To the Editor:
Chronic obstructive pulmonary disease (COPD) guidelines recommend escalation of inhaled therapy in a stepwise fashion for patients with respiratory symptoms, starting with short-acting bronchodilators and progressing to long-acting bronchodilators for those who do not have sufficient symptom control (1). Escalating therapy to an inhaled corticosteroid (ICS) is no longer recommended for patients without frequent or severe exacerbations, owing to risk of complications (e.g., pneumonia) exceeding potential benefit. Use of ICS among patients without these indications is common and represents potential overuse (2).
Prior studies have found that poor inhaler technique leads to reduced effectiveness, an unintentional form of nonadherence, and is associated with poor symptom control (3). Unintentional nonadherence to first-line rescue inhalers may therefore lead to escalation of long-acting inhaled medications that might not otherwise be needed. We hypothesized that unintentional nonadherence through poor albuterol metered-dose inhaler (MDI) technique would be associated with overuse of ICS among patients with mild to moderate COPD.
Methods
Design, setting, participants, and data source
We conducted a cross-sectional study using data collected through the COPD Outcomes-based Network for Clinical Effectiveness and Research Translation (CONCERT) (4). Potential participants were invited on the basis of electronic medical records indicating evidence for COPD. Participants completed in-person standardized questionnaires, spirometry, and medication review with a research assistant. We requested that participants bring all of their current medications to study visits. We provided a list of inhaled medications with accompanying pictures to those who did not.
Cohort selection
For these analyses, we included patients with airflow obstruction (post-bronchodilator forced expiratory volume in 1 s [FEV1]/forced vital capacity [FVC] ratio, <0.7). We excluded participants with an appropriate indication for ICS use, including 1) self-reported asthma, 2) self-reported COPD exacerbation in the prior 2 years, or 3) FEV1 less than 50% predicted, an appropriate indication at the time of study enrollment (5).
Primary exposure
A research assistant observed participants’ MDI use and recorded if each step was performed correctly, based on manufacturer’s directions. We defined “poor” MDI technique as completion of less than 75% of the steps correctly (6, 7).
Covariates
We evaluated potential confounders of the relationship between MDI technique and overuse of ICS, including causes of dyspnea unrelated to COPD (obesity, congestive heart failure, and coronary artery disease), severity of airflow obstruction (Global Initiative for Chronic Obstructive Lung Disease [GOLD] stage), dyspnea (modified Medical Research Council dyspnea scale score) (1), and spacer use.
Outcome
The outcome was presentation or self-reported use of an ICS inhaler during a study visit.
Statistical analysis
We created a mixed-effects Poisson model with robust standard error estimates adjusting for the covariates described above as fixed effects and recruitment site as a random effect (8). We estimated unadjusted and adjusted prevalence ratios (PR and APR, respectively) for ICS overuse associated with poor MDI technique (<75% of steps performed correctly) and with each individual error in correct MDI technique. We performed all analysis with Stata 15 software (StataCorp).
Results
Of the 1,206 patients recruited as part of CONCERT, we identified 95 with mild to moderate COPD using albuterol delivered through an MDI. Participants were predominantly white (85%) and male (61%), with a median age of 69 years (interquartile range, 62–77 yr). Thirty-one (33%) patients reported using ICS. ICS use was more common among patients with poor albuterol MDI technique (41%; n = 18 of 44) than among those with adequate technique (25%, n = 13 of 51) (Table 1).
Table 1.
Poor metered-dose inhaler technique is associated with increased likelihood of inhaled corticosteroid overuse among patients with chronic obstructive pulmonary disease
| Adequate MDI Technique | Poor MDI Technique | P Value | |
|---|---|---|---|
| No. of subjects | 51 | 44 | |
| ICS overuse, n (%) | 13 (25) | 18 (41) | |
| Crude prevalence ratio (95% CI) | 1 (Reference) | 1.6 (1.0–2.6) | 0.05 |
| Adjusted prevalence ratio* (95% CI) | 1 (Reference) | 2.4 (1.8–3.2) | <0.001 |
Definition of abbreviations: CI = confidence interval; ICS = inhaled corticosteroid; MDI = metered-dose inhaler.
Adjusted for age, sex, race, congestive heart failure, coronary artery disease, obesity, modified Medical Research Council dyspnea scale score, Global Initiative for Chronic Obstructive Lung Disease stage of airflow obstruction, and spacer use.
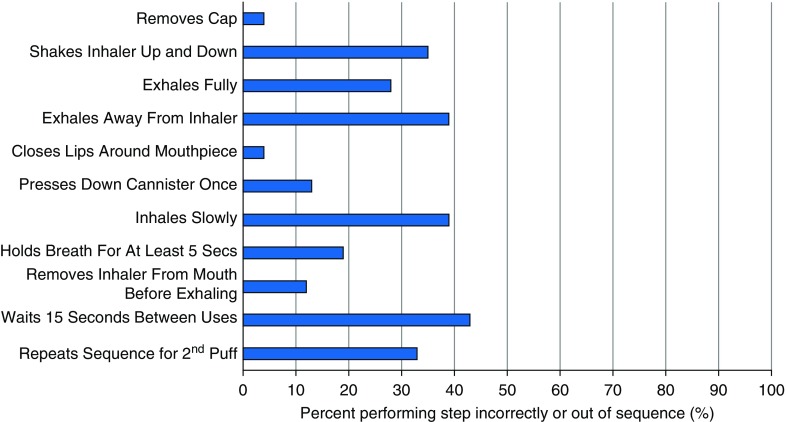
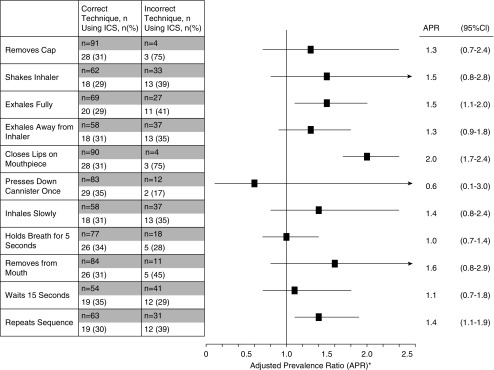
Unadjusted Poisson regression found a nonsignificant increased likelihood of ICS overuse associated with poor MDI technique (PR, 1.6; 95% confidence interval [CI], 1.0–2.6) (Table 1). After adjustment for confounding exposures, we found that poor MDI technique was associated with a significant increase in likelihood of ICS overuse (APR, 2.4; 95% CI, 1.8–3.2). Severity of airflow obstruction (APR, 3.0 for GOLD stage 2 vs. stage 1; 95% CI, 1.1–8.2) was associated with overuse; however, neither severity of patient-reported dyspnea nor comorbidities associated with dyspnea due to causes other than COPD (obesity, coronary artery disease, and congestive heart failure) were associated with overuse. Errors in correct MDI technique were common (Figure 1). Some individual errors were associated with ICS overuse (Figure 2).
Figure 1.
Patients with chronic obstructive pulmonary disease, without indication for an inhaled corticosteroid (e.g., severe airflow obstruction, asthma, or recent exacerbation), who reported using albuterol via metered-dose inhaler were observed using a metered-dose inhaler, and their technique was compared with manufacturer’s recommendation. Performing a step incorrectly or out of sequence was documented as an error.
Figure 2.
Participants with chronic obstructive pulmonary disease, without identifiable appropriate indication for inhaled corticosteroid (ICS), were observed by research staff using a metered-dose inhaler, and their technique was compared with manufacturer’s recommendation for correct sequence and procedure. For each individual step, we present adjusted prevalence ratios (APRs) measuring the association between failure to perform that step correctly and ICS overuse. Prevalence ratios were adjusted for potential confounders, including patient demographics (age, race, and sex), specific comorbidities associated with dyspnea (coronary artery disease, congestive heart failure, and obesity), disease severity (forced expiratory volume in 1 second), symptom severity (modified Medical Research Council dyspnea scale), and spacer use. Failure to exhale before activation, to close lips around mouthpiece, and to repeat sequence for a second inhalation were individually associated with increased likelihood of ICS overuse. Percentages reported in the table reflect the proportion of patients with ICS overuse among those who performed the step correctly or incorrectly. *Adjusted for age, gender, race, congestive heart failure, coronary artery disease, obesity, mMRC score, GOLD Stage of airflow obstruction, and spacer use. CI = confidence interval; GOLD = Global Initiative for Chronic Obstructive Lung Disease; mMRC = modified Medical Research Council.
Discussion
We found that poor MDI technique was associated with a twofold higher likelihood of ICS overuse among patients with mild to moderate COPD, raising the concern that clinicians are providing ICS to patients who may not require such escalation. Given the potential direct harms associated with ICS use and the indirect harms financially to patients and health systems, our results highlight the need for inhaler technique training.
Our results suggest significant room for improvement in reducing unintentional nonadherence to MDIs. For healthcare systems seeking to improve quality, interventions focused on initial inhaler training and maintenance may offer an opportunity to decrease respiratory symptoms, reduce unnecessary expenditures, and mitigate harms (e.g., pneumonia) resulting from ICS overuse (7). For those patients receiving potentially inappropriate ICS, these training sessions could mitigate the sense of loss when the therapy is withdrawn (9).
Our study has several potential limitations and strengths. We did not assess prior training in MDI use, although data suggest that the effects of training wane over time (7). We defined poor technique as less than 75% of steps performed correctly under direct observation, because this threshold has been associated with increased healthcare use (7). However, our finding that there are individual errors in MDI technique associated with ICS overuse could indicate that some errors are more critical than others. We used restriction to minimize confounding by unmeasured factors, including prescriber knowledge, prior inhaler training, and medication adherence, which resulted in a reduced sample size. Additional research would be necessary to confirm our findings. Although CONCERT recruited patients from diverse clinical settings, such as other large COPD trials, patients were predominantly white and male. Greater emphasis on recruiting patients reflecting the sex and racial and ethnic diversity of patients with COPD should remain a focus of future clinical studies.
Despite decades of experience with MDIs, our results suggest that there is ample room to improve inhaler technique. Moreover, we found that poor MDI technique increased risk of ICS overuse. These findings raise concerns that lack of emphasis on adequate initial training and appropriate monitoring may be leading to harms to patients and health systems. Our results provide an additional rationale for health systems to develop processes that improve inhaled medication technique and delivery.
Supplementary Material
Footnotes
Author disclosures are available with the text of this letter at www.atsjournals.org.
Contributor Information
Collaborators: for the CONCERT Investigators
References
- 1.Global Initiative for Chronic Lung Disease (GOLD) From the Global Strategy for the Diagnosis, Management and Prevention of COPD, Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2017. 2017 [accessed 2018 Dec 26]. Available from: http://goldcopd.org.
- 2.Yawn BP, Suissa S, Rossi A. Appropriate use of inhaled corticosteroids in COPD: the candidates for safe withdrawal. NPJ Prim Care Respir Med. 2016;26:16068. doi: 10.1038/npjpcrm.2016.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sulaiman I, Cushen B, Greene G, Seheult J, Seow D, Rawat F, et al. Objective assessment of adherence to inhalers by patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2017;195:1333–1343. doi: 10.1164/rccm.201604-0733OC. [DOI] [PubMed] [Google Scholar]
- 4.Prieto-Centurion V, Rolle AJ, Au DH, Carson SS, Henderson AG, Lee TA, et al. CONCERT Consortium. Multicenter study comparing case definitions used to identify patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2014;190:989–995. doi: 10.1164/rccm.201406-1166OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vestbo J, Hurd SS, Rodriguez-Roisin R. The 2011 revision of the global strategy for the diagnosis, management and prevention of COPD (GOLD)–why and what? Clin Respir J. 2012;6:208–214. doi: 10.1111/crj.12002. [DOI] [PubMed] [Google Scholar]
- 6.Melzer AC, Ghassemieh BJ, Gillespie SE, Lindenauer PK, McBurnie MA, Mularski RA, et al. Patient characteristics associated with poor inhaler technique among a cohort of patients with COPD. Respir Med. 2017;123:124–130. doi: 10.1016/j.rmed.2016.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Press VG, Arora VM, Trela KC, Adhikari R, Zadravecz FJ, Liao C, et al. Effectiveness of interventions to teach metered-dose and Diskus inhaler techniques: a randomized trial. Ann Am Thorac Soc. 2016;13:816–824. doi: 10.1513/AnnalsATS.201509-603OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barros AJ, Hirakata VN. Alternatives for logistic regression in cross-sectional studies: an empirical comparison of models that directly estimate the prevalence ratio. BMC Med Res Methodol. 2003;3:21. doi: 10.1186/1471-2288-3-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Helfrich CD, Rose AJ, Hartmann CW, van Bodegom-Vos L, Graham ID, Wood SJ, et al. How the dual process model of human cognition can inform efforts to de-implement ineffective and harmful clinical practices: a preliminary model of unlearning and substitution. J Eval Clin Pract. 2018;24:198–205. doi: 10.1111/jep.12855. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.