Abstract
Background
Care coordination is crucial to avoid potential risks of care fragmentation in people with complex care needs. While there are many empirical and conceptual approaches to measuring and improving care coordination, use of theory is limited by its complexity and the wide variability of available frameworks. We systematically identified and categorized existing care coordination theoretical frameworks in new ways to make the theory-to-practice link more accessible.
Methods
To identify relevant frameworks, we searched MEDLINE®, Cochrane, CINAHL, PsycINFO, and SocINDEX from 2010 to May 2018, and various other nonbibliographic sources. We summarized framework characteristics and organized them using categories from the Sustainable intEgrated chronic care modeLs for multi-morbidity: delivery, FInancing, and performancE (SELFIE) framework. Based on expert input, we then categorized available frameworks on consideration of whether they addressed contextual factors, what locus they addressed, and their design elements. We used predefined criteria for study selection and data abstraction.
Results
Among 4389 citations, we identified 37 widely diverse frameworks, including 16 recent frameworks unidentified by previous reviews. Few led to development of measures (39%) or initiatives (6%). We identified 5 that are most relevant to primary care. The 2018 framework by Weaver et al., describing relationships between a wide range of primary care-specific domains, may be the most useful to those investigating the effectiveness of primary care coordination approaches. We also identified 3 frameworks focused on locus and design features of implementation that could prove especially useful to those responsible for implementing care coordination.
Discussion
This review identified the most comprehensive frameworks and their main emphases for several general practice-relevant applications. Greater application of these frameworks in the design and evaluation of coordination approaches may increase their consistent implementation and measurement. Future research should emphasize implementation-focused frameworks that better identify factors and mechanisms through which an initiative achieves impact.
KEY WORDS: care coordination, integrated care, theoretical model, theoretical framework
BACKGROUND
Clinical care of complex patients often requires input from multiple providers from a variety of clinical disciplines and social services.1, 2 Lack of deliberate organization, cooperation, and information-sharing among patients and providers can lead to fragmented care, which can jeopardize the effectiveness, safety, and efficiency of health care delivery.2, 3 Improving care coordination for clinically complex patients could potentially improve their health care quality. A wide range of complex multicomponent care coordination initiatives have been developed, which often feature forms of case management and enhanced multidisciplinary team work.4 However, the results of their effect on clinically relevant patient outcomes have been mixed.4 Some experts have suggested that the suboptimal outcomes of some care coordination initiatives may be because they were not developed with grounding in theoretical frameworks that outline the broad range of factors that may influence care coordination, their mechanisms, and how to know if care coordination is working.
Many theoretical frameworks exist to provide guidance in improving, implementing, and evaluating care coordination. However, framework use is currently limited by complexity and wide variability in their focus.5 Theoretical frameworks provide valuable resources necessary to better understand effective care coordination pathways.6 Theoretical coordination initiatives risk potential wasted resources and insufficient care coordination process changes.3
Previous reviews of care coordination theoretical frameworks have detailed key coordination concepts and elements.5 However, they provide insufficient information to enable users to understand their focus and to identify which frameworks are most relevant in different settings. As a result, potential users are faced with a dizzying array of options without clear guidance on how to advance their aims. To select the most relevant frameworks, helpful information may include knowing whether a framework addresses contextual factors (i.e., external, immutable), an initiative’s locus (e.g., setting, level, purpose), or elements of its design (e.g., personal, relationship-oriented, technical means of coordination). Contextual factors may impact the adoption, implementation, and effectiveness of an initiative, and as such deserve consideration by program developers, implementers, or managers when designing, leading, or evaluating an initiative. Questions about locus, including an initiative’s intended purpose, setting, and scope, may arise when choosing among opportunities to enhance coordination or ensuring an initiative is sufficiently comprehensive. Key for implementation and scale is an understanding of an initiative’s design through the strategies employed and mechanisms of action, as well as relationships to health outcomes. Prior reviews have compared coordination frameworks, but have not been designed explicitly to achieve these utilitarian objectives. We extend previous reviews by systematically reviewing the literature to identify new care coordination theoretical frameworks published since 2010, to categorize their key components, approaches, and impact (i.e., led to development of measures or initiatives), and to compare frameworks in new ways.
METHODS
Overview of Review Process
We conducted this review in two steps: (1) we performed a rapid evidence review to provide an initial overview of frameworks’ key components and (2) we incorporated input from subject matter experts (including researchers who have developed frameworks and surveys for care coordination and integration and researchers and clinicians who have used them in designing, implementing, synthesizing, and evaluating care coordination initiatives) through telephone discussions to complete a more detailed analysis of frameworks’ key components and purposes. We report the methodological steps taken in the rapid evidence review step according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses for Scoping Reviews (PRISMA-ScR) guidelines.7
We conducted the initial rapid review8 in response to an urgent request by a US Department of Veterans Affairs’ Health Services Research & Development (HSR&D) Care Coordination State-Of-The-Art (SOTA) planning committee for use in informing a national conference (March 2018). Although guided by current standard Agency for Healthcare Research & Quality (AHRQ) systematic review methods,9 in order to meet a condensed timeframe of 3 months, we streamlined our process in two ways—both consistent with current rapid review standards10: (1) we limited our search to articles published subsequent to 2010, which was the end date covered by the most recent systematic review5; and (2) to minimize bias and error in all stages of the review, we used second-reviewer checking (i.e., “sequential review”) instead of independent dual review processes. For the second step, between May and August of 2018, we facilitated biweekly semi-structured telephone discussions among a smaller group of subject matter experts (MC, SSG, DH, KM, SS, EY) to increase the usefulness of our review in identifying which coordination frameworks are most relevant to clinical care. We shared written call summaries with the group to ensure consensus on our approach to distinguishing among framework components.
Search and Framework Selection
To identify frameworks, we searched MEDLINE®, Cochrane, CINAHL, PsycINFO, and SocINDEX from 2010 to May 2018, using terms for care coordination (e.g., coordinated care, integrated care, theory, framework, model, concept). Databases and search terms were selected based on use in previous reviews of this topic11, 12 (see our report8 for full search strategy). To identify additional frameworks, we also searched numerous other sources, including hand-searching reference lists and relevant journals, and queried experts selected to participate in the VA State-Of-The-Art Conference on Care Coordination. We used prespecified eligibility criteria developed in consultation with experts for study selection and data abstraction. We included frameworks referring explicitly to care coordination or related terms such as integration, which were developed with a purpose related to guiding or evaluating care coordination research or practice in adults. We limited the search to English-language articles involving human subjects.
Framework Assessment
For our initial categorization, we extracted data on several key characteristics and impacts,8 including their theoretical underpinnings (e.g., none specified, organizational design theory), how care coordination was defined, objective, key components, setting, target population, and impact in terms of bibliometrics (i.e., numbers of forward citations), and whether the framework had led to development of initiatives or measurement tools.
In the second phase, we further assessed the extent to which a framework addressed each of the widely applied six World Health Organization (WHO) health system components (i.e., service delivery, leadership and governance, workforce, financing, technologies and medical products, information and research), micro (care team), meso (organizational infrastructure and resources), and macro levels (regulatory, market, and policy environment), and whether individuals and their environments were at the center.
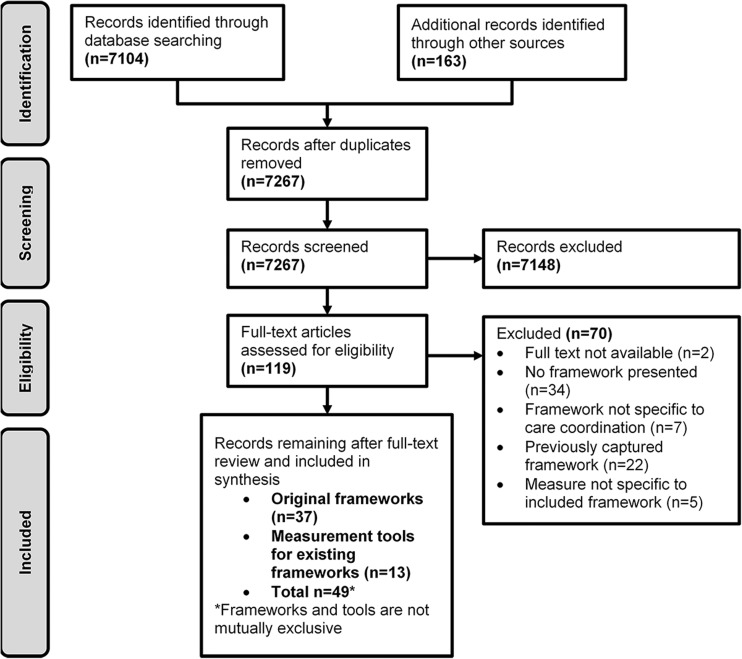
Finally, to distill the frameworks to facilitate use in policy and practice, we summarized all the characteristics under three domains focused on a framework’s purpose as recommended by experts (see Table 1). These three expert-created purpose domains include contextual factors, an initiative’s locus, and its design elements. Second-reviewer checking was used for full-text review and data abstraction (Fig. 1). A third reviewer resolved disagreements.8 As no standardized tool exists for assessing the validity of theoretical frameworks, we did not assess the risk of bias of individual studies or across studies.
Table 1.
Definitions of Expert-Developed Domains
| Domain | Definition | Relevance |
|---|---|---|
| Context | ||
| Context | Myriad of environmental conditions that may promote or detract from clinicians’ ability to coordinate care. Also called “outer context” in implementation studies. Changing these factors is typically out of the control of those trying to coordinate care | Can impact adoption, implementation, and effectiveness of an initiative and are most relevant to designing or evaluating an initiative |
| Locus | ||
| Setting |
Distinctions among where the coordination is taking place (e.g., primary care-specialist, primary care-hospital, primary care-family). Can be between or within and/or physical or organizational aspects |
Related questions may arise when choosing among opportunities to enhance coordination or ensuring an initiative is sufficiently comprehensive |
| Level | Distinction among the level in the system at which the coordination is taking place: micro, meso, macro; clinic, physician organization, health system; interpersonal, group, organization | |
| Purpose | Coordinating with what intent: addresses why it’s a goal; Highlights different goals; Addresses need for problem statement; Makes distinctions between potential purposes | |
| Design | ||
| Mechanisms | Emphasis on means of coordination (e.g., personal and relationship-oriented mechanisms versus technical/feedback-oriented mechanisms). | Reflecting on an initiative’s design can be key for implementation and scale to understand the strategies employed and the mechanisms through which it achieves its results. |
| Types of initiatives/situations | Emphasis on aspects of coordination (e.g., structural, functional, normative, interpersonal, and clinical). | |
Figure 1.
Literature flow chart
Our synthesis included quantitative analysis of the frequencies of key characteristics, as well as qualitative synthesis of similarities and differences among frameworks. We organized our discussion of frameworks based on their focus, including which frameworks addressed primary care, teams, measurement, implementation, and quality improvement/management. Within these categories, we generally highlighted the most comprehensive frameworks based on the number of components and the number of expert-created purpose domains they addressed. Although the goal of our original project was to broadly distinguish care coordination frameworks, regardless of the setting (e.g., primary care, intensive care), for this article, we additionally highlight the frameworks most relevant to primary care. Our original report provides additional details on all the theoretical frameworks that were reviewed.8
RESULTS
Overview of Characteristics and Components
Among 7267 citations, we identified 37 original frameworks, including 16 recent frameworks unidentified by previous reviews. Frameworks reflected a wide range of conceptual and structural diversity (Table 3). Among the 33 frameworks for which we had full texts, 54.5% were developed in the USA, 63.6% addressed overall health versus a specific disease (e.g., communicable disease) or setting (e.g., hospice, palliative care, intensive care), and 33.3% were considered patient-centered (i.e., explicitly naming patients/individuals as a key component that was placed at the center of the framework). Only one-third of frameworks explicitly identified a formal definition for care coordination or integration, with the McDonald et al. AHRQ definition as the most frequently cited.11 General theoretical bases for care coordination-specific frameworks were highly variable, with organizational design theory,58 which describes organization structure, as the most commonly cited (24.2%). The process used to select components for frameworks ranged from being unclear in the majority of frameworks to being based on formal literature review plus key informant discussions in a quarter of the cases. Frameworks most commonly emphasized means of coordination (e.g., personal and relationship-oriented mechanisms) (38%, Table 2) and most commonly (97%) included service delivery concepts, such as organizational and structural integration, person-centering (Table 3).
Table 3.
Characteristics of Included Care Coordination Models and Frameworks
| Characteristic | Number of frameworks (%)* |
|---|---|
| Developed in the USA | 18 (54.5)3, 11, 13, 16, 20, 22, 23, 25, 28, 30, 32, 35, 36, 40–44 |
| Based on VA data or done by VA researchers | 3 (9.1)3, 16, 40 |
| Person-centered frameworks (explicitly have “Person” or “Individual” at the center of the framework) | 11 (33.3)1, 14, 17, 21, 25, 26, 30, 32, 35, 39, 40 |
| Narrow focus (specific disease or setting, etc.) | 12 (36.4)14, 16, 17, 25, 28, 30, 32–34, 37, 39, 41 |
| Frameworks that have led to measures | 13 (39.4)19, 36, 46–56 |
| Frameworks with validated measures | 11 (33.3)11, 14, 19, 22, 25, 27, 30, 35, 39–41 |
| Frameworks that have led to initiatives† | 2 (6.1)29, 30 |
| Frameworks focused on organizing and/or evaluating measure | 3 (9.1)11, 15, 38 |
| Addressed concepts at care team level | 29 (87.9)1, 3, 5, 11, 13–17, 21–37, 39–41, 45 |
| Addressed concepts at organizational level | 30 (90.9)1, 3, 5, 11, 13–24, 26–30, 32–36, 38–41, 45 |
| Addressed concepts at regulatory and market level | 14 (42.4)1, 5, 13, 15, 17, 27, 29, 31, 34–37, 39, 41 |
| Addressed concepts at all 3 levels | 12 (36.4)1, 5, 13, 15, 17, 27, 29, 31, 34–36, 39, 41 |
| Addressed concepts of service delivery‡ | 32 (97.0)1, 3, 5, 11, 13–15, 17–41 |
| Addressed concepts of leadership and governance‡ | 22 (66.7)1, 3, 5, 15–19, 21–23, 27, 29, 31–36, 38–40 |
| Addressed concepts of workforce‡ | 24 (72.7)1, 3, 5, 11, 15–19, 21, 22, 24, 26–31, 33, 35–37, 39, 40 |
| Addressed concepts of financing‡ | 8 (24.3)1, 5, 14, 17–19, 34, 35 |
| Addressed concepts of technologies and medical products‡ | 9 (27.3)1, 5, 14, 21, 26–28, 31 |
| Addressed concepts of information and research‡ | 10 (30.3)1, 25, 26, 28, 34–36, 38, 40, 41 |
| Addressed ≥ 4/6 SELFIE domains‡ | 14 (42.4)1, 5, 17–19, 21, 26–28, 31, 34–36, 40 |
| Addressed all 6 SELFIE domains‡ | 1 (3.0)1 |
| Addressed ≥ 10/18 SELFIE sub-domains | 3 (9.1)1, 34, 36 |
*Denominator does not include Alter 1993,42 Klein 2001,43 Nadler 1988,44 or Watzlawick 2000,45 as we were unable to locate full-text articles of these publications (n = 33 frameworks total)
†Only captures initiatives defined in the original framework publication. We did not do a systematic search for initiatives from each framework
‡Based of World Health Organization Key Components of a Well Functioning Health System57
Table 2.
Frameworks Mapped to Domains of Context, Locus, and Design
| Author, year Framework name |
Context | Locus | Design | |||
|---|---|---|---|---|---|---|
| Context | Setting | Level | Purpose | Mechanisms | Types of initiatives/situations | |
|
Andersen, 199513 Anderson Behavior Framework |
X | x | x | |||
|
Bainbridge, 201014 NS |
x | x | x | |||
|
Bautista, 201615 NS |
X | x | ||||
|
Benzer, 201516 NS |
X | X | X | |||
|
Billings, 201417 INTERLINKS |
x | x | ||||
|
Bradbury, 201418 Aqua’s Integrated Care Framework |
x | x | X | |||
|
Calciolari, 201619 NS |
X | x | ||||
|
Donabedian, 196620 Donabedian’s Quality Framework |
X | x | x | |||
|
Evans, 201621 CCIC Framework |
x | X | x | |||
|
Gittell, 200222 Relational Coordination Framework |
X | X | x | |||
|
Gittell, 200423 Multi-level Framework |
X | X | x | x | x | |
|
Hepworth, 201024 Team Focused and Clinical Content Framework |
x | x | x | |||
|
Hodgson, 201725 Conceptual Model for Coordination and Medical Mistakes |
x | |||||
|
Kates, 201226 Quality Improvement and Innovation Partnership Improvement Framework |
x | x | x | X | ||
|
Leijten, 20181 SELFIE Framework |
X | X | X | |||
|
Lemieux-Charles, 200627 Integrated Team Effectiveness Model |
x | X | x | x | ||
|
Malhotra, 200728 Cognitive Workflow Model |
x | X | ||||
|
McDonald, 201411 Care Coordination Measurement Framework |
x | X | x | X | ||
|
Minkman, 201229 DMIC |
x | X | ||||
|
Oliver, 201030 Integrative Model |
x | X | x | |||
|
Palmer, 201831 Multimorbidity Care Model |
X | |||||
|
Radwin, 201632 NS |
X | |||||
|
Reader, 200933 Framework of Team Performance |
x | x | x | X | ||
|
Shigayeva, 201034 NS |
x | X | x | x | x | |
|
Singer, 201135 Integrated Patient Care Model |
X | x | x | x | ||
|
Singer, 201836 Conceptual Model of Integration Types |
x | X | x | X | x | X |
|
Siouta, 201637 NS |
X | x | x | |||
|
Strandberg-Larsen, 200938 NS |
x | x | x | |||
|
Valentijn, 201339 RMIC |
X | X | ||||
|
Van Houdt, 20135 NS |
x | x | x | |||
|
Weaver, 20183 NS |
x | X | x | X | ||
|
Young, 199740 NS |
X | X | X | |||
|
Zlateva, 201541 PCMH CC |
X | x | ||||
Unable to locate the full text for the following articles: Alter 199342; Klein 200143; Nadler 198844; Watzlawick 200045
X = major focus; x = minor focus
NS none specified; CCIC Context for Capabilities for Integrating Care; SELFIE Sustainable Integrated Chronic Care Models for Multi-morbidity; Delivery, Financing, and Performance; DMIC Development Model for Integrated Care; RMIC Rainbow Model of Integrated Care; PCMH CC Patient Centered Medical Home Care Coordination Conceptual Model
Comprehensiveness of Frameworks
The SELFIE framework was the most comprehensive in terms of the number of care coordination concepts it included (N = 56; e.g., named coordinator, remote monitoring, shared information systems).1 Most frameworks contained 50% or fewer of the SELFIE components. By structuring a wide range of care coordination concepts from micro to macro levels, the SELFIE framework offers a nomenclature that can be used as a starting point to describe and compare initiatives.
The 2018 framework by Singer et al.36 uses the related term “integration” and most comprehensively addressed relationships among five types of integration: structural, functional, normative, interpersonal, and process integration. The three hypothetical relationships it proposes include the following: (1) contextual factors are precursors to organizational and social integration; (2) more versus less structural integration is associated with more functional integration and that these in turn are associated with more normative, interpersonal, and process integration; and (3) these five types of integration will impact outcomes. This framework can be used to distinguish the main emphasis of an initiative or identify which types of integration are most relevant in different circumstances.
Primary Care-Focus of Frameworks
Most relevant to US primary care were three frameworks3, 16, 41 derived from primary care settings. The framework by Weaver and colleagues3 is the most comprehensive, addressing context, locus, and design domains, as well as service delivery, leadership and governance, and workforce domains (see full report). Its main purpose was to examine the factors leading to improved patient outcomes by distinguishing relationships among coordination mechanisms, processes, integrating conditions, and outcomes across multi-team systems. The 2012 primary care-focused framework by Kates et al.26 from Canada has a similar objective of describing key elements of high-performing primary care and supports required to attain it.26 Benzer et al.’s 2015 framework provides insights into how to facilitate the integration of mental health and primary care.16
Coordination of Care with External Partners as Focus of Frameworks
Most relevant to health care organizations coordinating care with external partners are five frameworks (15%)1, 3, 22, 23, 39 that explicitly emphasized distinctions among coordination levels. The SELFIE framework provides a comprehensive framework of components across micro, meso, and macro levels.1 By contrast, Gittell’s Relational Coordination Framework,22 Gittell’s Multi-level Framework,23 and the framework by Weaver et al.3 provide details on mechanisms linking intra- and inter-organization coordination. The Rainbow Model of Integrated Care (RMIC) provides an overview of both the six WHO types of integration and how they interact with different levels of care (micro, meso, macro).39
Team-Focus of Frameworks, Without Regard to Setting
Three care coordination frameworks were team-focused.24, 27, 33 The frameworks were from Australia,24 Canada,27 and the UK.33 Among these, the most comprehensive was the Integrated Team Effectiveness Model (ITEM), which addressed context, locus (setting and purpose), and design (mechanisms) domains and included service delivery, leadership and governance, workforce, and technologies and medical products primarily at the meso level. The team performance framework from Reader et al. was unique in that it focused on the intensive care unit.33
Measurement-Focus of Frameworks
Four frameworks were self-described as measurement-focused.34–36, 41 Three are from the USA35, 36, 41 and one is from the UK.34 Among these, the 2018 framework by Singer et al.36 is the most recent and most comprehensive, encompassing all expert-defined domains and subdomains of context, locus, and design and 12 SELFIE components in service delivery, leadership and governance, workforce, financing, and information and research.36 The Singer 2018 framework provides clear definitions of five different types of integration (i.e., structural, functional, normative, interpersonal, and process), describe how they interrelate, and propose how to measure them. Among other measurement-focused frameworks, Shigayeva et al.’s was the second most comprehensive, describing examples of four general levels of increasing integration based on TB and HIV/AIDS program integration.34 Other measurement-focused frameworks include Singer et al., which describes ideal targets for each of five coordination dimensions and two of patient-centeredness.35 Zlateva et al. suggest short-term and long-term outcomes specific to five care coordination domains essential to the Patient Centered Medical Home (PCMH).41
Measurement Tools or Initiatives Deriving from Frameworks
Minkman’s Development Model for Integrated Care (DMIC) is the only framework we identified that has both led to the development of a partially validated survey (face and construct validity) and formation of multidisciplinary teams incorporating the DMIC into stroke, acute myocardial infarction (AMI), or dementia care.29 Otherwise, we identified measures or tools stemming from 39% of the included frameworks.19, 36, 46–56 Most were surveys of health care providers, and most had some to extensive levels of validation. Other frameworks that showed potential for measure development or field use include several with qualitative assessments of a framework concept21, 23, 24, 29 and that hinted at future measures.1, 3, 31, 32, 36 Oliver’s Integrative Model is the only other framework that we identified that has explicitly led to development of an initiative, which involved incorporating telemedicine for hospice patients and caregivers.30
Several previous reviews have provided frameworks for summarizing care coordination measures.8, 15, 30 These reviews identified improvement in measurement quality as a future research need.11, 15, 38 The McDonald 2014 AHRQ Measures Atlas increased access to existing care coordination measures aligned with theoretical frameworks and noted that professional and system perspectives are missing in existing measures.11
Implementation-Focus of Frameworks
Only three frameworks described implementation strategies for settings in Australia,24 Canada,26 and the UK.18 Of these, the Kates et al. and Bradbury frameworks are the most comprehensive.18, 26 Kates et al. are unique in proposing an implementation strategy that includes incorporation of a quality improvement “coach,” an effective spread strategy, and description of system-level enablers. Bradbury is unique in describing their actual experiences translating theory into practice.18
Quality Improvement or Management Focus of Frameworks
Three frameworks focused on quality improvement/quality management and highlighted conditions thought to be associated with effective integration.21, 26, 29 All three address design concepts and variably address context and locus domains. The frameworks share several similar components, such as patient engagement, innovation, measurement and improvement, and partnerships. Among these, Minkman’s Development Model for Integrated Care (DMIC) is the most comprehensive, containing the greatest number of components.29
Focus of Frameworks on Care Coordination in Specialty Settings
Several frameworks focused on coordination in specialty settings,22, 23, 28, 30, 32, 37 such as how to integrate family involvement into hospice interdisciplinary team meetings,30 describing cognitive workflow in critical care,28 consideration of patient’s need for coordination based on interdisciplinarity, biological susceptibility, and procedural intensity,25 examples of best practices for care coordination approaches mapped to clinical, educational, and administrative work activities in surgery,40 and providing an understanding of elements of PCMH coordination initiatives.41 Although some situational factors addressed in these frameworks are unique to the specialty setting, such as the specific clinical workflow to manage an emergency in an intensive care unit, they demonstrate and reinforce the many mechanisms and mediation concepts that are common to all frameworks, such as trust, accountability, and communication.
DISCUSSION
This scoping review advanced previous work by making the theory-to-practice link more accessible. We did this by systematically classifying a large number of existing theoretical frameworks pertaining to care coordination in four ways: (1) comprehensiveness in terms of the number types of concepts they address (e.g., coordinators, remote monitoring); (2) the types of relationships they address (e.g., context, locus, design); (3) their intended use; and (4) their impact. Our intent was to enable users—including general internists and administrators—to more easily identify and select frameworks based on their needs and potential applications. To further support use of applicable care coordination theory, in a companion Perspectives article, subject matter experts lay out an approach for health care providers, researchers, and other stakeholders to apply relevant care coordination theory to four use cases.
Among the 37 care coordination theoretical frameworks we identified, few have led to development of measures (39%) or initiatives (6%). Although not all were intended to support measurement or initiative development, underuse of those that were may limit implementation of effective coordination approaches and their consistent measurement. The majority of frameworks identified the means of coordination as a major focus. This highlights their importance in implementing care coordination processes and the need to consider and understand their mediators and moderators. For example, a unique contribution of the primary care-based framework by Weaver et al.3 was its identification of accountability, predictability, common understanding, and trust as potentially important mediators that may limit or enhance coordinator processes.
We also identified three implementation-focused frameworks that could prove especially useful to those seeking to implement care coordination initiatives.18, 24, 26 As these frameworks describe underlying mechanisms of action, they may help implementers act according to an initiative’s intent. For care coordination implementers, designing an initiative or evaluating its impact, these three implementation-focused frameworks18, 24, 26 could identify factors that may influence the success or failure of an initiative.
The 16 frameworks highlighting care coordination design features could also help those implementing to develop more comprehensive initiatives through expanding their knowledge of the diverse range of available care coordination types and mechanisms ({Leijten, 2018 #7001}{Owens, 2010 #8548}{Agency for Healthcare Research and Quality, 2014 #3}{Tushman, 1978 #8545}{Shigayeva, 2010 #5959}{Kates, 2012 #1807}{Andersen, 1995 #6992}{Calciolari, 2016 #2918}{Gittell, 2004 #6996}{Singer, 2011 #2156}{Valentijn, 2013 #6094}{Young, 1997 #8346}{Bradbury, 2014 #4635}{Evans, 2016 #6068}{Malhotra, 2007 #6988}{Minkman, 2012 #6978}). These frameworks can also assist in the evaluation of initiatives. Qualitative or mixed methods investigations could add understanding to existing mechanisms. Quantitative investigations could rely on relevant theory and supportive evidence so as to avoid making ineffective changes in care coordination processes3 that lead to wasted resources.
We identified Minkman’s DMIC29 as the only framework which has led to both the development of a partially validated survey and an initiative. Thus, the DMIC may be considered an example for how to apply a relevant theory in developing and measuring and initiative. However, the DMIC had a relatively narrow disease focus—on care coordination mechanisms within stroke, acute myocardial infarction (AMI), and dementia settings in the Netherlands. Therefore, for guidance on how to measure a broader range of care coordination concepts, users may consider the measurement-focused framework by Singer et al. that comprehensively addresses all context, locus, and design domains and 12 SELFIE components in “Service Delivery,” “Leadership and Governance,” “Workforce,” “Financing,” and “Information and Research.”36
Potential limitations of our review methods include our literature search parameters and approach, sequential review process, and domain formation. For our literature search, limiting to English-language studies, coupled with the inconsistent terminology used in the literature on care coordination theoretical frameworks, may have increased our risk of missing relevant studies. We addressed this challenge by including a wide variety of terminology in our search strategy, as well as consulting with experts. Second, although sequential dual review is a widely used method, its comparison to independent dual review has not yet been empirically studied and may have increased the risk of error and bias. Third, as our process of developing the domains of context, locus, and design domains was somewhat informal (based on expert deliberations), it must be considered preliminary. Further development using more formalized processes may lead to domain refinement which could impact assessment of major focus, primary care relevance, and comprehensiveness. There are likely various ways of separating frameworks depending on the users’ needs. For example, separation by motivation—policy/government/regional versus operational/delivery system versus a mix—could be relevant in certain circumstances. Finally, as this review was not designed to identify all available measures—only those associated with frameworks—future research is needed to identify other measures that may exist in general and that provide system representation perspectives.
One of the main gaps in the care coordination frameworks reviewed herein was the limited guidance offered on comprehensive program implementation. We identified implementation-specific frameworks for use to guide implementation of initiatives from a locus and design perspective. None have incorporated contextual factors, which may be key in coordinating with external partners, and none were from US settings. Few of the frameworks identified in this review have led to development of initiatives for improving care coordination or have led to the development of measures that evaluate system representation perspective. These gaps were also identified, with a research agenda proposed for the VA, in several papers from a recent Special Issue on the Coordination of Chronic Care.6, 59–61
CONCLUSION
This review advanced previous reviews by comparing theoretical frameworks for care coordination in practical ways to increase their use. By distilling the care coordination theoretical frameworks into three expert-developed domains of context, locus, and design, we made theories more accessible to primary care settings in particular. Future research on care coordination frameworks should provide more guidance on how to implement care coordination in health systems and better maximize the use of existing frameworks for developing initiatives.
Acknowledgements
We would like to thank Julia Haskin, MA, for editorial support.
Funding
This material is based upon work supported by the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, Quality Enhancement Research Initiative (QUERI), Evidence-Based Synthesis Program (ESP). Dr. Yano’s time was supported by a VA HSR&D Senior Research Career Scientist Award (project no. RCS 05-195).
Compliance with Ethical Standards
Conflict of Interest
KP, JA, DB, DH, SSG, KM, SS, and BY declare no conflicts of interest. MC wishes to disclose a VA HSR&D IIR 12-346 Patient Experienced Integrated Care for Veterans with Multiple Chronic Conditions grant that ended 9/30/17 as a potential conflict of interest.
Disclaimer
The views expressed in this article are those of the authors and do not necessarily represent the position or policy of the Department of Veterans Affairs or the United States government.
Footnotes
Prior presentations: None
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Leijten FRM, Struckmann V, van Ginneken E, et al. The SELFIE framework for integrated care for multi-morbidity: Development and description. Health Policy. 2018;122(1):12–22. doi: 10.1016/j.healthpol.2017.06.002. [DOI] [PubMed] [Google Scholar]
- 2.Owens M. Medicine I of MR on E-B. Costs of uncoordinated care. In: Yong PL, Saunders RS, Olsen LA, editors. The Healthcare Imperative: Lowering Costs and Improving Outcomes: Workshop Series Summary. Washington (DC): National Academies Press (US); 2010. pp. 131–140. [PubMed] [Google Scholar]
- 3.Weaver SJ, Che XX, Petersen LA, Hysong SJ. Unpacking care coordination through a multiteam system lens: a conceptual framework and systematic review. Med Care. 2018;56(3):247–259. doi: 10.1097/MLR.0000000000000874. [DOI] [PubMed] [Google Scholar]
- 4.Smith SM, Soubhi H, Fortin M, Hudon C, O'Dowd T. Managing patients with multimorbidity: systematic review of interventions in primary care and community settings. BMJ 2012;345:e5205. [DOI] [PMC free article] [PubMed]
- 5.Van Houdt S, Heyrman J, Vanhaecht K, Sermeus W, De Lepeleire J. An in-depth analysis of theoretical frameworks for the study of care coordination. Int J Integr Care. 2013;13:e024–e024. doi: 10.5334/ijic.1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sheinfeld Gorin S, Haggstrom D. The coordination of chronic care: an introduction. Transl Behav Med 2018;8(3):313-317.
- 7.Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 8.Peterson K, Anderson J, Bourne D, Boundy E. Scoping Brief: Care Coordination Theoretical Models and Frameworks. 2018;VA ESP Project #09–199. [PubMed]
- 9.Agency for Healthcare Research and Quality. Methods Guide for Effectiveness and Comparative Effectiveness Reviews. AHRQ Publication No. 10(14)-EHC063-EF. Rockville, MD. 2014. [PubMed]
- 10.Tricco A, Langlois E, Straus S, editors. Rapid reviews to strengthen health policy and systems: a practical guide. Geneva: World Health Organization; 2017. [Google Scholar]
- 11.McDonald KM, Schultz E, Albin L, et al. Care Coordination Atlas Version 4 (Prepared by Stanford University under subcontract to American Institutes for Research on Contract No. HHSA290-2010-00005I). AHRQ Publication No. 14-0037- EF. Rockville, MD. 2014.
- 12.McDonald KM, Sundaram V, Bravata DM, Lewis R, Lin N, Kraft S, McKinnon M, Paguntalan H, Owens DK. Care Coordination. Vol 7 of: Shojania KG, McDonald KM, Wachter RM, Owens DK, editors. Closing the Quality Gap: A Critical Analysis of Quality Improvement Strategies. Technical Review 9 (Prepared by the Stanford University-UCSF Evidence-based Practice Center under contract 290-02-0017). AHRQ Publication No. 04(07)-0051-7. Rockville, MD. 2007.
- 13.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36(1):1–10. doi: 10.2307/2137284. [DOI] [PubMed] [Google Scholar]
- 14.Bainbridge D, Brazil K, Krueger P, Ploeg J, Taniguchi A. A proposed systems approach to the evaluation of integrated palliative care. BMC Palliat Care. 2010;9(1):8. doi: 10.1186/1472-684X-9-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bautista MAC, Nurjono M, Lim YW, Dessers E, Vrijhoef HJ. Instruments measuring integrated care: a systematic review of measurement properties. Milbank Q. 2016;94(4):862–917. doi: 10.1111/1468-0009.12233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Benzer JK, Cramer IE, Burgess JF, Mohr DC, Sullivan JL, Charns MP. How personal and standardized coordination impact implementation of integrated care. BMC Health Serv Res 2015;15(1). [DOI] [PMC free article] [PubMed]
- 17.Billings J, Leichsenring K. Methodological development of the interactive INTERLINKS Framework for Long-term Care. Int J Integr Care. 2014;14:e021. doi: 10.5334/ijic.1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bradbury E. Integrated care communities: putting change theory into practice. J Integr Care. 2014;22(4):132–141. doi: 10.1108/JICA-06-2014-0022. [DOI] [Google Scholar]
- 19.Calciolari S, Ilinca S. Unraveling care integration: Assessing its dimensions and antecedents in the Italian health system. Health Policy. 2016;120(1):129–138. doi: 10.1016/j.healthpol.2015.12.002. [DOI] [PubMed] [Google Scholar]
- 20.Donabedian A. Evaluating the quality of medical care. Milbank Mem Fund Q. 1966;44(3, Suppl):166–206. doi: 10.2307/3348969. [DOI] [PubMed] [Google Scholar]
- 21.Evans JM, Grudniewicz A, Baker GR, Wodchis WP. Organizational Context and Capabilities for Integrating Care: A framework for improvement. Int J Integr Care. 2016;16(3):15. doi: 10.5334/ijic.2416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gittell J. Coordinating mechanisms in care provider groups: Relational coordination as a mediator and input uncertainty as a moderator of performance effects. Manag Sci. 2002;48(11):1408–1426. doi: 10.1287/mnsc.48.11.1408.268. [DOI] [Google Scholar]
- 23.Gittell JH, Weiss L. Coordination networks within and across organizations: A multi-level Framework. J Manag Stud. 2004;41(1):127–153. doi: 10.1111/j.1467-6486.2004.00424.x. [DOI] [Google Scholar]
- 24.Hepworth J, Marley JE. Healthcare teams - a practical framework for integration. Aust Fam Physician. 2010;39(12):969–971. [PubMed] [Google Scholar]
- 25.Hodgson A, Etzkorn L, Everhart A, Nooney N, Bestrashniy J. Exploring the validity of developing an interdisciplinarity score of a patient's needs: care coordination, patient complexity, and patient safety indicators. J Healthc Qual. 2017;39(2):107–121. doi: 10.1097/JHQ.0000000000000062. [DOI] [PubMed] [Google Scholar]
- 26.Kates N, Hutchison B, O'Brien P, Fraser B, Wheeler S, Chapman C. Framework for advancing improvement in primary care. Healthc Pap. 2012;12(2):8–21. doi: 10.12927/hcpap.2012.22978. [DOI] [PubMed] [Google Scholar]
- 27.Lemieux-Charles L, McGuire WL. What do we know about health care team effectiveness? A review of the literature. Med Care Res Rev. 2006;63(3):263–300. doi: 10.1177/1077558706287003. [DOI] [PubMed] [Google Scholar]
- 28.Malhotra S, Jordan D, Shortliffe E, Patel VL. Workflow modeling in critical care: piecing together your own puzzle. J Biomed Inform. 2007;40(2):81–92. doi: 10.1016/j.jbi.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 29.Minkman MM. Developing integrated care. Towards a development model for integrated care. Int J Integr Care 2012;12.
- 30.Oliver D, Demiris G, Wittenberg-Lyles E, Porock D. The use of videophones for patient and family participation in hospice interdisciplinary team meetings: a promising approach. Eur J Cancer Care. 2010;19(6):729–735. doi: 10.1111/j.1365-2354.2009.01142.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Palmer K, Marengoni A, Forjaz MJ, et al. Multimorbidity care model: recommendations from the consensus meeting of the Joint Action on Chronic Diseases and Promoting Healthy Ageing across the Life Cycle (JA-CHRODIS) Health Policy. 2018;122(1):4–11. doi: 10.1016/j.healthpol.2017.09.006. [DOI] [PubMed] [Google Scholar]
- 32.Radwin LE, Castonguay D, Keenan CB, Hermann C. An expanded theoretical framework of care coordination across transitions in care settings. J Nurs Care Qual. 2016;31(3):269–274. doi: 10.1097/NCQ.0000000000000165. [DOI] [PubMed] [Google Scholar]
- 33.Reader TW, Flin R, Mearns K, Cuthbertson BH. Developing a team performance framework for the intensive care unit. Crit Care Med. 2009;37(5):1787–1793. doi: 10.1097/CCM.0b013e31819f0451. [DOI] [PubMed] [Google Scholar]
- 34.Shigayeva A, Atun R, McKee M, Coker R. Health systems, communicable diseases and integration. Health Policy Plan. 2010;25(suppl_1):i4–i20. doi: 10.1093/heapol/czq060. [DOI] [PubMed] [Google Scholar]
- 35.Singer SJ, Burgers J, Friedberg M, Rosenthal MB, Leape L, Schneider E. Defining and measuring integrated patient care: promoting the next frontier in health care delivery. Med Care Res Rev. 2011;68(1):112–127. doi: 10.1177/1077558710371485. [DOI] [PubMed] [Google Scholar]
- 36.Singer SJ, Kerrissey M, Friedberg M, Phillips R. A comprehensive theory of integration. Med Care Res Rev. 2018:1077558718767000. [DOI] [PubMed]
- 37.Siouta N, Van Beek K, Van der Eerden ME, et al. Integrated palliative care in Europe: a qualitative systematic literature review of empirically-tested models in cancer and chronic disease. BMC Palliat Care. 2016;15:56. doi: 10.1186/s12904-016-0130-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Strandberg-Larsen M, Krasnik A. Measurement of integrated healthcare delivery: a systematic review of methods and future research directions. Int J Integr Care 2009;9:e01. [DOI] [PMC free article] [PubMed]
- 39.Valentijn PP, Schepman SM, Opheij W, Bruijnzeels MA. Understanding integrated care: a comprehensive conceptual framework based on the integrative functions of primary care. Int J Integr Care. 2013;13:e010. doi: 10.5334/ijic.886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Young GJ, Charns MP, Daley J, Forbes MG, Henderson W, Khuri SF. Best practices for managing surgical services: the role of coordination. Health Care Manag Rev. 1997;22(4):72–81. doi: 10.1097/00004010-199710000-00010. [DOI] [PubMed] [Google Scholar]
- 41.Zlateva I, Anderson D, Coman E, Khatri K, Tian T, Fifield J. Development and validation of the Medical Home Care Coordination Survey for assessing care coordination in the primary care setting from the patient and provider perspectives. BMC Health Serv Res. 2015;15:226. doi: 10.1186/s12913-015-0893-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Alter C, Hage J. Organizations working together. Newbury Park: Sage Publications, Inc; 1993. [Google Scholar]
- 43.Klein G. Features of team coordination. In: McNeese M, Salas E, Endesley M, editors. New trends in cooperative activities: Understanding system dynamics in complex environments. Santa Monica: Human Factors & Ergonomics Society; 2001. pp. 68–95. [Google Scholar]
- 44.Nadler D, Tushman M. Strategic organization design: Concepts, tools & processes. Glenview: Scott Foresman & Co; 1988. [Google Scholar]
- 45.Watzlawick P, Beavin JH, Jackson DD. Menschliche Kommunikation: Formen, Störungen, Paradoxien. Huber; 2000.
- 46.Advancing Quality Alliance. System Integration Framework Assessment. 2014. Available from: https://www.aquanw.nhs.uk/resources/integration/integrated-caretoolkit/AQuA%20Framework%20Assessment.pdf.
- 47.Agency for Healthcare Research and Quality. Care Coordination Measure for Primary Care Survey. Prepared under Contract No. HHS290–2010-00005I. AHRQ Publication No. 16–0042-1-EF2016, Rockville: Agency for Healthcare Research and Quality.
- 48.Angus L, Valentijn PP. From micro to macro: assessing implementation of integrated care in Australia. Aust J Prim Health 2017. [DOI] [PubMed]
- 49.Bainbridge D, Brazil K, Krueger P, Ploeg J, Taniguchi A, Darnay J. Measuring horizontal integration among health care providers in the community: an examination of a collaborative process within a palliative care network. J Interprof Care. 2015;29(3):245–252. doi: 10.3109/13561820.2014.984019. [DOI] [PubMed] [Google Scholar]
- 50.Gittell JH, Fairfield KM, Bierbaum B, et al. Impact of relational coordination on quality of care, postoperative pain and functioning, and length of stay: a nine-hospital study of surgical patients. Med Care. 2000;38(8):807–819. doi: 10.1097/00005650-200008000-00005. [DOI] [PubMed] [Google Scholar]
- 51.Nurjono M, Valentijn PP, Bautista MA, Wei LY, Vrijhoef HJ. A prospective validation study of a rainbow model of integrated care measurement tool in Singapore. Int J Integr Care. 2016;16(1):1. doi: 10.5334/ijic.2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Oliver DP, Wittenberg-Lyles EM, Day M. Measuring interdisciplinary perceptions of collaboration on hospice teams. Am J Hosp Palliat Med. 2007;24(1):49–53. doi: 10.1177/1049909106295283. [DOI] [PubMed] [Google Scholar]
- 53.Singer SJ, Friedberg MW, Kiang MV, Dunn T, Kuhn DM. Development and preliminary validation of the Patient Perceptions of Integrated Care survey. Med Care Res Rev. 2013;70(2):143–164. doi: 10.1177/1077558712465654. [DOI] [PubMed] [Google Scholar]
- 54.Valentijn P, Angus L, Boesveld I, Nurjono M, Ruwaard D, Vrijhoef H. Validating the Rainbow Model of Integrated Care Measurement Tool: results from three pilot studies in the Netherlands, Singapore and Australia. Int J Integr Care 2017;17(3).
- 55.Van Dijk-de Vries AN, Duimel-Peeters IG, Muris JW, Wesseling GJ, Beusmans GH, Vrijhoef HJ. Effectiveness of teamwork in an integrated care setting for patients with copd: development and testing of a self-evaluation instrument for interprofessional teams. Int J Integr Care. 2016;16(1):9. doi: 10.5334/ijic.2454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Young GJ, Charns MP, Desai K, et al. Patterns of coordination and clinical outcomes: a study of surgical services. Health Serv Res. 1998;33(5 Pt 1):1211–1236. [PMC free article] [PubMed] [Google Scholar]
- 57.World Health Organization. Key components of a well functioning health system. 2010. Available from: https://www.who.int/healthsystems/EN_HSSkeycomponents.pdf?ua=1.
- 58.Tushman ML, Nadler DA. Information processing as an integrating concept in organizational design. Acad Manag Rev. 1978;3(3):613–624. [Google Scholar]
- 59.Kilbourne AM, Hynes D, O’Toole T, Atkins D. A research agenda for care coordination for chronic conditions: aligning implementation, technology, and policy strategies. Transl Behav Med. 2018;8(3):515–521. doi: 10.1093/tbm/ibx084. [DOI] [PubMed] [Google Scholar]
- 60.Weaver SJ, Jacobsen PB. Cancer care coordination: opportunities for healthcare delivery research. Transl Behav Med. 2018;8(3):503–508. doi: 10.1093/tbm/ibx079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Elwood WN, Huss K, Roof RA, et al. NIH research opportunities for the prevention and treatment for chronic conditions. Transl Behav Med. 2018;8(3):509–514. doi: 10.1093/tbm/ibx085. [DOI] [PMC free article] [PubMed] [Google Scholar]