Abstract
Acromioclavicular joint (ACJ) injury is a common shoulder injury. There are various techniques of ACJ reconstruction. Superficial infection after ACJ reconstruction is not an uncommon complication. However, osteomyelitis post ACJ reconstruction has never been highlighted as a possible complication. Our patient is a 31-year-old male who sustained a Rockwood 5 ACJ dislocation and had anatomical ACJ reconstruction with autogenous gracilis and semitendinosus graft. Our technique involved the anatomical reconstruction of the ACJ and the coracoclavicular ligament with the usage of two bioscrews and the temporary stabilisation of the ACJ with two k-wires. As in any orthopaedic surgery, infection is often disastrous especially when the surgery involves implants. It can be disastrous with high morbidity to the patient as well as a costly complication to treat. Therefore, we wish to highlight this case as despite its rarity, osteomyelitis can be devastating to the patient and should be prevented if possible.
Keywords: Acromioclavicular joint dislocation, Acromioclavicular joint reconstruction, Infection, Osteomyelitis, Complication
Introduction
There are various techniques of acromioclavicular joint (ACJ) reconstruction. Infection after ACJ reconstruction is a possible complication. However, osteomyelitis post acromioclavicular joint anatomical reconstruction has never been highlighted as a possible complication. We wish to report a case of osteomyelitis post anatomical ACJ reconstruction with autogenous gracilis and semitendinosus graft.
Case report
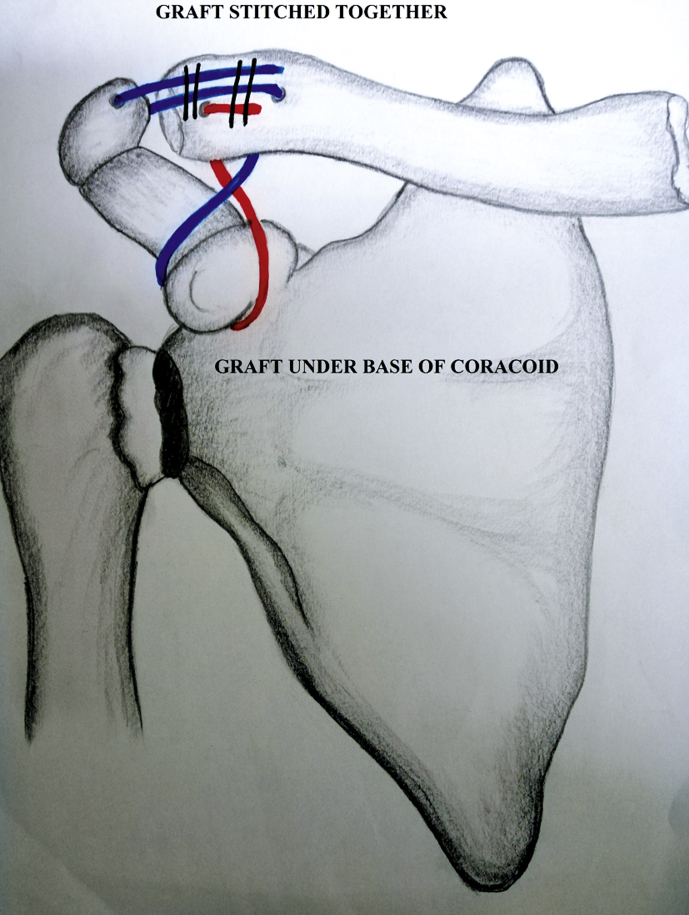
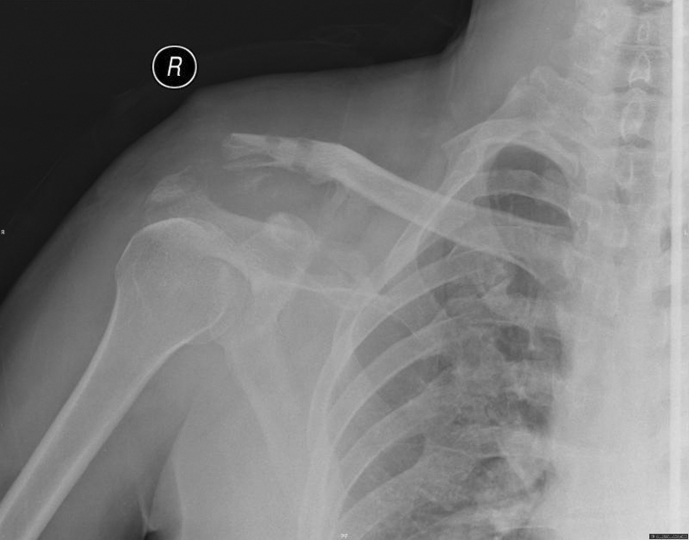
A 31 year-old male, right hand dominant forklift operator, was involved in a motor vehicle accident where he sustained polytrauma with right acromioclavicular joint disruption (Rockwood 5) (Fig. 1). He subsequently underwent anatomical ACJ reconstruction. We performed the case in a semi reclined position with the arm by the side. Gracilis and semitendinosus autograft were harvested from the knee. A bra strap incision was made 1–2 cm medial to the ACJ extending to the coracoid process. A ‘T’ incision is made on the clavicle with subperiosteal elevation over the muscle, fascia and capsule. The coracoid process and its medial and lateral borders were identified. Two tunnels for the clavicle and one for the acromion were drilled. Bone tunnels were then created over the clavicle 25 mm from the ACJ in the centre of the clavicle, the other 35 mm from the ACJ, more posteriorly. The acromion bone tunnel were created 10mm from the ACJ. The auto graft was then passed under the coracoid process after crossing the graft and through the bone tunnels. The bone tunnel was then secured with a PEEK tenodesis screw (Arthrex, Naples, Florida) 25mm from the ACJ. The remaining graft was passed from the superior surface of the clavicle to the undersurface of the acromion and then pulled onto the superior surface of the acromion (Fig. 2). Two kirchner wires were then passed from the acromion to the clavicle stopping short of the PEEK tenodesis screw (Arthrex, Naples, Florida) (Fig. 3). Another PEEK tenodesis screw (Arthrex, Naples, Florida) was the inserted in the clavicular bone tunnel 35mm from the ACJ with the autograft under tension. The autograft that was pulled onto the superior surface of the acromion was then sutured to itself medially. The wound was irrigated and closed in layers. The surgery was uneventful and patient was discharged two days after the surgery (Fig. 4). Postoperative one week, the patient claimed that he noted that the wire became loosened but did not seek medical advice. Postoperative two weeks, one of the wires was dislodged and patient then sought medical advice. On further questioning, the patient admitted that he had not been doing dressing for the pin sites and left them uncovered. We noted that there was erythema around the pin sites and pus tracking out of them. The second kirschner wire was then removed together with the sutures. Patient was then admitted for intravenous (iv) cefuroxime. The inflammatory markers on admission were total white cell of 8.8 × 109/L, c-reactive protein of 19.26 mg/L and erythrocyte sedimentation rate of 78 mm/h. The wound culture and sensitivity (c&s) which was taken grew methicillin resistant staphylococcus aureus (MRSA) after three days of incubation and the patient was then started on iv vancomycin. After five days of antibiotic, wound inspection revealed two sinuses overlying the wound with seropurulent discharge over the pin sites. The radiograph showed bony erosion over the distal clavicle and acromion (Fig. 5). Patient was then planned for wound debridement. Twelve days after the initial wound debridement, patient had another wound debridement and the autograft as well as the tenodesis screw implants were removed. Intra-operative findings showed unhealthy autograft tissue towards the pin site with the most lateral screw loosened leaving the medial screw intact (Fig. 6). Both screws were removed. Immediate range of movement exercises were allowed and started post-operatively. However, repeat wound c&s taken intra-operatively grew extended spectrum beta lactamase (ESBL) Klebsiella pneumonia. Patient was then started on iv meropenem and vancomycin was stopped and replaced with oral fusidic acid. Post-operative day eleven, the patient completed seventeen days of iv vancomycin, eleven days of iv meropenem and twenty-four days of oral fusidic acid. The wound was clean with no slough or pus discharge. However, repeat radiograph showed osteomyelitis with extensive bony erosion over the distal clavicle and acromion (Fig. 7). Patient was then allowed home and was asked to complete another three weeks of oral unasyn. During his follow-up, the wound did not heal and the patient required another wound debridement and antibiotic loaded cement beads were inserted. The wound c&s grew MRSA. However, the bone and tissue c&s taken intra-operatively grew pseudomonas aeruginosa which was sensitive to ceftazidime and gentamicin. Patient was started on iv vancomycin and iv ceftazidime. The antibiotic loaded cement beads were then removed two weeks later and repeat bone and tissue c&s showed no growth. The patient was then discharged after completing three weeks of iv antibiotics and was told to complete another three weeks of oral fusidic acid and rifampicin. The inflammatory markers on discharge were total white cell of 3.2 × 109/L, c-reactive protein of 6.51 mg/L and erythrocyte sedimentation rate of 10 mm/h. The patient is under our surveillance and was symptom free with full range of motion on his last follow-up. Patient however complained of weakness on lifting heavy objects and was not keen for a revision surgery.
Fig. 1.
Preoperative radiograph showing acromioclavicular joint dislocation (Rockwood 5).
Fig. 2.
Sketch showing surgical technique of anatomical ACJ reconstruction without the kirchner wires.
Fig. 3.
Sketch showing position of kirchner wires after placement of autograft.
Fig. 4.

Postoperative radiograph post anatomical ACJ reconstruction with two kirchner wires in-situ.
Fig. 5.
Postoperative radiograph post removal of kirchner wires at 4 weeks showing early osteomyelitic changes to the distal clavicle and acromion with erosion of the bone.
Fig. 6.

Intra-operative findings showed unhealthy and infected semitendinosus and gracilis autograft tissue which were removed.
Fig. 7.
Postoperative radiograph post removal of kirchner wires at 5 weeks showing extensive osteomyelitic changes to the distal clavicle and acromion with extensive erosion of the bone.
Discussion
ACJ injury is a common shoulder injury and approximately 9% of the shoulder girdle injury involve the ACJ.1 If treated operatively, there are numerous techniques of performing an acromioclavicular joint reconstruction and none can represent the gold standard of treatment. Clavert et al.2 reported a 22.4% overall complication rate and as high as 41% in radiological loss of reduction. Another study reported a 27.1% overall complication rate with 23.7% of the patients requiring a second surgery.3 Our technique utilized two tunnels with the usage of the semitendinosus and gracilis autograft in reconstructing the coracoclavicular and acromioclavicular ligaments. This technique enabled vertical stability by the coracoclavicular ligament reconstruction and horizontal stability by AC ligament reconstruction. The acromioclavicular joint were held in place with two kirchner wires while awaiting the incorporation of the autograft. The kirchner wires were then left for six weeks with daily pin site dressing. While infection in ACJ reconstruction is not uncommon and ranges from 0 to 9%, osteomyelitis is rarely reported.4, 5 We believe that one of the causes of infection could be due to the fact that the patient had got poor hygiene and did not perform daily pin site dressing. This had led to devastating infection with multiple bacterial organism requiring prolonged antibiotics treatment as well as multiple surgeries to eradicate the infection. While this technique has served us well in most of our case, this single case of osteomyelitis has caused us to rethink our technique of temporary stabilising the ACJ with kirchner wires. We recommend the usage of a cerclage wire instead of kirchner wires to hold the acromioclavicular joint in place while awaiting the incorporation of the autograft. The disadvantage of this technique remains that we have to remove the cerclage wire at a later date. Patient education on the recognition of the signs of infection with subsequent prompt treatment may improve the outcome as well.
ACJ reconstruction is a surgery with various possible complications. As in any orthopaedic surgery, infection is often disastrous especially when the surgery involves implants. It can be disastrous with high morbidity to the patient as well as a costly complication to treat. We believe that our technique is not the gold standard for the treatment of ACJ injuries and the gold standard remains elusive. We wish to highlight this case as despite its rarity, osteomyelitis can be devastating to the patient and should be prevented if possible.
Funding
Nil.
Acknowledgments
We wish to acknowledge the patient for his consent for the publication of this case report and any accompanying images.
Footnotes
Peer review under responsibility of Chinese Medical Association.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.cjtee.2019.03.004.
Ethical statement
Patient's consent for the publication of this case report and any accompanying images has been obtained.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Rockwood C.A., Jr. Disorders of the acromioclavicular joint. In: Rockwood C.A. Jr., Matsen F.A. III, editors. The Shoulder. WB Saunders; Philadelphia: 1985. pp. 413–476. [Google Scholar]
- 2.Clavert P., Meyer A., Boyer P. Complication rates and types of failure after arthroscopic acute acromioclavicular dislocation fixation. Prospective multicenter study of 116 cases. Orthop Traumatol Surg Res. 2015;101(suppl):S313–S316. doi: 10.1016/j.otsr.2015.09.012. [DOI] [PubMed] [Google Scholar]
- 3.Martetschläger F., Horan M.P., Warth R.J. Complications after anatomic fixation and reconstruction of the coracoclavicular ligaments. Am J Sports Med. 2013;41:2896–2903. doi: 10.1177/0363546513502459. [DOI] [PubMed] [Google Scholar]
- 4.Provencher M., LeClere L., Romeo A. Springer; 2009. Avoiding and Managing Complications of Surgery of the Acromioclavicular Joint. [Google Scholar]
- 5.Neault M.A., Nuber G.W., Marymont J.V. Infections after surgical repair of acromioclavicular separations with nonabsorbable tape or suture. J Shoulder Elb Surg. 1996;5:477–478. doi: 10.1016/s1058-2746(96)80021-8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.