Abstract
Little change over the decades has been seen in adults meeting moderate-to-vigorous physical activity (MVPA) guidelines. Numerous individual-level interventions to increase MVPA have been designed, mostly static interventions without consideration for neighborhood context. Recent technologies make adaptive interventions for MVPA feasible. Unlike static interventions, adaptive intervention components (e.g., goal setting) adjust frequently to an individual’s performance. Such technologies also allow for more precise delivery of “smaller, sooner incentives” that may result in greater MVPA than “larger, later incentives”. Combined, these factors could enhance MVPA adoption. Additionally, a central tenet of ecological models is that MVPA is sensitive to neighborhood environment design; lower-walkable neighborhoods constrain MVPA adoption and maintenance, limiting the effects of individual-level interventions. Higher-walkable neighborhoods are hypothesized to enhance MVPA interventions. Few prospective studies have addressed this premise. This report describes the rationale, design, intervention components, and baseline sample of a study testing individual-level adaptive goal-setting and incentive interventions for MVPA adoption and maintenance over 2 years among adults from neighborhoods known to vary in neighborhood walkability. We scaled these evidenced-based interventions and tested them against static-goal-setting and delayed-incentive comparisons in a 2×2 factorial randomized trial to increase MVPA among 512 healthy insufficiently-active adults. Participants (64.3% female, M age = 45.5 ± 9.1 years, M BMI = 33.9 ± 7.3 kg/m2, 18.8% Hispanic, 84.0% White) were recruited from May 2016 to May 2018 from block groups ranked on GIS-measured neighborhood walkability and socioeconomic status (SES) and classified into four neighborhood types: “high walkable/high SES,” “high walkable/low SES,” “low walkable/high SES,” and “low walkable/low SES.” Results from this ongoing study will provide evidence for some of the central research questions of ecological models.
Keywords: Physical Activity, Adaptive interventions, Built Environment, Financial Incentives, Rewards
1. INTRODUCTION
The proportion of adults meeting physical activity (PA) guidelines has not changed meaningfully over the last two decades [1-3], prompting numerous studies of how to increase PA using diverse strategies grounded in multiple behavioral theories and models. A meta-analysis of individual-level interventions to increase PA among healthy adults (N=99,001, 358 papers) found a mean difference of 2.1 min/day favoring interventions over controls [4], a difference insufficient to produce meaningful change in population health. Such findings indicate a dire need for more potent interventions to increase and maintain individuals’ PA to elicit health benefits.
1.1. Adaptive Goal Setting.
Adaptive interventions have been proposed as novel alternatives to static interventions for behavior change [5]. Adaptive intervention components respond repeatedly and uniquely to variations in an individual’s performance over time. Compared to traditional PA interventions with static goals (e.g., 30 min/day), adaptive goal setting harnesses continuously-measured variability in PA and offers dynamic goals in response to daily performance [6, 7]. Developments in internet-connected activity monitors facilitate intensive measurement that allow for adaptive components to precisely shape an individual’s performance over time [7-10]. In a series of studies, Adams et al. tested adaptive goal interventions and found greater improvements in steps/day over 4-6 months compared to static step goals [11-13]. Korinek et al. and Poirier et al. also tested varieties of adaptive step goal programs and found improvements in steps/day over 6 and 16 week periods, respectively [14, 15].
1.2. Financial Incentives.
Several theoretical approaches incorporate principles of positive reinforcement [16, 17], which have been proposed as unifying tenets for preventive medicine [18]. “Smaller, sooner incentives” for goal attainment (e.g., $1 per goal), are possible with mobile technologies and are hypothesized to result in greater PA than “larger, later incentives” (e.g., $100 at study end) [12, 13, 19]. Combining financial reinforcement with adaptive goals has the potential to enhance PA adoption and maintenance [12, 13]. A recent meta-analysis found financial incentives, relative to comparison treatments, were more effective for changing health behaviors, including PA [20].
1.3. Built Environments.
Observational studies consistently show that PA is sensitive to the design of neighborhood environments [21, 22]. A core hypothesis of ecological models [23, 24] is that individually-oriented behavior change interventions should be more effective when built environments, along with social and policy environments, support the target behavior. Only two studies found that aspects of neighborhood environments (e.g., walkability, availability of fitness outlets) may moderate individual-level interventions (although in inconsistent directions) [25, 26], while two other studies have found no evidence of moderation [27, 28]. All of these studies measured neighborhood features only after recruiting participants, rather than using a priori sampling designs that ensured sufficient between-neighborhood variability in PA-supportive environmental features.
Few prospective studies address the ecological model principle of interactions across levels of influence [26]. This report describes the rationale, design, intervention components, and baseline sample of a randomized trial testing individual-level adaptive goal setting and financial reinforcement interventions for PA adoption and maintenance among participants sampled from neighborhoods known to vary in neighborhood walkability and socioeconomic status (SES).
2. MATERIALS AND METHODS
The Walking Intervention Through Texting (WalkIT) Arizona study is a randomized 2 (Static Goal vs. Adaptive Goals) × 2 (Immediate Reinforcement vs. Delayed Reinforcement) factorial trial aimed at increasing moderate-to-vigorous physical activity (MVPA) among 512 insufficiently active men and women from the Maricopa County, Arizona region. Recruitment efforts began in May 2016 and ended in May 2018. Importantly, to test for interactions between intervention conditions and the built environment context in which participants live, we ranked all Maricopa County, Arizona census block groups on GIS-measured neighborhood walkability and socioeconomic status (SES) prior to participant recruitment and enrolled participants from four neighborhood types: “higher walkable/higher SES,” “higher walkable/lower SES,” “lower walkable/higher SES,” and “lower walkable/lower SES.” To account for the effects of extreme summer temperatures that occur in Maricopa County, Arizona (i.e., over 100 days with temperatures of ≥100° Fahrenheit [38° Celsius]), we balanced enrollment across calendar months. Thus, the factorial randomized trial testing four interventions lasting 12 months was nested in an observational design with participants sampled equally across calendar months and balanced across strata of the neighborhood sampling design. An additional 12-month period of no-intervention follow up evaluates the effects of neighborhood design on MVPA maintenance. This approach allows us to test, within a multi-level design, synergistic effects of the interventions and neighborhood-level walkability and SES characteristics on MVPA adoption by 12 months and MVPA maintenance at 18 and 24 months post-randomization after accounting for extreme temperatures. The WalkIT Arizona study is a federally funded trial registered prospectively at ClinicalTrials.gov (NCT02717663). The Institutional Review Board at Arizona State University approved protocols for this study.
2.1. Hypotheses.
The primary aims of this study test four hypotheses: H1) 12-month adaptive goal setting and immediate financial reinforcement (compared to static goal setting and delayed reinforcement) interventions will independently result in significantly greater increases in accelerometer-derived MVPA over 12 months (i.e., adoption), and during the follow-up period at 18 and 24 months (i.e., maintenance), regardless of neighborhood types; H2) the joint effects of adaptive goal setting and immediate reinforcement interventions will show significantly greater accelerometer-measured MVPA by 12 months and at 18 and 24 months than the other three intervention groups, regardless of neighborhood type; H3) the differences in MVPA adoption by 12 months and maintenance at 18 and 24 months predicted under H1 will be relatively larger in higher walkable (vs. lower walkable) neighborhoods; and H4) the joint effects of adaptive goal and immediate reinforcement on adoption and maintenance of MVPA predicted under H2 will be relatively greater in higher walkable (vs. lower walkable) neighborhoods. Secondary aims test the hypotheses described above, but with self-reported walking for transportation and recreation as the outcome, rather than accelerometer-measured MVPA. Exploratory questions paralleling H3 and H4 will be addressed by comparing effects across high vs. low SES (rather than higher vs, lower walkable) neighborhoods.
2.2. Neighborhood selection.
Participants were sampled from Maricopa County, Arizona Census block groups (BG) that differed on SES and built environment features. BGs are the smallest administrative unit for which geographical, socioeconomic, and built environment information were available. The 2010 Census delineated 2,505 BGs in Maricopa County, the majority of which being in the Phoenix metropolitan region. Following Frank et al., [29] we ranked all Maricopa County BGs from low to high on median household income using the Census’ American Community Survey data and then categorized BGs falling in 1st through 5th deciles as “lower SES” and those in the 7th through 10th deciles as “higher SES.” The 6th decile was omitted to create separation between these strata to ensure that participants in BGs at the upper boundary of the low SES stratum and lower boundary of the high SES stratum were not mis-categorized.
Second, using existing BG-level data from regional spatial repositories in Maricopa County we create a composite walkability index as a function of 4 variables : residential density (ratio of dwelling units to the total land area devoted to residential use in the BG), land use mix (diversity of several land uses per BG with normalized scores ranging from 0 for single use to 1 indicating an even distribution across uses), street network connectivity (ratio of number of intersections with 3 or more legs to the land area of the BG), and public transit access (ratio of bus and rail stops to total area of the BG). The walkability index was calculated using the following formula: Walkability Index = [(z-score for net residential density) + (z-score for land use mix) + 2*(z-score for intersection density) + (z-score for transit access)] [29]. BGs were ranked and categorized into “lower walkable” (1st through 4th deciles) and “higher walkable” (7th though 10th deciles). The 5th and 6th walkability deciles were excluded to create sufficient separation between the lower and higher walkability strata and minimize the likelihood of mis - categorization.
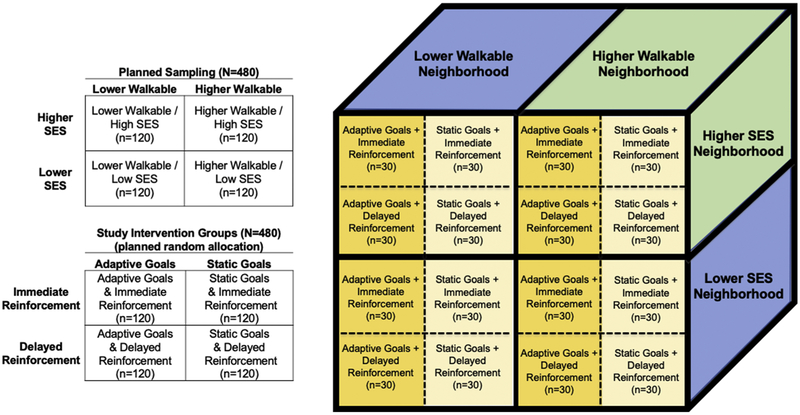
BGs were then classified according to their combined walkability and SES categorization yielding four neighborhood strata or types: “higher walkable/higher SES,” “higher walkable/lower SES,” “lower walkable/higher SES,” and “lower walkable/lower SES.” This neighborhood selection design has been used successfully in many observational studies of PA [29] among adults [30] and older adults [31, 32] in the US and internationally [33-35]. This approach facilitates the aim of sampling participants from neighborhoods with sufficient within-region variability in walkability and also controls for neighborhood SES by design (SES and walkability are often confounded in many built environment studies). Figure 1 provides an overview of the study design. We planned to sample 120 participants from each of the four SES-by-walkability strata (represented as quadrants in Figure 1) to obtain a relatively balanced sample across neighborhood types. Via blocked randomization (block size: 4), participants were assigned to one of four intervention groups after stratification by neighborhood type to balance the sample across intervention groups and neighborhoods. Participants were blinded to the neighborhood sampling strategy.
Figure 1.
Overview of the planned study design, sampling approach, and random assignment to groups.
2.3. Participant inclusion/exclusion criteria.
Based on a prior power analyses (described below), we estimated that approximately 480 participants would be needed to test hypotheses derived from the study’s primary aims and design. Eligible individuals needed to meet the following criteria: (1) living in one of the eligible neighborhood types, (2) an adult between 18 and 60 years of age, (3) inactive (as screened by International Physical Activity Questionnaire [IPAQ] short form and/or Stanford Usual PA Questionnaire) AND confirmed by baseline accelerometer measures, (4) generally healthy (defined by medical exclusions: no history of heart attack, stroke/mini stroke/TIA, diabetes, multiple sclerosis, lupus, solid organ tumor in the last 5 years, hematologic cancer in the last 2 years, ectatic aorta, atrial fibrillation, COPD, or exercise-induced asthma), (5) with no contraindications to increasing MVPA (assessed by the Physical Activity Readiness Questionnaire for Everyone (PAR-Q+)), (6) not currently pregnant, breast feeding or planning to become pregnant in the next 2 years, (7) not currently participating in PA, diet, or weight loss programs, (8) daily access to a mobile device with text messaging capabilities, (9) an iOS or Android smartphone, or a computer with Windows capabilities and internet access at home, (10) willing to wear an accelerometer on the wrist daily for 1 year, (11) willing to send and receive 2-3 text messages per day for 1 year, (12) not planning to move within the next 2 years, and (13) not planning to travel outside of the region for more than 30 consecutive days.
2.4. Targeted recruitment strategy.
We recruited healthy, insufficiently active adults from neighborhood types and associated BGs. The study was primarily marketed on Facebook, as this platform had sufficient flexibility to demographically and geographically target prospective participants on an ongoing basis. Facebook marketing tools allowed for exposing residents to recruitment ads who lived within a 1-mile radius (smallest area allowed) around the centroid of eligible block groups. We targeted men and women aged 18 to 60 years on Facebook using a variety of ads and images (see Fig. 2 for an example ad). Ads referred adults to the WalkIT Arizona website (www.walkitarizona.org), which provided more information about the trial requirements along with an online Qualtrics-based prescreening survey. The online survey explained the study in brief, requested online informed consent (via yes/no check-box), and assessed inclusion and exclusion criteria. In addition, the online survey asked prospective participants for their home addresses to: (a) determine if a prospective participant resided within an eligible neighborhood quadrant, and (b) ensure only one person per household was recruited. If multiple adults in a household qualified for the study, we recruited only one prioritizing males over females. Eligible adults were asked to join the study and informed they would receive one of four different PA interventions.
Figure 2.
Example Facebook ad for recruiting male participants using demographic and geographic targeting.
2.5. Orientation Visit and Baseline Phase.
Qualifying potential participants were invited to an orientation office visit and asked to provide written informed consent. Participants completed baseline survey measures, a laboratory walking protocol to calibrate the wrist-worn ActiGraph GT9X (ActiGraph, LLC, Pensacola, FL, USA) to each participant, a graded VO2 max test, and then were trained to wear, use and sync their accelerometer and its software. The GT9X is a small (3.5[w] × 3.5[h] × 1[d] cm), lightweight (14 g), triaxial accelerometer with an LCD screen appearing like a watch. The ActiGraph GT9X has extensive validation data available and uses the same internal mechanisms as previously validated generations (e.g., GT3X) [36, 37]. We instructed participants to wear the accelerometer on the preferred wrist during all waking hours (except when swimming) daily. Participants were asked to engage in their normal routines for the next 10 days. To reduce reactivity to the device, accelerometer feedback was masked during this period using a software feature. This baseline phase functioned as a “run-in period” to objectively assess participants’ MVPA eligibility and their ability to use the technology and adhere to the protocol before random assignment. Insufficiently active participants were randomized after a minimum of 9 full days of observation with successful and consistent uploading of data from their accelerometer. All participants earned $20 e-gift card for completing baseline phase.
2.6. Intervention Components
2.6.1. Self-monitoring.
Feedback from the ActiGraph GT9X was unmasked once participants were randomized to an intervention. Participants in all four intervention groups were asked to wear the accelerometer on their wrist daily throughout the 1-year intervention phase. Because classification of minutes as MVPA minutes required processing of the accelerometer data, participants were informed they could upload data (or “sync their device”) anytime to receive a text message that provided feedback for their accumulated MVPA minutes for the day; the watch did not display MVPA minutes due to the need to process these data. Participants were asked to sync their accelerometer at least once daily, nightly, or early the next morning, using ActiGraph’s Android/iOS compatible smartphone app or Windows-compatible desktop application. A sync transmitted data to ActiGraph’s Centrepoint Data Hub cloud system. The cloud system, in turn, notified our research servers of new data to be collected and processed, and then triggered a personalized message sent directly to the participant via text, see details in mHealth Systems, below. The syncing process within this research system did not expose participants to a commercial dashboard or any other alternative intervention. Syncing daily ensured that ASU researchers could remotely monitor each participant’s MVPA min/day, goal achievement, and provide adaptive goals, creating an automated feedback loop (as described below).
2.6.2. mHealth System.
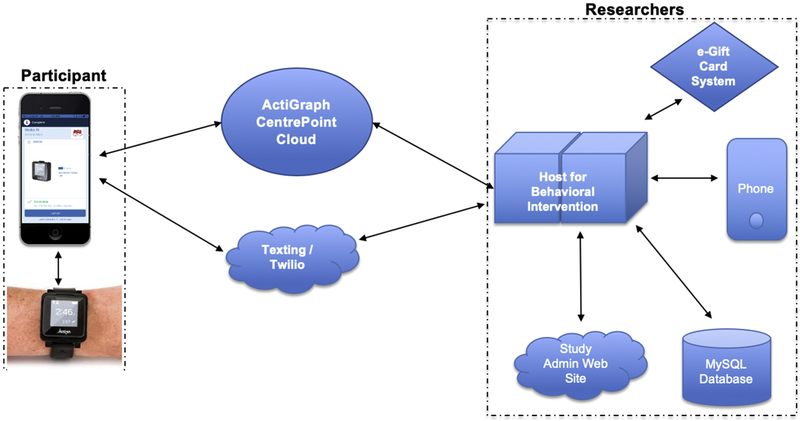
Figure 3 provides a high-level overview of our mHealth system. A study administration website allowed for initializing new participants in the mHealth system. For participants in all four intervention groups, the front end of our mHealth intervention included the accelerometer, the ActiGraph app and/or Windows software, and participants’ native cell phone text message app. The system worked as follows: once a participant synced, data were sent wirelessly from the accelerometer to ActiGraph’s cloud system. Only project researchers had access to the ActiGraph cloud, which informed the project’s host servers via an application programming interface (API) when any new data were received from a participant’s sync. As new participant were received by the cloud system, the project’s host server imported the data and processed them immediately. Transmitted data arrived from participant’s phones or computers to the research servers via ActiGraph's cloud within seconds to minutes after completion of a sync. Our mHealth algorithms determined the appropriate intervention components (e.g., feedback messages, reinforcement, and new exercise goals) to send back to the participant’s phone via text message via Twilio cloud communication backbone. At any time, project staff could push reminders, questions, or prompts to a single participant via text message, and participants could ask questions, report problems, or provide context to their activity; participant texts were forwarded immediately to project staff. MySQL databases logged and timestamped incoming and outgoing data and text messages. e-Gift cards were automatically purchased on demand and in real time from Tango Inc. as needed (more info below).
Figure 3.
Schematic for WalkIT Arizona study mHealth system with automated feedback loop.
2.6.3. Theoretical Grounding.
A behavioral psychology approach,[19, 38-41] incorporating principles of operant shaping, [16, 17] guided the design of intervention components, including antecedent prompts, goals, feedback, and use of financial incentives (i.e., positive reinforcement). Antecedent and positive reinforcement concepts are integrated into many theoretical models and theories [23, 24, 42-45] and have been proposed as unifying principles behind preventive medicine approaches [18]. As participants meet small exercise goals, earn encouraging feedback and incentives, and improve their fitness, they are expected to experience a reduction in perceived barriers and improved efficacy [46]. Although not directly targeted for change in the current study, unplanned social support (e.g., encouragement from friends or family) or other outcomes (e.g., improved mood) may occur and result in improvements to participants’ PA. Thus, operationalized theory-based components offer a high level of “theoretical fidelity,” and the use of technology in real-world contexts offer the opportunity for high “operational fidelity” [47].
2.6.4. Antecedent Prompts.
To encourage PA adoption, all four groups received antecedent prompt messages via their cell phone’s native text message app over the course of 1 year. We used an existing pool of messages from our preliminary studies with adults and developed additional messages to evoke motivation, overcome barriers (e.g., “Don’t like exercising alone? Invite a friend or family member!”), remind about benefits (e.g., “Remember, exercise is heart friendly!”), and provide other advice based on our previous studies and latest research [11]. Prompt messages were selected in a random sequence without replication from the pool of messages and delivered daily to each individual. Because all four groups received the same prompt messages, albeit in a random order, this content can be eliminated as an explanation for any differential changes observed across groups. Prompts helped participants in the less interactive conditions (i.e., static goals and delayed reinforcement groups) stay engaged in the study.
2.6.5. Physical Activity Goals.
Static and adaptive groups were both prescribed PA goals, sent via text message, in the form of minutes/day of MVPA (> 3 METs) and informed that this minimum intensity approximates walking briskly (≥100 steps/min) [48]. Both goal groups were also informed of an ultimate target by the end of the 1-year intervention period of at least 150 min/week of moderate-intensity aerobic PA [49]. Participants could sync their accelerometers any time to see how many MVPA minutes they had accumulated for the current day. Once a participant synced their accelerometer, our mHealth system assessed whether or not the participant met their goal for that day and provided feedback based on the intervention conditions described in sections 2.6.5.1 to 2.6.6.2 below. If a participant had not met their current day’s goal, an acknowledgment of a successful sync along with the current day’s accumulated MVPA minutes and current day’s goal were sent via text message (e.g., “Sync successful, 0 min today, Goal for 4/1 is 30 min). If the participant met the current day’s goal, the next day’s goal was sent along with feedback based on goal type and reinforcement type conditions.
2.6.5.1. Static PA Goals.
A common goal setting approach in PA interventions is to offer a static goal of 30 minutes daily on at least 5 days per week [50], which aligns with current PA guidelines to obtain 150 minutes/week. Participants in the static goal group were asked to accumulate 30 minutes or more of MVPA daily. For example, “Goal for 4/1 is 30 min.”. They were asked to accomplish this stationary goal on 5 or more days per week throughout the 1-year intervention phase. We expected the static goal group to meet fewer goals on average than the adaptive goal group.
2.6.5.2. Adaptive PA Goals.
Each day’s adaptive goal, unlike a static goal, had the potential to adjust upward or downward or stay the same, depending on the history of participant’s performance as measured by the accelerometer over the previous 9 observations. Participants were informed that goals could adjust up, down, or stay the same and because goals adjusted daily, each new goal was valid for that day only. This encouraged participants to sync daily without being reminded.
Adaptive goals were based on a percentile-rank algorithm developed, screened, refined, and tested with steps and MVPA across several preliminary studies [11-13]. The algorithm required: (1) continuous and repeated objective measures of MVPA, (2) ranking the sample window of 9 observations of MVPA from lowest to highest, and (3) calculating a new goal based on a 60th percentile criterion. For example, if the duration of MVPA on each of a participant’s previous 9 daily observations (ranked from lowest to highest) was 0, 0, 0, 0, 5, 7, 10, 14, and 17 mins/day, the 60th percentile would correspond to a goal of 7 minutes and this value would become the 10th (i.e., current or subsequent) day’s goal. Participants were asked to meet or exceed this 60th percentile goal (e.g., “Goal for 4/1 is 7 min.”). Our previous studies showed greater improvements in PA using 60-70th percentiles compared to lower percentiles [12, 13]. As time progressed, the algorithm used a 9-day sliding window that replaced the oldest observation with each new day’s measured activity. Combined with feedback, this algorithm was designed to progressively increase a participant's MVPA duration over time while holding the threshold for moderate intensity at 3 METs or higher. This adaptive goal setting approach relies on continuous remote monitoring of behavior, which required the accelerometer and cloud system described above in “mHealth System.” Participants in our preliminary studies commented that they preferred goals that adapted down or stayed the same when life events overwhelmed their ability to be active. In contrast, static goals (e.g., 30 min/day for static groups) may be beyond baseline abilities, difficult to accomplish during competing circumstances (e.g., childcare, sleep deprivation) or temporary conditions (e.g. illness, work travel), or assumed an unrealistic behavior change process (e.g., static or linear or monotonically increasing goals). The percentile approach may be particularly well-suited for insufficiently active populations. Based on our prior experience, we expected the adaptive group would meet an average of 40% to 70% of their goals over 1 year.
2.6.6. Positive Reinforcement.
Multiple behavior change theories acknowledge it is critical to identify and reinforce improvements to strengthen habits [23, 24,46, 51, 52]. Once their accelerometer was synced, all participants, regardless of group status, received differential feedback texts. Participants who did not meet their daily goals were texted a simple confirmation to acknowledge a sync was done correctly and provided their next goal (e.g., “Sync successful, 4 min today, Goal for 4/1 is 7 min.”). This approach avoided use of discouraging negative feedback. Each time participants in the adaptive group achieved their goal, they were sent positive feedback in the form of encouragement and praise messages (e.g., “You’re on target! Goal met! 10 min today… Goal for 4/1 is 8 min.”). Each time participants in the static goal group achieved their 30 min/day goal, they received a similar message (e.g., “You’re closer to improved health! Goal Met! 33 min today. Goal for 4/1 is 30 min.”).
We developed a message pool of 132 unique praise statements. For both immediate and delayed reinforcement groups, when meeting a goal, a randomly selected praise message from the pool was sent along with total MVPA minutes for that day and their next goal. This feedback was expected to help increase PA, assist with syncing adherence, and encouraged continued interaction with the system over the 1-year intervention period.
2.6.6.1. Immediate Financial Reinforcement.
In addition to praise, participants assigned to the immediate reinforcement group had opportunities to earn points for meeting MVPA goals on each day during the intervention year. Points acted as conditioned reinforcement in this “token economy” and earned points were exchanged for cash equivalent gift cards [53]. In the current study, each point was worth $0.01, and participants progressed through several financial reinforcement stages designed around historic research on schedules of reinforcement, as described below [54-57] to increase and maintain a deficit behavior. Based on behavioral theory, reinforcement stages started with a continuous, fixed magnitude stage (i.e., every met PA goal was reinforced and always earned 100 points) to develop a strong and consistent correlation between goal attainment and a positive consequence. For example, participants assigned to the immediate reinforcement group (regardless of goal group assignment) received feedback that included points earned for meeting a goal and their running point balance (e.g., Cheers, James! Goal met! 63 min yesterday. Reward points = 100! Balance is 400 points. Goal for 7/1 is 35 min). After meeting 24 daily goals, participants progressed to Stage 2, characterized by continuous, variable magnitude (VM) reinforcement (i.e., each PA goal met was reinforced, but points varied from 25 to 250 points). After Stage 2, participants progressed through several types of intermittent reinforcement stages (i.e., variable ratio (VR)) in the order shown in the Table 1. Starting with Stage 3, when a participant met a goal, sometimes this goal attainment was purposefully not reinforced with points to slowly begin increasing the average number of responses required to earn financial reinforcement (praise messages were always sent). Stage 3, for example, was designed as a VR 1.09 meaning that every 1.09 goals met on average over that stage earned some amount of points (i.e., only 22 out of 24 goals met were reinforced [1.09 = 24 successes earned 22 points/financial rewards]). This ratio slowly increased until Stage 6 (i.e., VR 1.50, 24 goals met earned only 16 financial rewards), helping to develop resistance to behavioral extinction through a shaping process based on performance [52, 54]. On days when a participant earned zero points for meeting their goal, they still received praise and a positive message about their health improvements (a longer-term consequence). For example, “Dynamite! Goal met! 72 min today, reward points = zero, but good news -- your health is improving! Balance = 125 points. Goal for 5/23 is 35 min”. Reinforcement stages advanced each time a participant achieved 24 goals, and after Stage 6, for those participants who exceed this stage, the stages regressed back to stage 5, 4 and 3 (repeating stage 3 until the end of the intervention phase) to ensure a sufficiently rich schedule of intermittent financial reinforcement throughout the year-long intervention. Participants did not earn or lose points/financial reinforcement for missing a goal, but could not earn points after the goal expired (goals expired at noon on the next day, which allowed participants to sync and receive credit in the morning for a previous day).
Table 1.
Overview of reinforcement stage progression for the immediate reinforcement groups.
| Reinforcement Stage |
Stage Description |
Reinforcement Schedule Type and Ratio* |
Probability of Reinforcement per Met Goal |
Range of Amounts Earned per Met Goal |
Total Possible Amount Earned per Stage |
|
|---|---|---|---|---|---|---|
| Baseline | None | -- | -- | -- | -- | |
| Need to meet 24 goals to advance stages | Stage 1 | Continuous, Fixed Magnitude | CRF-FM | 100.0% | $1.00 | $24.00 |
| Stage 2 | Continuous, Variable Magnitude | CRF-VM | 100.0% | $0.25-2.50 | $24.00 | |
| Stage 3 | Variable Ratio, Variable Magnitude | VR 1.09 | 91.7% | $0.50-2.50 | $24.00 | |
| Stage 4 | Variable Ratio, Variable Magnitude | VR 1.20 | 83.3% | $0.75-2.50 | $24.00 | |
| Stage 5 | Variable Ratio, Vriable Magnitude | VR 1.33 | 75.0% | $0.75-3.50 | $24.00 | |
| Stage 6 | Variable Ratio, Variable Magnitude | VR 1.50 | 66.7% | $0.75-5.00 | $24.00 |
CRF: Continuous reinforcement; FM: Fixed magnitude; VM: Variable magnitude
Immediate reinforcement participants (regardless of goal group) could meet up to 100% of their goals ($365, $1 per goal over 365 days), but much more probable based on our previous research [11, 12] is that the majority participants will earn as few as 40% and much as 73% of their goals on average (40% to 73% × 365 possible days = 146 to 265 goals met in total) over 1 year, which equals about $146 to $265 in incentives. Each time a participant accumulated at least 500 points ($5, the minimum gift card denomination at many companies), points were instantaneously exchanged for e-gift cards from Tango Inc. using the participants selection from a catalog of 12 available retailers (e.g., Amazon, Target, Sephora, Home Depot, Starbucks, etc.), and e-gift cards were sent immediately via email using our automated mHealth system that was online 24 hours/day, 365 days per year.
2.6.6.2. Delayed Reinforcement.
The delayed reinforcement group did not receive points, but rather earned an escalating amount of financial incentives every 60 days (i.e., $15 in month 2 (M2), $30 in M4, $50 in M6, $75 in M8, and $95 in M10) for participating and syncing their accelerometer. Delayed reinforcement group participants had the opportunity to earn $265 total during the intervention phase, which is equal to the maximum amount the immediate reinforcement group was expected to earn on average during the intervention phase. The same catalog of incentives and always-on mHealth system previously described was used to send e-gift cards to participants in the delayed reinforcement group, but only after syncing and on a pre-determined interval schedule.
2.7. Observation Period for Behavioral Maintenance (months 13-24)
Based on hypotheses from ecological models for PA,[23, 24, 58] we anticipated that individuals living in higher walkable neighborhood types would show significantly higher levels of MVPA at 18 and 24 months (i.e., maintenance) than individuals living in lower walkable types, controlling by design for neighborhood-level SES. At the end of 1 year, we invited participants to the office to complete 12-month measures (their second visit), return the accelerometer, and reminded them of the upcoming 1-year maintenance phase. Participants in each intervention group were encouraged to continue their MVPA over the next year. We reassessed MVPA at 18 months and 24 months to examine whether PA changes were sustained differentially across neighborhood types and treatment groups (main effects and interactions). At 18 and 24 months, we sent participants an accelerometer by mail, asked them to wear it for up to 10 days to capture at least 4 valid days of wear, and had them return it by mail in a prepaid padded envelope. Published research [30, 59] led us to anticipate that ~30% of participants would need to re-wear the accelerometer during each of the assessment waves because they would not have at least 4 days of valid wear time. During the maintenance phase, we masked the accelerometer to limit reactivity. In addition to a $20 e-gift card at baseline, participants could earn $25, $20, and $25 cash equivalent e-gift cards for completing 12-, 18- and 24-month measures, respectively, to promote participation in measurement activities for a planned total of $355 while in the study.
2.8. Primary Outcomes
2.8.1. Accelerometer and MVPA Bouts.
The primary outcome, accelerometer-derived “bouts” of MVPA min/day, where bouts are defined as sustained MVPA for at least 3 minutes or more (i.e., the minimum number of minutes needed to identify and measure continuous walking from other activities using the wrist placement), was measured with the ActiGraph GT9X. Vector magnitude (VM) counts from the wrist using epochs of 1 minute were used for estimating MVPA and wear time and non-wear time for the mHealth system and main outcome analyses. Relatedly, we used the recommended defaults of the validated Choi algorithm to distinguish between wear and non-wear times, with at least 90-minutes of consecutive zero or non-zero counts needed to define non-wear or wear, respectively, with an allowance for up to 2 minutes of nonzero counts related to artifactual movement [60, 61]. Accelerometer wear time will be used as a covariate in all analyses. Days with at least 6, 8, and 10 valid wearing hours will be examined in analyses because guidelines are lacking for how long participants must wear an accelerometer each day for a year.
2.8.2. Defining MVPA and walking cut-point protocol.
To calibrate the accelerometer for wrist wear, each participant completed a walking protocol to set a unique minimum VM threshold, or ‘cut-point’ for defining a minute of MVPA during their baseline office visit. The walking protocol consisted of a staged treadmill test while wearing both the accelerometer on the wrist and an indirect calorimetry apparatus to collect breath-by-breath VO2 data (Oxycon mobile, CareFusion Systems, Yorba Linda, CA). The protocol was specifically designed to capture walking at moderate intensity or greater (≥3.0 METs) and was designed as 5-minute period of standing rest followed by 3 walking stages lasting 6 minutes each. The protocol started at 2.0 mph and, after 6 minutes, speed was increased to 3.0 for 6 minutes followed by 4.0 mph for 6 minutes, with a 0% grade maintained throughout. Individual abilities of each participant were considered; in some cases, the fourth stage was not performed at 4.0 mph, but at the highest walking speed the participant could maintain. Similar to other cut-point protocols [62, 63], to allow for steady-state data to be used, only gas exchange data from the final 3 minutes of each stage was used and a quadradic regression model estimated each individual’s personalized VM cut-point for at least moderate-intensity ambulation (VO2 value greater than 3.0 METs).
Because of the study’s real-time nature and need to classify any every minute as MVPA or not after a participant synced daily (or more frequently), both the personalized VM cut-point had to be met or surpassed and the step count had to be >30 steps for any 1-minute epoch. The accelerometer’s built-in step count algorithm was used to reduce over-classification of movement as MVPA due to non-ambulatory activities (e.g., VM thresholds exceeded due to arm movement when standing or sitting). We examined new data sent via participant’s sync using a 5-minute moving window across the stream of synced real-time data (lengths of new data streams varied based on the time since the participant’s last sync [e.g. 1440 minutes for 24-hour period]). The onset of a MVPA bout occurred once these VM and step criteria lasted at least 3 non-contiguous minutes out of a moving 5-minute window, and the offset of a bout occurred once these MVPA criteria were not met for 3 contiguous minutes of a moving of 5-minute window. The minimum detectable MVPA bout by this approach was 3 minutes.
2.9. Secondary outcomes
2.9.1. IPAQ.
The International Physical Activity Questionnaire (IPAQ) long form (parts 2, 4, and 5) were used to measure self-reported PA over the last 7 days. Participants reported frequency, duration, and intensity of leisure and transportation-related physical activities and time spent sitting. Reliability and validity when compared to accelerometers is similar to other self-report measures of PA [64]. Domain-specific PA (e.g., transportation, recreation activities) and sedentary time in min/day were assessed to evaluate specific changes in PA domains [65] from baseline to months 12, 18, and 24.
2.9.2. NPAQ.
The Neighborhood Physical Activity Questionnaire (NPAQ) was used to assess environment-specific self-reported PA in a typical week. Participants reported usual weekly frequency and duration of recreational and transportation-related walking and bicycling inside and outside of their home neighborhoods[66]. The NPAQ, has been shown to reliably assess setting-specific PA in adults [66], was used to evaluate changes in PA (MET min/week) inside and outside participants’ home neighborhoods from baseline to 12-, 18-, and 24-months.
2.9.3. VO2 Max testing.
Maximum aerobic capacity (VO2peak) was estimated using a continuous treadmill ramp protocol (modified Balke protocol) [67]. This validated, well-tolerated graded exercise test maintained a constant speed (3.3 and 3.0 mph for men and women, respectively), and began at 2% grade. Workload was increased by raising the grade by 1% every minute thereafter until termination of the test. The protocol was modified based on subject abilities if the basal walking speeds (3.3 mph for men and 3.0 mph for women) were not sustainable by the participant. Peak VO2 was assessed at baseline and reassessed at 12 months. A VO2peak assessment was given to all individuals except those who declined. Borg rating of perceived exertion (RPE)[68] and heart rate was assessed each minute. VO2peak was assessed directly using breath-by-breath VO2 data supplied by the Oxycon. At baseline, this protocol occurred after the walking protocol described above and a period of rest.
2.9.4. Anthropometric measures.
Body Mass Index (BMI): A research assistant objectively measured height and weight by stadiometer and digital scale (in light clothing and no shoes), respectively. Each participant was measured a minimum of three times, until sufficient agreement between measurements was achieved, and the average calculated to reduce random error. BMI was computed using the following formula: weight (kg) divided by height squared (m2) at baseline and 12-months.
2.9.5. Psychosocial measures.
Several validated [69] psychosocial variables that are among the most consistent correlates of leisure PA were measured. These included: exercise self-efficacy [70], family and peer support for exercise [71], pros/cons of exercise [72], and enjoyment of physical activity [69]. Participants’ perceived benefits of and barriers to physical activity [73, 74] were also assessed. These measures were assessed at baseline, 12, 18, and 24 months.
2.9.6. Satisfaction.
At months 12 and 24, participants were asked to rate how motivating or burdensome specific study components felt to them and what their overall satisfaction was with the study. Participants were asked about their personal experiences with intervention components and their recommendations for improvement. This information will be helpful for understanding how participants experienced the study [75].
2.9.7. Adverse events.
We asked participants about any adverse events during the study and at the end of the adoption and maintenance phases (months 12 and 24, respectively) for data safety and IRB reports.
2.9.8. Individual-level GIS variables.
In addition to BG-specific walkability described above for screening, recruitment, and enrollment purposes, we also calculated an ‘individual-level’ walkability index and GIS variables around the home and worksite (for those adults who worked outside of their home). At the baseline visit, participants provided their home residence addresses, and when applicable, their worksite addresses or nearest cross-streets. Locations were geocoded using ArcGIS 10.5 (ESRI, Redlands, CA) with US Census Tigerline address feature. Each geocoded address was used to geoprocess spatial datasets and create ‘individual-level’ GIS variables related to transportation and recreational walking within 500- and 1000-meter street-networks from origin. Using the ‘individual-level’ buffer area, the following components were derived: residential density, land use mix, street network connectivity, and public transit access.
2.9. Covariates and other measures
2.9.1. Demographics and covariates.
Adults reported their gender (male or female), date of birth, race/ethnicity, education, number of motor vehicles/adults in household, marital status, number of adults and children in household, type of residence (single family, multifamily), and years at current address.
2.9.2. Self-reported Neighborhood Features.
Perceived urban form and neighborhood characteristics were measured at baseline and at any measurement wave that participants reported moving residences using the Neighborhood Environment Walkability Scale (NEWS) [76]. The NEWS has eight sections: residential density, proximity to non-residential land uses, access to services, street connectivity, walking and cycling facilities, aesthetics, traffic safety, and crime safety. The NEWS has shown good to excellent test-retest reliability and is able to accurately discriminate high and low walkable communities [77, 78]. NEWS scores can be used to explore the interaction between perceptions of walkability and the four individual-level interventions on changes to either objectively measured or self-reported PA (e.g. IPAQ or NPAQ).
2.9.3. Crime Safety.
Crime and fear of crime are often cited as contributors to low PA across the lifespan, but the data are surprisingly inconsistent [79]. A refined measure of crime and responses to crime developed from another study was adopted for the current study [79]. The survey assessed personal experiences with personal- and property-crimes, cognitive and emotional responses to crime, and behavioral responses to crime that affect PA within one’s neighborhood. Test-retest reliability for most scales was excellent or good. Overlapping items on NEWS crime subscale were omitted and measured within the crime safety survey. This crime safety survey was administered at baseline and months 12 and 24 in the current study. These variables may be covariates or moderators in exploratory analyses.
2.9.4. Delay Discount Rate.
Participants completed the 27-item Monetary Choice Questionnaire (MCQ) [80] at baseline, and 12 and 24 months to assess tolerance for reward delays. For each of the items, the participant was asked to choose between a hypothetical smaller, more immediate vs. larger, more delayed monetary reward. Scoring determined the tolerance for delayed rewards by locating the participant on referenced discounting curves: steeper curves indicated higher discounting rates and lower tolerance for reward delays. This measure can be used as a covariate or to explore the moderating effect of participants’ discounting rates on their randomly assigned goal-type or incentive-type group.
2.9.5. Sleep Quality.
The Pittsburgh Sleep Quality Index (PSQI) consists of 9 questions designed to assess sleep quality and disturbances in adults through seven components: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction. The PSQI instrument has demonstrated acceptable measures of validity and test-retest reliability [81]. Participants completed the survey at baseline, and 6, 12, 18, and 24 months. PSQI variables may be used as covariates, moderators, or outcomes in exploratory analyses.
2.9.6. Weather.
Because weather could be an important daily influence on MVPA, we obtained and recorded basic weather variables (i.e., daily high temperature, low temperature, and precipitation) from the National Oceanic and Atmospheric Administration during data collection. These data can be used as time-varying covariates to examine the relation of weather to MVPA.
3. STATISTICAL ANALYSES
3.1. Sample Size and Power.
To estimate the sample size required to address our four primary aims, we assumed intervention main effects (i.e., Static vs. Adaptive goals, and Immediate vs. Delayed financial reinforcement) of increases in MVPA of 2.1 min/day (derived from Conn et al. [4]) from baseline to post-intervention, power of .80, and alpha of .05). In simulations conducted using SAS PROC IML and PROC MIXED [82], the estimated required complete-case sample size was N = 320 participants. This represents a conservative estimate — due to computational limitations, simulations were based on only 90 repeated observations of MVPA as opposed to 365 daily observations expected by 12 months. Adjusting for an assumed BG-level intraclass correlation (ICC) of .01 for MVPA, an initial average BG size of 5 participants, and a 30% rate of participant loss (i.e., drop-outs and movers) by 24 months, the estimated required baseline sample size was N = 471 participants. Because our goal was to have balancedcell sizes across sampling and randomization stages, our target baseline sample size was a minimum of N = 480. Simulations indicated that this sample size should afford .80 power to detect interaction effects corresponding to a 4.2-min/day “difference in differences” in MVPA at 12 months—e.g., a 4.2-min/day difference between changes in Static vs. Adaptive goals at 12 months across low vs. high walkable neighborhood groups.
3.2. Data Analytic Plan.
We will first examine univariate and bivariate statistics to evaluate distributional properties of outcome measures and to identify potentially relevant confounders and covariates. Next, we will evaluate the degree of geographic (block group-level) clustering in outcome values using intraclass correlation coefficients (ICCs). Should ICCs be non-trivial (i.e., <.01), a random block group-level intercept term will be included in models corresponding to study aims (described below). We will also evaluate psychometric properties (e.g., internal consistency) of self-report multi-item measures of psychosocial variables.
We will test hypotheses using a generalized linear mixed model approach, with repeated assessments of accelerometer-assessed MVPA treated as being nested within persons, and, if warranted by block group-level ICCs, persons will be treated as nested within block groups. To minimize collinearity among interaction terms and constituent linear effects, we will use effect coded indicators (i.e., −1/1) as opposed to dummy coded (i.e., 0/1) indicators for dichotomous predictors. In all models, we will adjust for (a) covariates identified in preliminary analyses; (b) daily accelerometer wear time; (c) linear, quadratic, and cyclical (weekly, monthly) time effects; and (d) autocorrelated residuals. Choice of link function (e.g., identity, natural log) and error distribution (e.g., normal, negative binomial) will be driven by distributional characteristics of the outcome and tests of relative model fit. All analyses will be conducted using mixed model packages (e.g., lme4, nlme, glmmTMB) in R 3.5.2.
To address hypotheses regarding intervention effects at 12, 18, and 24 months, we will model the Intervention effect (either Static vs. Adaptive goals or Delayed vs. Immediate reinforcement) on changes to MVPA min/day from baseline to 12 (or 18 or 24) months using Intervention × Phase (e.g., Adaptive vs. Static × Baseline vs. Intervention) interaction terms. Significant interactions will be examined to characterize conditional effects (i.e., simple slopes) for Phase within intervention conditions. We hypothesize that the Phase effect will be more strongly positive for those in the Adaptive goals condition than for those in the Static goal condition and more strongly positive for those in the Immediate reinforcement condition than for those in the Delayed reinforcement condition.
We will then examine the interaction between a contrast comparing the Adaptive goal + Immediate reinforcement arm to the other three arms and Phase (Baseline vs. 12, 18, or 24 months). This interaction will capture differential baseline to post-intervention change in MVPA. A significant interaction will be probed to characterize conditional effects (i.e., simple slopes) of Phase for Adaptive goals + Immediate reinforcement arm and the other three arms combined. We hypothesize that the Phase effect will be more strongly positive for those in the Adaptive goal + Immediate reinforcement arm than for those in the other three arms.
Differences in intervention effects (e.g., Goal type × Phase effects) on MVPA adoption (by 12 months) and maintenance (at 18 and 24 months) across levels of neighborhood walkability will be modeled using Intervention × Phase × Walkability (individual-level walkability score) interaction terms. Here, significant interactions will be probed by estimating conditional effects (simple slopes) of Phase within Intervention condition (e.g., Static vs. Adaptive) at low (e.g., sample 25th percentile), average (sample mean), and high (e.g., sample 75th percentile) levels of walkability using procedures described by Aiken and West [83] and Preacher, Curran, and Bauer [84]. We hypothesize that the Phase effect will be most strongly positive for those in High Walkable (vs. Low Walkable) areas assigned to the Adaptive (vs. Static) goals condition and for those in High Walkable (vs. Low Walkable) areas assigned to the Immediate (vs. Delayed) reinforcement condition. Parallel models will be estimated with terms comparing the Adaptive goals + Immediate reinforcement arm to the other three arms in place of the Goal type and Reinforcement type main and interaction effects.
The analyses described above will be repeated, with some modifications, using self-reported walking for transportation and walking for recreation as outcomes, in place of accelerometer-measured MVPA. Models of self-report PA will not include adjustments for temporal trends or cycles or for accelerometer wear time. Also, these models will not include specification of temporal autocorrelation among residuals.
3.3. Missing data.
Given the potential for nonignorable missingness in our outcome data, we will explore various strategies for mitigating potential biases in estimates and loss of statistical power due to missing data, including standard intent-to-treat approaches, FIML-estimated models, models with auxiliary variables, and analysis of multiply-imputed data sets, to be followed by sensitivity analyses assessing robustness of conclusions drawn from each approach.
4. RESULTS
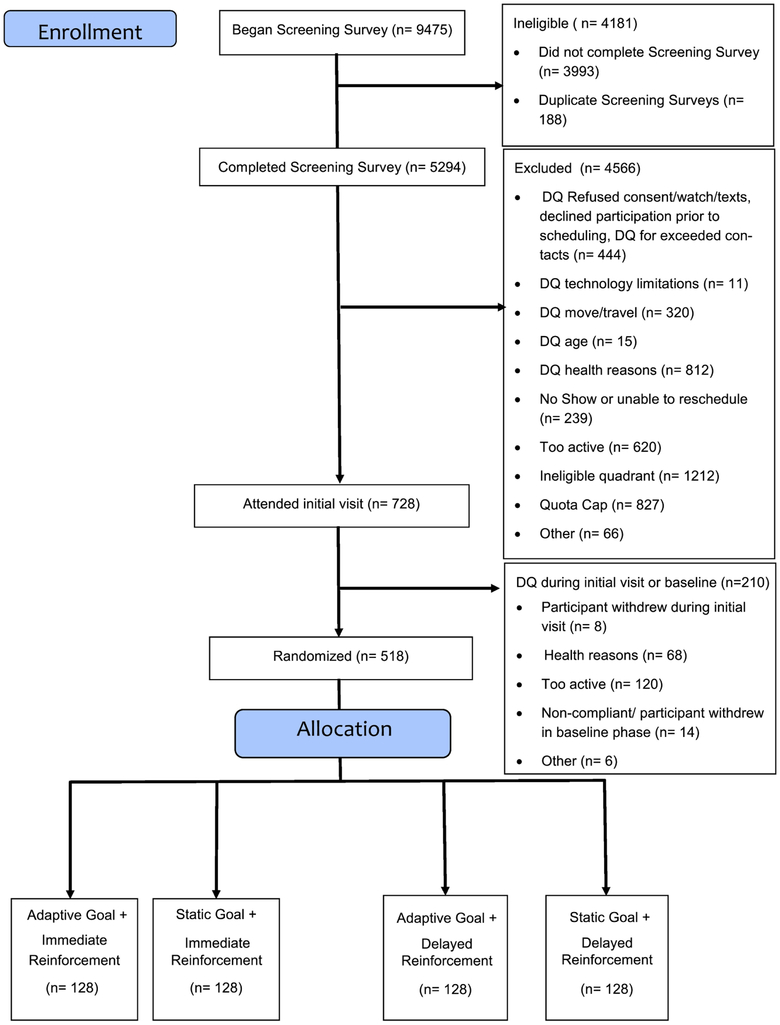
The CONSORT diagram in Figure 4 shows that 9,475 pre-screening surveys were started by individuals and 5,294 (55.9%) surveys were completed. Of these completed pre-screening surveys, 4,566 (86.2%) individuals were disqualified after review by study staff, refused to participate after being contacted, or could not be contacted. Main reasons for disqualification included living outside of an eligible neighborhood type (i.e., 6th decile of SES or 5th and 6th deciles of walkability), reported meeting PA guidelines, reported one of the disqualifying health reasons, or planned to move outside of the study area within next 2 years. A total of 827 adults were disqualified because we had already met a sampling quota for a specific neighborhood type. We invited eligible adults to an initial office visit of which 728 attended. Of those who attended, an additional 210 (4.6% of those pre-screened) were disqualified due to health reasons (e.g. hypertensive, mask anxiety), non-compliance with accelerometer wear protocols, or failing to complete baseline survey / walking protocol measures. During the 10-day baseline phase, more than half of the 210 adults were sufficiently active (i.e., meeting physical activity guidelines) as measured with a blinded ActiGraph GT9X. These individuals were also disqualified before randomization. Of the 728 who attended the baseline visit, 512 (11.2% of those prescreened) were randomized to one of four intervention arms.
Figure 4.
CONSORT flow diagram reflecting participant enrollment and allocation efforts.
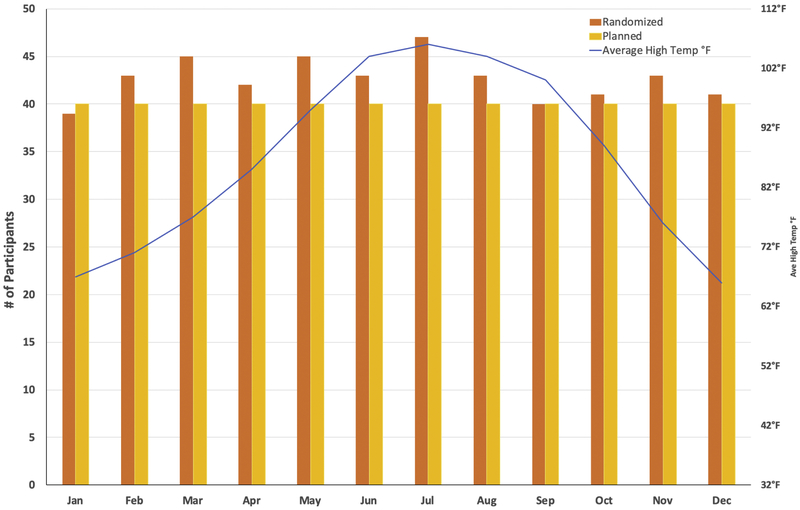
Figure 5 shows at least 40 participants were randomized in each calendar month, except January (39 randomized), generally achieving the plan to balance the sample across months. The minimum number of participants randomized by month was met even during months with the hottest average high temperatures (>100° Fahrenheit).
Figure 5.
Results of balancing participant recruitment and randomization by calendar month.
Table 2 shows personal characteristics of the 512 participants by SES and GIS-measured walkability as defined by the location of their home. The number of participants ranged from 136 in the ‘higher walkable / higher income’ and ‘lower walkable / higher income’ types to a 108 from ‘lower walkable / lower income’ type. As expected, participants’ reported household income was higher in the two ‘higher income’ neighborhood types, although median educational attainment was similar across all four neighborhood types. Although the ratio of women to men and average age was similar across neighborhood types, fewer participants from the two ‘lower-income’ neighborhood types reported children in the home. A greater proportion of adults from lower-income neighborhoods identified as non-White and Hispanic origin. Participants from the ‘lower walkable / higher income’ neighborhood type reported the greatest median household income, greatest proportion of adults identifying as non-Hispanic White, greatest proportion with children in the home, lived the farthest from work, and had the lowest smoking rates. Participants from the ‘higher walkable / lower income’ neighborhood reported the lowest median household income, lowest proportion identified as married or cohabiting and with children in the home, highest proportion identifying as non-White and Hispanic origin, highest average BMI and proportion of currently smoking,
Table 2.
Participant characteristics by sampled neighborhood types as defined by SES and GIS-measured walkability.
| Total (N=512) |
Higher Walk / Higher Income (n=136) |
Higher Walk / Lower Income (n=132) |
Lower Walk / Higher Income (n=136) |
Lower Walk / Lower Income (n=108) |
|
|---|---|---|---|---|---|
| Age, Mean (SD) | 45.5 (9.1) | 46.9 (8.9) | 44.3 (10.0) | 45.7 (8.1) | 44.7 (9.5) |
| BMI, Mean (SD) | 33.9 (7.3) | 33.6 (6.5) | 34.9 (8.0) | 33.2 (7.1) | 33.8 (7.4) |
| Female, % | 64.3 | 63.2 | 65.2 | 64.7 | 64.8 |
| Race and Ethnicitya | |||||
| Caucasian or white, % | 84.0 | 85.2 | 78.0 | 87.5 | 80.6 |
| African American or Black, % | 6.3 | 2.9 | 7.6 | 4.4 | 10.2 |
| American Indian or | |||||
| Alaskan Native, % | 2.7 | 2.2 | 5.3 | 0.7 | 2.8 |
| Asian, % | 2.3 | 2.9 | 1.5 | 2.9 | 1.9 |
| Native Hawaiian or other | |||||
| Pacific Islander, % | 1.4 | 0.7 | 0.0 | 1.5 | 3.7 |
| Prefer not to answer, % | 6.3 | 7.4 | 9.1 | 4.4 | 3.7 |
| Hispanic or Latino, % | 18.8 | 18.4 | 25.0 | 14.0 | 17.6 |
| Current tobacco smoker, % | 5.0 | 5.9 | 7.4 | 1.5 | 5.5 |
| Current E-smoker, % | 2.0 | 1.5 | 3.1 | 1.4 | 1.9 |
| Married or living with partner, % | 67.5 | 77.2 | 46.2 | 83.8 | 61.1 |
| Employed, full-time, % | 76.2 | 76.5 | 80.3 | 74.3 | 73.1 |
| Distance from home to work (meters), Median | 16,316 | 15,213 | 14,935 | 21,160 | 15,607 |
| Has 1 or more children in household, % | 49.1 | 50.0 | 35.7 | 66.2 | 42.6 |
| # Children in household, Mean (SD) | 1.0 (1.2) | .9 (1.1) | .7 (1.2) | 1.4 (1.3) | .8 (1.2) |
| Household income, medianb | $60,000-79,999 | $80,000-99,999 | $40,000-59,999 | $100,000-119,999 | $60,000-79,999 |
| Education, median | College graduate | College graduate | College graduate | College graduate | College graduate |
Race/ethnicity cumulative is > 100%. Participants were allowed to select "all that apply".
Median income category for Lower Walkable / Higher Income was 5.5. Rounded up to category 6 income for table.
Table 3 shows participant characteristics by group assignment. The block randomization process resulted in a balanced number of participants across groups.
Table 3.
Participant characteristics by randomized group allocation.
| Total (N=512) |
Adaptive Goal + Immediate Reward (n=128) |
Static Goal + Immediate Reward (n=128) |
Adaptive Goal + Delayed Reward (n=128) |
Static Goal+ Delayed Reward (n=128) |
|
|---|---|---|---|---|---|
| Age, Mean (SD) | 45.5 (9.1) | 45.6 (9.5) | 46.0 (8.9) | 46.7 (8.6) | 43.5 (9.3) |
| BMI, Mean (SD) | 33.9 (7.3) | 33.7 (7.3) | 33.8 (7.3) | 33.6 (7.0) | 34.5 (7.6) |
| Female, % | 64.3 | 64.1 | 62.5 | 63.3 | 68.0 |
| Race and Ethnicitya | |||||
| Caucasian or white, % | 84.0 | 84.4 | 82.8 | 82.0 | 82.8 |
| African American or Black, % | 6.3 | 3.9 | 7.0 | 7.0 | 6.3 |
| American Indian or Alaskan Native, % | 2.7 | 3.1 | 2.3 | 1.6 | 3.9 |
| Asian, % | 2.3 | 3.1 | 2.3 | 2.3 | 1.6 |
| Native Hawaiian or other Pacific Islander, % | 1.4 | 2.3 | 0.8 | 1.6 | 0.8 |
| Prefer not to answer, % | 6.3 | 3.9 | 6.3 | 7.8 | 7.0 |
| Hispanic or Latino, % | 18.8 | 17.2 | 20.3 | 18.8 | 18.8 |
| Current Tobacco Smoker, % | 5.0 | 2.4 | 7.8 | 3.9 | 6.3 |
| Current E-smoker, % | 2.0 | 1.6 | 2.4 | 0.8 | 3.2 |
| Married or living with partner, % | 67.5 | 64.1 | 66.4 | 72.7 | 67.2 |
| Employed, full-time, % | 76.2 | 76.6 | 75.8 | 73.4 | 78.9 |
| Distance from home to work (meters), Median | 16,316 | 15,368 | 16,718 | 15,597 | 16,926 |
| Has 1 or more children in household, % | 49.1 | 47.7 | 47.5 | 50.0 | 50.8 |
| # Children in household, Mean (SD) | 1.0 (1.2) | 1.0 (1.2) | 1.0 (1.3) | 1.0 (1.3) | 1.0 (1.1) |
| Household income, median | $60,000-79,999 | $80,000-99,999 | $60,000-79,999 | $60,000-79,999 | $80,000-99,999 |
| Education, median | College graduate | College graduate | College graduate | College graduate | College graduate |
Race/ethnicity cumulative is > 100%. Participants were allowed to select "all that apply".
4. DISCUSSION
The WalkIT Arizona study goes beyond investigating an individual-level intervention for adoption and maintenance of PA by testing four MVPA interventions in the context of high and low walkable neighborhoods. Thus, this project becomes more significant as accomplishment of the aims will provide critical information on multiple levels: 1) effect of an mHealth intervention with goal adaptation and immediate reinforcement on MVPA behavior, 2) interaction of individual-level interventions with environmental contexts, and 3) study of adoption and maintenance of PA. Each area addresses a major gap in the current behavior change science for PA.
mHealth [8] and theoretical advances[7, 9] have made adaptive interventions for MVPA feasible for individuals [85]. As noted by Collins et al, adaptive interventions have potential to reduce treatment mismatch, increase adherence, enhance potency, and truly personalize behavioral medicine [7]. Adaptive interventions may significantly enhance implementation of behavior change principles theoretically responsible for short- and long-term change. For example, mHealth interventions can improve goal setting by assessing progress much more frequently and quickly providing new, slightly more challenging goals to increase PA or stepping down goals when life overwhelms one’s ability to be active. Frequent monitoring and adjustments allow for more personalized behavior change interventions and, perhaps, greater engagement with the intervention components. Such mHealth technologies also allow for more precise and immediate use of feedback and financial contingencies by reinforcing behaviors in near-real time and while individuals interact with the free-living world. When combined, the fidelity and potency of adaptive goals and near-immediate reinforcement components approach the conceptual ideals for shaping behavior as envisioned by theoreticians [10, 23, 86]. Few behavioral interventions have approached lifestyle-change engineering from this theoretical perspective [6, 87].
Several corporate and government programs (e.g., Medicaid) [88, 89] and prevention programs (e.g., the Diabetes Prevention Program [i.e., DPP Dollars])[90] pay individuals small amounts for chronic disease–related change. However, the use of financial reinforcement to motivate behavior change is controversial. Although “crowding out” of intrinsic motivation is an often-cited concern about the use of financial reinforcement for increasing deficit behaviors, Promberger and Martau’s systematic review and meta-analysis examining the empirical literatures from both psychology and economics does not support this concern [91]. As concluded by these authors, in the psychology literature, higher levels of baseline behaviors imply higher levels of intrinsic motivation and lower levels of baseline behaviors imply lower levels of intrinsic motivation. By definition, at baseline, insufficiently active and sedentary adults have lower levels of PA and correspondingly lower levels of intrinsic motivation (otherwise activity levels would be higher, even under difficult circumstances). From the economics literature, the authors concluded that behaviors more frequently align with existing incentives and not in the opposite direction of that expected by incentive alignment or even with self-interest [91]. Thus, concerns about “crowding out” are unwarranted while encouraging MVPA adoption. As Farooqui et al. noted, although certain theoreticians raise concerns about the use of financial reinforcement for motivation, the empirical evidence to support this concern does not exist for PA [92].
More empirical questions could be asked about how to best use financial incentives for both adoption and maintenance of PA. Currently, incentive strategies vary widely and mainly include “loss framed” messaging and large deposit contracts in which participants earn back their initial deposits (i.e., negative reinforcement approach) [93, 94]. Small, frequent, and daily reinforcement for meeting PA goals are becoming more common [12, 20, 93, 94]. The current study, and especially the immediate reinforcement arm, was guided by these studies and basic research on the use of schedules of reinforcement [54]. In the first several months, financial reinforcement in the immediate reinforcement condition was contingent, continuous, and predicable for meeting MVPA goals (i.e., continuous fixed magnitude reinforcement schedule), and afterwards the reinforcement experience became more unpredictable as participants became more successful and progressed through reinforcement stages. This approach slowly introduced game-like features to the immediate reinforcement arm, but more importantly was expected to promote maintenance of MVPA through the use of variable magnitude and intermittent reinforcement schedules. Thus, the immediate reinforcement arm was designed to address commonly seen limitations in the use of financial reinforcement. As noted by previous researchers, few studies using financial reinforcement have been designed to promote both behavioral adaption and maintenance by slowing thinning out reinforcement over time via intermittent schedules to build resistance to behavioral extinction [11, 95, 96]. The current study and its factorial design will allow for testing the independent and joint effects of adaptive goals and immediate reinforcement to answer important questions about which combination of components are more active and potent within the current interventions for MVPA.
This study also offers the ability to test research questions about multi-level effects such as the joint contributions of individual-level interventions and free-living human contexts for PA. Built environments and policies are expected to potentiate or attenuate effects of individual-level behavior change interventions for physical activity. Randomizing individuals to living in specific neighborhoods, or developing interventions that enable a person to rapidly respond to specific activity/inactivity-promoting environments, however, is extremely challenging, and outside of the current reach of technology. Moreover, few researchers have yet to examine how neighborhood environments interact with interventions that target individuals, and the results have been mixed. For example, Kerr et al. reported that overweight adults who completed web-based PA and dietary behavior interventions and lived in lower walkable neighborhoods benefited from the individual-level intervention more than those in higher walkable neighborhoods,[26] counter to hypotheses that high walkability should potentiate individual-level PA intervention effects. None of the studies to date sampled participants from neighborhoods known to differ in walkability and then prospectively enrolled them into an individual-level intervention. Results of the current study will provide evidence for some of the central research questions of ecological models.
Only a small percentage (<8%) of US adults meet MVPA guidelines as measured objectively [1], with little change in population levels over the past two decades.[2, 3] To dramatically increase population-level PA to meet national guidelines may require: a) developing more potent behavior change interventions that harness technologies and personalization to adapt uniquely to individuals, b) changing our built environments to support MVPA, and (c) combining these two approaches. While the current ongoing study does not alter the built environment to support PA, it does personalize interventions and move in the direction of being able to answer to what extent individual-level interventions function differently in activity-supportive and unsupportive environments – an important gap in the PA literature.
Acknowledgement:
The authors kindly acknowledge support of Ms. Emily Foreman and Ms. Alison Cantley along with many undergraduate and graduate research assistants helping with data collection.
Funding:
This work was supported by the National Cancer Institute at the National Institutes of Health [R01CA198915]. The funding agency was not involved in any aspect of this study or manuscript.
Abbreviations
- PA
physical activity
- MVPA
Moderate-to-vigorous physical activity
- Min/day
minutes per day
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- [1].Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M, Physical activity in the United States measured by accelerometer, Med Sci Sports Exerc 40(1) (2008) 181–8. [DOI] [PubMed] [Google Scholar]
- [2].Brownson RC, Boehmer TK, Luke DA, Declining rates of physical activity in the United States: what are the contributors?, Annual review of public health 26(1) (2005) 421–43. [DOI] [PubMed] [Google Scholar]
- [3].C. Centers for Disease, Prevention, Trends in leisure-time physical inactivity by age, sex, and race/ethnicity--United States, 1994-2004, MMWR Morb.Mortal.Wkly.Rep 54(39) (2005) 991–994. [PubMed] [Google Scholar]
- [4].Conn VS, Hafdahl AR, Mehr DR, Interventions to increase physical activity among healthy adults: meta-analysis of outcomes, Am J Public Health 101(4) (2011) 751–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Riley WT, Serrano KJ, Nilsen W, Atienza AA, Mobile and Wireless Technologies in Health Behavior and the Potential for Intensively Adaptive Interventions, Curr Opin Psychol 5 (2015) 67–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Riley WT, Rivera DE, Atienza AA, Nilsen W, Allison SM, Mermelstein R, Health behavior models in the age of mobile interventions: are our theories up to the task?, Translational behavioral medicine 1(1) (2011) 53–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Collins LM, Murphy SA, Bierman KL, A conceptual framework for adaptive preventive interventions, Prevention science 5(3) (2004) 185–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Norman GJ, Zabinski MF, Adams MA, Rosenberg DE, Yaroch AL, Atienza AA, A Review of e-Health Interventions for Physical Activity and Dietary Behavior Change, Am.J.Prev.Med (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Murphy SA, Collins LM, Rush AJ, Customizing treatment to the patient: adaptive treatment strategies, Drug and alcohol dependence 88 Suppl 2 (2007) S1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Galbicka G, Shaping in the 21st century: Moving percentile schedules into applied settings, J Appl.Behav Anal 27(4) (1994) 739–760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Adams MA, Hurley JC, Todd M, Bhuiyan N, Jarrett CL, Tucker WJ, Hollingshead KE, Angadi SS, Adaptive goal setting and financial incentives: a 2 × 2 factorial randomized controlled trial to increase adults' physical activity, BMC public health 17(1) (2017) 286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Adams MA, Sallis JF, Norman GJ, Hovell MF, Hekler EB, Perata E, An adaptive physical activity intervention for overweight adults: a randomized controlled trial, PloS one 8(12) (2013) e82901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Adams MA, A Pedometer-based Intervention to Increase Physical Activity:Applying Frequent, Adaptive Goals and a Percentile Schedule of Reinforcement, University of California, San Diego, San Diego, California, 2009. [Google Scholar]
- [14].Korinek EV, Phatak SS, Martin CA, Freigoun MT, Rivera DE, Adams MA, Klasnja P, Buman MP, Hekler EB, Adaptive step goals and rewards: a longitudinal growth model of daily steps for a smartphone-based walking intervention, J Behav Med 41(1) (2018) 74–86. [DOI] [PubMed] [Google Scholar]
- [15].Poirier J, Bennett WL, Jerome GJ, Shah NG, Lazo M, Yeh HC, Clark JM, Cobb NK, Effectiveness of an Activity Tracker- and Internet-Based Adaptive Walking Program for Adults: A Randomized Controlled Trial, Journal of medical Internet research 18(2) (2016) e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Miltenberger RG, Behavior Modification: Principles and Procedures, Wadsworth Publishing Company, Belmont, CA, 2001. [Google Scholar]
- [17].Epstein LH, Integrating theoretical approaches to promote physical activity, Am J Prev Med 15(4) (1998) 257–65. [DOI] [PubMed] [Google Scholar]
- [18].Biglan A, Selection by consequences: one unifying principle for a transdisciplinary science of prevention, Prevention science 4(4) (2003) 213–32. [DOI] [PubMed] [Google Scholar]
- [19].Bickel WK, Vuchinich RE, Reframing health behavior change with behavioral economics, Lawrence Erlbaum, Mahwah, N.J., 2000. [Google Scholar]
- [20].Giles EL, Robalino S, McColl E, Sniehotta FF, Adams J, The effectiveness of financial incentives for health behaviour change: systematic review and meta-analysis, PloS one 9(3) (2014) e90347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Sallis JF, Cerin E, Conway TL, Adams MA, Frank LD, Pratt M, Salvo D, Schipperijn J, Smith G, Cain KL, Davey R, Kerr J, Lai PC, Mitas J, Reis R, Sarmiento OL, Schofield G, Troelsen J, Van Dyck D, De Bourdeaudhuij I, Owen N, Physical activity in relation to urban environments in 14 cities worldwide: a cross-sectional study, Lancet 387(10034) (2016) 2207–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Bauman AE, Reis RS, Sallis JF, Wells JC, Loos RJ, Martin BW, Lancet Physical Activity Series Working Group, Correlates of physical activity: why are some people physically active and others not?, Lancet 380(9838) (2012) 258–71. [DOI] [PubMed] [Google Scholar]
- [23].Hovell MF, Wahlgren DR, Adams MA, The logical and empirical basis for the Behavioral Ecological Model, in: DiClemente RJ (Ed.), Emerging Theories in Health Promotion Practice and Research, Jossey-Bass, San Francisco, 2009. [Google Scholar]
- [24].Sallis JF, Owen N, Fisher E, Ecological models of health behavior, in: Glanz K, Rimer BK, Viswanath K (Eds.), Health Behavior and Health Education: Theory, Research, and Practice, Jossey-Bass, San Francisco, 2009, pp. 465–482. [Google Scholar]
- [25].Barnes R, Giles-Corti B, Bauman A, Rosenberg M, Bull FC, Leavy JE, Does neighbourhood walkability moderate the effects of mass media communication strategies to promote regular physical activity?, Annals of behavioral medicine 45 Suppl 1 (2013) S86–94. [DOI] [PubMed] [Google Scholar]
- [26].Kerr J, Norman GJ, Adams MA, Ryan S, Frank L, Sallis JF, Calfas KJ, Patrick K, Do neighborhood environments moderate the effect of physical activity lifestyle interventions in adults?, Health Place 16(5) (2010) 903–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Michael YL, Carlson NE, Analysis of Individual Social-ecological Mediators and Moderators and Their Ability to Explain Effect of a Randomized Neighborhood Walking Intervention, International Journal of Behavioral Nutrition and Physical Activity 6 (2009) 49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Riley DL, Mark AE, Kristjansson E, Sawada MC, Reid RD, Neighbourhood walkability and physical activity among family members of people with heart disease who participated in a randomized controlled trial of a behavioural risk reduction intervention, Health Place 21 (2013) 148–55. [DOI] [PubMed] [Google Scholar]
- [29].Frank LD, Sallis JF, Saelens BE, Leary L, Cain K, Conway TL, Hess PM, The development of a walkability index: application to the Neighborhood Quality of Life Study, British journal of sports medicine 44(13) (2010) 924–33. [DOI] [PubMed] [Google Scholar]
- [30].Sallis JF, Saelens BE, Frank LD, Conway TL, Slymen DJ, Cain KL, Chapman JE, Kerr J, Neighborhood built environment and income: examining multiple health outcomes, Social science & medicine 68(7) (2009) 1285–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].King A, Sallis J, Frank L, Saelens B, Ahn D, Conway T, Cain K, Neighborhood Design, Physical Function, and Healthful Lifestyles in Older Adults: Results from the Seniors Neighborhood Quality of Life Study, Int J Behav Med 17 (2010) 252–253. [Google Scholar]
- [32].King AC, Sallis JF, Frank LD, Saelens BE, Cain K, Conway TL, Chapman JE, Ahn DK, Kerr J, Aging in neighborhoods differing in walkability and income: associations with physical activity and obesity in older adults, Social science & medicine 73(10) (2011) 1525–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Van Dyck D, Cardon G, Deforche B, Sallis JF, Owen N, De Bourdeaudhuij I, Neighborhood SES and walkability are related to physical activity behavior in Belgian adults, Prev Med 50 Suppl 1 (2010) S74–9. [DOI] [PubMed] [Google Scholar]
- [34].Sugiyama T, Cerin E, Owen N, Oyeyemi AL, Conway TL, Van Dyck D, Schipperijn J, Macfarlane DJ, Salvo D, Reis RS, Mitas J, Sarmiento OL, Davey R, Schofield G, Orzanco-Garralda R, Sallis JF, Perceived neighbourhood environmental attributes associated with adults recreational walking: IPEN Adult study in 12 countries, Health Place 28C (2014) 22–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Owen N, Cerin E, Leslie E, duToit L, Coffee N, Frank LD, Bauman AE, Hugo G, Saelens BE, Sallis JF, Neighborhood walkability and the walking behavior of Australian adults, Am J Prev Med 33(5) (2007) 387–95. [DOI] [PubMed] [Google Scholar]
- [36].Welk GJ, Physical activity assessment for health-related research, (2002). [Google Scholar]
- [37].Welk GJ, Schaben JA, Morrow JR Jr., Reliability of accelerometry-based activity monitors: a generalizability study, Med Sci Sports Exerc 36(9) (2004) 1637–45. [PubMed] [Google Scholar]
- [38].Rachlin H, The science of self-control, Harvard University Press, Cambridge, Mass, 2000. [Google Scholar]
- [39].Coleman KJ, Paluch RA, Epstein LH, A method for the delivery of reinforcement during exercise, Behavior Research Methods Instruments & Computers 29(2) (1997) 286–290. [Google Scholar]
- [40].Epstein LH, Roemmich JN, Reducing sedentary behavior: role in modifying physical activity, Exercise and Sport Sciences Reviews 29(3) (2001) 103–8. [DOI] [PubMed] [Google Scholar]
- [41].Epstein LH, Roemmich JN, Paluch RA, Raynor HA, Physical activity as a substitute for sedentary behavior in youth, Ann.Behav Med 29(3) (2005) 200–209. [DOI] [PubMed] [Google Scholar]
- [42].Adams MA, Norman GJ, Hovell MF, Sallis JF, Patrick K, Reconceptualizing decisional balance in an adolescent sun protection intervention: mediating effects and theoretical interpretations, Health Psychol 28(2) (2009) 217–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Prochaska JO, Velicer WF, Rossi JS, Goldstein MG, Marcus BH, Rakowski W, Fiore C, Harlow LL, Redding CA, Rosenbloom D, et al. , Stages of change and decisional balance for 12 problem behaviors, Health Psychol 13(1) (1994) 39–46. [DOI] [PubMed] [Google Scholar]
- [44].Bandura A, Health promotion by social cognitive means, Health education & behavior 31(2)(2004)143–64. [DOI] [PubMed] [Google Scholar]
- [45].Williams DM, Anderson ES, Winett RA, A review of the outcome expectancy construct in physical activity research, Annals of behavioral medicine 29(1) (2005) 70–9. [DOI] [PubMed] [Google Scholar]
- [46].Bandura A, Self-efficacy: the exercise of control, WH Freeman, New York, 1997. [Google Scholar]
- [47].Rovniak LS, Hovell MF, Wojcik JR, Winett RA, Martinez-Donate AP, Enhancing theoretical fidelity: an e-mail-based walking program demonstration, Am J Health Promot 20(2) (2005) 85–95. [DOI] [PubMed] [Google Scholar]
- [48].Marshall SJ, Levy SS, Tudor-Locke CE, Kolkhorst FW, Wooten KM, Ji M, Macera CA, Ainsworth BE, Translating physical activity recommendations into a pedometer-based step goal: 3000 steps in 30 minutes, Am J Prev Med 36(5) (2009) 410–5. [DOI] [PubMed] [Google Scholar]
- [49].U.S. Department of Health and Human Services, 2008 Physical Activity Guidelines for Americans, 2008. [Google Scholar]
- [50].G. Diabetes Prevention Program Research, The Diabetes Prevention Program (DPP): description of lifestyle intervention, Diabetes Care 25(12) (2002) 2165–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Prochaska JO, Redding CA, Evers KE, The Transtheoretical Model and Stages of Change, in: Glanz K, Lewis FM, Rimer BK (Eds.), Health Behavior and Health Education: Theory Research and Practice, Jossey-Bass Inc., San Francisco, 1997, pp. 60–84. [Google Scholar]
- [52].Skinner BF, Science and human behavior, Macmillan, New York, 1953. [Google Scholar]
- [53].Kazdin AE, The token economy: a decade later, Journal of applied behavior analysis 15(3) (1982) 431–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Ferster CB, Skinner BF, Schedules of Reinforcement, Appleton-Century-Crofts, New York:, 1957. [Google Scholar]
- [55].Cohen SL, Chelland S, Ball KT, LeMura LM, Effects of fixed ratio schedules of reinforcement on exercise by college students, Percept.Mot.Skills 94(3 Pt 2) (2002) 1177–1186. [DOI] [PubMed] [Google Scholar]
- [56].Epstein LH, Smith JA, Vara LS, Rodefer JS, Behavioral economic analysis of activity choice in obese children, Health Psychol 10(5) (1991) 311–316. [DOI] [PubMed] [Google Scholar]
- [57].Lattal KA, Neef NA, Recent reinforcement-schedule research and applied behavior analysis, J Appl.Behav Anal 29(2) (1996) 213–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Sallis JF, Cervero RB, Ascher W, Henderson KA, Kraft MK, Kerr J, An ecological approach to creating active living communities, Annual review of public health 27 (2006) 297–322. [DOI] [PubMed] [Google Scholar]
- [59].Matthews CE, Hagstromer M, Pober DM, Bowles HR, Best practices for using physical activity monitors in population-based research, Med Sci Sports Exerc 44(1 Suppl 1) (2012) S68–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Choi L, Liu Z, Matthews CE, Buchowski MS, Validation of accelerometer wear and nonwear time classification algorithm, Med Sci Sports Exerc 43(2) (2011) 357–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Choi L, Ward SC, Schnelle JF, Buchowski MS, Assessment of wear/nonwear time classification algorithms for triaxial accelerometer, Med Sci Sports Exerc 44(10) (2012) 2009–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [62].Freedson PS, Melanson E, Sirard J, Calibration of the Computer Science and Applications, Inc. accelerometer, Med Sci Sports Exerc 30(5) (1998) 777–81. [DOI] [PubMed] [Google Scholar]
- [63].Barnett A, van den Hoek D, Barnett D, Cerin E, Measuring moderate-intensity walking in older adults using the ActiGraph accelerometer, BMC Geriatr 16(1) (2016) 211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE, Pratt M, Ekelund U, Yngve A, Sallis JF, Oja P, International Physical Activity Questionnaire: 12-country reliability and validity, Med Sci Sports Exerc 35(8) (2003) 1381–95. [DOI] [PubMed] [Google Scholar]
- [65].Nicaise V, Crespo NC, Marshall S, Agreement between the IPAQ and accelerometer for detecting intervention-related changes in physical activity in a sample of Latina women, Journal of Physical Activity and Health 11(4) (2014) 846–52. [DOI] [PubMed] [Google Scholar]
- [66].Giles-Corti B, Timperio A, Cutt H, Pikora TJ, Bull FCL, Knuiman M, Bulsara M, Van Niel K, Shilton T, Development of a reliable measure of walking within and outside the local neighborhood: RESIDE's Neighborhood Physical Activity Questionnaire, Preventive Medicine 42(6) (2006) 455–459. [DOI] [PubMed] [Google Scholar]
- [67].Balke B, Ware RW, An experimental study of physical fitness of Air Force personnel, U S Armed Forces Med J 10(6) (1959) 675–88. [PubMed] [Google Scholar]
- [68].Borg GA, Psychophysical bases of perceived exertion, Med Sci Sports Exerc 14(5) (1982) 377–81. [PubMed] [Google Scholar]
- [69].Carlson JA, Sallis JF, Wagner N, Calfas KJ, Patrick K, Groesz LM, Norman GJ, Brief physical activity-related psychosocial measures: reliability and construct validity, Journal of Physical Activity and Health 9(8) (2012) 1178–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [70].Sallis JF, Pinski RB, Grossman RM, Patterson TL, Nader PR, The development of self-efficacy scales for health-related diet and exercise behaviors, Health Education Research 3(3) (1988) 283–292. [Google Scholar]
- [71].Sallis JF, Grossman RM, Pinski RB, Patterson TL, Nader PR, The development of scales to measure social support for diet and exercise behaviors, Prev Med 16(6) (1987) 825–36. [DOI] [PubMed] [Google Scholar]
- [72].Marcus BH, Rakowski W, Rossi JS, Assessing motivational readiness and decision making for exercise, Health Psychol 11(4) (1992) 257–61. [DOI] [PubMed] [Google Scholar]
- [73].Sallis JF, Hovell MF, Hofstetter CR, Faucher P, Elder JP, Blanchard J, Caspersen CJ, Powell KE, Christenson GM, A multivariate study of determinants of vigorous exercise in a community sample, Prev.Med 18(1) (1989) 20–34. [DOI] [PubMed] [Google Scholar]
- [74].Hovell MF, Sallis JF, Hofstetter CR, Spry VM, Faucher P, Caspersen CJ, Identifying correlates of walking for exercise: an epidemiologic prerequisite for physical activity promotion, Prev.Med 18(6) (1989) 856–866. [DOI] [PubMed] [Google Scholar]
- [75].Winett RA, Moore JF, Anderson ES, Extending the concept of social validity: behavior analysis for disease prevention and health promotion, Journal of applied behavior analysis 24(2) (1991) 215–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [76].Saelens BE, Sallis JF, Black JB, Chen D, Neighborhood-based differences in physical activity: an environment scale evaluation, American Journal of Public Health 93(9) (2003) 1552–1558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [77].Cerin E, Conway TL, Saelens BE, Frank LD, Sallis JF, Cross-validation of the factorial structure of the Neighborhood Environment Walkability Scale (NEWS) and its abbreviated form (NEWS-A), International Journal of Behavioral Nutrition and Physical Activity 6 (2009) 32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [78].Adams MA, Ryan S, Kerr J, Sallis JF, Patrick K, Frank L, Norman GJ, Validation of the Neighborhood Environment Walkability Scale (NEWS) Items Using Geographic Information Systems, Journal of Physical Activity and Health 6(Supp 1) (2009) S113–S123. [DOI] [PubMed] [Google Scholar]
- [79].Patch C, Conway T, Gavand KA, Saelens B, Adams MA, Cain K, Engelberg JK, Mayes L, Roesch SC, Sallis JF, Crime and physical activity: Development of a conceptual framework and measures, Journal of Physical Activity and Health (in press). [DOI] [PubMed] [Google Scholar]
- [80].Kirby KN, Petry NM, Bickel WK, Heroin addicts have higher discount rates for delayed rewards than non-drug-using controls, Journal of experimental psychology. General 128(1) (1999) 78–87. [DOI] [PubMed] [Google Scholar]
- [81].Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ, The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research, Psychiatry Res 28(2) (1989) 193–213. [DOI] [PubMed] [Google Scholar]
- [82].Psioda M, Random effects simulation for sample size calculations using SAS ®., Paper presented at the annual meeting of Southeast SAS Users Group, Durham, NC, USA, 2012. [Google Scholar]
- [83].Aiken LS, West SG, Multiple Regression: Testing and Interpreting Interactions SAGE Publications, Inc, Thousand Oaks, California, 1991. [Google Scholar]
- [84].Preacher KJ, Curran PJ, Bauer DJ, Computational tools for probing interactions in multiple linear regression, multilevel modeling, and latent curve analysis, J Educ Behav Stat 31(4) (2006) 437–448. [Google Scholar]
- [85].Riley WT, Martin CA, Rivera DE, Hekler EB, Adams MA, Buman MP, Pavel M, King AC, Development of a dynamic computational model of social cognitive theory, Translational behavioral medicine 6(4) (2016) 483–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [86].Berardi V, Carretero-Gonzalez R, Klepeis NE, Ghanipoor Machiani S, Jahangiri A, Bellettiere J, Hovell M, Computational model for behavior shaping as an adaptive health intervention strategy, Translational behavioral medicine 8(2) (2018) 183–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [87].Martin CA, Rivera DE, Riley WT, Hekler EB, Buman MP, Adams MA, King AC, A dynamical systems model of Social Cognitive Theory, American Control Conference (ACC), 2014, 2014, pp. 2407–2412. [Google Scholar]
- [88].Centers for Medicare and Medicaid Services, Medicaid Incentives for Prevention of Chronic Diseases (MIPCD) Program, 2011. http://www.cms.gov/MIPCD/. (Accessed 5/11/2011.
- [89].Miles A, Medicaid To Offer Rewards For Healthy Behavior, Los Angeles Times, Los Angeles, 4/August/2011. [Google Scholar]
- [90].Wing R, Gillis B, The Diabetes Prevention Program's Lifestyle Change Program Manual of Operations, Appendix G: Tool Box, University of Pittsburgh, Pittsburgh, PA, 1996. [Google Scholar]
- [91].Promberger M, Marteau TM, When do financial incentives reduce intrinsic motivation? comparing behaviors studied in psychological and economic literatures, Health Psychol 32(9) (2013) 950–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [92].Farooqui MA, Tan YT, Bilger M, Finkelstein EA, Effects of financial incentives on motivating physical activity among older adults: results from a discrete choice experiment, BMC public health 14 (2014) 141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [93].Patel MS, Asch DA, Rosin R, Small DS, Bellamy SL, Heuer J, Sproat S, Hyson C, Haff N, Lee SM, Wesby L, Hoffer K, Shuttleworth D, Taylor DH, Hilbert V, Zhu J, Yang L, Wang X, Volpp KG, Framing Financial Incentives to Increase Physical Activity Among Overweight and Obese Adults: A Randomized, Controlled Trial, Ann Intern Med 164(6) (2016) 385–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [94].Jeffery RW, Financial incentives and weight control, Prev Med 55 Suppl (2012) S61–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [95].Mitchell MS, Goodman JM, Alter DA, John LK, Oh PI, Pakosh MT, Faulkner GE, Financial incentives for exercise adherence in adults: systematic review and meta-analysis, Am J Prev Med 45(5) (2013) 658–67. [DOI] [PubMed] [Google Scholar]
- [96].Mantzari E, Vogt F, Shemilt I, Wei Y, Higgins JP, Marteau TM, Personal financial incentives for changing habitual health-related behaviors: A systematic review and meta-analysis, Prev Med 75 (2015) 75–85. [DOI] [PMC free article] [PubMed] [Google Scholar]