Watch a video presentation of this article
Watch the interview with the author
Answer questions and earn CME
Abbreviations
- AH
alcoholic hepatitis
- ALT
alanine aminotransferase
- AST
aspartate aminotransferase
- CI
confidence interval
- DAMP
damage‐associated molecular pattern
- IL
interleukin
- INR
international normalized ratio
- LPS
lipopolysaccharide
- mDF
Maddrey Discriminant Function
- MELD
Model for End‐Stage Liver Disease
- PAMP
pathogen‐associated molecular pattern
- PT
prothrombin time
- STOPAH
Steroids or Pentoxifylline in Alcoholic Hepatitis
- TNF‐α
tumor necrosis factor‐α
Excessive alcohol consumption leads to both acute and chronic liver diseases. Acute liver injury caused by alcohol, or alcoholic hepatitis (AH), is a highly morbid condition with 30‐day mortality greater than 30% among patients with severe disease.1 Despite extensive research efforts over the last 50 years, management of severe AH remains a clinical challenge with few effective treatment options. This review will discuss treatment approaches for patients with AH and highlight novel therapeutic options currently under development.
Pathophysiology
The hallmark of AH is liver inflammation, marked by dense neutrophilic infiltrates and prominent increases of inflammatory cytokines.2 Alcohol induces cell death in hepatocytes, leading to the release of damage‐associated molecular patterns (DAMPs) that potently activate the immune system. Chronic alcohol exposure can also lead to increased gut permeability and elevation of circulating bacterial products such as lipopolysaccharide (LPS), which is a strong activator of immune response3 (Fig. 1). AH may occur in the presence or absence of liver fibrosis, and underlying liver fibrosis is an independent risk factor for mortality in AH.4 Even in the absence of significant liver fibrosis, AH can increase intrahepatic resistance, leading to portal hypertension and associated complications.
Figure 1.
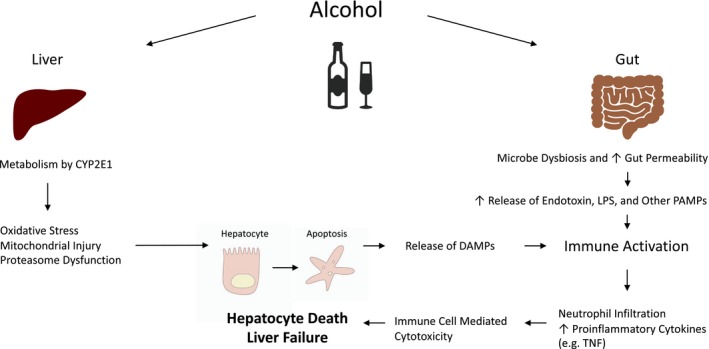
Pathophysiology of alcohol‐induced liver injury.
Diagnosis
Clinical manifestations of AH may include jaundice, anorexia, fever, abdominal pain, and liver decompensations due to portal hypertension.2 Typically, laboratory studies will show moderately elevated transaminases (rarely >500 IU/L), with aspartate aminotransferase‐to‐alanine aminotransferase ratio greater than 1.5. Bilirubin is elevated in acute AH as a defining feature of this disease. Findings of malnutrition may be seen in chronic alcohol abusers. In the United States, AH is often diagnosed based on clinical findings, with rapid onset of jaundice and transaminitis in the context of heavy alcohol use.5 Although liver biopsy may help to preclude alternative diagnoses of liver injury, it is not required for diagnosis of AH and is typically reserved in situations where the diagnosis is unclear. Characteristic features of AH on biopsy include ballooning degeneration of hepatocytes, alcoholic hyaline (Mallory‐Denk bodies) within damaged hepatocytes, cholestasis, and neutrophilic infiltrates.2
Management
Risk Stratification
The prognosis of AH is largely determined by severity of liver inflammation and dysfunction. A number of empirical scoring systems have been validated to help risk‐stratify patients with AH (Table 1); most commonly used in clinical practice are the Maddrey Discriminant Function (mDF) and the Model for End‐Stage Liver Disease (MELD) score. Those patients with mDF ≥32 or MELD >20 are generally considered to have severe disease and should be considered for treatment with corticosteroids.1, 6 A calculator of predicated mortality of AH based on MELD score is available through the Mayo Clinic website (MELD Score and 90‐Day Mortality Rate for Alcoholic Hepatitis Calculator: https://www.mayoclinic.org/medical-professionals/transplant-medicine/calculators/meld-score-and-90-day-mortality-rate-for-alcoholic-hepatitis/itt-20434719) based on data derived from a cohort study by Dunn et al.6 (Fig. 2). Others with milder diseases are generally monitored with supportive care. A management algorithm is outlined in Fig. 3.
Table 1.
Clinical Tools for Risk Stratification of Patients With AH
| Clinical Tools | Parameters | Cutoff Value for Severe Hepatitis |
|---|---|---|
| mDF | PT, total bilirubin | ≥32 |
| MELD | Total bilirubin, INR, creatinine | >20 |
| Glasgow Alcoholic Hepatitis Score (GAHS) | Age, total bilirubin, PT, blood urea nitrogen, white blood cell count | ≥9 |
| Age‐Bilirubin‐INR‐Creatinine Score (ABIC) | Age, total bilirubin, INR, and creatinine | ≥9 |
| Hepatic Histological Score | Fibrosis, neutrophilic infiltration, bilirubinostasis, presence of megamitochondria | ≥6 |
| Lille Score | Age, total bilirubin, albumin, PT, creatinine | >0.45 |
Figure 2.
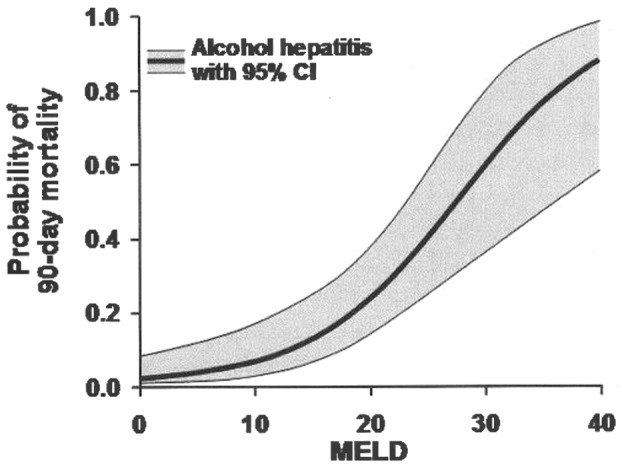
Ninety‐day mortality clinical calculator. Adapted with permission from Hepatology.6 Copyright 2005, American Association for the Study of Liver Diseases.
Figure 3.
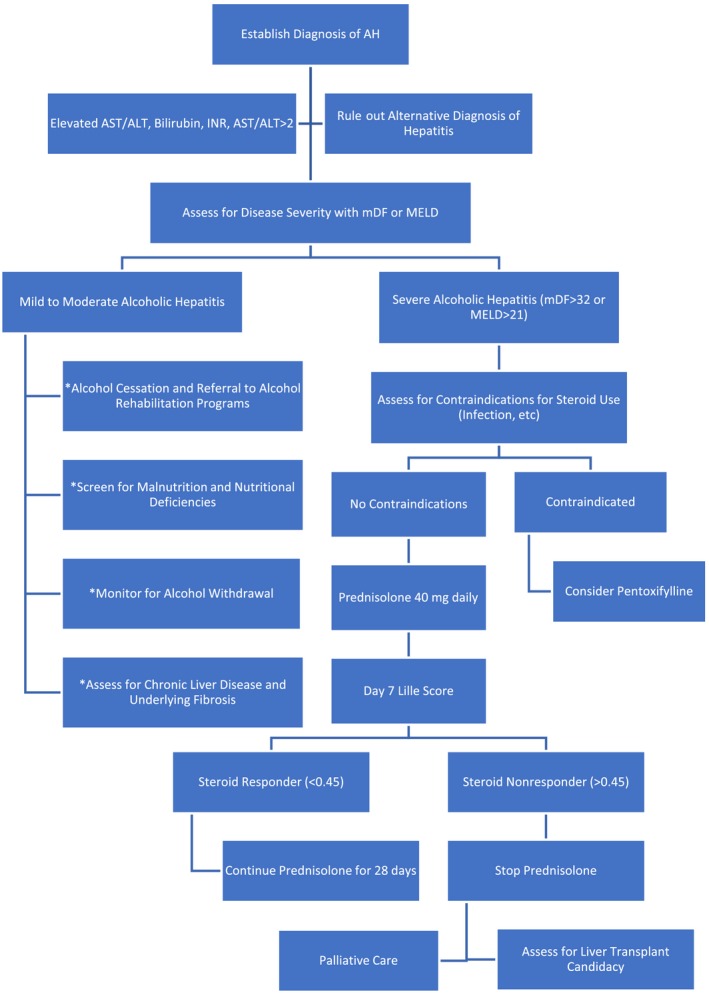
Management algorithm of AH. *These general management steps should be applied to all patients with AH.
Corticosteroids and Pentoxifylline
Corticosteroids have long been used in the treatment of severe AH1 given their anti‐inflammatory properties. Pentoxifylline is a phosphodiesterase inhibitor and an inhibitor of tumor necrosis factor‐α (TNF‐α), a key inflammatory cytokine in AH. The efficacies of steroids and pentoxifylline have been heterogenous in various clinical trials. A frequently cited study, the Steroids or Pentoxifylline in Alcoholic Hepatitis (STOPAH) trial is the largest randomized clinical trial on management of AH conducted to date. In STOPAH, a trend toward mortality reduction was seen in patients treated with prednisolone at 28 days, but no benefit at 3 months or 1 year.7 Rate of infection was also higher in patients treated with steroids in this study. Pentoxifylline has been previously shown to decrease mortality in patients with hepatorenal syndrome8; however, the STOPAH trial failed to show a mortality benefit with pentoxifylline.7 In practice, it is reasonable to treat patients with severe AH with prednisolone 40 mg daily in the absence of contraindications, after infection has been ruled out. The benefit of corticosteroids should be assessed at day 7 with Lille score. A score less than 0.45 indicates response to corticosteroids, and corticosteroids should be continued for 28 days, whereas a score greater than 0.45 indicates a lack of response, and corticosteroids should be stopped. Many patients have contraindications to corticosteroids, limiting their generalized use. Lack of benefit of corticosteroids beyond 1 month also limits enthusiasm of their use in many circles.
Nutrition
Malnutrition adversely affects outcome in AH, and several studies suggested improved clinical outcomes with nutritional supplementation.9, 10 Unfortunately, anorexia is a common manifestation of AH, and presence of other complications, such as ascites and hepatic encephalopathy, can often hinder oral intake, necessitating an alternative route of access to achieve caloric goal. Given concern for increased susceptibility to infection in AH, enteral access is often preferred over parental access. Vitamin and mineral deficiencies are common among patients with AH and should be aggressively repleted when present (Table 2).
Table 2.
Nutrition Goals and Common Micronutrient Deficiencies in AH
| Daily Intake Recommendations | |
|---|---|
| Protein | 1‐1.5 g/kg/day |
| Calories | 30‐40 kcal/kg/day |
| Common micronutrient deficiencies | Thiamine, zinc, calcium, magnesium, B12, folate, vitamin A/D/E/K |
Management of Other Complications
Patients with AH are at high risk for infections. Evidence in support of prophylactic antibiotics use in AH is currently lacking, but a thorough assessment for potential infections, including sampling of blood, urine, and ascitic fluid when present, should be obtained in patients with severe AH. Other complications of portal hypertension such as jaundice, ascites, hepatic encephalopathy, and variceal bleeding may be present, even in the absence of liver cirrhosis. Acute kidney injury is a strong negative predicator of outcomes in AH, and nephrotoxic medications and prerenal azotemia should be avoided when possible.11
Alcohol Cessation
Complete abstinence from alcohol is advocated for patients with AH. Unfortunately, recidivism rate is high. Alcohol rehabilitation programs should be recommended to all patients. Participation in groups such as Alcoholic Anonymous should be encouraged.
Liver Transplantation
Liver transplantation is an effective treatment of severe AH, but recidivism is a significant concern. Six months of alcohol cessation is a common prerequisite to liver transplantation, but this requirement is not always practical for patients who are acutely ill. In patients with severe AH who are not responding to corticosteroids, early liver transplantation has been demonstrated to significantly improve survival.12 Liver transplant evaluation, including a thorough psychiatric evaluation, should be considered for patients who did not respond to corticosteroid therapy and fulfill the following criteria: (1) good insights into their alcohol use disorder and recognition of alcohol abuse as the cause of their liver disease, (2) commitment to alcohol sobriety and willingness to complete required substance rehabilitation programs, and (3) good social support and adequate resources to assist with posttransplant care. A very small percentage of patients with AH fall into this category.
Other Therapeutics in Development
Many anti‐inflammatory agents have been studied in the context of AH, with a number of therapeutics currently in clinical trials. TNF‐α inhibitors infliximab and etanercept have previously been studied in AH but failed to benefit because of increased rate of infections.13 Other anti‐inflammatories, such as anti‐LPS antibodies, anti–Toll‐like receptor 4 antibodies, and interleukin (IL)‐1 receptor antagonist are currently in clinical trials.14 Antioxidants N‐acetylcysteine and metadoxine, caspase inhibitor emricasan, cytokine IL‐22, and farnesoid X receptor agonist obeticholic acid have also been studied in clinical trials for their hepatoprotective effects.14
Conclusion
AH is a highly morbid condition with few effective treatments. Mortality of AH has improved in recent decades through better management of complications, but remains formidable. Significant strides in patient outcome await the development of more efficacious therapeutics for AH.
Potential conflict of interest: Nothing to report.
References
- 1. Mathurin P, Mendenhall CL, Carithers RL, et al. Corticosteroids improve short‐term survival in patients with severe alcoholic hepatitis (AH): Individual data analysis of the last three randomized placebo controlled double blind trials of corticosteroids in severe AH. J Hepatol 2002;36:480‐487. [DOI] [PubMed] [Google Scholar]
- 2. Carithers RL, McClain CJ. Alcoholic liver disease In: Feldman M, Friedman LS, Brandt LJ, ed. Sleisenger and Fordtran’s Gastrointestinal and Liver Disease. 5th ed. St. Louis, MO: WB Saunders; 2016:1409‐1427. [Google Scholar]
- 3. Wang HJ, Gao B, Zakhari S, et al. Inflammation in alcoholic liver disease. Annu Rev Nutr 2012;32:343‐368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lackner C, Spindelboeck W, Haybaeck J, et al. Histological parameters and alcohol abstinence determine long‐term prognosis in patients with alcoholic liver disease. J Hepatol 2017;66:610‐618. [DOI] [PubMed] [Google Scholar]
- 5. Crabb DW, Bataller R, Chalasani NP, et al. Standard definitions and common data elements for clinical trials in patients with alcoholic hepatitis: Recommendation from the NIAAA Alcoholic Hepatitis Consortia. Gastroenterology 2016;150:785‐790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Dunn W, Jamil LH, Brown LS, et al. MELD accurately predicts mortality in patients with alcoholic hepatitis. Hepatology 2005;41:353‐358. [DOI] [PubMed] [Google Scholar]
- 7. Thursz MR, Richardson P, Allison M, et al. Prednisolone or pentoxifylline for alcoholic hepatitis. N Engl J Med 2015;372:1619‐1628. [DOI] [PubMed] [Google Scholar]
- 8. Akriviadis E, Botla R, Briggs W, et al. Pentoxifylline improves short‐term survival in severe acute alcoholic hepatitis: A double‐blind, placebo‐controlled trial. Gastroenterology 2000;119:1637‐1648. [DOI] [PubMed] [Google Scholar]
- 9. Fialla AD, Israelsen M, Hamberg O, et al. Nutritional therapy in cirrhosis or alcoholic hepatitis: A systematic review and meta‐analysis. Liver Int 2015;35:2072‐2078. [DOI] [PubMed] [Google Scholar]
- 10. Mitchell MC, Friedman LS, McClain CJ. Medical management of severe alcoholic hepatitis: Expert review from the Clinical Practice Updates Committee of the AGA Institute. Clin Gastroenterol Hepatol 2017;15:5‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Altamirano J, Fagundes C, Dominguez M, et al. Acute kidney injury is an early predictor of mortality for patients with alcoholic hepatitis. Clin Gastroenterol Hepatol 2012;10:e63. [DOI] [PubMed] [Google Scholar]
- 12. Mathurin P, Moreno C, Samuel D, et al. Early liver transplantation for severe alcoholic hepatitis. N Engl J Med 2011;365:1790‐1800. [DOI] [PubMed] [Google Scholar]
- 13. Naveau S, Chollet‐Martin S, Dharancy S, et al. A double‐blind randomized controlled trial of infliximab associated with prednisolone in acute alcoholic hepatitis. Hepatology 2004;39:1390‐1397. [DOI] [PubMed] [Google Scholar]
- 14. Singal AK, Shah VH. Therapeutic strategies for the treatment of alcoholic hepatitis. Semin Liver Dis 2016;36:56‐68. [DOI] [PubMed] [Google Scholar]


