Abstract
Appendiceal inversion is an uncommon incidental finding on colonoscopy that can mimic pathologic processes such as colon polyps and neoplasms due to its mass-like appearance. Endoscopic removal of these lesions has been associated with a higher risk of peritonitis and bleeding. Awareness of appendiceal inversion may potentially decrease unwarranted interventions as well as its associated risks. Although there are many reported cases of iatrogenic appendiceal inversion due to the traditional inversion-ligation technique performed during open appendectomy, there are few reported cases of asymptomatic appendiceal inversion without a known history of iatrogenic inversion. Here, we present a case of an asymptomatic patient with appendiceal inversion and no prior history of appendectomy. Furthermore, we discuss management and characteristic imaging findings of appendiceal inversion that may help to distinguish it from similarly appearing pathologic conditions.
Keywords: Appendiceal inversion, Inverted appendix, Colonoscopy
Background
Appendiceal inversion (AI) describes an appendix that is pulled into the lumen of the cecum. Although asymptomatic, AI should be recognized in the differential diagnosis of a cecal mass because it can mimic pathology such as polyps or neoplasms, oftentimes leading to invasive and unwarranted investigations. Known causes of AI include iatrogenic surgical procedures and intussusception [1].
The most common iatrogenic cause of AI occurs during open appendectomy when the base of the appendix is inverted into the cecum with a purse-string suture, a technique that is not used during laparoscopic appendectomy [2]. A series of 395 colonoscopies of patients with a history of open appendectomy found an oblong mass-like lesion corresponding to an inverted appendix in 6 of the patients [3]. A similar technique is performed as an alternative to incidental appendectomy, possibly resulting in AI [4]. This so-called inversion-ligation technique was traditionally performed to theoretically reduce the risk of peritoneal contamination. Subsequently, a prospective, randomized trial of 735 consecutive appendectomies showed no difference in incidence of peritonitis in patients undergoing inversion-ligation vs simple ligation without inversion [5]. Patients with AI due to inversion-ligation technique are generally asymptomatic.
Appendiceal intussusception occurs when the appendix is pulled into itself or into the cecum, a result of irregular appendicular peristalsis due to local irritation [6]. It is an exceedingly rare condition with an incidence of approximately 0.01% in patients undergoing appendectomy for presumed acute appendicitis [7]. Notably, appendiceal intussusception may occur due to appendiceal endometriosis [8]. Although often asymptomatic, patients may present with symptoms similar to those of acute appendicitis – including abdominal pain, vomiting, constipation, diarrhea, or blood in the stool. Oftentimes, patients present with intermittent symptoms over a period of weeks to months [9].
In addition, reports of asymptomatic patients without a history of appendiceal intussusception or inversion ligation of the appendiceal stump suggest the possibility of congenital occurrence of AI [10], [11].
Case presentation
A 55-year-old female with a history of abdominal hysterectomy and laparoscopic cholecystectomy was referred for computed tomography (CT) scan of the abdomen and pelvis with oral and intravenous contrast material for further evaluation of a cecal lesion seen on routine colonoscopy (Fig. 1). The patient had no family history of colon cancer and this was her second routine screening for colorectal cancer. The lesion was first seen 5 years prior on initial routine screening colonoscopy, but was interpreted as an inverted appendix by visual recognition alone during the colonoscopy and no further work-up was pursued other than a 5-year follow-up plan. Five years later, the provider of the second colonoscopy was not comfortable with ruling out a neoplastic process based on visual recognition alone and decided to pursue further work-up with a CT scan. A biopsy was avoided due to a higher risk of perforation in inverted appendices. The patient had no previous history of appendectomy. Other findings of the recent screening colonoscopy were diverticulosis and a <5-mm lesion of the ascending colon that was subsequently identified as a tubular adenoma. CT scan of the abdomen and pelvis showed findings consistent with AI (Fig. 2). Similar findings were seen in a prior CT scan dating back 4 years (Fig. 3).
Fig. 1.
Images obtained during colonoscopy demonstrating a tubular lesion in the ascending colon.
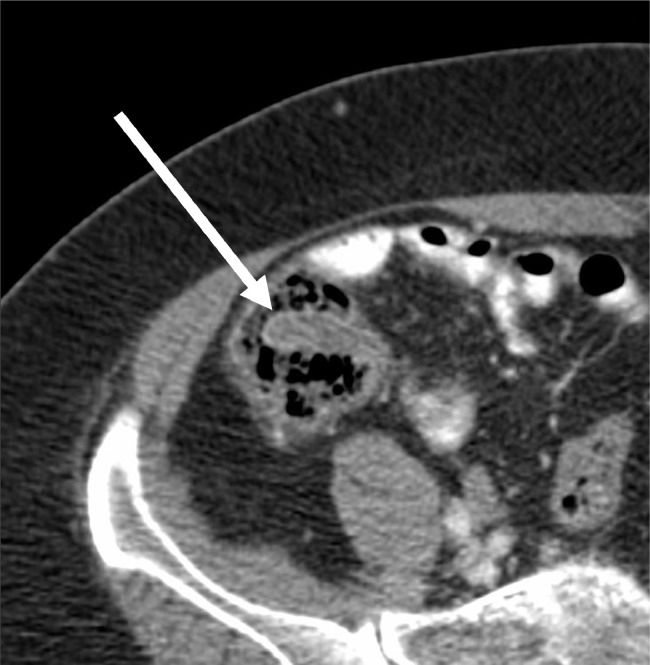
Fig. 2.
CT demonstrating an intraluminal tubular structure in the cecum.
Fig. 3.
Contrast CT 4 years prior demonstrating similar intraluminal tubular structure in the cecum.
Discussion and conclusion
Although relatively rare, an AI must be differentiated from a pathologic process, especially in patients with risk factors for neoplasms of the colon. AI must be included in the differential diagnosis of a polypoid lesion in the region of the appendix, especially when lacking the typical appearance of a neoplasm. Failure to do so may result in further unnecessary, invasive, and potentially harmful investigations. Although the risks are not well defined, anecdotal cases of peritonitis after biopsy or transection have been reported [12], [13]. In addition, simple colonoscopic removal may result in perforation [14].
Reported cases of AI are scarce in the literature, resulting in a lack of definitive guidelines for work-up. Thus, approach to care must be based on an informed clinical judgement that includes aspects of medical history and imaging modalities. Several clues may be helpful in determining whether further diagnostic work-up, such as biopsy, should be pursued. These include surgical history of open appendectomy, gross appearance on colonoscopy, and appearance on CT. A history of open appendectomy supports the diagnosis of AI due to the wide use of inversion-ligation technique during this procedure. The gross appearance of AI, which differs from the typical appearance of a neoplasm, can be recognized by the experienced colonoscopist. In our patient's case, although there was no prior history of open appendectomy, the initial colonoscopist was able to confidently recognize the appearance of the cecal mass as that of AI and opted not to pursue further work-up. However, the second colonoscopist opted for a CT scan of the abdomen and pelvis with oral and IV contrast to help rule out an appendiceal mucinous adenocarcinoma. A majority of epithelial tumors of the appendix demonstrate circumferential mucosal involvement with distension by mucus, known as a mucocele. Less than 50% of cases have curvilinear mural calcification, a characteristic of mucoceles [15]. One other common manifestation of mucinous adenocarcinoma is pseudomyxoma peritonei. In addition, mucinous cystadenoma of the appendix represents a rare cecal lesion that may mimic AI. Indeed, in a 2017 case report, Janczak et al describe a 66-year-old woman who presented with symptoms and radiologic findings consistent with a periappendiceal abscess [16]. Laparotomy revealed a large amount of gelatinous material in the peritoneal cavity as well as a ruptured mucinous cyst of the appendix. The appendix was excised. Subsequent microscopic examination revealed histopathologic features consistent with mucinous cystadenoma of the appendix with low-grade dysplasia. Fortunately, the patient recovered without complication or recurrence.
On CT, characteristics of AI include invagination of the appendix into the cecal lumen (Fig. 2). In our patient, these findings were present on a CT scan dating back 4 years prior, further supporting the diagnosis of AI (Fig. 3). When a cecal intraluminal projection is seen in this imaging study, the presence the appendix should first be confirmed to help narrow the differential of a polypoid lesion in this location.
Alternatively, a more aggressive approach may be pursued if the diagnosis remains uncertain. A simple biopsy of the mass with adequate sampling in combination with gross findings is an appropriate approach to rule out neoplasia. However, it may not be fully diagnostic of an AI because the histology of appendiceal tissue and colon are similar appearing [1]. If neoplasia is still a concern, resection is the appropriate next step in management. Reversal or resection of the AI should be avoided, as the lesion is benign and there is a high risk of peritonitis associated with surgical management [17].
References
- 1.Johnson E.K., Arcila M.E., Steele S.R. Appendiceal inversion: a diagnostic and therapeutic dilemma. JSLS. 2009;13(1):92–95. [PMC free article] [PubMed] [Google Scholar]; Johnson E.K., Arcila M.E., Steele S.R.. Appendiceal inversion: a diagnostic and therapeutic dilemma. JSLS. 2009;13(1):92–95. [PMC free article] [PubMed]
- 2.Waterland P., Khan F.S. The iatrogenic caecal polyp: can it be avoided? BMJ Case Rep. 2015;2015 doi: 10.1136/bcr-2015-209378. bcr2015209378. [DOI] [PMC free article] [PubMed] [Google Scholar]; Waterland P., Khan F.S.The iatrogenic caecal polyp: can it be avoided?BMJ Case Rep. 2015;2015:bcr2015209378. doi:10.1136/bcr-2015-209378. [DOI] [PMC free article] [PubMed]
- 3.Järvensivu P., Lehtola J., Karvonen A.L., Rinne A., Suramo I. Colonoscopic appearance of the remnant of the appendix after total inversion. Endoscopy. 1982;14:66–68. doi: 10.1055/s-2007-1021581. [DOI] [PubMed] [Google Scholar]; Järvensivu P., Lehtola J., Karvonen A.L., Rinne A., Suramo I.. Colonoscopic appearance of the remnant of the appendix after total inversion. Endoscopy. 1982;14. 66–8. 10.1055/s-2007-1021581. [DOI] [PubMed]
- 4.Voeller G.R., Fabian T.C. Inversion-ligation appendectomy for incidental appendectomy. Am J Surg. 1991;161(4):483–484. doi: 10.1016/0002-9610(91)91118-3. [DOI] [PubMed] [Google Scholar]; Voeller G.R., Fabian T.C.Inversion-ligation appendectomy for incidental appendectomy. Am J Surg. 1991;161(4):483–84 [DOI] [PubMed]
- 5.Engström L., Fenyö G. Appendicectomy: assessment of stump invagination versus simple ligation: a prospective, randomized trial. Br J Surg. 1985;72:971–972. doi: 10.1002/bjs.1800721212. [DOI] [PubMed] [Google Scholar]; Engström L., Fenyö G.. Appendicectomy: assessment of stump invagination versus simple ligation: a prospective, randomized trial. Br J Surg, 1985;72: 971–2. doi:10.1002/bjs.1800721212 [DOI] [PubMed]
- 6.Navarra G., Asopa V., Basaglia E., Jones M., Jiao L., Habib N. Mucous cystadenoma of the appendix: is it safe to remove it by a laparoscopic approach. Surg Endosc. 2003;17(5):833–834. doi: 10.1007/s00464-002-4266-6. [DOI] [PubMed] [Google Scholar]; Navarra G., Asopa V., Basaglia E., Jones M., Jiao L., Habib N.Mucous cystadenoma of the appendix: is it safe to remove it by a laparoscopic approach. Surg Endosc. 2003;17(5):833–4. [DOI] [PubMed]
- 7.Laalim S.A., Toughai I., Benjelloun E., Majdoub K.H.I., Mazaz K. Appendiceal intussusception to the cecum caused by mucocele of the appendix: Laparoscopic approach. Int J Surg Case Rep. 2012;3(9):445–447. doi: 10.1016/j.ijscr.2012.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]; Laalim S.A., Toughai I., Benjelloun E., Majdoub K.H.I., Mazaz K.. Appendiceal intussusception to the cecum caused by mucocele of the appendix: Laparoscopic approach. Int J Surg Case Rep. 2012;3(9):445–7. doi:10.1016/j.ijscr.2012.04.019. [DOI] [PMC free article] [PubMed]
- 8.Saleem A., Navarro P., Munson J.L., Hall J. Endometriosis of the appendix: report of three cases. Int J Surg Case Rep. 2011;2(2):16–19. doi: 10.1016/j.ijscr.2010.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]; Saleem A., Navarro P., Munson J.L., Hall J.. Endometriosis of the appendix: report of three cases. Int J Surg Case Rep. 2011;2(2):16–19. doi:10.1016/j.ijscr.2010.11.001. [DOI] [PMC free article] [PubMed]
- 9.Burchard P.R., Thomay A.A. Appendiceal intussusception in the setting of ulcerative colitis. J Surg Case Rep. 2018;2018(4) doi: 10.1093/jscr/rjy044. rjy044. [DOI] [PMC free article] [PubMed] [Google Scholar]; Burchard P.R., Thomay A.A.Appendiceal intussusception in the setting of ulcerative colitis. J Surg Case Rep. 2018;2018(4):rjy044. doi:10.1093/jscr/rjy044. [DOI] [PMC free article] [PubMed]
- 10.Yan S., Yeh Y., Lai M., Lee Y. Inverted appendix in an asymptomatic patient without intussusception or previous appendectomy. Colorectal Dis. 2010;12:e339–e340. doi: 10.1111/j.1463-1318.2010.02197.x. [DOI] [PubMed] [Google Scholar]; Yan S., Yeh Y., Lai M., Lee Y.. Inverted appendix in an asymptomatic patient without intussusception or previous appendectomy. Colorectal Dis, 2010:12: e339–40. doi:10.1111/j.1463-1318.2010.02197.x [DOI] [PubMed]
- 11.Holleman J.H., Jr, Sheffield T.E., Parker J.H., Jr, Martin B.F. Developmentally inverted appendix presenting as cecal polyp: case report. J Miss State Med Assoc. 1984;25(1(Jan)):7. [PubMed] [Google Scholar]; Holleman J.H. Jr, Sheffield T.E., Parker J.H. Jr, Martin B.F.. Developmentally inverted appendix presenting as cecal polyp: case report. J Miss State Med Assoc. 1984;25(1(Jan)):7. [PubMed]
- 12.Fazio R.A., Wickremesinghe P.C., Arsura E.L. Endoscopic removal of an intussuscepted appendix mimicking a polyp–an endoscopic hazard. Am J Gastroenterol. 1982;8:556–558. [PubMed] [Google Scholar]; Fazio R.A., Wickremesinghe P.C., Arsura E.L., et al. Endoscopic removal of an intussuscepted appendix mimicking a polyp–an endoscopic hazard, Am J Gastroenterol, 1982, 8:556–8. [PubMed]
- 13.Enander L.K., Gustavsson S. Colonoscopic appendectomy. Acta Chir Scand. 1979;145:575–576. [PubMed] [Google Scholar]; Enander L.K., Gustavsson S.. Colonoscopic appendectomy. Acta Chir Scand. 1979;145:575–6. [PubMed]
- 14.Saleem A., Navarro P., Munson J.L., Hall J. Endometriosis of the appendix: report of three cases. Int J Surg Case Rep. 2011;2(2):16–19. doi: 10.1016/j.ijscr.2010.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]; Saleem A., Navarro P., Munson J.L., Hall J.. Endometriosis of the appendix: report of three cases. Int J Surg Case Rep. 2011;2(2):16–19. doi:10.1016/j.ijscr.2010.11.001. [DOI] [PMC free article] [PubMed]
- 15.Pickhardt P.J., Levy A.D., Rohrmann C.A., Kende A.I. Primary neoplasms of the appendix: radiologic spectre of disease with pathologic correlation. Radiographics. 2003;23(3):645–662. doi: 10.1148/rg.233025134. [DOI] [PubMed] [Google Scholar]; Pickhardt P.J., Levy A.D., Rohrmann C.A., Kende A.I.. Primary neoplasms of the appendix: radiologic spectre of disease with pathologic correlation. Radiographics. 2003;23(3):645–62. https://doi.org/10.1148/rg.233025134 [DOI] [PubMed]
- 16.Janczak D., Szponder M., Janczak D., Lesniak M., Ziomek A., Chabowski M. Mucinous cystadenoma of the appendix—case report. Pol Przegl Chir. 2017;89(2):65–68. doi: 10.5604/01.3001.0009.9160. [DOI] [PubMed] [Google Scholar]; Janczak D., Szponder M., Janczak D., Lesniak M., Ziomek A., Chabowski M.. Mucinous cystadenoma of the appendix—case report. Pol Przegl Chir. 2017;89(2):65–68. [DOI] [PubMed]
- 17.Khawaja I.F. Diseases of the appendix recognized during colonoscopy. Saudi J Gastroenterol. 2002;8(2):43–52. [PubMed] [Google Scholar]; Khawaja I.F.Diseases of the appendix recognized during colonoscopy. Saudi J Gastroenterol. 2002;8(2):43–52. [PubMed]