Abstract
The aim of this meta-analysis was to evaluate the effectiveness of heat acclimatization (HA) on time trial (TT) performance, maximum oxygen uptake (VO2max), exercise heart rate (HRE), time trials heart rate (HRTT), maximal heart rate (HRM), core temperature (TC), mean skin temperature (TS), thermal comfort (TComf), plasma volume (PV), blood lactate concentration and rate of perceived exertion (RPE). Cochrane-CENTRAL, EMBASE, CINAHL and PubMed databases and reference lists of included studies were searched for randomized controlled trials that investigated the efficacy of HA in athletes. Data were then extracted from the entered studies for analyses. A total of 11 randomised controlled trials (215 participants; mean age, 26.09 years; 91% men) were included after screening of 508 titles and abstracts and 19 full-text articles. The pooled standard mean difference (SMD) between the HA and non-HA groups were 0.50 (95% CI: 0.03 to 0.97, p = 0.04) for TT performance and 1 (95% CI: 1 to 2, p = 0.007) for HRTT. The pooled mean difference (MD) between the HA and non-HA groups were -7 (95% CI: -13 to -1, p = 0.03) for HRM. The changes in TComf and RPE were too small to be meaningful. There were no significant differences between the HA and non-HA groups for VO2max, HRE, TC, TS, PV and blood lactate concentration (all p > 0.05). This meta-analysis implies that HA may improve tolerance to discomfort during heat exposure, but may not necessarily improve the associated physiological markers of improved performance.
Key points.
The primary finding of this analysis is that athletic performance is improved with heat acclimatization training
Our analysis was unable to determine the physiological variable(s) that are associated with improved performance
After heat acclimatization training athletes may be able to tolerate greater levels of thermal stress but our analysis was unable to determine physiological markers of adaption
Key words: Performance, heart rate, thermal comfort, rate of perceived exertion
Introduction
Hot and humid ambient environments affect the human physiological response to physical activity (No and Kwak, 2016; Tucker et al., 2004), and exercise-induced increases in core temperature (TC) and increased ambient temperature result in premature fatigue and loss of athletic performance (Al-Nawaiseh et al., 2013). Muscle and skin blood flow (Sawka et al., 2011), aerobic capacity (Tucker et al., 2004), early onset of anaerobic threshold (Tyka et al., 2009), stimulation and accumulation of stress hormones (Jones et al., 2010), increased anaerobic glycolysis, increased use of intramuscular glycogen and lactate accumulation (Tan et al., 2018), are all factors associated with increased body temperature during exercise. However, competitive athletes compete in a variety of environmental conditions, which emphasizes the importance of reducing the potential adverse effects of a hot environment on athletic performance (Al-Nawaiseh et al., 2013). Heat acclimatization (HA) has been undertaken by endurance athletes to enhance tolerance and exercise performance in hot conditions (Guy et al., 2016; Périard et al., 2015a). Generally, HA has been undertaken at sub-maximal intensities during exposure to elevated temperature and/or humidity (Taylor, 2014; Tyler et al., 2016). Some of these studies have reported beneficial responses, such as decreases in heart rate (HR), TC and skin temperatures (TS) (Brade et al., 2013).
Alterations in critical physiological parameters such as increased plasma volume (PV), reduced exercise HR (HRE) (Kelly et al., 2016; Sawka et al., 2011), lower resting and exercise TC (Sawka et al., 2011; Tyler et al., 2016), and improved maximal cardiac output (Sawka et al., 1985; Shvartz et al., 1977), can all lead to increased performance (Guy et al., 2016) via short and medium duration HA programs. These adaptations could be beneficial for consequent performance in the heat, as well as in the cold, where possible fluid loss may be considerable (Corbett et al., 2014). The apparent dose-response to HA proposes that 15 days or more is required to optimize performance (Guy et al., 2015). Nevertheless, PV, HR and TC adjustments can take place as quickly as four days, and sustained thermal adaptation needs to be maintained by regular exertional exposure to hot climates (Weller et al., 2007).
Numerous elite sporting competitions are programmed in geographical locations that involve exposure to hot and humid environments, such as the 2020 Tokyo Olympics and 2022 Qatar World Cup. Hence, it is essential that athletes should be readied for such competitions, especially those who live and exercise in cold environments or are unaccustomed to heat stress (Milne and Shaw, 2008).
A previous meta-analysis on HA efficacy was conducted (Tyler et al., 2016), but only included investigations up until February 2016 and also included non-randomized, controlled trials. Additional randomized controlled trials (RCTs) have since been published, and this argues in favor of carrying out an updated meta-analysis. This update includes data pooling for several outcomes that were previously not carried out because of insufficient outcome data. The aim of this meta-analysis was to update previous pooled analyses, using only level 1 (RCT) evidence, on outcome measures relating to thermoregulatory adaptations attributed to HA with athletic performance in RCTs.
Methods
Search strategy
This systematic review and meta-analysis has been reported using the PRISMA guidelines (Liberati et al., 2009). Accordingly, using a PubMed search strategy (1966 to Nov 1, 2018), we identified relevant articles by the following keywords: “acclimation”, “acclimatization”, “heat”, “acclimation and performance”, “temperature”, “exercise training in heat”. Then, after the initial screening, the references of all studies based on the inclusion and exclusion criteria were examined to find additional studies.
Study selection
Two reviewers separately looked at the titles and read the abstracts and filtered relevant articles to be included. The four-phase (identifying, screening, qualification and inclusion) method identified were used in the PRISMA report to diminish the number of primary search results.
Inclusion/exclusion criteria
Study design: full text articles of controlled trials and RCTs of heat exercise training of natural and artificial HA, excluding review articles, conference abstracts and study protocols.
Comparison intervention: study protocols that used heat training (HOT) with thermo-neutral training (NEUTRAL), in a pre-post design, excluding the studies on acute interventions (e.g., single-session interventions) and also water immersion interventions.
Population: Men and women (age ≥ 18 years) who identified as triathletes, runners, endurance athletes, cyclists or team sport athletes from both elite and sub elite competitive levels.
Publications: English language manuscripts published in specialised English journals.
Outcome measures
The outcome measurements of this meta-analysis were;
Time trial (TT) performance (in seconds): in included studies TT performance were measured with the test of maximal leg cycle exercise test (time to reach exhaustion), 5 km TT performance, 20-km cycling, and running 3 km TT on a motorized treadmill.
Maximum oxygen uptake (VO2max in ml/kg/min), Exercise (HRE), time trials (HRTT) and maximal heart rate (HRM).
Core (TC) and mean skin temperature (TS): in included studies TC was measured in the rectal (Guy et al., 2016; Lorenzo et al., 2010; Sunderland et al., 2008; Willmott et al., 2016), gastrointestinal (Chalmers et al., 2016; Petersen et al., 2010; Schmit et al., 2018), and oesophageal (Nielsen et al., 1993) sites. In addition, end exercise values (Lorenzo et al., 2010; Nielsen et al., 1993) and also delta temperature from pre-post values (Chalmers et al., 2016; Guy et al., 2016; Petersen et al., 2010; Schmit et al., 2018; Willmott et al., 2016) were used for TC and TS in included studies.
Thermal comfort (TComf): in included studies TComf was determined according to the 5-point scale, 8-point scale or a 10-point scale.
Plasma volume (PV in percent): change in PV (%) was estimated using the method of Dill and Costill 1974 or PV was calculated from body mass by the equation of Sawka et al 1992.
Blood lactate (mmol.L).
Rate of perceived exertion (RPE): in included studies RPE was measured using the Borg and Kaijser 2006 scales.
Statistical analysis
For all included studies, we summarized the effect size for any outcome by measuring the mean difference between the heat and neutral condition from before and after the intervention. If multiple articles were published from the same dataset then we checked the data in order to avoid using the same results for the same outcome measure on more than one occasion. Results were analyzed by weighted mean difference (MD), if the measurement method or reporting was identical. For outcomes using different measurement or reporting techniques a standardized mean difference (SMD) was used. All analyses were conducted using Review Manager 5.3 (The Nordic Cochrane Centre, Copenhagen, Denmark). Extracted outcome data employed were change in the mean ± SD. In studies that reported SE data, these were converted to SD. A random-effects inverse variance was employed. When a standardized mean difference (SMD) was used the guideline for commentary was used (Cohen, 1988), with 0.2 described as small, 0.5 medium and 0.8 as large. Where an article contained a control group and more than one HA group, we separately labelled each HA groups and adjusted the sample size of the control group according to the number of HA groups. We presented meta-analysis using forest plots and applied a 5% level of significance to describe the significance of results.
Heterogeneity: To evaluate the heterogeneity among the studies, the I2 statistic was employed, with values > 50% showing substantial heterogeneity (Higgins et al., 2003). The risk of publication bias was assessed using the Egger plot (Egger et al., 1997). Any analysis of heterogeneity depends on the number of trials included in a meta-analysis, which is generally small, and this limits the statistical power of the test. We therefore based evidence of asymmetry on P<0.1, and we present intercepts with 90% confidence intervals.
Study quality: Study quality and reporting was assessed using the validated TESTEX scale (Table 1) (Smart et al., 2015). This is a validated 15-point scale which evaluates quality of the study (5 points maximum) and reporting (10 points maximum). A study with a TESETX quality score of less than 10 was deemed of low quality.
Table 1.
Study quality assessment of included studies using the tool for the assessment of study quality in exercise (TESTEX).
| Study | Eligibility Criteria specified | Randomisation Details Specified |
Allocation concealed | Groups similar at baseline | Assessors blinded | Outcomes measures assessed >85% participants | Intention to treat analysis | Reporting between group statistical comparison |
Point measures & measures of variability |
Activity monitoring in control group |
Relative exercise intensity constant |
Exercise volume & Energy expenditure |
Overall TESTEX (/15) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Chalmers 2016 | 1 | 0 | 0 | 1 | 0 | 3 | 1 | 2 | 1 | 1 | 0 | 1 | 11 |
| Chen 2013 | 1 | 1 | 0 | 1 | 0 | 2 | 0 | 2 | 1 | 1 | 0 | 1 | 10 |
| Guy 2016 | 1 | 1 | 0 | 1 | 0 | 2 | 0 | 2 | 1 | 1 | 1 | 0 | 10 |
| Karlsen 2015 | 1 | 0 | 0 | 1 | 0 | 2 | 0 | 2 | 1 | 1 | 0 | 1 | 9 |
| Kelly 2016 | 1 | 1 | 0 | 0 | 0 | 2 | 0 | 2 | 1 | 1 | 0 | 1 | 9 |
| Lorenzo 2010 | 1 | 1 | 0 | 1 | 0 | 2 | 0 | 2 | 1 | 1 | 0 | 1 | 10 |
| Nielsen 1993 | 1 | 0 | 0 | 1 | 0 | 3 | 1 | 2 | 1 | 1 | 0 | 1 | 11 |
| Peterson 2010 | 1 | 1 | 0 | 1 | 0 | 2 | 0 | 2 | 1 | 1 | 0 | 1 | 10 |
| Schmit 2017 | 1 | 1 | 0 | 1 | 0 | 2 | 0 | 2 | 1 | 1 | 0 | 0 | 9 |
| Sunderland 2007 | 1 | 0 | 0 | 1 | 0 | 2 | 0 | 2 | 1 | 1 | 0 | 1 | 9 |
| Willmott 2016 | 1 | 1 | 0 | 1 | 0 | 2 | 0 | 2 | 1 | 1 | 1 | 0 | 10 |
Results
Study characteristics
Figure 1 displays the selection process employed to include manuscripts in our meta-analysis. Of 617 possibly associated articles reclaimed from the search, 113 were animal studies and a further 489 were excluded by title or abstract, leaving 19 full text articles. A further 4 were excluded as duplicate studies, two more were excluded as they used immersion water protocol and 2 used an acute protocol, leaving 11 studies for the meta-analysis.
Figure 1.
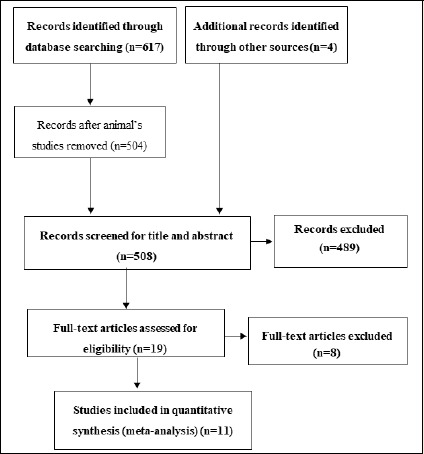
PRISMA flow diagram.
The characteristics of the included articles are shown in Table 2. The eleven included studies had a total of 215 subjects, 195 (91%) males and 20 (9%) females. There were 123 (57%) subjects in heat group and 92 (43%) in the non-heat group. The mean age of all subjects was 26.09 ± 0.09 years. All included articles were RCTs promulgated since 1993. Studies were performed in the United State (1), France (1), Taiwan (1), Denmark (2), England (2), and in Australia (4). The intervention period for studies ranged from 4-14 days and the mean length of each session was 59 min (range 27-90 min). The HOT protocols frequency were 4-14 days (1-2 session per day), 27-90 min in each session at 30% VO2 to 100% HRmax. The reviewed full-text studies were excluded from the analysis with 3 reasons (non-randomized control trial study, used an acute protocol, inadequate participants population).
Table 2.
Meta-analysis of heat acclimation included studies.
| Study | HA / C group |
HA activity | Intervention group: HA frequency and duration | Control group: frequency and duration |
Measure (Outcome) |
Performance test |
|---|---|---|---|---|---|---|
| Chalmers 2016 | Study 1: 9 / 9 Study 2: 12 / 11 |
Perceptually regulated treadmill exercise training |
Study 1: 5 days × 38 min in 35 °C and 30% RH Study 2: 4 days × 58 min in 35 °C and 30% RH |
Study 1: 5 days × 38 min in 19 °C and 30% RH Study 2: 4 days × 58 min in 19 °C and 30% RH |
HRE, TC, VO2max, PV, Blood Lactate, TComf, RPE | - |
| Chen 2013 | 7 / 7 | Cycling at 10% below VT to 10% above VT | 5 days × 35 min (mean) in 38.4°C ± 0.4°C, 52.0% ± 4.6% RH | 5 days × 35 min (mean) in 24.1°C ± 0.3°C, 51.5% ± 4.5% RH | VO2max, Performance, TS, HRM |
Maximal leg cycle exercise test (GXT): time to reach exhaustion |
| Guy 2016 | 8 / 8 | Cycling at 55 % VO2max Cycling at 50, 60, and 70 % VO2 max |
7 days × 40 min at 35°C and 70% RH 3 HST tests × 3 sets × 10 min at 35 °C and 70 % RH |
7 days × 40 min at 20°C, 45% RH 3 HST tests × 3 sets × 10 min at 35 °C and 70 % RH |
TC, Performance, HRTT, RPE, TComf, HRE |
5 km TT performance |
| Karlsen 2015 | 9 / 9 | Cycling at 80–100% HRMAX Cycling at moderate intensity |
14 days × 38 min in 35 °C 14 days × 90 min in 35 °C |
14 days × 38 min in 5–13 °C 14 days × 90 min in 5–13 °C |
VO2max, PV | - |
| Kelly 2016 | 7 / 7 | High Intensity Interval Training at 90% and 30% VO2 |
5 sessions × 27 min in 38.7 ± 0.5 °C; 34.4 ± 1.3 % RH | 5 sessions × 27 min in 22.3 ± 0.2 °C; 35.8 ± 0.6 % RH | HRE, TS, RPE, TComf |
- |
| Lorenzo 2010 | 12 / 8 | Cycling at 50 % VO2max | 10 days × 2 bouts × 45 min with 10 min rest in 40°C and 30% RH | 10 days × 2 bouts × 45 min with 10 min rest in 13°C and 30% RH | TC, V̇O2max, TS, HRM, PV, Blood Lactate, |
- |
| Nielsen 1993 | 8 / 5 | Cycling at 60 % VO2max | 9-12 days × 90 min in 40-42°C and 10-15% RH | 9-12 days × 90 min in 18-20°C and 10-15% RH | TC, TS, PV | - |
| Petersen 2010 | 6 / 6 | High intensity cycling | 4 days × 38 min (mean) in 30°C, 60% RH | 4 days × 38 min (mean) in 20°C, 60% RH | HRE, TC, TS, Blood Lactate, TComf | - |
| Schmit 2017 | 19 / 10 | Low intensity training or High intensity training |
5 days × 60 min in 30°C, 50% RH | Undertook some training sessions in the lab at 21°C, 50% RH | Performance, TC, HRTT, RPE |
20-km cycling TT in 35°C, 50% RH |
| Sunderland 2007 | 12 / 5 | Loughborough Intermittent Shuttle Test |
4 sessions × 38 min (mean) in 30°C, 24% RH | 4 sessions × 38 min (mean) in 18°C, 41% RH | TC, HRE, PV, Blood lactate, RPE, TComf |
- |
| Willmott 2016 | 14 / 7 | Cycling at 50 % VO2max | SDHA: 4 days × 45 min in 35.2 ±0.5°C, 60±2% RH TDHA: 2 days × 2 sessions × 45 min in 35.4±0.8, 61±3% RH |
4 days × 45 min in 21.7±0.6°C, 39±5 % RH | Performance, HRE, TC, PV, HRTT, RPE | 3 km TT performance in 30 °C, 60% RH |
HA = Heat Acclimation, HR = Heart Rate, RH = Relative Humidity, PV = Plasma Volume, VT = Ventilator Threshold, HST = Heat Stress Tests, HRTT = Heart Rate Time Trial, TC = Core Temperature, TS = Skin Temperature, HRE = Exercising Heart Rate, RPE = Rate of Perceived Exertion, TComf = Thermal Comfort, HRM = Maximum Heart Rate, HIIT = High Intensity Interval Training, SDHA = Single Session Per Day Heat Acclimation, TDHA = Twice Daily Heat Acclimation.
Outcome measures
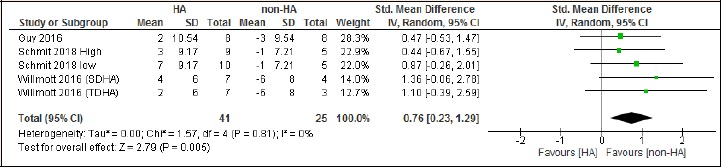
Change in Time Trial (TT) performance: The change in exercise TT performance following HA is depicted in Figure 3. Four studies reported the effects of HA on TT performance, nevertheless, six data sets were investigated owing to subgroups in the studies of Schmit et al. (2018) and Willmott et al. (2016). The SMD in the TT performance significantly changed after HA (SMD, 0.50; 95% CI, 0.03 to 0.97; p = 0.04).
Figure 3.
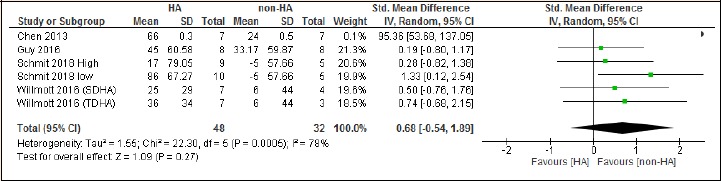
Forest plot of effect of HA on time trial performance.
Change in VO2max: The change in VO2max (ml.kg-1. min-1) following HA is displayed in Figure 4. Four studies evaluated the VO2max. HA did not have a significant effect on VO2max (MD, 2.51 ml.kg-1. min-1; 95% CI, -1.36 to 6.37; p = 0.20).
Figure 4.
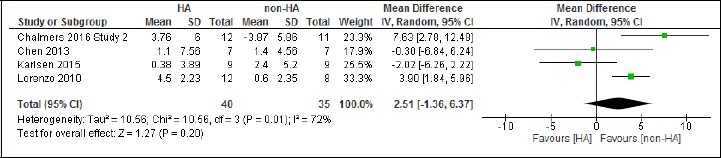
Forest plot of effect of HA on VO2max.
Change in Exercise Heart Rate (HRE): Five studies reported the effects of HA on HRE, however, seven intervention groups were evaluated owing to subgroups in the studies of Chalmers and Willmott. The MD in the HRE did not significantly change after HA (MD, -1 beats/min; 95% CI, -2 to 1; p = 0.15) (Figure 5).
Figure 5.
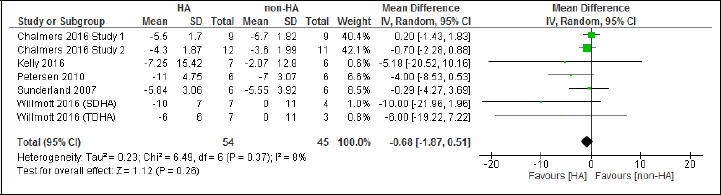
Forest plot of effect of HA on exercising heart rate.
Changes in Time Trial Heart Rate (HRTT): The effects of HA on HRTT was reported in three studies, nonetheless, owing to subgroups in the studies of Schmit and Willmott, five intervention groups were analyzed. Figure 6 reveals the SMD change in HRTT with HA. The change in HRTT was significantly higher in the HA groups (SMD, 1 beats/min; 95% CI, 1 to 2; p = 0.007).
Figure 6.
Forest plot of effect of HA on time trial heart rate.
Changes in Maximum Heart Rate (HRM): The effects of HA on HRM was reported in three studies, nonetheless, owing to subgroups in the studies, four data collections were reported. Figure 7 displays the MD changes in HRM with HA. The HRM decreased significantly after HA (MD, -7 beats/min; 95% CI, -13 to -1; p = 0.03).
Figure 7.
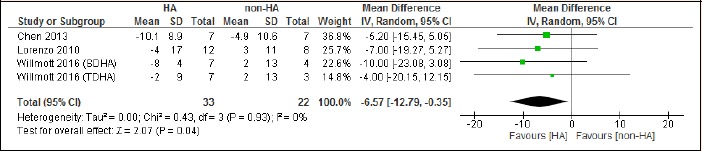
Forest plot of effect of HA on maximum heart rate.
Changes in Core Temperature (TC) and mean skin temperature (TS): The effects of HA on TC was reported in eight studies, however, owing to subgroups in the studies, 11 data collections were reported. On the other hand, the mean TS was reported in five studies. Figure 8 displays the MD changes in TC (A) and mean TS (B) with HA, respectively. Neither the changes of TC nor the changes of mean TS were significant. (MD, -0.05°C; 95% CI, -0.15 to 0.04; p = 0.28; MD, -0.31°C; 95% CI, -0.68 to 0.06; p = 0.10 for TC and mean TS respectively).
Figure 8.
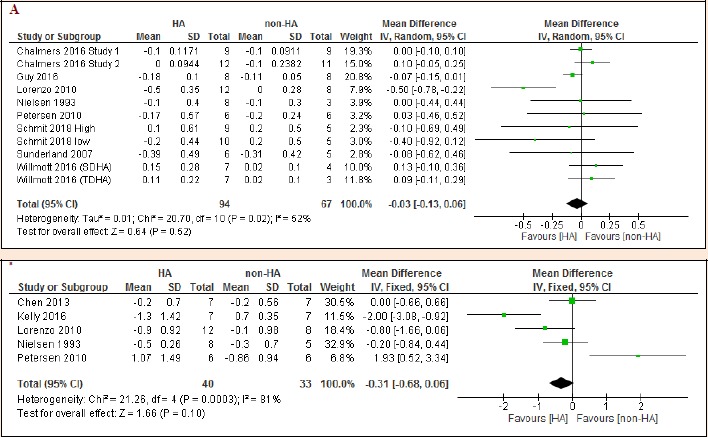
Forest plot of effect of HA on core temperature (A) and skin temperature (B).
Changes in Plasma Volume (PV): Six studies reported the effects of HA on PV, nevertheless, eight data collections were evaluated owing to subgroups in the studies. Figure 9 illustrates the SMD in the PV. PV did not change significantly after HA (SMD, 0.64 percent; 95% CI, -0.18 to 1.45; p = 0.13).
Figure 9.
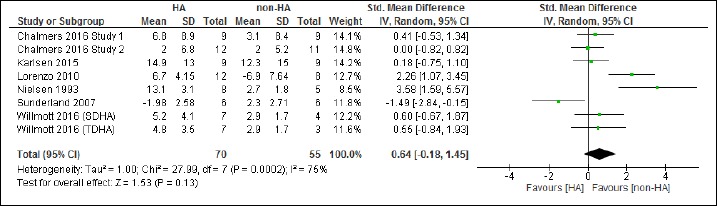
Forest plot of effect of HA on plasma volume.
Change in Blood Lactate: Four studies reported the effects of HA on blood lactate, nevertheless, five data sets were evaluated owing to subgroups in one of the studies. Figure 10 illustrates the MD in blood lactate which did not change significantly after HA (MD, 0.37 mmol.L; 95% CI, -0.22 to 0.97; p = 0.22).
Figure 10.
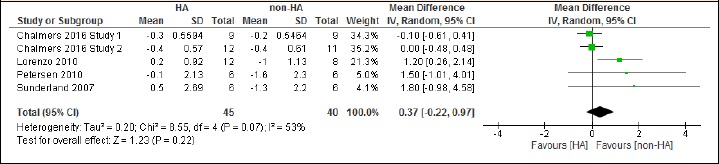
Forest plot of effect of HA on blood lactate.
Changes in TComf: The effects of HA on TComf was reported in five studies, however, owing to subgroups in the studies, six data collections were reported. The change in TComf was less than 0.2 of a unit and is therefore not reported graphically as it is not physiologically meaningful.
Changes in RPE: The effects of HA on the RPE was reported in six studies, however, owing to subgroups in the studies, nine data collections were reported. The change in RPE was less than 0.5 of a unit and is therefore not presented graphically as it is not physiologically meaningful.
Heterogeneity: For the analyses of TT performance, HRTT, HRM and TComf (all 0%) and also for the RPE analysis (6%) heterogeneity was low.
Study Quality: Median TESTEX score was 10 (see Table 1). Allocation concealment and assessor blinding were not performed in any of the included studies. Only two studies performed intention to treat analyses. Only two studies adjusted the relative training intensity.
Discussion
This meta-analysis aimed to update previous pooled analyses, using only level 1 RCT evidence on outcome measures relating to thermoregulatory adaptations attributed to HA during athletic performance. The results reveal that HA significantly improved TT performance, HRTT, HRM. The change in RPE and TComf were too small to be meaningful. However, there was no evidence of improvement in VO2max, HRE, TC, TS, PV and blood lactate concentration after HA. The relatively low levels of heterogeneity indicate data pooling was justified in the analyses.
TT Performance
Our result indicates HA had a significant effect on exercise TT performance. This finding is consistent with the results of Tyler et al. 2016, who reported HA had a moderately beneficial impact on exercise performance in the heat; nevertheless, they stated longer regimens (14 days) were more efficient than shorter programs (< 7 days). Another study has also suggested the extent of enhancements are dependent upon the training situation, exercise intensity and duration, environmental conditions and period of the HA protocol utilized (Périard et al., 2015b; Sunderland et al., 2008). Other work has shown that, by diminishing physiological pressure and reducing various other potential fatigue mechanisms, HA mediates improved performance (Nybo et al., 2011). The magnitude of HA advantage depends on the heat exposure frequency, with the highest effect sizes after long-term HA regimens, however both short-term and medium-term HA (8-14 days) shows moderate benefits (Tyler et al., 2016). Our sub-analysis also illustrates that the two studies with 5 days HA produced the highest alteration in TT performance (Chen et al., 2013; Schmit et al., 2018). Whilst there is no information to demonstrate the number of heat exposures required to improve performance, older work suggests full acclimatization may take up to one month (Horvath and Shelley, 1946).
VO2max and PV
Our results revealed no significant change in VO2max and PV following HA. A recent meta-analysis reported that HA had a moderate impact on reducing VO2max during steady-state, fixed-intensity exercise (Tyler et al., 2016). Blood volume adaptations in response to climate manipulation were first published via Barcroft et al. (1922). A full description of the hematologic adjustments correlated with heat exposure have been published in subsequent works thereafter, suggesting that alterations in PV occur quite quickly and induce a transient reduction in hemoglobin and hematocrit, and sometimes the concentration of plasma proteins (Bazett et al., 1940). It has been suggested that an increase in VO2max could be mediated by PV expansion (Périard et al., 2015a), increased myocardial efficiency, and enhanced ventricular compliance (Bhella et al., 2014; Opondo et al., 2015), which would provide larger end-diastolic volume. In our study, neither myocardial efficiency nor ventricular compliance was investigated. Kanstrup and Ekblom (1984) stated that PV expansion was counter-productive in that it enhanced maximal cardiac output 8% but declined hemoglobin concentration by 8%; therefore VO2max remained unaltered. Furthermore, our findings indicate that the size of PV increase is influenced by the number of days of HA, the hydration state when calculated, TS and whether the person is resting or exercising (Harrison, 1985; Kenefick et al., 2014; Sawka et al., 1983).
HRE, HRM and HRTT
The changes in HRM and HRTT after HA were statistically significant in the HA groups, but HRE was unchanged. The mechanisms of adaptation in HRE are various and complicated, however PV changes induced via exercise, may account for most of the exercise-induced hypervolemia up to 2-4 weeks (Convertino, 1991). Willmott et al., 2016 reported no statistically significant changes in resting or HRE after short-term HA. However, applying their predefined analytical limits, significant decreases of 4% (twice daily for 2 days) and 6% (once daily for 4 days) were seen in exercising HR from sessions 1–4, with no change in the control group (1%). These authors reported that this adjustment is typically concurrent with hypervolemia and is recommended to diminish HR by 1 beat.min-1 per 1% ΔPV, consistent with their analytical limits and previous investigations (Garrett et al., 2009; Lorenzo et al., 2010; Nielsen et al., 1993; Patterson et al., 2004).
TC and mean TS
Our results failed to show changes in TC and TS after HA. Tyler et al. (2016) reported a moderate-to-large positive impact of HA in reducing the TC prior to and during exercise and they also reported HA had a large impact in decreasing mean TS during exercise, these findings are different from our results. They stated that for short- (< 7 days) and medium-term (8-14 days) HA protocols, the effect sizes for Ts and TC were similar and smaller than in long-term HA (14 days) protocols. There is evidence that people living and training over many weeks in the heat might endure higher maximal TC than those undertaking HA training for just 1 or 2 weeks (Sawka et al., 2001), and trained people can tolerate higher TC (Mora-Rodriguez et al., 2010; Périard et al., 2012). In addition, it has been reported that trained runners completing an 8-km running TT in warm situations are capable of sustaining running velocity, notwithstanding a TC exceeding 40 °C (Ely et al., 2009). More recently, it was reported that trained cyclists approach a TC of 40.1–40.2 °C at the end of a 43.3-km TT in hot situations (Racinais et al., 2015). Consequently, it does appear that raised aerobic fitness presents an enhanced capability to tolerate higher TC. However, the extent to which HA provides such an advantage remains unclear.
Considerable proof of marked alterations in Tc and Ts exist in many physiological and biochemical functions at a crucial temperature in vivo and in vitro, and heterogeneity in thermo sensitivity exists among different tissues (Brinnel et al., 1987). The TC level can rely on several agents such as exercise intensity and duration, fitness, nutrition, dehydration and motivation; and hence would be expected to vary significantly in absolute terms. Moreover, TC relies on the measurement site and the temperature gradients that exist within the body, particularly throughout exercise heat storage (Nielsen et al., 1993; Nielsen et al., 1990).
Blood Lactate
Our results illustrate that blood lactate did not change significantly after HA and this conflicts with recent meta-analysis findings (Tyler et al., 2016). The decrease in blood lactate concentration through submaximal exercise after HA suggests a decline in glycolytic participation from the contracting muscle, and this is known to happen with more traditional HA programs (Febbraio et al., 1994). Moreover, a prior investigation suggested that the blood lactate alteration was in part due to a reduction in sympathoadrenal activation and levels of circulating catecholamines (Febbraio, 2001). Some investigators propose that metabolic conformities caused by HA during exercise are due to a diminishing aerobic metabolic rate (Aoyagi et al., 1994), or diminishing rate of glycogenolysis (Febbraio et al., 1996). Alternatively, the expanded PV and consequently total blood volume (Bass et al., 1955; Harrison et al., 1981) could affect blood lactate concentration via enhanced blood flow to the splanchnic circulation, improving lactate elimination (Rowell et al., 1968), and therefore delaying the onset of blood lactate accumulation.
RPE and TComf
The change in RPE and TComf were too small to be meaningful, in agreement with our findings, Tyler et al. (2016) stated HA had a moderate impact on RPE and small impact on TComf. TComf is a crucial stimulus which drives voluntary behavior (such as exercise performance and capability) in a warm situation, as it follows seasonal alterations in air temperature (De Dear and Brager, 2001). This emphasizes that TComf can be improved transiently in the heat via passive exposure to warmer temperatures. TComf is due to various psychophysical criteria, and it appears logical to recommend that HA could enhance TComf via shifting exposure to higher temperatures. Nevertheless, data concerning the effectiveness in doing so are currently inadequate to draw firm conclusions. Further investigation is also needed to examine the variation and specificity of adjustment between natural and artificial heat exposure and the potential for unnatural exposure to improve performance in natural competition. HA may vary with the environmental exercise situations to be faced, including the exercise task, solar radiation, and terrain/geography.
Study Quality
Median TESTEX score was 10. Allocation concealment and assessor blinding were not performed in any of the included studies, however this is unavoidable in HA experiments. Only two studies performed intention to treat analyses, this may be a reflection of the relatively low attrition rates due to small sample sizes of included studies, but ITT may also have been simply overlooked in some case where it was indicated . Only two studies adjusted the relative training intensity and this may explain why VO2max and related performance outcomes were unchanged, although by nature HA studies may be of insufficient duration to elicit changes in these parameters.
Limitations
Our meta-analysis has some limitations that should be considered. First, we only analyzed 11 RCTs, and eight of them have small sample sizes (n<20). This argues that more RCTs with larger sample sizes are needed to provide more definitive results. Second, exercise intensity and duration, environmental conditions and period of the HA protocol varied substantially in the utilized RCTs, and this may have impacted our results. Finally, about the data collecting, we calculated the mean differences between pre and post-intervention. Nevertheless, in cases where accurate p values within or between groups or 95% CI were unavailable, default p values were employed, and this may also have impacted our results. Egger plots suggest minimal likelihood of publication bias, indicating there may not be negative, unpublished datasets in existence. However, the small number of studies limited the relevance of Egger plots in these analyses.
Conclusion
HA has a beneficial effect on TT performance, HRTT, HRM, but was not statistically significant in VO2max, HRE, TC, mean TS, PV and blood lactate. The changes in RPE and TComf were too small to be meaningful. From a high performance coaching perspective, these findings suggest HA improves the athlete’s tolerance to discomfort during heat exposure, but may not alter the associated physiological markers of improved performance.
Acknowledgements
The authors report no conflict of interest.
Biographies
Gholam Rasul Mohammad RAHIMI
Employment
A doctoral researcher and a teacher in exercise and sports Science and exercise physiology.
Degree
PhD
Research interests
The effects of exercise in people with chronic diseases.
E-mail: rmohammadrahimi@mail.um.ac.ir

Alsaeedi Lafi ALBANAQI
Employment
Masters student in Biomedical Science at the University of New England, Australia.
Degree
BSc
E-mail:aalbanaq@myune.edu.au

Tom van der TOUW
Employment
Senior lecturer in biomedical science at the University of New England, Armidale, Australia.
Degree
PhD
Research interests
Chronic obstructive pulmonary disease, ischaemia-reperfusion and blood flow responses to isometric exercise
E-mail: tvandert@une.edu.au

Neil A. SMART
Employment
Prof., School of Science and Technology, University of New England, Australia
Degree
PhD
Research interests
The optimal exercise dose for managing a range of chronic illnesses including heart, lung, metabolic and renal.
E-mail: nsmart2@une.edu.au
References
- Al-Nawaiseh A., Bataynefh M.a., Alsuod H.J.J.o.E.P.O. (2013) Physiological Responses of Distance Runners during Normal and Warm Conditions. Journal of Exercise Physiology Online 16. [Google Scholar]
- Aoyagi Y., McLellan T.M., Shephard R.J. (1994) Effects of training and acclimation on heat tolerance in exercising men wearing protective clothing. European Journal of Applied Physiology and Occupational Physiology 68, 234-245. [DOI] [PubMed] [Google Scholar]
- Barcroft J., Meakins J., Davies H., Scott J.D., Fetter W. (1922) On the relation of external temperature to blood volume. Philosophical Transactions of the Royal Society B 211, 455. [Google Scholar]
- Bass D.E., Kleeman C.R., Quinn M., Henschel A., Hegnauer A.H. (1955) Mechanisms of acclimatization to heat in man. Medicine 34, 323-380. [DOI] [PubMed] [Google Scholar]
- Bazett H., Sunderman F., Doupe J., Scott J. (1940) Climatic effects on the volume and composition of blood in man. American Journal of Physiology-Legacy Content 129, 69-83. [Google Scholar]
- Bhella P.S., Hastings J.L., Fujimoto N., Shibata S., Carrick-Ranson G., Palmer M.D., Boyd K.N., Adams-Huet B., Levine B.D. (2014) Impact of lifelong exercise “dose” on left ventricular compliance and distensibility. Journal of the American College of Cardiology 64, 1257-1266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borg E., Kaijser L. (2006) A comparison between three rating scales for perceived exertion and two different work tests. Scandinavian Journal of Medicine & Science in Sports 16, 57-69. [DOI] [PubMed] [Google Scholar]
- Brade C., Dawson B., Wallman K.J.J.o.S.S. (2013) Effect of precooling and acclimation on repeat-sprint performance in heat. Journal of Sports Sciences 31, 779-786. [DOI] [PubMed] [Google Scholar]
- Brinnel H., Cabanac M., Hales J. (1987) Critical upper levels of body temperature, tissue thermosensitivity and selective brain cooling in hyperthermia. In: Proceedings of the 1st World Conference, Sydney-Australia; 27 Aoril-1 May, 1987 Heat stress; Physical Exertion and Environment. 209-240. [Google Scholar]
- Chalmers S., Esterman A., Eston R., Norton K. (2016) Brief heat training: no improvement of the lactate threshold in mild conditions. International Journal of Sports Physiology and Performance 11, 1029-1037. [DOI] [PubMed] [Google Scholar]
- Chen T.-I., Tsai P.-H., Lin J.-H., Lee N.-Y., Liang M.T. (2013) Effect of short-term heat acclimation on endurance time and skin blood flow in trained athletes. Open Access Journal of Sports Medicine 4, 161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J.J.N.L.E.A. (1988) Statistical power analysis for the behavioural sciences. Hillsdale. NJ: Lawrence Earlbaum Associates; 2. [Google Scholar]
- Convertino V.A. (1991) Blood volume: its adaptation to endurance training. Medicine and Science in Sports and Exercise 23, 1338-1348. [PubMed] [Google Scholar]
- Corbett J., Neal R.A., Lunt H.C., Tipton M.J.J.S.M. (2014) Adaptation to heat and exercise performance under cooler conditions: a new hot topic. Sports Medicine 44, 1323-1331. [DOI] [PubMed] [Google Scholar]
- De Dear R., Brager G.S. (2001) The adaptive model of thermal comfort and energy conservation in the built environment. International journal of biometeorology 45, 100-108. [DOI] [PubMed] [Google Scholar]
- Dill D.B., Costill D.L. (1974) Calculation of percentage changes in volumes of blood, plasma, and red cells in dehydration. Journal of Applied Physiology 37, 247-248. [DOI] [PubMed] [Google Scholar]
- Egger M., Smith G.D., Schneider M., Minder C. (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ: British Medical Journal 315, 629-634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ely B.R., Ely M.R., Cheuvront S.N., Kenefick R.W., DeGroot D.W., Montain S.J. (2009) Evidence against a 40 C core temperature threshold for fatigue in humans. Journal of Applied Physiology 107, 1519-1525. [DOI] [PubMed] [Google Scholar]
- Febbraio M.A. (2001) Alterations in energy metabolism during exercise and heat stress. Sports Medicine 31, 47-59. [DOI] [PubMed] [Google Scholar]
- Febbraio M.A., Snow R.J., Hargreaves M., Stathis C.G., Martin I.K., Carey M.F. (1994) Muscle metabolism during exercise and heat stress in trained men: effect of acclimation. Journal of Applied Physiology 76, 589-597. [DOI] [PubMed] [Google Scholar]
- Febbraio M.A., Snow R.J., Stathis C.G., Hargreaves M., Carey M.F. (1996) Blunting the rise in body temperature reduces muscle glycogenolysis during exercise in humans. Experimental Physiology: Translation and Integration 81, 685-693. [DOI] [PubMed] [Google Scholar]
- Garrett A.T., Goosens N.G., Rehrer N.G., Patterson M.J., Cotter J.D. (2009) Induction and decay of short-term heat acclimation. European Journal of Applied Physiology 107, 659. [DOI] [PubMed] [Google Scholar]
- Guy J.H., Deakin G.B., Edwards A.M., Miller C.M., Pyne D.B. (2015) Adaptation to hot environmental conditions: an exploration of the performance basis, procedures and future directions to optimise opportunities for elite athletes. Sports Medicine 45, 303-311. [DOI] [PubMed] [Google Scholar]
- Guy J.H., Pyne D.B., Deakin G.B., Miller C.M., Edwards A.M. (2016) Acclimation training improves endurance cycling performance in the heat without inducing endotoxemia. Frontiers in Physiology 7, 318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison M., Edwards R., Graveney M., Cochrane L.A., Davies J. (1981) Blood volume and plasma protein responses to heat acclimatization in humans. Journal of Applied Physiology 50, 597-604. [DOI] [PubMed] [Google Scholar]
- Harrison M.H. (1985) Effects on thermal stress and exercise on blood volume in humans. Physiological Reviews 65, 149-209. [DOI] [PubMed] [Google Scholar]
- Higgins J.P., Thompson S.G., Deeks J.J., Altman D.G. (2003) Measuring inconsistency in meta-analyses. BMJ: British Medical Journal 327, 557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horvath S., Shelley W. (1946) Acclimatization to extreme heat and its effect on the ability to work in less severe environments. American Journal of Physiology-Legacy Content 146, 336-343. [DOI] [PubMed] [Google Scholar]
- Jones D.A., Mundel T., Coxjaime P. (2010) Exercise, heat stress and the interleukin-6 response: support for temperaturemediated neuroendocrine regulatory mechanisms. Medicina Sportiva 14, 96-102. [Google Scholar]
- Kanstrup I.-l., Ekblom B. (1984) Blood volume and hemoglobin concentration as determinants of maximal aerobic power. Medicine and Science in Sports and Eercise 16, 256-262. [PubMed] [Google Scholar]
- Kelly M., Gastin P.B., Dwyer D.B., Sostaric S., Snow R.J. (2016) Short duration heat acclimation in Australian football players. Journal of Sports Science and Medicine 15, 118-125. [PMC free article] [PubMed] [Google Scholar]
- Kenefick R.W., Sollanek K.J., Charkoudian N., Sawka M.N. (2014) Impact of skin temperature and hydration on plasma volume responses during exercise. American Journal of Physiology-Heart and Circulatory Physiology 117(4), 413-420. [DOI] [PubMed] [Google Scholar]
- Liberati A., Altman D.G., Tetzlaff J., Mulrow C., Gøtzsche P.C., Ioannidis J.P., Clarke M., Devereaux P.J., Kleijnen J., Moher D. (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Medicine 6, e1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorenzo S., Halliwill J.R., Sawka M.N., Minson C.T. (2010) Heat acclimation improves exercise performance. Journal of Applied Physiology 109, 1140-1147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milne C., Shaw M. (2008) Travelling to China for the Beijing 2008 Olympic Games. British Journal of Sports Medicine 42, 321-326. [DOI] [PubMed] [Google Scholar]
- Mora-Rodriguez R., Del Coso J., Hamouti N., Estevez E., Ortega J.F. (2010) Aerobically trained individuals have greater increases in rectal temperature than untrained ones during exercise in the heat at similar relative intensities. European Journal of Applied Physiology 109, 973-981. [DOI] [PubMed] [Google Scholar]
- Nielsen B., Hales J., Strange S., Christensen N.J., Warberg J., Saltin B. (1993) Human circulatory and thermoregulatory adaptations with heat acclimation and exercise in a hot, dry environment. The Journal of Physiology 460, 467-485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nielsen B., Savard G., Richter E., Hargreaves M., Saltin B. (1990) Muscle blood flow and muscle metabolism during exercise and heat stress. Journal of Applied Physiology 69, 1040-1046. [DOI] [PubMed] [Google Scholar]
- No M., Kwak H.-B. (2016) Effects of environmental temperature on physiological responses during submaximal and maximal exercises in soccer players. Integrative Medicine Research 5, 216-222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nybo L., Rasmussen P., Sawka M.N. (2011) Performance in the heat—physiological factors of importance for hyperthermia-induced fatigue. Comprehensive Physiology 4, 657-689. [DOI] [PubMed] [Google Scholar]
- Opondo M.A., Sarma S., Levine B.D. (2015) The cardiovascular physiology of sports and exercise. Clinics in Sports Medicine 34, 391-404. [DOI] [PubMed] [Google Scholar]
- Patterson M.J., Stocks J.M., Taylor N.A. (2004) Sustained and generalized extracellular fluid expansion following heat acclimation. The Journal of Physiology 559, 327-334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Périard J., Racinais S., Sawka M. (2015a) Adaptations and mechanisms of human heat acclimation: applications for competitive athletes and sports. Scandinavian Journal of Medicine Science in Sports 25, 20-38. [DOI] [PubMed] [Google Scholar]
- Périard J., Racinais S., Sawka M. (2015b) Adaptations and mechanisms of human heat acclimation: applications for competitive athletes and sports. Scandinavian Journal of Medicine & Science in Sports 25, 20-38. [DOI] [PubMed] [Google Scholar]
- Périard J.D., Caillaud C., Thompson M.W. (2012) The role of aerobic fitness and exercise intensity on endurance performance in uncompensable heat stress conditions. European Journal of Applied Physiology 112, 1989-1999. [DOI] [PubMed] [Google Scholar]
- Petersen C.J., Portus M.R., Pyne D.B., Dawson B.T., Cramer M.N., Kellett A.D. (2010) Partial heat acclimation in cricketers using a 4-day high intensity cycling protocol. International Journal of Sports Physiology and Performance 5, 535-545. [DOI] [PubMed] [Google Scholar]
- Racinais S., Périard J.D., Karlsen A., Nybo L. (2015) Effect of heat and heat acclimatization on cycling time trial performance and pacing. Medicine and Science in Sports and Exercise 47, 601-606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowell L.B., Brengelmann G.L., Blackmon J.R., Twiss R.D., Kusumi F. (1968) Splanchnic blood flow and metabolism in heat-stressed man. Journal of Applied Physiology 24, 475-484. [DOI] [PubMed] [Google Scholar]
- Sawka M., Leon L., Montain S., Sonna L. (2011) Integrated physiological mechanisms of exercise performance, adaptation, and maladaptation to heat stress. Comprehensive Physiology 1, 1883-1928. [DOI] [PubMed] [Google Scholar]
- Sawka M.N., Latzka W.A., Montain S.J., Cadarette B.S., Kolka M.A., Kenneth K., Kraning I., Gonzalez R.R. (2001) Physiologic tolerance to uncompensable heat: intermittent exercise, field vs laboratory. Medicine & Science in Sports & Exercise 33, 422-430. [DOI] [PubMed] [Google Scholar]
- Sawka M.N., Toner M.M., Francesconi R.P., Pandolf K.B. (1983) Hypohydration and exercise: effects of heat acclimation, gender, and environment. Journal of Applied Physiology 55, 1147-1153. [DOI] [PubMed] [Google Scholar]
- Sawka M.N., Young A.J., Cadarette B.S., Levine L., Pandolf K.B. (1985) Influence of heat stress and acclimation on maximal aerobic power. European Journal of Applied Physiology and Occupational Physiology 53, 294-298. [DOI] [PubMed] [Google Scholar]
- Sawka M.N., Young A.J., Pandolf K.B., Dennis R.C., Valeri C.R. (1992) Erythrocyte, plasma, and blood volume of healthy young men. Medicine and Science in Sports and Exercise 24, 447-453. [PubMed] [Google Scholar]
- Schmit C., Duffield R., Hausswirth C., Brisswalter J., Le Meur Y. (2018) Optimizing Heat Acclimation for Endurance Athletes: High- Versus Low-Intensity Training. International Journal of Sports Physiology and Performance 13, 816-823. [DOI] [PubMed] [Google Scholar]
- Shvartz E., Shapiro Y., Magazanik A., Meroz A., Birnfeld H., Mechtinger A., Shibolet S.J.J.o.A.P. (1977) Heat acclimation, physical fitness, and responses to exercise in temperate and hot environments. Journal of Applied Physiology 43, 678-683. [DOI] [PubMed] [Google Scholar]
- Smart N.A., Waldron M., Ismail H., Giallauria F., Vigorito C., Cornelissen V., Dieberg G. (2015) Validation of a new tool for the assessment of study quality and reporting in exercise training studies: TESTEX. International Journal of Evidence-Based Healthcare 13, 9-18. [DOI] [PubMed] [Google Scholar]
- Sunderland C., Morris J.G., Nevill M. (2008) A heat acclimation protocol for team sports. British Journal of Sports Medicine 42, 327-333. [DOI] [PubMed] [Google Scholar]
- Tan X., Low I.C., Stephenson M.C., Soong T., Lee J.K. (2018) Neural basis of exertional fatigue in the heat: A review of magnetic resonance imaging methods. Scandinavian Journal of Medicine & Science in Sports 28, 807-818. [DOI] [PubMed] [Google Scholar]
- Taylor N.A.S. (2014) Human heat adaptation. Comprehensive Physiology 4, 325-365. [DOI] [PubMed] [Google Scholar]
- Tucker R., Rauch L., Harley Y.X., Noakes T.D.J.P.A. (2004) Impaired exercise performance in the heat is associated with an anticipatory reduction in skeletal muscle recruitment. Pflugers Archiv: European Journal of Physiology 448, 422-430. [DOI] [PubMed] [Google Scholar]
- Tyka A., Pałka T., Tyka A., Cisoń T., Szyguła Z.J.I.j.o.o.m. health, e. (2009) The influence of ambient temperature on power at anaerobic threshold determined based on blood lactate concentration and myoelectric signals. International Journal of Occupational Medicine and Environmental Health 22, 1-6. [DOI] [PubMed] [Google Scholar]
- Tyler C.J., Reeve T., Hodges G.J., Cheung S.S. (2016) The effects of heat adaptation on physiology, perception and exercise performance in the heat: a meta-analysis. Sports Medicine 46, 1699-1724. [DOI] [PubMed] [Google Scholar]
- Weller A.S., Linnane D.M., Jonkman A.G., Daanen H.A. (2007) Quantification of the decay and re-induction of heat acclimation in dry-heat following 12 and 26 days without exposure to heat stress. European Journal of Applied Physiology 102, 57-66. [DOI] [PubMed] [Google Scholar]
- Willmott A., Gibson O., Hayes M., Maxwell N. (2016) The effects of single versus twice daily short term heat acclimation on heat strain and 3000 m running performance in hot, humid conditions. Journal of Thermal Biology 56, 59-67. [DOI] [PubMed] [Google Scholar]


