Abstract
Addicted drugs like nicotine affect autonomic nervous system that results in arrhythmia and other cardiovascular diseases. Notable effects of Zen meditation on autonomic nervous system have been reported during the past decade. Holistic Detox Association (HDA) in Taiwan offered Zen-meditation program to drug addicts as the core scheme among a variety of drug addiction treatments. This paper reports the results of quantifying the cardiorespiratory interactions and autonomic nervous system function to evaluate the on-site effect of Zen meditation on drug rehab. Methods and schemes for quantifying time-domain heart rate variability were employed to electrocardiograph and respiratory signals. Peak-valley method was developed to quantify the respiratory sinus arrhythmia (RSA) behavior. Poincaré Plot Analysis was adopted to evaluate the cardiorespiratory functioning. Among 18 voluntary drug addicts during the 10-minute Zen meditation session, about two-third subjects have significant improvement in autonomic nervous system function characterized by heart rate variability (SDNN, RMSSD and pNN50). Group average of RSA increases from 33.43 ms(Rest) to 69.14 ms(AR Zen meditation). Poincaré-plot analysis reveals the improvement of SD1, SD2 and SD2/SD1 by respectively 14.7%, 19.8% and 8.8%. The group averages of all the parameters exhibit significantly positive changes in the 10-minute session of abdominal-respiration Zen meditation. Even the subject with heart transplant showed the improvement of all the quantitative indicators during the AR Zen meditation.
Keywords: Cardiorespiratory interaction, Drug addiction, Heart rate variability, Respiratory sinus arrhythmia, Zen meditation
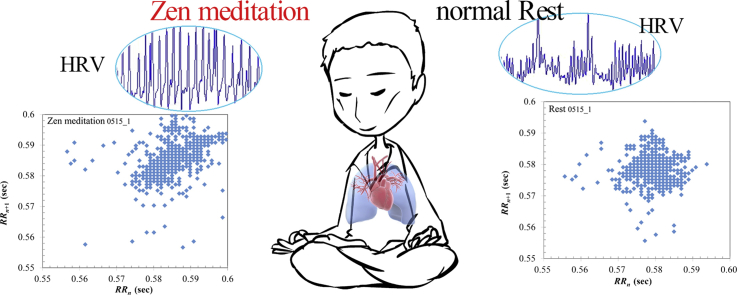
Graphical abstract
1. Introduction
Taiwan statistics about drug-related crimes showed an increase of 29.9% from 2014 to 2015, reported by Ministry of the Interior of Taiwan. The prison and jail surveys in US also revealed that the majority of offenders had either mental illness or substance use disorders.1 A number of different rehabilitation schemes for drug abusers have been reported since 1990s. Platt reported the success of vocational rehabilitation.2 In,3 effectiveness of drug abuse treatment program was evaluated by retention criterion. Long-term, integrated residential treatment was proposed to be helpful for individuals who did not respond to outpatient dual disorders interventions.4 Simpson and Sells analyzed the DARP (Drug Abuse Reporting Program) system containing ∼44,000 admissions and concluded the effectiveness of treatment in methadone maintenance, therapeutic communities, and outpatient drug-free programs in improving posttreatment performance with respect to drug use, criminality, and productive activities.5 In,6 McLellan et al. compared the efficacy of methadone hydrochloride therapy accompanied with counseling, medical care, or psychosocial services and concluded that significantly better outcomes in the group treated by enhanced methadone therapy with additional counseling and on-site medical/psychiatric, employment, and family therapy. During the past decade, intensive outpatient programs, as the emergent addict-rehab treatment of the 21th century, have been demonstrated to be as effective as inpatient treatment for most individuals.7 Olson and Lurigio reported the reduction of recidivism through the aftercare services for the releases who had been under the prison-based drug treatment during their imprisoned period.8 More publications were focused on the performance evaluation and comparison among different drug treatment programs.9,10
This paper presents our study of Zen-meditation effect on ANS (autonomic nervous system) balance and cardiorespiratory functioning for 18 voluntary participants under drug-rehab treatment. In the study, the ongoing physiological signals were recorded during the practice of HHIS (heart-to-heart imprint sealing) Zen meditation (Appendix). Signals recorded include electrocardiograph (ECG) and respiratory signals for further assessment of heart rate variability (HRV) and cardiorespiratory functioning.
The interaction between human cardiac and respiratory systems has been widely studied. These two systems act as two individual oscillators coupled by particular mechanisms. Respiratory sinus arrhythmia (RSA) demonstrates such kind of cardiorespiratory interactions. RSA is a natural variation in heart rate correlating with the respiratory cycle, that is, heart rate increases during inspiration and decreases during expiration. Consequently, RSA behavior is mostly correlated with the characteristic of HRV.11,12 The effects of various meditation techniques on RSA and HRV have been examined.13, 14, 15, 16, 17, 18 Major activities in LF ranges were reported in the study on Kundalini Yoga and Chinese Chi,14,15 Zazen meditation,16 and concentration meditation group.17 Nijjar addressed the significant changes in LF and HF norm as the indicator of improved sympatho-vagal balance.13
ROC Holistic Detox Association (HDA) is a nongovernmental organization in Taiwan which provides various types of support for drug rehabilitation since 2014. During the past year, HDA offered a series of programs beneficial for addicts to get their lives back in order. The lessons contain various activities, which are mainly the interaction with people, society, and the inner thoughts of addicts themselves. HHIS Zen-meditation practice, one of the core programs, is a healing scheme via brain-mind reformation rather than conventional medication or behavior control.
HHIS Zen meditation completely differs from those widely practiced meditation techniques. HHIS Zen follows the principle that heart dominates brain and mind, unlike the other meditations mainly based on body-mind intervention. Pioneering findings in scientific study of HHIS Zen meditation were reported in.19,20 Recently, more evidences revealed the heart-brain interactions significantly affected the health conditions.21 The heart is more than simply a blood pumping device. For thousands of years, Zen practitioners have been devoted their practice to disclosing the spiritual heart inside the organ heart.20 Through years of Zen-meditation practice, practitioners have their brain functions totally reformed into a so-called detached brain dominated by the spiritual heart. The heart-dominant state is activated by fetal-like respiration and ignition of mailuns locating at the glands or nerve plexuses. Cardiorespiratory functioning becomes important to explore the mechanism. Mailun-activation Zen meditation provides to the drug abusers an important scheme of rehabilitation by reforming the brain functioning.
2. Methods
While the program was underway, we collected the ECG and respiratory signals from the participants before and after a 20-minute practice of Zen meditation offered by the orthodox Zen Sect. Mailun-concentration Zen meditation was originally developed by the current Patriarch Wu Jue Miao Tian. The basic practice includes abdominal breathing and Mailun (particular energy spot) concentration to activate good potency beneficial to the body and mind. The program contains mindfulness training and Zen Meditation. Mindfulness training involves a series of practice including relaxation, breathing, mindfulness concentration and emotional management. The main idea of mindfulness training is to arouse the positive mood and emotion. Participants may accordingly refuse the drug and its negative effect on their own. Eighteen participants from Taipei District Prosecutors Office were all males (age range 21–47 years with statistics 32.8 ± 11.3 years). Subject 0515_1 had the heart transplant due to the severe heart failure caused by drug. Their participation in the experiment was completely voluntary. All participants signed the agreement form at their own free will. All procedures were consistent with the Declaration of Helsinki and were approved by the Institutional Review Board of National Chiao Tung University.
Experimental protocol involved two sessions: (Session I) relaxing, eyes-closed rest (10 min), and (Session II) abdominal-respiration (AR) Zen meditation (10 min). In Session II, drug-addict participants practiced Zen meditation with complete awareness and mindfulness on their abdominal respiration. NeXus-10 recording system (Mind Media B.V., The Netherlands) was employed to collect the ECG and respiratory signals, digitized at the sampling rate of, respectively, 256 Hz and 32 Hz.
To avoid muscular artefacts, ECG Lead II Chest Placement modified from the bipolar limb-lead II configuration was applied. Reference electrode is placed on the left mid-clavicular line, lead + is placed at the end of the left rib cage and aligned with the reference electrode, and lead − is placed on the right mid-clavicular line.
2.1. Evaluation of HRV parameters
Sympathetic nerve increases the heart rate (HR) and decreases HRV by stimulating the sinoatrial (SA) and atrioventricular (AV) nodes; while parasympathetic nerve slows down HR and increases HRV. Psychological and mental stress reduces HRV.22 Both physiological cardiovascular models and the development of new clinical characteristics benefit from HRV analyses.23
This study analyzed the time-domain HRV based on the statistical properties of the R-peak to R-peak (RR) intervals between successive normal heartbeats, called the normal-to-normal (NN) intervals. Consider a set of N's NN intervals, RRi, i = 1, …, N. The standard HRV parameters are computed by the following equations.24
Standard deviation of all NN intervals (msec):
| (1) |
where is the average of NN intervals.
Root mean square of differences between adjacent NN intervals (msec):
| (2) |
Percentage of number of pairs of adjacent NN intervals differing by more than 50 ms(%):
| (3) |
where NN50 is the number of pairs of adjacent intervals differing by more than 50 ms.
2.2. Quantification of RSA
RSA has been widely used as an index to signify the phenomenon of heart rate variation in accordance with respiration activity. In recent years, this theory was further expanded to encompass a wide range of hypotheses regarding physical, psychophysiological and even social functioning in humans.25 Although RSA decreases with age, adults in excellent cardiovascular health may have a more pronounced RSA. RSA also becomes less prominent in individuals with diabetes and cardiovascular disease.
Different methods for quantifying RSA have been proposed.26 Distinctions among these methods are mainly the assumption of RSA mechanism and its correlation with respiration. Time-domain RSA analysis evaluates the amplitude of heart-rate fluctuations regulated by the breathing cycle. This study employed the peak-valley method that computes the difference between the longest heartbeat interval during expiration () and the shortest heartbeat interval during inspiration ().27,28 At the jth respiratory cycle, RSA (msec) is quantified by
| (4) |
The percentage of normal RSA cycles (pRSA) proposed in this study indicates the probability of respiratory cycles that conform with the RSA behavior of increasing (decreasing) hear rate at inhalation (exhalation). Accordingly, pRSA (%) is the ratio of normal respiratory cycles to total respiratory cycles in a given time interval.
2.3. Poincaré plot analysis
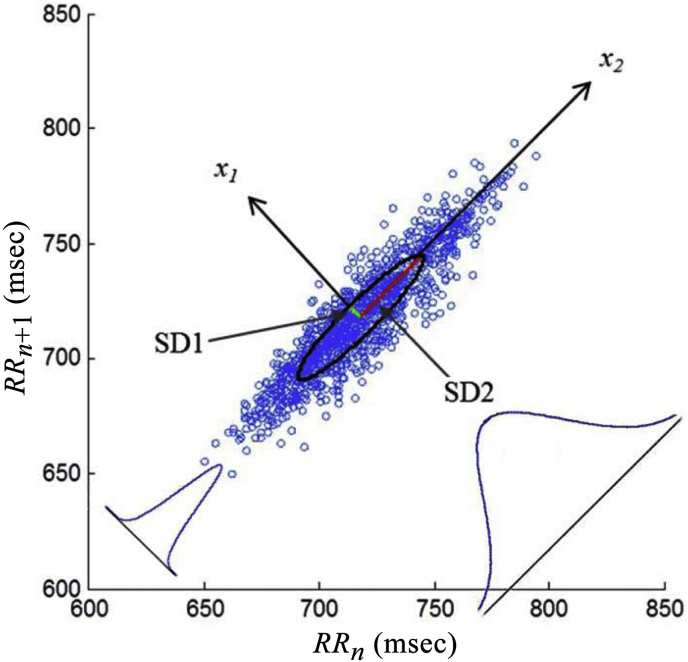
A Poincaré plot is a graph of aggregated, scattering dots (RRn, RRn+1) that sketches the succeeding RR interval (vertical coordinate) against the current RR interval (horizontal coordinate). Poincaré Plot Analysis (PPA) has become a popular method in HRV study due to its easily comprehensible mechanism and pictorial embedded features. PPA has been used in many clinical and physiological studies, mainly as a measure of autonomic modulation or randomness of the heart rate. Along the identity line of Poincaré plot, all points describe the consecutive cardiac beats of equal duration (RRn = RRn+1). The points above (beneath) the identity line, that is, RRn < RRn+1 (RRn > RRn+1), indicate the event of increasing (decreasing) cardiac interval.
The geometry of the Poincaré plot may carry important information of HRV. As illustrated in Fig. 1, the ellipse oriented by 45° is utilized to model the Poincaré-plot geometry.29 Three descriptors, SD1, SD2 and SD2/SD1, are evaluated.29,30 SD1 (SD2) is the standard deviation of the distribution of points projected on minor (major) axis (Fig. 1). HRV is often assessed by the power spectrum of the RR intervals (RRn), that is computed by the Fourier transform of the auto-covariance function of RRn. The auto-covariance function of RRn is computed by
| (5) |
where is the mean value of RR intervals. For stationary RR intervals, the auto-covariance function becomes
| (6) |
where γRR(m) is the autocorrelation function of RRn
| (7) |
Fig. 1.
The Poincaré plot of a 5-min ECG data. SD1 and SD2 are respectively the minor and major axis of an imaginary ellipse whose shape is visible in the plot.
Accordingly, SDNN can be computed by . The SD1 measure of Poincaré width can be related to the auto-covariance function by29,30
| (8) |
Similarly, the length of the Poincaré cloud (SD2) is
| (9) |
SD1 is usually interpreted as a measure of short-term HRV which is mainly caused by RSA. On the other hand, SD2 describes the long term HRV behavior. The ratio SD2/SD1 measures the balance between long-term and short-term HRV. The ratio greater than 1 (SD2 > SD1) indicates the state of sympathetic predominance; whereas a lower SD2/SD1 (∼1) reflects the increased parasympathetic or reduced sympathetic activity.
3. Results
Table 1 lists the average heart rate (HR), SDNN, RMSSD, and pNN50 in each Session. Two thirds of the participants have slower heart rate during the AR Zen meditation (Session II). Thirteen out of eighteen subjects have slower respiration in Session II. SDNN, as the time-domain index of ANS functioning, dramatically improves in transition from Rest to AR Zen meditation (group average increasing from 39.07 to 46.20, 18.3% increase). SDNN increases in 14 out of 18 participants. Group averages of RMSSD and pNN50 increase by 14.0% and 13.1%, respectively, in transition from Rest to AR Zen meditation. Student t-test reflects statistically significant difference between two sessions in the following parameters: respiration rate (p = .012), SDNN (p = .002), RMSSD (p = .044), and pNN50 (p = .064).
Table 1.
Average heart rate (beat/min), respiratory rate (breath/min), SDNN (msec), RMSSD (msec) and pNN50 (%) for each individual subject in Sessions I (Rest) and II (AR Zen meditation).
| Subject | Heart rate |
Respiratory rate |
SDNN |
RMSSD |
pNN50 |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| I Rest |
II AR |
I Rest |
II AR |
I Rest |
II AR |
I Rest |
II AR |
I Rest |
II AR |
|
| 1121_1 | 85.3 | 79.8 | 19.8 | 14.6 | 46.66 | 65.47 | 38.62 | 48.05 | 15.27 | 24.09 |
| 1205_1 | 63.6 | 60.6 | 17.6 | 18.0 | 63.79 | 71.98 | 54.17 | 60.20 | 32.95 | 37.62 |
| 1219_1 | 98.4 | 100.5 | 8.3 | 13.7 | 24.68 | 16.15 | 8.16 | 8.14 | 0.00 | 0.20 |
| 0130_1 | 79.9 | 82.4 | 8.7 | 5.5 | 29.88 | 35.16 | 18.92 | 17.93 | 1.03 | 1.75 |
| 0313_1 | 81.8 | 84.4 | 23.0 | 15.3 | 27.09 | 39.70 | 20.44 | 15.32 | 0.24 | 0.61 |
| 0327_1 | 62.8 | 60.1 | 14.0 | 6.6 | 97.22 | 107.64 | 71.04 | 90.53 | 36.03 | 42.40 |
| 0410_1 | 75.1 | 76.6 | 12.7 | 13.2 | 47.55 | 46.32 | 35.43 | 33.71 | 15.54 | 13.02 |
| 0417_1 | 99.2 | 91.8 | 8.2 | 14.5 | 35.07 | 44.91 | 14.48 | 16.70 | 0.86 | 1.11 |
| 0424_1 | 87.3 | 84.9 | 16.7 | 8.3 | 10.78 | 14.83 | 8.71 | 7.85 | 0.12 | 0.00 |
| 0424_2 | 74.0 | 71.7 | 18.1 | 10.4 | 54.30 | 65.51 | 37.53 | 43.41 | 8.28 | 18.16 |
| 0515_1 | 103.6 | 102.7 | 24.9 | 18.2 | 4.07 | 5.72 | 5.75 | 7.65 | 0.00 | 0.10 |
| 0515_2 | 83.3 | 81.1 | 16.0 | 15.0 | 160.28 | 191.84 | 257.24 | 299.22 | 81.25 | 76.80 |
| 0604_1 | 108.3 | 106.6 | 25.9 | 24.6 | 5.33 | 8.46 | 2.61 | 3.20 | 0.00 | 0.10 |
| 0604_2 | 101.7 | 99.2 | 21.6 | 9.7 | 28.26 | 24.46 | 26.01 | 15.31 | 1.90 | 0.41 |
| 0618_1 | 109.5 | 115.4 | 15.7 | 14.0 | 13.70 | 20.15 | 6.15 | 8.37 | 0.00 | 0.26 |
| 0618_2 | 90.2 | 89.6 | 17.9 | 14.8 | 18.86 | 24.98 | 10.10 | 14.72 | 0.00 | 0.56 |
| 0721_1 | 91.3 | 92.1 | 14.6 | 19.2 | 14.81 | 30.86 | 7.26 | 20.68 | 0.00 | 1.56 |
| 0721_2 | 94.8 | 93.7 | 14.7 | 7.9 | 20.98 | 17.53 | 9.46 | 9.35 | 0.00 | 0.00 |
| Average | 88.3 | 87.4 | 16.6 | 13.5 | 39.07 | 46.20 | 35.11 | 40.02 | 10.75 | 12.15 |
The results demonstrate the remarkable effect of 10-minute AR Zen meditation on slowing down the heart rate and respiration, yet, boosting up the ANS functioning. According to the subjects' self-narration in the post-experiment interview, they (16 out of 18) were able to experience the cleansing and rejuvenation of body and mind after the practice of AR Zen meditation. Some other case reports on Zen meditation experiences include: scalp tingling, whole-body heating, lightning in the head, halo light surrounding the body, cool and refreshing of the body, etc.
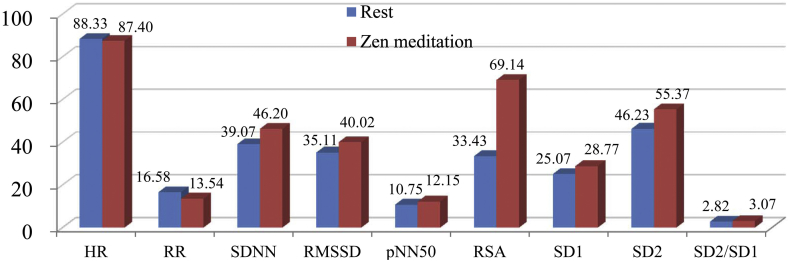
RSA performance quantified by equation (4) reveals an improvement by 106.8%, group average increasing from 33.43 ms(Rest) to 69.14 ms(AR Zen meditation). Individual RSA parameter raises up in 16 out of 18 subjects. In Poincaré plot analysis, both SD1 and SD2 increase in transition from Rest to AR Zen meditation. Group average of SD1 (SD2) increases from 25.07 ms(46.23 ms) to 28.77 (55.37), improved by 14.7% (19.8%). Student t-test exhibits statistically significant difference of SD1 (p = .039) and SD2 (p = .002) between two sessions. The ratio SD2/SD1 increases in Session AR Zen meditation in 11 out of 18 subjects. Group average of SD2/SD1 increases from 2.82 to 3.07 (8.8% increase). By excluding two extremal cases in the group, group average of SD1 (SD2) increases from 16.75 ms(43.37 ms) to 18.89 (51.64), improved by 12.8% (19.1%). The overall comparison is shown in Fig. 2. The bar chart illustrates the group averages of heart rate (HR in beat/min), respiratory rate (RR in breath/min), SDNN (msec), RMSSD (msec), pNN50 (%), RSA (msec), SD1 (msec), SD2 (msec) and SD2/SD1.
Fig. 2.
Group averages of each parameter (HR, RR, SDNN, RMSSD, pNN50, RSA, SD1, SD2 and SD2/SD1) in the session of Rest and AR Zen meditation.
4. Discussion
The human brain is still operating on the basis of ancient “fight-or-flight” response activated by amygdala and possibly recorded by hippocampus. The amygdala once in response to emotions tends to dominate the entire brain functioning. It is the collaboration of the emotion center and reward circuitry in human brain that allows addiction to intrude into the mind and lifestyle. HHIS Zen-meditation practitioners further realize the inherent causation law conducted by amygdala and hippocampus that encode (or, are programmed by) the subconscious and manas (subliminal consciousness). The functional characteristics of amygdala and hippocampus accordingly affect the behavioral traits and personality. Through Zen meditation, practitioners regulate the abdominal breathing to make the breathing slowly and deeply till entering into so-called fetal breathing. Such breathing manner rapidly initiates the process of transcending all sensory and conscious states. The process converts the clinging brain into tranquil, detached brain.
Since 1990s, a large number of practitioners have proved the efficacy of HHIS Zen meditation (Appendix) in treating many chronic diseases, infections, acute symptoms as well as mental and psychological problems. Hence, more people began to practice HHIS Zen meditation in Taiwan. Various cases of the effective treatment and health benefit of Zen meditation arouse our interest in the physiological, mental, and spiritual states during Zen meditation. In the course of investigating this particular practice, we disclose the remarkable distinctions of Zen meditation from those worldwide popular meditation practices including Yoga and transcendental meditation (TM) from India, Japanese Zen, and Tibetan Buddhism. Briefly, Zen meditation follows the “heart-dominating” principle while meditations are mostly “mind-cultivating” practices.
Under the supervision of well experienced Zen-meditation lecturers, the drug addicts and inmates from Taipei District Prosecutors Office have been practicing HHIS Zen meditation for two years. The accumulated effect helps many of them successfully go through difficulties during the detox treatment and recovery process. The main mechanism is based on the reformation of brain functioning. The hijacked pleasure-reward pathways becomes dominant over the executive power of the frontal lobes. HHIS Zen meditation remarkably enhances the hypothalamus and frontal-lobe functioning.28 Drug addicts accordingly strengthen their self-control willpower to overcome the addiction.
5. Conclusions
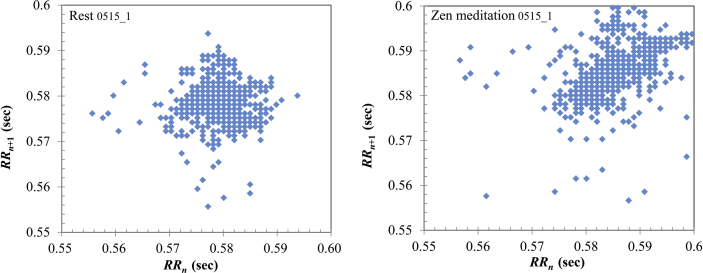
This paper presents our results of scientific study of the on-site effect of Zen-meditation practice on cardiorespiratory interactions and ANS functioning that may reflect both the physiological and psychological health conditions. The group averages of all the parameters exhibit significantly positive changes in the 10-minute session of abdominal-respiration Zen meditation. Even the participant with heart transplant showed the improvement of the following indicators during the AR Zen meditation: heart rate (103.6 → 102.7), respiration rate (24.9 → 18.2), SDNN (4.07 → 5.72), RMSSD (5.75 → 7.65), pNN50 (0.00 → 0.10), SD1 (4.08 → 5.47), SD2 (4.03 → 5.78), and SD2/SD1 (0.98 → 1.06). The pictorial illustration of Poincaré plot in Fig. 3 further demonstrates the remarkable improvement of cardiorespiratory functioning during the 10-minute abdominal-respiration Zen meditation.
Fig. 3.
Poincaré plot for subject 0515_1 with heart implant (a) in session I (normal rest), and (2) in session II (abdominal-respiration Zen meditation).
Conflicts of interest
The authors declare no conflict of interest.
Acknowledgement
This work was supported by the Ministry of Science and Technology of Taiwan under Grant MOST 104-2221-E-009-189-MY2. We greatly appreciate the kind support of the probation officers of Taipei District Prosecutors Office.
Footnotes
Peer review under responsibility of The Center for Food and Biomolecules, National Taiwan University.
Appendix.
HHIS Zen meditation was conveyed to China in 470–478 by patriarch Bodhidharma and then to Taiwan about one hundred years ago by the 84th patriarch Jing Zai. Current patriarch is master Wu Jue Miao Tian who firstly disclosed the ten mailun system.20 Zen-meditation practitioners evoke the invaluable potency of ten mailuns for driving and energizing the meridian system (qi-flow channels), nervous system, circulatory system, and many other organ systems. Chan Ding based on a more natural and intrinsic scheme leads to modulations of neural activity in frontal-central and temporal-parietal regions for launching for macrocosmic realm and transcending experiences. Intensively continuous focus on ChanXin (the third ventricle) may harmonize all the brain neurons in the way that brain becomes more tranquil and pure at every moment. This process of brain reformation substantially changes not only the physiological functioning of the brain but the mental, emotional, and psychological traits. Practitioners gradually reach the state of internal mental serenity with blissful spirit all the time.
References
- 1.Banerjee K. The changing landscape for substance use treatment in the U.S. J Drug Abuse. 2016;2(3):20. [Google Scholar]
- 2.Platt J.J. Vocational rehabilitation of drug abusers. Psychol Bull. 1995;117(3):416–433. doi: 10.1037/0033-2909.117.3.416. [DOI] [PubMed] [Google Scholar]
- 3.Simpson D.D., Joe G.W., Rowan-Szal G.A., Greener J.M. Drug abuse treatment process components that improve retention. J Subst Abuse Treat. 1997;14(6):565–572. doi: 10.1016/s0740-5472(97)00181-5. [DOI] [PubMed] [Google Scholar]
- 4.Drake R.E., Mueser K.T., Brunette M.F., McHugo G.J. A Review of treatments for people with severe mental illnesses and Co-Occurring substance use disorders. Psychiatr Rehabil J. 2004;27(4):360–374. doi: 10.2975/27.2004.360.374. [DOI] [PubMed] [Google Scholar]
- 5.Simpson D.D., Sells S.B. Effectiveness of treatment for drug abuse: an overview of the DARP research program. Adv Alcohol Subst Abuse. 1982;2(1):7–29. [Google Scholar]
- 6.McLellan A.T., Arndt I.O., Metzger D.S., Woody G.E., O'Brien C.P. The Effects of psychosocial services in substance abuse treatment. J Addict Nurs. 1993;5(2):38–47. [PubMed] [Google Scholar]
- 7.McCarty D., Braude L., Lyman D.R. Substance abuse intensive outpatient programs: assessing the evidence. Psychiatr Serv. 2014;65(6):718–726. doi: 10.1176/appi.ps.201300249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Olson D.E., Lurigio A.J. The long-term effects of prison-based drug treatment and aftercare services on recidivism. J Offender Rehabil. 2014;53(8):600–619. [Google Scholar]
- 9.Hser Y.I., Evans E., Huang D., Anglin D.M. Relationship between drug treatment services, retention, and outcomes. Psychiatr Serv. 2004;55(7):767–774. doi: 10.1176/appi.ps.55.7.767. [DOI] [PubMed] [Google Scholar]
- 10.Simpson D.D. A conceptual framework for drug treatment process and outcomes. J Subst Abuse Treat. 2004;27(2):99–121. doi: 10.1016/j.jsat.2004.06.001. [DOI] [PubMed] [Google Scholar]
- 11.Chen Z., Brown E.N., Barbieri R. Assessment of autonomic control and respiratory sinus arrhythmia using point process models of human heart beat dynamics. IEEE Trans Biomed Eng. 2009;56:1791–1802. doi: 10.1109/TBME.2009.2016349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Massagram W., Lubecke V.M., Host-Madsen A., Boric-Lubecke O. Assessment of heart rate variability and respiratory sinus arrhythmia via Doppler radar. IEEE Trans Microw Theor Tech. 2009;57:2542–2549. [Google Scholar]
- 13.Nijjar P.S., Puppala V.K., Dickinson O. Modulation of the autonomic nervous system assessed through heart rate variability by a mindfulness based stress reduction program. Int J Cardiol. 2014;177(2):557–559. doi: 10.1016/j.ijcard.2014.08.116. [DOI] [PubMed] [Google Scholar]
- 14.Peng C.K., Mietus J.E., Liu Y. Exaggerated heart rate oscillations during two meditation techniques. Int J Cardiol. 1999;70:101–107. doi: 10.1016/s0167-5273(99)00066-2. [DOI] [PubMed] [Google Scholar]
- 15.Peng C.K., Henry I.C., Mietus J.E. Heart rate dynamics during three forms of meditation. Int J Cardiol. 2004;95:19–27. doi: 10.1016/j.ijcard.2003.02.006. [DOI] [PubMed] [Google Scholar]
- 16.Cysarz D., Büssing A. Cardiorespiratory synchronization during Zen meditation. Eur J Appl Physiol. 2005;95:88–95. doi: 10.1007/s00421-005-1379-3. [DOI] [PubMed] [Google Scholar]
- 17.Phongsuphap S., Pongsupap Y., Chandanamattha P., Lursinsap C. Changes in heart rate variability during concentration meditation. Int J Cardiol. 2008;130:481–484. doi: 10.1016/j.ijcard.2007.06.103. [DOI] [PubMed] [Google Scholar]
- 18.Olex S., Newberg A., Figueredo V.M. Meditation: should a cardiologist care? Int J Cardiol. 2013;168:1805–1810. doi: 10.1016/j.ijcard.2013.06.086. [DOI] [PubMed] [Google Scholar]
- 19.Wu S.D., Lo P.C. Cardiorespiratory phase synchronization during normal rest and inward-attention meditation. Int J Cardiol. 2010;141:325–328. doi: 10.1016/j.ijcard.2008.11.137. [DOI] [PubMed] [Google Scholar]
- 20.Lo P.C., Huang M.L. Exploring preventive power of ten-mailuns actuation in Chan Ding. Int J Prevent Med Res. 2015;1:27–34. [Google Scholar]
- 21.Thayer J.F., Ahs F., Fredrikson M., Sollers J.J., Wager T.D., 3rd A meta-analysis of heart rate variability and neuroimaging studies: implications for heart rate variability as a marker of stress and health. Neurosci Biobehav Rev. 2012;36:747–756. doi: 10.1016/j.neubiorev.2011.11.009. [DOI] [PubMed] [Google Scholar]
- 22.Corrales M., Torres B., Esquivel A., Salazar M., Orellana J. Normal values of heart rate variability at rest in a young, healthy and active Mexican population. Health. 2012;4:377–385. [Google Scholar]
- 23.Sassi R., Cerutti S., Lombardi F. Advances in heart rate variability signal analysis: joint position statement by the e-Cardiology ESC Working Group and the European Heart Rhythm Association co-endorsed by the Asia Pacific Heart Rhythm Society. Europace. 2015;17:1341–1353. doi: 10.1093/europace/euv015. [DOI] [PubMed] [Google Scholar]
- 24.Camm A.J., Malik M., Bigger J.T. Heart rate variability: standards of measurement, physiological interpretation and clinical use. Task force of the European society of cardiology and the North American Society of Pacing and Electrophysiology. Circulation. 1996;93:1043–1065. [PubMed] [Google Scholar]
- 25.Sahar T., Shalev A.Y., Porges S.W. Vagal modulation of responses to mental challenge in posttraumatic stress disorder. Biol Psychiatr. 2001;49:637–643. doi: 10.1016/s0006-3223(00)01045-3. [DOI] [PubMed] [Google Scholar]
- 26.Denver J.W., Reed S.F., Porges S.W. Methodological issues in the quantification of respiratory sinus arrhythmia. Biol Psychol. 2007;74:286–294. doi: 10.1016/j.biopsycho.2005.09.00. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Grossman P., Stemmler G., Meinhardt E. Paced respiratory sinus arrhythmia as an index of cardiac parasympathetic tone during varying behavioral tasks. Psychophysiology. 1990;27:404–416. doi: 10.1111/j.1469-8986.1990.tb02335.x. [DOI] [PubMed] [Google Scholar]
- 28.Lo P.C., Huang M.L. Scientific propositions for brain reformation by mailun chan ding. Int J Electr Electron Eng (IJEEE) IASET. 2015;4(4):9–26. [Google Scholar]
- 29.Brennan M., Palaniswami M., Kamen P. Do existing measures of Poincare plot geometry reflect nonlinear features of heart rate variability? IEEE Trans Biomed Eng. 2001;48:1342–1347. doi: 10.1109/10.959330. [DOI] [PubMed] [Google Scholar]
- 30.Brennan M., Palaniswami M., Kamen P. Poincare plot interpretation using a physiological model of HRV based on a network of oscillators. Am J Physiol Heart Circ Physiol. 2002;283:H1873–H1886. doi: 10.1152/ajpheart.00405.2000. [DOI] [PubMed] [Google Scholar]