INTRODUCTION
West Virginia leads the USA in opioid overdoses, with a rate more than three times the national average.1 Post-overdose medications for opioid use disorder (MOUD) are protective against future deaths,2 yet are infrequently prescribed.2–4
Mental health disorders increase opioid overdose risk.5 Given the substantial burden of psychiatric comorbidities among people who overdose, it is important to understand how both MOUD and treatment for co-occurring mental health conditions change following overdoses.
METHODS
We obtained West Virginia Medicaid claims data for individuals enrolled under the Affordable Care Act expansion from 2014 to 2016. Opioid overdoses were identified using diagnosis codes for opioid poisoning (965.00-965.02, 965.09, E850.0-E850.2, appropriate T40 codes) as defined by ICD-9/10.6 Office visits (99x) for opioid use disorder (OUD) (304.00-304.03, 305.50-305.53, F11x) and counseling (H0004, H0031, H0036, H0040, H2036, 90791, 90792, 908x) and diagnoses for mental health conditions were determined using ICD-9/10 and the Current Procedural Terminology codes. Prescription drugs were classified using the First Data Bank three-digit hierarchical ingredient code. The sample was restricted to people continuously Medicaid-enrolled for 6 months prior to and 12 months following an overdose. Paired t tests were used to compare individual receipt of services and medications in months 1–3 prior to overdose versus other 3-month segments post-overdose. Unadjusted graphical displays were created to provide more detail on month-level trends. Analyses were conducted using STATA (StataCorp), Version 15. This study was exempted by the Johns Hopkins University Institutional Review Board.
RESULTS
Our sample included 301 people enrolled in West Virginia Medicaid who had a non-fatal overdose in 2014–2015. The sample was 60% male and 91% non-Hispanic White with mean age of 34.5 years; 54% of people had a diagnosis of depression, anxiety disorder, bipolar disorder, or schizophrenia (not shown).
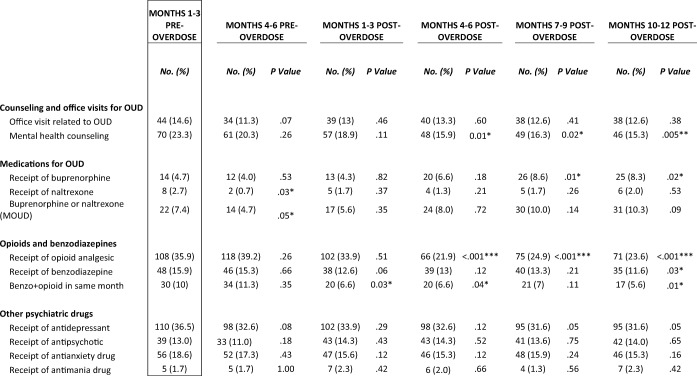
By 12 months post-overdose, individuals were more likely to receive buprenorphine (4.7% versus 8.3%, P = .02) and less likely to receive opioid analgesics (35.9% versus 23.6%, P < .001), or benzodiazepines (15.9% versus 11.6%, P = .03), compared to the 3 months prior to overdose. They were also less likely to receive mental health counseling (23.3% versus 15.3%, P = < .01). Differences were not significant for OUD office visits and receipt of naltrexone, antidepressants, antipsychotics, antianxiety, or antimania drugs (Table 1).
Table 1.
Services and Medications Pre- and Post-opioid Overdose by Time Segment
N = 301 non-fatal opioid overdose patients. Analysis uses West Virginia Medicaid claims data for individuals enrolled under the Affordable Care Act expansion from 2014 to 2016. Month 0 represents month of overdose. Percentages represent percent of individuals with receipt of any drug/service in time segment. Paired t tests compare individual receipt of services and medications in months 1–3 prior to overdose versus other 3-month segments post-overdose. Overdose poisoning codes = 965.00-965.02, 965.09, E850.0-E850.2, T40.yX1A, T40.yX1D, T40.yX1S, T40.yX4A, T40.yX4D, T40.yX4S, T40.yS2A, T40.yX2A, T40.601A, T40.601D, T40.601S, T40.604A, T40.604D, T40.604S, T40.691A, T40.691D, T40.691S, T40.694A, T40.694D, T40.694S; y = 0, 1, 2, 3, 4, 6. Opioid use disorder (OUD) codes = 304.00-304.03, 305.50-305.53, F11x. Office visit codes = 99x. Mental health counseling codes = H0004, H0036, H0031, H0040, H2036, 90791-2, 908x. Buprenorphine HIC = H3W. Naltrexone HIC = H3T. Opioid analgesic HIC = H3x except H3C, H3D, H3E, H3F, H3I, H3K, H3L, H3O, H3T, H3V, H3W, H3Y. Benzodiazepine HIC = H2F and “alprazozolam,” “lorazepam,” “clonazepam,” “diazepam,” “bromazepam.” Antidepressant HIC = H2S, H2U, H2W, H7B, H7C, H7D, H8P, H8T. Antipsychotic HIC = H2G, H7O, H7P, H7R, H7S, H7T, H7U, H7X, H8W. Antianxiety HIC = H2F. Antimania HIC = H2M. Drug claims without HIC codes were labeled using list of drug names generated from HIC algorithm for that drug. Proportions were compared using paired t tests. P value < .05*, < .01**, < .001**
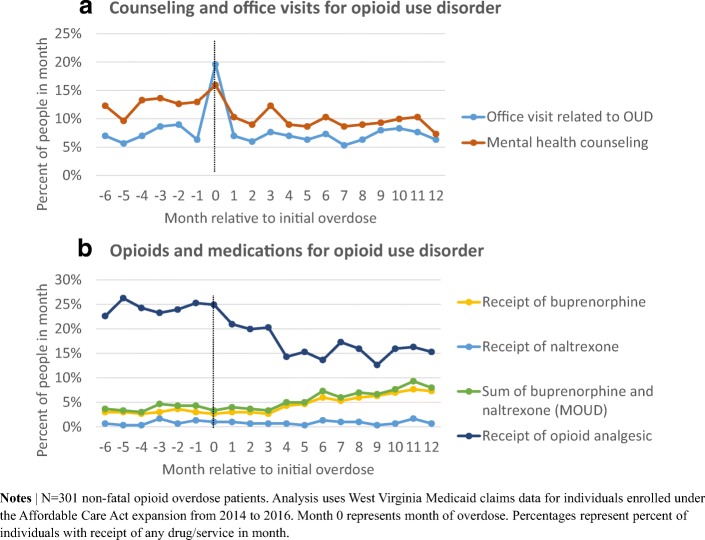
As month-level unadjusted analysis shows, OUD office visits spiked in the month of overdose, but then resumed pre-overdose trends (Fig. 1). In the 6 months after a non-fatal overdose, the proportion of people receiving buprenorphine increases by approximately 0.5 percentage points per month, while the proportion of people receiving opioid analgesics decreases by approximately 1.2 percentage points per month. At 12 months post-overdose, 7.3% of people received buprenorphine and 15.3% received opioid analgesics.
Figure 1.
Monthly receipt of services and medications pre- and post-opioid overdose.
DISCUSSION
Focusing on the state with the highest overdose rate, we find that use of buprenorphine significantly increased after a non-fatal overdose, but remained very low. Less than 10% of people every month post-overdose received MOUD or mental health counseling, which is below rates reported in other states.2, 3 In our analysis, MOUD only includes buprenorphine and naltrexone because West Virginia Medicaid did not cover methadone. Despite high rates of mental health comorbidities, people saw little to no change in receipt of counseling or medications for OUD or mental health conditions post-overdose.
With less than 10% of people receiving MOUD post-overdose among West Virginia Medicaid enrollees, a non-fatal overdose presents a major, under-utilized opportunity to increase treatment for opioid use disorder. Given the high burden of psychiatric comorbidities and the role of counseling in medication-assisted treatment for opioid use disorder, low rates of and declines in mental health counseling post-overdose also presents an important opportunity to improve treatment for people who experience an opioid overdose. Our study is the first to investigate changes in treatment for psychiatric comorbidities following a non-fatal overdose. Limitations of the study include restriction to those meeting continuous Medicaid eligibility requirements and inability of claims data to capture care not billed. Efforts to reduce risk of complications post-overdose should strive for adequate use of both MOUD and treatments for psychiatric conditions that are highly comorbid with OUD.
Acknowledgements
Funding disclosure: Dr. Saloner receives funding from the National Institute on Drug Abuse (K01 DA042139) and Dr. Stein receives funding from the National Institute on Drug Abuse (P50DA046351, R01DA045800-01).
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.National Institute on Drug Abuse. West Virginia Opioid Summary: Opioid-Related Overdose Deaths.; 2018. https://www.drugabuse.gov/drugs-abuse/opioids/opioid-summaries-by-state/west-virginia-opioid-summary. Accessed 6 November 2018.
- 2.Larochelle MR, Bernson D, Land T, et al. Medication for opioid use disorder after nonfatal opioid overdose and association with mortality: a cohort study. Ann Inter Med. 2018. [DOI] [PMC free article] [PubMed]
- 3.Frazier W, Cochran G, Lo-Ciganic W-H, et al. Medication-assisted treatment and opioid use before and after overdose in pennsylvania medicaid. JAMA. 2017;318(8):750–752. doi: 10.1001/jama.2017.7818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Larochelle MR, Liebschutz JM, Zhang F, Ross-Degnan D, Wharam JF. Opioid prescribing after nonfatal overdose and association with repeated overdose: a cohort study. Ann Intern Med. 2016;164(1):1. doi: 10.7326/M15-0038. [DOI] [PubMed] [Google Scholar]
- 5.Bohnert ASB, Ilgen MA, Ignacio RV, McCarthy JF, Valenstein M, Blow FC. Risk of death from accidental overdose associated with psychiatric and substance use disorders. Am J Psychiatry. 2012;169(1):64–70. doi: 10.1176/appi.ajp.2011.10101476. [DOI] [PubMed] [Google Scholar]
- 6.Moore B, Barrett M. Case Study: Exploring How Opioid-Related Diagnosis Codes Translate From ICD-9-CM to ICD-10-CM. U.S. Agency for Healthcare Research and Quality; 2017. https://www.hcup-us.ahrq.gov/reports/methods/methods.jsp. Accessed 6 November 2018.