Abstract
Purpose
Glenoid bone defect and the defect on the posterior-superior surface of the humerus “Hill-Sachs lesion” are the commonly seen bony lesions in patients with recurrent dislocation shoulder. Computed tomography (CT) scan is considered as the best option in assessing the bony defects in the recurrent dislocation shoulder. The aim of this study was to assess the clinical and radiological co-relation in the patients with recurrent dislocation shoulder.
Methods
Forty-four patients of recurrent dislocation shoulder who were evaluated between January 2015 and December 2017 at a tertiary care center, clinically and radiologically using CT scan and meeting the inclusion criteria, were included. The correlation between the clinical history of the number of dislocations and the bone loss using CT scan was evaluated. Two sided statistical tests were performed at a significance level of α = 0.05. The analysis was conducted using IBM SPSS STATISTICS (version 22.0).
Results
All the patients were male with mean age of 25.95 (SD ± 4.2) years were evaluated. Twenty-four patients sustained injury in sporting activities while 20 patients sustained injury in training. There were an average of 4.68 (SD ± 3.1, range 2–15, median 3) episodes of dislocation. Forty-one patients had the glenoid bone loss while 40 had the Hill-Sachs lesions. The mean glenoid width defect was 10.80% (range 0–27%) while the mean Hill-Sachs defect was 14.27 mm (range 0–26.6 mm). The mean area of bone loss of the glenoid surface was 10.81% (range 0–22.4%). The lesions were on track in 34 patients and off track in 10 patients.
Conclusions
CT scan of the shoulder joint is an effective method for assessing the amount of bone loss. The number of dislocations are correlated significantly with off-track lesions and the amount of bone loss on the glenoid and Hill-Sachs lesion. The glenoid width bone loss of more than 9.80% or Hill-Sachs defect of more than 14.80 mm are the critical defects after which the frequency of dislocations increases.
Keywords: Shoulder joint, Recurrent dislocation, Hill-Sachs lesion
Introduction
Recurrent dislocation of the shoulder joint (RDS) is a common injury in athletes and military personals who are involve in the rigorous activities.1 Bony defects of the glenoid and the defect on the posterior-superior surface of the humerus “Hill-Sachs lesion” are the common bony lesions in these patients.2 The amount of bone loss is considered as a significant risk factor for the recurrence of the instability of shoulder joint.3 Recently, Yamamoto et al.4, 5 have given the concept of glenoid track, and bony defect on the humeral and glenoid side in combination are considered as the bipolar bone lesion and the prognosis of shoulder instability is considered as inversely proportional to the amount of bipolar bone loss.
Various modalities have been used to assess the amount of bone loss like plain radiograph (X-ray), computerized tomography (CT) scan, and magnetic resonance imaging (MRI).6 X-ray is easily available, cheap but less accurate in assessing the amount of bone loss.7 CT scan is considered a better option than X-ray but it is associated with higher radiation exposure. MRI is another good option for assessing bony as well as soft tissue lesions. However, CT scan is considered as the best option for assessing the bony defects in the recurrent shoulder dislocation.6
The aim of this study was to assess the amount of bone loss using CT scan in patients with RDS and its correlation with clinical findings.
Methods
Study design
The current study was an observational study of the high demand personals with a history of RDS who were evaluated at tertiary care center during the period between January 2015 and December 2017. In all the patients planned for surgical intervention, MRI and CT scan of the shoulder were performed. The lesions of glenoid labrum, rotator cuff, biceps and superior labrum anterior and posterior (SLAP) were evaluated using MRI. While the CT scan of the shoulder was used to evaluate the glenoid and Hill-Sachs bone loss.
The inclusion criteria for this study: symptomatic cases of traumatic RDS; patients willing to participate. The exclusion criteria: bilateral RDS; patients who were operated earlier for any shoulder pathology; osteoarthritis of the shoulder joint; associated rotator cuff tear; posterior RDS; multi-directional or atraumatic RDS; patients with generalized ligamentous laxity.
Methodology
CT scans of both the shoulders of patients with symptomatic RDS were analyzed in this study. The clinical history of the patients was correlated with CT scan of the shoulder joint. The clinical evaluation included the age of the patient, side of involvement, mode of injury at the time of the first episode, number of episodes, the time between the first episode and CT scan.
The CT scans of shoulder joint were performed bilaterally pre-operatively in the supine position with the field of view covering both the shoulder joints. Axial and oblique coronal image (plane showing the maximum surface area of glenoid) reconstruction in 1 mm thin slices were obtained using 16 slice multi detector CT machine (Philips Brilliance 16 slice CT scanner, Netherland).
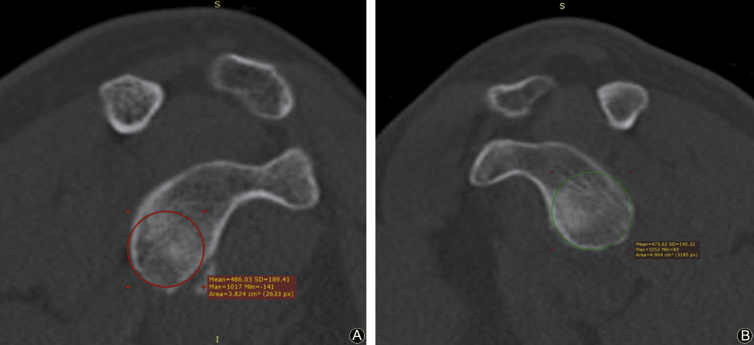
The area of bone loss of the glenoid surface was measured in oblique coronal images using the best-fit circle to inferior glenoid margin. It was compared with opposite normal glenoid surface area (Fig. 1A, B).8
Fig. 1.
Method of glenoid surface area measurement by ‘best fit circle surface area’: (A) Abnormal side (3.824 cm2), (B) Normal side (4.904 cm2).
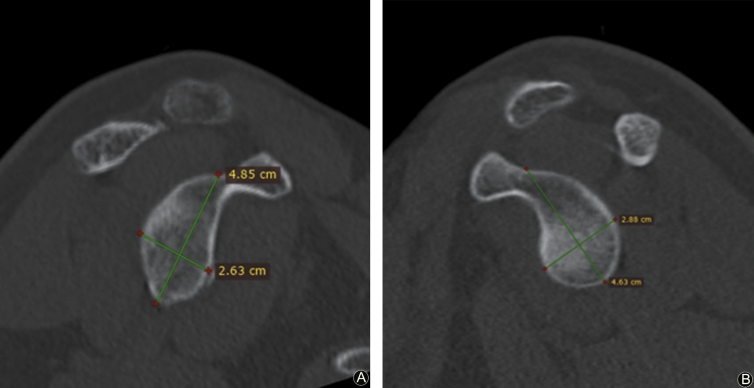
The width loss measurements of glenoid were performed using the Griffith index in which both the shoulders were compared and percentage bone loss was calculated. (Fig. 2 A, B).9, 10, 11
Fig. 2.
(A) (B) Glenoid width loss measurement using Griffith index - width measurements are made perpendicular to a line through the vertical axis of the glenoid and compared to the uninjured glenoid (injured width/normal width × 100) to determine percent width loss. (i.e. 2.63/2.88 × 100 = 91.32%, about 8.7% loss as compared to normal side).
One mm thin reconstructions of the humeral head in coronal plane were obtained from high-resolution axial images. The Hill-Sachs defect was measured corresponding to the largest size of the humeral defect in the coronal plane (Fig. 3).12
Fig. 3.
Method of Hill-Sachs defect measurement.
The bone loss of shoulder joint was labelled as on-track or off-track lesion on the basis of the amount of bipolar lesions.5 If the Hill-Sachs lesion remains on the glenoid surface (glenoid track) or the size of the Hill-Sachs lesion was smaller than the width of the glenoid, it was a non-engaging lesion and less likely to cause dislocation. Hence called as the on-track lesion.13 While if the lesion of Hill-Sachs goes out of (medial to) glenoid surface (glenoid track) or if the size of the Hill-Sachs lesion was more than the width of the glenoid. These lesions were engaging or off-track lesions.13
The correlation between the clinical history of the number of dislocations and the bone loss was evaluated in the present study.
Statistical analysis
Discrete categorical data were presented as n (%). Proportions were compared using Chi-square or Fisher's exact test whichever was applicable. The continuous data were given as mean ± SD, range or median and interquartile range, as appropriate. Normality of quantitative data was checked by measures of Kolmogorov Smirnov tests of normality. Normally distributed Student’s t-test was applied to compare 2 groups (track off/on). All statistical tests were two-sided and performed at a significance level of α = 0.05. The analysis was conducted using IBM SPSS STATISTICS (version 22.0).
The sample size was estimated based on assumption that the prevalence of recurrent dislocation shoulder is 1.7% in general population.16 To estimate this proportion with a 95% confidence interval (CI) of proportion & margin of error as 5% the sample size required was 30 subjects using the formula
Where: n0 is the sample size; z is the value for the selected alpha level, i.e. 1.96 for (0.05) at 95% confidence level. p is the estimated proportion of an attribute that is present in the population; q is 1-p; d is the acceptable margin of error for proportion being estimated.
Results
The study included 44 male patients who were evaluated clinically and radiologically at our center.
The average age of the patient at the time of first episode of dislocation was 25.95 years (SD ± 4.2 years). The mean height of the patients was 172.81 cm (range 164–184 cm). Twenty-four patients sustained the injury during sports (handball, volleyball, kabaddi, basketball, etc.). While 20 patients sustained the injury during training (fall from height/vertical rope climbing/running). The patients had on an average of 4.68 (SD ± 3.1, range 2–15, median 3) episodes of dislocation at the time of presentation to our center. Right shoulder was involved in 28 and left shoulder was involved in 16 patients.
The CT scan of the shoulder joint was performed at a mean duration of 35.36 months (SD ± 29.6, range 1–150 months) from the date of the first episode to our center. Forty-one patients had glenoid bone loss while 40 had Hill-Sachs lesions.
Bone loss of glenoid width, Hill-Sachs defect and bone loss area of the glenoid
The mean glenoid width defect was 10.80% (range 0–27%). The glenoid width defect was <5% in 9, 5–10% in 13, >10%–20% in 18 and > 20% in 4 patients. The mean Hill-Sachs defect was 14.27 mm (range 0–26.6 mm). The Hill-Sachs defect was 0–10 mm in 10, 10–15 mm in 25 and > 15 mm in 9 patients. The mean area of bone loss of the glenoid surface was 10.81% (range 0–22.4%). The area of bone loss of the glenoid surface was 0–10% in 22, 10–15% in 11 and > 15% in 11 patients.
On-track vs off-track lesions
On the basis of glenoid and Hill-Sachs bone loss. The lesions were on-track in 34 patients and off-track in 10 patients.
Correlation of number of dislocations and bone loss
The bone loss on glenoid and humerus side was compared with the number of dislocations. There was a significant correlation between the number of dislocations and bone loss of glenoid width (in percentage) using Spearman's rho test (p = 0.017). Also, there was a significant correlation between the number of dislocations and bone loss of Hill-Sachs defect (in mm) using Spearman's rho test (p = 0.035). However, the correlation between bone loss areas of the glenoid (mm2) with the number of dislocations was found to be not significant (p = 0.789).
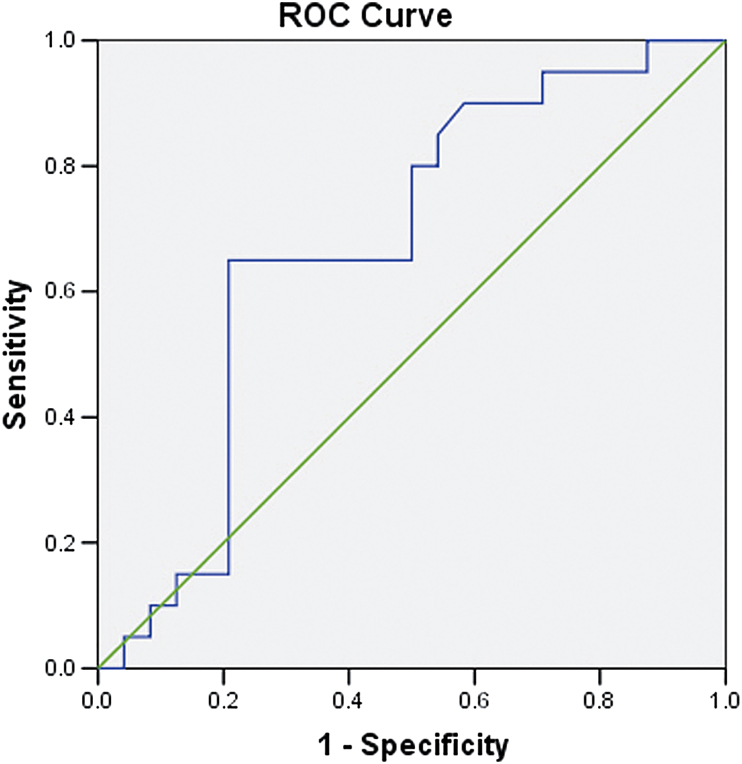
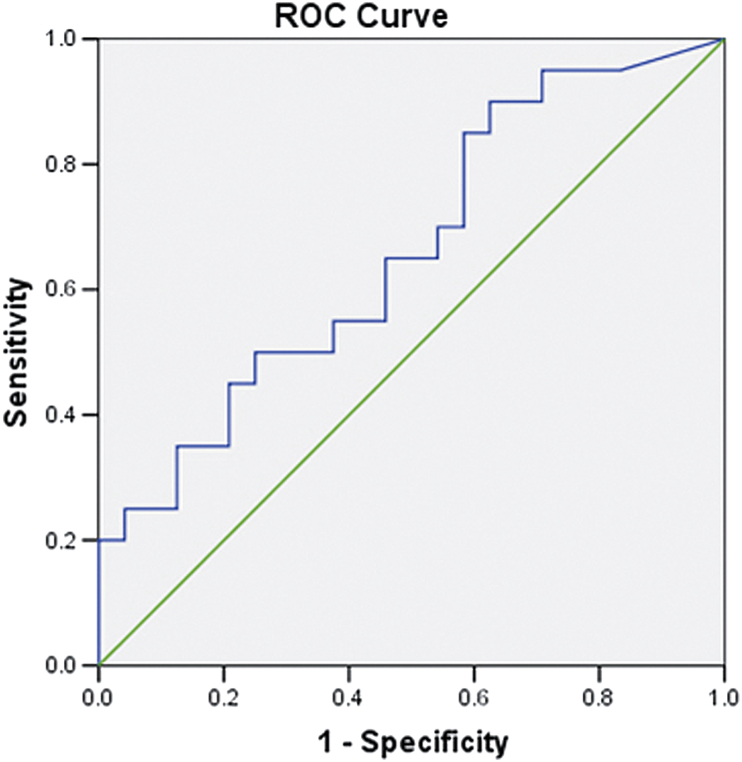
As the correlation between the number of dislocations and bone defect on the humeral and glenoid side was found to be significant. The number of dislocations [<3 and ≥ 3 (median dislocation were 3)] were compared with the bone loss of glenoid width and the Hill-Sachs defect using receiver operating characteristic (ROC) curve and T-test (Fig. 4, Fig. 5). It was found that when the percentage of bone loss was >9.60%, the higher number of dislocations were seen (p = 0.049, sensitivity 0.650 and specificity 0.417). Similarly, > 14.80 mm bone loss of Hill-Sachs defect is associated with higher number of dislocations (p = 0.043, sensitivity 0.650 and specificity 0.458).
Fig. 4.
ROC curve showing true positive and negative rate of dislocation when co-related with glenoid width defect.
Fig. 5.
ROC curve showing true positive and negative rate of dislocation when co-related with Hill- Sachs defect.
Correlation of number of dislocations and off/on-track lesion
The mean number of dislocations associated with off-track lesion were 6.60 while the mean number of dislocations associated with on-track lesion were 4.15. It was found that off-track lesions were associated with a significantly higher number of episodes of dislocations using Matt-Whitney test (p = 0.028).
Discussion
The amount of bone loss is considered as one of the key factors in predicting RDS.14 Also, various studies have reported higher reoccurrence rate associated with increased bone loss.1, 14, 15, 17 In the present study, the glenoid defect was present in 41 out of 44 patients (92.95%). While the Hill-Sachs defect was seen in 40 out of 44 patients (88.64%). Further, the defects on both sides were found to be more common than reported by various other studies.1, 17, 18, 19 One of the main reasons could be the inclusion of high demand professionals who are involved in various high velocity and rigorous activities.
We have studied the correlation between the number of dislocations and amount of bone loss using CT scan. Our group of patients was matched in terms of age, side involved, the height of the patients and mode of patients with the number of dislocations.
The correlation between the number of dislocation and the glenoid width defect was found to be significant (p = 0.017). This result of the present study is similar to various other studies.15, 18, 20 The correlation between the number of dislocation and Hill-Sachs defect was also found to be significant (p = 0.030). While the other study has found that Hill-Sachs defect has significant correlations with initial trauma and relocation.21 Furthermore, the correlation was found to be not significant when the number of dislocation were compared with the surface area loss of the glenoid. The surface area loss of glenoid is the total area of missing bone as compared to the normal side in patients with RDS. We believe that the maximum width defect which is generally anterior-inferior is significant risk factor as compared to the total surface area bone loss.
The height of the patient has been considered as one of the main variables to determine the size of glenoid and humerus which has been matched along with other variables in our study.21, 22 After equating the various variable it was found that higher number of dislocations (median > 3) were seen when percentage glenoid width bone loss is more than 9.80% or when the Hill-Sachs defect was more than 14.80 mm. These 2 parameters can also help us in deciding the management and type of surgery to be performed in case of RDS.
Yamamoto et al.4 gave the concept of the glenoid track which considered Hill-Sachs and glenoid defect in combination while evaluating patients with RDS. According to the glenoid track concept, the bone loss of the glenoid in RDS results in a smaller track of glenoid which is more likely to engage or dislocate in the presence of the humeral defect. The glenoid track concept also helps in determining the type of surgery required to tackle patient with RDS.19 Similar to this concept, the off-track lesions in our study were associated with more number of mean dislocations (6.600) as compared to the on-track lesions (4.150). (p = 0.028). These finding of our study are similar to the other studies.19
The present study has limitations, it is a retrospective study which subjects it to biases. Further, we have not studied the location of the glenoid bone loss and Hill-Sachs Lesions which can also be the factors for determining the reason for reoccurrence.4 Another drawback of the study is that we have not evaluated the correlation of various soft tissue injuries seen in the study with RDS. The effect of the various soft tissue injuries to the RDS cannot be ignored. However, the main aim of the study was to evaluate the various type of bone loss seen in RDS.
CT scan of the shoulder joint is an effective method for assessing the amount of bone loss on the glenoid side or the head of the humerus. The number of dislocations are correlated significantly with off track lesions, the amount of glenoid width bone loss and Hill-Sachs lesion. Furthermore, glenoid width bone loss of more than 9.80% or Hill-Sachs defect of more than 14.80 mm are the critical defects after which the frequency of dislocations increases.
Funding
Nil.
Acknowledgments
None at present.
Ethical statement
Ethical clearance was obtained from the institutional ethics committee of the hospital before the start of the study. Written informed consent was obtained from each patient before the conduct of the study.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Footnotes
Peer review under responsibility of Chinese Medical Association.
References
- 1.Nakagawa S., Ozaki R., Take Y. Relationship between glenoid defects and Hill-Sachs lesions in shoulders with traumatic anterior instability. Am J Sports Med. 2015;43:2763–2773. doi: 10.1177/0363546515597668. [DOI] [PubMed] [Google Scholar]
- 2.Sood M., Ghai A. Functional outcome after arthroscopic management of traumatic recurrent dislocation shoulder using Bankart repair and Remplissage techniques. Med J Armed Forces India. 2018;74:51–56. doi: 10.1016/j.mjafi.2017.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Burkhart S.S., De Beer J.F. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repair: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy. 2000;16:677–694. doi: 10.1053/jars.2000.17715. [DOI] [PubMed] [Google Scholar]
- 4.Yamamoto N., Itoi E., Abe H. Effect of an anterior glenoid defect on anterior shoulder stability: a cadaveric study. Am J Sports Med. 2009;37:949–954. doi: 10.1177/0363546508330139. [DOI] [PubMed] [Google Scholar]
- 5.Yamamoto N., Itoi E., Abe H. Contact between the glenoid and the humeral head in abduction, external rotation, and horizontal extension: a new concept of glenoid track. J Shoulder Elb Surg. 2007;16:649–656. doi: 10.1016/j.jse.2006.12.012. [DOI] [PubMed] [Google Scholar]
- 6.Rerko M.A., Pan X., Donaldson C. Comparison of various imaging techniques to quantify glenoid bone loss in shoulder instability. J Shoulder Elb Surg. 2013;22:528–534. doi: 10.1016/j.jse.2012.05.034. [DOI] [PubMed] [Google Scholar]
- 7.Itoi E., Lee S.B., Amrami K.K. Quantitative assessment of classic anteroinferior bony bankart lesions by radiography and computed tomography. Am J Sports Med. 2003;31:112–118. doi: 10.1177/03635465030310010301. [DOI] [PubMed] [Google Scholar]
- 8.Baudi P., Righi P., Bolognesi D. How to identify and calculate glenoid bone deficit. Chir Organi Mov. 2005;90:145–152. [PubMed] [Google Scholar]
- 9.Griffith J.F., Antonio G.E., Tong C.W. Anterior shoulder dislocation: quantification of glenoid bone loss with CT. AJR Am J Roentgenol. 2003;180:1423–1430. doi: 10.2214/ajr.180.5.1801423. [DOI] [PubMed] [Google Scholar]
- 10.Charousset C., Beauthier V., Bellaïche L. Can we improve radiological analysis of osseous lesions in chronic anterior shoulder instability? Orthop Traumatol Surg Res. 2010;96:S88–S93. doi: 10.1016/j.otsr.2010.09.006. [DOI] [PubMed] [Google Scholar]
- 11.Griffith J.F., Yung P.S., Antonio G.E. CT compared with arthroscopy in quantifying glenoid bone loss. AJR Am J Roentgenol. 2007;189:1490–1493. doi: 10.2214/AJR.07.2473. [DOI] [PubMed] [Google Scholar]
- 12.Trivedi S., Pomerantz M.L., Gross D. Shoulder instability in the setting of bipolar (glenoid and humeral head) bone loss: the glenoid track concept. Clin Orthop Relat Res. 2014;472:2352–2362. doi: 10.1007/s11999-014-3589-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Di Giacomo G., Itoi E., Burkhart S.S. Evolving concept of bipolar bone loss and the Hill-Sachs lesion: from “engaging/non-engaging” lesion to “on-track/off-track” lesion. Arthroscopy. 2014;30:90–98. doi: 10.1016/j.arthro.2013.10.004. [DOI] [PubMed] [Google Scholar]
- 14.Boileau P., Villalba M., Héry J.Y. Risk factors for recurrence of shoulder instability after arthroscopic Bankart repair. J Bone Joint Surg Am. 2006;88:1755–1763. doi: 10.2106/JBJS.E.00817. [DOI] [PubMed] [Google Scholar]
- 15.Milano G., Grasso A., Russo A. Analysis of risk factors for glenoid bone defect in anterior shoulder instability. Am J Sports Med. 2011;39:1870–1876. doi: 10.1177/0363546511411699. [DOI] [PubMed] [Google Scholar]
- 16.Dumont G.D., Russell R.D., Robertson W.J. Anterior shoulder instability: a review of pathoanatomy, diagnosis and treatment. Curr Rev Musculoskelet Med. 2011;4:200–207. doi: 10.1007/s12178-011-9092-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sugaya H., Moriishi J., Dohi M. Glenoid rim morphology in recurrent anterior glenohumeral instability. J Bone Joint Surg Am. 2003;85-A:878–884. doi: 10.2106/00004623-200305000-00016. [DOI] [PubMed] [Google Scholar]
- 18.Griffith J.F., Antonio G.E., Yung P.S. Prevalence, pattern, and spectrum of glenoid bone loss in anterior shoulder dislocation: CT analysis of 218 patients. AJR Am J Roentgenol. 2008;190:1247–1254. doi: 10.2214/AJR.07.3009. [DOI] [PubMed] [Google Scholar]
- 19.Ramhamadany E., Modi C.S. Current concepts in the management of recurrent anterior gleno-humeral joint instability with bone loss. World J Orthoped. 2016;7:343–354. doi: 10.5312/wjo.v7.i6.343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nakagawa S., Ozaki R., Take Y. Enlargement of glenoid defects in traumatic anterior shoulder instability: influence of the number of recurrences and type of sport. Orthop J Sports Med. 2014;2 doi: 10.1177/2325967114529920. 2325967114529920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Matsumura N., Oki S., Kitashiro M. Three-dimensional quantitative analysis of humeral head and glenoid bone defects with recurrent glenohumeral instability. J Shoulder Elb Surg. 2017;26:1662–1669. doi: 10.1016/j.jse.2017.03.009. [DOI] [PubMed] [Google Scholar]
- 22.Matsumura N., Oki S., Ogawa K. Three-dimensional anthropometric analysis of the glenohumeral joint in a normal Japanese population. J Shoulder Elb Surg. 2016;25:493–501. doi: 10.1016/j.jse.2015.08.003. [DOI] [PubMed] [Google Scholar]