Abstract
Prune Belly syndrome occurs in 1/40,000 live births and predominantly in males. It is characterized by triad: cryptorchidism, abdominal wall, and urinary tract abnormalities. Patients with partial or unilateral abdominal wall deficiency, unilateral undescended testis, and female neonates with abdominal wall laxity are classified as Pseudo Prune Belly syndrome. In the 3%–5% of patients with Prune Belly syndrome are affected by Pseudo Prune Belly syndrome, indeed case reports available are very few. We described a case of a male patient born with a large abdominal hernia. Thoracoabdominal X-ray confirmed the large abdominal hernia and revealed a malformation of the rib cage with curved ribs. Magnetic resonance imaging showed thinning of the abdominal wall and ultrasonography detected rectus and oblique muscles hypoplastic with diastasis rectus muscles and stretching of the Hunter's line. Cryptorchidism or urinary tract abnormalities were not detected. The first surgical operation was performed at 2 years of life when the general conditions were stable.
Keywords: Newborn, Diastasis recti, Pseudo Prune Belly
Introduction
Prune Belly syndrome (PBS), or Eagle-Barrett syndrome, is a rare congenital disorder that occurs in 1/40,000 live births and over 95% in male patients. In literature are reported less than 30 cases of PBS in female patients [1]. The etiology of PBS is unknown but is characterized by triad: cryptorchidism, abdominal wall, and urinary tract abnormalities [2]. Patients with partial or unilateral abdominal wall deficiency, unilateral undescended testis, and female neonates with abdominal wall laxity are classified as Pseudo Prune Belly syndrome (PPBS). The term “prune-belly” reflects the characteristic wrinkled appearance of the abdominal wall in the newborn due to the complete or partial absence of abdominal wall muscles. Clinical manifestations are very variable with renal or respiratory severe dysplasia and that can be cause of fetal mortality. The severity of renal dysplasia is the main prognostic factor. They have reported also cases of PBS with good physical and mental health conditions [3], [4]. Diagnosis of PBS is clinical and radiological investigations show only the extent of renal dysplasia and/or renal disfunction [5]. Only 3%–5% of patients with PBS are affected by PPBS, indeed case reports available are very few [6]. We describe a male newborn with unilateral abdominal wall deficiency. Diagnosis of PPBS was confirmed by ultrasonography (US) and magnetic resonance imaging (MRI) of the abdominal wall.
Case report
During pregnancy at 20 weeks of gestational age, health care providers detected polyhydramnios and pyelectasis. Furthermore, a large umbilical hernia was revealed by 3D ultrasonography GE Voluson E8 and it was suspected the omphalocele (Fig. 1). The amniocentesis was executed to analyze amniotic fluid, but the karyotype of the fetus was normal (46, XY). Parents were not nonconsanguineous. The woman was hospitalized in III level hospital due to the high risk of premature birth. Baby was born at 37 +5/7 weeks of gestational age by vaginal delivery. Apgar score was 5I and 6V while body weight, length, and head circumference were 3000 g, 48 cm, and 34 cm, respectively. Newborn was intubated and assisted with mechanical ventilation due to respiratory distress during the first 30 days of life. A large abdominal hernia was also observed (Fig. 2A). The infant showed a loose not hyperelastic skin, wrinkled at the root of the limbs, micrognathia, blepharophimosis, low-set ears with hypoplastic pavilions and ante-rotated ear lobes, the left lobe with dimples overlying The ophthalmologic examination and the US of the heart, kidney, brain, and diaphragm were normal. The thoracoabdominal X-ray revealed a malformation of the rib cage with curved ribs (Fig. 2B). MRI confirmed abdominal hernia (Fig. 3) and showed thinning of the abdominal wall (Fig. 4A) while the US detected the hypoplasia of the rectus and oblique muscles and diastasis recti with stretching of the Hunter's line (Fig. 4B). US allowed to plan a surgical operation of abdominoplastic without the need to implant an abdominal prosthesis. These clinical signs were considered attributable to a case of PPBS. At 5 months of life, the infant clinical conditions became stable. He was fed with nasogastric tube and gained body weight but appeared a right inguinal hernia (Fig. 5 A,B), therefore it was decided to postpone the surgical operation. Surgical operation was performed at 2 years of life but to reduce respiratory complications only the upper abdomen and inguinal hernia were closed (Fig. 6). Motor and language therapy were started to improve his ability to walk and play. Lower abdomen will be closed after the stabilization of his general conditions. Nowadays, the infant can be fed without medical device and has a good quality of life.
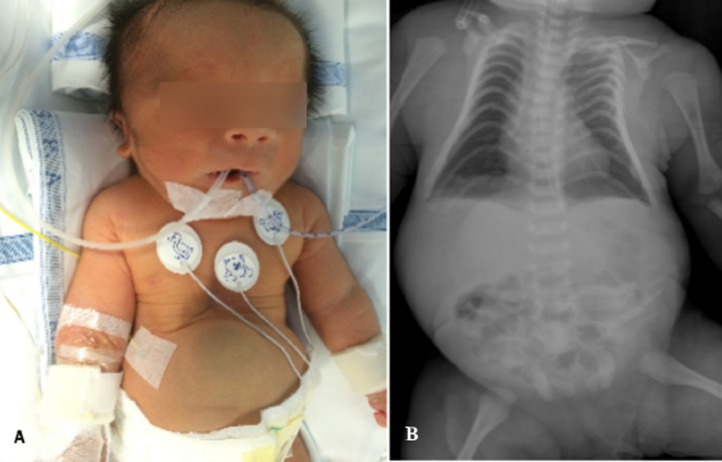
Fig. 1.
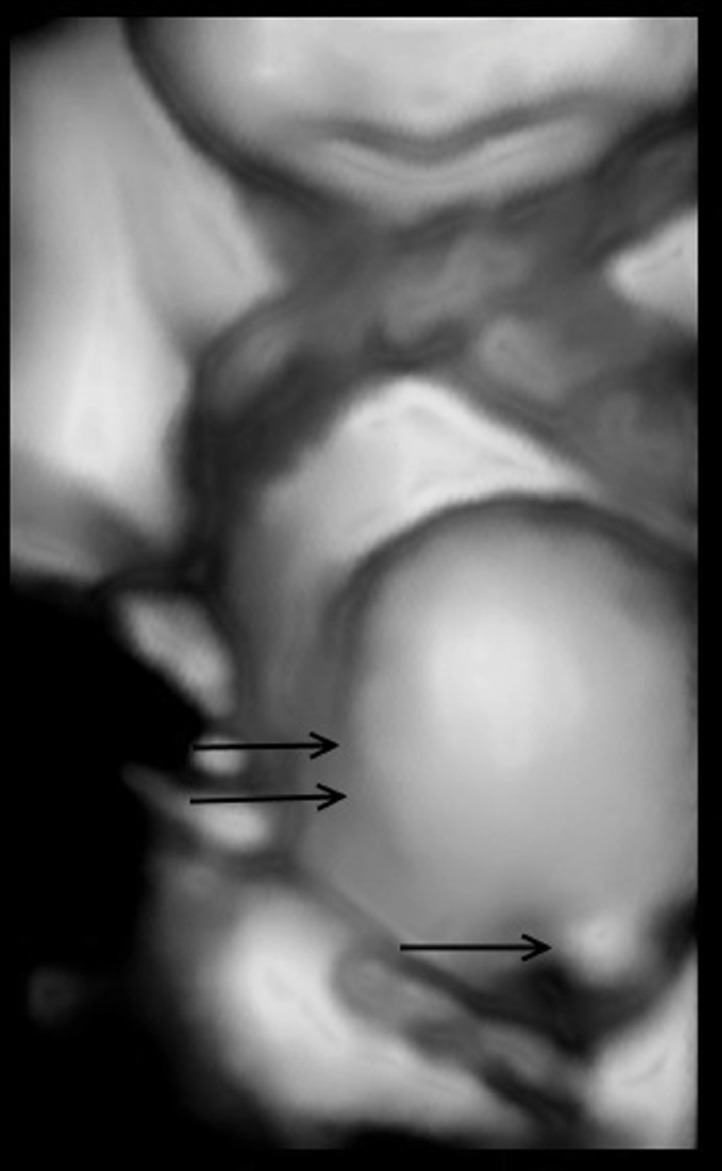
3D ultrasonography showed an umbilical hernia (one arrow) and the abdominal hernia (two arrows) that was wrongly evaluated as omphalocele.
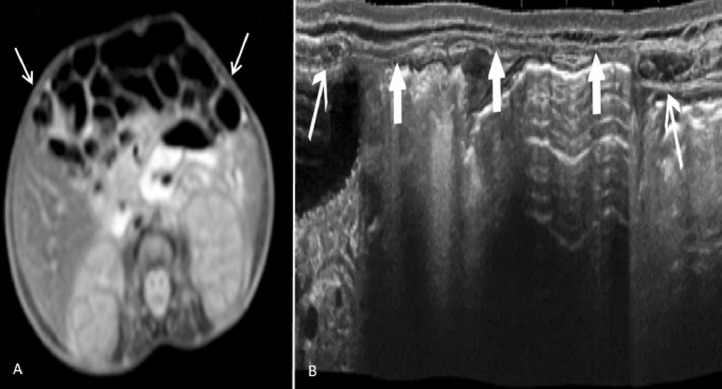
Fig. 2.
(A) The large abdominal hernia was noted on clinical examination and (B) the malformation of the rib cage was detected by thoracoabdominal X-ray.
Fig. 3.
T2-wighted MRI showed abdominal hernia (one arrow).
Fig. 4.
(A) T2-wighted MRI showed significant thinning of the abdominal wall (one arrow). (B) Ultrasonography (longview reconstruction) detected diastasis of the rectus muscles (thin long arrow) with stretching of the Hunter's line (thick arrow).
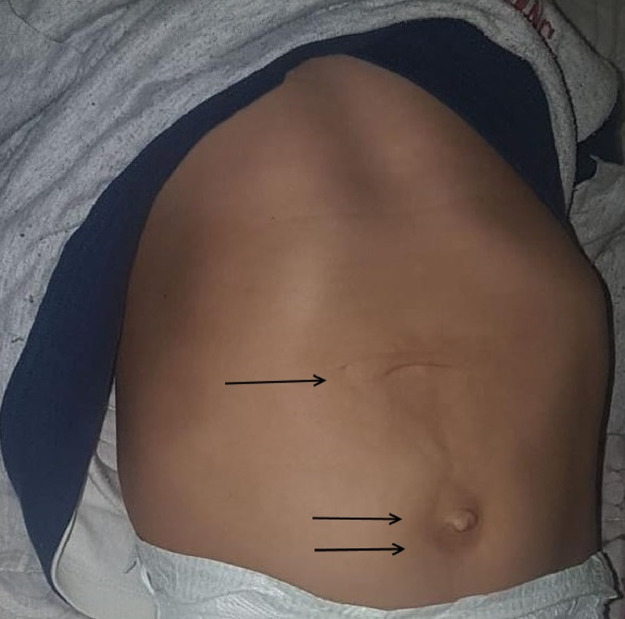
Fig. 5.
(A, B) The infant breathed without mechanical ventilation, fed with nasogastric tube. (A) When baby cried, abdominal hernia (two arrows) and inguinal hernia (one arrow) were more prominent. (B) When the nurse used a pacifier to calm the newborn, abdominal hernia (two arrows) and inguinal hernia (one arrow) were less prominent.
Fig. 6.
After the first surgical operation, upper abdomen was closed (one arrow) but lower abdomen still showed abdominal and umbilical hernia (two arrows).
Discussion and conclusion
The etiology of PBS remains unclear, it does not seem to have a genetic basis. However, this syndrome is predominant in male patients and suggests a possible genetic basis with autosomal recessive inheritance linked to sex [7]. The involvement of family factors as inbreeding is hypothesized and it is not uncommon in patients with PBS [3]. The origin of the malformations is also not clear. The origin of the malformations is also not clear. A possible explanation is the presence of the prenatal obstruction of the urinary tract which leads to dilation of the urinary tract and abdominal distension in the foetus. Abdominal distention leads to altered abdominal wall muscles resulting in hypoplasia [1]. A different explanation is that at the base there is an alteration of the mesodermal development due to the defective migration. Otherwise, the cause is the differentiation of the lateral mesoderm between the sixth and tenth week of gestation in the abdominal musculature or in the muscles of the urinary tract [1], [2], [3], [4]. The prognosis of the syndrome depends on renal dysplasia. They have been reported cases associated with oligoanuria due to a very severe renal dysplasia and other cases with a renal dysplasia that determined a progressive renal insufficiency or a minimal renal alteration with a favorable prognosis [4]. The presentation of cryptorchidism is also varied. More severe forms were observed in association with a state of testicular agenesis and in which the testicles were formed but there was a subsequent alteration of the migration with a failed positioning at the level of the scrotal sac [6]. It is possible in some cases to observe the association of the classic triad with anomalies in other districts. Routh et al performed a study on 133 newborns and found in 58% of the cases the presence of pulmonary abnormalities that can be explained by oligodramnios [8]. Cardiac, gastrointestinal, and skeletal abnormalities were reported between 23% and 25% of cases [9]. The diagnosis of PBS is prenatal using routine US. The characteristics of the syndrome can be diagnosed as early as 12 weeks of gestation [10]. If the diagnosis is not performed ultrasonographically at the prenatal level, it is performed clinically after birth. The therapy is not unique, depends on the patient's starting conditions. Surgical treatment includes abdominoplasty, bilateral orchiopessia, and treatment of urinary anomalies. The surgical approach is generally undertaken at the patient's first life year [10]. There is a variant of the syndrome known as PPBS. PPBS is generally characterized by partial or unilateral abdominal wall deficiency or unilateral undescended testis that can usually be palpable in the inguinal canal. Chan and Bird reported a case report with vertical transmission and isolated abdominal defect, while Digilio et al described a case of diastasis recti and weakness of the line alba with vertical transmission [11], [12]. Shoshany et al [13] also described the possible presence of an accessory scrotum. Renal dysplasia is described in about a quarter of affected patients [6]. Ureteral bladder reflux is present in almost 75% of patients. The position of the navel may be abnormal. Gastrointestinal abnormalities are also common. Olori et al [14] reported a case of PPBS and microcolon. Arterial hypertension is also frequent, and it often requires starting drugs like hydralazine. The diagnosis of PBS or PPBS is based on the clinical suspicion that must be postulated considering the multiple variability of presentation of the syndrome. US assessment must be performed as the first instrumental examination to assess renal impairment. The diagnostic evaluation is then completed with MRI [15]. In addition to instrumental examinations, it is possible to assess the progress of renal function through creatinine monitoring. Levels of creatinine above 7 mg/l are often associated with worsening renal function. The prognosis in these patients is conditioned by renal function and the risk of urinary septicemia. Surgery involves reconstruction of the abdominal wall with the possible reconstruction of the urinary system. Our patient is case of PPBS, which can be considered as a possible variant of the syndrome. The component of renal anomaly was missing as confirmed by US. However, US allowed to consider a less invasive surgical operation revealing hypoplasia of rectus muscles and diastasis recti. Our patient was subjected to a first phase of surgical intervention that allowed to close upper abdomen and right inguinal hernia. As reported in literature, the absence of renal alterations was associated with a good prognosis. The important abdominal impairment caused a respiratory alteration, indeed it required an invasive and then noninvasive type of ventilatory support for a total of 30 days. In consideration of the present literature, our patient was clinically considered affected by PPBS. The first surgical operation was performed at 2 years of life when the general conditions were stable, and the body weight was adequate. Currently, the patient is 3 years old and a second abdominal plastic surgery is planned. Our case wants to emphasize that we should not talk about PBS only in the presence of the classic triad and moreover its variants can present more nuanced symptoms and signs. These variants must be recognized to be managed both internalistically and surgically.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.radcr.2019.05.019.
Appendix. Supplementary materials
References
- 1.Fette A. Associated rare anomalies in prune belly syndrome: a case report. J Ped Surg Case Reports. 2015;3:65–71. [Google Scholar]; Fette A.Associated rare anomalies in prune belly syndrome: a case report. J Ped Surg Case Reports3 (2015); 65–71
- 2.Grover H., Sethi S., Garg J., Ahluwalia A.P. Pseudo prune belly syndrome: diagnosis by imaging- a case report and brief review. Pol J Radiol. 2017;82:252–257. doi: 10.12659/PJR.899743. [DOI] [PMC free article] [PubMed] [Google Scholar]; Grover H., Sethi S., Garg J., Ahluwalia A.P.Pseudo prune belly syndrome: diagnosis by imaging- a case report and brief review. Pol J Radiol. 2017;82:252–7. [DOI] [PMC free article] [PubMed]
- 3.Diao B., Diallo Y., Fall P.A., Ngom G., Fall B., Ndoye A.K. Prune belly syndrome: epidemiologic, clinic and therapeutic aspects. Prog Urol. 2008;18:470–474. doi: 10.1016/j.purol.2008.04.003. [DOI] [PubMed] [Google Scholar]; Diao B., Diallo Y., Fall P.A., Ngom G., Fall B., Ndoye A.K., et al. Prune belly syndrome: epidemiologic, clinic and therapeutic aspects. Prog Urol. 2008; 18:470–4. [DOI] [PubMed]
- 4.Zugor V., Schott G.E., Labanaris A.P. The Prune Belly syndrome: urological aspects and long-term outcomes of a rare disease. Pediatr Rep. 2012;4(2):e20. doi: 10.4081/pr.2012.e20. [DOI] [PMC free article] [PubMed] [Google Scholar]; Zugor V., Schott G.E., Labanaris A.P.The Prune Belly syndrome: urological aspects and long-term outcomes of a rare disease. Pediatr Rep. 2012; 4(2):e20. [DOI] [PMC free article] [PubMed]
- 5.García Luzardo M.R., Valenciano Fuente B., Bas Suárez P., Bello Naranjo A.M. Pseudo-prune-belly syndrome: a Prune-Belly without cryptorchidism. Anales de Pediatrìa. 2011;75(1):70–72. doi: 10.1016/j.anpedi.2010.11.023. [DOI] [PubMed] [Google Scholar]; García Luzardo M.R., Valenciano Fuente B., Bas Suárez P., Bello Naranjo A.M.Pseudo-prune-belly syndrome: a Prune-Belly without cryptorchidism. Anales de Pediatrìa2011;75(1):70–2. [DOI] [PubMed]
- 6.Bellah R.D., States L.J., Duckett J.W. Pseudoprune-belly syndrome: imaging findings and clinical outcome. AJR Am J Roentgenol. 1996;167(6):1389–1393. doi: 10.2214/ajr.167.6.8956564. [DOI] [PubMed] [Google Scholar]; Bellah R.D., States L.J., Duckett J.W.Pseudoprune-belly syndrome: imaging findings and clinical outcome. AJR Am J Roentgenol. 1996;167(6):1389–93. [DOI] [PubMed]
- 7.Routh J.C., Huang L., Retik A.B., Nelson C.P. Contemporary epidemiology and characterization of newborn males with prune belly syndrome. Urology. 2010;76:44–48. doi: 10.1016/j.urology.2009.12.072. [DOI] [PubMed] [Google Scholar]; Routh J.C., Huang L., Retik A.B., Nelson C.P.Contemporary epidemiology and characterization of newborn males with prune belly syndrome. Urology2010; 76:44–8. [DOI] [PubMed]
- 8.Reinberg Y., Shapiro E., Manivel J.C., Manley C.B., Pettinato G., Gonzalez R. Prune belly syndrome in females: a triad of abdominal musculature deficiency and anomalies of the urinary and genital systems. J Pediatr. 1991;118:395–398. doi: 10.1016/s0022-3476(05)82153-5. [DOI] [PubMed] [Google Scholar]; Reinberg Y., Shapiro E., Manivel J.C., Manley C.B., Pettinato G., Gonzalez R.Prune belly syndrome in females: a triad of abdominal musculature deficiency and anomalies of the urinary and genital systems. J Pediatr. 1991; 118:395–8. [DOI] [PubMed]
- 9.Letter to the Editor “Pseudo-prune belly syndrome”: an under-reported phenotypic variant of prune belly syndrome. J Pediatr Urol. 2017;13:656–657. doi: 10.1016/j.jpurol.2017.08.015. [DOI] [PubMed] [Google Scholar]; Letter to the Editor “Pseudo-prune belly syndrome”: an under-reported phenotypic variant of prune belly syndromeJ Pediatr Urol (2017) 13, 656–7 [DOI] [PubMed]
- 10.Achour R., Bennour W., Ksibi I., Cheour M., Hamila T., Hmid R.B. Prune belly syndrome: approaches to its diagnosis and management. Intractable Rare Dis Res. 2018;7(4):271–274. doi: 10.5582/irdr.2018.01094. [DOI] [PMC free article] [PubMed] [Google Scholar]; Achour R., Bennour W., Ksibi I., Cheour M., Hamila T., Hmid R.B., et al. Prune belly syndrome: approaches to its diagnosis and management. Intractable Rare Dis Res. 2018;7(4):271–4. doi: 10.5582/irdr.2018.01094. [DOI] [PMC free article] [PubMed]
- 11.Chan Y-C, Bird L.M. Vertically transmitted hypoplasia of the abdominal wall musculature. Clin Dysmorphol. 2004;13:7–10. doi: 10.1097/00019605-200401000-00002. [DOI] [PubMed] [Google Scholar]; Chan Y-C, Bird L.M.Vertically transmitted hypoplasia of the abdominal wall musculature. Clin Dysmorphol2004; 13:7–10. [DOI] [PubMed]
- 12.Digilio M.C., Capolino R., Dallapiccola B. Autosomal dominant transmission of nonsyndromic diastasis recti and weakness of the linea alba. Am J Med Genet. 2008;146A:254–256. doi: 10.1002/ajmg.a.32044. [DOI] [PubMed] [Google Scholar]; Digilio M.C., Capolino R., Dallapiccola B.Autosomal dominant transmission of nonsyndromic diastasis recti and weakness of the linea alba. Am J Med Genet2008; 146A:254–6. [DOI] [PubMed]
- 13.Shoshany G., Gottfied E., Bar-Maor J.A. Accessory scrotum and anorectal malformation associated with “pseudo” prune belly in a neonate. J Perinatol. 1996;16:224–226. [PubMed] [Google Scholar]; Shoshany G., Gottfied E., Bar-Maor J.A.Accessory scrotum and anorectal malformation associated with “pseudo” prune belly in a neonate. J Perinatol1996;16:224–6. [PubMed]
- 14.Olori S., Ameh E.A., Mshelbwala P., Gomna A. Pseudoprune belly syndrome; its’ associations and management challenge in a developing country: a case report. Niger J Med. 2008;17(2):214–216. doi: 10.4314/njm.v17i2.37387. [DOI] [PubMed] [Google Scholar]; Olori S., Ameh E.A., Mshelbwala P., Gomna A.Pseudoprune belly syndrome; its’ associations and management challenge in a developing country: a case report. Niger J Med2008;17(2):214–6. [DOI] [PubMed]
- 15.Grover H., Sethi S., Garg J., Ahluwalia A.P. Pseudo prune belly syndrome: diagnosis revealed by imaging -a case report and brief review. Pol J Radiol. 2017;82:252–257. doi: 10.12659/PJR.899743. [DOI] [PMC free article] [PubMed] [Google Scholar]; Grover H., Sethi S., Garg J., Ahluwalia A.P.Pseudo prune belly syndrome: diagnosis revealed by imaging -a case report and brief review. Pol J Radiol2017;82:252–7. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.