Abstract
A growing corpus of evidence reveals that smoking patterns of migrant women tend to converge with that of the host population over time (‘acculturation paradox’). In this paper we aim to adopt a health equity perspective by studying the extent to which this pattern reflects a convergence with the group of natives who are more socioeconomically disadvantaged. Using population-based registers, we study 1,194,296 women who gave birth in Sweden between 1991 and 2012. Using logistic regression, we estimated odds ratios to assess the effect of duration of residence on the association between smoking during pregnancy and women's origin (classified according to inequality-adjusted Human Development Index (iHDI) of the country of birth). Sibling information and multilevel models were used to assess the extent to which our results might be affected by the cross-sectional nature of the data. Smoking during pregnancy increases with duration of residence among migrants from all levels of iHDI to such an extent that they tend to converge or increase in relation to the levels of the Swedish population with low education and low income, leaving behind the native population with high education and income. The results are robust to possible selection bias related to the cross-sectional nature of the data. Our findings indicate the need of a health equity perspective and suggest the use of ‘unequal assimilation’ rather than ‘acculturation paradox’ as a more suitable framework to interpret these findings.
Keywords: Assimilation paradox, Acculturation paradox, Tobacco, Migration, Social determinants, Unequal assimilation
Highlights
-
•
Smoking during pregnancy (SDP) increased among migrants with their duration of residence in Sweden.
-
•
SDP among migrant women tended to converge to the level of Swedish-born women with lower education and income level.
-
•
Social determinants of health might be a suitable framework to interpret these results.
Introduction
Smoking during pregnancy is associated with a myriad of health outcomes at birth with implications for the newborn's future health. It is, for example, associated with low birthweight (Juárez & Merlo, 2013), which is linked, in turn, to an increased risk of obesity (Gillman et al., 2004), coronary heart disease (Barker, 1995), type-2 diabetes (Barker et al., 1993), hypertension (Leon et al., 1998), among many others adverse outcomes across the life course (Mu et al., 2014; Tong, Baghurst, & McMichael, 2006), including death (Juárez et al., 2016).
With exceptions, such as Finnish women in Sweden, studies on smoking during pregnancy have shown that the migrant population usually shows lower prevalence of smoking compared to nationals (Bosdriesz et al., 2013). However, a growing corpus of evidence reveals that migrants start smoking after some years in the receiving context (i.e. with their duration of residence), to such an extent that they converge with the levels of the native population (Reiss et al., 2015a, 2015b,a,Reiss, Schunck, & Razum, 2015; Urquia, Janevic, & Hjern, 2014). The pattern of convergence has been interpreted as a natural process by which the newcomers embrace lifestyles and behaviors that are predominant in the receiving context (a sort of ‘regression to the mean’).
Duration of residence and acculturation
The observation that migrants' health outcomes tend to converge with the levels of natives with increasing duration of residence has been described as the result of individual preferences for the host-country culture (‘acculturation’) in opposition to those of the sending country (Abraído-Lanza, Chao, & Flórez, 2005; Berry, 2005; Lara et al., 2005).
This has been the dominant explanation when interpreting empirical findings in public health research (Acevedo-Garcia et al., 2010; Lara et al., 2005), although it entails a number of theoretical and methodological limitations. To start with, the dominant cultural interpretation is generally imposed ad hoc since most studies considering duration of residence are descriptive and do not attempt to scrutinize any specific explanation. Interestingly, however, duration of residence has been used as an index of acculturation (Abraído-Lanza et al., 2005, 2006; Commodore-Mensah et al., 2016), even when nothing in that information refers to the mechanism involved, except perhaps that the underlying cause might concern time.
Secondly, the fact that the process of ‘becoming similar’ to the host population (of developed countries) involves the adoption of risky health behaviors among people coming from the less developed world has received scarce attention. Both the adoption of risky health behaviors and their adverse health consequences (which include losing their initial health advantages or healthy migrant paradox) have being implicitly interpreted as an unintended consequence of a process of accommodation that is ultimately beneficial for the full participation of migrants in society (Berry, 1997; Moussa et al., 2010), with no consideration of the role of the receiving context in such deterioration. This unintended consequence has been indistinctly referred to in the literature as ‘acculturation paradox’ (Ramírez et al., 2018), ‘unhealthy acculturation’ (Lara et al., 2005) or ‘unhealthy assimilation’ (Antecol & Bedard, 2006).
Finally, the fact that this cultural interpretation assumes that changes in health behaviors are driven by an individual preference for the host-country culture ultimately circumscribes the phenomenon to individual choices and rational decisions, in line with the so called ‘health behavior paradigm’ in public health (Lynch, Kaplan, & Salonen, 1997), disregarding the fact that, in the receiving contexts, risky health behaviors (including smoking) are over-represented among persons with a low socioeconomic position (Margerison-Zilko & Cubbin, 2013; Moussa et al., 2009). In other words, the cultural assumption tends to ignore the role of social determinants in the adoption of health behaviours.
The centrality of ‘culture’ when describing behavioural changes among migrants is observed in the dominant models used in the literature (such as Berry's model) (Berry, 1997), where concepts such as assimilation, integration, or marginalization cannot be detached from the cultural paradigm ultimately conceptualized as different acculturation strategies.
Social determinants of health. An alternative framework
In contrast to the acculturation explanation, the social determinants of health framework situates risk factors (health behaviours included) beyond the individual domain. This framework has its roots in the theory of the fundamental causes of health and disease, developed by Link and Phelan (Link & Phelan, 1995), that postulated risk factors as proximate causes operating through a more persistent association between social determinants (distal factors) and health. The theory posits that key resources (such as knowledge, money, and social connections) that are important to avoid risks and adopt protective strategies are unevenly distributed across different socioeconomic groups (Phelan, Link, & Tehranifar, 2010), leading in turn to health inequities. Hence, considering the existing socioeconomic gradient of smoking during pregnancy in the receiving country, the increased levels of smoking observed among women with increasing duration of residence might well reflect a convergence with the group of natives who are socioeconomically disadvantaged. This observation, if confirmed empirically, would bring support to a health inequity perspective to the dominant cultural explanation.
While the predominant cultural approach, present in the current literature, mainly focuses on the evidence that migrants adopt behaviours that make them look similar to the native population (here lies the interest in using the native-born population as reference), the social determinants of health perspective focuses on the fact that migrants adopt risky health behaviours that are socially patterned among natives, reflecting social inequities in health (here lies the interest in considering the native-born population as a socially heterogeneous group). Thus, if with increasing duration of residence migrants do converge with the levels of the native population with low education and income, then we have evidence to suspect that the receiving context (as opposed to the sending context) would play a substantial role in explaining such a path. Furthermore, evidence in this direction would suggest that the underlying mechanism of behavioural change is related to avoidable and unfair inequalities (i.e., inequities), rather than culture and norms and, therefore, alternative terms should be proposed to acculturation in order to better describe the phenomenon.
The Swedish migratory context
Within the European context, Sweden has a relatively long tradition as a receiving country (dating back to World War II). Although, with the onset of the global economic recession of the 1970s Sweden, limited the entrance of labour migrants, it adopted a friendly approach to asylum seekers and refugees (Hjern, 2012), being today one of the European countries with the largest share of refugees per capita (Integration Migration Out, 2015). However, despite its humanitarian approach, the migration flows to Sweden have been diverse in terms of age, gender, and reason for migration by country of birth and period. Today, migrants represent around 20% of the total population from more than a hundred sending countries: from other Nordic countries, ∼15% (mainly from Finland), from the European Union, ∼25 (from Germany, The UK), Rest of Europe ∼5 (mainly Poland, Rumania), Asia, ∼30 (predominantly from Iran, Iraq, Turkey, Lebanon Thailand, China, Philippines), Africa, ∼13 (the horn of Africa) and South America, ∼2 (mainly Chile) (Statistics Sweden. 2019 [, 2019).
Specific aims
The aims of this study are threefold: 1)- to assess the effect of duration of residence on the association between maternal origin (categorized according to the levels of inequality-adjusted Human Development Index (iHDI) and smoking during pregnancy in Sweden. We will use the native-born Swedish population as the reference group to assess whether there is a convergence trend as suggested in the literature. 2)- to evaluate whether the above pattern differs when considering Swedish-born women with different levels of education and income as the comparison group. 3)- to evaluate the extent to which our results could be affected by the cross-sectional nature of the data using sibling information. This latter aim refers to the common and generalized limitation in this field, when examining duration effects using cross-sectional data, insofar as the findings are inferred from the comparison of different women with different durations of residence rather than the same women over time (Juárez & Hjern, 2017). Hence, efforts are needed to disentangle compositional from duration effects.
Methods
Study population
This observational study is conducted with population-registers linked individually by the Swedish authorities using a unique personal number. This study contains primarily information from the Swedish Medical Birth Register between 1 January 1991 and 31 December 2012. It includes maternal and child information of ≈99% of all births occurring in Sweden (Cnattingius et al., 1990). Additionally, other registers were used: the Total Population Register to retrieve information on the country of origin of the mother and her duration of residence in Sweden; the Swedish Income and Enumeration Survey for socio-economic information (i.e. maternal education and disposable household income).
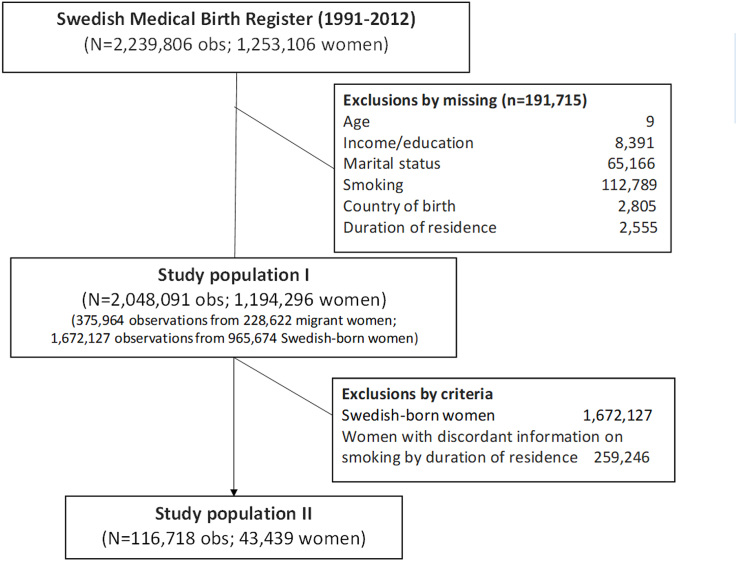
Fig. 1 shows the sample selection. From a total of 2,239,806 observations (births) (corresponding to 1,253,106 mothers), we excluded missing on any of the covariates included in the study (8.6%), of which country of birth; duration of residence, and smoking during pregnancy represents a total of 5.3%. The total sample consisted on 2,048,091 observations (91%) and 1,194,296 women.
Fig. 1.
Flowchart and study population.
Thereafter, to assess the potential effect of using cross-sectional data when looking at duration-effect, we selected women who had more than one child during the study period with discordant information on duration of residence. This means that we included in the analysis women who gave birth to at least one child when they had spent between 6 and 15 years in Sweden (reference category) and at least a second one in one of the other two categories of duration of residence (either ≤5 or ≥16 years). This latter sub-sample consisted of 166,718 observations (births) from 43,439 migrant women.
Covariates
Smoking during pregnancy is our outcome variable. Mothers report this information to midwives in one of their prenatal visits (usually around week 12). Although the original variable is categorized into more and less than 10 cigarettes per day if the mother smoked, in this study, we only consider whether the mother smoked or not. Women's country of birth was classified according to the levels of the Human Development Index (HDI) designed by the United Nation Development Programme. This categorization will allow us to evaluate whether migrants reproduce the gradient observed when comparing different countries worldwide (Corrao et al., 2000). The HDI is a composite indicator that ranks countries according to three main dimensions (life expectancy, education and gross national income per capita) and classifies them into: low, medium, high and very high level of HDI. In this study, we used a version of the HDI which takes inequities also into account (inequality adjusted Human Development Index (iHDI).
Duration of residence was calculated by subtracting the year of birth of the women's child to the women's year of arrival to Sweden and classified into less than or 5 years, 6–15 years and 16 years or more.
Other variables considered in this study were: women's age categorized into 14–20, 21–25, 26–30,31-35 and 36–50; family situation grouped into women who cohabit or are single or other; household disposable income measured the year before giving birth. It was first divided into quintiles and thereafter categorized into low (1st and 2nd quintile), medium (3rd quintile) and high (4th quintile). Education level was defined in three categories: low (basic education), medium (secondary) and high (university). Year of giving birth was also categorized into 1991–1996, 1997–2002, 2003–2007 and 2008–2012.
Statistical analyses
To assess the association between duration of residence and smoking during pregnancy, we estimated Odds Ratios (OR) with 95% confidence intervals (95% CI) using logistic regression models adjusted for robust standard errors. The models were stratified by categories of duration of residence in order to use the Swedish-born population as a reference group. Thereafter, we replicated the analyses considering the Swedish-born population with low or high income and education as the reference group. This latter approach was made to better evaluate with which stratum of the Swedish-born population migrants tend to converge over time. All models included the year of giving birth and women's age to control for calendar and cohort effect, as well as women's education, income, and family situation to adjust for changes in socioeconomic characteristics over time.
We used sibling information to conduct a between- and within-women comparison to assess the extent to which our results could be affected by the cross-sectional nature of the data. Hence, we run and compared a first model that estimates the association between duration of residence (using the category 6–15 years as reference) and smoking during pregnancy among migrant women (between-women analyses) with a second model conducted with a sub-sample of migrants who had more than one child with discordant information on duration of residence (within-women comparison). This latter group is therefore composed by a group of women with truly longitudinal information. The first analysis estimated robust standard errors to account for the presence of sibling in the sample. For the latter, we ran multilevel logistic regressions to account for the nested structure of the data. By comparing the results of women with longitudinal data (the within-women comparison) with those unrelated women who had children with different duration of residence (between-women analyses), we will able to have a sense of the extent to which our cross-sectional approach can be used to infer duration effects.
This study was approved by the Central Ethical Review Board of Stockholm in 2013 (decision no 2013/1058–32).
Results
Table 1 shows the characteristics of the study population. 38% of the foreign-born women come from countries with low or medium level of iHDI. Compared to the Swedish-born women, foreigners were more likely to have low income (68% vs 34%), low education (35% vs 10%) and to be single mothers (8% vs 5%). Table 2 presents the proportion of women who smoke during pregnancy by the level of iHDI and their duration of residence. Overall, foreign-born women coming from low and medium iHDI show considerably lower proportions of smoking (2.5% and 3.8%) than the Swedish-born women (12.5%), while those born in high and very high iHDI have relatively similar proportion than those of the Swedish-born (12.8% and 15.2%, respectively). With the exception of women from high iHDI, all groups show a clear gradient toward an increase smoking prevalence with increasing duration of residence.
Table 1.
Characteristics for women giving birth in Sweden 1991–2012
| Sweden (1,672,127) |
Immigrants (375,964) |
|
|---|---|---|
| N (%) | N (%) | |
| Categories of iHDI | ||
| Low | 44,866 (12.0) | |
| Medium | 96,110 (26.0) | |
| High | 131,248 (35.0) | |
| Very high | 103,740 (28.0) | |
| Income level | ||
| Low | 563,929 (33.7) | 254,890 (67.8) |
| Medium | 366,173 (21.9) | 46,369 (12.3) |
| High | 742,025 (44.4) | 74,705 (19.9) |
| Educational level | ||
| Low | 173,877 (10.4) | 130,019 (34.6) |
| Medium | 828,040 (49.5) | 126,804 (33.7) |
| High | 670,210 (40.1) | 119,141 (31.7) |
| Family situation | ||
| Cohabitant | 1,591,288 (95.2) | 345,362 (91.9) |
| Single/other | 80,839 (4.8) | 30,602 (8.1) |
| Year of giving birth | ||
| 1991–1996 | 495,867 (29.7) | 82,533 (22.0) |
| 1997–2002 | 401,794 (24.0) | 82,747 (22.0) |
| 2003–2007 | 372,649 (22.3) | 88,767 (23.6) |
| 2008–2012 | 401,817 (24.0) | 121,91 (32.4) |
| Maternal age | ||
| 26–30 | 600,031 (35.9) | 119,589 (31.8) |
| 14-20 | 303,780 (18.2) | 80,495 (21.4) |
| 21-25 | 52,684 (3.2) | 16,782 (4.5) |
| 31-35 | 500,346 (29.9) | 102,112 (27.2) |
| 36-50 | 215,286 (12.9) | 56,986 (15.2) |
Table 2.
Smoking during pregnancy by origin (Swedish- and foreign-born by level of iHDI) and duration of residence.
| Non-smokers N (%) |
Smokers N (%) |
Total | |
|---|---|---|---|
| Sweden | 1,463,025 (87.49) | 209,102 (12,51) | 1,672,127 (100) |
| Migrants by level of iHDI | |||
| Low iHDI | |||
| ≤5 | 25,767 (98.71) | 336 (1.29) | 26,103 (100) |
| 6 to 15 | 14,681 (96.80) | 485 (3.20) | 15,166 (100) |
| ≥16 | 3312 (92.08) | 285 (7.92) | 3597 (100) |
| Total | 43,760 (97.53) | 1106 (2.47) | 44,866 (100) |
| Medium iHDI | |||
| ≤5 | 51,129 (97.72) | 1191 (2.28) | 52,320 (100) |
| 6 to 15 | 28,685 (95.37) | 1392 (4.63) | 30,077 (100) |
| ≥16 | 12,647 (92.23) | 1066 (7.77) | 13,713 (100) |
| Total | 92,461 (96.20) | 3649(3.80) | 96,110 (100) |
| High iHDI | |||
| ≤5 | 55,777 (88.50) | 7248 (11.5) | 63,025 (100) |
| 6 to 15 | 36,984 (85.96) | 6042 (14.04) | 43,026 (100) |
| ≥16 | 21,648 (85.91) | 3549 (14.09) | 25,197 (100) |
| Total | 114,409 (87.17) | 16,839(12.83) | 131,248 (100) |
| Very high iHDI | |||
| ≤5 | 34,804 (88.35) | 4589 (11.65) | 39,393 (100) |
| 6 to 15 | 24,494 (86.38) | 3861 (13.62) | 28,355 (100) |
| ≥16 | 2866 (79.63) | 7332 (20.37) | 35,992 (100) |
| Total | 62,164 (84.79) | 15,782(15.21) | 103,740 (100) |
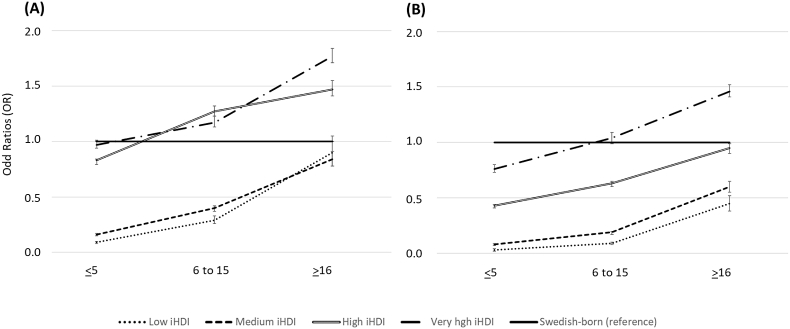
Fig. 2 displays the association between women's origin (defined by the iHDI) and smoking during pregnancy by duration of residence by different levels of adjustments (A and B). As a general pattern, foreign-born women showed higher ORs of smoking during pregnancy with increasing duration of residence in Sweden, showing a gradient by level of iHDI at all categories of duration of residence. The adjusted model (B) shows that, compared to the Swedish-born population, women from all levels of iHDI showed lower ORs with less than 6 years in Sweden (ORlow:0.03 [95%CI: 0.03,0.03]; ORmedium:0.08 [95%CI:0.07,0.08]; ORhigh:0.43 [95%CI:0.42,0.45] and ORveryhigh:0.76 [95%CI:0.73,0.79]). From them, women from countries with very high level of iHDI showed a convergence with the Swedish population in the category 6–15 years in Sweden (ORveryhigh:1.03 [95%CI:0.99,1.08]), while a higher OR after 16 years of residence (ORveryhigh:1.46 [95%CI:1.41,1.52]). Women from countries with high level of iHDI converged with the Swedish population after 15 years among those from high iHDI countries (ORhigh:0.95 [95%CI:0.91,1.00]), while those from countries with low and medium iHDI showed a convergence trend over time but always with lower ORs compared to Swedes (for ≥16: ORlow:0.45 [95%CI:0.38,0.52] and ORmedium:0.60 [95%CI:0.55,0.66]).
Fig. 2.
Women's origin (defined by the iHDI) and smoking during pregnancy by duration of residence. Logistic regressions with different levels of adjustments. Model (A) adjusted for year of birth and maternal age and model (B) adjusted for year of birth, maternal age, family situation, and income.
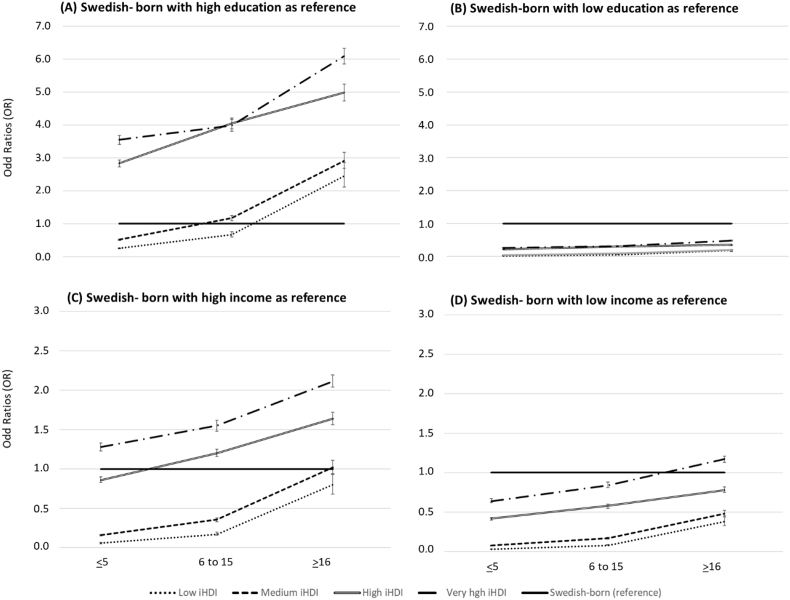
Fig. 3 shows the association between women's origin (defined by the iHDI) and smoking during pregnancy by duration of residence considering the Swedish-born population with high (A) and low (B) education as a reference. Compared to Swedish women with low level of education, migrant women from all iHDI presented lower ORs in all categories of duration of residence, with a small convergence pattern observed among women from countries with very high level of iHDI. A different picture was observed when considering Swedish women with high education as reference (B). Women coming from countries with high and very high levels of iHDI had increased (and increasing) ORs by duration of residence (for high, OR≤5:2.84 [95%CI:2.74,2.95]; OR6-15:4.05. [95%CI:3.89,4.21]; OR≥16:4.99 [95%CI:4.74,5.25]. For very high, OR≤5:3.55 [95%CI:3.41,3.69]; OR6-15:3.99 [95%CI:3.81,4.17]; OR≥16:6.09. [95%CI:5.85,6.33]. Women from countries of low and medium levels of iHDI departed from lower ORs in the first category of duration of residence but they reversed after some time in Sweden (ORmedium:1.17 [95%CI:1.09,1.25] between 6 and 15 years and ORlow:2.45 [95%CI:2.11,2.86] after 15 years).
Fig. 3.
Women's origin (defined by the iHDI) and smoking during pregnancy by duration of residence considering the Swedish-born population with high (A) and low (B) education as a reference. Logistic regressions models adjusted for year of birth, maternal age, family situation, and income.
Table 3 shows the association of duration of residence among migrants within each category of iHDI comparing the whole number of migrants with a sub-sample of those with more than one child during the study period with discordant information on duration of residence. As observed in the table, the results are consistent, showing an increasing risk of smoking during pregnancy with increasing duration of residence. The fact that the effect goes in the same direction between study designs suggests no or limited bias due to the cross-sectional effect of the data.
Table 3.
Odd Ratios (OR) for smoking during pregnancy with 95% Confidence Intervals (95%CI). Comparison between models for the general migrant population (A) and for a sub-sample of siblings with discordant maternal times of residence (B).
| N | All migrants (n = 375,964) |
Sub-sample (n = 116,718) |
||||
|---|---|---|---|---|---|---|
| OR | 95% CI | N | OR | 95% CI | ||
| Migrants by level of iHDI | ||||||
| Low | ||||||
| ≤5 | 15,166 | 0.33*** | [0.28,0.38] | 9601 | 0.35*** | [0.21,0.56] |
| 6 to 15 (ref) | 26,103 | 1 | 8755 | 1 | ||
| ≥16 | 3597 | 3.26*** | [2.79,3.80] | 1224 | 3.27*** | [1.65,6.50] |
| Medium | ||||||
| ≤5 | 30,077 | 0.45*** | [0.41,0.49] | 16,041 | 0.18*** | [0.13,0.26] |
| 6 to 15 (ref) | 52,320 | 1 | 14,330 | 1 | ||
| ≥16 | 13,713 | 2.16*** | [1.98,2.35] | 2222 | 3.38*** | [2.12,5.40] |
| High | ||||||
| ≤5 | 43,026 | 0.74*** | [0.71,0.77] | 22,089 | 0.55*** | [0.48,0.63] |
| 6 to 15 (ref) | 63,025 | 1 | 16,593 | 1 | ||
| ≥16 | 25,197 | 1.09*** | [1.05,1.14] | 4835 | 1.57*** | [1.30,1.90] |
| Very high | ||||||
| ≤5 | 28,355 | 0.82*** | [0.79,0.86] | 10,833 | 0.29*** | [0.23,0.36] |
| 6 to 15 (ref) | 39,393 | 1 | 8062 | 1 | ||
| ≥16 | 35,992 | 1.49*** | [1.43,1.56] | 2133 | 6.50*** | [4.75,8.89] |
Models adjusted for maternal age and year of birth.
Logistic regression was used for the general sample with robust standard errors and multilevel logistic regression for the discordant subsample.
Note: The general migrant group has 375,9640 observations from 228,622 migrant women.
The discordant sample has 166,718 observations from 43,439 women.
Discussion
Main findings
Our study shows that smoking during pregnancy increases with duration of residence among migrant women from all levels of iHDI in Sweden. The results are robust to possible selection bias related to the cross-sectional nature of the data, as they were consistent in the within-women analysis.
Compared to the general Swedish-born women, all migrant groups presented lower levels of smoking that either tended to converge (the case of low and medium iHDI), converged (high iHDI) or increased (very high iHDI) with time spent in Sweden. This result is in line with previous studies conducted in Sweden (Urquia et al., 2014) and other contexts (Reiss et al., 2015b), showing that migrants tend to adopt this harmful habit with their duration of residence. This trend, which follows the broader international evidence on the adoption of risky-health behaviours among migrants (Abraído-Lanza et al., 2005; Antecol & Bedard, 2006; Lindström & Sundquist, 2005) and the second generation (Hjern & Allebeck, 2004; Svensson & Hagquist, 2010), has been predominantly explained in line with the acculturation hypothesis and, although some have mentioned the importance of considering different social groups (Urquia et al., 2014), no previous study has empirically looked into this before us.
When considering different social groups as the reference category among Swedes, a more pronounced pattern emerged. Smoking during pregnancy increases with duration of residence among migrants from all levels of iHDI to such an extent that they showed a tendency to converge with the low-educated Swedish population, leaving behind the native population with high education. This is even more clearly observed when income is considered instead, as not only most groups converge to the levels of smoking of low-income natives (low, medium and high iHDI), but some even exceed their levels (very high iHDI).
Although determining the mechanisms involved in explaining our findings exceeds our goal and possibilities, it seems quite clear that our findings highlight the unequal nature of the ‘acculturation’ pattern among migrants, and therefore call for the adoption of an inequity perspective (as opposed to a cultural one) in the understanding of smoking adoption among migrants as well as when designing preventive policies. Given our results, we advocate for the concept of unequal assimilation, which, as opposed to the cultural one, sheds light on the structural factors behind the existence of different patterns of ‘adaptation’ (Abraído-Lanza et al., 2006; Viruell-Fuentes, 2007; Zhou, 1997).
Studies have pointed out that segregation (mainly residential) is associated with unhealthy behaviours, including smoking during pregnancy (Bell et al., 2007). Migrants usually live in disadvantaged areas where smoking is more prevalent. These areas might create the conditions for them to adopt risky health behaviours, as they might be exposed to (new) social norms existing among the less privileged groups of the host society with whom they interact (Echeverría et al., 2015). Alternatively to this process of acceptance of social norms and emulation of actions, the adoption of smoking can be part of a coping strategy against chronic stressful situations derived from the sense of isolation (as a consequence of segregation), the experience of ethnic discrimination (racism) (Bell et al., 2007; Borrell et al., 2013) and/or perceived inequality (Slopen et al., 2013). Although future studies should disentangle the pathways in the adoption of smoking with increasing duration of residence, our results suggest that the main driving force is linked to social inequalities. Furthermore, the adoption of smoking might act as a possible mechanism on the (re)production of health inequities within and across generations. Smoking is not only associated to health outcomes that might limit the full integration of women into society (Lundborg, 2007), but it is also linked to a number of adverse health outcomes for the child (Juárez & Merlo, 2013), with long term implications for the child's development (Breslau et al., 2005).
The results partially fit into the ‘segmented assimilation theory’. This is a sociological formulation that also highlights the heterogenous features of the assimilation process while focusing on the socioeconomic incorporation of the second-generation migrants into the receiving society (the United States). This theory predicts that individuals with a foreign background would experience an assimilation to the underclass (Portes & Zhou, 1993). Thus, for example, individuals originally from the middle class would assimilate into the lower class and so on. Although our study does not examine migrants' socioeconomic assimilation (and do not differentiate migrants by levels of education and income), smoking, as many other risky health behaviours, are socially patterned and, therefore, our results might be in line with such a theory. Hence, it would be expected to see a smoking gradient by level of iHDI which would converge with the levels of smoking among natives with lower income and education (the reference in our case). However, although with increased duration of residence migrants from high and very high iHDI tend to exceed the levels of the Swedish population with high education and income (in line with the segmented assimilation theory), all categories of migrants still show an advantage compared to natives with low education and income. Our findings therefore suggest that the segmented assimilation theory might not apply to all contexts and outcomes, and/or that it might better apply to the second-generation.
The pattern observed across levels of iHDI in our study is consistent with those observed in cross-country comparisons (Corrao et al., 2000). This finding suggests the influence of the context of origin in this gradient, while the effect of duration of residence might show the influence of the host country. These combined findings therefore confirm previous studies which advocate for the importance of considering both contexts in public health research (Acevedo-Garcia et al., 2012).
Strength and limitations
In this study we incorporate a health equity perspective into a debate in which cultural interpretations are dominant. Furthermore, we tried to overcome some of the more important limitations of these studies, notably the use of cross-sectional information to evaluate time effects. The relatively long migratory tradition of Sweden permits to assess changes by duration of residence beyond 16 years. This is a strength compared to other studies, as it reveals that the actual tendency toward a convergence with the levels of the native population (which is true for most groups in the first years) might end up surpassing the levels of the natives. However, despite these strengths, the study has also some limitations. For example, we could not include secondhand smoke or smokeless forms of tobacco, such as snus use, cigars and pipes as it was not available in our setting. Furthermore, smoking during pregnancy is reported by women to the midwives and, hence, a proportion of misreported information is expected. A validation study conducted in Sweden reported the information in the Swedish Medical Birth Register to be quite reliable (Mattsson et al., 2016). However, though such validation did not consider the migrant population specifically, we do not have any indication to expect the information to be of lower quality among migrants. It is likely that a number of former smokers are included in the category of ‘non-smokers’, as pregnant women are especially encouraged to quit. Unfortunately, we cannot identify former smokers from our setting, but we can speculate that they might be predominantly highly educated women (thus, exacerbating the social differences observed in our study), since prior research shows that they are more likely to follow health recommendations (Oxman et al., 2009). It is precisely these aspects that make us cautious to extrapolate our findings to the whole population. Also, there is relatively large proportion of missing smoking during pregnancy (5%). To assess the stability of our results, we conducted sensitivity analyses considering women with missing information as ‘smokers’. The results (shown under request) are consistent with our main findings. Finally, the information on education is problematic among women in reproductive ages since part of the Swedish-born women might be completing their tertiary education and, hence, our results might be underestimated.
Conclusion
Our study shows that smoking during pregnancy increases among migrants with their duration of residence, converging with the levels of the Swedish-born population and, specifically, with those with low education and income. Our study calls for the adoption of an inequity perspective in the understanding of smoking adoption among migrants as well as when designing preventive policies.
Declaration of interests
None.
Funding
This research was supported by the Swedish Research Council for Health, Working Life and Welfare (FORTE #2016-07128), the Swedish Research Council (VR #2018/018-25) and NordForsk (#7465).
Acknowledgments
The authors would like to thank MSc. Helena Honkaniemi for her assistance with the figures.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2019.100416.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Abraído-Lanza A.F., Chao M.T., Flórez K.R. Do healthy behaviors decline with greater acculturation?: Implications for the Latino mortality paradox. Social Science & Medicine. 2005;61(6):1243–1255. doi: 10.1016/j.socscimed.2005.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abraído-Lanza A.F. Toward a theory-driven model of acculturation in public health research. American Journal of Public Health. 2006;96(8):1342–1346. doi: 10.2105/AJPH.2005.064980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Acevedo-Garcia D. The effect of immigrant generation and duration on self-rated health among US adults 2003-2007. Social Science & Medicine. 2010;71(6):1161–1172. doi: 10.1016/j.socscimed.2010.05.034. [DOI] [PubMed] [Google Scholar]
- Acevedo-Garcia D. Integrating social epidemiology into immigrant health research: A cross-national framework. Social Science & Medicine. 2012;75(12):2060–2068. doi: 10.1016/j.socscimed.2012.04.040. [DOI] [PubMed] [Google Scholar]
- Antecol H., Bedard K. Unhealthy assimilation: Why do immigrants converge to American health status level? Demography. 2006;43(2):337–360. doi: 10.1353/dem.2006.0011. [DOI] [PubMed] [Google Scholar]
- Barker D.J.P. Fetal origins of coronary heart disease. BMJ. 1995;311:171–174. doi: 10.1136/bmj.311.6998.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barker D.J.P. Type 2 (non-insulin-dependent) diabetes mellitus, hypertension and hyperlipidaemia (syndrome X): Relation to reduced fetal growth. Diabetologia. 1993;36:62–67. doi: 10.1007/BF00399095. [DOI] [PubMed] [Google Scholar]
- Bell J.F. Associations between residential segregation and smoking during pregnancy among urban African-American women. Journal of Urban Health. 2007;84(3):372–388. doi: 10.1007/s11524-006-9152-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berry J.W. Immigration, Acculturation, and Adaptation Applied Psychology. 1997;46(1):5–68. [Google Scholar]
- Berry J.W. Acculturation: Living successfully in two cultures. International Journal of Intercultural Relations. 2005;29:697–712. [Google Scholar]
- Borrell L.N. Racial discrimination, racial/ethnic segregation, and health behaviors in the CARDIA study. Ethnicity and Health. 2013;18(3):227–243. doi: 10.1080/13557858.2012.713092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bosdriesz J. Smoking prevalence among migrants in the US compared to the US-born and the population in countries of origin. PLoS One. 2013;8(3) doi: 10.1371/journal.pone.0058654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau N. Maternal smoking during pregnancy and offspring IQ. International Journal of Epidemiology. 2005;34(5):1047–1053. doi: 10.1093/ije/dyi163. [DOI] [PubMed] [Google Scholar]
- Cnattingius S. A quality study of a medical birth registry. Scandinavian Journal of Social Medicine. 1990;18:143–148. doi: 10.1177/140349489001800209. [DOI] [PubMed] [Google Scholar]
- Commodore-Mensah Y. Length of residence in the United States is associated with a higher prevalence of cardiometabolic risk factors in immigrants: A contemporary analysis of the national HealthInterview Survey. Journal American Heart Association. 2016;4(5) doi: 10.1161/JAHA.116.004059. 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corrao M.A. Building the evidence base for global tobacco control. Bulletin of the World Health Organization. 2000;78(7):884–890. [PMC free article] [PubMed] [Google Scholar]
- Echeverría S.E. Social norms and its correlates as a pathway to smoking among young Latino adults. Social Science & Medicine. 2015;124:187–195. doi: 10.1016/j.socscimed.2014.11.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillman M.W. A life course approach to obesity. In: Diana K., Ben-Shlomo Y., editors. A life course approach to chronic disease epidemiology. Oxford University Press; Oxford: 2004. [Google Scholar]
- Hjern A. Migration and public health: Health in Sweden: The national public health report 2012. Chapter 13. Scandinavian Journal of Public Health. 2012;40(9):255–267. doi: 10.1177/1403494812459610. [DOI] [PubMed] [Google Scholar]
- Hjern A., Allebeck P. Alcohol-related disorders in first- and second-generation immigrants in Sweden: A national cohort study. Addiction. 2004;99(2):229–236. doi: 10.1046/j.1360-0443.2003.00562.x. [DOI] [PubMed] [Google Scholar]
- Integration migration outlook. OECD; Paris: 2015. [Google Scholar]
- Juárez S. Birth characteristics and all-cause mortality: A sibling analysis using the uppsala birth cohort multigenerational study. Journal of Development Origins Health and Disease. 2016;7(4):374–383. doi: 10.1017/S2040174416000179. [DOI] [PubMed] [Google Scholar]
- Juárez S., Hjern A. The weight of inequalities: Duration of residence and offspring's birthweight among migrants in Sweden. Social Science & Medicine. 2017;175:81–90. doi: 10.1016/j.socscimed.2016.12.045. [DOI] [PubMed] [Google Scholar]
- Juárez S., Merlo J. Revisiting the effect of maternal smoking during pregnancy on offspring birthweight: A quasi-experimental sibling analysis in Sweden. PLoS One. 2013;8(4) doi: 10.1371/journal.pone.0061734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lara M. Acculturation and latino health in the United States: A review of the literature and its sociopolitical context. Annual Review of Public Health. 2005;26:367–397. doi: 10.1146/annurev.publhealth.26.021304.144615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leon D.A. Reduced fetal growth rate and increased risk death from ischaemic heart disease: Cohort study of 15000 Swedish men and women born 1915-29. BMJ. 1998;317:241–245. doi: 10.1136/bmj.317.7153.241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindström M., Sundquist K. The impact of country of birth and time in Sweden on overweight and obesity: A population-based study. Scandinavian Journal of Public Health. 2005;33(4):276–284. doi: 10.1080/14034940510005653. [DOI] [PubMed] [Google Scholar]
- Link B.G., Phelan J. Social conditions as fundamental causes of health inequalities. Journal of Heath ans Social Behavior. 1995;35:80–94. (Forty Years of Medical Sociology: The State of the Art and Directions for the Future) [PubMed] [Google Scholar]
- Lundborg P. Does smoking increase sick leave? Evidence using register data on Swedish workers. Tobacco Control. 2007;16(2):114–118. doi: 10.1136/tc.2006.017798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynch J.W., Kaplan G.A., Salonen J.T. Why do poor people behave poorly? Variation in adult health behaviours and psychosocial characteristics by stages of the socioeconomic lifecourse. Social Science & Medicine. 1997;44:809–819. doi: 10.1016/s0277-9536(96)00191-8. [DOI] [PubMed] [Google Scholar]
- Margerison-Zilko C., Cubbin C. Socioeconomic disparities in tobacco-related health outcomes across racial/ethnic groups in the United States: National Health Interview Survey 2010. Nicotine & Tobacco Research. 2013;15(6):1161–1165. doi: 10.1093/ntr/nts256. [DOI] [PubMed] [Google Scholar]
- Mattsson K. Cotinine validation of self-reported smoking during pregnancy in the Swedish Medical Birth Register. Nicotine & Tobacco Research. 2016;18(1):79–83. doi: 10.1093/ntr/ntv087. [DOI] [PubMed] [Google Scholar]
- Moussa K. Socioeconomic differences in smoking trends among pregnant women at first antenatal visit in Sweden 1982-2001: Increasing importance of educational level for the total burden of smoking. Tobacco Control. 2009;18(2):92–97. doi: 10.1136/tc.2008.026336. [DOI] [PubMed] [Google Scholar]
- Moussa K. Are time-trends of smoking among pregnant immigrant women in Sweden determined by cultural or socioeconomic factors? MC Public Health. 2010;10(1):374. doi: 10.1186/1471-2458-10-374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mu M. Birth weight and subsequent risk of asthma: A systematic review and meta-analysis. Heart Lung & Circulation. 2014;23(6):511–519. doi: 10.1016/j.hlc.2013.11.018. [DOI] [PubMed] [Google Scholar]
- Oxman D. SUPPORT Tools for evidence-informed health Policymaking (STP) 10: Taking equity into consideration when assessing the findings of a systematic review. Health Research Policy and Systems. 2009;7(1):S10. doi: 10.1186/1478-4505-7-S1-S10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phelan J.C., Link B.G., Tehranifar P. Social conditions as fundamental causes of health inequalities: Theory, evidence, and policy implications. Journal of Health and Social Behavior. 2010;51:S28–S40. doi: 10.1177/0022146510383498. [DOI] [PubMed] [Google Scholar]
- Portes A., Zhou M. The new second generation: Segmented assimilation and its variants. The Annals of the American Academy of Political and Social Science. 1993;530:74–96. [Google Scholar]
- Ramírez S.A. Questioning the dietary acculturation paradox: A mixed-methods study of the relationship between food and ethnic identity in a group of Mexican-American women. Journal of the Academy of Nutrition and Dietetics. 2018;18(3):431–439. doi: 10.1016/j.jand.2017.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reiss K. Smoking during pregnancy among Turkish immigrants in Germany-are there associations with acculturation? Nicotine & Tobacco Research. 2015;17(6):643–652. doi: 10.1093/ntr/ntu237. [DOI] [PubMed] [Google Scholar]
- Reiss K., Schunck R., Razum O. Effect of length of stay on smoking among Turkish and Eastern European immigrants in Germany—interpretation in the light of the smoking epidemic model and the acculturation theory. Nt J Environ Res Public Health. 2015;12:15925–15936. doi: 10.3390/ijerph121215030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slopen N. Psychosocial stress and cigarette smoking persistence, cessation, and relapse over 9-10 years: A prospective study of middle-aged adults in the United States. Cancer Causes & Control. 2013;24(10):1849–1863. doi: 10.1007/s10552-013-0262-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Statistics Sweden. 2019. http://www.statistikdatabasen.scb.se [cited 2019 02-02]; Available from: [Google Scholar]
- Svensson M., Hagquist C. Adolescent alcohol and illicit drug use among first- and second-generation immigrants in Sweden. Scandinavian Journal of Public Health. 2010;38(2):184–191. doi: 10.1177/1403494809353822. [DOI] [PubMed] [Google Scholar]
- Tong S., Baghurst P., McMichael A. Birthweight and cognitive development during childhood. Journal of Paediatrics and Child Health. 2006;42(3):98–103. doi: 10.1111/j.1440-1754.2006.00805.x. [DOI] [PubMed] [Google Scholar]
- Urquia M.L., Janevic T., Hjern A. Smoking during pregnancy among immigrants to Sweden, 1992-2008: The effects of secular trends and time since migration. The European Journal of Public Health. 2014;24(1):122–127. doi: 10.1093/eurpub/ckt048. [DOI] [PubMed] [Google Scholar]
- Viruell-Fuentes E.A. Beyond acculturation: Immigration, discrimination, and health research among Mexicans in the United States. Social Science & Medicine. 2007;65(7):1524–1535. doi: 10.1016/j.socscimed.2007.05.010. [DOI] [PubMed] [Google Scholar]
- Zhou M. Segmented assimilation: Issues, controversies, and recent research on the new second generation. International Migration Review. 1997;31(4):975–1008. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.