Abstract
Purpose
Primary reconstruction via transconjunctival approach is a standardized treatment option for orbital floor fractures. The aim of this study was to compare the findings of specific ophthalmologic assessment with the patient's complaints after fracture reduction.
Methods
A retrospective medical chart analysis was performed on patients who had undergone transconjunctival orbital floor fracture reduction for fracture therapy with resorbable foil (ethisorb sheet or polydioxanone foil). A follow-up assessment including ophthalmological evaluation regarding visual acuity (eye chart projector), binocular visual field screening (Bagolini striated glasses test) and diplopia (cover test, Hess screen test) was conducted. Additionally, a questionnaire was performed to assess patients' satisfaction.
Results
A total of 53 patients with a mean follow-up of 23 months (ranging from 11 to 72) after surgical therapy were included. Diplopia was present preoperatively in 23 (43.4%) and reduced in follow-up examination (n = 12, 22.6%). Limitations in ocular motility reduced from 37.7% to 7.5%. The questionnaire about the patient's satisfaction revealed excellent outcomes in relation to the functional and esthetical parameters.
Conclusion
Transconjunctival approach is a safe approach for orbital fracture therapy. Postoperative diplopia is nearly never perceptible for the individual and differs to pathologic findings in the ophthalmic assessment.
Keywords: Orbital floor fractures, Blow out fractures, Transconjunctival approach, Clinical outcome
Introduction
Fractures of the orbital floor are often part of midfacial fractures or happen alone as a blow-out fracture.1 Several advances in imaging techniques such as high-resolution computed tomography (CT) and cone beam CT as well magnetic resonance imaging allow three-dimensional fracture analysis for better decision making regarding surgical intervention.2 The goal of surgical therapy is to relieve incarcerated tissue and/or cover the bony defect of the orbital floor with a resorbable implant or titanium mesh for greater defects to restore the orbital volume and the key area.3 Nowadays even patient specific implants are becoming increasingly popular, however long-term results are still missing in primary as well as secondary reconstruction.4 While different surgical approaches to the orbital floor are described such as subciliary, subtarsal and transconjunctival, the latter is without visible scarring and presents a low complication rate.5 The complications post-surgery vary in incidence and impact on patient's well-being. The incidence of ectropion can be decreased by using the transconjunctival approach instead of the subciliary approach.6 The most common complication after open reduction of orbital floor fractures is initial diplopia with a reported incidence of up to 86%.7, 8, 9 In most cases, this initial diplopia disappears after a few weeks but permanent subjective diplopia remains a complication with an incidence rate up to 10%.3, 10 Orbital dystopia as a long-term postoperative complication is common with an incidence of up to 27% and is regularly treated with a secondary surgery to revise the implant or to augment with another one.11 A rare complication is the orbital compartment syndrome which needs immediate therapy.12 The worst complication is the loss of vision due to the intervention and is reported up to 3.1%.13 Most of the aforementioned studies highlight the main postoperative symptoms, a focus on the patient's satisfaction is mainly lacking with only one relevant study existing to date.14 In the light of these findings, the aim of this study was to compare the findings of specific ophthalmologic assessment with the patient's complaints after transconjunctival fracture reduction of the orbital floor.
Methods
This was a retrospective cohort study with clinical follow up assessment in orbital floor fracture patients who received transconjunctival fracture reduction using resorbable membranes. The study was performed in accordance with the Declaration of Helsinki and approved by the institutional committee on research ethics (approval certificate no. EA4/146/16).
Study variables
The primary outcome was diplopia and ocular movement before and after surgery in the follow-up. Secondary outcomes included ectropion, entropion, infraorbital dysesthesia and patients' satisfaction with function and esthetic.
Study population
All patients who were treated with transconjunctival fracture reduction for repair of orbital floor fracture in the Department of Maxillofacial surgery at the University Hospital Charité - Universitätsmedizin Berlin, Campus Virchow, in a period of 48 months were enrolled in this study. The indications for surgical therapy were the combination of radiologic findings of orbital floor fractures and the symptoms of diplopia which did not resolve.
Data collection
The following demographic and laboratory data were obtained from the medical charts from all participants: age, gender, etiology of trauma, fracture type, preoperative symptoms, operative procedure and general diseases.
Follow-up
All patients were summoned for a follow-up examination consisting of three separate stages. The first stage was an interview evaluating the patient's subjective limitations in relation to the performed orbital surgery. Three techniques were applied during the interview: yes-no questions, forced-choice questions and a verbal rating scale. The rating scale was used to measure the subject's opinion on functional and esthetic results of the operation using a visual analogue scale from “1” to “6” - “1” was used to describe excellent results and “6” the worst possible results. Patients were also asked to state if they perceived double vision and if it interfered with their daily activities. Interviews were performed before the ophthalmic exams in order to prevent patients from giving biased answers.
The second stage was clinical examination, entailing palpatory inspection of periorbital bony edges, assessment of entropion/ectropion, scarring, enophthalmos/exophthalmos, hypophthalmos and blunt and sharp sensory deficiency of N. infraorbitalis. Vertical eye displacement was determined using photographs taken during examination.
An orthoptic assessment was performed afterwards regarding visual acuity (eye chart projector), binocular visual field screening (Bagolini striated glasses test) and diplopia (cover test, Hess screen test).
Study design
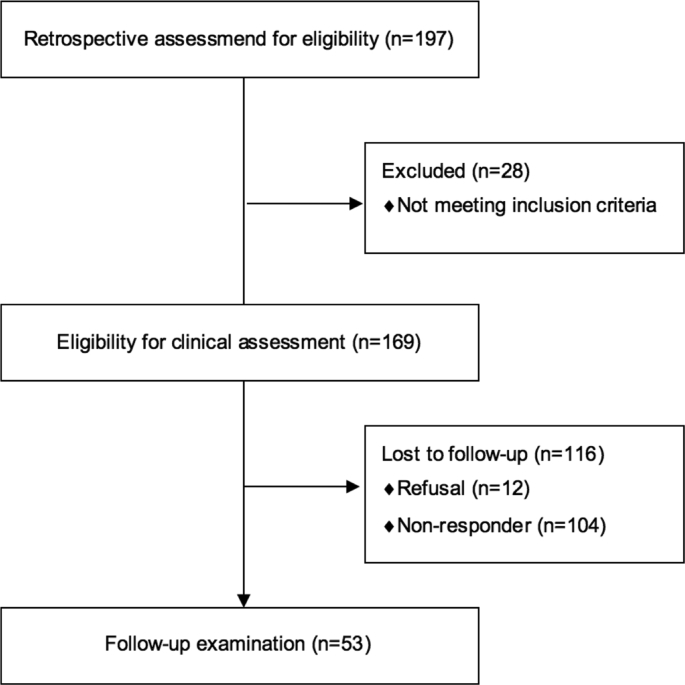
Fig. 1 shows the flow chart of the study.
Fig. 1.
Flow-chart of the study.
Statistical analysis
Categorical data were described by absolute and relative frequencies. Differences in distribution were analysed using Pearson's chi-squared test or McNemar's test. Data showing Gaussian distribution were presented as mean and standard deviation, whereas data lacking Gaussian distribution were presented as median and interquartile range. Due to the exploratory nature of the retrospective study without peer group, an alpha-error correction was not used. All p-value information is descriptive and p < 0.05 was considered significant. Data were analysed using SPSS v22 (IBM Corp, Armonk, NY, USA).
Results
Demographics and etiology
A total of 169 patients were eligible for clinical assessment. The patients' median age was 36 years (ranged from 6 to 90 years). Gender distribution was 116 males and 53 females (ratio 2.2:1). There were significantly (p < 0.001) more fractures with dislocation (87.6%, n = 148). The etiology of the fractures is given in Fig. 2.
Fig. 2.
Etiology of the fractures.
The surgical intervention took place in median at the third day after trauma and the transconjunctival approach was used to gain access to the orbital floor in all patients. The materials for covering the defect were Ethisorb® patches (Ethicon, Norderstedt, Germany) in 13.2% of the cases and polydioxanone foils (PDS, Ethicon, Norderstedt, Germany) in 86.8% of the cases. The median follow-up interval was 23 months (range: 11–72 months). The return rate was 31.4% (n = 53).
Diplopia
Diplopia was present preoperatively in 23 (43.4%) of the followed-up patients and proved significantly (p = 0.019, McNemar's Test) reduced in follow-up examination after surgery (n = 12, 22.6%), although 7% (n = 4) patients had diplopia as a new symptom after surgery.
Orthoptic follow-up examination showed that of the 8 (15.1%) patients with pre- and postoperative diplopia, only 5 noticed the double vision and all 8 patients felt that their symptoms had subjectively improved. None of the 4 patients with diplopia first present postoperatively noticed the double vision on their own.
Ocular motility
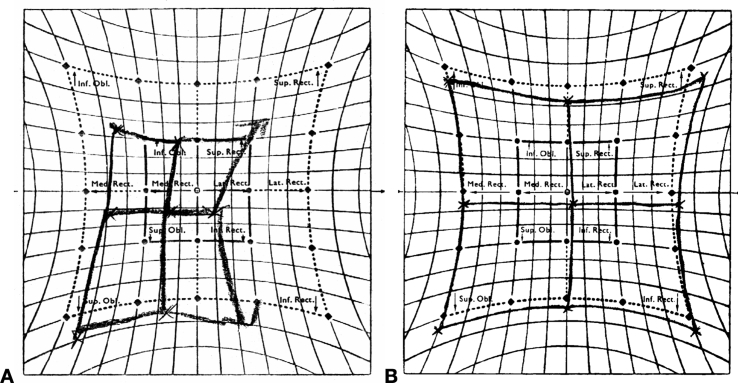
Limitations in ocular motility were present in 20 (37.7%) of 53 patients during preoperative examination, of which 16 (80%) also had preoperative diplopia. Follow-up revealed that only 4 (7.5%) retained limited eye movement and McNemar's Test showed significant postoperative improvement of ocular motility (p = 0.027). A Hess screen test demonstrating restricted preoperative ocular motility and postoperative resolution is given in Fig. 3. However, 5 of 53 (9.4%) patients developed new motility restrictions after surgery resulting in a total of 9 (17%) patients with deficient ocular motility.
Fig. 3.
Hess screen example of a patient with preoperative ocular motility restrictions of the right globe. (A) Underaction of the right rectus lateralis muscle and the superior rectus muscle due to entrapment of the globe; (B) Nearly normalized movement of the same patient post-surgery.
Orbital displacement
A significant association could be established between postoperative vertical dystopia like downward displacement of the eye and the occurrence of diplopia as well as limited ocular motility using the chi-squared test (p < 0.001). Downward displacement of the bulb was diagnosed in 12 of 53 (22.6%) patients, all of which exhibited diplopia and 8 (66.7%) also presented with reduced ocular motility. The chi-squared test showed that there was no significant relationship between eye displacement and the type of fracture (p = 0.906).
Membrane material
We observed no significant difference between the used materials (Ethisorp patches or polydioxanone foil) during the orbital floor surgery in the matter of occurrence of postoperative diplopia (p = 0.076) or downward displacement of the eye (p = 0.809).
Time of surgery
Results showed a significant improvement of postoperative diplopia (p = 0.039) and ocular motility (p = 0.022) when surgical intervention took place shortly after trauma within the first three days.
Malposition of the eyelid
There was no sign of postoperative ectropion or entropion in any of the followed-up patients.
Sensitivity
Sensitivity of the infraorbital nerve was impaired in 69.8% (n = 37) of patients prior to surgery with 49.1% (n = 26) exhibiting deficient sensitivity during follow-up examination. Statistical analysis using McNemar's Test showed a significant improvement in sensitivity (p = 0.043) and 7 of these 26 patients displayed sensory disturbances only after surgery.
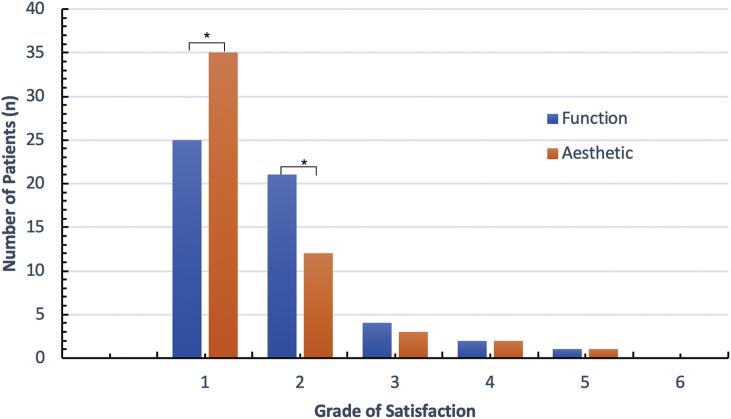
Patient's satisfaction
The chi-squared test showed that the majority of patients were satisfied with the postoperative results with 86,8% assigning grades “1” and “2” in functional outcome and 88.7% grades “1” and “2” in esthetic outcome (p < 0,001). Detailed results are given in Fig. 4. A total of 13 (24.5%) of the followed-up subjects exhibited postoperative deficits in the shape of diplopia or limited ocular motility, 8 of which suffered from both symptoms (61.5%), 4 (30.8%) showed only diplopia and 1 (7.7%) showed only reduced ocular motility. Subjective assessment by these patients is given in Fig. 5.
Fig. 4.
Subjective assessment of postoperative functional and esthetic results by followed-up patients (n = 53) in a grading system with 1 = excellent results to 6 = the worst possible results. Absolute values. *p < 0.001.
Fig. 5.
Subjective assessment of postoperative functional and esthetic results by followed-up patients with postoperative deficits (n = 13) in a grading system with 1 = excellent results to 6 = the worst possible results. Absolute values.
Discussion
Demographics and etiology
The patient collective of this study is similar to other studies, with orbital floor fractures occurring mainly in men and patients between 20 and 40 years of age.3, 15 Interpersonal violence was the main cause of injury, which is in line with several other studies.15, 16
Diplopia
In our study, diplopia was present preoperatively in 43.4% of patients and persisted with 22.6% patients. It was the second most common symptom of orbital floor fractures in our patient collective. Liu et al.17 found an incidence of 50% after 6 months, Brucoli et al.8 42.5% after 39 months, Ramphul and Hoffmann3 19.8% after 6 months and Lee et al.18 21.6% after 12 months. A better outcome can be explained by a less intensive assessment: several studies did not make use of specific ophthalmologic diagnostics and asked patients for subjective perception of double vision or performed a confrontation visual field test with a finger or a pencil.15, 19 If we discount the cases of postoperative diplopia not noticed by the patients in our study, we can report an incidence of postoperative diplopia of about 13.2%. Bartoli et al.20 also examined combined fractures of the zygomatic complex and found that diplopia occurred in 20.2% and persisted with 16.4% of patients at the 6-month follow-up, which is comparable with our postoperative diplopia incidence of 22.6% at follow-up examination. Of the 22.6% patients in our study with persistent diplopia, 8 displayed diplopia preoperatively and reported improved symptoms, 3 did not notice the double vision and 4 patients whose diplopia developed postoperatively did not know they suffered from diplopia prior to ophthalmic examination (detection only by ophthalmologic assessment).
Ocular motility
The follow-up revealed that 20% of our patients still suffered from limited eye movement and McNemar's Test showed significant postoperative improvement of ocular motility (p = 0.027). Besides the fact that many studies differ in the depth of assessment of extraocular muscle movement and present different results, the general trend of improving movement over time is evident. For example, the study of Liu et al.17 presents a decline in movement restrictions from 53.3% one month postoperatively to 16.3% after 6 months. The study of Kasaee et al.15 found a decrease of movement restriction from 31.1% one month after surgery to 6.1% after 6 months.
The majority of our patients (80%) with postoperative reduced movement had preoperative motility restrictions. However 9.4% patients developed new motility restrictions after surgery resulting in a total of 17% patients with deficient ocular motility. These results are confirmed by the work of Ramphul and Hoffman3 who found that the presence of preoperative diplopia is statistically associated with postoperative decline in ocular movement. Remarkable is the fact that none of our patients subjectively perceived any limitations in eye movement prior to the follow-up examination.
Orbital displacement
In the present study, displacement of the bulb was diagnosed in 22.6% patients, which is concordant to other studies reporting incidences of enophthalmos following surgical repair from 7% to 27%.8, 9, 21
Time of surgery
The timing of the operation is a controversial topic. Our results showed a significant improvement of postoperative diplopia (p = 0.039) and ocular motility (p = 0.022) when surgical intervention took place shortly after trauma within the first three days.
Other studies had similar results regarding the influence of time to surgery: e. g. Kasaee et al.15 recommend surgery within 4.5 days after trauma. Other studies prefer longer intervals like Poeschl et al.22 who suggest a waiting time of 7 days or Brucoli et al.8 who recommend a surgical intervention within the first 2 weeks. Summarizing, a meta-analysis of Damgaard et al.23 presented a better outcome for diplopia with surgery within the first 2 weeks.
Membrane material
As we found no significant correlation between the used material and the presence of diplopia other studies presented similar results. Polydioxanone as the most used material in our study was also evaluated in the study of Beck-Broichsitter et al.24 and presented no correlation to long-term complications. Similar results were presented with ethisorb patches – which are used off-label - as covering material in the study of Jank et al.25 and Blake et al.26 A recent study from Ramphul and Hoffmann3 found no significant association of other used materials (titanium mesh, Medpor, a combination of Medpor and mesh, and gelatin film) and diplopia in their study, too. Compared to titanium implants our results showed a slightly better outcome ranging between 24.6 and 29.8%.27
Malposition of the eyelid
As we found no malposition of the eyelid in our study, other investigations confirmed these results.6, 28 Further studies presented different results: the study of Pausch et al.29 showed a higher risk for entropion using the transconjunctival approach compared to a subciliary incision. The group of Strobel5 found no differences between the two approaches in the non-expert and expert assessment groups.
Sensitivity
The major symptoms of our cohort were sensory disturbances of the infraorbital nerve with 69.8% (n = 37) prior to surgery and a decrease to 49.1% (n = 26) at follow-up examination.
Although statistical analysis showed a significant improvement in sensitivity (p = 0.043), complete resolution of the nerve dysfunction is often not possible and explains the high grade of dysfunction after surgery. Our results are conform with other studies who presented hypesthesia/dysesthesia up to 55%.8, 20
Patient's satisfaction
Many studies in the field of orbital floor fracture therapy are available, yet an assessment of the patient's satisfaction is hard to find. The study of Holtmann et al.30 asked for contentedness in relation to foreign body sensation, diplopia, en- and exophthalmos and showed high contentedness in the cohort. In the study of Bartoli et al.20 the complaints about the scarring were named but a general questionnaire was not performed. In the retrospective study of Poeschl et al.22 with 60 patients included, the complaint of one patient about ectropion was noted but a general questionnaire was not performed. In our study the assessment of patient's compliants with a questionnaire revealed an interesting difference between the perception of subjective discomfort and objective findings in the ophtalmologic verification.
Limitations
The retrospective design of our study is one limitation leading to a relatively small sample size due to inconsistent follow-up assessment and different times of assessment. To the best of our knowledge, this study was the first which assess the patient's subjective satisfaction in relation to the objective functional and esthetic outcome.
Conclusion
Within the limitations of the present study, it can be concluded that the transconjunctival approach is a safe way to gain access to the orbit for fracture therapy. It should be pointed out, despite the good postoperative results, that some patients developed diplopia only postoperatively and that an existing hypesthesia could only be improved in the minority of the patients. Therefore, the indication even for minimal invasive orbital surgery should remain strict. Finally, the comparability of ophthalmological symptoms between studies is complicated by a non-uniform assessment. Here, a standardized procedure for future comparisons would be desirable.
Funding
Nil.
Acknowledgements
The present study is included in the doctoral thesis of Britta Ciesla.
Footnotes
Peer review under responsibility of Chinese Medical Association.
Ethical statement
The study was performed in accordance with the Declaration of Helsinki and approved by the institutional committee on research ethics (approval certificate no. EA4/146/16).
Conflicts of interest
The authors state that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this article. All authors have viewed and agreed to the submission.
References
- 1.Roccia F., Savoini M., Ramieri G. An analysis of 711 victims of interpersonal violence to the face, Turin, Italy. J Cranio-Maxillo-Fac Surg. 2016;44:1025–1028. doi: 10.1016/j.jcms.2016.05.021. [DOI] [PubMed] [Google Scholar]
- 2.Marinho R.O., Freire-Maia B. Management of fractures of the zygomaticomaxillary complex. Oral Maxillofac Surg Clin. 2013;25:617–636. doi: 10.1016/j.coms.2013.07.011. [DOI] [PubMed] [Google Scholar]
- 3.Ramphul A., Hoffman G. Does preoperative diplopia determine the incidence of postoperative diplopia after repair of orbital floor fracture? An institutional review. J Oral Maxillofac Surg. 2017;75:565–575. doi: 10.1016/j.joms.2016.10.036. [DOI] [PubMed] [Google Scholar]
- 4.Raisian S., Fallahi H.R., Khiabani K.S. Customized titanium mesh based on the 3D printed model vs. Manual intraoperative bending of titanium mesh for reconstructing of orbital bone fracture: a randomized clinical trial. Rev Recent Clin Trials. 2017;12:154–158. doi: 10.2174/1574887112666170821165206. [DOI] [PubMed] [Google Scholar]
- 5.Strobel L., Hölzle F., Riediger D. Subtarsal versus transconjunctival approach-esthetic and functional long-term experience. J Oral Maxillofac Surg. 2016;74:2230–2238. doi: 10.1016/j.joms.2016.06.181. [DOI] [PubMed] [Google Scholar]
- 6.Raschke G., Rieger U., Bader R.D. Outcomes analysis of eyelid deformities using photograph-assisted standardized anthropometry in 311 patients after orbital fracture treatment. J Trauma Acute Care Surg. 2012;73:1319–1325. doi: 10.1097/TA.0b013e318265cc92. [DOI] [PubMed] [Google Scholar]
- 7.Biesman B.S., Hornblass A., Lisman R. Diplopia after surgical repair of orbital floor fractures. Ophthalmic Plast Reconstr Surg. 1996;12:9–16. doi: 10.1097/00002341-199603000-00002. Discussion 17. [DOI] [PubMed] [Google Scholar]
- 8.Brucoli M., Arcuri F., Cavenaghi R. Analysis of complications after surgical repair of orbital fractures. J Craniofac Surg. 2011;22:1387–1390. doi: 10.1097/SCS.0b013e31821cc317. [DOI] [PubMed] [Google Scholar]
- 9.Hoşal B.M., Beatty R.L. Diplopia and enophthalmos after surgical repair of blowout fracture. Orbit. 2002;21:27–33. doi: 10.1076/orbi.21.1.27.2598. [DOI] [PubMed] [Google Scholar]
- 10.Balaji S.M. Residual diplopia in treated orbital bone fractures. Ann Maxillofac Surg. 2013;3:40–45. doi: 10.4103/2231-0746.110078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tarsitano A., Badiali G., Pizzigallo A. Orbital reconstruction: patient-specific orbital floor reconstruction using a mirroring technique and a customized titanium mesh. J Craniofac Surg. 2016;27:1822–1825. doi: 10.1097/SCS.0000000000002907. [DOI] [PubMed] [Google Scholar]
- 12.Voss J.O., Hartwig S., Doll C. The “tight orbit”: incidence and management of the orbital compartment syndrome. J Cranio-Maxillofacial Surg. 2016;44:1008–1014. doi: 10.1016/j.jcms.2016.05.015. [DOI] [PubMed] [Google Scholar]
- 13.Gosau M., Schöneich M., Draenert F.G. Retrospective analysis of orbital floor fractures--complications, outcome, and review of literature. Clin Oral Investig. 2011;15:305–313. doi: 10.1007/s00784-010-0385-y. [DOI] [PubMed] [Google Scholar]
- 14.Safi A.F., Richter M.T., Rothamel D. Influence of the volume of soft tissue herniation on clinical symptoms of patients with orbital floor fractures. J Cranio-Maxillo-Fac Surg. 2016;44:1929–1934. doi: 10.1016/j.jcms.2016.09.004. [DOI] [PubMed] [Google Scholar]
- 15.Kasaee A., Mirmohammadsadeghi A., Kazemnezhad F. The predictive factors of diplopia and extraocular movement limitations in isolated pure blow-out fracture. J Curr Ophthalmol. 2017;29:54–58. doi: 10.1016/j.joco.2016.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Higashino T., Hirabayashi S., Eguchi T. Straightforward factors for predicting the prognosis of blow-out fractures. J Craniofac Surg. 2011;22:1210–1214. doi: 10.1097/SCS.0b013e31821c0d13. [DOI] [PubMed] [Google Scholar]
- 17.Liu S.R., Song X.F., Li Z.K. Postoperative improvement of diplopia and extraocular muscle movement in patients with reconstructive surgeries for orbital floor fractures. J Craniofac Surg. 2016;27:2043–2049. doi: 10.1097/SCS.0000000000003192. [DOI] [PubMed] [Google Scholar]
- 18.Lee S.C., Park S.H., Han S.K. Prognostic factors of orbital fractures with muscle incarceration. Arch Plast Surg. 2017;44:407–412. doi: 10.5999/aps.2017.44.5.407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Anand L., Sealey C. Orbital fractures treated in Auckland from 2010-2015: review of patient outcomes. N Z Med J. 2017;130:21–26. [PubMed] [Google Scholar]
- 20.Bartoli D., Fadda M.T., Battisti A. Retrospective analysis of 301 patients with orbital floor fracture. J Cranio-Maxillo-Fac Surg. 2015;43:244–247. doi: 10.1016/j.jcms.2014.11.015. [DOI] [PubMed] [Google Scholar]
- 21.Chi M.J., Ku M., Shin K.H. An analysis of 733 surgically treated blowout fractures. Ophthalmolqica. 2010;224:167–175. doi: 10.1159/000238932. [DOI] [PubMed] [Google Scholar]
- 22.Poeschl P.W., Baumann A., Dorner G. Functional outcome after surgical treatment of orbital floor fractures. Clin Oral Investig. 2012;16:1297–1303. doi: 10.1007/s00784-011-0609-9. [DOI] [PubMed] [Google Scholar]
- 23.Damgaard O.E., Larsen C.G., Felding U.A. Surgical timing of the orbital “blowout” fracture: a systematic review and meta-analysis. Otolaryngol Head Neck Surg. 2016;155:387–390. doi: 10.1177/0194599816647943. [DOI] [PubMed] [Google Scholar]
- 24.Beck-Broichsitter B.E., Acar C., Kandzia C. Reconstruction of the orbital floor with polydioxanone: a long-term clinical survey of up to 12 years. Br J Oral Maxillofac Surg. 2015;53:736–740. doi: 10.1016/j.bjoms.2015.05.010. [DOI] [PubMed] [Google Scholar]
- 25.Jank S., Emshoff R., Schuchter B. Orbital floor reconstruction with flexible Ethisorb patches: a retrospective long-term follow-up study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;95:16–22. doi: 10.1067/moe.2003.11. [DOI] [PubMed] [Google Scholar]
- 26.Blake F., Blessmann M., Smeets R. Long-term follow-up of blowout fractures of the orbital floor reconstructed with a polyglactin 910/PDS implant. Eur J Trauma Emerg Surg. 2011;37:609–613. doi: 10.1007/s00068-011-0081-x. [DOI] [PubMed] [Google Scholar]
- 27.Zimmerer R.M., Ellis E., 3rd, Aniceto G.S. A prospective multicenter study to compare the precision of posttraumatic internal orbital reconstruction with standard preformed and individualized orbital implants. J Cranio-Maxillo-Fac Surg. 2016;44:1485–1497. doi: 10.1016/j.jcms.2016.07.014. [DOI] [PubMed] [Google Scholar]
- 28.Yoon S.H., Lee J.H. The reliability of the transconjunctival approach for orbital exposure: measurement of positional changes in the lower eyelid. Arch Craniofacial Surg. 2017;18:249–254. doi: 10.7181/acfs.2017.18.4.249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pausch N.C., Sirintawat N., Wagner R. Lower eyelid complications associated with transconjunctival versus subciliary approaches to orbital floor fractures. Oral Maxillofac Surg. 2016;20:51–55. doi: 10.1007/s10006-015-0526-1. [DOI] [PubMed] [Google Scholar]
- 30.Holtmann H., Eren H., Sander K. Orbital floor fractures--short- and intermediate-term complications depending on treatment procedures. Head Face Med. 2016;12:1. doi: 10.1186/s13005-015-0096-3. [DOI] [PMC free article] [PubMed] [Google Scholar]