Abstract
Background
Compulsory mental health hospital admissions are increasing in several European countries but are coercive and potentially distressing. It is important to identify which mental health service models and interventions are effective in reducing compulsory admissions.
Methods
We conducted a rapid evidence synthesis to explore whether there is any evidence for an effect on compulsory admissions for 15 types of psychosocial intervention, identified by an expert group as potentially relevant to reducing compulsory admission. A search for randomised controlled trials (RCTs) reporting compulsory admission as a primary or secondary outcome or adverse event was carried out using clinical guidelines, recent systematic reviews, and database searches postdating these reviews.
Findings
We found 949 RCTs reporting on the interventions of interest, of which 19 reported on compulsory admission. Our narrative synthesis found some evidence for the effectiveness of crisis planning and self-management, while evidence for early intervention services was mixed. We did not find evidence to support adherence therapy, care from crisis resolution teams and assertive community treatment, but numbers of relevant studies were very small. We found no trials which tested effects on compulsory admission of the nine other intervention types.
Interpretation
Crisis planning and self-management interventions with a relapse prevention element are most promising for preventing compulsory admissions. Given our broad search strategy, the lack of evidence demonstrates that there is an urgent need for more research on interventions which may reduce compulsory admissions.
Funding
Independent research commissioned and funded by the National Institute for Health Research Policy Research Programme.
Keywords: Compulsory admissions, Mental health act, Involuntary hospitalisations
Research in context
Evidence before this study
A previous systematic review and meta-analysis on interventions that may reduce compulsory admissions found very few effective interventions and little relevant literature overall, with evidence only supporting the effectiveness of crisis plans. We conducted a rapid evidence synthesis to update this review using a broader search strategy. A search for randomised controlled trials (RCTs) reporting compulsory admission as an outcome or adverse event was carried out for 15 types of psychosocial intervention (identified by an expert group as potentially relevant to reducing compulsory admission). Searches were performed using clinical guidelines, recent systematic reviews of each intervention type (search period from database inception to 9th July 2018), and searches for individual trials post-dating these reviews in MEDLINE, Embase, and the ISRCTN registry of clinical trials.
Added value of this study
The added value was in the breadth of our search, identifying trials where compulsory admission was a secondary outcome or adverse event, which may thus not have been included in previous reviews. In total we found 949 randomised controlled trials reporting on 15 types of psychosocial intervention, of which only 19 reported on compulsory admission. Our findings supported those of the previous systematic review, providing evidence for the effectiveness of crisis planning and self-management while some, but not all, trials showed a significant effect for early intervention in psychosis. For most other models examined, evidence was negative or very limited.
Implications of all the available evidence
Improving access to crisis planning and self-management interventions and successfully implementing them within practice should be a priority for policy makers and service planners. However, the inconclusive findings on the effectiveness of most other interventions for reducing compulsory admissions, even with inclusion of secondary as well as primary outcomes, indicates a pressing need for more research. All trials of potentially relevant interventions should pre-register compulsory admissions as an outcome, report compulsory admission data even if not the primary outcome, and consider compulsory admissions when performing power calculations. Avoiding compulsory admission is a high priority for both service users and policy makers, yet researchers have so far accumulated very little evidence on which to act.
Alt-text: Unlabelled Box
1. Background
Compulsory admissions are admissions to a hospital or mental health facility without an individual's consent and according to local judicial procedures [1]. Grounds for compulsory admission vary between countries, but often include an identified need for treatment to which people are unable or unwilling to consent, and which cannot safely and effectively be delivered in the community. Compulsory admissions are increasing in many European countries [2], [3], [4], [5]. In England, for example, the rate of compulsory admissions has increased nearly fourfold from 1984 to 2016 [6].
Identifying interventions that reduce compulsory admissions is a priority for a number of reasons. While they can reduce short-term risks, and about half of patients subsequently agree with the decision [7], compulsory admission is coercive by definition. It can be traumatic for patients and their relatives and carers [8], may undermine an individual's dignity, and conflicts with shared decision making and autonomous approaches to psychiatric care [9], [10], [11], [12].
Additionally, the therapeutic value of compulsory admissions remains uncertain. Clinical benefits are hard to evaluate robustly owing to the absence of a valid comparison group. Some studies have drawn comparisons with voluntary patients, though they are limited by the clinical differences between these groups. Symptomatic improvement seems to be similar for voluntary and compulsorily admitted patients, but voluntary patients typically have better social outcomes [13], [14], [15].
It is therefore important to identify which mental health services and interventions are effective in reducing rates of compulsory admissions. A systematic review and meta-analysis on this topic found very few effective interventions and little relevant literature overall, with evidence only supporting the effectiveness of crisis plans [1]. However, the search completed for this review was conducted in April 2015 so requires updating. The search strategy also only included papers referring to compulsory admissions in the title or abstract so some papers reporting compulsory admissions as secondary outcomes or adverse events were likely missed. Moreover, it was limited to trials of adult psychiatric patients aged 18–65, although people of all ages may be compulsorily admitted. For example, in 2017–2018, 1177 children under 18 and 10,006 adults over 65 were detained under the Mental Health Act in England [16].
Our aim was therefore to conduct an updated search with wider scope for any evidence of an effect on compulsory admission, including studies of relevant interventions where compulsory admission has been examined as a secondary outcome or adverse event. We aimed to provide an overview of which interventions have shown any evidence of an effect on compulsory admissions, which interventions have so far been found to have little or no effect, and which have yet to be examined. As well as underpinning future research and intervention development, our work was conducted to inform the Independent Review of the Mental Health Act in England conducted in 2017–18 [17].
2. Methods
The protocol for this review was prospectively registered on PROSPERO (registration ID: CRD42018104006).
2.1. Inclusion Criteria
Inclusion criteria were developed using the PICOS (Participant, Intervention, Comparison, Outcome and Study design) framework [18]. Trials that included participants with a diagnosis of any mental health disorder, regardless of their age, were eligible for inclusion. This did not include RCTs of participants with primary diagnoses of intellectual disability or substance misuse.
A list was generated of 15 broad intervention types through iterative discussion with experts, including the Working Group for the Independent Review of the Mental Health Act in England and the management group for the National Institute for Health Research Mental Health Policy Research Unit. Experts included academics, clinicians, policy makers, researchers, and service users. Psychosocial interventions were included if these groups considered that there was a mechanism or mechanisms by which they might prevent compulsory admissions, or if experts were already aware of trials which reported compulsory admissions. See Table 1 for a brief description of each intervention type, and Supplementary Materials Appendix 2 for further details of the interventions used in the included trials. Where several names exist for the same or very similar interventions, these were grouped as follows: acute day units or day hospitals; adherence therapy or compliance therapy; advance statements or crisis plans; assertive community treatment or assertive outreach or intensive case management; cognitive behavioural therapy for psychosis (CBTp); community rehabilitation services; compulsory community treatment or community treatment orders or involuntary outpatient commitment; crisis houses; crisis intervention or crisis resolution teams; early intervention services for psychosis (EIS); family interventions for psychosis; housing interventions or supported housing or housing first interventions; Open Dialogue; self-management or relapse prevention interventions; vocational interventions or supported employment; individual placement and support.
Table 1.
Brief definition of each type of intervention.
| Intervention | Definition |
|---|---|
| Acute day units | Non-residential services providing some combination of structured therapeutic groups and activities and access to support and treatment for those in a mental health crisis; an alternative to inpatient treatment. |
| Adherence therapy | Any reward, motivation or therapeutic intervention that aims to reduce individuals' psychiatric symptoms by enhancing adherence with medication. |
| Assertive community treatment | A multi-disciplinary community team approach, designed for people with psychosis with complex needs and frequent hospital admissions, characterised by a whole-team approach, small caseloads, and sustained assertive engagement. |
| Cognitive behavioural therapy for psychosis | An individual therapy which uses an awareness of the relationship between thoughts, feelings, and behaviour to reduce the impact of delusions and hallucinations on functioning. |
| Community rehabilitation services | Multidisciplinary community mental health teams that maintain long-term care and support for people with psychosis with high levels of need and difficulties with social functioning. |
| Compulsory community treatment | A legal order requiring individuals to accept specified treatment in the community, overseen by a responsible clinician. |
| Crisis houses | Offer intensive short-term support and treatment for individuals to manage and resolve mental health crises in a non-hospital residential setting. |
| Crisis plans | Plans made by staff and individuals together for future psychiatric emergencies, aiming to facilitate early detection and treatment of relapse, including the patient's preferences for treatment in the event of loss of decision-making capacity. |
| Crisis resolution teams | Multidisciplinary teams providing intensive, short-term support and treatment for individuals in their own home during a mental health crisis. |
| Early intervention services for psychosis | Multidisciplinary community mental health teams that aim to form strong therapeutic relationships and to provide a full range of effective clinical and social interventions to people in the early stages of psychosis, aiming to improve long-term prognosis and engagement with services. |
| Family interventions for psychosis | Therapeutic approaches involving individuals with psychosis and their family to enhance family communication and problem-solving skills and improve support within the family and from services. |
| Housing interventions | Any interventions aiming to improve housing conditions in order to improve mental health and social functioning. |
| Self-management interventions | Interventions aiming to provide individuals with the knowledge and skills to recognise and manage their own mental health problems, including responding to early warning signs of crises. Often clinician-supported for people with psychosis but may also be provided online or through a manual. |
| Vocational interventions | Any activities designed to help people find, get, and keep employment or to improve their workplace experience and success. |
Note. Adherence therapy includes compliance therapy. Crisis plans includes advance statements. Crisis resolution teams includes crisis intervention. Assertive community treatment includes assertive outreach and intensive case management. Self-management interventions include relapse prevention.
Studies were included if they compared any of the above interventions with another active treatment or treatment as usual, however this was defined. The outcome of interest was number of participants with compulsory admissions, regardless of whether this was measured as a primary or secondary outcome or adverse event, and regardless of whether it was included in the abstract. Where compulsory admissions were stated as an outcome in the trial protocol or paper but were not reported in trial results, or were reported only among descriptive statistics, authors were contacted for more information. Only published randomised controlled trials (RCTs) were considered for inclusion.
2.2. Search Strategy and Study Selection
Our search strategy was aimed at rapid identification of all trials reporting compulsory admissions in any capacity and had two stages. Firstly, six resources were searched from their inception until 9th July 2018 for systematic reviews of each of the listed interventions, with screening of systematic reviews based on title and abstract. These resources were: Cochrane Database of Systematic Reviews; National Institute for Health and Care Excellence (NICE) Guideline (2014) — Psychosis and schizophrenia in adults: prevention and management (CG178); NICE Guideline (2016) — Bipolar disorder: assessment and management (CG185); University of York Centre for Reviews and Dissemination (CRD) database, including the Cochrane Database of Abstracts of Reviews of Effects (DARE); Prospero international prospective register of systematic reviews; MEDLINE electronic database (Ovid version). Only the clinical guidelines for psychosis and bipolar disorder were searched, rather than those for other diagnoses, as these clinical populations are most commonly compulsorily admitted [19], [20], [21], [22], [23].
Search terms for each intervention were combined with terms for systematic review. For example: (“acute day unit*” OR “day hospital*”) AND (“systematic review” OR “meta analysis” OR “meta-analysis”). Where several relevant systematic reviews were identified, the broadest (in terms of inclusion criteria) and the most recent were chosen for each of the listed interventions. The full texts of all RCTs included in these systematic reviews were then screened for eligibility to determine whether they reported compulsory admissions.
In the second stage, we searched for individual trials which post-dated the most recent identified systematic review of each of the listed intervention types (search completed on 9th July 2018). This search combined terms for each intervention with terms for RCTs, for example: (“acute day unit*” OR “day hospital*”) AND (“random* control* trial” OR “RCT”). We performed this search on three databases: MEDLINE and Embase (Ovid versions) and the ISRCTN (International Standard Randomised Controlled Trials Number) registry of clinical trials. Titles and abstracts of the search results were screened for eligibility, followed by the full texts of papers reporting trials of included interventions. The listed interventions were divided among three study authors (JKB, TM, HRS), who each searched independently and resolved any uncertainties by consulting with the other two authors. See Supplementary Materials Appendix 1 for more information on the search strategy and results.
2.3. Data Synthesis
Data were extracted and reviewed in Microsoft Excel. Study characteristics and compulsory admissions data were extracted for all eligible trials, including date, country, service setting, target population and inclusion criteria, number of participants, RCT design, a description of each intervention, and follow-up length (Supplementary Materials Appendix 2).
For RCTs which reported descriptive data without performing statistical analyses of compulsory admissions, we performed post-hoc analyses using univariate statistics to investigate whether there was evidence to support the effectiveness of these interventions. Analyses were performed using the immediate commands in Stata 14 [24]. A narrative synthesis of the included trials was then conducted, grouped according to intervention type and evidence available.
2.4. Risk of Bias Assessment
Risk of bias was assessed for each included study using the Cochrane Collaboration Risk of Bias Tool [25] using the following domains: random sequence generation, allocation concealment, incomplete outcome data, and selective reporting. Each trial was rated as unclear, low, or high for every domain. Two reviewers (HRS, TM) conducted risk of bias assessments independently and any discrepancies were resolved through discussion, including a third author (JKB) if necessary.
No trials were able to blind participants or clinicians, due to the nature of the interventions, so this was not included in the risk of bias assessment. Blinding of outcome assessors also was not included because our outcome was an objective event assessed or cross-checked in computer records; compulsory admissions are unlikely to be affected by detection bias.
3. Results
3.1. Study Characteristics
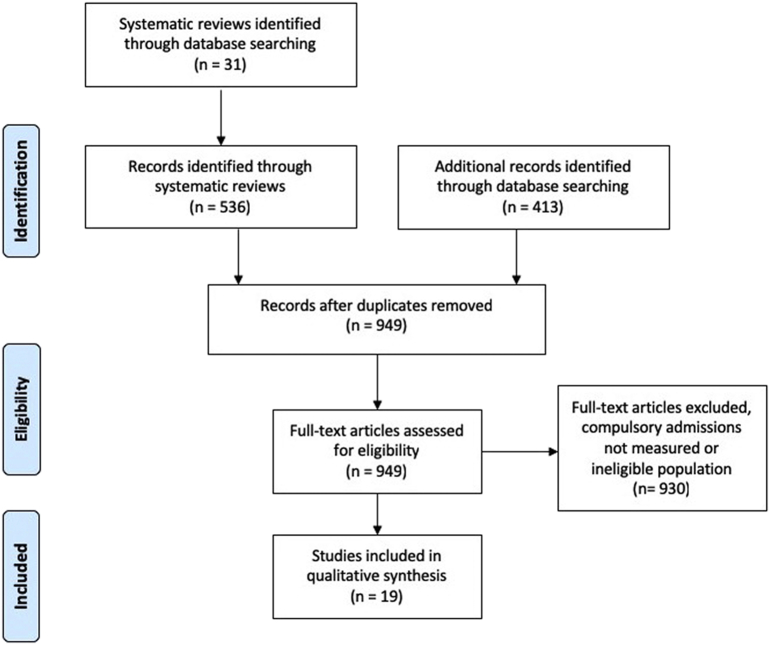
A total of 949 studies were found and screened. Fig. 1 shows the number of records identified, included and excluded, and the reasons for exclusions, Table 2 shows a breakdown by intervention, and Supplementary Materials Appendix 1 has further details of screening. For community rehabilitation services and Open Dialogue, our search yielded no suitable systematic reviews from which to extract trials, and no eligible RCTs. No RCTs reporting compulsory admissions were found for acute day units, compulsory community treatment, family interventions for psychosis, housing interventions, or vocational interventions. The effects of these interventions on compulsory admissions therefore could not be evaluated in this review.
Fig. 1.
Flow diagram of randomised controlled trials identified and eligible for inclusion.
Table 2.
Summary of papers retrieved.
| Intervention | Number of RCTs |
|||
|---|---|---|---|---|
| Screened | Eligible (data on compulsory admissions available) | Descriptive data on compulsory admissions reported (not analysed) | Compulsory admissions analysed as an outcome | |
| Acute day units Day hospitals |
18 | 0 | – | – |
| Adherence therapy Compliance therapy |
46 | 3 | 2 | 1 |
| Advance statements Crisis plans |
22 | 4 | 0 | 4 |
| Assertive community treatment Intensive case management Assertive outreach |
146 | 2 | 1 | 1 |
| Cognitive behavioural therapy for psychosis | 85 | 4 | 4 | 0 |
| Community rehabilitation services | 20 | 0 | – | – |
| Compulsory community treatment Community treatment orders Involuntary outpatient commitment |
4 | 0 | – | – |
| Crisis houses | 32 | 1 | 1 | 0 |
| Crisis intervention Crisis resolution teams |
45 | 1 | 0 | 1 |
| Early intervention services for psychosis | 26 | 3 | 0 | 3 |
| Family interventions for psychosis | 82 | 0 | – | – |
| Housing interventions Supported housing Housing first |
73 | 0 | – | – |
| Open dialogue | 0 | – | – | – |
| Self-management interventions Relapse prevention |
258 | 1 | 0 | 1 |
| Vocational interventions Supported employment Individual placement and support |
92 | 0 | – | – |
| Total | 949 | 19 | 8 | 11 |
Nineteen RCTs were identified as evaluating compulsory admissions. Crisis plans and CBTp were evaluated by four RCTs each, adherence therapy and EIS were evaluated by three RCTs each, and two RCTs evaluated assertive community treatment. Only one trial was found evaluating each of crisis houses, crisis resolution teams, and self-management interventions.
Twelve of the trials were conducted in the United Kingdom, two in the Netherlands, and one each in Denmark, Hong Kong, Norway, Switzerland, and the United States of America. The trials were evenly spread across the last three decades, with the most recent trial ending in 2017.
Most RCTs included people with severe mental illness. Some studied mixed populations from secondary mental health services, including people with depression and personality disorders. In all trials, the majority of participants had a diagnosis of schizophrenia or schizophrenia-like disorders. Most RCTs reported that the majority of participants were of white ethnicity, ranging from 31% to 74% across trials. Follow-up periods ranged from immediately post-intervention to 12 years.
In all but two trials, interventions were compared to treatment as usual (TAU). TAU generally consisted of standard community psychiatric care, usually with a coordinated care programme delivered by a multidisciplinary team. One RCT gave the control group a leaflet about local mental health services and the Mental Health Act, in addition to TAU [26]. Another assigned participants to antipsychotics, cognitive behavioural therapy (CBT), or antipsychotics plus CBT but reported compulsory admissions on an as-treated basis, including a group who received neither antipsychotics nor CBT (so effectively had TAU) [27].
Six trials reported compulsory admission as a primary outcome (one trial of EIS [28], all trials of crisis plans [26], [29], [30], [31] and self-management [32]). The remaining trials reported compulsory admissions as a secondary outcome (nine trials) [33], [34], [35], [36], [37], [38], [39], [40], [41], adverse event (two trials) [27], [42], or data was provided via email by the authors (two trials) [43], [44]. To increase the scope of our review, RCTs reporting descriptive statistics were included even if authors had not responded to requests for information or had not been able to provide statistical analyses. See Table 3 for an overview of the available evidence on the effectiveness of each intervention for reducing compulsory admissions.
Table 3.
Effects of each intervention on number of participants with one or more compulsory admission.
| No. of participants with one or more compulsory admission/total participants in group (%) |
Evidence for effectiveness | ||
|---|---|---|---|
| Intervention group | Control group | ||
| Adherence therapy | |||
| Staring 2010 | 1/53 (2%) | 6/52 (12%) | Fisher's exact test p = 0.053 (one-sided) |
| Priebe 2013 | 15/78 (20%) | 14/60 (25%) | χ2 (1) = 0·47, p = 0·50a |
| Chien 2015 | Not reported (N = 54) | Not reported (N = 56) | p > 0·25 |
| Assertive community treatment | |||
| Harrison-Read 2002 | N = 97 Approx. 20% per year (n not reported) |
N = 96 Approx. 20% per year (n not reported) |
Unable to test |
| Killaspy 2006 | 60/124 (47%) | 54/119 (44%) | χ2 (1) = 0·22, p = 0·64a |
| Cognitive behavioural therapy for psychosis | |||
| Jolley 2003 | 0/8 (0%) | 1/8 (13%) | χ2 (1) = 1·07, p = 0·30a |
| Trower 2004 | 1/18 (6%) | 4/20 (20%) | Unable to test (see note) |
| Morrison 2014 | 0/37 (0%) | 3/37 (8%) | χ2 (1) = 3·13, p = 0·08a |
| Morrison 2018 |
CBT only: 2/20 (10%) Combination: 1/21 (5%) |
Neither antipsychotics nor CBT: 0/13 (0%) Antipsychotics only: 0/21 (0%) |
χ2 (3) = 3·32, p = 0·34a |
| Crisis houses | |||
| Fenton 1998 | 6/69 (12%) | Not reported (N = 50) | Unable to test (see note) |
| Crisis plans | |||
| Papageorgiou 2002 | 15/79 (19%) | 16/77 (21%) | χ2 (1) = 0·08, p = 0·78 |
| Henderson 2004 | 10/80 (13%) | 21/80 (26%) | RR = 0·48, 95% CI 0·24 to 0·95, p = 0·03 |
| Thornicroft 2013 | 49/267 (18%) | 56/280 (20%) | OR = 0·90, 95% CI 0·58 to 1·39, p = 0·63 |
| Ruchlewska 2014 | Emergency: 19/139 (14%) Court-ordered: 18/139 (13%) |
Emergency: 14/73 (19%) Court-ordered: 19/73 (26%) |
Emergency admissions: χ2 (1) = 1·11, p = 0·29a Court-ordered admissions: χ2 (1) = 5·68, p = 0·02a |
| Crisis resolution teams | |||
| Johnson 2005 | 8 weeks: 16/135 (12%) 6 months: 24/134 (18%) |
8 weeks: 24/125 (19%) 6 months: 32/124 (26%) |
8 w: OR = 0·57, 95% CI = 0·28 to 1·1, p = 0·10 6 m: OR = 0·63, 95% CI = 0·35 to 1·2, p = 0·13 |
| Early intervention services for psychosis | |||
| Craig 2004 | 17/68 (25%) | 27/65 (42%) | χ2 (1) = 4·11, p = 0·04b |
| Øhlenschlæger 2008 | 28/167 (17%) | 23/161 (14%) | OR = 1·21, 95% CI = 0·66 to 2·20, p > 0·05 |
| Sigrúnarson 2013 | 11/28 (39%) | 12/17 (71%) | χ2 (1) = 4·15, p = 0·04 |
| Self-management interventions | |||
| Lay 2018 | 21/75 (28%) | 40/93 (43%) | RR = 0·55, 95% CI = 0·33 to 0·94, p = 0·03 |
Note. Adherence therapy includes compliance therapy. Crisis plans includes advance statements. Crisis resolution teams includes crisis intervention. Assertive community treatment includes assertive outreach and intensive case management. Self-management interventions includes relapse prevention. RR = risk ratio. OR = odds ratio. In the RCT by Trower and colleagues (2004), N in each study arm was not clear at the time of measurement; we have reported N at randomisation (study authors were contacted but could not provide data for this trial). In the RCT by Fenton and colleagues (1998), between 0 and 2 patients were compulsorily admitted in the control group, but the text is ambiguous (study authors were contacted but could not provide data).
Denotes that we performed the statistical test using summary statistics provided in the RCTs. Analyses were performed using the immediate commands in Stata 14.
Denotes an unpublished result, provided via communication with the authors.
3.2. Risk of Bias Assessment
Supplementary Materials Appendix 3 summarises the risk of bias assessments. The overall risk of bias was low for most studies. Four trials had unclear risk of selection bias due to random sequence generation with insufficient detail provided [28], [32], [36], [37], but the rest had low risk of bias. Similarly, four trials had unclear risk of selection bias due to allocation concealment [28], [32], [35], [40], but the remaining trials all had low risk of selection bias.
In thirteen studies, the risk of attrition bias was low. The primary outcome of compulsory admissions was largely collected from hospital records meaning that there was little missing data in these studies. However, risk of attrition bias was high in four studies as dropout was unbalanced between groups [30], [32], [34], [38]. The risk of attrition bias was unclear in two studies [35], [37] owing to insufficient information.
The risk of reporting bias was unclear for nine studies, as no protocols were registered or published. For trials where protocols were available, nine had low risk of bias and one had a high risk of reporting bias because compulsory admissions were not included as an outcome in the original study protocol [28].
3.3. Interventions with Evidence to Support Their Effectiveness
3.3.1. Self-management
Only one RCT of self-management was eligible for inclusion in our review [32]. Participants who had one or more compulsory admission in the previous two years received a programme that primarily addressed their self-management skills. This included crisis planning, psychoeducation, and preventive monitoring by a psychologist independent of the patient's care team. After adjusting for confounders, the intervention reduced risk of compulsory readmission by 45% compared to TAU (risk ratio = 0·55, 95% CI 0·33 to 0·94, p = 0·03). However, the attrition rate in this trial was 29% overall, and unequal between intervention and control groups, leading to some concerns about study quality.
3.3.2. Crisis Plans
Two RCTs found evidence that crisis plans reduced compulsory admissions for people with psychotic illness or bipolar disorder who had experienced a psychiatric hospital admission or crisis in the previous two years [26], [31]. In a single-site English trial, over 15 months, 13% of participants who had made joint crisis plans with their care coordinator, psychiatrist, and project worker were admitted to hospital involuntarily, compared to 26% of those in the control group who received leaflets (risk ratio = 0·48, 95% CI 0·24 to 0·95, p = 0·03) [26]. In a recent trial of crisis plans in the Netherlands [31], participants who formulated a crisis plan with a patient advocate or clinician had fewer court-ordered admissions (13%) than the control group (26%; χ2 (1) = 5·68, p = 0·02). This RCT distinguished emergency compulsory admissions from those planned in advance by court order and did not find evidence for a reduction in emergency compulsory admissions (χ2 (1) = 1·11, p = 0·29). However, 14% of those who formulated crisis plans had emergency compulsory admissions, compared to 19% of the control group.
Two other trials found no evidence for a reduction in compulsory admissions using crisis plans compared to treatment as usual [29], [30]. In both of these trials, a smaller proportion of participants who made crisis plans experienced compulsory admissions than those receiving TAU, but these differences were non-significant (Table 3).
De Jong and colleagues identified all four of these trials in their systematic review and meta-analysis, reporting a 23% reduction in the risk of compulsory admission as a pooled effect of the 4 RCTs (relative risk = 0·77, 95% CI 0·60 to 0·98, I2 = 2·2%) [1]. Overall, the evidence is promising, suggesting that making a crisis plan may reduce subsequent compulsory admissions.
3.4. Interventions with Mixed Evidence to Support Their Effectiveness
3.4.1. Early Intervention Services for Psychosis
In all EIS trials, TAU consisted of treatment from a non-specialist community mental health team. Two RCTs of EIS provided evidence for a reduction in compulsory admissions [39], [43]. For people diagnosed with psychosis, care from a specialised EIS team in England resulted in significantly fewer compulsory admissions than standard care [43]. In the 18 months following the intervention, 25% of those receiving care from an EIS had at least one involuntary admission, compared to 42% of those receiving standard care (χ2 (1) = 4·11, p = 0·04). A Norwegian RCT with an extremely long 12-year follow-up period reported similarly positive results [39]. Those who received care from an EIS were less likely to have a compulsory admission in the subsequent 12 years (39%) than the control group (71%; χ2 (1) = 4·15, p = 0·04).
However, the largest, Danish RCT of EIS (n = 328) [28], found no evidence that care from an EIS versus standard care reduced compulsory admissions over the subsequent 12 months. In this trial, 17% of the intervention group had a compulsory admission compared to 14% of the control group (odds ratio = 1·21, 95% CI 0·66 to 2·20, p > 0·05). Although a non-significant difference, the intervention group did spend fewer days compulsorily admitted (mean = 48·9, SD = 43·8) than the control group (mean = 74·5, SD = 70·4; p > 0·05). The EIS model in this trial was very similar to both other RCTs, except that cognitive behavioural therapy was not offered. However, there was a markedly lower rate of compulsory admissions in the standard care group in this Danish trial than in the other two trials. Thus, there are mixed findings so far as to whether care from an EIS does reduce compulsory admissions for people in the early stages of psychosis.
3.5. Interventions Lacking Clear Evidence
3.5.1. Adherence Therapy
We found three recent trials of adherence therapy from Hong Kong, the Netherlands, and the UK, all of which included participants who had schizophrenia spectrum disorders and poor adherence to antipsychotic medication [33], [38], [40]. The earliest trial compared treatment adherence therapy (motivational interviewing, medication optimisation and behavioural training) to TAU [40]. In the following 6 months, 2% of those receiving the intervention and 12% of those in the control group had at least one compulsory admission. This difference in compulsory admissions tended to statistical significance (Fisher's exact test one-sided p = 0·053) [40].
A trial using motivational interviewing-based adherence therapy found no evidence that this reduced compulsory admissions over 6 months compared to TAU (p > 0·25; Table 3) [33]. Another RCT using financial incentives to improve adherence [38] found 20% of the intervention group and 25% of the control group experienced compulsory admissions. In a post-hoc analysis, we found no evidence for a statistically significant difference between study arms (χ2 (1) = 0·47, p = 0·50). Overall, current evidence does not indicate that adherence therapy (including financial incentives) is effective in reducing risk of subsequent compulsory admissions.
3.5.2. Crisis Resolution Teams
In the only included trial of crisis resolution teams in England [36], participants in the experimental group had fewer total hospital admissions in the 8 weeks following the crisis. However, while the direction of effect favoured crisis team care, there was no significant difference in compulsory admissions for care from a crisis resolution team compared to standard care at either 8 weeks (odds ratio = 0·57, 95% CI 0·28 to 1·1, p = 0·10) or 6 months (odds ratio = 0·63, 95% CI 0·35 to 1·2, p = 0·13).
3.5.3. Assertive Community Treatment (ACT)
Two trials of ACT, both English, found no effect on compulsory admissions. The first [35] reported that compulsory admissions were “similar in the two treatment groups”, with approximately 20% of participants being admitted compulsorily every year. They did not report statistical analyses of compulsory admissions, but these numbers suggest that there is no evidence for the efficacy of ACT in reducing compulsory admissions. The second trial of ACT also provided no evidence of a reduction in compulsory admissions in our post-hoc analyses (Table 3) [44]. However, neither trial included services which were of consistently high fidelity to the ACT model. Neither offered services 24 h a day and, in the first RCT, patients remained under their existing consultant psychiatrist [35]. In the second, fidelity scores were high for one and fair for the other ACT team, meaning the intervention was only ACT-like for some participants [44].
The remaining RCTs (five trials of CBTp and crisis houses) did not perform statistical analyses of compulsory admissions (Table 3). We performed post-hoc analyses to indicate whether there was evidence to support the effectiveness of these interventions.
3.5.4. Cognitive Behavioural Therapy for Psychosis
Three English trials of CBTp [37], [41], [42] reported more compulsory admissions in the control than the intervention arm, although the fourth and most recent English trial reported more among the groups receiving CBTp (either alone or in conjunction with antipsychotic medication) [27]. However, none of these small trials were powered to evaluate compulsory admissions and they did not show a significant effect on compulsory admissions in post-hoc analyses (Table 3). We are therefore unable to evaluate the effectiveness of these interventions in reducing compulsory admissions.
3.5.5. Crisis Houses
The single included trial examining crisis houses presented only descriptive statistics [34]. This American RCT reported more compulsory admissions in the intervention than the control group, but the number of compulsory admissions in the control group was ambiguous so we could not statistically test for evidence to support this association (Table 3).
4. Discussion
We found nineteen RCTs which reported compulsory admissions as an outcome (primary or secondary) or adverse event. Risk of bias in included studies was generally low, suggesting that they were relatively high quality RCTs. Inclusion of compulsory admissions as an outcome in trials was rare, even in studies evaluating interventions which might reasonably be expected to reduce compulsory admissions. Less than 2% of trials screened for inclusion in this rapid evidence synthesis reported compulsory admissions. Even when included as a study outcome, reporting was inconsistent.
Only trials of crisis planning interventions tended to be designed to evaluate compulsory admissions as a main outcome, and these showed promise as an effective intervention. There was evidence that a self-management programme with a crisis planning element reduced compulsory admissions, and mixed evidence regarding EIS teams. In the cases of adherence therapy, care from crisis resolution teams, or assertive community treatment, there were some studies in which effects on compulsory admission were not found, but numbers of studies and rates of compulsory admission were small, studies were not powered to detect effects on compulsory admission, and compulsory admission was not a primary outcome measure.
We could not evaluate the effect of acute day units, community rehabilitation services, compulsory community treatment, family interventions for psychosis, housing interventions, Open Dialogue, or vocational interventions on compulsory admissions in even the most preliminary way as no eligible trials were found for these interventions. Additionally, trials of CBTp and crisis houses only reported descriptive data on compulsory admissions, so their effectiveness could not be assessed fully.
The self-management programme [32] overlapped in content with the crisis plan interventions included in this review [26], [29], [30], [31]. All included a relapse prevention planning element, where participants are supported by a clinician to identify their early warning signs of relapse and plan and share personal coping strategies and desired support from clinicians and carers. The self-management programme included an additional active monitoring element, supported by a psychologist independent of the care team [32]. A recent systematic review included all five of these trials in a meta-analysis of broadly-defined crisis planning interventions [45]. This meta-analysis supports the results of De Jong and colleagues [1], finding a pooled effect of a 25% reduction in compulsory admissions among those receiving crisis planning interventions compared to standard care [45]. According to both of these meta-analyses and our review, crisis planning interventions show greatest promise in preventing compulsory admissions.
EISs are multidisciplinary community teams offering a relatively intensive approach, focused on psychological and social recovery, to people following a first episode of psychosis [43]. There were some promising findings for this approach, especially where compulsory admission rates were high. However, no evidence of an effect in a large trial in the field means a clear conclusion cannot be drawn. Little published evidence was available regarding longer-term models of community care.
This rapid evidence synthesis used a broader search strategy to retrieve articles than the previous systematic review [1], searching protocols and full texts for compulsory admissions data. Trials reporting compulsory admission as a primary or secondary outcome, or as an adverse event, were all retrieved, allowing an overview of trial evidence of all types. A broad range of interventions were included as well as international trials across a wide time period.
Our review provided an up-to-date summary of all current evidence to support the Independent Review of the Mental Health Act in England in 2018. It was systematic but not necessarily comprehensive. The review only included papers that clearly distinguished compulsory from voluntary admissions. This may have led to missed evidence from studies measuring compulsory admissions but not clearly reporting them.
A range of experts helped to generate our list of interventions, but it is nonetheless possible that we missed some candidates. Our search strategy included databases which would include trials for any diagnostic groups, but only the NICE guidelines for psychosis and bipolar disorder were searched. Additionally, several of the interventions included in this review specifically target people with psychotic disorders. This was an efficient choice given that people with psychosis are the group most often involuntarily admitted [19], [20], [21], [22], [23] and other aspects of the search did include non-psychotic populations. In our expert consultation to identify relevant interventions, we did not begin from a pre-defined focus on psychosis, and the nominated interventions included many that are relevant to a range of clinical groups (e.g. crisis services, self-management interventions). Nevertheless, some relevant interventions for other clinical groups who can be compulsorily admitted to psychiatric hospital (e.g. people with dementia or a personality disorder) may not have been included.
Due to the small number of eligible trials and heterogeneity within each intervention type regarding treatment content, trial criteria, and context, we did not conduct any quantitative synthesis of trial results. Without meta-analyses, however, our results are hard to interpret. For example, for crisis plans and self-management interventions two out of five RCTs showed no evidence of reductions in compulsory admissions, and one provided mixed evidence. However, pooled evidence from meta-analyses on the same topic demonstrates a significant reduction in compulsory admissions [1], [45].
Despite the wide scope of this review, we found only nineteen trials which measured the effect of the intervention on compulsory admissions, even with the inclusion of secondary outcomes and reports on adverse events. This was surprising and concerning, as compulsory admissions are becoming more common [2], [3], [4], [5], [6] and being admitted compulsorily is often a distressing experience for patients and their relatives [8], [10], [11], [12], [46]. For many interventions, the trials included in our review represent only a small fraction of those published, as compulsory admission is rarely included as an outcome measure, despite being relatively easy to measure from routine data in the UK. When compulsory admissions were measured in trials, reporting standards were often very low. Of the nineteen trials included in our review, eight did not originally test whether interventions were associated with a significant reduction in participants' risk of compulsory admissions.
The majority of included trials recorded compulsory admissions as a secondary outcome or adverse event, and often only a small proportion of participants in both groups were admitted. These trials are therefore likely to have been underpowered to detect a significant difference between groups on this rare binary outcome, reflected in the wide confidence intervals in many of the reported comparisons. For example, the trial of crisis resolution teams [36] reports effects of moderate size in reducing compulsory admissions, but these results were not statistically significant. More trials are required for all interventions in this review before a clear picture emerges of which have any promise in reducing admissions.
In addition, trials were spread across seven countries and over the last three decades. As a result, variations in service provision, standards of practice, and legislative systems may limit generalisability.
Overall, this rapid evidence synthesis indicates that crisis planning and self-management interventions with a relapse prevention planning and monitoring element are most promising for preventing compulsory admissions. Improving access to these interventions and successfully implementing them within practice is therefore a priority for policy makers and service planners. This review also suggests that the provision of specialist EIS teams for people with first onset psychosis may succeed in reducing compulsory admissions as well as achieving other more well-established benefits for service users [47], [48].
For all other interventions, only a small proportion of trials evaluated compulsory admissions and our findings are based on a few trials only. Interventions for which we lack evidence may still be effective in reducing compulsory admissions, and interventions which our review suggests have some promise may not be effective in reducing compulsory admissions across all contexts. It is therefore not possible to make any further recommendations for practice.
The inconclusive findings on the effectiveness of most interventions indicates a need for more research. Trials should pre-register compulsory admissions as an outcome, report compulsory admission data even if not the primary outcome, and consider this outcome when performing power calculations. Given the lengthy nature of trials, the potential selection bias in recruiting people at high risk of admission, and the large numbers likely to be needed for good power with this binary outcome, other ways to explore the effectiveness of interventions should be considered. For example, observational studies could use routine data to provide preliminary findings.
Compulsory and voluntary admissions should not be reported jointly under the umbrella label of hospitalisations or admissions. They have distinct impacts for everyone involved [13], [14] and therefore the effectiveness of interventions in reducing each type of admission should be evaluated separately. However, failing to do so may be partially due to international differences in recording of admissions. In the UK, standard clinical records show whether an admission is voluntary or compulsory. In the USA, hospitalisations are recorded routinely but to determine whether those hospitalisations are voluntary or involuntary requires special data collection efforts. In a recent large project on psychiatric hospitalisations, Blyler and colleagues were not able to obtain data on whether admissions were compulsory or voluntary from 43 of 59 included facilities [49]. Compulsory admissions are also not distinguished from voluntary admissions in Medicaid and Medicare billing records, which many researchers use to record objective outcomes. Recording of admissions must therefore improve in clinical records if these are to be used for research outcomes.
Finally, further research is required to understand which interventions work for whom. The majority of participants in trials to date have been of White ethnicity. However, in over 1 million patients using mental health services in England, being from a Black ethnic group was associated with 2·94 times higher odds of a compulsory admission compared to White patients [50]. RCT samples do not reflect the characteristics of those compulsorily admitted, raising questions about whether we can generalise findings. We need further evidence including diverse groups of people and evaluating the efficacy of interventions according to individual characteristics (such as age, ethnicity, gender, and mental health problems), service provision, legislative systems, and types of compulsory admissions.
Lived Experience Perspective by Karen Machin, Sarah Markham and Karen Persaud.
It can be exceedingly difficult for someone heading towards, or in crisis, to access support. Findings from this review indicate that although there is no certainty about what type of support may be successful in terms of avoiding compulsory admission, self-management interventions and crisis plans seem to have some efficacy. We suggest that factors may include the quality of implementation or length of the intervention, where in the individual's mental health trajectory they receive the intervention, and whether the intervention is suitable for each individual's needs given their individual circumstances.
Topics such as peer support, carer involvement or wider social support networks were outside the scope of this review. The clinical trials considered didn't appear to consider the impact of individual participants' ethnicity, culture, first language and religion. These variables effect use of mental health services, and we anticipate this might be mirrored in research participation. We suggest future studies investigate the effect of these variables on the efficacy of interventions. It may be of value to engage with qualitative research into service users' and carers' experiences and views on this subject.
We anticipated that data on compulsory admissions would be relatively simple to access, especially as they are an important outcome measure. However, we acknowledge international differences in data collection due to the differences in individual health systems.
Compulsory admissions remain controversial due to associations with human rights and other ethical dilemmas. According to the Interim Report [DHSC, 2018] of the current review of the MHA, people held under the Act are vulnerable to “potential coercive mistreatment”, which can lead to physical and psychological harm. Carers may be left feeling distraught, disempowered and isolated. Consequently, we recommend that compulsory admission should be an outcome measure for research into the efficacy of mental health care, treatment, and support modalities.
Karen Machin, Sarah Markham and Karen Persaud are members of the Lived Experience Working Group for the National Institute for Health Research Mental Health Policy Research Unit.
Acknowledgments
Acknowledgements
We would like to thank all trial authors who assisted us with our enquiries and provided data where available: Prof Max Birchwood, Dr. Crystal Blyler, Prof Tom Burns, Dr. Daniel Chandler, Professor Tom Craig, Dr. Phil Harrison-Read, Dr. Suzanne Jolley, Prof Helen Killaspy, Prof Tony Morrison, Prof Stefan Priebe, and Prof Marvin Swartz. We would also like to thank Natasha Lyons, Sahar Hadidimoud, and Dr. Ahmad Ali for their contributions.
Authors' contributions
BLE and SJ conceptualised this review and designed the original protocol. JKB, TM and HRS developed the search criteria, performed the searches and screening, extracted and analysed the data, and drafted the manuscript with input from all other study authors. BLE advised on the extraction of the data. KM, SM and KP co-authored the lived experience perspective. BLE provided senior supervision. All authors read and revised the whole report.
Declaration of Interests
All researchers report grants from the National Institute for Health Research Policy Research Programme during the conduct of the study. No other conflicts of interest exist.
Funding
This paper is based on independent research commissioned and funded by the National Institute for Health Research Policy Research Programme, through the NIHR Mental Health Policy Research Unit. The views expressed are those of the authors and not necessarily those of the NHS, the National Institute for Health Research, the Department of Health and Social Care or its arm's length bodies, and other Government Departments.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.eclinm.2019.03.017.
Appendix A. Supplementary data
Supplementary material
References
- 1.De Jong M.H. Interventions to reduce compulsory psychiatric admissions a systematic review and meta-analysis. JAMA Psychiat. 2016;73:657–664. doi: 10.1001/jamapsychiatry.2016.0501. [DOI] [PubMed] [Google Scholar]
- 2.Centre HaSCI . Uses of the mental health act: annual statistics, 2014/15. Health and social care information Centre. 2015. Inpatients formally detained in hospitals under the Mental Health Act 1983, and patients subject to supervised community treatment. [Google Scholar]
- 3.Keown P., Weich S., Bhui K.S., Scott J. Association between provision of mental illness beds and rate of involuntary admissions in the NHS in England 1988-2008: ecological study. BMJ. 2011;343:d3736. doi: 10.1136/bmj.d3736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schoevaerts K., Bruffaerts R., Mulder C.L., Vandenberghe J. An increase of compulsory admissions in Belgium and the Netherlands: an epidemiological exploration. Tijdschr Psychiatr. 2013;55:45–55. [PubMed] [Google Scholar]
- 5.Zolkowska K., Cantor-Graae E., McNeil T.F. Increased rates of psychosis among immigrants to Sweden: is migration a risk factor for psychosis? Psychol Med. 2001;31:669–678. doi: 10.1017/s0033291701003786. [DOI] [PubMed] [Google Scholar]
- 6.Keown P., Murphy H., McKenna D., McKinnon I. Changes in the use of the Mental Health Act 1983 in England 1984/85 to 2015/16. Br J Psychiatry. 2018;213:595–599. doi: 10.1192/bjp.2018.123. [DOI] [PubMed] [Google Scholar]
- 7.Priebe S. Patients' views of involuntary hospital admission after 1 and 3 months: prospective study in 11 European countries. Br J Psychiatry. 2010;196:179–185. doi: 10.1192/bjp.bp.109.068916. [DOI] [PubMed] [Google Scholar]
- 8.Frueh B.C., Knapp R.G., Cusack K.J., Grubaugh A.L., Sauvageot J.A. Patients' reports of traumatic or harmful experiences within the psychiatric setting. Psychiatr Serv. 2005;56:1123–1133. doi: 10.1176/appi.ps.56.9.1123. [DOI] [PubMed] [Google Scholar]
- 9.Mental Health Alliance . 2017. A Mental Health Act fit for tomorrow: an agenda for reform. [Google Scholar]
- 10.Katsakou C., Priebe S. Patient's experiences of involuntary hospital admission and treatment: a review of qualitative studies. Epidemiol Psychiatr Sci. 2007;16:172–178. doi: 10.1017/s1121189x00004802. [DOI] [PubMed] [Google Scholar]
- 11.Sheehan K.A., Burns T. Perceived coercion and the therapeutic relationship: a neglected association? Psychiatr Serv. 2011;62:471–476. doi: 10.1176/ps.62.5.pss6205_0471. [DOI] [PubMed] [Google Scholar]
- 12.Weich S. Experiences of acute mental health care in an ethnically diverse inner city: qualitative interview study. Soc Psychiatry Psychiatr Epidemiol. 2012;47:119–128. doi: 10.1007/s00127-010-0314-z. [DOI] [PubMed] [Google Scholar]
- 13.Kallert T.W., Glöckner M., Schützwohl M. Involuntary vs. voluntary hospital admission: a systematic literature review on outcome diversity. Eur Arch Psychiatry Clin Neurosci. 2008;258:195–209. doi: 10.1007/s00406-007-0777-4. [DOI] [PubMed] [Google Scholar]
- 14.Lloyd-Evans B. 2018. Best practice within psychiatric hospitals for detained patients. Discussion paper for the Mental Health Act Review. [Google Scholar]
- 15.Priebe S. Predictors of clinical and social outcomes following involuntary hospital admission: a prospective observational study. Eur Arch Psychiatry Clin Neurosci. 2011;261:377–386. doi: 10.1007/s00406-010-0179-x. [DOI] [PubMed] [Google Scholar]
- 16.NHS Digital . 2018. Mental Health Act statistics, annual figures: 2017–18. [Google Scholar]
- 17.Independent Review of the Mental Health Act Modernising the Mental Health Act: increasing choice, reducing compulsion. Final report of the Independent Review of the Mental Health Act. 1983;1983(2018) [Google Scholar]
- 18.Moher D., Liberati A., Tetzlaff J., Altman D.G. The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6 [PMC free article] [PubMed] [Google Scholar]
- 19.Balducci P.M., Bernardini F., Pauselli L., Tortorella A., Compton M.T. Correlates of involuntary admission: findings from an Italian inpatient psychiatric unit. Psychiatr Danub. 2017;29:490–496. doi: 10.24869/psyd.2017.490. [DOI] [PubMed] [Google Scholar]
- 20.Gilhooley J. Voluntary and involuntary psychiatric admissions in a suburban area: comparison with national rates, diagnosis and other correlates of involuntary admission status. Ir J Psychol Med. 2017;34:243–249. doi: 10.1017/ipm.2017.44. [DOI] [PubMed] [Google Scholar]
- 21.Lay B., Nordt C., Rössler W. Variation in use of coercive measures in psychiatric hospitals. Eur Psychiatry. 2011;26:244–251. doi: 10.1016/j.eurpsy.2010.11.007. [DOI] [PubMed] [Google Scholar]
- 22.Myklebust L.H., Sørgaard K., Røtvold K., Wynn R. Factors of importance to involuntary admission. Nord J Psychiatry. 2012;66:178–182. doi: 10.3109/08039488.2011.611252. [DOI] [PubMed] [Google Scholar]
- 23.Sanguineti V.R., Samuel S.E., Schwartz S.L., Robeson M.R. Retrospective study of 2,200 involuntary psychiatric admissions and readmissions. Am J Psychiatry. 1996;153:392–396. doi: 10.1176/ajp.153.3.392. [DOI] [PubMed] [Google Scholar]
- 24.StataCorp . StataCorp LP; College Station, TX: 2015. Stata statistical software: release 14. [Google Scholar]
- 25.Higgins J.P.T. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Henderson C. Effect of joint crisis plans on use of compulsory treatment in psychiatry: single blind randomised controlled trial. BMJ. 2004;329:136. doi: 10.1136/bmj.38155.585046.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Morrison A.P. Antipsychotic drugs versus cognitive behavioural therapy versus a combination of both in people with psychosis: a randomised controlled pilot and feasibility study. Lancet Psychiatry. 2018;5:411–423. doi: 10.1016/S2215-0366(18)30096-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Øhlenschlæger J. Effect of integrated treatment on the use of coercive measures in first-episode schizophrenia-spectrum disorder. A randomized clinical trial. Int J Law Psychiatry. 2008;31:72–76. doi: 10.1016/j.ijlp.2007.11.003. [DOI] [PubMed] [Google Scholar]
- 29.Papageorgiou A., King M., Janmohamed A., Davidson O., Dawson J. Advance directives for patients compulsorily admitted to hospital with serious mental illness: randomised controlled trial. Br J Psychiatry. 2002;181:513–519. doi: 10.1192/bjp.181.6.513. [DOI] [PubMed] [Google Scholar]
- 30.Thornicroft G. Clinical outcomes of joint crisis plans to reduce compulsory treatment for people with psychosis: a randomised controlled trial. Lancet. 2013;381:1634–1641. doi: 10.1016/S0140-6736(13)60105-1. [DOI] [PubMed] [Google Scholar]
- 31.Ruchlewska A. Effect of crisis plans on admissions and emergency visits: a randomized controlled trial. PLoS One. 2014;9(1–7) doi: 10.1371/journal.pone.0091882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lay B., Kawohl W., Rössler W. Outcomes of a psycho-education and monitoring programme to prevent compulsory admission to psychiatric inpatient care: a randomised controlled trial. Psychol Med. 2018;48:849–860. doi: 10.1017/S0033291717002239. [DOI] [PubMed] [Google Scholar]
- 33.Chien W.T., Mui J.H.C., Cheung E.F.C., Gray R. Effects of motivational interviewing-based adherence therapy for schizophrenia spectrum disorders: a randomized controlled trial. Trials. 2015;16:1–14. doi: 10.1186/s13063-015-0785-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fenton W.S., Mosher L.R., Herrell J.M., Blyler C.R. Randomized trial of general hospital and residential alternative care for patients with severe and persistent mental illness. Am J Psychiatry. 1998;155:516–522. doi: 10.1176/ajp.155.4.516. [DOI] [PubMed] [Google Scholar]
- 35.Harrison-Read P. Heavy users of acute psychiatric beds: randomized controlled trial of enhanced community management in an outer London borough. Psychol Med. 2002;32:403–416. doi: 10.1017/s0033291702005305. [DOI] [PubMed] [Google Scholar]
- 36.Johnson S. Randomised controlled trial of acute mental health care by a crisis resolution team: the north Islington crisis study. BMJ. 2005;331:599–602. doi: 10.1136/bmj.38519.678148.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jolley S. Cognitive therapy in early psychosis: a pilot randomized controlled trial. Behav Cogn Psychother. 2003;31:473–478. [Google Scholar]
- 38.Priebe S. Effectiveness of financial incentives to improve adherence to maintenance treatment with antipsychotics: cluster randomised controlled trial. BMJ. 2013;347:f5847. doi: 10.1136/bmj.f5847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sigrúnarson V., Gråwe R.W., Morken G. Integrated treatment vs. treatment-as-usual for recent onset schizophrenia; 12 year follow-up on a randomized controlled trial. BMC Psychiatry. 2013;13(200) doi: 10.1186/1471-244X-13-200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Staring A.B.P. Treatment adherence therapy in people with psychotic disorders: randomised controlled trial. Br J Psychiatry. 2010;197:448–455. doi: 10.1192/bjp.bp.110.077289. [DOI] [PubMed] [Google Scholar]
- 41.Trower P. Cognitive therapy for command hallucinations: randomised controlled trial. Br J Psychiatry. 2004;184:312–320. doi: 10.1192/bjp.184.4.312. [DOI] [PubMed] [Google Scholar]
- 42.Morrison A.P. Cognitive therapy for people with schizophrenia spectrum disorders not taking antipsychotic drugs: a single-blind randomised controlled trial. Lancet. 2014;383:1395–1403. doi: 10.1016/S0140-6736(13)62246-1. [DOI] [PubMed] [Google Scholar]
- 43.Craig T.K.J. The Lambeth Early Onset (LEO) Team: randomised controlled trial of the effectiveness of specialised care for early psychosis. BMJ. 2004;329:1067–1070. doi: 10.1136/bmj.38246.594873.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Killaspy H. The REACT study: randomised evaluation of assertive community treatment in north London. Br Med J. 2006;332:815–818. doi: 10.1136/bmj.38773.518322.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.E. Molyneaux, A. Turner, B. Candy, S. Johnson and B. Lloyd-Evans, Crisis planning interventions for people with psychotic illness or bipolar disorder: a systematic review and meta-analyses (in preparation). [DOI] [PMC free article] [PubMed]
- 46.Merson S., Tyrer P., Carlen D., Johnson T. The cost of treatment of psychiatric emergencies: a comparison of hospital and community services. Psychol Med. 1996;26:727–734. doi: 10.1017/s0033291700037740. [DOI] [PubMed] [Google Scholar]
- 47.Marshall M., Rathbone J. Early intervention for psychosis. Schizophr Bull. 2011;37:1111–1114. doi: 10.1093/schbul/sbr110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Randall J.R. A systematic review of the effect of early interventions for psychosis on the usage of inpatient services. Schizophr Bull. 2015;41:1379–1386. doi: 10.1093/schbul/sbv016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mathematica Policy Research . volume 1. 2016. Medicaid emergency psychiatric services demonstration evaluation: final report. [Google Scholar]
- 50.Weich S. Variation in compulsory psychiatric inpatient admission in England: a cross-sectional, multilevel analysis. Heal Serv Deliv Res. 2014;2(90) [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material