as “tobacco use only” (tbc-only use).
The next class included 552 (31%) of the lifetime cocaine users. Individuals in class 2 had nearly zero probability of current cocaine use but high probability of current tobacco use (75%) and approximately 50% probability of current alcohol and marijuana use. This class was summarized as “alcohol, marijuana and tobacco use” (alc-mj-tbc use).
Class 3 included 255 (13%) of the lifetime cocaine users with around zero probability of current cocaine use, but high probabilities of current prescription sedative use (87%) use, and moderate probability of current tobacco (58%) and prescription opioid use (42%). This class was summarized as “tobacco, prescription opioid and sedative use” (tbc-Rx use).
Class 4 included 154 (9%) of the lifetime cocaine users, and all individuals in this class reported current cocaine use. They also had 64%, 68% and 81% probabilities of current marijuana use, alcohol, and tobacco use, respectively. This class was summarized as “cocaine, alcohol, marijuana and tobacco use” (coc-alc-mj-tbc use).
The final class, class 5, included 34 (2%) of the lifetime cocaine users. Individuals in this class had a 57% probability of current cocaine use. They also had high probabilities of concurrent use of alcohol (74%), marijuana (88%), tobacco (100%), prescription opioids (82%) and prescription sedatives (77%). This is the only class that had some probabilities of current other stimulant (22%) and heroin use (15%). This class was labeled “cocaine-polysubstance use” (coc-poly use).
3.4. Factors associated with class membership
Table 3 shows the results of demographic composition and the prevalence of having recent ED visits and mental health conditions in each class. From the Mantel Haenszel Chi-square test, we found statistical differences between classes on sex, marital status, employment status, ED visits and all three mental health conditions. All variables were further analyzed in multivariate logistic regression models and results are shown in Table 4.
Table 3.
Latent class and demographic factors, ED visits, and mental health conditions bivariate analyses.
| Class 1 (tbc-only) |
Class 2 (alc-mj-tbc) |
Class 3 (tbc-Rx) |
Class 4 (coc-alc-mj-tbc) |
Class 5 (coc-poly) |
p value | |
|---|---|---|---|---|---|---|
| n = 801 | n = 552 | n = 255 | n = 154 | n = 34 | ||
| Mean Age (SD) | 50.3 (11.8) | 45.5 (12.7) | 50.3 (11.1) | 46.3 (12.0) | 38.1 (11.1) | |
| n (%) | n (%) | n (%) | n (%) | n (%) | <0.0001 | |
| Sex: Male | 454 (56.8) | 328 (59.7) | 97 (38.5) | 95 (61.7) | 16 (47.1) | 0.0498 |
| Race: Black | 411 (51.3) | 264 (47.8) | 84 (32.9) | 105 (68.2) | 9 (26.5) | 0.6156 |
| Race: White | 349 (43.6) | 244 (44.2) | 157 (61.6) | 38 (24.7) | 20 (58.8) | |
| Race: Other | 41 (5.1) | 44 (8.0) | 14 (5.5) | 11 (7.1) | 5 (14.8) | |
| Marital status: Single | 662 (82.7) | 470 (85.1) | 214 (83.9) | 144 (93.6) | 27 (79.4) | 0.0253 |
| Employment status: Unemployed | 590 (74.0) | 398 (72.5) | 219 (86.2) | 123 (79.9) | 24 (70.6) | 0.0119 |
| Education: High school or below | 489 (61.1) | 381 (69.2) | 140 (55.1) | 119 (77.8) | 21 (61.8) | 0.0527 |
| ED visit in the past 6 months | 293 (36.6) | 209 (37.9) | 124 (48.6) | 68 (44.2) | 25 (75.5) | <0.0001 |
| Anxiety | 244 (30.5) | 197 (35.7) | 185 (72.6) | 57 (37.0) | 26 (76.5) | <0.0001 |
| Depression | 305 (38.1) | 237 (42.9) | 192 (75.3) | 81 (52.6) | 26 (76.5) | <0.0001 |
| Bipolar disorder | 114 (14.2) | 111 (20.2) | 96 (37.7) | 35 (22.7) | 19 (55.9) | <0.0001 |
Table 4.
Adjusted odds ratios (aOR) and 95% confidence intervals from multivariate logistic regression models (ref = class 1 (tbc-only)).
| Class 2 (alc-mj-tbc) |
Class 3 (tbc-Rx) |
Class 4 (coc-alc-mj-tbc) |
Class 5 (coc-poly) |
|
|---|---|---|---|---|
| aOR (95%CI) | aOR (95%CI) | aOR (95%CI) | aOR (95%CI) | |
| Age | ||||
| Every 10-year increase | 0.75 (0.68, 0.82)⁎⁎ | 1.15 (1.00, 1.32)⁎⁎ | 0.74 (0.63, 0.86)⁎ | 0.53 (0.38, 0.72)⁎⁎ |
| Gender (ref: Female) | ||||
| Male | 1.29 (1.02, 1.63)⁎ | 0.64 (0.47, 0.88)⁎⁎ | 1.39 (0.96, 2.03) | 1.54 (0.72, 3.33) |
| Race (ref: Black) | ||||
| White | 1.02 (0.80, 1.31) | 1.32 (0.94, 1.85) | 0.38 (0.25, 0.58)⁎⁎ | 1.29 (0.55, 3.21) |
| Other | 1.45 (0.90, 2.35) | 0.98 (0.47, 1.95) | 0.92 (0.42, 1.87) | 2.44 (0.66, 8.12) |
| Marital status (ref: Married) | ||||
| Single | 1.15 (0.85, 1.57) | 1.04 (0.70, 1.58) | 2.76 (1.47, 5.77)⁎ | 0.74 (0.32,1.95) |
| Employment (ref: Employed) | ||||
| Unemployed | 0.93 (0.71, 1.21) | 1.51 (0.99, 2.34) | 1.00 (0.64, 1.60) | 0.72 (0.31, 1.77) |
| Education (ref: Above high school) | ||||
| High school or below | 1.41 (1.11, 1.82)⁎⁎ | 0.86 (0.62, 1.19) | 1.76 (1.16, 2.74)⁎⁎ | 1.03 (0.49, 2.25) |
| ED visits in the past 6 months (ref: No) | ||||
| Yes | 0.99 (0.78, 1.25) | 1.19 (0.87, 1.63) | 1.13 (0.78, 1.63) | 3.61 (1.65, 8.61)⁎⁎ |
| Anxiety (ref: No) | ||||
| Yes | 1.04 (0.79, 1.38) | 3.15 (2.18, 4.60)⁎⁎ | 1.10 (0.71, 1.70) | 2.77 (1.12, 7.51)⁎ |
| Depression (ref: No) | ||||
| Yes | 1.15 (0.89, 1.50) | 2.01 (1.39, 3.94)⁎⁎ | 1.81 (1.19, 2.73)⁎⁎ | 1.87 (0.75, 5.01) |
| Bipolar disorder (ref: No) | ||||
| Yes | 1.29 (0.94, 1.77) | 1.78 (1.24, 2.55)⁎⁎ | 1.38 (0.85, 2.20) | 3.11 (1.43, 6.89)⁎⁎ |
p-value < 0.05.
p-value < 0.01.
3.5. Class membership and demographics
The mean age of individuals in the “tbc-only use” class was 50.3. Compared to them, users in other classes were significantly younger, except for people in the “tbc-Rx use” class which were older. Compared to the “tbc-only use” class, males were more likely to be in the “alc-mj-tbc use” class (aOR = 1.29, 95%CI 1.02, 1.63), while females were more likely to be in the “tbc-Rx use” class (aOR = 0.64, 95%CI 0.47, 0.88). Being single was uniquely associated with being in the “coc-alc-mj-tbc use” class (aOR = 2.76, 95%CI 1.47, 5.77). Compared to the “tbc-only use” class, having lower educational level was associated with 41% and 76% increased odds of being in the “alc-mj-tbc use” and “coc-alc-mj-tbc use” class, respectively. Race and employment status were not associated with the class membership.
3.6. Class membership and ED visits
Users in the “coc-poly use” class were 3.61 times more likely than individuals in the “tbc-only use” class to have at least one ED visit in the past six months, and this risk was also significantly higher than all other classes, since the 95% CI of this class did not overlap with the 95% CIs of other classes.
3.7. Class membership and mental health
Compared to the “tbc-only use” class, individuals in the “alc-mj-tbc use” class had significantly higher odds of anxiety, depression and bipolar disorder; individuals in the “coc-alc-mj-tbc use” class had 80% increased risk of having depression; individuals in the “coc-poly use” class had 2.77 and 3.11 times the odds of having anxiety and bipolar disorder, respectively.
4. Discussion
We aimed to identify patterns of past 30-day polysubstance use among lifetime cocaine users including a broad range of substances in a North Central Florida community sample. LCA produced a five-class solution. The classes were: 1) tobacco use only (tbc-only use, 45%), 2) alcohol, marijuana and tobacco use (alc-mj-tbc use, 31%), 3) tobacco, prescription opioid and sedative use (tbc-Rx use, 13%), 4) cocaine, alcohol, marijuana and tobacco use (coc-alc-mj-tbc use, 9%), 5) cocaine-polysubstance use (coc-poly use, 2%).
The “coc-poly use” class had the youngest mean age among all five classes. This is consistent with previous studies, as the youngest group was more likely to report current and repeated cocaine use (Ramo, Grov, Delucchi, Kelly, & Parsons, 2011) and using more substances concurrently with cocaine (Quek et al., 2013). In addition, we found that being male was uniquely associated with higher odds of being in the “alc-mj-tbc use class; being female and older were associated only with the “tbc-Rx use” class; being single was only associated with the “coc-alc-mj-tbc use” class. Results from NSDUH indicated that the prevalence of past-year cocaine use was highest in non-Hispanic blacks (2.3%), followed by non-Hispanic whites (1.8%) (John & Wu, 2017). This is consistent with our finding that blaskcs were significantly more likely than whites to be in the “coc-alc-mj-tbc use” class. Our findings suggest that interventions on preventing prescription opioids and sedative polysubstance use should be targeted at older women; while interventions on preventing cocaine, alcohol, marijuana and tobacco polysubstance use should be focused on younger single blacks of both genders who had higher educational levels.
Tobacco use usually precedes the initiation of cocaine use (Kandel & Kandel, 2015). We found that even when lifetime time cocaine users stopped using cocaine (i.e. class “tbc-only use”, “alc-mj-tbc use”, and “tbc-Rx use”), they still report tobacco use in the past 30 days. In addition, among individuals in the “coc-alc-mj-tbc use” class, who were all current cocaine users, tobacco was the substance that had the highest probability of being concurrently used with cocaine. Further, all individuals in the “coc-poly use” class, who had 57% probability of current cocaine use, reported tobacco use in the past 30 days. Other studies have found similar results, with tobacco use rates being three times higher in cocaine users than in the general population (De La Garza et al., 2016). In prior studies, cocaine users who also used tobacco are more likely to use both of the substances more frequently than cocaine only users (Roll, Higgins, Budney, Bickel, & Badger, 1996). Tobacco use may increase the reinforcing effects of cocaine use and aggravate cocaine craving (Brewer, Mahoney, Nerumalla, Newton, & De La Garza, 2013). These findings highlight the importance of tobacco intervention programs (Baca & Yahne, 2009; Campbell, Le, Tajima, & Guydish, 2017). These programs may serve as prevention efforts for cocaine initiation, and as harm reduction efforts among lifetime cocaine users to reduce concurrent polysubstance use and the risk of substance use disorder.
Moreover, we identified two classes that contain current cocaine users, and both groups were concurrently using more than one substance along with cocaine. Most polysubstance use studies have focused on comparing the use of two substances to mono-substance use (Gonçalves & Nappo, 2015; Hedden et al., 2009; Leeman et al., 2016; Winhusen et al., 2013). However, previous literature has shown that polysubstance use of more than two drugs is common among cocaine users. One study in Tennessee found that concurrent cocaine, marijuana and alcohol use was one of the most common three substance use combinations among 70,427 patients from 183 mental health treatment agencies (Kedia, Sell, & Relyea, 2007). Another study found that the four substance use combinations of cocaine, prescription opioids, alcohol, and marijuana was also prevalent among community recruited non-medical prescription drug users (Acheampong, Lasopa, Striley, & Cottler, 2016). In the current analyses, a polysubstance use pattern involving six substances (cocaine, alcohol, marijuana, tobacco, prescription opioids and sedatives) was identified. Although the proportion of lifetime cocaine users classified in this class was small (2%), it provides meaningful results. Individuals in this class had the highest odds of self-reported bipolar disorder (OR = 3.11, 95% CI 1.43, 6.89) and 2.77 times the odds of anxiety compared to the “tbc-only use” class. Although the risk of depression was not statistically higher in this class, 76.5% reported having depression. In addition, the risk of having an ED visit in the past 6 months was higher than any other class (non-overlapping 95% CIs). The “coc-poly use” class was also the only group that had any probabilities of past 30-day heroin and other stimulant use. These findings highlight the importance of assessing polysubstance use beyond two-drug combinations and indicate the need for mental health screening, counseling, and overdose prevention for this group.
Furthermore, the biggest difference between the “alc-mj-tbc use” and “coc-alc-mj-tbc use” classes was that the former class had approximately zero probability of current cocaine use, while the latter had 100% probability of cocaine use. Interestingly, although the ORs in class 4 were higher than the ORs in class 2 for having a recent ED visit and having mental health conditions, the differences did not reach statistically significant levels (CIs were overlapping). From this result, it is fair to say that among lifetime cocaine users, current cocaine use is not the strongest indicator of overall risk for negative outcomes. In addition, individuals in the “tbc-Rx use” class who had no current cocaine use had significantly higher risks of having anxiety, depression, and bipolar disorder than the “tbc-only use” class. This may be because prescription sedatives are often prescribed as a treatment for many neurological and psychological conditions including anxiety, insomnia, and muscle relaxation (Griffin, Kaye, Bueno, & Kaye, 2013; Moore, Pariente, & Bégaud, 2015); prescription opioids are prescribed to treat both chronic and acute pain (Beaudoin, Lin, Guan, & Merchant, 2014; Boudreau et al., 2009). Conditions such as anxiety, insomnia, and muscle relaxation commonly co-occur with pain and that may be one possible reason for using sedatives with opioid analgesics (Holland et al., 1991; Serdarevic, Osborne, Striley, & Cottler, 2017). Both opioids and sedatives are central nervous system depressants and the combined use of both drugs can result in significant respiratory depression (Jann, Kennedy, & Lopez, 2014) and increase overdose risk (Dowell, Haegerich, & Chou, 2016; Sun et al., 2017). In our analysis, 48.6% of individuals in the “tbc-Rx use” class reported having a recent ED visit, the second highest proportion among all classes (the “coc-poly use” class was the highest which also had a high probability of prescription opioid and sedative use). Lastly, although cocaine, prescription stimulants, and amphetamines (speed) are all stimulants, our study shows that cocaine was not likely to be used with other stimulants.
4.1. Strengths and limitations
The present findings should be considered in light of several limitations. First, a cross-sectional study design was used and thus no clear temporal relationship or causality can be concluded from the observed associations. The timeframe of the questions differs. For example, substance use questions were framed as using in the past 30 days, while ED visits, and mental health questions, were framed as past 6-month and lifetime questions, respectively. It is possible that ED visits and mental health conditions tended to precede the substance use reported in this study. Second, all data were collected through self-report. Participants may have under reported their substance use patterns, even though we used the past 30-day window to increase accurate recall and the confidentiality of the data were explained. In addition, it is possible that some mental health conditions are self-diagnosed rather than diagnosed by a health professional. However, previous studies have found that self-reported mental health disorders are highly correlated with clinician-rated diagnoses (Ferdinand, 2007; Uher et al., 2012). Third, in our measurement of prescription drug use, we did not differentiate medical and non-medical use. Past studies have found that prescription drug users who also concurrently use cocaine are more likely to engage in non-medical use of prescription drugs (McCabe, Knight, Teter, & Wechsler, 2005; McCabe, West, Teter, & Boyd, 2012). Therefore, even though both “tbc-Rx use” and “coc-poly use” classes had a high probability of prescription opioid and sedative use, it is possible that more lifetime cocaine users in the “coc-poly use” class were using these drugs non-medically than those in the “tbc-Rx use” class. Lastly, the study did not attempt to ask participants about their frequency and quantity of substance use, the sequence of how different substances were used together or the presence/absence of substance use disorder. Future polysubstance use studies should consider including this information in their measurement to further assess cocaine polysubstance use patterns. We also do not have information to differentiate crack cocaine users from powder cocaine users and it is possible that crack users endorsed slightly different polysubstance use patterns than powder cocaine users (Gossop, Manning, & Ridge, 2006).
Despite these limitations, the current study, to our knowledge, is the first latent class analysis conducted among lifetime cocaine users to examine their past 30-day substance use patterns. A broad range of substances was measured to better determine the patterns. We also included a brief class description of different class number solutions in hoping that this information can help other researchers to replicate and reproduce the results. In addition, the study sample was a large diverse community sample with a large sub-sample of lifetime cocaine users (n = 1797). This increases the generalizability of the study findings. Since the study is community-based, the findings can be used to directly guide local interventions to target at the burdens and the needs of the community.
5. Conclusions
Overall, these results highlight that there are different past 30-day substance use patterns among lifetime cocaine users. Most of the lifetime cocaine users reported no cocaine use in the past 30 days. Approximately 11% of lifetime cocaine users used cocaine in the past 30 days with two different concurrent substance use patterns: one class featured concurrent cocaine, alcohol, marijuana and tobacco use; another featured concurrent polysubstance use involving six substances. In addition, we found that among lifetime cocaine users, current cocaine use is not the strongest indicator of overall risk for negative outcomes, rather prescription medication use and complex polysubstance use patterns are stronger indicators of greater risk. Moreover, past 30-day tobacco use is common among lifetime cocaine users regardless of class membership. Lastly, we found cocaine is not likely to be used with other stimulants such as prescription stimulants, and amphetamines (speed).
Conflict of interests
None to declare.
Acknowledgments
HealthStreet program is supported by the Clinical and Translational Science Institute (CTSI) and the University of Florida (UF) College of Public Health & Health Professions and College of Medicine. Clinical and Translational Science Institute is supported in part by the National Institutes of Health/National Centre for Advancing Translational Sciences Clinical and Translational Science Award to the University of Florida [Grant Number UL1 TR001427].
References
- Acheampong A.B., Lasopa S., Striley C.W., Cottler L.B. Gender differences in the association between religion/spirituality and Simultaneous Polysubstance Use (SPU) Journal of Religion and Health. 2016;55(5):1574–1584. doi: 10.1007/s10943-015-0168-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agrawal A., Lynskey M.T., Madden P.A., Bucholz K.K., Heath A.C. A latent class analysis of illicit drug abuse/dependence: Results from the National Epidemiological Survey on Alcohol and Related Conditions. Addiction. 2007;102(1):94–104. doi: 10.1111/j.1360-0443.2006.01630.x. [DOI] [PubMed] [Google Scholar]
- Al-Tayyib A.A., Rice E., Rhoades H., Riggs P. Association between prescription drug misuse and injection among runaway and homeless youth. Drug and Alcohol Dependence. 2014;134:406–409. doi: 10.1016/j.drugalcdep.2013.10.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baca C.T., Yahne C.E. Smoking cessation during substance abuse treatment: What you need to know. Journal of Substance Abuse Treatment. 2009;36(2):205–219. doi: 10.1016/j.jsat.2008.06.003. [DOI] [PubMed] [Google Scholar]
- Beaudoin F.L., Lin C., Guan W., Merchant R.C. Low-dose ketamine improves pain relief in patients receiving intravenous opioids for acute pain in the emergency department: Results of a randomized, double-blind, clinical trial. Academic Emergency Medicine. 2014;21(11):1193–1202. doi: 10.1111/acem.12510. [DOI] [PubMed] [Google Scholar]
- Blow F.C., Walton M.A., Barry K.L., Murray R.L., Cunningham R.M., Massey L.S. Alcohol and drug use among patients presenting to an inner-city emergency department: A latent class analysis. Addictive Behaviors. 2011;36(8):793–800. doi: 10.1016/j.addbeh.2010.12.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borders T.F., Booth B.M. Stimulant use, religiosity, and the odds of developing or maintaining an alcohol use disorder over time. Journal of Studies on Alcohol and Drugs. 2013;74(3):369–377. [PMC free article] [PubMed] [Google Scholar]
- Boudreau D., Von Korff M., Rutter C.M., Saunders K., Ray G.T., Sullivan M.D. Trends in long-term opioid therapy for chronic non-cancer pain. Pharmacoepidemiology and Drug Safety. 2009;18(12):1166–1175. doi: 10.1002/pds.1833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer A.J., Mahoney J.J., Nerumalla C.S., Newton T.F., De La Garza R. The influence of smoking cigarettes on the high and desire for cocaine among active cocaine users. Pharmacology, Biochemistry, and Behavior. 2013;106:132–136. doi: 10.1016/j.pbb.2013.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell B.K., Le T., Tajima B., Guydish J. Quitting smoking during substance use disorders treatment: Patient and treatment-related variables. Journal of Substance Abuse Treatment. 2017;73:40–46. doi: 10.1016/j.jsat.2016.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Celeux G., Soromenho G. An entropy criterion for assessing the number of clusters in a mixture model. Journal of Classification. 1996:195–212. [Google Scholar]
- Chen L.Y., Crum R.M., Martins S.S., Kaufmann C.N., Strain E.C., Mojtabai R. Patterns of concurrent substance use among nonmedical ADHD stimulant users: Results from the National Survey on Drug Use and Health. Drug and Alcohol Dependence. 2014;142:86–90. doi: 10.1016/j.drugalcdep.2014.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Boni R.B., Bastos F.I., de Vasconcellos M., Oliveira F., Limberger R.P., Pechansky F. Drug use among drivers who drank on alcohol outlets from Porto Alegre, Brazil. Accident; Analysis and Prevention. 2014;62:137–142. doi: 10.1016/j.aap.2013.09.017. [DOI] [PubMed] [Google Scholar]
- De La Garza R., Yoon J.H., Thompson-Lake D.G., Haile C.N., Eisenhofer J.D., Newton T.F. Treadmill exercise improves fitness and reduces craving and use of cocaine in individuals with concurrent cocaine and tobacco-use disorder. Psychiatry Research. 2016;245:133–140. doi: 10.1016/j.psychres.2016.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dowell D., Haegerich T.M., Chou R.C.D.C. Guideline for prescribing opioids for chronic pain–United States, 2016. JAMA. 2016;315(15):1624–1645. doi: 10.1001/jama.2016.1464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans E., Kelleghan A., Li L., Min J., Huang D., Urada D. Gender differences in mortality among treated opioid dependent patients. Drug and Alcohol Dependence. 2015;155:228–235. doi: 10.1016/j.drugalcdep.2015.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans-Polce R., Lanza S., Maggs J. Heterogeneity of alcohol, tobacco, and other substance use behaviors in U.S. college students: A latent class analysis. Addictive Behaviors. 2016;53:80–85. doi: 10.1016/j.addbeh.2015.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferdinand R.F. Predicting anxiety diagnoses with the youth self-report. Depression and Anxiety. 2007;24(1):32–40. doi: 10.1002/da.20186. [DOI] [PubMed] [Google Scholar]
- Florida Drug-Related Outcomes Surveillance and Tracking System Drug-caused deaths per 100,000 population. 2003–2016. https://frost.med.ufl.edu/frost/2018
- Gonçalves J.R., Nappo S.A. Factors that lead to the use of crack cocaine in combination with marijuana in Brazil: A qualitative study. BMC Public Health. 2015;15:706. doi: 10.1186/s12889-015-2063-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gossop M., Manning V., Ridge G. Concurrent use of alcohol and cocaine: Differences in patterns of use and problems among users of crack cocaine and cocaine powder. Alcohol and Alcoholism. 2006;41(2):121–125. doi: 10.1093/alcalc/agh260. [DOI] [PubMed] [Google Scholar]
- Griffin C.E., Kaye A.M., Bueno F.R., Kaye A.D. Benzodiazepine pharmacology and central nervous system-mediated effects. The Ochsner Journal. 2013;13(2):214–223. [PMC free article] [PubMed] [Google Scholar]
- Hedden S.L., Malcolm R.J., Latimer W.W. Differences between adult non-drug users versus alcohol, cocaine and concurrent alcohol and cocaine problem users. Addictive Behaviors. 2009;34(3):323–326. doi: 10.1016/j.addbeh.2008.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herman-Stahl M.A., Krebs C.P., Kroutil L.A., Heller D.C. Risk and protective factors for nonmedical use of prescription stimulants and methamphetamine among adolescents. The Journal of Adolescent Health. 2006;39(3):374–380. doi: 10.1016/j.jadohealth.2006.01.006. [DOI] [PubMed] [Google Scholar]
- Holland J.C., Morrow G.R., Schmale A., Derogatis L., Stefanek M., Berenson S. A randomized clinical trial of alprazolam versus progressive muscle relaxation in cancer patients with anxiety and depressive symptoms. Journal of Clinical Oncology. 1991;9(6):1004–1011. doi: 10.1200/JCO.1991.9.6.1004. [DOI] [PubMed] [Google Scholar]
- Hou S., Zhan M., Zheng X., Zhan C.G., Zheng F. Kinetic characterization of human butyrylcholinesterase mutants for the hydrolysis of cocaethylene. The Biochemical Journal. 2014;460(3):447–457. doi: 10.1042/BJ20140360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jann M., Kennedy W.K., Lopez G. Benzodiazepines: A major component in unintentional prescription drug overdoses with opioid analgesics. Journal of Pharmacy Practice. 2014;27(1):5–16. doi: 10.1177/0897190013515001. [DOI] [PubMed] [Google Scholar]
- John W.S., Wu L.T. Trends and correlates of cocaine use and cocaine use disorder in the United States from 2011 to 2015. Drug and Alcohol Dependence. 2017;180:376–384. doi: 10.1016/j.drugalcdep.2017.08.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kandel D., Kandel E. The gateway hypothesis of substance abuse: Developmental, biological and societal perspectives. Acta Paediatrica. 2015;104(2):130–137. doi: 10.1111/apa.12851. [DOI] [PubMed] [Google Scholar]
- Kedia S., Sell M.A., Relyea G. Mono-versus polydrug abuse patterns among publicly funded clients. Substance Abuse Treatment, Prevention, and Policy. 2007;2:33. doi: 10.1186/1747-597X-2-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly P.J., Robinson L.D., Baker A.L., Deane F.P., McKetin R., Hudson S. Polysubstance use in treatment seekers who inject amphetamine: Drug use profiles, injecting practices and quality of life. Addictive Behaviors. 2017;71:25–30. doi: 10.1016/j.addbeh.2017.02.006. [DOI] [PubMed] [Google Scholar]
- Lanza S.T., Collins L.M., Lemmon D.R., Schafer J.L. PROC LCA: A SAS procedure for latent class analysis. Structural Equation Modeling. 2007;14(4):671–694. doi: 10.1080/10705510701575602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leeman R.F., Sun Q., Bogart D., Beseler C.L., Sofuoglu M. Comparisons of cocaine-only, opioid-only, and users of both substances in the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Substance Use & Misuse. 2016;51(5):553–564. doi: 10.3109/10826084.2015.1122063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y., Williamson V., Setlow B., Cottler L., Knackstedt L. The importance of considering polysubstance use: Lessons from cocaine research (in press) Drug and Alcohol Dependence. 2018;192:16–28. doi: 10.1016/j.drugalcdep.2018.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lo Y., Mendell N., Rubin D. Testing the number of components in a normal mixture. Biometrika. 2001:767–778. [Google Scholar]
- Lubke G.H., Muthén B. Investigating population heterogeneity with factor mixture models. Psychological Methods. 2005;10(1):21–39. doi: 10.1037/1082-989X.10.1.21. [DOI] [PubMed] [Google Scholar]
- Macdonald S., Pakula B., Martin G., Wells S., Borges G., Roth E. Health profiles of clients in substance abuse treatment: A comparison of clients dependent on alcohol or cocaine with those concurrently dependent. Substance Use & Misuse. 2014;49(14):1899–1907. doi: 10.3109/10826084.2014.935791. [DOI] [PubMed] [Google Scholar]
- McCabe S.E., Knight J.R., Teter C.J., Wechsler H. Non-medical use of prescription stimulants among US college students: Prevalence and correlates from a national survey. Addiction. 2005;100(1):96–106. doi: 10.1111/j.1360-0443.2005.00944.x. [DOI] [PubMed] [Google Scholar]
- McCabe S.E., West B.T., Teter C.J., Boyd C.J. Co-ingestion of prescription opioids and other drugs among high school seniors: Results from a national study. Drug and Alcohol Dependence. 2012;126(1–2):65–70. doi: 10.1016/j.drugalcdep.2012.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore N., Pariente A., Bégaud B. Why are benzodiazepines not yet controlled substances? JAMA Psychiatry. 2015;72(2):110–111. doi: 10.1001/jamapsychiatry.2014.2190. [DOI] [PubMed] [Google Scholar]
- NIDA . 2015. Drug factors: Nationwide trends. [Google Scholar]
- Nylund L.K., Asparouhov T., Muthén O.B. Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Structural Equation Modeling: A Multidisciplinary Journal. 2007;14(7):535–569. [Google Scholar]
- Ojha S.P., Sigdel S., Meyer-Thompson H.G., Oechsler H., Verthein U. 'South Asian cocktail'–The concurrent use of opioids, benzodiazepines and antihistamines among injecting drug users in Nepal and associations with HIV risk behaviour. Harm Reduction Journal. 2014;11:17. doi: 10.1186/1477-7517-11-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oviedo-Joekes E., Sordo L., Guh D., Marsh D.C., Lock K., Brissette S. Predictors of non-use of illicit heroin in opioid injection maintenance treatment of long-term heroin dependence. Addictive Behaviors. 2015;41:81–86. doi: 10.1016/j.addbeh.2014.10.003. [DOI] [PubMed] [Google Scholar]
- Quek L.H., Chan G.C., White A., Connor J.P., Baker P.J., Saunders J.B. Concurrent and simultaneous polydrug use: Latent class analysis of an Australian nationally representative sample of young adults. Frontiers in Public Health. 2013;1:61. doi: 10.3389/fpubh.2013.00061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramo D.E., Grov C., Delucchi K.L., Kelly B.C., Parsons J.T. Cocaine use trajectories of club drug-using young adults recruited using time-space sampling. Addictive Behaviors. 2011;36(12):1292–1300. doi: 10.1016/j.addbeh.2011.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roll J.M., Higgins S.T., Budney A.J., Bickel W.K., Badger G.J. A comparison of cocaine-dependent cigarette smokers and non-smokers on demographic, drug use and other characteristics. Drug and Alcohol Dependence. 1996;40(3):195–201. doi: 10.1016/0376-8716(96)01219-7. [DOI] [PubMed] [Google Scholar]
- Scherer M., Harrell P., Romano E. Marijuana and other substance use among motor vehicle operators: A latent class analysis. Journal of Studies on Alcohol and Drugs. 2015;76(6):916–923. doi: 10.15288/jsad.2015.76.916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz B., Wetzler S., Swanson A., Sung S.C. Subtyping of substance use disorders in a high-risk welfare-to-work sample: A latent class analysis. Journal of Substance Abuse Treatment. 2010;38(4):366–374. doi: 10.1016/j.jsat.2010.03.001. [DOI] [PubMed] [Google Scholar]
- Serdarevic M., Osborne V., Striley C.W., Cottler L.B. The association between insomnia and prescription opioid use: Results from a community sample in Northeast Florida. Sleep Health. 2017;3(5):368–372. doi: 10.1016/j.sleh.2017.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiu-Yee K., Brincks A.M., Feaster D.J., Frimpong J.A., Nijhawan A., Mandler R.N. Patterns of substance use and arrest histories among hospitalized HIV drug users: A latent class analysis. AIDS and Behavior. 2018;22(9):2757–2765. doi: 10.1007/s10461-017-2024-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun E.C., Dixit A., Humphreys K., Darnall B.D., Baker L.C., Mackey S. Association between concurrent use of prescription opioids and benzodiazepines and overdose: Retrospective analysis. BMJ. 2017;356:j760. doi: 10.1136/bmj.j760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Office of National Drug Control Policy (ONDCP) 2018. New annual data released by White House Drug Policy Office shows record high cocaine cultivation and production in Colombia.https://www.whitehouse.gov/briefings-statements/new-annual-data-released-white-house-drug-policy-office-shows-record-high-cocaine-cultivation-production-colombia/2018 Retrieved from. [Google Scholar]
- Trenz R.C., Scherer M., Duncan A., Harrell P.T., Moleko A.G., Latimer W.W. Latent class analysis of polysubstance use, sexual risk behaviors, and infectious disease among South African drug users. Drug and Alcohol Dependence. 2013;132(3):441–448. doi: 10.1016/j.drugalcdep.2013.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uher R., Perlis R.H., Placentino A., Dernovšek M.Z., Henigsberg N., Mors O. Self-report and clinician-rated measures of depression severity: Can one replace the other? Depression and Anxiety. 2012;29(12):1043–1049. doi: 10.1002/da.21993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White A., Chan G.C., Quek L.H., Connor J.P., Saunders J.B., Baker P. The topography of multiple drug use among adolescent Australians: Findings from the National Drug Strategy Household Survey. Addictive Behaviors. 2013;38(4):2068–2073. doi: 10.1016/j.addbeh.2013.01.001. [DOI] [PubMed] [Google Scholar]
- Winhusen T.M., Adinoff B., Lewis D.F., Brigham G.S., Gardin J.G., Sonne S.C. A tale of two stimulants: Mentholated cigarettes may play a role in cocaine, but not methamphetamine, dependence. Drug and Alcohol Dependence. 2013;133(3):845–851. doi: 10.1016/j.drugalcdep.2013.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]