Abstract
Background:
Cognitive deficits, a core feature contributing to disability in schizophrenia, are present in milder form in individuals at clinical high risk (CHR) for psychosis. This study investigated the feasibility of Cognition for Learning and Understanding Everyday Social Situations (CLUES), an integrated neurocognitive and social cognitive treatment for youth at CHR.
Method:
This was an open, pilot feasibility trial. Seventeen individuals meeting CHR criteria were assessed prior to and following participation in CLUES for changes in symptoms, social and role functioning, and cognition. Participant attitudes towards CLUES were also examined.
Results:
Participants significantly improved in social functioning [t(16)=−4.20, p=.001, d= 1.02], and trended for improvement in reaction time [t(15)=2.09, p=.054, d= .52] from baseline to end of treatment. No other measures significantly changed. No participants transitioned to full psychosis during the treatment and follow up period. Participants reported they generally liked CLUES and found it helpful.
Conclusion:
While limited by the small sample size and the open label design, our preliminary results indicate that CLUES is feasible and shows promise in improving social functioning. However, further investigation is warranted in order to determine its efficacy. Future directions should include conducting a randomized controlled trial in order to compare the efficacy of CLUES to another intervention.
Introduction
Cognitive deficits are core features of schizophrenia (Green et al., 2000). Cognitive deficits in schizophrenia impact psychomotor speed, memory, attention, reasoning, and social cognition (Nuechterlein et al., 2004; Green et al., 2012), and contribute to social and functional disability (Keshavan and Hogarty, 1999). Cognitive deficits are present in a mild form during the prodromal, or clinical high risk (CHR) phase of the illness and decline (Giuliano et al., 2012) before the first psychotic episode (Mesholam-Gately et al., 2009). Therefore, intervention for CHR may prevent cognitive decline during the critical period of adolescence.
Recent meta-analyses show that psychosocial approaches to cognitive remediation are effective in schizophrenia (Wykes et al., 2011). Cognitive Enhancement Therapy (CET), (Hogarty et al., 2004), is an intensive, 18-month psychosocial cognitive rehabilitation program addressing social and non-social cognitive deficits through computerized neurocognitive remediation sessions with a peer and a coach, and social-cognitive rehabilitation groups (see Hogarty and Greenwald, 2006). CET improves cognition, social cognition and employment in early course schizophrenia (Eack et al., 2009; Eack et al., 2011), with durable effects one year following end of treatment (Eack et al., 2010). CET may also protect against gray matter loss (Eack et al., 2010). Building upon what is known from the effectiveness of CET for individuals with early course psychosis (Eack et al., 2009), we sought to develop a similar intervention for youth at risk for psychosis. Initial studies investigating the impact of psychosocial (family and cognitive therapy) and pharmacological approaches to treating CHR have shown promise for reducing rates of conversion to psychosis (Schmidt et al., 2015). However, to our knowledge, no prior studies have applied a comprehensive, multifaceted cognitive remediation program for youth at CHR, targeting neurocognitive and social cognitive processes in order to improve functioning.
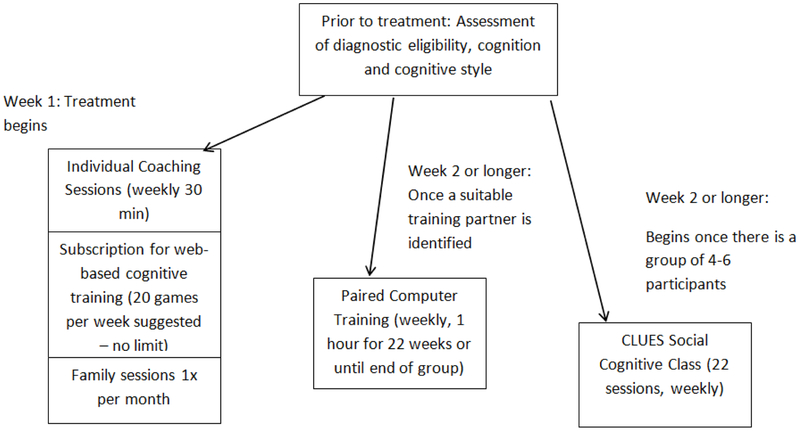
The Cognition for Learning and for Understanding Everyday Social Situations (CLUES) intervention was designed for youth at CHR for psychosis and inspired by CET. To make the treatment appropriate for individuals at CHR, the treatment included the following modifications and additions: 1) shortened treatment length (6 months); 2) content targeted for individuals at CHR 3) engaging/developmentally relevant social-cognitive group materials for a younger population, 4) monthly family sessions; 5) internet-based neurocognitive training done at home to supplement the clinician-facilitated neurocognitive training sessions completed with a peer; 6) Included content to enhance engagement and address comorbid symptoms, including information about growth mindset (Dweck, 1999), Acceptance and Commitment Therapy (ACT, (Hayes et al., 1999), and mindfulness (Cramer et al., 2016). See Figure 1 and supplemental material for CLUES treatment model. Our goal was to develop and pilot CLUES, and to assess its acceptability, tolerability and feasibility in an open trial.
Figure 1.
Overview of CLUES Treatment Components
Methods
We present combined data from two open label feasibility projects examining CLUES: a) CLUES CEDAR: de-identified quality assurance data collected when CLUES was offered as a clinical service at the Center for Early Detection, Assessment and Response to Risk (CEDAR Clinic, Friedman-Yakoobian et al., 2018); and b) CLUES R34: a pilot NIMH funded trial (5R34MH105596). These projects were reviewed by the Institutional Review Boards at the Beth Israel Deaconess Medical Center and the Massachusetts Department of Mental Health. For the R34 study, informed consent was obtained from adult participants. For those under age 18, consent was obtained from parents/ guardians and assent was obtained from the minor. Both studies had a nearly identical treatment design, treatment setting, and outcomes assessments. The R34 study occurred a few months after the CLUES CEDAR pilot trial and included additional assessments and some minor enhancements to group materials (see supplement for details). This paper presents measures that were common to both studies. All participants were assessed prior to starting CLUES and at the end of treatment.
Participants were recruited via social media, online advertisements, community clinicians, schools and universities. Participants were enrolled if they met the following criteria: 1) Ages 15-30, 2) At least moderate difficulty with motivation, organization or flexibility, causing disruption in social or role functioning as measured by an assessment of cognitive styles and social cognition (Cognitive Styles and Social Cognition Eligibility Interview, Hogarty, Flesher, and Greenwald, 2006 or Styles of Thinking Assessment and Rating Scale, Gnong-Granato et al., unpublished), 3) Met Criteria of Prodromal states (COPS) on the Structured Interview for Psychosis Risk Syndromes (SIPS, (Miller et al., 2003) or met early, broad, criteria for CHR (Keshavan et al., 2011). Exclusion criteria were: 1) a full psychotic disorder, 2) significant neurological or medical disorders causing cognitive impairment, 3) > 24 months (lifetime) exposure to antipsychotic treatment, 4) DSM-IV substance abuse or dependence in the past 3 months, 5) < 6th grade reading level, and 6) current, persistent suicidal or homicidal behavior.
Participants completed assessments before and at the end of about 6 months CLUES treatment (ET). Participants were assessed by trained and reliable raters for demographic data, CHR symptoms (SIPS, Miller et al., 2003), social and role functioning (Global Functioning: Social and Role Scales, Cornblatt et al., 2007; Niendam et al., 2006), processing speed (Brief Assessment of Cognition in Schizophrenia (BACS) symbol coding, (Keefe et al., 2004; Nuechterlein et al., 2008), reaction time (ORM, Ben-Yishay, 1981), estimated premorbid IQ (Wide Range Achievement Test, WRAT; Wilkinson and Robertson, 2006) or Wechsler Test of Adult Reading (WTAR; Wechsler, 2001), and social cognition (Mayer-Salovey-Caruso Emotional Intelligence Test, MSCEIT, Mayer et al., 2003). CHR eligibility was determined via consensus ratings by experienced raters.
Additionally, participants were surveyed monthly about their experience in CLUES, i.e. how much they liked each part of CLUES and how helpful they felt CLUES was for them in different areas of cognition/ functioning using a Likert scale ranging from 0 (not at all) to 4 (a lot). For this paper, we analyzed the last monthly satisfaction questionnaire for each participant.
All participants took part in the CLUES intervention (see supplement for additional information about individual, paired cognitive remediation, group and family components of CLUES). Participants were paid for completing study assessments but were not paid for participating in treatment sessions or cognitive training.
Results
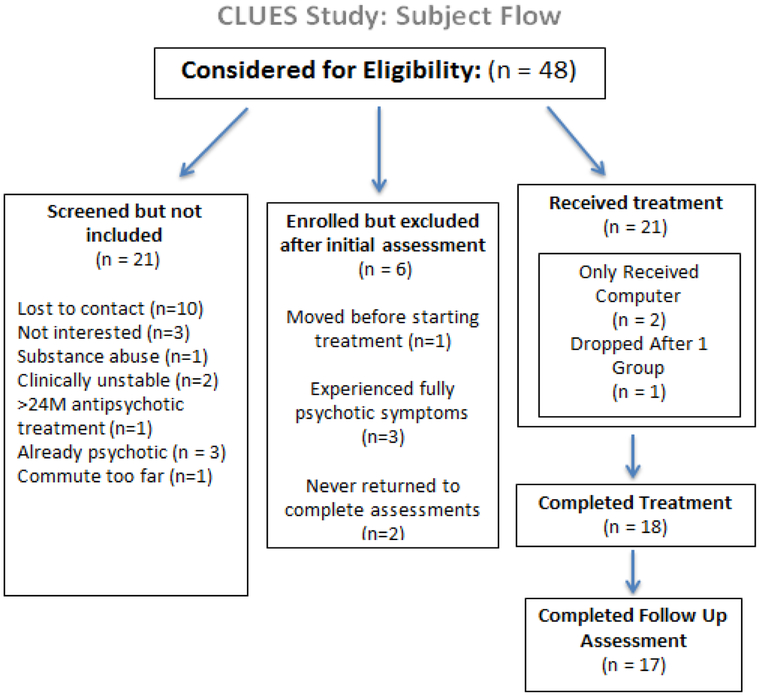
See Figure 2 for participant flow and reasons for exclusion or dropout. Of 48 screened individuals, 21 had partial clues treatment, 18 completed the treatment, and 17 completed both baseline and ET assessments. For those who began CLUES treatment, the attrition rate was 19%. Demographics are presented in Table 1.
Figure 2.
Participant Flow Consort Diagram
Table 1:
Demographics
| Demographic Characteristics |
Total (n=17) | |
|---|---|---|
| Age (years) Mean (SD); Range | 20.53 (4.0); 15-30 | |
| Gender (n) | 14 Male | |
| 3 Female | ||
| Racial Identification (n) | 12 | White |
| 3 | Black or African American | |
| 2 | Interracial | |
| Highest Level of Education (n) | 5 | Some grade school, not completed high school |
| 10 | High school | |
| 2 | College/University | |
| Premorbid IQ* Mean (SD); Range | 112.1 (13.8); 76-134 |
For CLUES CEDAR, premorbid IQ was calculated using the Wide Range Achievement Test (WRAT). For CLUES R34 OT, premorbid IQ was calculated using the Wechsler Test of Adult Reading (WTAR).
On average, participants attended 17.4 out of 22 group sessions (median 18, range 8-21), with 70.6% of participants attending at least 70% (16 of 22) group sessions. On average, participants attended 17.7 computer sessions (median 17, range 4-42) with 58.8% of participants attending at least 16 computer sessions. They attended an average of 19.5 individual coaching sessions (median 19, range 4-29), with 82.4% of participants attending at least 16 sessions. Participants were expected to complete 20 web-based cognitive remediation games per week, or 440 games total. Web-based cognitive training participation had a large range, since some participants played a lot (the program provided unlimited access to games) and others played none at all. On average, participants played 242.2 web-based cognitive training games (median 83, range 0-1926), but only 17.6% of participants completed 440 games.
Participants significantly improved in social functioning [t(16)=−4.20, p=.001, d= 1.02], trended for improvement in reaction time [t(15)=2.09, p=.054, d= .52] from baseline to end of treatment. No other measures significantly changed (Table 2). Fifteen of the 17 participants assessed at follow-up continued to meet CHR criteria and two experienced a remission of symptoms. No participants transitioned to full psychosis during the treatment and follow up period.
Table 2.
CEDAR Pilot + R34 Open Trial Baseline vs End of treatment Overlapping Assessments (paired t tests)
| Outcome Measure | Baseline M (SD) |
End of Treatment M (SD) |
BL vs ET P* Cohen’s d |
|---|---|---|---|
| Global Functioning Social Functioning (n=17) | 5.8 (1.1) | 6.6 (1.2) | **p=.001, d= 1.02 |
| Global Functioning Role Functioning (n=17) | 5.3 (2.0) | 6.1 (1.9) | p= .150, d= 0.37 |
| BACS Symbol Coding (n=16) | 63.3 (16.7) | 65.9 (15.7) | p=.314, d= 0.26 |
| ORM reaction time (n=16) | 241.0 (39.3) |
225.0 (29.8) | p=.054, d= 0.52 |
| MSCEIT (n=15) | 91.0 (10.1) | 91.8 (11.4) | p=.687, d= 0.11 |
Paired t-test performed using IBM SPSS Statistics for Windows, Version 21.0
Indicates significant at p<.01 level
Fourteen CLUES participants provided satisfaction data at the end of CLUES treatment. On a 0-4 scale ranging from “not at all” to “a lot”, 86% of participants rated CLUES as two or higher for helpfulness and 79% rated CLUES as a two or higher for how much they liked the program. In regard to specific components of CLUES, individual sessions and CLUES group were generally rated as the most helpful part of CLUES (modes both = 4), followed by web-based cognitive training and paired computer sessions (modes both = 1). In rating their perceived impact of CLUES on specific cognitive abilities, participants generally rated clues between two and three on the 0-4 scale. Several participants appreciated social interactions in CLUES. For example, one participant wrote, “The social component of CLUES [was] the most helpful, ranging from the group meetings to interacting with other workers and participants.” Several participants indicated they did not enjoy the computer games. One wrote, “They should find more exciting computer training games.”
Discussion
This study provides initial support for feasibility of CLUES for CHR youth. Participants attended at least 70% of group, individual and paired computer sessions and reported satisfaction with the program. Participants significantly improved in social functioning. Adherence to the web-based cognitive training portion of CLUES was poor, similar to other reported findings for web-based computer training in CHR youth. Piskulic et al.(2015) reported a high rate of attrition (48%) in a study using a web-based cognitive training program for youth at CHR, even though they paid participants each time they trained. Participants rated the cognitive training programs as boring; youth were hard to engage given availability of more engaging, commercial computer games. Paired computer session games found better adherence than the web-based games, perhaps due their social aspects (missing sessions meant standing up their partner and coach, participants anecdotally indicated enjoying interacting with their computer partner).
Although participants trended towards improvement in reaction time, other cognitive and social cognitive assessments did not change. This could reflect relatively few cognitive training sessions (average 17 clinic sessions +12 hours at home) or could indicate that CLUES sessions were more focused on improving social functioning rather than cognition. Additionally, CLUES participants were selected for impairments in motivation, organization or flexibility that impacted social or role functioning and the treatment specifically targeted these areas. They were not selected for impairments with neurocognition, so some CLUES participants had relatively good cognitive functioning even at baseline. Therefore, it may not be surprising that cognition did not improve following treatment.
Importantly, cognitive functioning did not decline. Of note, the goal of CLUES was not only to improve cognition but to prevent decline. Furthermore, none of 17 participants transitioned to full psychosis during CLUES intervention. The improvement in social functioning observed among CLUES participants is promising, given that CHR youth show significant social functioning difficulties, social functioning appears to be a predictor of later transition to psychosis (Addington et al., 2017), and that no treatments thus far have been associated with significant improvements in social functioning (Devoe et al., 2018).
While limited by the small sample size and the open label design, our preliminary results indicate that CLUES is feasible and shows promise in improving social functioning. However, further investigation is warranted in order to determine its efficacy. Future directions should include conducting a randomized controlled trial in order to compare the efficacy of CLUES to another intervention. Additionally, utilizing participants’ feedback about the likeability and helpfulness of different aspects of CLUES could be helpful in enhancing the program and maximizing engagement.
Supplementary Material
Acknowledgement:
All authors of this manuscript, “An Integrated Neurocognitive and Social-Cognitive Treatment for Youth at Clinical High Risk for Psychosis: Cognition for Learning and for Understanding Everyday Social Situations (CLUES)” have reviewed and approved this version being submitted. This is the authors’ original work and it has not been published or submitted for consideration of publication elsewhere.
Role of the Funding Source
Financial support for this work came from NIMH 1R34MH105596, the Sidney R. Baer, Jr. Foundation and the Massachusetts Department of Mental Health. Additionally, Lumos Labs provided a 50% discount ($749.38) for participant subscriptions used for web-based cognitive training and provided weekly usage reports to the study coordinators.
None of the funding sources played any role in the writing of this manuscript or in the decision to submit it for publication.
Financial support for this work came from NIMH 1R34MH105596, the Sidney R. Baer, Jr. Foundation and the Massachusetts Department of Mental Health. Additionally, Lumos Labs provided a 50% discount ($749.38) for participant subscriptions used for web-based cognitive training and provided weekly usage reports to the study coordinators.
Footnotes
Conflict of interest Statement
There are no known conflicts of interest associated with this publication and there has been no significant financial support for this work that could have influenced its outcome.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References:
- Addington J, Liu L, Perkins DO, Carrion RE, Keefe RSE, Woods SW, 2017. The role of cognition and social functioning as predictors in the transition to psychosis for youth with attenuated psychotic symptoms. Schizophr Bull 43(1), 57–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben-Yishay Y, 1981. Working approaches to remediation of cognitive deficits in brain damaged persons. New York University Medical Center, New York. [Google Scholar]
- Cornblatt BA, Auther AM, Niendam T, Smith CW, Zinberg J, Bearden CE, Cannon TD, 2007. Preliminary findings for two new measures of social and role functioning in the prodromal phase of schizophrenia. Schizophr Bull 33(3), 688–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cramer H, Lauche R, Haller H, Langhorst J, Dobos G, 2016. Mindfulness- and Acceptance-based Interventions for Psychosis: A Systematic Review and Meta-analysis. Glob Adv Health Med 5(1), 30–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devoe DJ, Farris MS, Townes P, Addington J, 2018. Interventions and social functioning in youth at risk of psychosis: A systematic review and meta-analysis. Early Interv Psychiatry. [DOI] [PubMed] [Google Scholar]
- Dweck CS, 1999. Self-theories: Their role in motivation, personality, and development. Psychology Press, Philadelphia, PA. [Google Scholar]
- Eack SM, Greenwald DP, Hogarty SS, Cooley S, DiBarry AL, Montrose DM, Keshavan MS, 2009. Cognitive enhancement therapy for early-course schizophrenia:effects of a two-year randomized controlled trial. Psychiatr Serv 60(11), 1468–1476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eack SM, Greenwald DP, Hogarty SS, Keshavan MS, 2010. One-year durability of the effects of cognitive enhancement therapy on functional outcome in early schizophrenia. Schizophr Res 120(1–3), 210–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eack SM, Hogarty GE, Greenwald DP, Hogarty SS, Keshavan MS, 2011. Effects of Cognitive Enhancement Therapy on Employment Outcomes in Early Schizophrenia: Results From a Two-Year Randomized Trial. Res Soc Work Pract 21(1), 32–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman-Yakoobian M, West ML, O’Donovan K, Gnong-Granato A, Woodberry KA, Zimmet S, Giuliano AJ, Keshavan MS, Seidman LJ, 2018. Center for Early Detection, Assessment, and Response to Risk: History, Description, and Future Directions. Harvard Review of Psychiatry 26(5), 274–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giuliano AJ, Mesholam-Gately RI, Sorenson SM, Woodberry KA, Seidman LJ, 2012. Neurocognition in the psychosis risk syndrome: a quantitative and qualitative review. Curr Pharm Des 18(4), 399–415. [DOI] [PubMed] [Google Scholar]
- Green MF, Hellemann G, Horan WP, Lee J, Wynn JK, 2012. From perception to functional outcome in schizophrenia: modeling the role of ability and motivation. Arch Gen Psychiatry 69(12), 1216–1224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green MF, Kern RS, Braff DL, Mintz J, 2000. Neurocognitive deficits and functional outcome in schizophrenia: are we measuring the “right stuff”? Schizophr Bull 26(1), 119–136. [DOI] [PubMed] [Google Scholar]
- Hayes SC, Strosahl KD, Wilson KG, 1999. Acceptance and Commitment Therapy: An experiential approach to behavior change. . The Guildford Press, New York, NY. [Google Scholar]
- Hogarty GE, Flesher S, Ulrich R, Carter M, Greenwald D, Pogue-Geile M, Keshavan MS, Cooley S, DiBarry AL, Garrett A, Parepally H, Zoretich R, 2004. Cognitive enhancement therapy for schizophrenia. Effects of a 2-year randomized trial on cognition and behavior. Arch Gen Psychiatry 61(9), 866–876. [DOI] [PubMed] [Google Scholar]
- Hogarty GE, Greenwald D, 2006. Cognitive Enhancement Therapy: The Training Manual. University of Pittsburgh Medical Center: Authors, Available through www.CognitiveEnhancementTherapy.com. [Google Scholar]
- Keefe RS, Goldberg TE, Harvey PD, Gold JM, Poe MP, Coughenour L, 2004. The Brief Assessment of Cognition in Schizophrenia: reliability, sensitivity, and comparison with a standard neurocognitive battery. Schizophr Res 68(2–3), 283–297. [DOI] [PubMed] [Google Scholar]
- Keshavan MS, DeLisi LE, Seidman LJ, 2011. Early and broadly defined psychosis risk mental states. Schizophr Res 126(1–3), 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keshavan MS, Hogarty GE, 1999. Brain maturational processes and delayed onset in schizophrenia. Development and psychopathology 11(3), 525–543. [DOI] [PubMed] [Google Scholar]
- Mayer JD, Salovey P, Caruso DR, Sitarenios G, 2003. Measuring emotional intelligence with the MSCEIT V2.0. Emotion 3, 97–105. [DOI] [PubMed] [Google Scholar]
- Mesholam-Gately RI, Giuliano AJ, Goff KP, Faraone SV, Seidman LJ, 2009. Neurocognition in First-Episode Schizophrenia: A Meta-Analytic Review. Neuropsychology 23(3), 315–336. [DOI] [PubMed] [Google Scholar]
- Miller TJ, McGlashan TH, Rosen JL, 2003. Prodromal assessment with the structured interview for prodromal syndromes and the scale of prodromal symptoms: predictive validity, interrater reliability, and training to reliability. Schizophr Bull 29, 703–715. [DOI] [PubMed] [Google Scholar]
- Niendam TA, Bearden CE, Johnson JK, McKinley M, Loewy R, O’Brien M, Nuechterlein KH, Green MF, Cannon TD, 2006. Neurocognitive performance and functional disability in the psychosis prodrome. Schizophrenia Research 84(1), 100–111. [DOI] [PubMed] [Google Scholar]
- Nuechterlein KH, Barch DM, Gold JM, Goldberg TE, Green MF, Heaton RK, 2004. Identification of separable cognitive factors in schizophrenia. Schizophr Res 72(1), 29–39. [DOI] [PubMed] [Google Scholar]
- Nuechterlein KH, Green MF, Kern RS, Baade LE, Barch DM, Cohen JD, Essock S, Fenton WS, Frese F.J.r., Gold JM, Goldberg T, Heaton RK, Keefe RS, Kraemer H, Mesholam-Gately RI, Seidman LJ, Stover E, Weinberger DR, Young AS, Zalcman S, Marder SR, 2008. The MATRICS Consensus Cognitive Battery, part 1: test selection, reliability, and validity. Am J Psychiatry 165(2), 203–213. [DOI] [PubMed] [Google Scholar]
- Piskulic D, Barbato M, Liu L, Addington J, 2015. Pilot study of cognitive remediation therapy on cognition in young people at clinical high risk of psychosis. Psychiatry Res 225(1–2), 93–98. [DOI] [PubMed] [Google Scholar]
- Schmidt SJ, Schultze-Lutter F, Schimmelmann BG, et al. , 2015. EPA guidance on the early intervention in clinical high risk states of psychoses. Eur Psychiatry 30, 388–404. [DOI] [PubMed] [Google Scholar]
- Stafford M, Jackson H, Mayo-Wilson E, Morrison AP, Kendall T, 2013. Early interventions to prevent psychosis: Systematic review and meta-analysis. British Medical Journal 346(fl85). [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Gaag M, Smit F, Bechdolf A, French P, Linszen DH, Yung AR, McGorry P, Cuijpers P, 2013. Preventing a first episode of psychosis: meta-analysis of randomized controlled prevention trials of 12 month and longer-term follow-ups. Schizophr Res 149(1–3), 56–62. [DOI] [PubMed] [Google Scholar]
- Wechsler D, 2001. Wechsler Test of Adult Reading: WTAR. The Psychological Corporation, San Antonio, TX. [Google Scholar]
- Wilkinson GS, Robertson GJ, 2006. Wide Range Achievement Test 4 Professional Manual. Psychological Assessment Resources, Lutz, FL. [Google Scholar]
- Woodberry KA, Shapiro DI, Bryant C, Seidman LJ, 2016. Progress and future directions in research on the psychosis prodrome: A review for clinicians. Harvard Review of Psychiatry 24(2), 87–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wykes T, Huddy V, Cellard C, McGurk SR, P C, 2011. A meta-analysis of cognitive remediation for schizophrenia: methodology and effect sizes. Am J Psychiatry 168(5), 472–485. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.