Abstract
Purpose of Review
The purpose of this article is to review common hand and wrist injuries experienced by tennis players.
Recent Findings
A myriad of different wrist pathologies can be seen in tennis players ranging from metacarpal and carpal stress fractures to triangular fibrocartilage injuries and ulnar impaction. These vary depending upon the nature of the player, stroke mechanics, and time point within the season.
Summary
A broad differential should guide work-up and management of wrist pain in tennis players.
Keywords: Tennis, Wrist pain, Tennis swing
Introduction
Epidemiology
With the ever increasing globalization of the sport, there has been a surge in the number of recreational tennis players [1–4]. Within the USA alone, there are an estimated 18 million participants, and the number continues to grow [3•, 5••]. Reported tennis injury rates range from 0.05 to 2.9 injuries per player per year or 0.04 to 3.0 injuries per 1000 h played [1]. Lower extremity injuries are more common that upper extremity injuries, with the majority of upper extremity injuries being chronic in nature [1]. The focus of this article is to review hand and wrist injuries encountered in tennis players.
Biomechanics
Given that most upper extremity injuries are chronic and result from non-contact mechanisms, the kinetic chain that generates a tennis serve is implicated as the root cause of upper extremity injuries in tennis [1]. The athletes vary in terms of their serve and groundstroke styles [6•, 7•]. The serve has been broken down to (1) wind-up, (2) early cocking, (3) late cocking, (4) acceleration, and (5) follow through. Forehand or backhand groundstrokes have been broken down to (1) racket preparation, (2) acceleration, and (3) follow through. The kinetic chain, or the route of energy that flows through the body during a serve or groundstroke, allows for effective transfer of energy to the ball. The hip, knee, shoulder, elbow, and wrist joints serve as sequential links in the kinetic chain that absorb, generate, and transmit energy. During these strokes, safe and efficient energy transmission through the kinetic chain depends on endurance and technique. As energy transfer between links becomes inefficient secondary to fatigue or poor technique, joints in the chain can become overloaded and subsequently injured. In an energy flow comparison between injured and non-injured tennis players, injured players demonstrated lower quality of energy flow through the kinetic chain, lower ball velocity, and higher rates of energy absorbed by the shoulder and elbow joint compared with non-injured players [8, 9].
The load delivered to the wrist during the forehand stroke varies depending on hand grip position [3•]. The four traditional single-handed hand grip positions include the continental, Eastern, semi-Western, and the Western (Fig. 1) [10].
Fig. 1.
a Eastern forehand grip. b Continental forehand grip (The pictures are courtesy of our colleagues as the United States Professional Tennis Association (USPTA))
In a survey of 370 division III and IV tennis players in Italy, Tagliafico and colleagues found that the Eastern grip position was associated with radial-sided wrist injuries (i.e., FCR tenosynovitis [n = 5], DeQuervain syndrome [n = 6], and intersection syndrome [n = 1]), while the Western and semi-Western grip positions were associated with ulnar-sided wrist injuries (i.e., ECU injuries [n = 30], TFCC lesions [n = 5]) [1]. Notably, none of the players used the continental, 75% of those injured used the Western or semi-Western grip, and 25% of those injured used the Eastern grip.
The impact position of the ball on the racquet and grip tightness can affect force transmission on the wrist [12, 13]. A 3D computer simulation model was used to examine the effect of these two parameters during a backhand groundstroke [13]. Off-centered impacts below the longitudinal axis of the racquet substantially increased wrist extension torque when compared with an impact that occurred at the center of the racquet [13]. Increased grip pressure resulted in a decrease in racquet rotation in the hand and a 20% increase in wrist extension torque compared with the normal grip condition. Ball-racquet location and grip tightness are important parameters when assessing the cause of a wrist or elbow problem in tennis players.
Hand and wrist injuries
Ulnar-sided disorders
Most ulnar-sided disorders are not mutually exclusive and as such should have a framework for their work up [14••]. Kakar and Garcia-Elias proposed the four-leaf clover algorithm to help the practitioner have a structured algorithm that considers the myriad of potential etiologies that cause DRUJ pain and develop a treatment plan. Decisions are based on the status of the sigmoid notch, the cartilage at the DRUJ, the nature of the static restraints (e.g., the TFCC), and the functionality of the dynamic stabilizers of the DRUJ, such as the ECU [14••]. Although we discuss several specific causes of ulnar-sided wrist pain in tennis players, it is important to use an algorithmic approach when diagnosing the cause of pain in these athletes to mitigate against poor outcomes and frustrations of the athlete.
Extensor carpi ulnaris (ECU) pathology is one of the most common etiologies of ulnar-sided wrist pain in tennis players [6•, 15, 16]. The ECU tendon and its fibrosseous subsheath are at particular risk during a forehand groundstroke [6•]. Injury occurs with repetitive overloading by forces that are transmitted to the wrist during impact of the racquet with a tennis ball. When top-spin is generated during this stroke, it requires that the player grips the racquet with a technique that further predisposes the ECU to injury by positioning the wrist in excessive ulnar deviation. The ECU tendon has also been recognized to be at risk for injury during a double handed backhand stroke [16]. A review of 12 elite tennis players who presented with traumatic ECU instability revealed that 10 of 12 of these injuries occurred in the non-dominant wrist (i.e., hand closest to the racquet head) while performing a double-handed backhand stroke, possibly due to eccentric contraction of the ECU muscle at the time of impact [16, 17].
Repetitive injury to the ECU tendon can result in ECU tendonitis or tenosynovitis [6•]. This can manifest with pain, clicking, and swelling along the ECU tendon that is exacerbated with wrist flexion, ulnar deviation, and supination. Alternatively, an acute injury can result in rupture of the subsheath or tendon. The ECU tendon runs in a fibro-osseous subsheath that is stabilized to the dorsal medial aspect of the ulna by a “labrum”-like tissue called the linea jugata, which deepens the concavity of the sulcus as well as the extensor retinculum that drapes over this subsheath and inserts onto the pisiform and triquetrum (Fig. 2) [16].
Fig. 2.
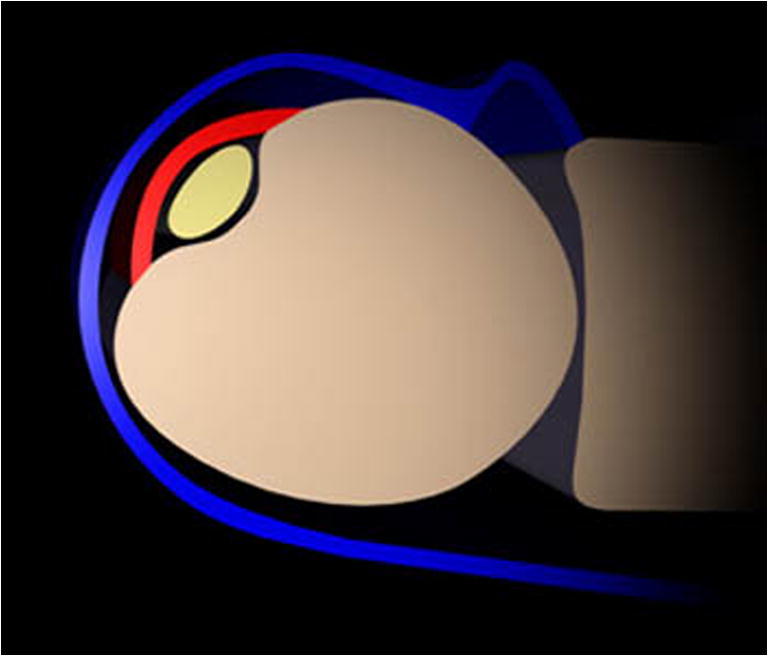
Illustration of the ECU tendon (yellow) within its subsheath (red) and enveloping extensor retinaculum (blue) (permission granted from Radsource http://radsource.us/extensor-carpi-ulnaris-subsheath-injury/)
A ruptured subsheath that can cause ECU tendon instability has been associated with a low forehand stroke that requires sudden supination of the flexed and ulnarly deviated wrist [6•]. Once the subsheath ruptures or detaches from the ulna, the ECU tendon is able to subluxate over the ulnar border especially during forearm supination.
Upon examination, patients may have swelling over the distal ulna with tenderness along its course that can be exacerbated with passive supination of the forearm [16]. The ECU synergy test has been demonstrated to effectively distinguish between ECU tendonitis and subsheath instability [18]. With the forearm in maximum supination, resisted abduction of the thumb and index finger results with the activation of the ECRL muscle with radial deviation of the wrist. To neutralize this, the ECU is activated, thereby stabilizing the wrist. The “ice cream scoop test” is also suggestive of ECU tendon instability [19]. The patient’s wrist is first positioned in pronation, ulnar deviation, and extension. The patient is then asked to simulate the maneuver that is used to scoop ice cream. The wrist moves into supination in the ulnar deviated position against the examiner resistance. If this produces a snapping or pain of the ECU tendon and reproduces the patients symptoms, the test is considered positive.
Radiographs should be obtained to rule out osseous pathology, and advanced imaging (i.e., MRI (Fig. 3) or dynamic ultrasound) may be used to supplement the history and physical examination findings [20••, 21••]. This is particularly important given the high incidence of ECU pathology in asymptomatic tennis players. Sole and colleagues used static and dynamic ultrasound to examine the ECU tendons in 26 asymptomatic recreational tennis players [21]. The authors found evidence of tendinosis or partial tears of the ECU in 92% (24/26) of the players, and 73% (19/26) players were found to have ECU instability in at least 1 wrist, despite the lack of clinical symptoms.
Fig. 3.
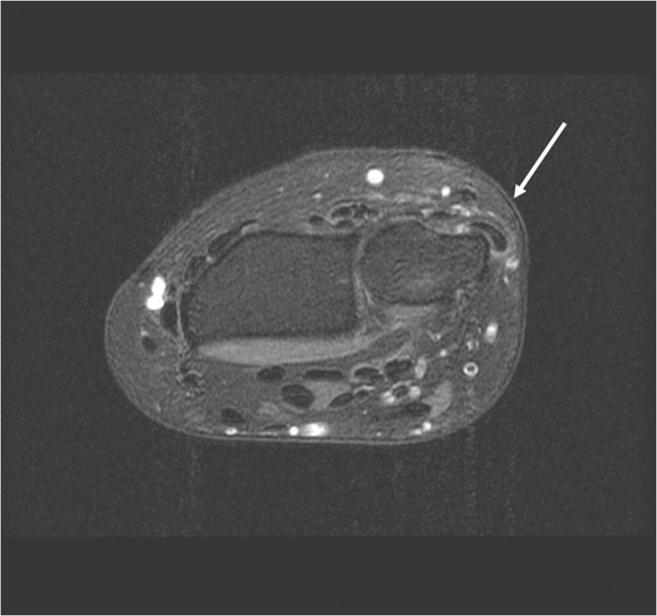
MRI demonstrating ECU tendon subluxation
ECU tendonitis is initially managed conservatively with non-steroidal anti-inflammatory drugs (NSAIDs), ice, activity modification, and splinting [6•]. If symptoms persist, a corticosteroid injection may alleviate the symptoms but care needs to ensure that the injection is placed appropriately to guard against fat atrophy and skin hypopigmentation. In cases of acute ECU instability, the wrist is initially managed with 6 weeks of above elbow casting/splinting with the wrist in pronation, extension, and radial deviation. Jeantroux and colleagues used MRI to evaluate 16 patients who were immobilized after an acute ECU subluxation injury [22]. All patients were treated with prolonged immobilization. On initial evaluation, 15 of these patients were demonstrated to have developed a pouch secondary to an ECU subsheath tear into which the ECU tendon can subluxate. Follow-up MRIs obtained in eight of these patients revealed that the pouch decreased in size with immobilization. Montalvan and colleagues immobilized five elite tennis players in a short arm plaster splint with the wrist in extension for 2–3 months after an acute ECU subluxation injury. If the tendon was found to be unstable on exam after 2 months of immobilization, the wrist was immobilized for another month. They reported that all five players had no evidence of persistent instability and were able to return to play 5 to 6 months after injury [16].
If ECU instability persists, several ECU subsheath reconstruction or tendon stabilization techniques have been successful at restoring stability, including anatomical repair of subsheath with or without ECU groove deepening, reconstruction with an extensor retinaculum graft, a radially or ulnar-based extensor retinaculum flap or reconstruction with a strip of flexor carpi ulnaris [16, 23••, 24•]. Inoue and Tamura reviewed 12 patients with recurrent ECU tendon instability who were treated with either ECU reconstruction with a strip extensor retinaculum (n = 5) or direct anatomic repair (n = 7) of the ECU subsheath or periosteum [25]. All 12 patients were reported to have regained normal motion, had completed resolution of pain and instability, and were able to return to previous work and sport activities.
Triangular fibrocartilage complex (TFCC) tears
The TFCC serves an important role in distal radioulnar joint (DRUJ) stability, as well as load transmission across the wrist. Injury to the TFCC, either acute or chronic, results in functional impairment related to ulnar-sided wrist pain and diminished grip strength [26]. The TFCC is comprised of eight components: triangular fibrocartilage disc proper, dorsal and volar radioulnar ligaments, meniscus homolog, ulcocarpal collateral ligament, ulnolunate ligmanet, ulnotriquetral ligament, and the extensor ulnaris tendon subsheath (Fig. 4) [27••, 28•].
Fig. 4.
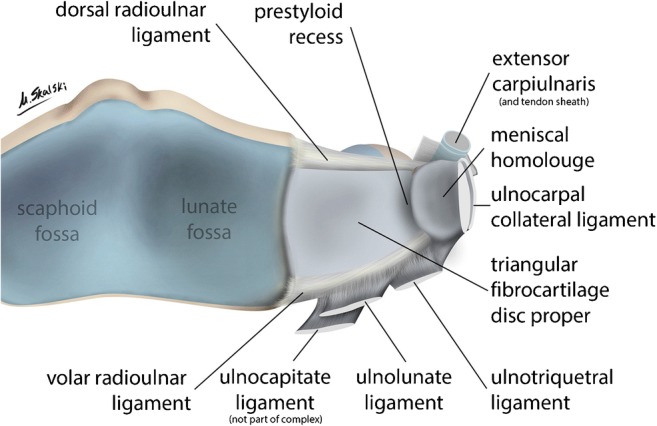
Illustration of the triangular fibrocartilage complex (TFCC). a–c Overview of the TFCC. d UL: ulnolunate, UT: ulnotriquetral, RU: radioulnar (reprinted with permission from Elsevier: Skalski MR, White EA, Patel DB, Schein AJ, RiveraMelo H, Matcuk GR. The traumatized TFCC: An illustrated review of the anatomy and injury patterns of the triangular fibrocartilage complex. Curr Probl Diagn Radiol. 2016;45(1):39–50. 10.1067/j.cpradiol.2015.05.004)
TFCC injuries can be traumatic or degenerative in nature. Patients complain of ulnar sided wrist pain, which is exacerbated with loading and rotation movements of the wrist. On examination, they may have tenderness at the fovea [29•]. The maneuver is performed with the patients forearm in neutral rotation. The examiner uses their thumb to apply a distally directed force between the ulnar styloid and the FCU tendon. The test is considered to be positive if it reproduces the pain experienced by the patient, and the pain is more severe than the pain produced with this same maneuver on the contralateral, normal side. With superficial tears the DRUJ remains stable but this stability can be compromised with foveal disruptions of the TFCC [26, 27••, 30••].
Radiographs should be obtained to rule out osseous pathology and are often negative unless accompanied by an ulna styloid fracture. Nakamura and colleagues examined the relationship between the displacement of the distal radius fracture, characteristics of the ulnar styloid fracture, and foveal disruption of the radioulnar ligaments that results in DRUJ instability [31]. Univariate analyses revealed that decreased radial inclination, increased radial shortening, and greater than 4-mm displacement of the ulnar styloid fragment were predictors of foveal avulsion of the radioulnar ligaments, which were associated with DRUJ instability. If a TFCC tear is suspected, an MRI can be obtained to evaluate the ulnar side of the wrist and assess for concomitant pathology. The specificity and sensitivity of the MRI for diagnosing ulnar-sided wrist pathology are 76 and 44%, repectively [13, 32•]. MR arthrography increases the sensitivity and specificity to 84 and 85%, respectively [32•]. Notably, interpretation of MRIs of 103 wrist MRIs of asymptomatic volunteers revealed TFCC abnormalities in 37% of the MRIs highlighting that advanced imaging should be utilized to confirm clinical assessment [33].
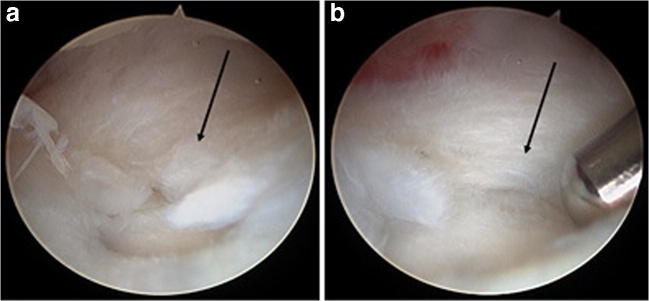
The Palmer classification categorizes TFCC injuries based on etiology and anatomic location [34••]. Class 1 lesions that result from a traumatic etiology, such as rotational injury to the wrist or a fall onto pronated or hyperextended wrist, are subclassified into four types: central tear (type A), traumatic avulsion from ulnar insertion (type B), distal avulsions of the TFCC (type C), or radial avulsion of TFCC (type D) [34••]. A class 2 lesion that results from a degenerative etiology, such as ulnar impaction syndrome, is subclassified into five types: wear of central portion without a perforation (type A), type A plus chondromalacia of the lunate, ulnar head or both (type B), perforation of the TFCC (type C), rupture of the lunotriquetral ligament as well as ulnar head and lunate cartilage degradation (type D), and type D plus ulocarpal arthritis (type E) [34••]. Initial management of TFCC injuries includes a series of conservative modalities, including NSAIDs, above elbow splinting to limit pronosupination, activity modification, and steroid injections [26]. Should these modalities fail, wrist arthroscopy is the gold standard for diagnosis of TFCC pathology. The blood supply of the TFCC determines which tears are amenable to repair or debridement [27••]. The central region of the TFCC is avascular and will not heal despite repair, while the peripheral region of the TFCC is amenable to repair [26, 27••]. Given the relative avascularity of the central region, these tears are often debrided, whereas the vascularized peripheral sided TFCC are amenable to open or arthroscopic treatment (Fig. 5).
Fig. 5.
a Central tear of the TFCC. b Arthroscopic debridement of central TFCC tear
Ulnotriquetral (UT) ligament split tears can present with ulnar-sided wrist pain [29•]. Repetitive forearm supination or pronation with the wrist extended predisposes these athletes to this injury [29•]. The UT ligament is a thickening of the wrist capsule and is one of the three primary stabilizers of the ulnar wrist [29•, 35–37]. This ligament originates from the palmar radioulnar ligament and the ulnar styloid and inserts onto triquetrum [29•] and is in its longest position with the wrist in extension and radial deviation [38]. As such, the ligament is suspected to be under the highest degree of tension, and therefore, at the highest risk for injury [29•]. Three hypothesis have been suggested for why the UT ligament tends to tear along its longitudinal axis: (1) force propagation through the normal anatomical perforations; (2) forces that result from traction and countertorsion; and (3) failure between the two distinct origin points of the ligament at the TFCC and ulnar styloid [35].
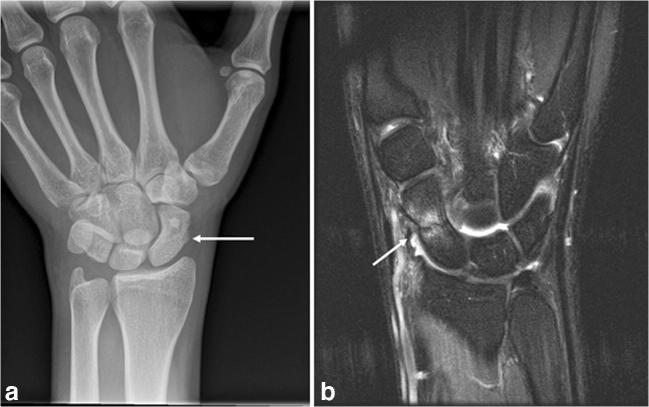
The majority of patients with UT ligament split tears report a discrete traumatic event that occurs with the wrist hyperextended and the forearm supinated [39]. Patients report ulnar-sided wrist pain that is exacerbated with pronosupination and gripping [39]. While range of motion of the wrist is generally unaffected, grip strength is diminished [39]. On examination, the most revealing maneuver is the ulnar fovea sign [29•]. The presence of DRUJ instability in association with a positive ulnar fovea sign is more consistent with a foveal disruption TFCC injury [29•]. Plain radiographs are often negative with [29•] MRI having a sensitivity of between 30 and 58% (Fig. 6) [40].
Fig. 6.
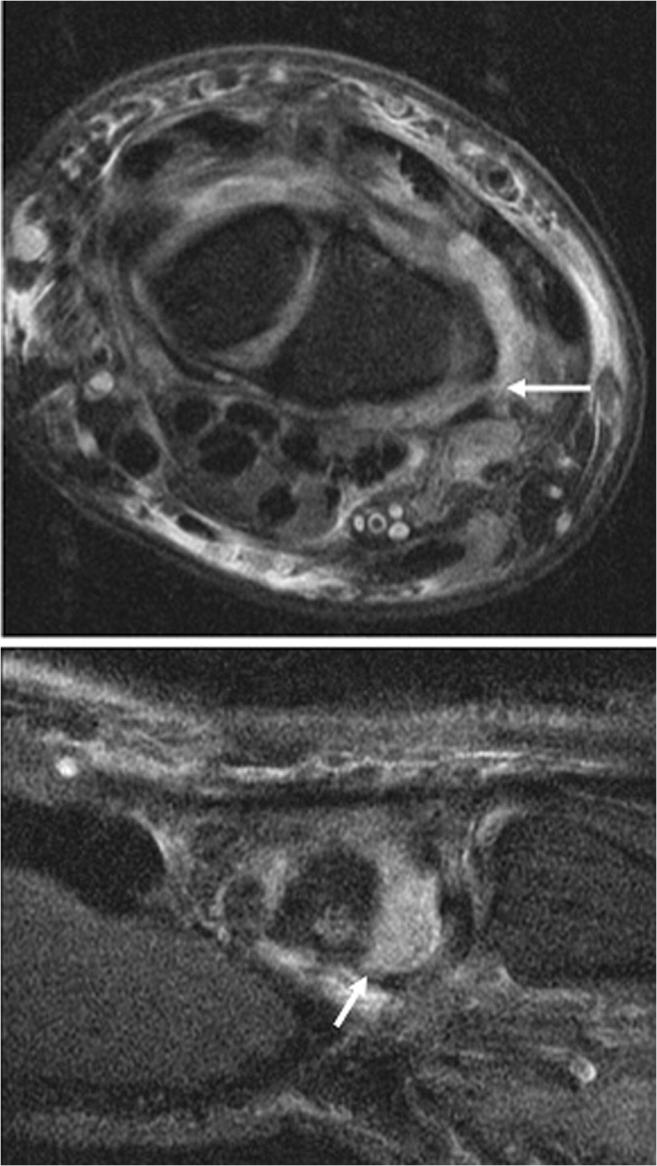
MRI demonstrating UT split tear (arrows)
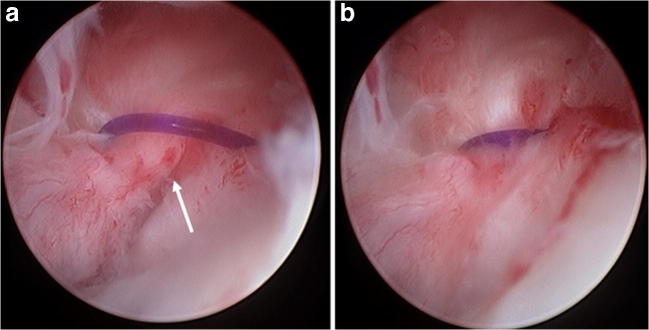
Non-operative treatment includes above elbow splinting or casting in neutral position for 6 weeks followed by a guided rehabilitation regimen. Should these patients fail non-operative treatment, the UT ligament split tears are amenable to arthroscopic repair (Fig. 7). In a series of UT ligament repairs, 90% of patients were reported to be satisfied and had no limitations in their activities after recovering from this intervention [39].
Fig. 7.
a UT ligament split tear (arrow). b UT ligament split tear after repair
Ulnar impaction syndrome is a source of ulnar wrist pain that results from the direct impact of the distal end of the ulna onto the ulnar carpus in patients with congential or acquired ulnar positive variance [41]. Palmer and Werner demonstrated that axial load transmission increased over twofold from 18 to 42% with just 2.5 mm of ulnar positive variance [42]. Patients present with insidious onset of ulnar wrist pain that is aggravated with the forearm in pronation and wrist in ulnar deviation [42]. True PA radiographs are examined for ulnar variance. If ulnar neutral or negative variance is noted, a pronated power grip view may reveal relative lengthening of the ulna. Additionally, radiographs will reveal evidence of degenerative changes (i.e., subchondral sclerosis and cysts) at the distal ulna, lunate, and triquetrum. MRI can effectively identify these focal degenerative changes as well as concomitant TFCC pathology. Imaeda and colleagues obtained MRIs in 30 wrists (27 patients) who were diagnosed with ulnar impaction syndrome [43]. A focal abnormal signal intensity at the ulnar proximal border of the lunate was identified in 87% of these wrists.
Conservative treatment of ulnar impaction syndrome includes NSAIDs, intermittent immobilization, and activity modification [44]. While ulnar impaction syndrome is not a condition that is isolated to tennis players, dynamic ulnar impaction syndrome (DUIS) was recently reported in the literature as a source of simultaneous TFCC injury and ulnar-sided wrist pain in two tennis players [45•]. It occurs when the ulna abuts the carpus during forearm pronation, where the radius becomes shorter relative to the ulna in individuals with an ulnar minus or neutral wrist [45•]. Both athletes underwent an arthroscopic wafer procedure, as well as debridement of the TFCC and loose bodies. One of the two patients had a simultaneous scapholunate ligament (SLL) tear that was addressed with debridement and percutaneous pinning. The patient with the isolated DUIS was reported to return to sport with no pain 4 months after the surgery.
The primary objective of surgical interventions is to unload the ulnocarpal joint by reducing ulnar positive variance [34••, 41]. Options include an ulnar shortening (metaphyseal or diaphyseal) osteotomy or resection of the ulnar head (i.e., open or arthroscopic wafer resection) (Fig. 8) [34••, 41]. A recent comparison of ulnar shortening osteotomy (n = 23) and arthroscopic wafer procedure (n = 19) for idiopathic ulnar impaction syndrome reported that at 3 months, patients who underwent the arthroscopic wafer procedure had better grip strength and DASH score and that the outcomes were similar at 6, 12, and 24 months. Stockton and colleagues conducted a systematic review of 36 studies that examined the outcomes related to surgical treatment of ulnar impaction syndrome. The three surgical interventions that were examined included ulnar shortening ostetomy, open, and arthroscopic wafer procedures. The authors noted good or excellent outcomes in 82% of patients who underwent an arthroscopic wafer procedure, 87% who underwent an open wafer procedure, and 76% of patients who underwent an ulnar shortending osteotomy [46••]. Although their study appears to show that the wafer procedure is superior to an ulnar shortening osteotomy, they reported that they could not establish clinical superiority in their study.
Fig. 8.
a Ulnar positive wrist. b Correction of ulnar positive variance with ulnar shortening osteotomy
Hook of hamate fractures can result from an acute traumatic event (i.e., fall onto outstretched hand) or from repetitive impaction of the handle of the racquet against the carpus (Fig. 9) [47•].
Fig. 9.
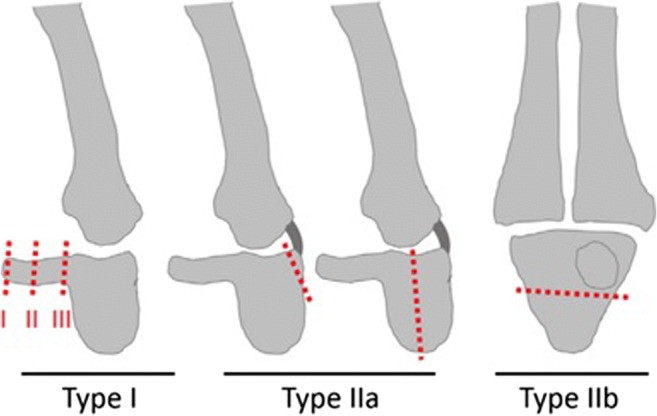
Modified Milch’s classification of hamate fractures. Type I: hook fractures—I(I): avulsion fractures; I (II): middle hook fracture; Type I(III): base hook fracture . Type IIa: coronal body fractures. Type IIb: transverse body fractures [48, 49]. (Figure reprinted by permission from Nature/Springer/Palgrave), J Huazhong Univ Sci Technolog Med Sci.: L. Xiong G, Dai L, Zheng W, Sun Y, Tian G. Clinical classification and treatment strategy of hamate hook fracture. 2010;30(6):762–766. 10.1007/s11596-010-0654-7))
Patients often present with non-specific symptoms, including tenderness in the hypothenar eminence, ulnar nerve parasthesias, and even possible rupture of the ulnar flexor digitorum profundus tendons. Patients are tender over the hook of the hamate and should be examined for the integrity of the flexor tendons and ulnar nerve. The examiner needs to have a high index of suspicion for this diagnosis as standard AP and lateral plain radiographs can miss the fracture. A carpal tunnel view or advanced imaging, such as a CT scan, can help delineate this injury (Fig. 10) [20••]. Non-displaced acute fractures of the hook of the hamate can be treated conservatively with a short arm cast [47•]. Displaced fractures and fracture non-unions of the hook of the hamate can be treated by either fixation or excision [47•]. After excision, patients rehabilitation can be accelerated once the wound has healed but should be warned of scar sensitivity that can be protected using a padded glove. Kadar and colleagues reviewed 51 cases of hook of the hamate fractures, 37 of which were managed non-operatively and 14 were managed operatively (4 ORIF and 10 excisions) [50•]. Both groups had good clinical results achieving 80% of grip strength compared with uninjured side and a mean Quickdash of 2. Twelve patients in the non-operative group resulted in non-union.
Fig. 10.

Carpal tunnel view of hamate fracture (arrow)
Radial-sided disorders
First dorsal compartment tendonitis (Dequervain’s) is a common source of radial-sided wrist pain in tennis players, especially in those with an Eastern grip [51]. The contents of the first dorsal compartment include the abductor pollicis longus (APL),extensor pollicis brevis (EPB), [52•]. The compartment has been demonstrated to contain a septum that divides the APL and EPB in approximately 50% of wrists [52•]. Cumulative over use of the wrist results in inflammation and thickening of peritendinous tissues of the APL and the EPB tendons. This results in tenderness and swelling at the dorsal wrist overlying the first dorsal compartment. Patients complain of pain overlying the tip of radial styloid process, difficulty with twisting, lifting and grasping activities involving the thumb, and diminished grip strength [53, 54]. On examination, patients have tenderness of the first dorsal compartment overlying the radial styloid. Eichoff first described a method of eliciting pain in patients with first dorsal compartment tenosynovitis by asking the patient to grip their thumb with their ipsilateral palm [54]. A positive test is associated with severe discomfort associate with this maneuver. Finklestein reported that patients with first dorsal compartment tenosynovitis will experience excruciating pain when the examiner grabs the patient’s thumb and abducts the hand ulnarly [55].
Radiographs can be obtained to rule out other causes of radial wrist pain, such as carpometacarpal or scaphotrapeziotrapezoidal arthritis or an occult scaphoid fracture if the history signifies a recent or past fall [54]. Ultrasound of first dorsal compartment tendonitis demonstrates diffuse circumferential hypoechoic thickening of the synovial sheath, which appears as a double target pattern [53]. This modality can be used to confirm the diagnosis and help the examiner target the compartment with an injection if indicated [53]. MRI has been demonstrated to be an effective modality for preoperatively detecting multiple tendon slips and compartmentalization of the first dorsal compartment, in addition to identifying evidence of tenosynovitis [56••].
Non-operative treatment includes activity modification, thumb spica immobilization, corticosteroid injections, and therapy [57••]. Weiss and colleagues demonstrated that 69% of patients had complete resolution of symptoms with injection alone, 57% with injection plus splint, and only 30% with splint alone [58]. If patients continue to have refractory symptoms, surgical release of the first dorsal compartment with careful release of all the subsheaths of the EPB tendon slips and protection of the dorsal senory branch of the radial and lateral antebrachial cutaneous nerves is advocated with excellent results [52•]. Scheller and colleagues reported 100% resolution of symptoms after surgical release of 94 patients with first dorsal compartment tenosynovitis [59].
Intersection syndrome can be seen within tennis players where [11] the first dorsal (APL and EPB) and second dorsal compartments (extensor carpi radialis brevis [ECRB] and extensor carpi radial longus [ECRL]) intersect about 4 cm proximal to the wrist. Patients present with pain localized to this area. Onset of pain is most often gradual and is associated with repetitive activity. While the muscle bellies of APL and EPB have been demonstrated to be swollen, the main cause of the pain is suspected to be tenosynovitis of the ECRL and ECRB [60].
On examination, patients have swelling, tenderness, and erythema approximately 4 cm proximal to the wrist [60]. A specific sign on exam is the presence of crepitus that is produced with wrist extension and flexion; however, this may not be present in all patients with this condition [60]. Imaging should include radiographs to rule out osseous injury, and ultrasound or MRI could be obtained to support the diagnosis [61].
Treatment of intersection initially includes activity modification, wrist extension splinting, therapy, or corticosteroid injections. This algorithm is thought to be effective in approximately 60% of patients. If patients fail to respond to this conservative treatment regimen, isolated release of the second dorsal compartment can be effective in treating this condition [60]. Grundberg and Reagan reported complete resolution of symptoms in 13 patients with intersection syndrome who had isolated release of the second dorsal compartment [60].
Stress fractures of the scaphoid have been associated with repetitive dorsiflexion of the wrist [62]. In a recent report, a tennis player was diagnosed with a scaphoid stress fracture after he presented with severe dorsal wrist pain after a backhand groundstroke [62]. The patient reported 4 months of antecedent dorsal wrist pain that was exacerbated with dorsiflexion of the wrist. On examination, patients are tender within the anatomical snuffbox. Radiographs should include an AP, lateral, and scaphoid view. If the radiographs are negative, an MRI scan may help with the diagnosis of these injuries (Fig. 11). Further evaluation with a CT scan can reveal sclerosis at the edge of the fracture line consistent with an antecedent stress fracture. Treatment can comprise of cast treatment until union versus surgical stabilization. Bond and colleagues randomized patients with non-displaced scaphoid fractures to undergo percutaneous compression screw fixation versus cast immobilization [63]. They reported that patients who underwent surgical stabilization of the fracture had a significantly shorter time to union at 7 weeks compared with 12 weeks. Similarly, Inoue and Shinoya reviewed their series of acute scaphoid fractures who either underwent percutaneous screw fixation or casting and reported that the screw fixation group had a significantly shorter time to union (6 weeks vs 10 weeks) [64].
Fig. 11.
a Non-displaced scaphoid waist fracture (arrow). b T2-weighted MRI demonstrating extensive evidence of scaphoid waist fracture (arrow)
Metacarpal stress fractures, secondary to repetitive microtrauma, can present as a cause of hand pain in the athlete as a sequelae of the repetitive impact of the racquet handle, increased training and swing intensity, and alterations in biomechanics of the grip that could result from altering the racquet grip diameter [3•]. On examination, tenderness is located over the affected metacarpal. Plain radiographs could reveal nonspecific cortical thickening and sclerosis. While bone scintigraphy can demonstrate increased uptake at a stress fracture site and can be used in combination with plain radiographs to confirm the presence of a metacarpal stress fracture, this diagnostic modality is invasive and exposes the patient to additional radiation. As such, MRI scans are more commonly used to detect these injuries. Stress fractures are successfully managed with a 6–10-week period of rest and activity modification with return to sport at 8–16 weeks [65].
Conclusion
With changes in racquet technology, grips, and the increasing forces generated during the tennis stroke, there is an increasing incidence of hand and wrist injuries in tennis athletes. Having a detailed understanding of the anatomic structures at risk can improve the accuracy and timeliness of the diagnosis of these injuries and the appropriate treatment. By dividing the conditions into radial and ulnar sided disorders, the players, trainers, and practitioners can succinctly manage these disorders.
Compliance with ethical standards
Conflict of Interest
Joseph A. Gil and Sanjeev Kakar each declare no potential conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Injuries in Overhead Athletes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Pluim BM, Staal JB, Windler GE, Jayanthi N. Tennis injuries: occurrence, aetiology, and prevention. Br J Sports Med. 2006;40(5):415–423. doi: 10.1136/bjsm.2005.023184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kibler WB, Safran MR. Musculoskeletal injuries in the young tennis player. Clin Sports Med. 2000;19(4):781–792. doi: 10.1016/S0278-5919(05)70237-4. [DOI] [PubMed] [Google Scholar]
- 3.Dines JS, Bedi A, Williams PN, Dodson CC, Ellenbecker TS, Altchek DW, Windler G, Dines DM. Tennis injuries. J Am Acad Orthop Surg. 2015;23(3):181–189. doi: 10.5435/JAAOS-D-13-00148. [DOI] [PubMed] [Google Scholar]
- 4.Abrams GD, Renstrom PA, Safran MR. Epidemiology of musculoskeletal injury in the tennis player. Br J Sports Med. 2012;46(7):492–498. doi: 10.1136/bjsports-2012-091164. [DOI] [PubMed] [Google Scholar]
- 5.Fu MC, Ellenbecker TS, Renstrom PA, Windler GS, Dines DM. Epidemiology of injuries in tennis players. Curr Rev Musculoskelet Med. 2018;11(1):1–5. doi: 10.1007/s12178-018-9452-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chung KC, Lark ME. Upper extremity injuries in tennis players: diagnosis, treatment, and management. Hand Clin. 2017;33(1):175–186. doi: 10.1016/j.hcl.2016.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abrams GD, Sheets AL, Andriacchi TP, Safran MR. Review of tennis serve motion analysis and the biomechanics of three serve types with implications for injury. Sport Biomech. 2011;10(4):378–390. doi: 10.1080/14763141.2011.629302. [DOI] [PubMed] [Google Scholar]
- 8.Martin C, Bideau B, Bideau N, Nicolas G, Delamarche P, Kulpa R. Energy flow analysis during the tennis serve: comparison between injured and noninjured tennis players. Am J Sports Med. 2014;42(11):2751–2760. doi: 10.1177/0363546514547173. [DOI] [PubMed] [Google Scholar]
- 9.Martin C, Bideau B, Bideau N, Nicolas G, Delamarche P, Kulpa R. Energy flow analysis during the tennis serve. Am J Sports Med. 2014;42(11):2751–2760. doi: 10.1177/0363546514547173. [DOI] [PubMed] [Google Scholar]
- 10.Tagliafico A, Cadoni A, Bignotti B, Martinoli C. High-resolution ultrasound of rotator cuff and biceps reflection pulley in non-elite junior tennis players: anatomical study. BMC Musculoskelet Disord. 2014;15(1):241. doi: 10.1186/1471-2474-15-241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tagliafico AS, Ameri P, Michaud J, Derchi LE, Sormani MP, Martinoli C. Wrist injuries in nonprofessional tennis players: relationships with different grips. Am J Sports Med. 2009;37(4):760–767. doi: 10.1177/0363546508328112. [DOI] [PubMed] [Google Scholar]
- 12.Pluim BM. The evolution and impact of science in tennis: eight advances for performance and health. Br J Sports Med. 2014;48(Suppl 1):i3–i5. doi: 10.1136/bjsports-2014-093434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.King MA, Kentel BB, Mitchell SR. The effects of ball impact location and grip tightness on the arm, racquet and ball for one-handed tennis backhand groundstrokes. J Biomech. 2012;45(6):1048–1052. doi: 10.1016/j.jbiomech.2011.12.028. [DOI] [PubMed] [Google Scholar]
- 14.Kakar S, Garcia-Elias M. “The Four-leaf clover” treatment algorithm: a practical approach to manage disorders of the distal radioulnar joint. J Hand Surg Am. 2016;41(4):551–564. doi: 10.1016/j.jhsa.2016.01.005. [DOI] [PubMed] [Google Scholar]
- 15.Graham TJ. Pathologies of the extensor carpi ulnaris (ECU) tendon and its investments in the athlete. Hand Clin. 2012;28(3):345–356. doi: 10.1016/j.hcl.2012.05.049. [DOI] [PubMed] [Google Scholar]
- 16.Montalvan B, Parier J, Brasseur JL, Le Viet D, Drape JL. Extensor carpi ulnaris injuries in tennis players: a study of 28 cases. Br J Sports Med. 2006;40(5):424–429. doi: 10.1136/bjsm.2005.023275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Blackwell JR, Cole KJ. Wrist kinematics differ in expert and novice tennis players performing the backhand stroke: implications for tennis elbow. J Biomech. 1994;27(5):509–516. doi: 10.1016/0021-9290(94)90062-0. [DOI] [PubMed] [Google Scholar]
- 18.Ruland RT, Hogan CJ. The ECU synergy test: an aid to diagnose ECU tendonitis. J Hand Surg Am. 2008;33(10):1777–1782. doi: 10.1016/j.jhsa.2008.08.018. [DOI] [PubMed] [Google Scholar]
- 19.Ng CY, Hayton MJ. Ice cream scoop test: a novel clinical test to diagnose extensor carpi ulnaris instability. J Hand Surg Eur Vol. 2013;38(5):569–570. doi: 10.1177/1753193412460816. [DOI] [PubMed] [Google Scholar]
- 20.Spicer PJ, Romesberg A, Kamineni S, Beaman FD. Ultrasound of extensor carpi ulnaris tendon subluxation in a tennis player. Ultrasound Q. 2016;32(2):191–193. doi: 10.1097/RUQ.0000000000000177. [DOI] [PubMed] [Google Scholar]
- 21.Sole JS, Wisniewski SJ, Newcomer KL, Maida E, Smith J. Sonographic evaluation of the extensor carpi ulnaris in asymptomatic tennis players. PM&R. 2015;7(3):255–263. doi: 10.1016/j.pmrj.2014.08.951. [DOI] [PubMed] [Google Scholar]
- 22.Jeantroux J, Becce F, Guerini H, Montalvan B, Le Viet D, Drapé J-L. Athletic injuries of the extensor carpi ulnaris subsheath: MRI findings and utility of gadolinium-enhanced fat-saturated T1-weighted sequences with wrist pronation and supination. Eur Radiol. 2011;21(1):160–166. doi: 10.1007/s00330-010-1887-3. [DOI] [PubMed] [Google Scholar]
- 23.Ruchelsman DE, Vitale MA. Extensor carpi ulnaris subsheath reconstruction. J Hand Surg Am. 2016;41(11):e433–e439. doi: 10.1016/j.jhsa.2016.08.009. [DOI] [PubMed] [Google Scholar]
- 24.Conroy C, Ruchelsman DE, Vitale MA. Extensor carpi ulnaris instability in athletes—diagnosis and treatment. Oper Tech Sports Med. 2016;24(2):139–147. doi: 10.1053/j.otsm.2016.01.003. [DOI] [Google Scholar]
- 25.Inoue G, Tamura Y. Surgical treatment for recurrent dislocation of the extensor carpi ulnaris tendon. J Hand Surg Br Eur Vol. 2001;26(6):556–559. doi: 10.1054/jhsb.2001.0615. [DOI] [PubMed] [Google Scholar]
- 26.Wysocki RW, Richard MJ, Crowe MM, Leversedge FJ, Ruch DS. Arthroscopic treatment of peripheral triangular fibrocartilage complex tears with the deep fibers intact. J Hand Surg Am. 2012;37(3):509–516. doi: 10.1016/j.jhsa.2011.12.023. [DOI] [PubMed] [Google Scholar]
- 27.Skalski, MR WEA, Patel DB, Schein AJ, RiveraMelo H, Matcuk GR. The traumatized TFCC: an illustrated review of the anatomy and injury patterns of the triangular fibrocartilage complex. Curr Probl Diagn Radiol. 2016;45(1):39–50. doi: 10.1067/j.cpradiol.2015.05.004. [DOI] [PubMed] [Google Scholar]
- 28.Pidgeon TS, Waryasz G, Carnevale J, DaSilva MF. Triangular fibrocartilage complex. JBJS Rev. 2015;3(1):1. doi: 10.2106/JBJS.RVW.N.00053. [DOI] [PubMed] [Google Scholar]
- 29.Hyatt BT, Rhee PC. Longitudinal split tears of the ulnotriquetral ligament. Oper Tech Sports Med. 2016;24(2):126–130. doi: 10.1053/j.otsm.2016.01.004. [DOI] [Google Scholar]
- 30.Cody ME, Nakamura DT, Small KM, Yoshioka HMR. Imaging of the triangular fibrocartilage complex. Magn Reson Imaging Clin N Am. 2015;23(3):393–403. doi: 10.1016/j.mric.2015.04.001. [DOI] [PubMed] [Google Scholar]
- 31.Nakamura T, Iwamoto T, Matsumura N, Sato K, Toyama Y. Radiographic and arthroscopic assessment of DRUJ instability due to foveal avulsion of the radioulnar ligament in distal radius fractures. J Wrist Surg. 2014;03(01):012–017. doi: 10.1055/s-0033-1364175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.DaSilva MF, Goodman AD, Gil JA, Akelman E. Evaluation of ulnar-sided wrist pain. J Am Acad Orthop Surg. 2017;25(8):e150–e156. doi: 10.5435/JAAOS-D-16-00407. [DOI] [PubMed] [Google Scholar]
- 33.Iordache SD, Rowan R, Garvin GJ, Osman S, Grewal R, Faber KJ. Prevalence of triangular fibrocartilage complex abnormalities on MRI scans of asymptomatic wrists. J Hand Surg Am. 2012;37(1):98–103. doi: 10.1016/j.jhsa.2011.10.006. [DOI] [PubMed] [Google Scholar]
- 34.Kirchberger MC, Unglaub F, Mühldorfer-Fodor M, et al. Update TFCC: histology and pathology, classification, examination and diagnostics. Arch Orthop Trauma Surg. 2015;135(3):427–437. doi: 10.1007/s00402-015-2153-6. [DOI] [PubMed] [Google Scholar]
- 35.Berger RA. The anatomy of the ligaments of the wrist and distal radioulnar joints. Clin Orthop Relat Res. 2001;383:32–40. doi: 10.1097/00003086-200102000-00006. [DOI] [PubMed] [Google Scholar]
- 36.Garcia-Elias M. Soft-tissue anatomy and relationships about the distal ulna. Hand Clin. 1998;14(2):165–176. [PubMed] [Google Scholar]
- 37.Sasao S, Beppu M, Kihara H, Hirata K, Takagi M. An anatomical study of the ligaments of the ulnar compartment of the wrist. Hand Surg. 2003;8(2):219–226. doi: 10.1142/S0218810403001844. [DOI] [PubMed] [Google Scholar]
- 38.Tang JB, Gu XK, Xu J, Gu JH. In vivo length changes of carpal ligaments of the wrist during dart-throwing motion. J Hand Surg Am. 2011;36(2):284–290. doi: 10.1016/j.jhsa.2010.11.025. [DOI] [PubMed] [Google Scholar]
- 39.Tay S-C, Berger RA, Parker WL. Longitudinal split tears of the ulnotriquetral ligament. Hand Clin. 2010;26(4):495–501. doi: 10.1016/j.hcl.2010.07.004. [DOI] [PubMed] [Google Scholar]
- 40.Ringler MD, Howe BM, Amrami KK, Hagen CE, Berger RA. Utility of magnetic resonance imaging for detection of longitudinal split tear of the ulnotriquetral ligament. J Hand Surg Am. 2013;38(9):1723–1727. doi: 10.1016/j.jhsa.2013.05.040. [DOI] [PubMed] [Google Scholar]
- 41.Sachar K. Ulnar-sided wrist pain: evaluation and treatment of triangular fibrocartilage complex tears, ulnocarpal impaction syndrome, and lunotriquetral ligament tears. J Hand Surg Am. 2012;37(7):1489–1500. doi: 10.1016/j.jhsa.2012.04.036. [DOI] [PubMed] [Google Scholar]
- 42.Palmer AK, Werner FW. Biomechanics of the distal radioulnar joint. Clin Orthop Relat Res. 187:26–35 http://www.ncbi.nlm.nih.gov/pubmed/6744728. Accessed 20 Aug 2018. [PubMed]
- 43.Imaeda T, Nakamura R, Shionoya K, Makino N. Ulnar impaction syndrome: MR imaging findings. Radiology. 1996;201(2):495–500. doi: 10.1148/radiology.201.2.8888248. [DOI] [PubMed] [Google Scholar]
- 44.Sachar K. Ulnar-sided wrist pain: evaluation and treatment of triangular fibrocartilage complex tears, ulnocarpal impaction syndrome, and lunotriquetral ligament tears. J Hand Surg Am. 2008;33(9):1669–1679. doi: 10.1016/j.jhsa.2008.08.026. [DOI] [PubMed] [Google Scholar]
- 45.França Bisneto E de N. Dynamic ulnar impaction syndrome in tennis players: report of two cases. Rev Bras Ortop. 2017;52(5):621–624. doi: 10.1016/j.rbo.2016.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Stockton DJ, Pelletier M-E, Pike JM. Operative treatment of ulnar impaction syndrome: a systematic review. J Hand Surg Eur Vol. 2015;40(5):470–476. doi: 10.1177/1753193414541749. [DOI] [PubMed] [Google Scholar]
- 47.Josipovic M, Bozic D, Bohacek I, Smoljanovic T, Bojanic I. Hamate hook nonunion initially mistaken for ulnar nerve compression: a case report with review of literature. Wien Klin Wochenschr. 2017;129(3–4):136–140. doi: 10.1007/s00508-016-1114-6. [DOI] [PubMed] [Google Scholar]
- 48.Xiong G, Dai L, Zheng W, Sun Y, Tian G. Clinical classification and treatment strategy of hamate hook fracture. J Huazhong Univ Sci Technol Med Sci. 2010;30(6):762–766. doi: 10.1007/s11596-010-0654-7. [DOI] [PubMed] [Google Scholar]
- 49.Lutter C, Schweizer A, Hochholzer T, Bayer T, Schöffl V. Pulling harder than the hamate tolerates: evaluation of hamate injuries in rock climbing and bouldering. Wilderness Environ Med. 2016;27(4):492–499. doi: 10.1016/j.wem.2016.09.003. [DOI] [PubMed] [Google Scholar]
- 50.Kadar A, Bishop AT, Suchyta MA, Moran SL. Diagnosis and management of hook of hamate fractures. J Hand Surg Eur Vol. 2018;43(5):539–545. doi: 10.1177/1753193417729603. [DOI] [PubMed] [Google Scholar]
- 51.Osterman AL, Moskow L, Low DW. Soft-tissue injuries of the hand and wrist in racquet sports. Clin Sports Med. 1988;7(2):329–348. [PubMed] [Google Scholar]
- 52.Nam YS, Doh G, Hong KY, Lim S, Eo S. Anatomical study of the first dorsal extensor compartment for the treatment of de Quervain’s disease. Ann Anat. 2018;218:250–255. doi: 10.1016/j.aanat.2018.04.007. [DOI] [PubMed] [Google Scholar]
- 53.Kamel M, Moghazy K, Eid H, Mansour R. Ultrasonographic diagnosis of de Quervain’s tenosynovitis. Ann Rheum Dis. 2002;61(11):1034–1035. doi: 10.1136/ard.61.11.1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Dawson C, Mudgal CS. Staged description of the Finkelstein test. J Hand Surg Am. 2010;35(9):1513–1515. doi: 10.1016/j.jhsa.2010.05.022. [DOI] [PubMed] [Google Scholar]
- 55.FINKELSTEIN H. Stenosing Tendovaginitis at the radial styloid process. J Bone Jt Surg. 1930;12(3):509–540. [Google Scholar]
- 56.Chang CY, Kheterpal AB, Vicentini JRT, Huang AJ. Variations of anatomy on MRI of the first extensor compartment of the wrist and association with DeQuervain tenosynovitis. Skelet Radiol. 2017;46(8):1047–1056. doi: 10.1007/s00256-017-2639-0. [DOI] [PubMed] [Google Scholar]
- 57.•• Kutsikovich J, Merrell G. Accuracy of injection into the first dorsal compartment: a cadaveric ultrasound study. J Hand Surg Am. 2018. 10.1016/j.jhsa.2018.01.020. This article described the compartmentalization of the first dorsal compartment. If an injection or surgery neglects to address all compartments, the intervention may fail. [DOI] [PubMed]
- 58.Weiss A-PC, Akelman E, Tabatabai M. Treatment of de Quervain’s disease. J Hand Surg Am. 1994;19(4):595–598. doi: 10.1016/0363-5023(94)90262-3. [DOI] [PubMed] [Google Scholar]
- 59.Scheller A, Schuh R, Hönle W, Schuh A. Long-term results of surgical release of de Quervain’s stenosing tenosynovitis. Int Orthop. 2009;33(5):1301–1303. doi: 10.1007/s00264-008-0667-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Grundberg AB, Reagan DS. Pathologic anatomy of the forearm: intersection syndrome. J Hand Surg Am. 1985;10(2):299–302. doi: 10.1016/S0363-5023(85)80129-5. [DOI] [PubMed] [Google Scholar]
- 61.Draghi F, Bortolotto C. Intersection syndrome: ultrasound imaging. Skelet Radiol. 2014;43(3):283–287. doi: 10.1007/s00256-013-1786-1. [DOI] [PubMed] [Google Scholar]
- 62.Kohyama S, Kanamori A, Tanaka T, Hara Y, Yamazaki M. Stress fracture of the scaphoid in an elite junior tennis player: a case report and review of the literature. J Med Case Rep. 2016;10(1):8. doi: 10.1186/s13256-015-0785-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Bond CD, Shin AY, McBride MT, Dao KD. Percutaneous screw fixation or cast immobilization for nondisplaced scaphoid fractures. J Bone Joint Surg Am 2001;83-A(4):483–488. http://www.ncbi.nlm.nih.gov/pubmed/11315775. Accessed 7 Oct 2018. [DOI] [PubMed]
- 64.Inoue G, Shionoya K. Herbert screw fixation by limited access for acute fractures of the scaphoid. J Bone Joint Surg Br. 1997;79(3):418–421. doi: 10.1302/0301-620X.79B3.7254. [DOI] [PubMed] [Google Scholar]
- 65.Balius R, Pedret C, Estruch A, Hernández G, Ruiz-Cotorro Á, Mota J. Stress fractures of the metacarpal bones in adolescent tennis players. Am J Sports Med. 2010;38(6):1215–1220. doi: 10.1177/0363546509358322. [DOI] [PubMed] [Google Scholar]