Abstract
Background
As older adults approach the end‐of‐life (EOL), many are faced with complex decisions including whether to use medical advances to prolong life. Limited information exists on the priorities of older adults at the EOL.
Objective
This study aimed to explore patient and family experiences and identify factors deemed important to quality EOL care.
Method
A descriptive qualitative study involving three focus group discussions (n = 18) and six in‐depth interviews with older adults suffering from either a terminal condition and/or caregivers were conducted in NSW, Australia. Data were analysed thematically.
Results
Seven major themes were identified as follows: quality as a priority, sense of control, life on hold, need for health system support, being at home, talking about death and competent and caring health professionals. An underpinning priority throughout the seven themes was knowing and adhering to patient's wishes.
Conclusion
Our study highlights that to better adhere to EOL patient's wishes a reorganization of care needs is required. The readiness of the health system to cater for this expectation is questionable as real choices may not be available in acute hospital settings. With an ageing population, a reorganization of care which influences the way we manage terminal patients is required.
Keywords: care priorities, end‐of‐life, family caregivers, older adults, qualitative study
1. INTRODUCTION
Increased use of emergency services and hospitalizations among older people who are dying1 often includes intensive procedures2 that can prolong suffering and are too late to be of benefit.3, 4 Evidence that patients or families has been consulted regarding their preferences for future care and how this consultation has occurred is limited but critical to the provision of appropriate end‐of‐life (EOL) care.5
Older patients and their families are usually provided with information about hospital‐based treatment options6, 7 regardless of whether they wish to spend their last days in an acute care hospital.8, 9 You et al10 report that patients and families lack understanding of the implications of life‐sustaining treatments, with Wilmott and colleagues11 finding that a patient's substitute decision makers do not always act in the patient's best interest. As a result, a patient's wishes may not be known or honoured. Additional factors that can further complicate EOL decision making are as follows: the low public awareness12; cultural values affecting care preferences at the EOL;13, 14 family denial of the patient's prognosis;15 potential cognitive impairment in old age;16 conflicting family pressures;17, 18 and the level of a doctor's professional expertise in communicating a terminal prognosis sensitively.19
Health professionals providing quality EOL care across all health services must have an understanding of the family and patient's perception of what is appropriate and contributes to high‐quality care, and what constitutes a “good death.”20, 21, 22 This information is necessary to fully inform clinical and other support staff providing EOL health services. Existing data that demonstrate the use of medically inappropriate treatments at the end‐of‐life and the importance of engaging in advance care planning may assist to inform more honest end‐of‐life discussion.23, 24
Research to date on EOL care has been predominantly conducted in the cancer realm.25 With more people dying from diseases of ageing,26 this research, although informative, does not take into consideration the EOL trajectory of other terminal conditions. The Australian government recognizes the importance of providing high‐quality EOL care27 and developing guiding principles and essential elements for the provision of safe and high‐quality EOL care.28 Despite the Australian government's support for EOL care, a recent Australian‐based study found that only fourteen per cent of non‐cancer patients in the last year of life, with irreversible conditions which were considered amenable for palliative care, received specialist palliative care compared to more than two‐thirds of cancer patients.29 These non‐cancer patient conditions included the following: heart, renal and liver failure; COPD; HIV/AIDS; dementia; and Motor neurone, Parkinson's and Huntington's disease.
This study aimed to determine older terminally ill patients and caregivers’ priorities, perceptions and appropriateness in EOL care.
1.1. Objectives
Define current consumer priorities in EOL care for older terminal patients, their caregivers
Elucidate the main components of “quality” at EOL
Explore the perceived impact of treatment for terminal illness on the individual and their caregivers
Identify the important health service factors for quality EOL care
2. METHODS
2.1. Sample frame—Consumer EOL advisory group
The sample frame was members of the UNSW consumer EOL advisory group, established to identify priority concerns to inform on the public perspective of our research projects. Between November 2015 and March 2016, a call for older adults/carers of older adults to participate in the UNSW consumer EOL advisory group was undertaken through advertisements in academic and hospital/aged care networks and by word of mouth. The UNSW consumer EOL advisory group membership eligibility included the following: direct experience of health services for advanced chronic illness including terminal care either for a relative, friend or themselves; or experience in providing physical and social aspects of care for frail terminal older adults and/or their relatives towards their EOL; or commitment to the concept of improving the EOL experience for themselves or others. Those who were interested in becoming a member of the consumer advisor group responded via email and/or telephone. A total of 37 people, mostly aged over 60 years, joined the consumer EOL advisory group. However, it also included younger adults (30‐49 years) who informally cared for older people. Consumer group members attend a maximum of four consultations per year, with participation for each consultation voluntary. This study reports result from the Round 3 consultations.
2.2. Sample and data collection
All of the consumer EOL advisory group members were invited to participate in Focus Group Discussions (FGD) or In‐depth Interviews (IDI). A total of 24 (65%) agreed to participate. Ninety‐minute FGDs were conducted on the same day in April 2016 and 90‐minute (IDI) were undertaken during the month of June 2016. All FGDs comprised both terminally ill patients and caregivers in each group. One member of the study team (EL) conducted all IDI with patients being at home, which were necessary to capture perspectives of those who were unable to participate in FGD. This was due to geographical difficulty, as 30% of the Australian population reside outside major cities30 or due to the participant's poor physical health from their terminal condition which impacted on their mobility and transport capacity. Members of the study team developed the FGD guide which included four main topics EOL care, quality of life factors, family impact and health‐care provision (Appendix S1). The IDI guide that reflected the FGD topic was also generated for those who lived away from the city where the study was conducted or for those volunteers who were too ill to attend the focus groups. Written consent was obtained from each participant. Three study team members with either a psychology (RH) or a nursing background (EL, LH), who were trained in qualitative methods, facilitated the three 90‐minute FGDs in a private meeting room on a University campus. The facilitator guided participants through each of the topics. The FGDs were audio‐recorded and written notes were also taken by the team members. One team member (EL) was present for all FGDs and listened to the transcripts from all FGDs to ensure consistency. EL conducted all IDI using the agreed guide.
2.3. Data analysis
The audio‐recorded qualitative data were transcribed verbatim and managed using NVivo software (version 11 QSR, International Pty Melbourne, Victoria, Australia).
Thematic content analysis was used to elicit themes from participants regarding whether quality or length of life was most valued, attributes of good quality living, the effect of EOL involvement on caregivers and their experiences and expectations of health professionals providing this care. Two team members (RH, EL) undertook the thematic analysis,31 initially repeatedly reading the transcripts and then labelling the text in the NVivo software. Each team member then independently grouped labels into related themes around consistent or divergent issues arising. These researchers held iterative discussions in which they reflected on the emerging themes32 and then refined the themes into a final set of agreed categories. A third researcher (LH) who observed the FGD independently reviewed the categories and themes within these for face validity.
3. RESULTS
The final sample included 24 participants, 17 females and 7 males. Eighteen participants attended FGDs and six had an IDI. Ten participants suffered from a chronic progressive or life‐limiting illness including Chronic Kidney Disease with multiple transplants (1); Advanced Parkinson's Disease (1); Breast Cancer (1); Heart failure (2); COPD and inoperable brain tumour (1); Motor Neuron Disease (1); Organic dementia (1); frailty (2). Fourteen participants were carers of those who had suffered a terminal condition and faced EOL decisions. The sample was ethnically diverse with 14 born in Australia and 10 born in the Mediterranean, Eastern Europe, South Asia, Middle East and American countries. Participants were predominately aged 60 years and older (20), and five subjects lived in rural/regional Australia.
Seven themes emerged from the analysis of the FGD and the IDI transcripts: quality as a priority, sense of control, life on hold, need for health system support, being at home, talking about death and competent and caring health professionals. An underpinning priority that fed through the six themes was knowing and adhering to what the patient wants. Figure 1 illustrates these themes and the factors within each theme that were assessed by the participants as being a priority for optimal EOL care. Each theme is also described below with supporting quotes.
Figure 1.
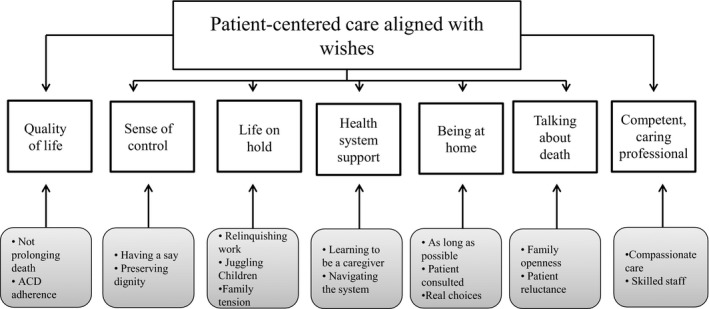
Themes on patient and family priorities at the EOL
3.1. Quality as a priority
Participants across the FGD and IDI agreed that a good quality of life was the most important consideration in EOL care; prolonging an uncomfortable existence was not the goal. Discontent with models of care that were not sensitive and responsive to quality of life considerations surfaced quickly in the discussion. Whilst rapid consensus was achieved regarding quality of life as the most important factor in EOL decisions, further exploration of the conceptualization of quality revealed nuanced understanding of what quality means to any given patient is critical to making EOL decisions. Prolonging life was, however, identified as an important consideration when there continues to be hope for treatment and when a patient is of a younger age.
I don't want to prolong my life at all. As long as I'm independent I'm quite happy but if I become reliant on other people I do not wish to live under the circumstance.
(Male, COPD and inoperable brain tumour)
I have no interest in the quantity of my life; I have every interest in the quality.
(Female, Organic dementia)
“So in prolonging life was there also quality of life during that prolonging? For me, that's a major question”
(Female, Caregiver)
Participants suggested that when making assessments and decisions about whether prolonging life is beneficial to the patient, understanding and adhering to the patient's wishes was seen as an essential part of personalised care. One example raised by many was the need for recognition of and adherence to advanced care directives when in place.
A year before that she had…gone to the solicitor and written that she didn't want any pharmaceutical, medical or surgical intervention. I came in the next day and she was being pumped full of antibiotics
(Female, Caregiver)
Part of the medical system is this giving of medications, keeping the medications on, ignoring directives like ‘Don't Resuscitate
(Female, Caregiver)
3.2. Sense of control
Participants did not define a discrete set of quality of life factors, but converged on the notion that a good quality of life is when an individual has control and can meet their own personal standards and expectations. These standards and expectations were perceived as dynamic throughout life and at the EOL as physical and cognitive abilities deteriorate.
So my quality of life description is ‐ and it's very personal ‐ up until I was 80 was to make 80 and it was going to give me the quality of life I wanted. After I turned 80 and then I'd had a fall this week…
(Male, Advanced Parkinson's Disease)
Quality of life when I think about myself is about having a say in my life and being able to have some self‐agency and to be able to have a say in what happens to me and to be able to have some capacity to direct things.
(Female, Motor Neuron Disease)
Good quality of life was consistently conceptualized as being able to do the things a person enjoys and maintaining their sense of self through these activities, or as the patient's ability to achieve their aspirations whatever those may be. Many examples were provided, particularly by carers, of activities and interests that, for their loved one, were markers of good quality existence.
He was a passionate music lover and that had been one of his great loves. So right up in fact to the moment that he was dying he was listening to his favourite.
(Female, Caregiver)
Loss of control was consistently identified by the participants as a loss of quality of life and linked to a perceived loss of dignity. Caregiver participants experienced distress at watching a loved one losing control of their thoughts and actions.
So by this time she gets to the nursing home, she's faecally incontinent; she's urinary incontinent; had to hoist her up on that thing to hose her down; you know absolutely awful.
(Female, Caregiver)
For someone with a mental disease, brain degeneration, as my husband has, who has no quality of life…everything has to be done for him… but we have to wait until there is another medical disease before he can be placed into palliative care.
(Female, Caregiver)
3.3. Putting family life on hold
Caregiver participants described the impact of their loved one's life‐limiting illness as putting their life on hold to care for another, making financial, career and personal compromises in order to do this. All of the participants who had experienced caring for a loved one at the EOL discussed common features of this caring role.
In the last year of my mother's life I had three fairly young children. I used to go at 6:30 am or 6:00 am to visit her so I could get home in time to take the kids to school. I was also at full time university…I did it somehow but it certainly impacted.
(Female, Caregiver)
It was enormously stressful because this is over a period of six years. My sister was working, I wasn't, but our parents lived separate from both of us so we had lot of the car driving, a lot of expense.
(Female, Caregiver)
“Juggling” family life and caring responsibilities was a challenge, with many participants highlighting the uneven distribution of caring responsibilities between family members. In some cases, this raised tensions between family members, and in some cases led to the process of agreeing roles.
“My sister and I are very different, but we negotiated the care really, really well, because we both acknowledged what our strengths were and we did them.”
(Female, Caregiver)
“I guess as the person who takes on the most of the caring role you sometimes feel a bit abandoned by the rest of your family because it's just presumed you will be there…”
(Female, Caregiver)
Carer participants described EOL care as emotionally difficult. Feelings of guilt, denial, distress and sadness were noted in addition to the physical and logistical challenges of caring for a loved one. Although caregiver participants sought to adhere to patients’ preferences regarding not prolonging their life, conflicting feelings occurred as participant caregivers also did not want to lose their loved one.
I think I've had both those feelings; wanting them to hang around, but also wishing them a speedy goodbye for their sake.
(Female, Caregiver)
3.4. Need for health system support
Both patients and caregivers identified challenges in navigating the health system, although these were conceptualized differently. For patients, attending appointments for care at the EOL could be challenging, with the difficulty of multiple visits to services that were not localized, compounded by poor mobility and the associated costs of transport.
I have to go to (X) hospital for several injections a couple of times per week and if for instance I went by taxi it cost me 100 dollars or more return but if I take public transport I have to take three different busses and a train and if everything went bad it could take me up to 6 hours in transport
(Male, COPD and inoperable brain tumour)
For caregivers, navigating the complex health system and learning to be a carer for the first time was physically and emotionally challenging. Respondents converged on the difficulties of liaising with multiple services and providers, trying to establish service availability and also gaining access. Navigating the system was particularly challenging whilst being a caregiver, and in some cases, working in professional employment alongside the caring role. The need for greater support system was noted by many during the discussion.
I would like to see them (caregivers) being formally supported in some way….supports people through what they're learning, because you're learning stuff. You know it's like this whole new world.
(Female, Caregiver)
I'd really like to see something in institutions where there was somebody who would help coordinate some kind of care amongst the people who care about this person
(Female, Caregiver)
3.5. Being at home (at EOL)
Participants agreed that it was generally preferable to stay at home for as long as possible. Consultation with health providers and choice regarding the location of their treatment and care was identified as important.
Dad was in palliative care and basically he didn't want to be there at all…one day mum went in and he said take me home….So he was home for a week and then passed away at home, but at least he met his wishes.
(Male, Caregiver)
The hospital is an alternative, I would never say the home is an alternative… the hospital has to be the last place on earth in any country that you would need to go simply to die.
(Female, Caregiver)
Yet caregiver participants identified cases in which this was not possible, such as when the person or their caregiver did not have the ability to provide the care required. In these cases, carer participants often reported a need for greater support from other social or community‐based services to facilitate care at home.
We knew we couldn't deal with it at home ourselves, but had there been other kinds of care, that would have been perfect. He would have still been in his own garden and done his own little pottering around the place as he always did
(Female, Caregiver)
She couldn't cope at home and she's gone into an old age home and that's much better all‐round than trying to cope at home.
(Male, Caregiver)
3.6. Talking about death
Openness about impending death, honesty and transparency between patients, their family and health‐care providers was viewed as important in ensuring appropriate, patient‐centred, EOL care.
Yet participants highlighted the difficulty of talking about death at every level; between patients, family, health professionals and at a societal level. Discussions about the EOL were identified as limited, lacking, too late and emotionally challenging, leading to a lack of sufficient understanding of each patient's wishes.
I think it's a bit the same as the culture, the kind of health culture, there's not a kind of a literacy in our community, in our society around death. It's not easily spoken about.
(Female, Caregiver)
Caregiver participants often described the reluctance of their loved one to talk about their deterioration and what they wanted. Some identified this as culturally influenced but the participants generally agreed that discussions about death were uncommon across cultures.
The doctor brought up the question of the directive to see whether to switch off the life support machine just in case … but she hated to talk about that. Plus with our cultural background they don't like to talk about it.
(Male, Caregiver)
She was actually very grateful for the way that the doctor spoke to her… and I think all of us that were in that chemo room with all the other women, we recognised that in him, that that's the way he operated and I think everybody appreciated that kind of honesty.
(Female, Caregiver)
3.7. Competent and caring health professionals
Participants identified that a consultative, patient‐centred care approach was critical. They stated that health professionals, who were compassionate, respectful, and ensured patient dignity, played a significant role in providing quality EOL care to patients and caregivers.
…Good relationships with the primary health team is what I think is absolutely essential…. …A good relationship someone who understands you and understands the family and who will work with other professionals….
(Female, Motor Neuron Disease)
She came in to find her with an oxygen mask on and we had said no resuscitation. The doctor said something like she won't need that anymore and walked out the door. That was how my sister discovered mum had died.
(Female, Caregiver)
4. DISCUSSION
The priorities for high‐quality EOL care identified by the study participants, who were caregivers of people who have had or are experiencing terminal conditions or patients who were suffering from a terminal illness themselves were as follows: quality as a priority, sense of control, how to manage life on hold, need for health system support being able to remain at home if possible, talking about death to know what patient wishes are, and having competent and caring health professionals. In particular, our data highlight the importance of knowing and adhering to patient's wishes (if known) when providing EOL care.
Our findings reinforce the call for patient‐centred care, that is, health care that is responsive to the preferences, needs and values of each patient33 regardless of whether the goals of care are curative and interventional or focused on a palliative approach. Our findings also support the need to include consumer voices in facilitating health service improvement.34
According to other research with terminal patients and their caregivers, priorities for high‐quality EOL care have included the following: the need for professional communication, honest consultation on preferences, respect for patient dignity, support in navigating the health system, control in decision‐making, consideration of the burden on family life, and access to skilled health practitioners who are good communicators.35, 36, 37, 38 A systematic review in 2015 of quantitative studies in Canada, US and the UK aiming to find the most important aspects of inpatient EOL care of palliative patients and their family found similar results to our study in Australia.23 Since that review, we identified two relevant qualitative studies which included people in the United Kingdom with dementia39and caregivers of people with advance cancer in Australia.40 Despite the disease‐specific study populations, there were similarities between our study which included caregivers and terminally ill who were suffering a broad range of terminal conditions and the themes identified in the dementia and cancer populations which included the following: being at home (or a home‐like environment) at the EOL; competent and skilled health professionals at the EOL; being comfortable as important components of good EOL care;39 and the readiness of caregivers to engage in EOL discussions.40
In our qualitative study, participants strongly favoured higher quality supportive care as opposed to prolonging life at all costs, which is consistent with an Australian survey finding that the majority of older adults believe quality of life is “paramount.”14 However, participants reported that when making decisions about prolonging life there was inconsistency in the degree to which patient and family had been involved in EOL care contexts. Specifically, participants reported that, health professionals did not always follow patient wishes and advance directives. Factors have been identified before as contributing to this limited involvement of health consumers such as a lack of clear written documentation to facilitate decision making at the time of admission;41 clinician‐consumer divergent opinion on the prognosis or interpretation of the words “terminal”;42 pressure from relatives;43 and the relationship between the health professional, patient and caregiver.44
The preference to be at home for their EOL care reported in our study is consistent with Foreman and colleagues population survey in Australia over a decade ago that reported 70% of Australians preferred home as a place of death if suffering from a terminal illness.45 Yet as Pollock46 (2015) identifies, there are difficulties with regard to the management of severe symptoms away from hospitals. Our participants were aware that in many cases, home death was not possible due to the challenges of an EOL context, including the increasing care needs as the person deteriorates, the patient‐provider relationship, the role and feelings of family or friends who were caregivers, and the availability or feasibility of the health system to provide particular services. Our caregivers also expressed the need for system support to navigate the health‐care system for loved ones which they often felt unprepared for. Jeff's47 et al (2017) found similar results in Canadian caregivers of older adults that reported complexity and challenges navigating the health system during interfacility care transitions.
Recent evidence indicates that the use of early community‐based palliative care referrals is associated with a reduction in hospital emergency department use in patients with dementia in the last year of life48 and in reducing cancer patients’ transfer to acute hospitals in the last 90 days before death.49 Consistent with our consumers’ preferences, the provision of a palliative care approach in any setting including home‐based has shown to enhance satisfaction and increase the likelihood of death at home50 as well as being more cost‐effective.51 However, existing models of EOL care for frail older adults would require significant changes to be implemented according to patient's wishes if many prefer to die at home.52 As is described in the national consensus statement for safe and high‐quality EOL care, with an ageing population, a reorganization of care and the way we manage terminal patients is required.28
Despite recommendations on addressing EOL care outside of acute care settings that respect patient preferences to die at home and support informal caregivers,53 many patients still spend their last days in an acute hospital.54 Most western health systems do not appear ready for widespread community supported palliative care, as illustrated by previously reported barriers; the absence of skilled EOL workforce outside specialist health‐care facilities;55 substantial out‐of‐pocket costs of residential aged care;56 and the lack of infrastructure to meet demand in countries with universal health care has resulted in long waiting lists for eligibility assessment.57, 58 Failures in organisations to support advanced care planning in partnership with patients, along with ineffective communication will continue to prevent optimal and safe EOL care for the frail older adults.
This qualitative study involved public consultation and representation of views including those of different ages, ethnicity and experience of health care. Involving older people as advisors has shown to enhance the relevance of health services research.34 The information collected in our consultation covered recent experiences in the health system and home settings and is of relevance for clinicians and health service planners. IDI supplemented the FGD findings with extensive details from less physically mobile health service consumers.
A possible limitation of our study is that the majority of participants were females and caregivers. However, as females are often the informal caregivers of chronically ill patients36, this may in fact be representative of the reality of informal caregivers. The fact that we only conducted three FGD could also be considered as a limitation; however, saturation was rapidly achieved even with three FGD. While our study confirmed that consulting patients and families about this sensitive topic is feasible in Australia, this consultation did not happen at a time of acute medical crisis. It could be argued that our study did not take into account patient and family preferences at those critical times, as studies have shown that preferences can change over time depending on a person's state of health.59 However, we believe the views our participants are further enriched by the ability for retrospection without the influence of an acute emotion.
5. CONCLUSIONS
This consultation identified priorities and preferences by consumers through their experiences of the delivery of EOL care. It confirmed that the health system still faces two persistent barriers to the delivery of satisfactory, safe and high‐quality end‐of life‐care for consumers: shortage of strategies to address the unmet needs of terminally ill older adults and caregivers, and the need for health professionals to deliver more skilled communication incorporating personal values. Unfounded perceptions that patients and carers are not open to EOL conversations or shared decisions on goals of care at the EOL such as limitations of treatment need to be revisited. With an ageing population, a reorganization of care to optimize the way we manage terminal patients is overdue. The readiness of patients and families for proactive engagement in advance care planning represents an opportunity to slow down unsustainable public demands for aggressive care and promote effective communication to prevent suboptimal and unsafe EOL care for the frail older adults.
ETHICAL APPROVAL
Ethics approval was granted by the University of New South Wales Human Research Ethics Advisory Panel (HREAP # HC16159).
INFORMED CONSENT
Informed consent was obtained from all individual participants included in the study.
ACKNOWLEDGEMENTS
We thank members of the consumer advisory group for their insightful contributions to this research. Mr Chhorvoin Om provided initial assistance with concurrent thematic interpretation of data from one of the focus groups.
CONFLICT OF INTEREST
The authors declare they have no conflict of interest.
Supporting information
Lewis ET, Harrison R, Hanly L, et al. End‐of‐life priorities of older adults with terminal illness and caregivers: A qualitative consultation. Health Expect. 2019;22:405–414. 10.1111/hex.12860
Funding Information
This work was supported by a grant from the National Health and Medical Research Council of Australia (grant number 1054146). The sponsor had no role in the design, methods, subject recruitment, data collection, analysis or decision to publish.
REFERENCES
- 1. Feng Z, Coots LA, Kaganova Y, Wiener JM. Hospital and ED use among medicare beneficiaries with dementia varies by setting and proximity to death. Health Aff. 2014;33:683‐690. [DOI] [PubMed] [Google Scholar]
- 2. Luta X, Maessen M, Egger M, Stuck AE, Goodman D, Clough‐Gorr KM. Measuring intensity of end of life care: a systematic review. PLoS ONE. 2015;10:e0123764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Cardona‐Morrell M, Kim J, Anstey M, Mitchell I, Hillman K. Non‐ beneficial treatments in hospital at the end of life – A systematic review and meta‐analysis on extent of the problem. Int J Qual Health Care. 2016;28:456‐469. [DOI] [PubMed] [Google Scholar]
- 4. Goodman DC, Fisher ES, Morden NE, Jacobson JO, Mpp KM, Bronner KK. Quality of end‐of‐life cancer care for medicare beneficiaries regional and hospital‐specific analyses. Labanon NH: Dartmouth Institute for Health Policy and Clinical Practice; 2010. [PubMed] [Google Scholar]
- 5. Parker SM, Clayton JM, Hancock K, et al. A systematic review of prognostic/End‐of‐life communication with adults in the advanced stages of a life‐limiting illness: patient/caregiver preferences for the content, style, and timing of information. J Pain Symptom Manage. 2007;34:81‐93. [DOI] [PubMed] [Google Scholar]
- 6. Curtis JR. Communicating about end‐of‐life care with patients and families in the intensive care unit. Crit Care Clin. 2004;20:363‐380, viii. [DOI] [PubMed] [Google Scholar]
- 7. McDonagh JR, Elliott TB, Engelberg RA, et al. Family satisfaction with family conferences about end‐of‐life care in the intensive care unit: increased proportion of family speech is associated with increased satisfaction. Crit Care Med. 2004;32:1484‐1488. [DOI] [PubMed] [Google Scholar]
- 8. Brazil K, Howell D, Bedard M, Krueger P, Heidebrecht C. Preferences for place of care and place of death among informal caregivers of the terminally ill. Palliat Med. 2005;19:492‐499. [DOI] [PubMed] [Google Scholar]
- 9. Seifart C, Hofmann M, Bar T, Riera Knorrenschild J, Seifart U, Rief W. Breaking bad news‐what patients want and what they get: evaluating the SPIKES protocol in Germany. Ann Oncol. 2014;25:707‐711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. You JJ, Downar J, Fowler RA, et al. Barriers to goals of care discussions with seriously ill hospitalized patients and their families: a multicenter survey of clinicians. JAMA Intern Med. 2015;175:549‐556. [DOI] [PubMed] [Google Scholar]
- 11. Willmott L, White B, Smith MK, Wilkinson DJ. Withholding and withdrawing life‐sustaining treatment in a patient's best interests: Australian judicial deliberations. Med J Aust. 2014;201:545‐547. [DOI] [PubMed] [Google Scholar]
- 12. Long AC, Curtis JR. Enhancing informed decision making: is more information always better? Crit Care Med. 2015;43:713‐714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Cohen CJ, Chen Y, Orbach H, Freier‐Dror Y, Auslander G, Breuer GS. Social values as an independent factor affecting end of life medical decision making. Med Health Care Philos. 2015;18:71‐80. [DOI] [PubMed] [Google Scholar]
- 14. Corke C. Personal values profiling and advance care planning. BMJ Supportive & Palliative Care. 2013;3:226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Zier LS, Burack JH, Micco G, Chipman AK, Frank JA, White DB. Surrogate decision makers’ responses to physicians’ predictions of medical futility. Chest. 2009;136:110‐117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mold JW. Facilitating shared decision making with patients. Am Fam Physician. 2006;74(1209–1210):1212. [PubMed] [Google Scholar]
- 17. Hillman K, Chen J. Conflict resolution in end of life treatment decisions: an Evidence Check rapid review brokered by the Sax Institute for the Centre for Epidemiology and Research. Sydney: The Sax Institute; 2008. [Google Scholar]
- 18. Gordon M, Perri G. Conflicting demands of family at the end of life and challenges for the palliative care team. Annals of Long‐Term Care. 2015;23:25‐28. [Google Scholar]
- 19. Baile WF, Buckman R, Lenzi R, Glober G, Beale EA, Kudelka AP. SPIKES—a six‐step protocol for delivering bad news: application to the patient with cancer. Oncologist. 2000;5:302‐311. [DOI] [PubMed] [Google Scholar]
- 20. Proulx K, Jacelon C. Dying with dignity: the good patient versus the good death. Am J Hosp Palliat Care. 2004;21:116‐120. [DOI] [PubMed] [Google Scholar]
- 21. Steinhauser KE, Clipp EC, McNeilly M, Christakis NA, McIntyre LM, Tulsky JA. In search of a good death: observations of patients, families, and providers. Ann Intern Med. 2000;132:825‐832. [DOI] [PubMed] [Google Scholar]
- 22. Kehl KA. Moving toward peace: an analysis of the concept of a good death. Am J Hosp Palliat Care. 2006;23:277‐286. [DOI] [PubMed] [Google Scholar]
- 23. Virdun C, Luckett T, Davidson PM, Phillips J. Dying in the hospital setting: a systematic review of quantitative studies identifying the elements of end‐of‐life care that patients and their families rank as being most important. Palliat Med. 2015;29:774‐796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Brinkman‐Stoppelenburg A, Rietjens JAC, van der Heide A. The effects of advance care planning on end‐of‐life care: a systematic review. Palliat Med. 2014;28:1000‐1025. [DOI] [PubMed] [Google Scholar]
- 25. Kearns T, Cornally N, Molloy W. Patient reported outcome measures of quality of end‐of‐life care: a systematic review. Maturitas. 2017;96:16‐25. [DOI] [PubMed] [Google Scholar]
- 26. Christensen K, Doblhammer G, Rau R, Vaupel JW. Ageing populations: the challenges ahead. The Lancet. 2009;374:1196‐1208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Mitchell GK. Palliative care in Australia. The Ochsner Journal. 2011;11:334‐337. [PMC free article] [PubMed] [Google Scholar]
- 28. Australian Commission on Safety and Quality in Health Care . National Consensus Statement: Essential elements for safe and high‐quality end‐of‐life care In: ACSQHC, ed2015
- 29. Rosenwax L, Spilsbury K, McNamara BA, Semmens JB. A retrospective population based cohort study of access to specialist palliative care in the last year of life: who is still missing out a decade on? BMC Palliative Care. 2016;15:46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Australian Bureau of Statistics . Census of Population and Housing: Reflecting Australia ‐ Stories from the Census, 2016. (no.2071.0). 2018.
- 31. Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Research in Psychology. 2006;3:77‐101. [Google Scholar]
- 32. Lambert C, Jomeen J, McSherry W. Reflexivity: A review of the literature in the context of midwifery research. British Journal of Midwifery. 2010;18:321‐326. [Google Scholar]
- 33. Epstein RM, Fiscella K, Lesser CS, Stange KC. Why the nation needs a policy push on patient‐centered health care. Health Aff. 2010;29:1489‐1495. [DOI] [PubMed] [Google Scholar]
- 34. Backhouse T, Kenkmann A, Lane K, Penhale B, Poland F, Killett A. Older care‐home residents as collaborators or advisors in research: a systematic review. Age Ageing 2016;45:337‐345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Abdul‐Razzak A, Sherifali D, You J, Simon J, Brazil K. ‘Talk to me’: a mixed methods study on preferred physician behaviours during end‐of‐life communication from the patient perspective. Health Expect. 2016;19:883‐896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Sautter JM, Tulsky JA, Johnson KS, et al. Caregiver experience during advanced chronic illness and last year of life. J Am Geriatr Soc. 2014;62:1082‐1090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Periyakoil VS, Eric N, Helena K. Patient‐reported barriers to high‐quality, end‐of‐life care: a multiethnic, multilingual, mixed‐methods study. J Palliat Med 2016;19:373‐379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Simon J, Porterfield P, Bouchal SR, Heyland D. ‘Not yet’ and ‘Just ask’: barriers and facilitators to advance care planning—a qualitative descriptive study of the perspectives of seriously ill, older patients and their families. BMJ Support Palliat Care. 2015;5:54‐62. [DOI] [PubMed] [Google Scholar]
- 39. Poole M, Bamford C, McLellan E, et al. End‐of‐life care: a qualitative study comparing the views of people with dementia and family carers. Palliat Med. 2017;32:631‐642. [DOI] [PubMed] [Google Scholar]
- 40. Collins A, McLachlan S‐A, Philip J. How should we talk about palliative care, death and dying? A qualitative study exploring perspectives from caregivers of people with advanced cancer. Palliat Med. 2017;32:861‐869. [DOI] [PubMed] [Google Scholar]
- 41. Nyman DJ, Sprung CL. End‐of‐life decision making in the intensive care unit. Am J Respir Crit Care Med. 2000;26:1414‐1420. [DOI] [PubMed] [Google Scholar]
- 42. Messinger‐rapport B, Baum E, Smith M. Advance care planning: beyond the living will. Clevel Clin J Med. 2009;76:276‐285. [DOI] [PubMed] [Google Scholar]
- 43. Hardin SB, Yusufaly YA. Difficult end‐of‐life treatment decisions: do other factors trump advance directives? Arch Intern Med. 2004;164:1531‐1533. [DOI] [PubMed] [Google Scholar]
- 44. Caswell G, Pollock K, Harwood R, Porock D. Communication between family carers and health professionals about end‐of‐life care for older people in the acute hospital setting: a qualitative study. BMC Palliative Care. 2015;14:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Foreman LM, Hunt RW, Luke CG, Roder DM. Factors predictive of preferred place of death in the general population of South Australia. Palliat Med. 2006;20:447‐453. [DOI] [PubMed] [Google Scholar]
- 46. Pollock K. Is home always the best and preferred place of death? BMJ (Clinical research ed). 2015;351:h4855. [DOI] [PubMed] [Google Scholar]
- 47. Jeffs L, Saragosa M, Law MP, Kuluski K, Espin S, Merkley J. The role of caregivers in interfacility care transitions: a qualitative study. Patient Prefer Adherence. 2017;11:1443‐1450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Rosenwax L, Spilsbury K, Arendts G, McNamara B, Semmens J. Community‐based palliative care is associated with reduced emergency department use by people with dementia in their last year of life: a retrospective cohort study. Palliat Med. 2015;29:727‐736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. McNamara BA, Rosenwax LK, Murray K, Currow DC. Early Admission to Community‐Based Palliative Care Reduces Use of Emergency Departments in the Ninety Days before Death. J Palliat Med. 2013;16:774‐779. [DOI] [PubMed] [Google Scholar]
- 50. Brumley R, Enguidanos S, Jamison P, et al. Increased satisfaction with care and lower costs: results of a randomized trial of in‐home palliative care. J Am Geriatr Soc. 2007;55:993‐1000. [DOI] [PubMed] [Google Scholar]
- 51. Smith S, Brick A, O'Hara S, Normand C. Evidence on the cost and cost‐effectiveness of palliative care: a literature review. Palliat Med. 2014;28:130‐150. [DOI] [PubMed] [Google Scholar]
- 52. Katelaris A. Time to rethink end‐of‐life care [Editorial]. Med J Aust. 2011;194:563. [DOI] [PubMed] [Google Scholar]
- 53. Gray B. England's approach to improving end‐of‐life care: a strategy for honoring patients’ choices. The Commonwealth Fund 2011;15:1‐13. [PubMed] [Google Scholar]
- 54. De Roo ML, Miccinesi G, Onwuteaka‐Philipsen BD, et al. Actual and preferred place of death of home‐dwelling patients in four european countries: making sense of quality indicators. PLoS ONE. 2014;9:e93762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Duffield CM, Twigg DE, Pugh JD, Evans G, Dimitrelis S, Roche MA. The Use of unregulated staff: time for regulation? Policy Polit Nurs Pract. 2014;15:42‐48. [DOI] [PubMed] [Google Scholar]
- 56. Kelley AS, McGarry K, Fahle S, Marshall SM, Du Q, Skinner JS. Out‐of‐pocket spending in the last five years of life. J Gen Intern Med. 2013;28:304‐309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Henderson EJ, Caplan GA. Home sweet home? community care for older people in Australia. J Am Med Dir Assoc. 2008;9:88‐94. [DOI] [PubMed] [Google Scholar]
- 58. Taylor C, Donoghue J. New ways to provide community aged care services. Australas J Ageing. 2015;34:199‐200. [DOI] [PubMed] [Google Scholar]
- 59. Glass DC, Kelsall HL, Slegers C, et al. A telephone survey of factors affecting willingness to participate in health research surveys. BMC Public Health. 2015;15:1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


