Abstract
Purpose
To demonstrate survival and integration of mature photoreceptors transplanted with the retinal pigment epithelium (RPE).
Methods
Full-thickness retina with attached RPE was harvested from healthy adult rats. Grafts were implanted into two rat models of retinal degeneration, Royal College of Surgeons (RCS) and S334ter-3. Survival of the host and transplanted retina was monitored using optical coherence tomography (OCT) for up to 6 months. The retinal structure and synaptogenesis between the host and transplant was assessed by histology and immunohistochemistry.
Results
OCT and histology demonstrated a well-preserved photoreceptor layer with inner and outer segments, while the inner retinal layers of the transplant largely disappeared. Grafts, including RPE, survived better than without and the transplanted RPE appeared as a monolayer integrated with the native one. Synaptogenesis was observed through sprouting of new dendrites from the host bipolar cells and synaptic connections forming with cells of the transplant. However, in many samples, a glial fibrillary acidic protein–positive membrane separated the host retina and the graft.
Conclusions
Presence of RPE in the graft improved the survival of transplanted photoreceptors. Functional integration between the transplant and the host retina is likely to be further enhanced if formation of a glial seal could be prevented. Transplantation of the mature photoreceptors with RPE may be a practical approach to restoration of sight in retinal degeneration.
Translational Relevance
This approach to restoration of sight in patients with photoreceptor degeneration can be rapidly advanced to clinical testing. In patients with central scotoma, autologous transplantation of the peripheral retina can be an option.
Keywords: retinal degeneration, photoreceptor transplantation, RPE transplantation
Introduction
Loss of photoreceptors in inherited retinal diseases or age-related macular degeneration (AMD) can lead to blindness. Transplantation of photoreceptors is one of the most natural ideas when thinking about restoration of sight in such conditions. First, human retinas can be harvested several hours postmortem and kept healthy in culture for days.1 Second, the laminar organization of the retina allows relatively simple implantation of the sheet graft in the subretinal space. Third, the immune privilege of the subretinal space2–4 helps reduce the chance of rejection.
Efforts toward retinal transplantation started with the assumption that only fetal retinas can survive and be plastic enough to reconnect to the host retina. Survival of the fetal rat retina in the anterior chamber of the maternal eye was demonstrated as early as 1959.5 More recent experiments demonstrated survival of the fetal retinal grafts in the subretinal space and some evidence of reconnection between the host and the transplant.6–9
Based on those encouraging results, retinal sheets from unborn fetuses were transplanted into several patients with retinitis pigmentosa (RP) and AMD.10–14 Majority of Radtke's patients showed an improvement of visual acuity in the transplanted eye, with the best improvement from 20/800 to 20/200 over 5 years.14 Despite this proof of concept, ethical concerns with the use of unborn fetuses15 and limited availability of the fetal tissue precluded adaptation of this approach. Another limitation of the fetal graft is that the ganglion cell layer (GCL) does not disappear after transplantation and prevents effective connectivity between the donor and the host retinas.7
Since the earliest description of fetal retinal plasticity in transplantation,16 several approaches involving photoreceptor precursors from stem cells were developed. Some signs of survival and integration17 were initially demonstrated, but in a limited number of cells.18,19 However, integration and formation of outer segments (OS) was observed only when at least a fraction of the host outer nuclear layer (ONL) was still present, but did not exhibit normal and uniform polarization when injected in dystrophic retinas.20 Results from that study were later attributed to host photoreceptor cells contaminated by intercellular transfer of cytoplasmic content from the fluorescently labeled cells, rather than integration.21
While the synaptic plasticity in the donor photoreceptors is essential for the success of the graft, the host bipolar cells must also be able to form new synaptic contacts. Interestingly, following local photoreceptor coagulation by laser, adult bipolar cells that have been deprived from presynaptic inputs have been shown to reach out tens of microns away from the lesion to establish new functional connections with photoreceptors.22,23
Full-thickness retinal transplantation has been also performed using neonatal donor retina and stem cell–derived three-dimensional retinal organoid grafts.24,25 These grafts are not fully differentiated at the time implantation. Three-dimensional retinal organoids exhibited signs of dysfunctional and nondirectional photoreceptors, with the formation of rosettes.25 Transplantation of fetal photoreceptors coupled with retinal pigment epithelium (RPE) has provided encouraging results in animals26 and humans13 with degenerate retina. While the presence of RPE on those transplants was beneficial, ethical concerns and limited availability of the fetal tissue still precluded adaptation of this approach.
Transplantation of mature retinal sheets without RPE in a light-induced degeneration model demonstrated better structural integrity of the outer retina when transplanted with the inner retina, compared with transplantation of the photoreceptors alone.27 However, the absence of RPE in these grafts reduces the translational applicability of the technique, as it would not be suitable for patients having dysfunctional RPE in diseases, such as AMD.
We investigated here the feasibility of mature retinal allografts transplanted together with RPE in two different models of retinal degeneration. In the first model, the Royal College of Surgeon (RCS) rat, a mutation in the MERTK gene reduces the phagocytic capability of the RPE, leading to degeneration of photoreceptors by 4 months.28 While it's one of the forms of RP, this condition would require transplantation of not only photoreceptors but also functional RPE, thereby mimicking requirements for treatment of geographic atrophy. The S334ter-3 rats were used as an alternative model, where photoreceptors degenerate by 2 months due to a mutation in the rhodopsin, while the RPE remains fully functional.29
Materials and Methods
Experimental Design
This study was designed to evaluate the outcomes of mature photoreceptors transplantation from healthy rats into two different rat models of retinal degeneration. Following the development of a surgical technique, we included in this analysis all the transplants, which displayed a discernable layering on optical coherence tomography (OCT), 1 week after transplantation. Therefore, this study does not describe the success rate of the transplantation procedure itself, but rather the extent of tissue integration, when the graft is not rejected.
Animals
Rats with retinal degeneration were obtained from the colonies of RCS (P139–P257, n = 6) or S334ter-3 (source RRRC, strain SD-Tg(S334ter)3Lav, P72–P90, n = 7) maintained at the Stanford Animal Facility. Long-Evans (LE, P18–P50, n = 8) rats were purchased from Charles River (Wilmington, MA). All animals were housed in a 12-hour light/12-hour dark cycle, with food and water ad libitum. All experimental procedures were conducted in accordance with the institutional guidelines and conformed to the ARVO Statement for the Use of Animals in Ophthalmic and Vision Research.
Graft Preparation
Properly designed and performed transplantation procedure is one of the key factors in success of the graft (Fig. 1 and Supplementary Video S1). Donor rats (LE, n = 8) were deeply anesthetized with a mixture of ketamine (75 mg/kg) and xylazine (5 mg/kg) and euthanized with an intracardiac injection of Beutanesia (0.5 mL). Eyes were enucleated and placed in oxygenated Ames's solution (SIGMA, St. Louis, MO) at room temperature for further dissection. The anterior segment was removed and the lens was slowly pulled away, along with the vitreous. If some vitreous was still present on the retinal side, it was removed using forceps. One-millimeter diameter biopsy punch was used to isolate the transplant. At that time, most RPE cells stayed attached to the retina (Supplementary Fig. S1B). The transplant was kept in oxygenated Ames solution until the donor was ready—typically 10 to 15 minutes. It was then loaded into a custom-made hydraulic tool (Supplementary Fig. S1C), having a 200-μm high, 1-mm wide microchannel connected to a syringe with viscoelastic gel (Viscoat; Alcon, Puurs, Belgium).
Figure 1.
In vivo evaluation of the transplant's structural preservation. (A) OCT of the transplanted retina over time. One week (1W) after transplantation (D0), the host retina has reattached and maintains its laminar structure. After 1 month (1M), the OS of the transplant have grown back (yellow arrows) while its inner retina has thinned and this structure is still maintained at 3 months. (B) Time course of the transplant thickness, up to 4 months, averaged over eight animals (dots colored per animal). The data were fitted with an exponential function (red line), y = y∞ + (y0 − y∞) · e−t/τ with y∞ = 88 ± 8 μm, y0 = 217 ± 18 μm and τ = 3 ± 1 days (± indicate the 95% confidence interval). Note that animals were terminated at different time points, but all of them reached the steady state (t > 4τ). (C) Initial and steady-state thickness of the inner and outer layers of the transplant. The inner layers (GCL, IPL, INL) of the transplant decreased from 107 to 32 μm, while the outer layers (OPL, ONL, OS) decreased less, from 110 to 56 μm.
Transplantation
As a recipient, we used two animal models of retinal degeneration, the RCS rat and the S334ter-3 rat. Both models exhibit complete photoreceptor degeneration with the difference of dysfunctional RPE in RCS rats and fully functional RPE in S334ter-3 rats.
Recipient rats were anesthetized with a mixture of ketamine (75 mg/kg) and xylazine (5 mg/kg), topical anesthetics (tetracaine, 0.5%). Dilation drops (phenylephrine 2.5%, tropicamide 1%) were applied to the operated eye. The recipient eye was prepared with a transscleral incision followed by retinal detachment with balanced salt solution (BSS) and viscoelastic injection in the subretinal space (Supplementary Fig. S1D), followed by insertion of the transplant into the subretinal space under visual control (Supplementary Fig. S1E). BSS was then injected into the vitreous cavity to reattach the host retina over the transplant. Placement of the graft and reattachment of the host retina was verified with OCT (Supplementary Figs. S1F, S1G).
OCT Imaging
Spectral-domain OCT images were obtained by using HRA2-Spectralis (Heidelberg Engineering, Heidelberg, Germany), with the cornea covered with viscoelastic and a coverslip to cancel its optical power (Supplementary Figs. S1F, S1G). Pupils were fully dilated and throughout the procedure, 1% methylcellulose was used to maintain corneal clarity. Transplanted rats were followed from day 0 (D0) until sacrifice. ONL layer thickness was measured at the center of the transplant.
Histology
For histology, animals were sacrificed at D1, D13, and D42. Prior to enucleation, the superior edge of the eye was marked under deep anesthesia. Both eyes of each animal were enucleated and fixed in 1% paraformaldehyde and 1.25% glutaraldehyde fixative prepared with 5 mM calcium chloride and 5% sucrose for 24 hours at room temperature. The cornea and lens were removed, leaving a posterior eye cup, which was dehydrated through a graded series of alcohols, infiltrated in propylene oxide, and embedded in epoxy. The 0.5-μm thick sections were taken using Reichert Ultracut E (Reichert-Jung, Vienna, Austria), stained with 0.5% toluidine blue, and serial sections of the slides were examined by light microscopy.
Immunohistochemistry
For immunohistochemistry, animals were sacrificed at 1, 2, 4, and 6 months. Before enucleation, the superior edge of the eye was marked under deep anesthesia. Both eyes of each animal were enucleated and fixed in 4% paraformaldehyde overnight. The cornea and lens were removed, and the eyecup was embedded in the optimal cutting compound, frozen, and sectioned with 12-μm thickness. The sections were permeabilized with triton incubated overnight with the following antibodies: protein kinase C-α (PKCα), SC-8393, 1:100; Santa Cruz Biotechnologies, Santa Cruz, CA; Bassoon, VAM-PS003, 1:1000; Stressgen, San Diego, CA; and Cone Arrestin, AB15282, 1:1000; Millipore, Billerica, MA, and 2 hours in secondary antibodies, Alexa Fluor 488 and Alexa Fluor 594, R37114, A11058, A21206, 1:100; Thermo Fisher Scientific, Rockford, IL, with 4′,6-diamidino-2-phenylindole (DAPI). Sections were imaged using confocal microscope (LSM780; Zeiss, Jena, Germany) and Airyscan (LSM880; Zeiss).
Statistical Analysis
The layers thickness in the transplants was measured in vivo using OCT at various time points in eight animals, and then histologically at the end of the follow-up period. The exponential fit was obtained on all the data points, and the 95% confidence interval was calculated using the Matlab fitting toolbox (The MathWorks, Natick, MA). Length of the glial seal (the hyperreflective layer between the host and transplant) was measured on the central OCT section at the last time point of the follow-up for each animal.
Results
Because retinal ischemia and severing the ganglion cell axons cause the loss of the inner retinal neurons,30–32 while photoreceptors in these conditions survive due to choroidal circulation, we decided to transplant mature, full-thickness retinas, with the hypothesis that only the outer retina would survive after the transplantation. We developed and implemented a surgical procedure that minimizes damage to both host and donor tissue (Supplementary Fig. S1 and Video S1). Survival of the transplant over time was assessed with OCT (Figs. 1A, 1B), by monitoring the thickness of the retinal layers. Transplants without RPE, as well the ones that underwent very traumatic surgery, showed a rapid (<1 week) loss of photoreceptors. However, when RPE cells stayed attached to the retinal transplant, we observed long-term survival of the photoreceptors in both models of retinal degeneration (Supplementary Fig. S2). Thickness of the transplant rapidly (τ = 3 ± 1 days) decreased from 217 ± 18 to 88 ± 8 μm (± values indicate 95% confidence interval, n = 8), and remained stable after that (Fig. 1C). As expected, most of the thinning was in the inner layers (GCL; inner plexiform layer, IPL; and inner nuclear layer, INL) of the transplant, from 109 ± 6 to 31 ± 4 μm (−70%, Fig. 1D), while the outer layers (outer plexiform layer, OPL; ONL; and inner/outer segments, IS/OS) thinned by approximately 50%.
Histology confirmed the atrophy of the inner retinal layers of the transplant as early as 2 weeks after transplantation (Fig. 2). At the same time, photoreceptors remained well preserved, with six to seven layers of the nuclei in the ONL, and well-defined IS/OS. Disappearance of the RGC layer of the transplant, likely due to severance of the axons, brought the IPL of the transplant in direct contact with the INL of the host.
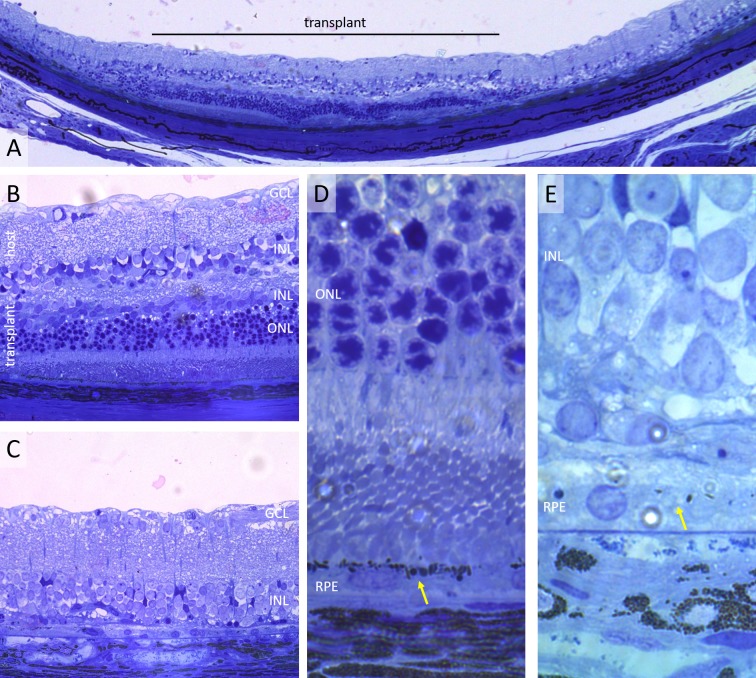
Figure 2.
Histology of transplanted retina 2 weeks postsurgery. (A) Wide view of the transplanted retina (LE transplanted into RCS rat) showing the 1-mm transplant (black line) and the control area outside it. (B, C) Higher magnification of the same sample showing excellent preservation of the transplanted photoreceptors (B), compared with the area outside the transplant (C). The inner retina of the transplant is significantly thinned, with no distinct GCL. (D, E) The close up illustrates pigmented RPE monolayer under the transplant (yellow arrow [D]), as opposed to nonpigmented RPE in a control area (E).
In RCS rats, RPE cells cannot properly recycle the photoreceptor OS, leading to accumulation of subretinal debris and the subsequent loss of photoreceptors.28 Following co-transplantation of RPE along with the retina, we observed the presence of pigmented endosomes in the RPE layer (Fig. 2D), indicating some phagocytic function,33 as opposed to lack of pigment in the nontransplanted area. The transplanted RPE appeared as a monolayer rather than an additional layer on top of native RPE, either due to fusion of the two layers or disruption of the initial RPE during subretinal surgery. This second hypothesis would explain why even in S334ter rats, where RPE is functional, we found that retinal transplants without RPE did not survive.
In the majority of samples, the periphery of the transplant displayed a high degree of integration, with 53.7 ± 10% (standard error of the mean) of its length having no visible boundary between the host and transplant (Fig. 3A), and excellent preservation of the photoreceptor IS/OS. Immunohistochemistry demonstrated layered structure in both the transplant and the host retina (PKCα in rod bipolar cells, Figs. 3C, 3D), as well as preservation of the cone OS (cone Arrestin, Fig. 3B).
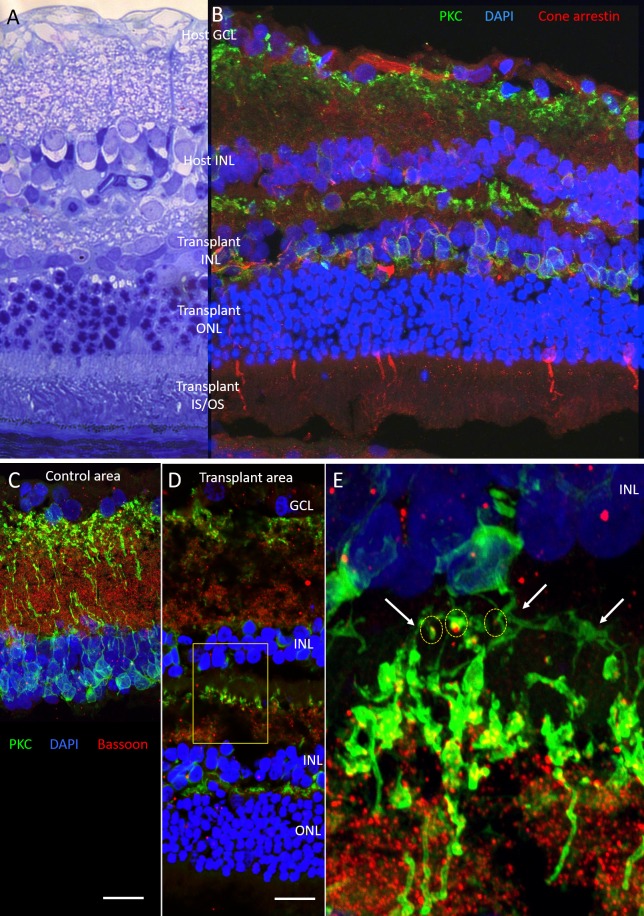
Figure 3.
Photoreceptors preservation and synaptic connections between the host and transplanted bipolar cells. (A) Histology shows excellent preservation of the photoreceptors, including their IS/OS 13 days after surgery (RCS rat transplanted from a LE donor). In this example, there is no insulating layer between the transplant and the host, and tissues seem to have fused. (B) Confocal image of another sample (S334ter-3 transplanted from a LE) 61 days after surgery. Cone arrestin (red) shows cone photoreceptors with their OS. PKCα (green) and DAPI (blue) show the plexiform and nuclear layers in the transplant and the host retina. (C) Nontransplanted and (D) transplanted areas stained with PKC (rod bipolar cells), Bassoon (presynaptic ribbon synapses), and 4′,6-diamidino-2-phenylindole. (E) Close-up of the area between the host and the transplant, where bipolar cells from the host (top INL) send dendrites into the IPL of the transplant (white arrows), which co-localize with presynaptic bassoon staining (red), as outlined with the yellow circles.
Confocal microscopy showed that, unlike the control area, where no vertical extension of the bipolar cell dendrites could be observed (Fig. 3C), in the transplanted areas, dendrites were extending from the host bipolar cells into the IPL of the transplant (Supplementary Video S2). Co-localization of the dendritic tips of the host rod bipolar cells with bassoon presynaptic marker (Figs. 3D, 3E) indicated the synaptogenesis between the bipolar cells of the host and the transplant. Such connection occurred predominantly near the edges of the transplant. To eliminate the possibility of the co-localization being ectopic contacts, future work will be centered on electron microscopy, electrophysiologic, and behavioral studies after transplantation.
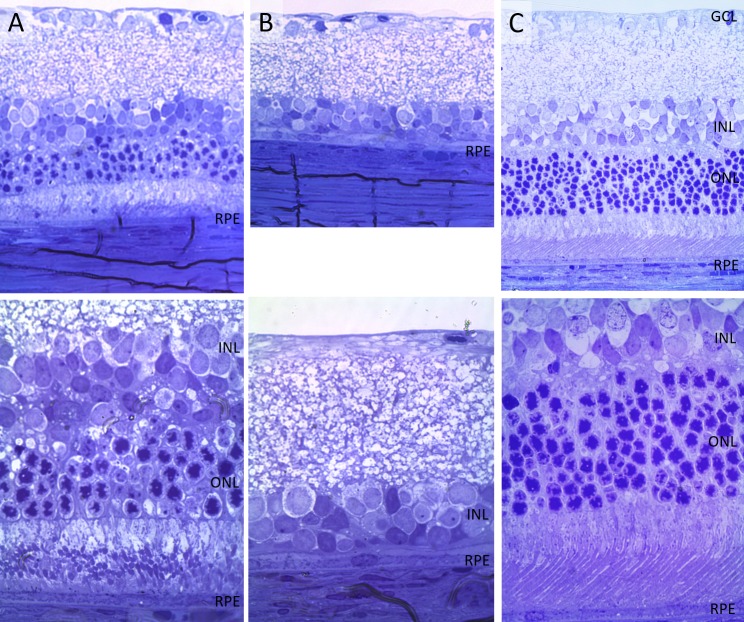
Some samples displayed even higher degree of integration, with a complete fusion between the inner retina of the host and the transplant (Fig. 4). Such integration demonstrates that in ideal conditions, the ischemia produced by the transplant harvesting can indeed result in a loss of its inner retina, bringing the grafted photoreceptors into direct contact with the host bipolar cells.
Figure 4.
Histology of a transplanted retina at 6 months postoperative, compared with control and with wild-type retina. (A) The transplanted area has nearly normal anatomy, with a single INL and transplanted photoreceptors merging with the host retina (from a LE into S334ter rat). (B) The nontransplanted area completely lacking photoreceptors. (C) A healthy LE rat retina is shown here for comparison. Top row is imaged via ×40 objective and bottom row via ×100.
In other samples, a glial fibrillary acidic protein–positive layer was observed in the center of the transplant, which prevented cell processes from reaching the other side (Supplementary Fig. S3). This layer appeared in OCT as a hyperreflective membrane developing over time, and could be due to the initial presence of the inner limiting membrane (ILM). Indeed, this membrane has been shown to serve as a scaffold for cellular proliferation in retinal pathologies.34 This issue could be overcome by ILM peeling from the donor tissue prior to transplantation. It is also possible that direct connection between the host bipolar cells and transplanted photoreceptors could be facilitated by prior removal of the inner retina using retinal artery occlusion a few weeks before harvesting.
Discussion
Transplantation of mature RPE/photoreceptors holds a high potential for rapid clinical implementation. First, human retinas can be harvested up to several hours postmortem and kept alive in culture for days1 or even translocated within the same eye.35 Second, the laminar organization of the retina allows relatively simple implantation of the sheet graft into subretinal space. Third, the immune privilege of the subretinal space2–4 decreases the chance of rejection.
Several reasons could be behind the lack of reproducibility in previous clinical attempts of retinal transplantation. Some of them did not co-transplant RPE cells along with photoreceptors,36,37 some only used retinal microaggregates with no preserved structure or orientation.12 In the most convincing study, retinal/RPE sheets from unborn fetuses were transplanted into the central retina of several patients with RP and AMD.14,38 Some of the patients showed an improvement of visual acuity in the transplanted eye, with the best increase from 20/800 to 20/200 over 5 years.14
The extension of dendrites by the host bipolar cells in search of the new connections we showed here is in agreement with our previous observations that bipolar cells deafferented by photocoagulation extend dendrites toward the edges of the lesion and establish new functional connections with photoreceptors outside of the damage zone.22,23 This suggests that reconnection is driven by bipolar cells rather than photoreceptors, and it likely involves secretion of proper cytokines by the mature photoreceptors, which is less likely to occur with underdeveloped stem cells.
Prior to our findings of better survival of the transplanted photoreceptors coupled to RPE, we tried a range of controls and other transplantation techniques, which did not work (Supplementary Fig. S2). In particular, we observed no survival of the donor grafts having no RPE attached. We also tried retinal transplantation under the healthy retinas. However, the chronic retinal detachment created by the graft triggers degeneration of the host photoreceptors, accompanied by an inflammatory reaction, leading to elimination of the transplant as well.
While fetal retina has been documented to have higher stability to immune degradation in the subconjunctival space than adult full-thickness neuroretinal grafts,39 the use of mature donor tissue may offer multiple advantages. First, fetal retinas seem to develop into a three-layered structure with a thick IPL and RGC layer that could limit the establishment of synaptic connections to the host.9 Second, availability of the mature donor tissue eliminates an ethical and legal impasse. Finally, it opens the door to autologous transplantation in patients with central scotoma, such as geographic atrophy in AMD, with a technique similar to closure of macular hole.35 Autologous transplantation in human patients would allow addressing some of the basic questions about photoreceptors survival and rewiring, without the confounding factors of histocompatibility. In addition, if removal of the inner retinal cells prior to transplantation would facilitate integration, that could be induced regionally by branch arterial occlusion with laser.40
Supplementary Material
Acknowledgments
The authors thank Mehmet Solyali and the Stanford Physics Machine Shop for their help in design and fabrication the implantation device.
Supported by grants from the Air Force Office of Scientific Research (FA9550-17-1-0237), by Research to Prevent Blindness Inc., and by the National Eye Institute (P30-EY026877).
Disclosure: H. Lorach, None; S. Kang, None; M.B. Bhuckory, None; A. Trouillet, None; R. Dalal, None; M. Marmor, None; D. Palanker, None
References
- 1.Busskamp V, Duebel J, Balya D, et al. Genetic reactivation of cone photoreceptors restores visual responses in retinitis pigmentosa. Science. 2010;329:413–417. doi: 10.1126/science.1190897. [DOI] [PubMed] [Google Scholar]
- 2.Jiang LQ, Jorquera M, Streilein JW. Subretinal space and vitreous cavity as immunologically privileged sites for retinal allografts. Invest Ophthalmol Vis Sci. 1993;34:3347–3354. [PubMed] [Google Scholar]
- 3.Larsson J, Juliusson B, Holmdahl B, Ehinger B. MHC expression in syngeneic and allogeneic retinal cell transplants in the rat. Graefes Arch Clin Exp Ophthalmol. 1999;237:82–85. doi: 10.1007/s004170050199. [DOI] [PubMed] [Google Scholar]
- 4.Streilein JW, Ma N, Wenkel H, Ng TF, Zamiri P. Immunobiology and privilege of neuronal retina and pigment epithelium transplants. Vision Res. 2002;42:487–495. doi: 10.1016/s0042-6989(01)00185-7. [DOI] [PubMed] [Google Scholar]
- 5.Royo PE, Quay WB. Retinal transplantation from fetal to maternal mammalian eye. Growth. 1959;23:313–336. [PubMed] [Google Scholar]
- 6.Aramant RB, Seiler MJ. Progress in retinal sheet transplantation. Prog Retin Eye Res. 2004;23:475–494. doi: 10.1016/j.preteyeres.2004.05.003. [DOI] [PubMed] [Google Scholar]
- 7.Aramant RB, Seiler MJ. Retinal transplantation–advantages of intact fetal sheets. Prog Retin Eye Res. 2002;21:57–73. doi: 10.1016/s1350-9462(01)00020-9. [DOI] [PubMed] [Google Scholar]
- 8.Thomas BB, Aramant RB, Sadda SR, Seiler MJ. Retinal transplantation. A treatment strategy for retinal degenerative diseases. Adv Exp Med Biol. 2006;572:367–376. [PubMed] [Google Scholar]
- 9.Seiler MJ, Lin RE, McLelland BT, et al. Vision recovery and connectivity by fetal retinal sheet transplantation in an immunodeficient retinal degenerate rat model. Invest Ophthalmol Vis Sci. 2017;58:614–630. doi: 10.1167/iovs.15-19028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Radtke ND, Aramant RB, Seiler M, Petry HM. Preliminary report: indications of improved visual function after retinal sheet transplantation in retinitis pigmentosa patients. Am J Ophthalmol. 1999;128:384–387. doi: 10.1016/s0002-9394(99)00250-0. [DOI] [PubMed] [Google Scholar]
- 11.del Cerro M, Humayun MS, Sadda SR, et al. Histologic correlation of human neural retinal transplantation. Invest Ophthalmol Vis Sci. 2000;41:3142–3148. [PubMed] [Google Scholar]
- 12.Humayun MS, de Juan E, Jr, del Cerro M, et al. Human neural retinal transplantation. Invest Ophthalmol Vis Sci. 2000;41:3100–3106. [PubMed] [Google Scholar]
- 13.Radtke ND, Seiler MJ, Aramant RB, Petry HM, Pidwell DJ. Transplantation of intact sheets of fetal neural retina with its retinal pigment epithelium in retinitis pigmentosa patients. Am J Ophthalmol. 2002;133:544–550. doi: 10.1016/s0002-9394(02)01322-3. [DOI] [PubMed] [Google Scholar]
- 14.Radtke ND, Aramant RB, Petry HM, Green PT, Pidwell DJ, Seiler MJ. Vision improvement in retinal degeneration patients by implantation of retina together with retinal pigment epithelium. Am J Ophthalmol. 2008;146:172–182. doi: 10.1016/j.ajo.2008.04.009. [DOI] [PubMed] [Google Scholar]
- 15.Hurd RE. Ethical issues surrounding the transplantation of human fetal tissues. Clin Res. 1992;40:661–666. [PubMed] [Google Scholar]
- 16.Aramant R, Seiler M, Turner JE. Donor age influences on the success of retinal grafts to adult rat retina. Invest Ophthalmol Vis Sci. 1988;29:498–503. [PubMed] [Google Scholar]
- 17.Seiler MJ, Aramant RB, Thomas BB, Peng Q, Sadda SR, Keirstead HS. Visual restoration and transplant connectivity in degenerate rats implanted with retinal progenitor sheets. Eur J Neurosci. 2010;31:508–520. doi: 10.1111/j.1460-9568.2010.07085.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.MacLaren RE, Pearson RA, MacNeil A, et al. Retinal repair by transplantation of photoreceptor precursors. Nature. 2006;444:203–207. doi: 10.1038/nature05161. [DOI] [PubMed] [Google Scholar]
- 19.Pearson RA, Barber AC, Rizzi M, et al. Restoration of vision after transplantation of photoreceptors. Nature. 2012;485:99–103. doi: 10.1038/nature10997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Barber AC, Hippert C, Duran Y, et al. Repair of the degenerate retina by photoreceptor transplantation. Proc Natl Acad Sci U S A. 2013;110:354–359. doi: 10.1073/pnas.1212677110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Singh MS, Balmer J, Barnard AR, et al. Transplanted photoreceptor precursors transfer proteins to host photoreceptors by a mechanism of cytoplasmic fusion. Nat Commun. 2016;7:13537. doi: 10.1038/ncomms13537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Beier C, Hovhannisyan A, Weiser S, et al. Deafferented adult rod bipolar cells create new synapses with photoreceptors to restore vision. J Neurosci. 2017;37:4635–4644. doi: 10.1523/JNEUROSCI.2570-16.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Beier C, Kung J, Huie P, Dalal R, Palanker D, Sher A. Bipolar cells restructure dendrites after selective ablation of photoreceptors. Invest Ophthalmol Vis Sci. 2014;55:4171–4171. [Google Scholar]
- 24.Ghosh F, Wong F, Johansson K, Bruun A, Petters RM. Transplantation of full-thickness retina in the rhodopsin transgenic pig. Retina. 2004;24:98. doi: 10.1097/00006982-200402000-00014. [DOI] [PubMed] [Google Scholar]
- 25.McLelland BT, Lin B, Mathur A, et al. Transplanted hESC-derived retina organoid sheets differentiate, integrate, and improve visual function in retinal degenerate rats. Invest Ophthalmol Vis Sci. 2018;59:2586–2603. doi: 10.1167/iovs.17-23646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li SY, Yin ZQ, Chen SJ, Chen LF, Liu Y. Rescue from light-induced retinal degeneration by human fetal retinal transplantation in minipigs. Curr Eye Res. 2009;34:523–535. doi: 10.1080/02713680902936148. [DOI] [PubMed] [Google Scholar]
- 27.Silverman MS, Hughes SE, Valentino TL, Liu Y. Photoreceptor transplantation: anatomic, electrophysiologic, and behavioral evidence for the functional reconstruction of retinas lacking photoreceptors. Exp Neurol. 1992;115:87–94. doi: 10.1016/0014-4886(92)90227-h. [DOI] [PubMed] [Google Scholar]
- 28.LaVail MM, Sidman RL, Gerhardt CO. Congenic strains of RCS rats with inherited retinal dystrophy. J Hered. 1975;66:242–244. doi: 10.1093/oxfordjournals.jhered.a108621. [DOI] [PubMed] [Google Scholar]
- 29.Ray A, Sun GJ, Chan L, Grzywacz NM, Weiland J, Lee EJ. Morphological alterations in retinal neurons in the S334ter-line3 transgenic rat. Cell Tissue Res. 2010;339:481–491. doi: 10.1007/s00441-009-0916-5. [DOI] [PubMed] [Google Scholar]
- 30.Magharious MM, D'Onofrio PM, Koeberle PD. Optic nerve transection: a model of adult neuron apoptosis in the central nervous system. J Vis Exp. 2011;51 doi: 10.3791/2241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rovere G, Nadal-Nicolás FM, Agudo-Barriuso M, et al. Comparison of retinal nerve fiber layer thinning and retinal ganglion cell loss after optic nerve transection in adult albino rats. Invest Ophthalmol Vis Sci. 2015;56:4487–4498. doi: 10.1167/iovs.15-17145. [DOI] [PubMed] [Google Scholar]
- 32.Ritter M, Sacu S, Deák GG, et al. In vivo identification of alteration of inner neurosensory layers in branch retinal artery occlusion. Br J Ophthalmol. 2012;96:201–207. doi: 10.1136/bjo.2010.198937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schraermeyer U, Peters S, Thumann G, Kociok N, Heimann K. Melanin granules of retinal pigment epithelium are connected with the lysosomal degradation pathway. Exp Eye Res. 1999;68:237–245. doi: 10.1006/exer.1998.0596. [DOI] [PubMed] [Google Scholar]
- 34.Semeraro F, Morescalchi F, Duse S, Gambicorti E, Russo A, Costagliola C. Current trends about inner limiting membrane peeling in surgery for epiretinal membranes. J Ophthalmol. 2015;2015:671905. doi: 10.1155/2015/671905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Grewal DS, Mahmoud TH. Autologous neurosensory retinal free flap for closure of refractory myopic macular holes. JAMA Ophthalmol. 2016;134:229–230. doi: 10.1001/jamaophthalmol.2015.5237. [DOI] [PubMed] [Google Scholar]
- 36.Kaplan HJ, Tezel TH, Berger AS, Wolf ML, Del Priore LV. Human photoreceptor transplantation in retinitis pigmentosa. A safety study. Arch Ophthalmol. 1997;115:1168–1172. doi: 10.1001/archopht.1997.01100160338012. [DOI] [PubMed] [Google Scholar]
- 37.Berger AS, Tezel TH, Del Priore LV, Kaplan HJ. Photoreceptor transplantation in retinitis pigmentosa: short-term follow-up. Ophthalmology. 2003;110:383–391. doi: 10.1016/S0161-6420(02)01738-4. [DOI] [PubMed] [Google Scholar]
- 38.Zarbin MA. Retinal pigment epithelium-retina transplantation for retinal degenerative disease. Am J Ophthalmol. 2008;146:151–153. doi: 10.1016/j.ajo.2008.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ghosh F, Rauer O, Arnér K. Immune privilege of allogeneic neuroretinal transplants in the subconjunctival space. Graefes Arch Clin Exp. 2008;246:1715–1722. doi: 10.1007/s00417-008-0933-1. [DOI] [PubMed] [Google Scholar]
- 40.Furashova O, Matthé E. Retinal changes in different grades of retinal artery occlusion: an optical coherence tomography study. Invest Ophthalmol Vis Sci. 2017;58:5209–5216. doi: 10.1167/iovs.17-22411. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.