Abstract
Purpose of Review
The purpose of this paper was to review the current psychometric properties of patient-reported outcome measures that are commonly used for patients with patellofemoral instability. This review provides evidence to guide the selection of subjective outcome measures for assessing outcomes in clinical care and research studies.
Recent Findings
At the present time, there are two patient-reported outcome measures that have been designed for, and tested on, large cohorts of patellofemoral instability patients, the Banff Patella Instability Instrument (BPII) and the Norwich Patellar Instability Score (NPI). The BPII is a wholistic quality of life outcome measure and the NPI is a symptom score.
Summary
The use of disease-specific outcome measures such as the BPII and NPI, in combination with generic knee, functional activity, and/or psychological outcome measures that have been proven to be valid and reliable for the patellofemoral instability population, is most likely to provide a well-rounded evaluation of treatment outcomes.
Electronic supplementary material
The online version of this article (10.1007/s12178-019-09537-7) contains supplementary material, which is available to authorized users.
Keywords: Patellofemoral instability, Patellar dislocation, Patient-reported outcome measure, Banff Patella Instability Instrument, Norwich Patellar Instability Score, Kujala score
Introduction
Patellofemoral instability is a potentially debilitating condition, with an incidence of up to 77/100,000 person/years in a high-risk population [1–5]. The peak incidence of first-time patellar dislocation occurs between the ages of 15–19, with an estimated recurrence rate ranging between 17 and 70% depending on risk factors [1, 6, 7]. Over half of patellar dislocations occur during athletic activity, and as youth participation in formal sporting endeavors increases the incidence of patellofemoral instability can be expected to rise [1, 6, 8]. Patients with patellar dislocation or subluxation experience disabling symptoms with activity which frequently limit their recreational activities and quality of life (QOL) [9, 10, 11••].
In addition to the symptoms of instability, anterior knee pain is commonly overlaid in this population [12]. Historically, patellofemoral instability patients were consolidated with typical anterior knee pain patients under the umbrella term of “patellofemoral pain syndrome.” Measurement of treatment outcomes in this broad patient population was frequently completed using generic knee pain outcome tools. However, anterior knee pain can be caused by a variety of etiologies, the majority of which are unrelated to patellofemoral instability. This homogenization of heterogenous patient populations has resulted in confusion in the literature when assessing treatments and outcomes for patellofemoral instability.
Accurate comparison of treatment strategies is not possible without appropriate outcome tools, ideally validated for use specifically in patients with patellofemoral instability [13]. The importance of patient-reported satisfaction, as well as improvement in symptomatology, is becoming increasingly recognized in the orthopedic literature, and a significant increase in available patient-reported outcome measures (PROMs) has occurred [13]. Fortunately, this growth has included PROMs specific to patellofemoral instability, and the work to improve the validity and responsiveness of these outcome measures is ongoing. A number of studies have assessed the psychometric properties of the subjective outcome measures commonly used in patients with patellofemoral instability, reporting on the validity, reliability, responsiveness, and cross-cultural adaptation the outcome measures used for the assessment of this patient population [14, 15•, 16•, 17, 18••, 19, 20•].
Despite the high number of pediatric patients that present with patellofemoral instability, there has been minimal work undertaken to validate disease-specific PROMs in younger patients. Outcome tools designed for and tested on adults may not measure parameters important to, or appropriate for, the younger patient. In addition, advanced language used in these outcome measures may make items difficult to understand which could result in unanswered or misinterpreted questions. Therefore, outcome instruments specifically validated for both the age group and pathology of interest are essential.
There are a variety of patient-reported outcome measures used in the literature for the assessment of patients with patellofemoral instability. Despite widespread use, few have been specifically validated in a patellofemoral instability population (Table 1). The purpose of this review is to critically assess the commonly used outcome tools for patellofemoral instability, with an emphasis on the evidence for validity, reliability, and responsiveness in this patient population. Additional discussion of tools validated for use in pediatric patients is included.
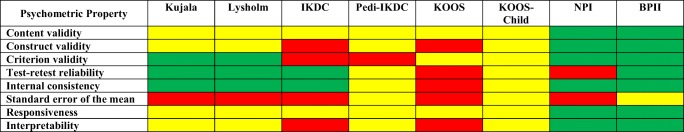
Table 1.
Assessment of measurement properties of the PROMs in patients with patellofemoral instability
A benchmark minimum of 30 patellofemoral instability patients with separate psychometric evaluation of the disease-specific patient group was required to meet the standard for the measurement properties displayed in this table
Red, no published evidence, or does not meet the minimum standard of psychometric evaluation; yellow, insufficient evidence to meet standard of psychometric evaluation; green, good level of evidence from psychometric evaluation
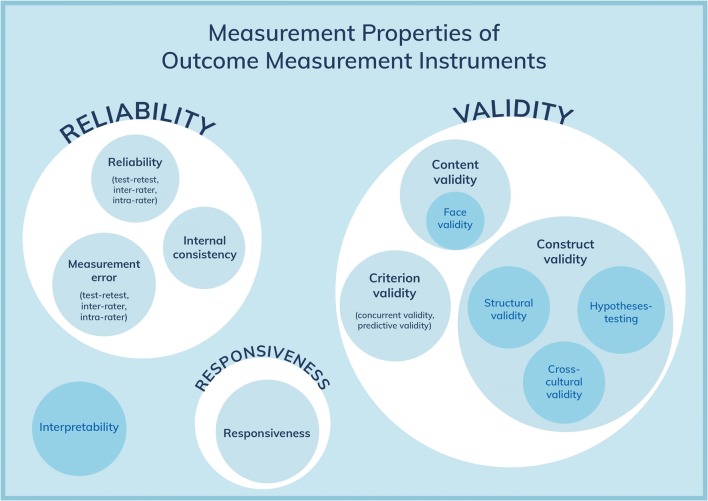
The COSMIN Framework
The COnsensus-based Standards for the Selection of health Measurement INstruments (COSMIN) initiative aims to improve the quality of, and aid in the appropriate selection of, measurement tools in the medical field [13, 21]. An international panel developed a checklist-based approach to formally and systematically assess the quality of outcome tools. A complete COSMIN validation requires a systematic literature review followed by a detailed analysis of all available data for a tool. Overall, the COSMIN panel recommends the assessment of three main taxonomic areas of an outcome measure: reliability (including internal consistency, reliability, and measurement error), validity (including content validity, construct validity, and criterion validity), and responsiveness (Fig. 1). In addition, the panel recommends the evaluation of interpretability, which relates to the ease of use for the clinician or researcher. The COSMIN checklist provides a helpful framework for the review of medical outcome tools, including PROMs for patellofemoral instability.
Fig. 1.
The COSMIN Taxonomy of Measurement Properties relevant for evaluating PROMs [22]
Patient-Reported Outcome Scores in Use for Patellofemoral Instability
Kujala Anterior Knee Pain Scale
The Kujala Anterior Knee Pain Scale was originally published in 1993 by Kujala in Helsinki, Finland [23]. Created to assess anterior knee pain, the Kujala scale consists of 13 questions covering a range of physical symptoms and limitations that are presented in a multiple choice answer format, with a different point value assigned to each answer. No clear rationale was presented for the weighting of the answers, and the authors acknowledge that the questions were created based on expert opinion [23]. The maximum score is 100, with higher scores indicating better function. Despite the Kujala scale being utilized widely in the patellofemoral instability literature, only one question directly assesses instability symptoms [20•, 24–26].
Validity
Face validity of the Kujala scale was initiated through non-systematic item generation by clinical experts in patellofemoral pain [23]. In the original manuscript, the authors reported on 68 patients consisting of four groups: control, anterior knee pain, patellar subluxation, and patellar dislocation. This publication included data validating the scores against objective MRI measurements. The Kujala scale has subsequently been validated for anterior knee pain in multiple studies [27–29].
Studies of the Kujala scale assessing patients with patellofemoral instability have reported no floor effects but ceiling effects of up to 19% [14, 15•, 16•]. In cross-cultural adaptations, there was a very strong correlation to the Oxford knee score (r = 0.96), and moderate to high correlations to the KOOS subscales (r = 0.65–0.84), and the Lysholm scale (r = 0.88) [15•, 16•]. The Kujala scale has also demonstrated moderate convergent validity with the more recently published disease-specific PROMs for patellofemoral instability: the Banff Patella Instability Instrument (r = 0.5, p < 0.001) and the Norwich Patellar Instability Score (r = 0.5, p < 0.001) [18••, 30, 31••, 32••].
Reliability
The Kujala scale has demonstrated high internal consistency (Cronbach’s alpha coefficient = 0.82–0.93), and high test-retest reliability (intraclass correlation coefficient (ICC) = 0.86–0.96) for patients with patellofemoral instability [14, 15•, 16•]. The standard error of measurement (SEM) for patellofemoral instability patients does not appear to have been reported for the Kujala scale.
Responsiveness
Responsiveness, measured using the standardized response mean (SRM) and Cohen’s d to assess change over time in patients with patellofemoral instability from pre- to 12-month post-operative, demonstrated that the Kujala scale had excellent responsiveness in this short-term time frame (d = 0.96; SRM = 1.3) [14, 15•, 16•].
Additional Information
Although the Kujala Anterior Knee Pain Scale is the most commonly used PROM in the pediatric patellofemoral instability literature, it has not been validated for use in a pediatric population [33]. Normative data is available from the original control group of 17 healthy adult patients, who scored an average of 99.9, compared with 82.8 for patients with anterior knee pain, and 62.2 for patients with patellofemoral instability [23]. There does not appear to be a published MCID for patellofemoral instability patients.
The Kujala scale did not distinguish patients with single patellar dislocation from those suffering recurrent symptoms [14]. However, the scale did demonstrate a moderate correlation (r = 0.71) with the visual analogue pain scale in a cross-cultural adaptation [16•]. Some researchers have recommended using additional or alternative outcome measures for the assessment of patellofemoral instability treatment outcomes due to increased ceiling effects in longer-term follow-up, as well as suggesting that the strength of study results are limited by the pain rather than instability focus of the Kujala scale [34, 35].
Translations of the Kujala scale are available in Italian, French, German, Greek, Thai, Spanish, Dutch, Persian, Brazilian Portuguese, Turkish, Chinese, and Arabic [15•, 16•, 36–45]. Readability of the English version is rated at a grade-reading level of 5.0 (Table 2); however, it should be noted that some of the wording may be difficult for patients to interpret and may result in questions going unanswered [27]. For example, the use of “atrophy” in item 12 is more a medical rather than a lay term.
Table 2.
Comparison of PROMs used in patellofemoral instability literature
| Kujala | Lysholm | IKDC | Pedi-IKDC | KOOS | KOOS-Child | NPI | BPII 2.0 | |
|---|---|---|---|---|---|---|---|---|
| Year initially published | 1993 | 1982 | 2001 | 2011 | 1998 | 2012 | 2012 | 2013 |
| Original construct | Anterior knee pain | Ligament instability | Knee pathology | Knee pathology | Knee pathology including OA | Knee pathology | Patellofemoral instability | Patellofemoral instability |
| Target population | Adults | 12 years to adult | Adults | 10–18 years | 16 years to elderly | 7–18 years | Adults | 10 years to adult |
| Number of items | 13 | 8 | 18 | 13 | 42 | 39 | 19 | 23 |
| Response options | Multiple choice | Multiple choice | Likert scale | Likert scale | Likert scale | Likert scale | Likert scale | VAS |
| Scoring | Variable point values for each selection | Variable point values for each selection | Weighted responses | Weighted responses | Normalized, domains reported separately | Weighted and normalized, domains reported separately | Weighted responses | Measured distance on VAS |
| Range of scores (worst to best) | 0–100 | 0–100 | 0–100 | 0–100 | 0–100 for each domain | 0–100 | 100–0 | 0–100 |
| Completion time for patient | 4 min | 3 min | 10 min | 10 min | 10 min | 10–20 min | 4 min | 5 min |
| Normative data available |
Yes^ [23] 100/100 |
Yes [46] 94/100 |
Yes [47] 86–89/100 |
Yes [48] 87.4/100 |
Yes [49] Variable |
Yes [49] Variable |
No | No |
| Original language | Finnish, published in English | Swedish, published in English | English | English | English and Swedish | Swedish and English | English | English |
| Available translations | > 10 | > 5 | > 10 | Danish | > 50 | > 5 | German | German, French |
| Reading grade level* | 5.0 | 5.7 | 8.7 | 5.6 | 4.8 | 4.7 | 5.9 | 7.1 |
*Reading level was calculated by using the composite grade level algorithm available at www.readability.io
^n = 17 from original control group
Lysholm Knee Scoring Scale and Fulkerson Scale
The Lysholm Knee Scoring Scale was developed by Lysholm and Gillquist in Linkoping, Sweden, in 1982 [50]. The scale was developed as a modification of the Larsen scale, designed to measure outcomes following knee ligament surgery, in particular anterior cruciate ligament reconstruction. Although not designed for use in patellofemoral instability, it gained a foothold in the literature because for many years it was one of the few standardized PROMs available for knee instability pathology. Specific to patellofemoral instability, Fulkerson et al. modified the scale in 1990 by altering the instability and pain item weighting in an effort to make the questionnaire more specific to patellofemoral disorders [51].
The Lysholm Knee Scoring Scale contains eight questions with multiple choice answers assessing functional limitations as well as symptoms such as pain and swelling [50]. A different point value is awarded for each answer, for a total score out of 100. A higher score indicates better function. The Fulkerson scale consists of seven questions and has similar multiple choice scoring as the Lysholm scale, with significant weighting for pain which can score up to 45 points out of the overall total score of 100.
Validity
Face validity of the Lysholm scale was obtained through non-systematic item generation by clinical experts in knee ligament instability [50]. The Lysholm Knee Scoring scale was first validated in patients with patellofemoral instability by Paxton et al. and subsequently further validated in cross-cultural adaptations [14, 15•, 16•]. No floor effects have been reported but ceiling effects of up to 21% were identified for both the Lysholm and Fulkerson scales [14]. The Lysholm scale has demonstrated convergent validity with very strong correlation to the Fulkerson scale (r = 0.93) and the Kujala scale (r = 0.86), and divergent validity with the IKDC (r = − 0.51) [14]. In cross-cultural adaptations, there was a very strong correlation with the Oxford Knee Score for the Lysholm and Fulkerson scales, respectively (r = 0.94 and r = 0.93) [15•].
Reliability
The Lysholm and Fulkerson scales have demonstrated moderate to high internal consistency (Cronbach’s alpha coefficient = 0.70–0.91), and high test-retest reliability (ICC = 0.88) for patellofemoral instability [14, 15•]. The SEM for patients with patellofemoral instability does not appear to have been reported.
Responsiveness
Responsiveness, measured using SRM and Cohen’s d to assess change over time in patients with patellofemoral instability from pre- to 12-month post-operative, demonstrated that the Lysholm and Fulkerson scales had excellent responsiveness in short-term follow-up [15•, 16•].
Additional Information
Although the Lysholm scale has been validated for use in patients as young as 12 years as a knee-specific outcome score, it has not been specifically validated in a pediatric population [33]. Normative data has been published in which the average score was found to be 94 in healthy knees, and this did not vary with age [46, 52]. No MCID has been reported for patients with patellofemoral instability.
In assessment of patients with one-time compared with recurrent patellofemoral instability, the Fulkerson and Lysholm scales were able to differentiate between these patient groups. The recurrent instability group demonstrated lower scores on the Fulkerson (p < 0.01) and Lysholm scales (p < 0.05) at 2-year follow-up [14]. The Lysholm has been translated and published in Dutch, Chinese, Turkish, Italian, German, and Polish [15•, 16•, 53–56].
International Knee Documentation Committee Subjective Knee Evaluation Form
The International Knee Documentation Committee (IKDC) Subjective Evaluation Form was first developed by an international committee of experts in 1993 using a formalized testing process with the goal of creating a standardized, patient-assessed, knee-specific outcome form [57]. Following multiple refinements based on analysis of patients’ responses to the outcome measure, the presently accepted IKDC Subjective Knee Evaluation Form was published in 2001 [57].
The IKDC includes 18 questions covering three domains: symptoms, physical activity, and function. The items are answered on Likert scales of varying values. IKDC scores are calculated by dividing the total score by the highest possible score for the items answered, and multiplying by 100, with higher scores indicating better function. A patient must answer at least 90% (16/18 items) for the score to be considered valid [57].
Validity
The IKDC has been validated in patients with patellofemoral instability [14]. The IKDC has demonstrated significant ceiling effects (47%) indicating poor content validity for the patellofemoral instability population [14]. The IKDC did not correlate well to the Lysholm, Kujala, or Fulkerson scales indicating that it may not be measuring the same construct, namely patellofemoral instability [14].
Reliability
The IKDC has demonstrated good psychometric properties for general knee injuries but the data for patellofemoral instability is less clear [47, 58]. The IKDC has demonstrated moderate to high internal consistency (Cronbach’s alpha coefficient = 0.84) and a test-retest reliability of 0.82 in patients with patellofemoral instability [14]. The SEM for patellofemoral instability patients does not appear to have been reported.
Responsiveness
The responsiveness of the IKDC for patellofemoral instability patients does not appear to have been reported. Recent studies on the outcomes of patients after various patellofemoral stabilization procedures have utilized the IKDC as the PROM. These studies demonstrated that there was statistically significant improvement in IKDC score, pre- to post-operatively similar to the Kujala, but the psychometric properties of the instrument were not specifically reported [59–61].
Additional Information
Normative data is available for the IKDC for ages 18–89 and average scores have been found to vary with age and gender [47]. MCID has not been determined for the patellofemoral instability population. Published translations for the IKDC are available in Chinese, Swedish, Greek, Turkish, German, Thai, Korean, Brazilian Portuguese, Dutch, Italian, and French [62–72].
Pediatric IKDC Subjective Knee Evaluation Form
The Pediatric IKDC Subjective Knee Evaluation Form (Pedi-IKDC) was developed in 2011 by Kocher et al. in Boston, USA. It was designed for youth aged 10–18 years to specifically assess symptoms, function, and sports activity in patients with various knee pathologies. The Pedi-IKDC was the first knee-specific PROM score to be rigorously validated in a pediatric population. It has not been modified since its initial publication.
The Pedi-IKDC was developed after qualitative interviews were performed with children to critically evaluate the comprehension and relevance of the IKDC, and modifications were made accordingly to create a 13-item tool. The Pedi-IKDC assesses function, participation in sports/recreation, and activities of daily living. A final score is calculated out of 100, with higher scores indicating better function and fewer symptoms [73].
The original publication of the Pedi-IKDC included rigorous psychometric evaluation of a sample of 589 American participants, aged between 10 and 18 years, of which 17% had a diagnosis of patella subluxation or dislocation [73]. A sub-analysis specifically for patellofemoral instability was not performed, nor was it performed in the subsequent Danish translation validation. Psychometric testing of the Pedi-IKDC reported below is taken from large groups of pediatric patients with a variety of knee conditions that included 17–27% patellofemoral instability [73, 74].
Validity
Content and construct validity were confirmed in the original publication [73]. For the Pedi-IKDC total score, the floor effect was 0% and the ceiling effect was 1% [73]. There were five individual items that demonstrated a ceiling effect greater than 30% and 16 items that were over 15%. None of the 18 items demonstrated an unacceptable floor effect of > 30%; however, six had a floor effect greater than 15% [73]. Of note, when used in a “healthy” population, a high ceiling effect was observed [48].
Reliability
The Pedi-IKDC has demonstrated high internal consistency (Cronbach’s alpha coefficient = 0.9–0.91) [73, 74]. The test-retest reliability was excellent (ICC = 0.9) and the SEM has been reported at 4.1 [74].
Responsiveness
A large effect size (1.36) was shown for patients undergoing surgical treatment for their knee condition with a SRM of 0.9–1.35 [73, 74]. The minimal clinically important change was 12.0 [74].
Additional Information
Normative data for the Pedi-IKDC has been published in 2000 American youths between 10 and 18 years old [48]. The MCID is reported as 12.0 (SD 13.5) [74]. Recent studies on the outcomes of patients after patellofemoral stabilization have utilized the Pedi-IKDC as their PROM [75]. The Pedi-IKDC has been published and formally validated in Danish [74].
Knee Injury and Osteoarthritis Outcome Score
The Knee Injury and Osteoarthritis Outcome Score (KOOS) was developed in Lund, Sweden, in 1998 by Roos et al. [76]. The goal was to develop a PROM that included relevant questions for both an acute knee injury as well as osteoarthritis, to enable long-term use to follow the progression from injury to arthritis. Modifications since publishing include the addition of an optional patellofemoral subscale (KOOS-PF) that can be added to the full KOOS or used independently [77]. The KOOS-PF is designed for a patellofemoral pain and osteoarthritis population and has not been validated in instability patients [77].
The original KOOS consists of five different domains, each of which is scored on a five-point Likert scale and reported separately: pain (nine items), symptoms (seven items), activities of daily living (17 items), sport and recreation function (five items), and knee-related QOL (four items). An average of responses for each subdomain is obtained and then normalized to a score out of 100 with higher scores indicating better function.
Validity
The KOOS has demonstrated psychometric properties for a variety of knee conditions, but has not been separately evaluated in a patellofemoral instability population [76, 78]. The five KOOS subscales have demonstrated convergent validity with the Kujala score (r = 0.65–0.84; p < 0.001) [16•]. The KOOS was found to have divergent correlation to the Norwich Patellar Instability Instrument in patients with patellofemoral instability, suggesting that the KOOS may not be a first-line choice for studying patellofemoral instability [32••].
Reliability
Reliability of the KOOS has not been reported for the patellofemoral instability population.
Responsiveness
In patellofemoral instability patients, the KOOS QOL subscale showed responsiveness to change from pre- to 12-month post-operatively with a large Cohen’s d effect size (d = 1.56) [16•]. The other KOOS subscales demonstrated only small to medium effect size for pre- to post-surgical change [16•]. Recent studies on the outcomes of patients after various patellofemoral stabilization procedures have utilized the KOOS as a PROM. These studies demonstrated that there was statistically significant improvement in KOOS scores, pre- to post-operatively, similar to the Kujala, but the psychometric properties of the instrument were not specifically reported [19, 79–81].
Additional Information
The KOOS is recommended for ages 16 to elderly; younger children should use the KOOS-Child tool [49, 82]. Normative data has been established and is available for each subscale [49]. KOOS scores were found to vary according to age and gender. MCID has not been reported for a patellofemoral instability population. Translations are available online in 51 languages [83].
Knee Injury and Osteoarthritis Outcome Score for Children
The Knee Injury and Osteoarthritis Outcome Score for Children (KOOS-Child) was developed by Örtqvist et al. in Stockholm, Sweden, and was published in 2012 [84]. In-depth qualitative interviews with children were used to identify areas of confusion in the KOOS instructions, item wording, and scale-use, and items were modified accordingly. In 2014, an item-reduced version was published which has been used for subsequent validation work [82].
The KOOS-Child score consists of 39 questions that are presented as a five-point Likert scale that is divided into five subscale domains: pain, knee problems (symptoms), difficulty during daily activities, function in sport and play, and knee-related QOL. The KOOS-Child domain scores are designed to be assessed separately, and no composite score is reported. Average scores for each domain are normalized to range from 0 (extreme symptoms) to 100 (no symptoms) [82].
Psychometric testing of the KOOS-Child reported below was performed in a cohort of 115 children ranging in age from 7 to 16, with a variety of knee pathologies, of whom 37% had patellofemoral instability. A sub-analysis specifically for patellofemoral instability was not performed [82].
Validity
Content validity was confirmed through expert opinion and interviews with pediatric patients [84]. Construct validity was confirmed by convergence with similar items from the Child Health Assessment Questionnaire (CHAQ), the EuroQol for youth (EQ-5D-Y), and five purpose-specific visual analogue scale (VAS) items [82]. There were no floor effects and the highest ceiling effect was for the “Activities of Daily Living” subscale with 15% [82].
Reliability
Test-retest reliability is acceptable, with an ICC of 0.78–0.91 depending on the subscale tested [82]. Internal consistency was demonstrated for all subscales (Cronbach’s alpha 0.8–0.9) except for the “symptoms” subscale, which had a Cronbach’s alpha of 0.59 [82]. SEM are reported as 5.28–8.14 depending on the subscale [82].
Responsiveness
Responsiveness was evaluated by correlating changes in the KOOS-Child score and a scale of Global Perceived Effect, after a 3-month time period in which a variety of interventions, including no treatment, were implemented. All KOOS-Child subscales demonstrated responsiveness to change with a moderate effect size (0.42–0.78) in patients who reported an improvement in their symptoms, and a small effect size (0.12–0.21) in patients who reported stable symptoms [82]. One recent study has used the KOOS-Child for pediatric patients undergoing both operative and non-operative management for a first-time patellar dislocation [81].
Additional Information
Normative data has been established for the KOOS-Child and is available for each subscale [49]. The MCID for patients with patellofemoral instability has not been established. KOOS-Child was originally developed and validated in Swedish then was secondarily translated into English for publication. Translations in Danish, Greek, Norwegian, and Persian are available online. Formal validation of the French translation has been published [85].
Norwich Patellar Instability Score (Appendix 1)
The Norwich Patellar Instability (NPI) score was originally published in 2014 by Smith et al. in Norwich, UK [32••]. It was developed at the same time as the Banff Patella Instability Instrument in response to the lack of a disease-specific outcome measure for patellofemoral instability [17]. The NPI is a physical symptoms score, designed to assess patient-perceived patellar instability symptoms. It has not undergone modification since its original published format.
The NPI score is a self-administered 19-item questionnaire that assesses symptoms during activities that may produce patellofemoral instability, using a five-point Likert scale with options from “always” to “never.” The questions assess activities of daily life as well as sporting activities, and are designed to encompass both high and low energy movements as well as both uniplanar and multi-directional movements. The activities were selected after surveying patients with a history of patella dislocation and were refined through a literature search [86]. The NPI has a complex weighting algorithm where items that would be expected to elicit symptoms in most instability patients, such as twisting during sports, have a low maximum score assigned and activities that would only be symptomatic for patients with highly unstable patellae, such as turning to look over the shoulder, have more potential points assigned. The total score is then divided by the maximum number of points available for items completed (maximum 250 points if all 19 items are answered) to obtain a percentage. A higher percentage score indicates higher instability, and therefore, worse function [32••].
Validity
Face validity for the NPI score was formally established with the use of literature search methods and formal patient surveys. The NPI has demonstrated construct validity with other PROMs used for patellofemoral instability, including convergent validity to the Kujala scale (rs = − 0.66), Lysholm scale (rs = − 0.54), and BPII 2.0 (rs = − 0.53) [18••, 31••, 32••]. The NPI score is the only disease-specific tool that has been validated specifically in a first-time dislocation population [31••]. An identified shortcoming of the NPI score is its potential floor effect across all 19 items, especially in the conservatively managed population, which may limit its ability to demonstrate improvement in these patients over time [31••]. Additionally, over 80% of respondents after an initial dislocation selected “do not do” as a response for at least one question, suggesting that content validity could be improved to better reflect the activities performed in this population [31••].
Reliability
Internal consistency has been reported as high, with a Cronbach alpha coefficient of 0.93 [31••, 32••]. Test-retest reliability has not been published.
Responsiveness
The NPI demonstrated parallel responsiveness in first-time dislocators to improvements in the Lysholm scale, the Tegner Activity Score, and isometric knee extension strength [31••].
Additional Information
The NPI has not been validated for a pediatric population. At this time, no normative data for the NPI score has been published. There is also no reported MCID for the NPI. The NPI has been translated into German for research purposes, but a formally validated translation has not been published [87•].
Banff Patella Instability Instrument (Appendix 2)
The Banff Patella Instability Instrument (BPII) was initially published in 2013 by Hiemstra et al. in Banff, Canada [30]. It was created to fill the void in the literature at the time for PROMs specifically created for patellofemoral instability patients. It was originally modified from the previously validated ACL-QOL instrument [30]. In 2016, the BPII underwent a factor analysis and item reduction, and the BPII 2.0 was introduced as the updated format [11••, 18••]. The ICCs between BPII and BPII 2.0 were high at all time points pre-operatively (0.82) to 24 months post-operative (0.94). It is a patient-reported, disease-specific QOL score that consists of 23 questions across five domains covering symptoms/physical complains, work-related concerns, recreational activity and sport participation/competition, lifestyle, and social/emotional. Patients mark their answers on a visual analogue scale measuring 100 mm in length. Each item is equally weighted with the final score calculated as an average of the scores from all answered items. A higher score reflects a higher QOL.
Validity
Validity has been formally established in patient populations with patellofemoral instability, both pre- and post-stabilization procedures. Face and content validity were established through a modified Ebel procedure [30]. Construct validity has been established by correlating the BPII to the Kujala scale and the Norwich Patella Instability Score to demonstrate convergence (p < 0.001) [18••]. The BPII indicated a degree of predictive validity in an assessment of surgical failures, whereby post-operative BPII scores were statistically significantly lower in patients who subsequently suffered a surgical failure compared with intact surgery for both MPFL reconstructions (p = 0.048) and MPFL imbrications (p = 0.003) (In press). The BPII 2.0 has been further validated with the successful cross-cultural adaptation in to German [87•].
Reliability
Reliability for the BPII is high. Internal consistency was calculated using the Cronbach alpha reliability coefficient for BPII and was found to be > 0.95, indicating very high internal consistency [30]. Subsequently, the BPII 2.0 has demonstrated a Cronbach’s alpha coefficient > 0.90 from pre- to 12 months post-operatively [11••]. Test-retest was established for the BPII 2.0 (ICC 0.97) [11••, 30].
Responsiveness
Responsiveness to change of both BPII and BPII 2.0 has been shown for pre- and post-surgical patients. BPII 2.0 scores were statistically different at four time points between initial consultation and 24 months post-operative, as demonstrated with an analysis of variance (F3,267 = 58.46, p < 0.01) [11••]. Additionally, correlation with responsiveness was demonstrated for BPII 2.0 by anchoring with a seven-point Likert scale where patients rated their improvement post-operatively from “significantly worse” to “significantly better” (r = 0.56 and r = 0.54) [11••]. No floor or ceiling effect has been observed for the BPII [11••, 30].
Additional Information
The initial validity and reliability assessments of the BPII included both adult and pediatric patients [30]. In addition, the BPII has been validated specifically in adolescents (n = 45, mean age 16.2, range 10.3–17.9), making it the only disease-specific PROM validated for use in the pediatric population [88••]. Development of the BPII 2.0 through the factor analysis and item reduction process included specific changes to make the outcome measure even more useable for a pediatric audience. Importantly, questions referring to “work” were modified to include “school concerns” [11••]. The BPII 2.0 has recently been assessed in a multi-center concurrent validation to the Pedi-IKDC, demonstrating a moderate correlation (r = 0.65) between the outcome measures, as well high test-retest reliability (ICC = 0.94), and no floor or ceiling effects (In Press). The SEM was calculated as 2.13.
Normative data is not available for the BPII. The MCID has not been assessed with a receiver operating characteristic (ROC) curve; however, using one half the standard deviation of the mean pre-operative score provides an estimated MCID of 6.2 [11••].
The BPII 2.0 has been formally translated and validated for German speakers, including populations from Germany, Austria, and Switzerland [87•] and is currently undergoing validation in Dutch, Spanish, Portuguese, Finnish, and French.
Discussion
Standardized patient-reported outcome measures are essential for assessing effectiveness of treatment and clinical response. PROMs should be critically appraised for validity, reliability, responsiveness, and interpretability. The COSMIN checklist provides a helpful framework for this assessment. Patient-reported tools reduce bias in the reporting of treatment outcomes however no single questionnaire is likely to be suitable for assessing all patients presenting with patellofemoral instability. Outcome measures can assess different aspects of the patient experience, with commonly evaluated areas including QOL, disability, functional limitation or status, range and burden of symptoms, and patient satisfaction [89]. PROM tools may include multiple categories or may focus on a single domain. It can be advantageous to include multiple tools when assessing a patient outcome so that a broader perspective of the patient experience is evaluated.
While numerous outcome measures have been adopted for use in the patellofemoral instability population, very few have undergone rigorous psychometric testing. In many cases, generic outcome measures were selected due to the lack of disease-specific measures. Ideally, PROM scores should be validated for the specific patient condition and population of interest. The Banff Patella Instability Instrument (BPII and BPII 2.0) and the Norwich Patella Instability score (NPI) have been specifically developed and subsequently validated for use in patellofemoral instability patients. Ongoing evaluation of these outcome measures is required to meet criteria in all nine areas of the COSMIN taxonomy. At the present time, research has been undertaken for the NPI in 6/9 areas in the COSMIN checklist, while the BPII has undertaken work in 8/9 areas.
Pediatric patients have unique functional considerations as well as abilities to understand outcome tool questions. Therefore, adult PROMs may not be appropriate for use with younger patients and tools validated for use in pediatric patients should be selected whenever possible. The BPII and BPII 2.0 have been validated for use in an adolescent population and currently this is the only disease-specific PROM validated for pediatric patients.
None of the outcome scores reported on in this paper have a specific psychological focus which is known to exert a substantial influence on patient outcomes [90]. Although QOL scores do assess a component of these factors, efforts should be made to assess the validity, reliability, and responsiveness of psychological outcome measures for patients with patellofemoral instability. Overall, the use of appropriate, critically validated, patient-reported outcome measures will contribute to stronger evaluation of treatments for the challenging clinical entity of patellofemoral instability.
Conclusion
At the present time, there are only two patient-reported outcome measures that have been designed and tested on large patient cohorts in the patellofemoral instability population, the BPII and NPI. The BPII is a wholistic QOL outcome measure and the NPI is a symptom score. Use of these tools in combination with generic knee outcome measures, activity assessment measures, and/or psychological outcome measures that have been proven to be valid and reliable across the spectrum of the patellofemoral instability patient population is most likely to provide a well-rounded evaluation of treatment outcomes.
Electronic Supplementary Material
(PDF 303 kb)
(PDF 90.7 kb)
Compliance with Ethical Standards
Conflict of Interest
Laurie A. Hiemstra and Sarah Kerslake report that the Banff Patellofemoral Instability Instrument (BPII & BPII 2.0) patient-reported outcome measure assessed in the manuscript was developed and researched by them both. Every effort has been undertaken to assess each outcome measure using the same criteria to avoid bias of interpretation and presentation of the critical review. Jessica L. Page declares no potential conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Outcomes Research in Orthopedics
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Waterman BR, Belmont PJ, Owens BD. Patellar dislocation in the United States: role of sex, age, race, and athletic participation. J Knee Surg. 2012;25:51–57. doi: 10.1055/s-0031-1286199. [DOI] [PubMed] [Google Scholar]
- 2.Sillanpää P, Mattila VM, Iivonen T, Visuri T, Pihlajamäki H. Incidence and risk factors of acute traumatic primary patellar dislocation. Med Sci Sports Exerc. 2008;40:606–611. doi: 10.1249/MSS.0b013e318160740f. [DOI] [PubMed] [Google Scholar]
- 3.Nietosvaara Y, Aalto K, Kallio PE. Acute patellar dislocation in children: incidence and associated osteochondral fractures. J Pediatr Orthop. 14:513–5 Available from: http://www.ncbi.nlm.nih.gov/pubmed/8077438. [DOI] [PubMed]
- 4.Hsiao M, Owens BD, Burks R, Sturdivant RX, Cameron KL. Incidence of acute traumatic patellar dislocation among active-duty United States military service members. Am J Sports Med. 2010;38:1997–2004. doi: 10.1177/0363546510371423. [DOI] [PubMed] [Google Scholar]
- 5.Sanders TL, Pareek A, Hewett TE, Stuart MJ, Dahm DL, Krych AJ. Incidence of first-time lateral patellar dislocation: a 21-year population-based study. Sports Health. 2018;10:146–151. doi: 10.1177/1941738117725055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fithian DC, Paxton EW, Lou SM, Silva P, Davis DK, Elias DA, et al. Epidemiology and natural history of acute patellar dislocation. Am J Sports Med. 2004;32:1114–1121. doi: 10.1177/0363546503260788. [DOI] [PubMed] [Google Scholar]
- 7.Lewallen L, Mcintosh A, Dahm D. First-time patellofemoral dislocation: risk factors for recurrent instability. J Knee Surg. 2015;28:303–310. doi: 10.1055/s-0034-1398373. [DOI] [PubMed] [Google Scholar]
- 8.Fabricant PD, Kocher MS. Anterior cruciate ligament injuries in children and adolescents. Orthop Clin North Am. 2016;47:777–788. doi: 10.1016/j.ocl.2016.05.004. [DOI] [PubMed] [Google Scholar]
- 9.Hiemstra LA, Kerslake S, Loewen M, Lafave M. Effect of trochlear dysplasia on outcomes after isolated soft tissue stabilization for patellar instability. Am J Sports Med. 2016;44:1515–1523. doi: 10.1177/0363546516635626. [DOI] [PubMed] [Google Scholar]
- 10.Hiemstra LA, Kerslake S, Lafave M. Medial patellofemoral ligament reconstruction femoral tunnel accuracy: relationship to disease-specific quality of life. Orthop J Sport Med. 2017;5:1–7. doi: 10.1177/2325967116687749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lafave MR, Hiemstra L, Kerslake S. Factor analysis and item reduction of the Banff Patella instability instrument (BPII): introduction of BPII 2.0. Am J Sports Med. 2016;44:2081–2086. doi: 10.1177/0363546516644605. [DOI] [PubMed] [Google Scholar]
- 12.Feller JA, Richmond AK, Wasiak J. Medial patellofemoral ligament reconstruction as an isolated or combined procedure for recurrent patellar instability. Knee Surgery, Sport Traumatol Arthrosc. 2014;22:2470–2476. doi: 10.1007/s00167-014-3132-0. [DOI] [PubMed] [Google Scholar]
- 13.Prinsen CAC, Mokkink LB, Bouter LM, Alonso J, Patrick DL, de Vet HCW, Terwee CB. COSMIN guideline for systematic reviews of patient-reported outcome measures. Qual Life Res. 2018;27:1147–1157. doi: 10.1007/s11136-018-1798-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Paxton EW, Fithian DC, Lou SM, Silva P. The reliability and validity of knee-specific and general health instruments in assessing acute patellar dislocation outcomes. Am J Sports Med. 2003;31:487–492. doi: 10.1177/03635465030310040201. [DOI] [PubMed] [Google Scholar]
- 15.• Cerciello S, Corona K, Morris BJ, Visonà E, Maccauro G, Maffulli N, et al. Cross-cultural adaptation and validation of the Italian versions of the Kujala, Larsen, Lysholm and Fulkerson scores in patients with patellofemoral disorders. J Orthop Traumatol. Springer International Publishing; 2018;19. 10.1186/s10195-018-0508-9. Cross-cultural adaptation looking specifically at outcomes measures in the Italian language for patients with patellofemoral instability. Includes the knee-specific outcome measures commonly used in this patient population. [DOI] [PMC free article] [PubMed]
- 16.• Dammerer D, Liebensteiner MC, Kujala UM, Emmanuel K, Kopf S, Dirisamer F, et al. Validation of the German version of the Kujala score in patients with patellofemoral instability: a prospective multi-centre study. Arch Orthop Trauma Surg. Springer Berlin Heidelberg; 2018;138:527–35. 10.1007/s00402-018-2881-5. Cross-cultural adaptation looking specifically at outcomes measures for patients with patellofemoral instability. [DOI] [PMC free article] [PubMed]
- 17.Smith TO, Davies L, O’Driscoll M-L, Donell ST. An evaluation of the clinical tests and outcome measures used to assess patellar instability. Knee. 2008;15:255–262. doi: 10.1016/j.knee.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 18.Hiemstra LA, Kerslake S, Lafave M, Mohtadi NG. Concurrent validation of the Banff Patella Instability Instrument to the Norwich Patellar Instability Score and the Kujala Score in patients with patellofemoral instability. Orthop J Sport Med. 2016;4:1–11. doi: 10.1177/2325967116646085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Matsushita T, Oka S, Araki D, Nishida K, Tanaka T, Kanzaki N, et al. Patient-based outcomes after medial patellofemoral ligament reconstruction. Int Orthop. 2017;41:1147–1153. doi: 10.1007/s00264-017-3433-2. [DOI] [PubMed] [Google Scholar]
- 20.Moiz M, Smith N, Smith TO, Chawla A, Thompson P, Metcalfe A. Clinical outcomes after the nonoperative management of lateral patellar dislocations: a systematic review. Orthop J Sport Med. 2018;6:2325967118766275. doi: 10.1177/2325967118766275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mokkink LB, Terwee CB, Knol DL, Stratford PW, Alonso J, Patrick DL, et al. The COSMIN checklist for evaluating the methodological quality of studies on measurement properties: a clarification of its content. BMC Med Res Methodol. 2010;10:1–6. doi: 10.1186/1471-2288-10-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.COSMIN. COSMIN taxonomy of measurement properties [Internet]. [cited 2018 Dec 16]. Available from: https://www.cosmin.nl/tools/cosmin-taxonomy-measurement-properties/.
- 23.Kujala UM, Jaakkola LH, Koskinen SK, Taimela S, Hurme M, Nelimarkka O. Scoring of patellofemoral disorders. Arthroscopy. 1993;9:159–163. doi: 10.1016/S0749-8063(05)80366-4. [DOI] [PubMed] [Google Scholar]
- 24.Tompkins MA, Arendt EA. Patellar instability factors in isolated medial patellofemoral ligament reconstructions—what does the literature tell us? A systematic review. Am J Sports Med. 2015;43:2318–2327. doi: 10.1177/0363546515571544. [DOI] [PubMed] [Google Scholar]
- 25.Balcarek P, Rehn S, Howells NR, Eldridge JD, Kita K, Dejour D, et al. Results of medial patellofemoral ligament reconstruction compared with trochleoplasty plus individual extensor apparatus balancing in patellar instability caused by severe trochlear dysplasia: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2017:3869–25, 3877 Available from: http://www.ncbi.nlm.nih.gov/pubmed/27796419. [DOI] [PubMed]
- 26.Testa EA, Camathias C, Amsler F, Henle P, Friederich NF, Hirschmann MT. Surgical treatment of patellofemoral instability using trochleoplasty or MPFL reconstruction: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2017;25:2309–2320. doi: 10.1007/s00167-015-3698-1. [DOI] [PubMed] [Google Scholar]
- 27.Watson CJ, Propps M, Ratner J, Zeigler DL, Horton P, Smith SS. Reliability and responsiveness of the lower extremity functional scale and the anterior knee pain scale in patients with anterior knee pain. J Orthop Sport Phys Ther. 2005;35:136–146. doi: 10.2519/jospt.2005.35.3.136. [DOI] [PubMed] [Google Scholar]
- 28.Ittenbach RF, Huang G, Foss KDB, Hewett TE, Myer GD. Reliability and validity of the anterior knee pain scale: applications for use as an epidemiologic screener. PLoS One. 2016;11:1–6. doi: 10.1371/journal.pone.0159204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Esculier J-F, Roy J-S, Bouyer LJ. Psychometric evidence of self-reported questionnaires for patellofemoral pain syndrome: a systematic review. Disabil Rehabil. 2013;35:2181–2190. doi: 10.3109/09638288.2013.774061. [DOI] [PubMed] [Google Scholar]
- 30.Hiemstra LA, Kerslake S, Lafave MR, Heard SM, Buchko GML, Mohtadi NGH. Initial validity and reliability of the Banff Patella Instability Instrument. Am J Sports Med. 2013;41:1629–1635. doi: 10.1177/0363546513487981. [DOI] [PubMed] [Google Scholar]
- 31.•• Smith TO, Chester R, Hunt N, Cross JL, Clark A, Donell ST. The Norwich Patellar Instability Score: validity, internal consistency and responsiveness for people conservatively-managed following first-time patellar dislocation. Knee. Elsevier B.V.; 2016;23:256–60. 10.1016/j.knee.2015.10.003. Psychometric evaluation of the NPI, one of two disease-specific outcomes for patients with patellofemoral instaiblity, evaluated in the first-time dislocator. [DOI] [PubMed]
- 32.Smith TO, Donell ST, Clark A, Chester R, Cross J, Kader DF, et al. The development, validation and internal consistency of the Norwich Patellar Instability (NPI) score. Knee Surgery, Sport Traumatol Arthrosc. 2014;22:324–335. doi: 10.1007/s00167-012-2359-x. [DOI] [PubMed] [Google Scholar]
- 33.Gao B, Dwivedi S, Fabricant PD, Cruz AI. Patterns in outcomes reporting of operatively managed pediatric patellofemoral instability: a systematic review and meta-analysis. Am J Sports Med. 2018;036354651876515. 10.1177/0363546518765152. [DOI] [PubMed]
- 34.Utting MR, Mulford JS, Eldridge JDJ. A prospective evaluation of trochleoplasty for the treatment of patellofemoral dislocation and instability. J Bone Joint Surg Br. 2008;90:180–185. doi: 10.1302/0301-620X.90B2.20017. [DOI] [PubMed] [Google Scholar]
- 35.Camathias C, Studer K, Kiapour A, Rutz E, Vavken P. Trochleoplasty as a solitary treatment for recurrent patellar dislocation results in good clinical outcome in adolescents. Am J Sports Med. 2016;44:2855–2863. doi: 10.1177/0363546516652894. [DOI] [PubMed] [Google Scholar]
- 36.Cheung RTH, Ngai SPC, Lam PL, Chiu JKW, Fung EYH. Chinese translation and validation of the Kujala scale for patients with patellofemoral pain. Disabil Rehabil. 2012;34:510–513. doi: 10.3109/09638288.2011.610494. [DOI] [PubMed] [Google Scholar]
- 37.Hamdan M, Haddad B, Isleem U, Hamad A, Hussein L, Shawareb Y, et al. Validation of the Arabic version of the Kujala patellofemoral pain scoring system. J Orthop Sci. 2018; Available from: http://www.ncbi.nlm.nih.gov/pubmed/30316659. [DOI] [PubMed]
- 38.Buckinx F, Bornheim S, Remy G, Van Beveren J, Reginster J, Bruyère O, et al. French translation and validation of the “Anterior Knee Pain Scale” (AKPS) Disabil Rehabil. 2017;0:1–6. doi: 10.1080/09638288.2017.1419288. [DOI] [PubMed] [Google Scholar]
- 39.Papadopoulos C, Constantinou A, Cheimonidou AZ, Stasinopoulos D. Greek cultural adaption and validation of the Kujala anterior knee pain scale in patients with patellofemoral pain syndrome. Disabil Rehabil. 2017;39:704–708. doi: 10.3109/09638288.2016.1161834. [DOI] [PubMed] [Google Scholar]
- 40.Sakunkaruna S, Sakunkaruna Y, Sakulsriprasert P. Thai version of the Kujala patellofemoral questionnaire in knee pain patients: cross-cultural validation and test-retest reliability. J Med Assoc Thai. 2015;98(Suppl 5):S81–S85. [PubMed] [Google Scholar]
- 41.Gil-Gámez J, Pecos-Martín D, Kujala UM, Martínez-Merinero P, Montañez-Aguilera FJ, Romero-Franco N, et al. Validation and cultural adaptation of “Kujala Score” in Spanish. Knee Surgery, Sport Traumatol Arthrosc. 2016;24:2845–2853. doi: 10.1007/s00167-015-3521-z. [DOI] [PubMed] [Google Scholar]
- 42.Ummels PEJ, Lenssen AF, Barendrecht M, Beurskens AJHM. Reliability of the Dutch translation of the Kujala patellofemoral score questionnaire. Physiother Res Int. 2017;22:299–319. doi: 10.1002/pri.1649. [DOI] [PubMed] [Google Scholar]
- 43.Negahban H, Pouretezad M, Yazdi MJS, Sohani SM, Mazaheri M, Salavati M, Aryan N, Salehi R. Persian translation and validation of the Kujala patellofemoral scale in patients with patellofemoral pain syndrome. Disabil Rehabil. 2012;34:2259–2263. doi: 10.3109/09638288.2012.683480. [DOI] [PubMed] [Google Scholar]
- 44.da Cunha RA, Hazime FA, da Silva Martins MC, Ferreira M, de Castro PA, Ejnisman B. Translation, cross-cultural adaptation, and clinimetric testing of instruments used to assess patients with ankle sprain in the Brazilian population. J Orthop Sport Phys Ther [Internet] 2016;46:1042–1050. doi: 10.2519/jospt.2016.6218. [DOI] [PubMed] [Google Scholar]
- 45.Kuru T, Dereli EE, Yaliman A. Validity of the Turkish version of the Kujala patellofemoral score in patellofemoral pain syndrome. Acta Orthop Traumatol Turc. 2010;44:152–156. doi: 10.3944/AOTT.2010.2252. [DOI] [PubMed] [Google Scholar]
- 46.Briggs KK, Steadman JR, Hay CJ, Hines SL. Lysholm score and tegner activity level in individuals with normal knees. Am J Sports Med. 2009;37:898–901. doi: 10.1177/0363546508330149. [DOI] [PubMed] [Google Scholar]
- 47.Anderson AF, Irrgang JJ, Kocher MS, Mann BJ, Harrast JJ. International Knee Documentation Committee. The International Knee Documentation Committee Subjective Knee Evaluation Form: normative data. Am J Sports Med. 2006;34:128–135. doi: 10.1177/0363546505280214. [DOI] [PubMed] [Google Scholar]
- 48.Nasreddine AY, Connell PL, Kalish LA, Nelson S, Iversen MD, Anderson AF, Kocher MS. The pediatric international knee documentation committee (Pedi-IKDC) subjective knee evaluation form. Am J Sports Med. 2017;45:527–534. doi: 10.1177/0363546516672456. [DOI] [PubMed] [Google Scholar]
- 49.Baldwin JN, McKay MJ, Simic M, Hiller CE, Moloney N, Nightingale EJ, et al. Self-reported knee pain and disability among healthy individuals: reference data and factors associated with the Knee injury and Osteoarthritis Outcome Score (KOOS) and KOOS-Child. Osteoarthr Cartil. 2017;25:1282–1290. doi: 10.1016/j.joca.2017.03.007. [DOI] [PubMed] [Google Scholar]
- 50.Lysholm J. Lysholm - 1982 Evaluation of knee ligament surgery results wiht special emphasis on use of a scoring scale.pdf. 150–4. [DOI] [PubMed]
- 51.Fulkerson JP, Becker GJ, Meaney JA, Miranda M, Folcik MA. Anteromedial tibial tubercle transfer without bone graft. Am J Sports Med. 1990;18:490–496. doi: 10.1177/036354659001800508. [DOI] [PubMed] [Google Scholar]
- 52.Demirdjian AM, Petrie SG, Guanche CA, Thomas KA. The outcomes of two knee scoring questionnaires in a normal population. Am J Sports Med. 26:46–51. Available from: http://www.ncbi.nlm.nih.gov/pubmed/9474400. [DOI] [PubMed]
- 53.Eshuis R, Lentjes GW, Tegner Y, Wolterbeek N, Veen MR. Dutch Translation and cross-cultural adaptation of the Lysholm Score and Tegner Activity Scale for patients with anterior cruciate ligament injuries. J Orthop Sports Phys Ther. 2016 [cited 2018 Dec 5];46:976–83. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27681449. [DOI] [PubMed]
- 54.Wang W, Liu L, Chang X, Jia ZY, Zhao JZ, Xu WD. Cross-cultural translation of the Lysholm knee score in Chinese and its validation in patients with anterior cruciate ligament injury. BMC Musculoskelet Disord. 2016;17:436. doi: 10.1186/s12891-016-1283-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Celik D, Coşkunsu D, Kiliçoğlu O. Translation and cultural adaptation of the Turkish Lysholm knee scale: ease of use, validity, and reliability. Clin Orthop Relat Res. 2013;471:2602–2610. doi: 10.1007/s11999-013-3046-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Piontek T, Ciemniewska-Gorzela K, Naczk J, Cichy K, Szulc A. Linguistic and cultural adaptation into Polish of the IKDC 2000 subjective knee evaluation form and the Lysholm scale. Polish Orthop Traumatol. 2012;77:115–119. [PubMed] [Google Scholar]
- 57.Irrgang JJ, Anderson AF, Boland AL, Harner CD, Kurosaka M, Neyret P, et al. Development and Validation of the International Knee Documentation Committee Subjective Knee Form *. 2001;29:600–13. [DOI] [PubMed]
- 58.Greco NJ, Anderson AF, Mann BJ, Cole BJ, Farr J, Nissen CW, et al. Responsiveness of the International Knee Documentation Committee Subjective Knee Form in Comparison to the Western Ontario and McMaster Universities Osteoarthritis Index, Modified Cincinnati Knee Rating System, and Short Form 36 in Patients with Focal Articular Cartilage Defects. Am J Sports Med. 2010 [cited 2018 Dec 5];38:891–902. 10.1177/0363546509354163. [DOI] [PubMed]
- 59.Neri T, Parker DA, Beach A, Gensac C, Boyer B, Farizon F, et al. Medial patellofemoral ligament reconstruction with or without tibial tubercle transfer is an effective treatment for patellofemoral instability. Knee Surg Sports Traumatol Arthrosc [Internet]. 2018; Available from: http://www.ncbi.nlm.nih.gov/pubmed/30167754. [DOI] [PubMed]
- 60.Wind RJP, Heesterbeek PJC, Wymenga AB. A combined procedure with Bereiter-type trochleoplasty leads to a stable patellofemoral joint at 5-year follow-up. Knee Surg Sports Traumatol Arthrosc. 2018; Available from: http://www.ncbi.nlm.nih.gov/pubmed/29947843. [DOI] [PubMed]
- 61.Yang Y, Zhang Q. Reconstruction of the medial patellofemoral ligament and reinforcement of the medial patellotibial ligament is an effective treatment for patellofemoral instability with patella alta. Knee Surg Sports Traumatol Arthrosc. 2018; Available from: http://www.ncbi.nlm.nih.gov/pubmed/30421164. [DOI] [PubMed]
- 62.Jia Z-Y, Zhang C, Zou Y, Huang X, Xu W-D. Translation and validation of the Simplified Chinese version of International Knee Documentation Committee Subjective Knee Form. Arch Orthop Trauma Surg. 2018;138:1433–1441. doi: 10.1007/s00402-018-2973-2. [DOI] [PubMed] [Google Scholar]
- 63.Fu S-N, Chan Y-H. Translation and validation of Chinese version of International Knee Documentation Committee Subjective Knee Form. Disabil Rehabil. 2011 [cited 2018 Dec 5];33:1186–9. 10.3109/09638288.2010.524274 [DOI] [PubMed]
- 64.Lertwanich P, Praphruetkit T, Keyurapan E, Lamsam C, Kulthanan T. Validity and reliability of Thai version of the International Knee Documentation Committee Subjective Knee Form. J Med Assoc Thai. 2008;91:1218–1225. [PubMed] [Google Scholar]
- 65.Tigerstrand Grevnerts H, Grävare Silbernagel K, Sonesson S, Ardern C, Österberg A, Gauffin H, et al. Translation and testing of measurement properties of the Swedish version of the IKDC subjective knee form. Scand J Med Sci Sports. 2017 [cited 2018 Dec 5];27:554–62. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28207954. [DOI] [PubMed]
- 66.Koumantakis GA, Tsoligkas K, Papoutsidakis A, Ververidis A, Drosos GI. Cross-cultural adaptation and validation of the International Knee Documentation Committee Subjective Knee Form in Greek. J Orthop Traumatol. 2016 [cited 2018 Dec 5];17:123–9. 10.1007/s10195-015-0362-y [DOI] [PMC free article] [PubMed]
- 67.Çelik D, Coşkunsu D, KiliÇoğlu Ö, Ergönül Ö, Irrgang JJ. Translation and cross-cultural adaptation of the international knee documentation committee subjective knee form into Turkish. J Orthop Sports Phys Ther. 2014 [cited 2018 Dec 5];44:899–909. 10.2519/jospt.2014.4865. [DOI] [PubMed]
- 68.Kümmel D, Preiss S, Harder LP, Leunig M, Impellizzeri FM. Measurement properties of the German version of the IKDC subjective knee form (IKDC-SKF). J patient-reported outcomes. 2018;2:31. Available from: http://www.ncbi.nlm.nih.gov/pubmed/30294711. [DOI] [PMC free article] [PubMed]
- 69.Kim JG, Ha JK, Lee JY, Seo SS, Choi CH, Lee MC. Translation and validation of the korean version of the international knee documentation committee subjective knee form. Knee Surg Relat Res. 2013 [cited 2018 Dec 5];25:106–11. 10.5792/ksrr.2013.25.3.106 [DOI] [PMC free article] [PubMed]
- 70.Metsavaht L, Leporace G, Riberto M, de Mello Sposito MM, Batista LA. Translation and cross-cultural adaptation of the Brazilian version of the International Knee Documentation Committee Subjective Knee Form: validity and reproducibility. Am J Sports Med. 2010 [cited 2018 Dec 5];38:1894–9. 10.1177/0363546510365314. [DOI] [PubMed]
- 71.van de Graaf VA, Wolterbeek N, Scholtes VAB, Mutsaerts ELAR, Poolman RW. Reliability and validity of the IKDC, KOOS, and WOMAC for patients with meniscal injuries. Am J Sports Med [Internet]. 2014 [cited 2018 Dec 5];42:1408–16. 10.1177/0363546514524698. [DOI] [PubMed]
- 72.Higgins LD, Taylor MK, Park D, Ghodadra N, Marchant M, Pietrobon R, et al. Fiabilité et validité du questionnaire d’évaluation subjective du genou de l’IKDC (Comité international de documentation du genou). Rev Rhum. Elsevier Masson; 2007 [cited 2018 Dec 5];74:1264–9. Available from: https://www.sciencedirect.com/science/article/pii/S1169833007003791
- 73.Kocher MS, Smith JT, Iversen MD, Brustowicz K, Ogunwole O, Andersen J, Yoo WJ, McFeely ED, Anderson AF, Zurakowski D. Reliability, validity, and responsiveness of a modified international knee documentation committee subjective knee form (Pedi-IKDC) in children with knee disorders. Am J Sports Med. 2011;39:933–939. doi: 10.1177/0363546510383002. [DOI] [PubMed] [Google Scholar]
- 74.Jacobsen JS, Knudsen P, Fynbo C, Rolving N, Warming S. Reproducibility and responsiveness of a Danish Pedi-IKDC subjective knee form for children with knee disorders. Scand J Med Sci Sport. 2016;26:1408–1414. doi: 10.1111/sms.12589. [DOI] [PubMed] [Google Scholar]
- 75.Spang RC, Tepolt FA, Paschos NK, Redler LH, Davis EA, Kocher MS. Combined reconstruction of the medial patellofemoral ligament (MPFL) and medial quadriceps tendon-femoral ligament (MQTFL) for patellar instability in children and adolescents: surgical technique and outcomes. J Pediatr Orthop. 2019;39:e54–e61. doi: 10.1097/BPO.0000000000001259. [DOI] [PubMed] [Google Scholar]
- 76.Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee Injury and Osteoarthritis Outcome Score (KOOS)—development of a self-administered outcome measure. J Orthop Sport Phys Ther. 1998;28:88–96. doi: 10.2519/jospt.1998.28.2.88. [DOI] [PubMed] [Google Scholar]
- 77.Crossley KM, Macri EM, Cowan SM, Collins NJ, Roos EM. The patellofemoral pain and osteoarthritis subscale of the KOOS (KOOS-PF): development and validation using the COSMIN checklist. Br J Sports Med. 2018;52:1130–1136. doi: 10.1136/bjsports-2016-096776. [DOI] [PubMed] [Google Scholar]
- 78.AOSSM Outcomes Task Force. Summary of clinical outcome measures for sports-related knee injuries: final report [Internet]. 2012. Available from: https://www.sportsmed.org/AOSSMIMIS/members/downloads/research/ClinicalOutcomeMeasuresKnee.pdf
- 79.Mulliez A, Lambrecht D, Verbruggen D, Van Der Straeten C, Verdonk P, Victor J. Clinical outcome in MPFL reconstruction with and without tuberositas transposition. Knee Surg Sports Traumatol Arthrosc. 2017;25:2708–2714. doi: 10.1007/s00167-015-3654-0. [DOI] [PubMed] [Google Scholar]
- 80.Blønd L, Haugegaard M. Combined arthroscopic deepening trochleoplasty and reconstruction of the medial patellofemoral ligament for patients with recurrent patella dislocation and trochlear dysplasia. Knee Surg Sports Traumatol Arthrosc. 2014;22:2484–2490. doi: 10.1007/s00167-013-2422-2. [DOI] [PubMed] [Google Scholar]
- 81.Askenberger M, Bengtsson Moström E, Ekström W, Arendt EA, Hellsten A, Mikkelsen C, Janarv PM. Operative repair of medial patellofemoral ligament injury versus knee brace in children with an acute first-time traumatic patellar dislocation: a randomized controlled trial. Am J Sports Med. 2018;46:2328–2340. doi: 10.1177/0363546518770616. [DOI] [PubMed] [Google Scholar]
- 82.Örtqvist M, Iversen MD, Janarv PM, Broström EW, Roos EM. Psychometric properties of the knee injury and osteoarthritis outcome score for children (KOOS-Child) in children with knee disorders. Br J Sports Med. 2014;48:1437–1446. doi: 10.1136/bjsports-2013-093164. [DOI] [PubMed] [Google Scholar]
- 83.Roos E. KOOS Website. 2018. [Google Scholar]
- 84.Örtqvist M, Roos EM, Broström EW, Janarv PM, Iversen MD. Development of the Knee Injury and Osteoarthritis Outcome Score for Children (KOOS-Child): comprehensibility and content validity. Acta Orthop. 2012;83:666–673. doi: 10.3109/17453674.2012.747921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Rioux Trottier E, Beauséjour M, Lamer S, Glavas P, Grimard G, Nault M-L. Validation of the French version of the KOOS-child questionnaire. Knee Surg Sports Traumatol Arthrosc. 2018; Available from: http://www.ncbi.nlm.nih.gov/pubmed/30465095. [DOI] [PubMed]
- 86.Smith TO, Donell ST, Chester R, Clark A, Stephenson R. What activities do patients with patellar instability perceive makes their patella unstable? Knee. Elsevier B.V.; 2011;18:333–339. 10.1016/j.knee.2010.07.003 [DOI] [PubMed]
- 87.• Becher C, Attal R, Balcarek P, Dirisamer F, Liebensteiner M, Pagenstert G, et al. Successful adaption of the Banff Patella Instability Instrument (BPII) 2.0 into German. Knee Surgery, Sport Traumatol Arthrosc. Springer Berlin Heidelberg; 2017;26:1–6. Validation of the BPII in the German language providing cross-cultural validity for the BPII. [DOI] [PubMed]
- 88.•• Lafave MR, Hiemstra LA, Kerslake S. Validity, reliability, and responsiveness of the Banff Patellar Instability Instrument (BPII) in a Adolescent Population. J Pediatr Orthop. 2018;38:e629–33. Available from: http://www.ncbi.nlm.nih.gov/pubmed/30199460. Validation of the BPII in the adolescent population. The only disease-specific PROM validated in the paediatric age group. [DOI] [PubMed]
- 89.Cella D, Hahn EA, Jensen SE, Butt Z, Nowinski CJ, Rothrock N, Lohr K. Types of patient-reported outcomes. RTI Press; 2015. Available from: https://www.ncbi.nlm.nih.gov/books/NBK424381/. [PubMed]
- 90.Ardern CL, Österberg A, Tagesson S, Gauf H, Webster KE, Kvist J. The impact of psychological readiness to return to sport and recreational activities after anterior cruciate ligament reconstruction. Br J Sports Med. 2014;48:1613–1619. doi: 10.1136/bjsports-2014-093842. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 303 kb)
(PDF 90.7 kb)