Abstract
Purpose of Review
Heterotopic ossification (HO) in hip arthroscopy is a common post-operative complication. This review was undertaken to provide an update (2014 present) on the current literature regarding HO in hip arthroscopy.
Recent Findings
Risk factors for HO post-hip arthroscopy include male gender, mixed impingement, picture, and the size of CAM resection. HO prophylaxis with NSAIDs has been proven to decrease the rate of HO post-hip arthroscopy; however, there is inherent risk to long-standing NSAIDs therapy. HO post-hip arthroscopy is not uncommon as a radiological finding, but symptomatic HO post-hip arthroscopy requiring revision surgery is a rare event, at < 1%. The outcomes for revision surgery for HO excision have fair outcomes.
Summary
The hip arthroscopist should stratify their patients based on known risk factors, and determine whether NSAIDs prophylaxis is warranted.
Keywords: Hip arthroscopy, Heterotopic ossification, Prophylaxis, NSAIDs, Complication, Revision surgery
Introduction
Heterotopic ossification (HO) post-hip arthroscopy is a known complication which is not uncommon. The incidence of HO post-hip arthroscopy has been reported as high as 46% [1••]; however, most studies evaluating the incidence of HO in hip arthroscopy report a 1–12% range of occurrence [2–6]. It still remains unclear how many of these reported cases are symptomatic versus simply a radiographic HO diagnosis, and whether there is any clinical relevance. A significant amount of work has been published surrounding this topic since 2014, including 12 articles specifically dedicated to discussing HO in hip arthroscopy (Table 1) [1••, 7•, 8•, 9•, 10, 11•, 12•, 13•, 14•, 15•, 16•, 17]. There are another 45 articles published in a general review of complications post-hip arthroscopy which included non-specific discussions about HO. As hip arthroscopy is a rapidly evolving topic in the orthopedic literature, this review has been restricted to publications within the most recent 5 years (2014–2018 inclusive) to allow for a comprehensive yet succinct update on the topic.
Table 1.
List of publications commenting specifically on heterotopic ossification and hip arthroscopy between 2014 and 2018, inclusive
| Authors | Journal | Year | LOE | Conclusions |
|---|---|---|---|---|
| Beckmann et al. [7•] | AJSM | 2014 | 3; CS |
Prophylactic therapy: 500 mg naproxen BID for 3 weeks. At risk: mixed impingement (osteoplasty, rim trim) Results: no prophylaxis = 16.6 times more chance of HO Complications: ARF, hematochezia, acute colitis/gastritis |
| Uquillas and Youm [8•] | JBJS | 2014 | 5; CR | Small symptomatic lesions may be treated with US-guided pulsed lavage. N = 1 Case study. |
| Amar et al. [9•] | Arthroscopy | 2015 | 3; RR |
Prophylactic therapy: none Results: control group (capsule left open) 44% HO; study group (capsule closure) 28% HO. Not statistically significant |
| Amar et al. [10] | JHPS | 2015 | 5; LR | Review paper outlining incidence, risk factors, diagnosis, prophylactic measures, management of HO in hip arthroscopy. |
| Beckmann et al. [1••] | JBJS | 2015 | 1; RCT |
Prophylactic therapy: 500 mg naproxen BID for 3 weeks Results: study was stopped as the efficacy of naproxen group was clearly demonstrated at midterm analysis (46% HO in placebo vs 4% in naproxen group). Complications: adverse events were equal between placebo and naproxen groups |
| Loken, S [11•] | JBJS—commentary | 2015 | 5; EO | Provides commentary and expert opinion on the above RCT authored by Beckmann et al. Only 1 symptomatic HO pt. was revised due to HO. The rest was radiographic HO. Must consider negative effects on repaired labrum and/or capsule as well as innate NSAID risks. |
| Rath et al. [12•] | AJSM | 2015 | 3; CS |
Prophylactic therapy: 600 mg etodolac (COX-2 inhibitor) daily for 2 weeks. Results: 36% HO in control group (no NSAIDs); 0% HO in study group (etodolac). Complications: 2 discontinued prophylaxis for GI symptoms |
| Yeung et al. [13•] | Arthroscopy | 2016 | 3; SR |
1662 patients investigating NSAIDs prophylaxis in hip arthroscopy. Prophylactic therapy: variable Results: incidence 13.4% HO without NSAIDs, 3.3% HO with NSAIDs prophylaxis. Most patients were asymptomatic. Complications: not consistently reported. |
| Miller, GK [14•] | Arthroscopy—commentary | 2016 | 5; EO | Provides commentary and expert opinion on the above systematic review authored by Yeung et al. Must consider negative effects NSAIDs when using as prophylaxis. Low rate of symptomatic HO post-hip arthroscopy. |
| Redmond et al. [15•] | JHPS | 2017 | 3; RR |
Prophylactic therapy: aspirin 325 mg BID for 6 weeks Results: revision hip arthroscopy for HO excision demonstrated overall improvement; however, few achieved good to excellent results. Complications: 21% conversion to THA or re-revision hip scope. |
| Warschawski et al. [16•] | JOCR | 2017 | 5; CR |
Prophylactic therapy: left hip (none), right hip (etodolac 600 mg daily for 2 weeks) Results: grade 3 HO on the left hip (asymptomatic), no HO on the right hip. Suggests routine HO prophylaxis. Complications: Nil, N = 1 case study. |
| Barth et al. [17] | JOSPT | 2018 | 5; CR |
Prophylactic therapy: non-specific Re-revised for HO excision, with indomethacin post-op and pain resolved. N = 1 case study. |
AJSM, American Journal of Sports Medicine; JBJS, Journal of Bone and Joint Surgery; Arthroscopy, The Journal of Arthroscopic and Related Surgery; JOSPT, Journal of Orthopedics and Sports Physical Therapy; JHPS, Journal of Hip Preservation Surgery; JOCR, Journal of Orthopedic Case Reports; CS, cohort study; CR, case report; RCT, randomized controlled trial; SR, systematic review; RR, retrospective review; EO, expert opinion; LR, literature review
Background
HO is a process where normal bone forms in locations such as extraskeletal soft tissue. HO is known to form in traumatic, inflammatory, and post-surgical settings. HO is dependent on three common parameters to allow formation: (1) an inflammatory process, (2) available and local osteogenic cells, and (3) a vascular rich environment [18]. The HO formation process has been investigated extensively; however, the exact molecular pathway has yet to be established. In general, inflamed and traumatized tissue starts to be replaced by bone. Specific to the hip, this bone formation can then be asymptomatic or symptomatic manifesting as pain, impingement, or decreased range of motion [8•, 10, 19]. The symptomatology of the HO will then guide the appropriate management.
The Brooker classification is a radiological classification developed in 1973 to help categorize HO post-hip arthroplasty [20]. There are 4 types of HO as described by Brooker (Table 2). This classification system has been borrowed from the total hip arthroplasty literature for use in hip arthroscopy. This classification helps the orthopedic community use common verbiage when discussing HO surrounding the hip joint.
Table 2.
Brooker classification of heterotopic ossification [20]
| Degree | Description |
|---|---|
| I | Islands of bone within the soft tissue about the hip |
| II | Bone spurs from the pelvis or proximal end of the femur, leaving at least 1 cm between opposing bone surfaces |
| III | Bone spurs from the pelvis or proximal end of the femur, reducing the space between opposing bone surfaces to less than 1 cm |
| IV | Apparent bone ankylosis of the hip |
Study Selection
Eligibility Criteria
A systematic search was carried out to identify all publications containing data on the topic of HO and relation to hip arthroscopy. Included were any publications that included topics related to hip arthroscopy, HO, and perioperative management of HO. Excluded were publications that dated prior to 2014, that did not include hip arthroscopy or HO, were conference abstracts, or were published in languages other than English.
Identification of Studies
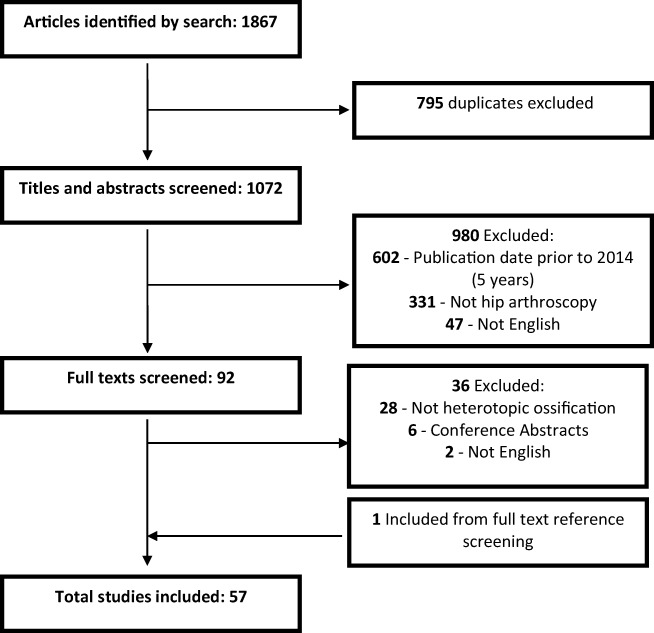
A systematic electronic search was performed using EMBASE, MEDLINE via Ovid, and PubMed for electronic publications ahead of print (with no date limits to August 2018). A combination of MeSH headings were used as outlined in Table 3. After exclusion of duplicates, titles and abstracts were screened based on our eligibility criteria by two independent reviewers (AK, EL). The remaining studies then underwent a full-text screen based on these criteria. A total of 57 studies were included (Fig. 1), 12 articles which discussed specifically HO in hip arthroscopy and another 45 articles published on a general review of complications post-hip arthroscopy which included non-specific discussions about HO.
Table 3.
MeSH headings used for electronic search strategy for Ovid Medline, and PubMed
| # | MeSH headings |
|---|---|
| 1 | Hip arthroscopy.mp. or hip arthroscopy/ |
| 2 | Heterotopic ossification.mp. or heterotopic ossification/ |
| 3 | Heterotopic ossification.mp. or heterotopic ossification/ |
| 4 | Femoroacetabular impingement.mp. or femoroacetabular impingement/ |
| 5 | Indomethacin.mp. or indomethacin/ |
| 6 | Radiation.mp. or radiation/ |
| 7 | Irradiation.mp. or irradiation/ |
| 8 | Complications.mp. or complications/ |
Fig. 1.
Flowchart depicting eligibility criteria
Discussion
Risk Factors
The literature has supported in the past the classic risk factors for HO post-hip arthroplasty. These include male gender, type of arthritis, previous surgery, trauma, inflammatory conditions, head injury, and others [21]. Knowledge of hip arthroscopy-specific risk factors for HO is important to the hip arthroscopy surgeon, as this allows for appropriate stratification for possible post-operative prophylaxis. The literature prior to 2014 has shown that male gender, femoral osteoplasty, and unrepaired capsulotomy were risk factors for HO post-hip arthroscopy [5, 19]. In the recent 5 years, this has been confirmed by Beckmann et al. who show that risk of HO is increased with a mixed impingement picture requiring simultaneous rim trim and femoral osteoplasty [7•]. Furthermore, degree of resection of the CAM lesion may be predictive of HO, where a larger CAM requiring a larger resection may be at an increased risk for HO development [7•]. In Beckman et al. study, there was a trend towards unrepaired capsulotomy increasing the risk for HO, but the authors did state a larger data set would be needed to draw any firm conclusion regarding repaired versus unrepaired capsulotomy and HO formation [7•]. A recent study showed that capsular closure does not affect the rate of post-operative HO [9•].
In summary, risk factors may include male gender, mixed impingement picture where combined rim trim and femoral osteoplasty is required, the volume of CAM resected based on the alpha angle, and unrepaired capsulotomy in the setting of bony correction.
Location
HO mass formation post-hip arthroscopy most commonly occurs at the anterior aspect of the hip [1••, 7•]. There is no convincing evidence that the formation of HO has a pattern other than spatial location at the anterior hip. At this point, it is hard to determine why some HO forms closer to the capsule versus in the abductor musculature [11•]. This anterior location may be more irritating to patients especially during hip flexion. The more lateral-based HO formations may be less symptomatic, but the literature is unclear about this.
In summary, location of HO formation is usually anterior hip joint and can be deep in the capsule area (Figs. 2 and 3) and cause range of motion deficits, pain, and impingement symptoms during hip flexion. More lateral HO in the abductor musculature may be less symptomatic.
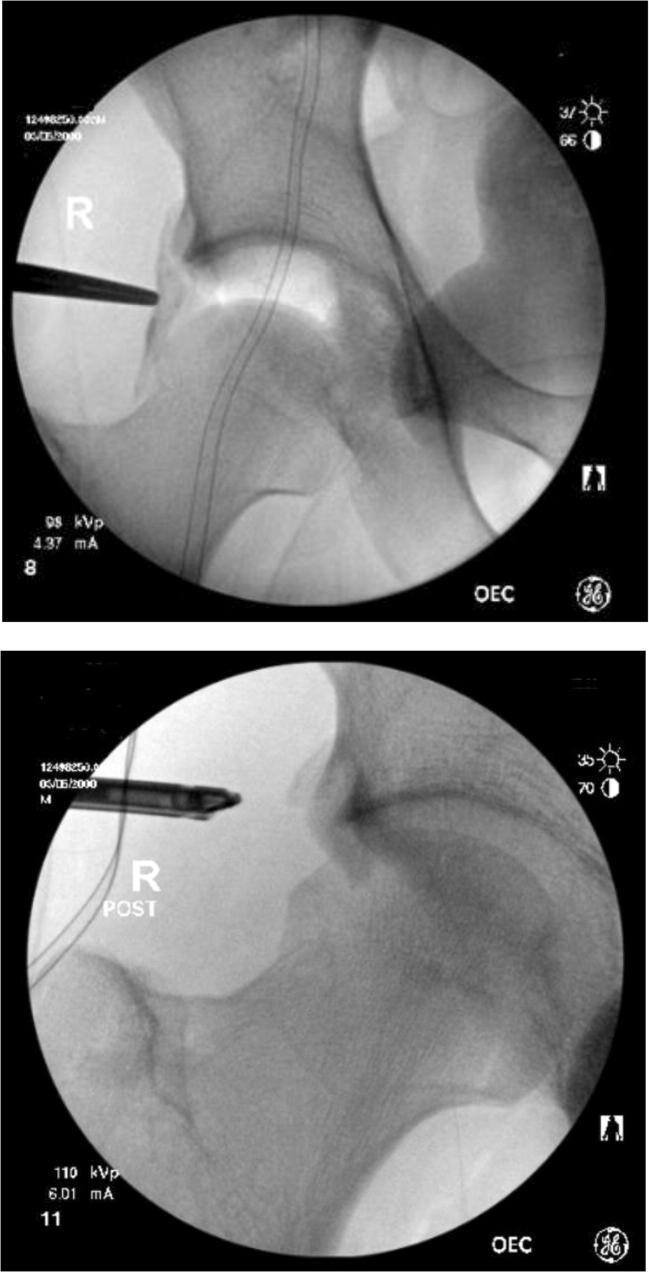
Fig. 2.
18-year-old male athlete with formation of grade 3 HO at the anterolateral hip capsule (iliofemoral ligament) post-hip arthroscopy for FAI. Patient was exhibiting restricted ROM and impingement pain not responding to conservative measures
Fig. 3.
Fluoroscopic images of the same patient during arthroscopic excision of HO. Pre-excision and post-excision are shown
Prophylaxis
Prophylaxis against HO post-hip arthroscopy can come in a variety of forms; however, the most common is NSAIDs. Frequently used NSAIDs in the past 5 years of literature are shown in Table 4. Naproxen 500 mg (mg), orally twice a day for 3 weeks, seems to be the most common choice of prophylaxis [1••, 7•, 13•]. The only randomized controlled trial (RCT) in the recent literature shows that naproxen 500 mg, orally twice a day for 3 weeks, decreases the HO rate post-hip arthroscopy from 46% (placebo group) to 4% (naproxen group) [1••]. In a retrospective review published in 2016, 600 mg of etodolac daily for 2 weeks was used, and the reported rate of HO in the no prophylaxis group was 36%, whereas in the etodolac group was 0% [12•].
Table 4.
List of documented NSAIDs prophylactic regiments in the recent literature 2014–2018
| Generic drug name (brands) | Dose, frequency, and duration | Advantages | Disadvantages |
|---|---|---|---|
| Naproxen (Naprosyn) | 500 mg BID for 3 weeks |
• Nonselective COX-inhibitor, less cardiac risks [22]. |
• Nonselective COX-inhibitor, more GI risks [23] • Less compliance (GI upset) |
| Etodolac (Lodine) | 600 mg daily for 2 weeks |
• Selective COX-2 inhibitor, more cardiac risks [22] • One-day dose (increases compliance) • Lower duration |
• Selective COX-2 inhibitor, less GI irritation increases compliance [23] |
| Acetylsalicylic acid (Aspirin) | 325 mg BID for 6 weeks |
• Nonselective COX-inhibitor, less cardiac risk [22] • Added VTE prophylaxis benefit |
• Nonselective COX-inhibitor, more GI risk [23] • Platelet inhibitor, bleeding risk |
VTE, venous thromboembolism; BID, twice daily; COX, cyclooxygenase; mg, milligrams
It has been recently shown that radiation is the most efficacious method at preventing HO formation after total hip arthroplasty (THA) [24]. External beam radiation is usually reserved for post-HO excision or revision cases as it does have a higher risk profile than NSAIDs [24]. It is also less readily available than NSAIDs. External beam radiation has not been used extensively in hip arthroscopy cases. The usual dose would be 700 cGy one-time dose within < 4 h pre-operatively to < 72 h post-operatively [25, 26].
In summary, HO prophylaxis with NSAIDs has been proven to decrease the rate of HO post-hip arthroscopy. There are a variety of possible NSAIDs regiments each with their respective benefits and risks (Table 4). External beam radiation is not reported in hip arthroscopy for HO prophylaxis and should be reserved for recurrent, hard to treat cases. Care must be taken to educate the patient population about this risk of sarcoma formation post-radiation therapy, albeit exceedingly rare in a single-dose regiment such as in HO prophylaxis.
Symptomatic HO
The chance of HO development as a post-operative complication should be discussed with the patient pre-operatively to allow for anticipation and avoid difficult follow-up conversations. However, the majority of HO is asymptomatic and therefore does not require intervention. Of those who have HO post-hip arthroscopy, only 25% are symptomatic and undergo excision or revision surgery [5, 7•]. However, an RCT published in 2015 which is the best available evidence did show that only one patient out of a total 106 patient study required revision surgery for symptomatic HO, a less than 1% revision rate [1••, 11•]. Albeit, the revision patient was in the placebo group and the statistical significance was not commented on in the paper. Other studies, who document a large reduction in HO post-hip arthroscopy with NSAIDs prophylaxis, do not make any comment on symptomatology, which is a considerable weakness as it is important to know what the clinical benefit, and not just the radiological benefit, may be [12•]. There has been significant disagreement with perspective of the significance of HO post-hip arthroscopy in the literature which has been outlined in multiple editorial commentaries published [11•, 14•].
In summary, HO post-hip arthroscopy is not uncommon as a radiological finding. Symptomatic HO post-hip arthroscopy requiring revision surgery is a rare event, < 1% [1••].
Interventional Radiology
Ultrasound (US)-guided lavage has been used in the past for other calcified soft tissue entities such as calcific tendinitis of the rotator cuff with reasonable results [27, 28]. The literature is scarce on adopting this technique for HO management; however, a single-case report discusses this technique for HO in hip arthroscopy and shows good result [8•]. A 51-year-old male patient post-hip arthroscopy had symptomatic HO which did not respond to physiotherapy and oral medications. This patient underwent US-guided lavage of the HO mass and subsequent therapeutic steroid injected into the area. Resolution of the HO both radiographically as well as clinically (resolution of pain) occurred at the 6-month mark with no complications [8•]. Albeit, the recommendation is for small lesions only and this paper treated a Brooker 1 HO mass measuring 1.3 × 0.08 × 1.1 cm.
In summary, small Brooker 1 HO bony masses which are symptomatic but perhaps too small for surgical excision could go through a trial treatment of US-guided lavage therapy, knowing there is a lack of strong evidence for this intervention.
Revision Surgery
Those requiring intervention such as revision surgery for HO excision is a rarity [1••, 11•, 19] and is patient specific depending on pain, impingement, and decreased range of motion. Nonetheless, the surgeon must be aware of relevant patient workup as well as management options available to them. Prior to deciding on an arthroscopic versus open approach, an imaging workup is mandated. It is our preference, depending on the location and the size of the HO mass, for consideration of computed tomography (CT) angiogram as a part of the pre-operative imaging workup. This is a prudent step as if there is any concern for proximity to major vessels; the CT angiogram will be able to confirm abutment or encasement within the HO mass. This should then prompt the orthopedic surgeon to avoid arthroscopic excision, and plan for an open excision with either vascular or plastic surgery colleagues available to minimize vascular complications.
Redmond et al. reported on a group of 19 patients who had revision surgery for HO excision. They used modified Harris hip score (mHHS) for patient-reported outcomes and found average 20-point increase in the mHHS; however, most remained in the “fair” range. Likewise, there were only 3 patients with a mHHS over 80 (good to excellent results) [15•].
In summary, revision surgery for HO excision may be necessary in symptomatic individuals, and post-operative NSAIDs prophylaxis would be warranted in these situations. The results of revision surgery have been reported as “fair,” with limited patients getting good to excellent results [15•].
Risk of NSAIDs Prophylaxis
NSAIDs are known to put the gastrointestinal (GI) system and genitourinary system at risk. There is inherent risk to routine prophylaxis with NSAIDs as outlined in Table 4, including GI irritation, stomach ulceration, bleeding, and acute kidney injury. Beckmann et al. found in their 2014 study that 2 patients had serious complications; 1 patient developed acute kidney injury, and another patient acute colitis leading to hematochezia [7•]. Furthermore, in their RCT published in 2015, out of the 106 combined patients in both the placebo and naproxen group a total of 41 adverse events were documented, 19 in the placebo group and 22 in the naproxen group [1••]. To reduce the GI side effects, a selective COX-2 inhibitor can be used. In 2016, Rath et al. used etodolac 600-mg oral daily for 2 weeks. They had 2 adverse GI events in the form of stomach irritation, and no bleeding was documented. They argue the selective COX-2 inhibitor provides same prophylactic HO effect with less GI side effects. Furthermore, they cut their duration down to 2 weeks to help with the side-effect risk profile [12•].
In summary, the argument has been made that clinical benefit of routine prophylaxis is still largely unknown. There are obvious negative effects such as GI upset, bleeding, and kidney failure and some more theoretical negative effects such as healing potential of a repaired labrum [11•]. Our recommendation to mitigate GI side effects is to couple the NSAIDs with gastric protection for the duration of the NSAIDs use.
Conclusion
There is enough literature to note that heterotopic ossification post-hip arthroscopy is a relatively common complication of surgery. There is also evidence that prophylaxis significantly decreases the rate of radiographic HO post-hip arthroscopy. There are specific risk factors for HO in hip arthroscopy which may guide the hip arthroscopist to stratify patient risk and adopt one of the many different prophylactic NSAIDs regiments available, albeit not without medication adverse events. However, it is prudent to consider and acknowledge the difference between radiographic diagnosis of HO versus symptomatic HO requiring intervention. In the most recent 5 years, symptomatic HO requiring revision surgery post-hip arthroscopy has been shown in the 1–25% range. Revision surgery for HO excision has fair clinical results. Post-revision surgery for HO, consideration of a 1 dose of 700-cGy treatment of external beam radiation within 72 h of the procedure and adjuvant NSAIDs coupled with gastric protection would be prudent to try to curb recurrence.
Compliance with Ethical Standards
Conflict of Interest
Adrian Z. Kurz, Eugenie LeRoux, Michael Riediger, Ryan Coughlin, Nicole Simunovic, and Andrew Duong each declare no potential conflicts of interest.
Jovan R. Laskovski reports personal fees from Smith and Nephew and Conmed Linvatec.
Olufemi R. Ayeni is on the speakers’ bureaus for Conmed and Smith and Nephew. Dr. Ayeni is a section editor for Current Reviews in Musculoskeletal Medicine.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Outcomes Research in Orthopedics
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Beckmann JT, Wylie JD, Potter MQ, Maak TG, Greene TH, Aoki SK. Effect of naproxen prophylaxis on heterotopic ossification following hip arthroscopy: a double-blind randomized placebo-controlled trial. J Bone Joint Surg Am. 2015;97(24):2032–2037. doi: 10.2106/JBJS.N.01156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ong C, Hall M, Youm T. Surgical technique: arthroscopic treatment of heterotopic ossification of the hip after prior hip arthroscopy. Clin Orthop. 2013;471(4):1277–1282. doi: 10.1007/s11999-012-2627-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Clohisy JC, Zebala LP, Nepple JJ, Pashos G. Combined hip arthroscopy and limited open osteochondroplasty for anterior femoroacetabular impingement. J Bone Joint Surg Am. 2010;92(8):1697–1706. doi: 10.2106/JBJS.I.00326. [DOI] [PubMed] [Google Scholar]
- 4.Larson CM, Giveans MR. Arthroscopic management of femoroacetabular impingement: early outcomes measures. Arthroscopy. 2008;24(5):540–546. doi: 10.1016/j.arthro.2007.11.007. [DOI] [PubMed] [Google Scholar]
- 5.Bedi A, Zbeda RM, Bueno VF, Downie B, Dolan M, Kelly BT. The incidence of heterotopic ossification after hip arthroscopy. Am J Sports Med. 2012;40(4):854–863. doi: 10.1177/0363546511434285. [DOI] [PubMed] [Google Scholar]
- 6.Randelli F, Pierannunzii L, Banci L, Ragone V, Aliprandi A, Buly R. Heterotopic ossifications after arthroscopic management of femoroacetabular impingement: the role of NSAID prophylaxis. J Orthop Traumatol. 2010;11(4):245–250. doi: 10.1007/s10195-010-0121-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Beckmann JT, Wylie JD, Kapron AL, Hanson JA, Maak TG, Aoki SK. The Effect of NSAID Prophylaxis and Operative Variables on Heterotopic Ossification After Hip Arthroscopy. Am J Sports Med. 2014;42(6):1359–1364. doi: 10.1177/0363546514526361. [DOI] [PubMed] [Google Scholar]
- 8.Uquillas CA, Youm T. Ultrasound-guided pulse lavage for heterotopic ossification after prior hip arthroscopy: a case report. JBJS Case Connect. 2014;4(3):e74–e76. doi: 10.2106/JBJS.CC.M.00192. [DOI] [PubMed] [Google Scholar]
- 9.Amar E, Warschawski Y, Sampson TG, Atoun E, Steinberg EL, Rath E. Capsular closure does not affect development of heterotopic ossification after hip arthroscopy. Arthroscopy. 2015;31(2):225–230. doi: 10.1016/j.arthro.2014.08.026. [DOI] [PubMed] [Google Scholar]
- 10.Amar E, Sharfman ZT, Rath E. Heterotopic ossification after hip arthroscopy. J Hip Preserv Surg. 2015;2(4):355–363. doi: 10.1093/jhps/hnv052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hip LS. Arthroscopy and heterotopic ossification: is NSAID prophylaxis justified? Commentary on an article by James T. Beckmann, MD, MS, et al.: “Effect of naproxen prophylaxis on heterotopic ossification following hip arthroscopy: a double-blind randomized placebo-controlled trial”. J Bone Joint Surg Am. 2015;97(24):e80. doi: 10.2106/JBJS.O.00922. [DOI] [PubMed] [Google Scholar]
- 12.Rath E, Warschawski Y, Maman E, Dolkart O, Sharfman ZT, Salai M, et al. Selective COX-2 inhibitors significantly reduce the occurrence of heterotopic ossification after hip arthroscopic surgery. Am J Sports Med. 2016;44(3):677–681. doi: 10.1177/0363546515618623. [DOI] [PubMed] [Google Scholar]
- 13.Yeung M, Jamshidi S, Horner N, Simunovic N, Karlsson J, Ayeni OR. Efficacy of nonsteroidal anti-inflammatory drug prophylaxis for heterotrophic ossification in hip arthroscopy: a systematic review. Arthroscopy. 2016;32(3):519–525. doi: 10.1016/j.arthro.2015.08.007. [DOI] [PubMed] [Google Scholar]
- 14.Miller GK. Editorial Commentary: The efficacy of nonsteroidal anti-inflammatory drugs for prophylaxis of heterotopic ossification in hip arthroscopy--do we treat patients or X-rays? Arthroscopy. 2016;32(3):526–527. doi: 10.1016/j.arthro.2015.12.035. [DOI] [PubMed] [Google Scholar]
- 15.Redmond JM, Keegan MA, Gupta A, Worsham JR, Hammarstedt JE, Domb BG. Outcomes of heterotopic ossification excision following revision hip arthroscopy. J Hip Preserv Surg. 2017;4(2):164–169. doi: 10.1093/jhps/hnx010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Warschawski Y, Sharfman ZT, Amar E, Rath E. Anti-inflammatory prophylaxis prevents heterotopic ossification in contralateral side hip arthroscopy: a case report. J Orthop Case Rep. 2017;7(1):20–23. doi: 10.13107/jocr.2250-0685.670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Barth M, Willett GM, Oliphant K. Heterotopic ossification following hip arthroscopy. J Orthop Sports Phys Ther. 2018;48(4):344. doi: 10.2519/jospt.2018.7420. [DOI] [PubMed] [Google Scholar]
- 18.Kaplan FS, Glaser DL, Hebela N, Shore EM. Heterotopic ossification. J Am Acad Orthop Surg. 2004;12(2):116–125. doi: 10.5435/00124635-200403000-00007. [DOI] [PubMed] [Google Scholar]
- 19.Rath E, Sherman H, Sampson TG, Ben Tov T, Maman E, Amar E. The incidence of heterotopic ossification in hip arthroscopy. Arthroscopy. 2013;29(3):427–433. doi: 10.1016/j.arthro.2012.10.015. [DOI] [PubMed] [Google Scholar]
- 20.Brooker AF, Bowerman JW, Robinson RA, Riley LH. Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg Am. 1973;55(8):1629–1632. doi: 10.2106/00004623-197355080-00006. [DOI] [PubMed] [Google Scholar]
- 21.Ritter MA, Vaughan RB. Ectopic ossification after total hip arthroplasty. Predisposing factors, frequency, and effect on results. J Bone Joint Surg Am. 1977;59(3):345–351. doi: 10.2106/00004623-197759030-00009. [DOI] [PubMed] [Google Scholar]
- 22.Chan CC, Reid CM, Aw T-J, Liew D, Haas SJ, Krum H. Do COX-2 inhibitors raise blood pressure more than nonselective NSAIDs and placebo? An updated meta-analysis. J Hypertens. 2009;27(12):2332–2341. doi: 10.1097/HJH.0b013e3283310dc9. [DOI] [PubMed] [Google Scholar]
- 23.Zhu X-T, Chen L, Lin J-H. Selective COX-2 inhibitor versus non-selective COX-2 inhibitor for the prevention of heterotopic ossification after total hip arthroplasty. Medicine (Baltimore) 2018;97(31):e11649. doi: 10.1097/MD.0000000000011649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cai L, Wang Z, Luo X, She W, Zhang H. Optimal strategies for the prevention of heterotopic ossification after total hip arthroplasty: a network meta-analysis. Int J Surg. 2019;62:74–85. doi: 10.1016/j.ijsu.2018.12.011. [DOI] [PubMed] [Google Scholar]
- 25.Baird EO, Kang QK. Prophylaxis of heterotopic ossification – an updated review. J Orthop Surg. 2009;4:12. doi: 10.1186/1749-799X-4-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Juarez JK, Wenke JC, Rivera JC. Treatments and preventative measures for trauma-induced heterotopic ossification: a review. Clin Transl Sci. 2018;11(4):365–370. doi: 10.1111/cts.12552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Battaglia M, Guaraldi F, Gori D, Castiello E, Arvat E, Sudanese A. Efficacy of triamcinolone acetate and methylprednisolone acetonide for intrabursal injection after ultrasound-guided percutaneous treatment in painful shoulder calcific tendonitis: a randomized controlled trial. Acta Radiol. 2017;58(8):964–970. doi: 10.1177/0284185116678275. [DOI] [PubMed] [Google Scholar]
- 28.de Witte PB, Kolk A, Overes F, Nelissen RGHH, Reijnierse M. Rotator cuff calcific tendinitis: ultrasound-guided needling and lavage versus subacromial corticosteroids: five-year outcomes of a randomized controlled trial. Am J Sports Med. 2017;45(14):3305–14. doi: 10.1177/0363546517721686. [DOI] [PubMed] [Google Scholar]