Abstract
Background
Disparities in health outcome exist among patients according to socioeconomic status. However, little is known regarding the differences in healthcare experiences across the various levels of income of patients. In a nationally representative US adult population, we evaluate the differences in healthcare experiences based on patient level of income.
Objectives
To evaluate the differences in patient healthcare experiences based on level of income.
Patients and Methods
We identified 68,447 individuals (mean age, 48 ± 18 years; 55% female) representing 176.8 million US adults, who had an established healthcare provider in the 2010–2013 Medical Expenditure Panel Survey cohort. This retrospective study examined the differences in all five patient-reported healthcare experience measures (access to care, provider responsiveness, patient-provider communication, shared decision-making, and patient satisfaction) under the Consumer Assessment of Healthcare Providers and Systems (CAHPS) survey. We examined the relationship between patient income and their healthcare experience.
Results
Overall, 32% of the study participants were high-income earners while 23% had very-low income. Lower income was consistently associated with poor patient report on healthcare experience. Compared with those with high income, very-low-income-earning participants had 1.63 times greater odds (OR 1.63, 95% CI 1.45–1.82) of experiencing difficulty accessing care, had 1.34 times higher odds (OR 1.34, 95% CI 1.25–1.45) of experiencing poor communication, had higher odds (OR 1.68, 95% CI 1.46–1.92) of experiencing delays in healthcare delivery, and were more likely to report poor provider satisfaction (OR 1.48, 95% CI 1.37–1.61).
Conclusion
Lower income-earning patients have poorer healthcare experience in all aspects of access and quality of care. Targeted policies focusing on improving communication, engagement, and satisfaction are needed to enhance patient healthcare experience for this vulnerable population.
Electronic supplementary material
The online version of this article (10.1007/s11606-019-04848-4) contains supplementary material, which is available to authorized users.
KEY WORDS: patient-reported experience, quality of care, socioeconomic disparities
INTRODUCTION
Patient-centered care as evidenced by an improvement in patient report on healthcare experience has been identified by the Department of Health and Human Services (DHHS) as one of the strategies vital to the improvement of healthcare delivery and outcomes.1 While there may have been substantial improvements in care and outcomes, major health disparities continue to exist, particularly for patients with limited economic resources.2 Compared with high-income adults, those with limited financial resources have a fourfold higher rate of poor patient-reported health status.3, 4 As a part of its Healthy People 2020 initiative, the US DHHS has focused on eliminating healthcare disparities as one of its major objectives for the year 2020.5 Despite significant emphasis on understanding the socioeconomic differences (particularly differences in the level of income) in health report and outcome, the factors underlying such differences are poorly understood.
Patient experience with the health system especially among the vulnerable low-income population and their perception of the care received remain a critically important, yet poorly understood aspect of healthcare delivery. The Consumer Assessment of Healthcare Provider and Systems (CAHPS) survey, which assesses patient healthcare experiences, provides an opportunity to understand the existing disparities in healthcare quality and delivery.
A few studies have suggested an association between some socioeconomic factors and some of the individual domains of patient experience.6, 7 However, insights into all domains of patient-reported healthcare experiences and the influence of an individual’s level of income on these matrices remain relatively scarce. In an attempt to bridge this knowledge gap, using a nationally representative sample of US adults, we sought to explore the differences in various aspects of healthcare experience (access to care, provider responsiveness, patient-provider communication, shared decision-making, and patient satisfaction) across different patient income groups.
METHODS
We used data from the Medical Expenditure Panel Survey (MEPS) 2010–2013 which is compiled by the Agency for Healthcare Research and Quality.8 The MEPS has several components, one of which is the household component, reported annually and is nationally representative of the non-institutionalized US civilian population. It contains de-identified data from samples drawn from individuals who responded to the previous year’s National Health Interview Survey, conducted by the National Center for Health Statistics.9 Each year, a new panel of households is sampled and the data for each panel are gathered in five rounds of interviews over two and half years.9 Variance estimation stratum and person weights are assigned to reflect survey non-response and population estimates from the respondents surveyed.10, 11
Study Population
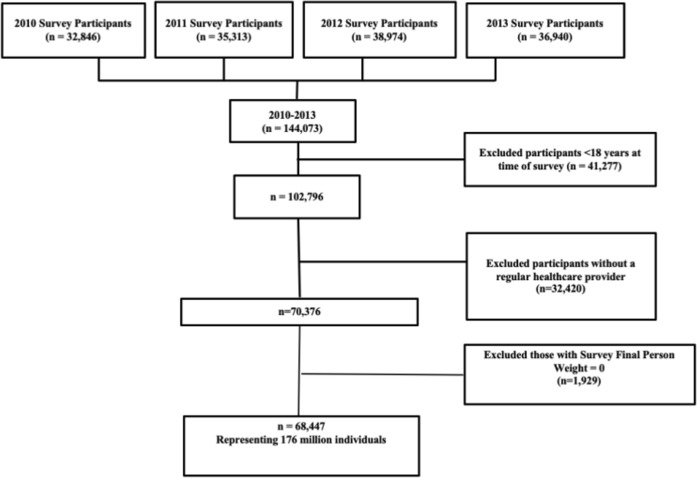
The MEPS dataset from 2010 to 2013 contains 144,073 observations. In our study, we included all individuals ≥ 18 years old and had a positive sampling weight (for national representativeness). This study was designed to capture income-level differences in patient-reported healthcare experience, which may be influenced by the interaction between patients and their healthcare providers. We therefore excluded individuals without a regular healthcare provider. Overall, the study population consisted of 68,447 individuals representing an estimated 176.8 million adults with an established healthcare provider (Fig. 1). According to the US DHHS guidelines, since MEPS is a de-identified publicly available dataset, this study did not require institutional review board approval.12
Figure 1.
Flow chart of study participant selection process.
Study Variables and Outcomes
We used the Andersen’s behavioral model of health services—a popular framework to assess access to healthcare—to select variables that could influence healthcare experience. This is a multilevel model that incorporates both individual and contextual determinants of health, classifying these factors into three major categories (predisposing, enabling, and need factors).13Predisposing factors include the socio-demographic characteristics. Enabling factors include insurance coverage, possession of a regular source of healthcare, and healthcare access. Need factors focus on an individual’s assessment and perception of health and the need for medical care.13 We used level of income as the independent variable. The outcome of interest focused on aspects of need factors including (1) consumer access to healthcare provider; (2) provider responsiveness; (3) patient-provider communication; (4) shared decision-making; and (5) satisfaction with healthcare.
The level of income of the participants was inferred based on family income as a proportion of federal poverty level (FPL). The FPL is a metric released every year by the DHHS as a measure of income and it is used to evaluate the eligibility of individuals for government insurance programs. The information on poverty status was derived from MEPS participant-reported household income, stratified into poor/very-low income (< 100 to < 125% FPL), low income (125 to < 200% FPL), middle income (200 to < 400% FPL), and high income (≥ 400% of FPL).
We collected socio-demographic information from the MEPS full year consolidated file. The burden of comorbid conditions was estimated using the grouped Charlson Comorbidity Index, which has been extensively described elsewhere.14, 15
The following components of patient experience were assessed using questions from the CAHPS survey, listed on Table e1, as published by the AHRQ researchers on the MEPS website.8
Access to Healthcare Provider
To assess the quality of access to healthcare providers, we used the following questions posed to the participants from the CAHPS survey: (1) difficulty in getting to their usual source of healthcare, (2) difficulty in contacting their healthcare provider via phone, and (3) difficulty in contacting their healthcare provider afterhours (Table e1). As recommended by CAHPS, the responses were categorized on an ordinal scale: 1 point (always/usually difficult), 2 points (sometimes difficult), and 3 points (never difficult). The responses to these three questions were added and the total score ranged from 3 to 9 with higher scores representing better patient-reported access. We developed a weighted average response, labeled from 1 to 3 representing poor, average, and optimal access to healthcare provider respectively. Based on prior studies, the composite scoring system has shown high internal reliability.16, 17
Responsiveness of Healthcare Providers
A similar methodology was used to create a composite score for the responsiveness of healthcare providers. The questions used to assess this metric are provided in Table e1 (Supplemental material). The responses to the questions were recorded on a Likert scale and we reported it as an ordinal weighted average response: 1 (poor), 2 (average), 3 (optimal).
Patient-Provider Communication
We used questions recommended by the CAHPS consortium as a measure for the assessment of communication between patients and their healthcare providers (Supplemental material—Table e1).17, 18 We summed the responses and developed a weighted average response from 1 to 3 with 1 indicating poor, 2 average, and 3 optimal patient-provider communication.1 The responses to the PPC-related questions are also components of the ALERT model (Always, Listen Carefully, Explain Things Understandably, Respect What the Patient Has to Say, Time Management), designed to help physicians recall the CAHPS questions.1
Shared Decision-making
Similar to the other domains of patient experience, we developed a weighted average response labeled 1 (poor), 2 (average) and 3 (optimal) from the participants’ responses to the questions listed in Table e1. A similar methodology has been used to create this domain of patient experience and has been described elsewhere.19
Patient Satisfaction
Respondents were asked to rate the healthcare they received from 0 to 10 where 0 = worst healthcare possible and 10 = best healthcare possible (Supplemental material—Table e1). We divided the responses into quartiles and collapsed it into a binary variable by making the lowest quartile an outcome of interest, indicating a poor healthcare rating/patient satisfaction.
Other variables utilized in this study include age, sex, race/ethnicity, insurance status, level of education, and geographical region. Four categories were used for age (18–39, 40–64, 65–74, and ≥ 75); two categories for sex (male, female); four categories for race/ethnicity (non-Hispanic White, African American, Asian, and Hispanic); four categories for health insurance type (uninsured, Medicaid, Medicare, and private); three categories for the level of education (less than high school, high school/GED, some college or higher); and four categories for geographical region (Northeast, Midwest, South, and West).
Statistical Analysis
We used survey-based analysis approach that accounted for person weights to obtain nationally representative estimates of the US adult population, along with variance estimates. We conducted unadjusted and adjusted models of regression analysis using the poor composite summary response for each of the domains of patient experience as the outcome variable, and the respondents’ level of income as the predictor variable. Stata version 14 (Stata-Corp LP, College Station, TX) was used in the analysis. The adjusted models accounted for age, sex, race/ethnicity, insurance status, level of education, region, and comorbid conditions. As a sensitivity analysis, additional regression analysis (adjusted) of poor composite response in all the domains of patient experience, using a participant’s level of income as the primary predictor among all respondents, including those who did not report having a regular healthcare provider was conducted. Further sub-analysis also included adjustments for self-perception of general health where MEPS participants described their general health on a 5-point Likert scale: 1—excellent, 2—very good, 3—good, 4—fair, and 5—poor.
Throughout our analysis, we used 95% confidence intervals and a two-sided p value < 0.05 to interpret the level of statistical significance.
RESULTS
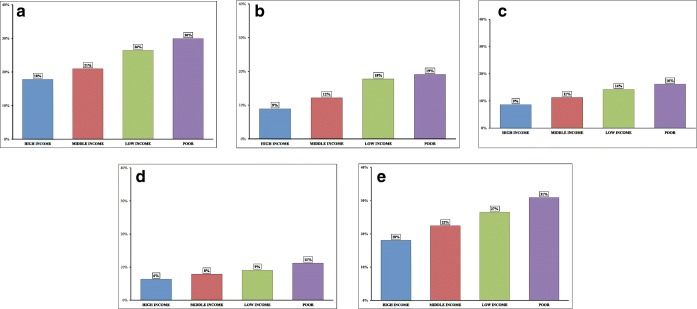
The total study sample consisted of 68,447 participants ≥ 18 years of age (48 ± 18 years, 55% female), which equates to about 176.8 million US adults reporting access to an established healthcare provider. Overall, 32% of the study participants were high-income earners while 23% earned very-low income. Across all levels of income, the majority of the respondents were White, non-Hispanic; 80.8% of high-income earners were White and 55.4% of very-low-income earners were White (Table 1). Overall, a greater proportion of respondents with low income based on federal poverty level reported a negative experience with their healthcare providers (Table 2). Figure 2 a–e shows the proportional differences in poor healthcare experience, based on the level of income.
Table 1.
Weighted Sample Characteristics of Non-institutionalized US Adults Aged ≥ 18 Years, MEPS 2010–2013
| High income | Middle income | Low income | Poor/very-low income | p value | |
|---|---|---|---|---|---|
| N | 22,059 (32%) | 20,542 (30%) | 10,418 (15%) | 15,428 (23%) | |
| Weighted sample | 75,177,189 | 52,661,245 | 22,250,035 | 26,720,771 | |
| Age groups in years (%) | |||||
| 18–39 | 26.9 | 34.9 | 33.4 | 38.7 | < 0.001 |
| 40–64 | 43.2 | 43.1 | 35.5 | 39.1 | |
| 65–74 | 23.3 | 11.5 | 14.4 | 10.4 | |
| ≥ 75 | 6.6 | 10.5 | 16.7 | 11.8 | |
| Sex | |||||
| Female | 50.5 | 55.1 | 59.3 | 63.1 | < 0.001 |
| Male | 49.5 | 44.9 | 40.7 | 36.9 | |
| Race/ethnicity | |||||
| Non-Hispanic White | 80.8 | 71.6 | 63.4 | 55.4 | < 0.001 |
| African Americans | 6.9 | 11.1 | 13.7 | 20.5 | |
| Asians | 5.4 | 4.3 | 4.1 | 4.1 | |
| Hispanics | 6.9 | 13.0 | 18.8 | 20.0 | |
| Insurance status | |||||
| Uninsured | 3.2 | 8.7 | 14.9 | 18.5 | < 0.001 |
| Private | 78.7 | 65.9 | 40.9 | 22.6 | |
| Medicaid | 1.0 | 5.2 | 14.2 | 35.8 | |
| Medicare | 17.1 | 20.2 | 30.0 | 23.1 | |
| Education | |||||
| Less than high school | 7.1 | 16.5 | 27.0 | 35.9 | < 0.001 |
| High school/GED | 39.8 | 45.8 | 44.7 | 40.1 | |
| Some college or higher | 53.1 | 37.7 | 28.3 | 24.0 | |
| Marital status | |||||
| Married | 68.6 | 54.8 | 46.1 | 31.0 | < 0.001 |
| Widowed | 4.4 | 7.6 | 12.6 | 10.8 | |
| Divorced | 8.6 | 12.9 | 14.3 | 17.7 | |
| Separated | 0.8 | 1.8 | 2.6 | 4.8 | |
| Never married | 17.6 | 22.9 | 24.4 | 35.7 | |
| Employment status | |||||
| Currently unemployed | 25.0 | 33.7 | 49.6 | 65.8 | < 0.001 |
| Currently employed | 72.3 | 63.4 | 46.6 | 30.4 | |
| Currently unemployed but was employed within the last 12 months | 2.7 | 2.9 | 3.8 | 3.8 | |
| Region | |||||
| Northeast | 21.5 | 18.1 | 17.0 | 18.9 | < 0.001 |
| Midwest | 22.5 | 24.8 | 22.2 | 20.9 | |
| South | 32.8 | 35.5 | 37.0 | 37.6 | |
| West | 23.2 | 21.6 | 23.8 | 22.4 | |
Table 2.
Proportional Differences in Negative Responses to the Individual Components of Patient Experience
| High income | Middle income | Low income | Poor/very-low income | p value | |
|---|---|---|---|---|---|
| N | 22,059 | 20,542 | 10,418 | 15,428 | |
| Weighted sample | 75,177,189 | 52,661,245 | 22,250,035 | 26,720,771 | |
| Poor access to provider | |||||
| 1. How difficult is it to get to your usual source of healthcare—always/usually difficult % (95% CI) | 3.1 (2.71–3.52) | 4.6 (4.14–5.00) | 6.7 (5.97–7.64) | 10.0 (9.09–10.74) | < 0.001 |
| 2. How difficult is it to contact your usual source of healthcare by phone—always/usually difficult % (95% CI) | 12.8 (12.01–13.71) | 14.1 (13.14–15.16) | 16.9 (15.69–18.35) | 18.2 (17.00–19.52) | < 0.001 |
| 3. How difficult is it to contact your usual source of healthcare afterhours—always/usually difficult % (95% CI) | 30.4 (28.69–32.09) | 34.7 (32.94–36.59) | 40.7 (38.59–42.92) | 43.6 (41.65–45.56) | < 0.001 |
| Poor provider responsiveness | |||||
| 1. How often you got needed care right away—never/sometimes % (95% CI) | 8.3 (7.47–9.27) | 12.3 (11.22–13.49) | 15.8 (14.06–17.68) | 17.0 (15.60–18.53) | < 0.001 |
| 2. How often you got a healthcare appointment as soon as it was needed—never/sometimes % (95% CI) | 11.9 (11.21–12.58) | 14.2 (13.39–15.03) | 15.0 (13.86–16.29) | 17.6 (16.44–18.71) | < 0.001 |
| 3. How often it was easy to get care, tests or treatment you or a doctor believed necessary—never/sometimes % (95% CI) | 4.7 (4.20–5.24) | 7.5 (6.83–8.16) | 10.3 (9.36–11.33) | 14.3 (13.25–15.43) | < 0.001 |
| Poor patient-provider communication | |||||
| 1. How often healthcare providers explained things in a way that was easy to understand—never/sometimes % (95% CI) | 3.7 (3.37–4.10) | 6.2 (5.73–6.73) | 8.6 (7.72–9.59) | 10.8 (9.89–11.74) | < 0.001 |
| 2. How often providers showed respect for what you had to say—never/sometimes % (95% CI) | 3.9 (3.51–4.29) | 6.0 (5.49–6.57) | 8.3 (7.49–9.23) | 10.2 (9.42–10.99) | < 0.001 |
| 3. How often providers spent enough time with you—never/sometimes % (95% CI) | 7.6 (7.15–8.16) | 10.4 (9.71–11.14) | 12.5 (11.52–13.64) | 14.8 (13.84–15.88) | < 0.001 |
| 4. How often providers listened carefully to you—never/sometimes % (95% CI) | 4.9 (4.44–5.34) | 7.3 (6.72–7.84) | 9.6 (8.86–10.69) | 11.8 (10.98–12.65) | < 0.001 |
| Poor shared decision-making | |||||
| 1. Does your provider ask/ show respect for medical, traditional and alternative treatments that the person is happy with—never/sometimes % (95% CI) | 7.3 (6.67–8.01) | 8.2 (7.55–8.91) | 8.8 (7.80–9.83) | 10.7 (9.72–11.74) | < 0.001 |
| 2. Does your provider ask you to help make decisions between choices of treatments—never/sometimes % (95% CI) | 12.2 (11.26–13.19) | 14.1 (13.24–14.99) | 16.6 (15.26–18.04) | 19.1 (17.82–20.43) | < 0.001 |
| 3. Does your provider present and explain all options to you—never/sometimes % (95% CI) | 4.2 (3.76–4.71) | 4.6 (4.19–5.12) | 5.3 (4.67–6.06) | 6.1 (5.53–6.76) | < 0.001 |
| 4. Does your provider ask about prescription medications /treatments other doctors may give you—never/sometimes % (95% CI) | 15.2 (14.14–16.35) | 17.3 (16.34–18.20) | 19.6 (18.41–20.94) | 19.7 (18.48–20.95) | < 0.001 |
| Poor patient satisfaction | |||||
| Rating of healthcare from doctors and other healthcare providers—poor rating % (95% CI) | 18.1 (17.26–18.87) | 22.5 (21.44–23.49) | 26.5 (25.09–27.99) | 30.9 (29.43–32.42) | < 0.001 |
Figure 2.
Proportional differences in the composite scores for patient-reported experiences, based on income level—poor access to healthcare provider (a), poor provider responsiveness (b), poor patient-provider communication (c), poor shared decision-making (d), poor patient satisfaction (e)
Access to Healthcare Provider
Across races, a greater proportion of participants with low-income status reported difficulty in accessing their healthcare providers compared with participants with high income (White, non-Hispanic 29% vs 18%, Hispanic 32% vs 20%, African Americans 29% vs 16%, Asians 32% vs 21%), as shown in Figure e1 (Supplemental material). A similar distribution is noted across the different age groups, insurance status, and comorbid conditions (Supplemental material—Figs. e2–e4). Overall, while 18% of respondents with high income reported difficulty in gaining access to their healthcare providers, 30% of individuals with a very-low income reported a similar difficulty. Compared with participants with high income, respondents reporting very-low income were 1.63 times more likely to experience difficulties in accessing their healthcare providers (OR 1.63, 95% CI 1.45–1.82) and this association persisted following adjustments for covariates (age, sex, race, health insurance, education, region, and comorbidities) (Table 3).
Table 3.
Odds Ratios for Negative Patient-Reported Healthcare Experiences Based on the Level of Income
| High income | Middle income | Low income | Poor/very-low income | |
|---|---|---|---|---|
| Access to provider—poor vs optimal | ||||
| Model 1 | Ref | 1.28 (1.15–1.42) | 1.50 (1.33–1.69) | 1.63 (1.45–1.82) |
| Model 2 | Ref | 1.28 (1.15–1.43) | 1.40 (1.24–1.59) | 1.47 (1.30–1.66) |
| Provider responsiveness—poor vs optimal | ||||
| Model 1 | Ref | 1.24 (1.09–1.40) | 1.62 (1.40–1.88) | 1.68 (1.46–1.92) |
| Model 2 | Ref | 1.20 (1.06–1.37) | 1.60 (1.36–1.87) | 1.46 (1.24–1.72) |
| Patient-provider communication—poor vs optimal | ||||
| Model 1 | Ref | 1.12 (1.05–1.19) | 1.16 (1.07–1.25) | 1.34 (1.25–1.45) |
| Model 2 | Ref | 1.09 (1.02–1.16) | 1.10 (1.01–1.19) | 1.19 (1.10–1.29) |
| Shared decision-making—poor vs optimal | ||||
| Model 1 | Ref | 1.13 (1.05–1.22) | 1.29 (1.18–1.40) | 1.37 (1.27–1.49) |
| Model 2 | Ref | 1.13 (1.05–1.22) | 1.25 (1.14–1.37) | 1.30 (1.19–1.42) |
| Patient satisfaction—poor vs optimal | ||||
| Model 1 | Ref | 1.13 (1.05–1.21) | 1.26 (1.16–1.37) | 1.48 (1.37–1.61) |
| Model 2 | Ref | 1.13 (1.05–1.22) | 1.31 (1.20–1.43) | 1.38 (1.25–1.52) |
Model 1: Unadjusted odds ratio
Model 2: Odds ratio adjusted for age, sex, race, region, health insurance, educational status, and Charlson comorbidity index
Responsiveness of Healthcare Providers
Overall, a greater proportion of low-income-earning respondents were critical of the responsiveness of their healthcare providers (very-low 19% vs high income 9%) (Fig. 2a). Across races, compared with high-income-earning individuals, a larger percentage of participants with a very-low income reported poor provider responsiveness (White, non-Hispanic 18% vs 8%, Hispanic 22% vs 10%, African Americans 20% vs 11%, Asians 33% vs 18%) (Supplemental material—Fig. e1). Individuals with very-low income had higher odds of experiencing delay in healthcare delivery (OR 1.68, 95% CI 1.46–1.92). The association was still statistically significant following adjustments for covariates (Table 3).
Patient-Provider Communication
The proportion of individuals reporting poor communication with their healthcare providers was higher among participants with very-low income (very-low income 16% vs high income 9%). Across all insurance status, the percentage of individuals reporting poor communication with their providers was more among lower income-earning respondents (uninsured: very-low 22% vs high income 14%; private: very-low 14% vs high income 9%; Medicaid: very-low 20% vs high income 20%; Medicare: very-low 11% vs high income 6%) (Supplemental material—Fig. e2). Individuals with very-low income were 1.34 times more likely to report poor communication with their providers when compared with participants in the high-income bracket (OR 1.34, 95% CI 1.25–1.45) (Table 3).
Shared Decision-making
As shown in Figure 2 d, a higher proportion of participants with very-low income reported poor participation in decision-making during the encounter with their healthcare provider (very-low 11% vs high income 6%). Individuals with a very-low income had greater odds of reporting non-participation in the decision-making process compared with respondents with high income (OR 1.37, 95% CI 1.27–1.49) (Table 3).
Overall Satisfaction
Similar to the other domains of healthcare experience, the proportion of participants dissatisfied with the healthcare received was more among those with low income (very-low 31% vs high income 18%, p < 0.001) (Fig. 2e). Compared with individuals with a high income, respondents with very-low income had higher odds of reporting dissatisfaction with the healthcare received (OR 1.48, 95% CI 1.37–1.61) (Table 3).
Overall, compared with the high-income group, individuals with very-low income had a 1.66 greater odds of reporting difficulties in getting necessary care and treatment (OR 1.66, 95% CI 1.49–1.85) and were more likely to report that their healthcare providers never showed respect for their opinion (OR 1.27, 95% CI 1.16–1.39). The odds of reporting a negative healthcare experience using each question from the five domains of patient experience based on their level of income is reported in Table e2 (Supplemental material). Sub-analysis of the association of poor patient-reported experience with level of income to include individuals who did not report having a regular healthcare provider (Supplemental material—Table e3) and further adjustments for self-perception of general health (Supplemental material—Table e4) yielded similar results.
DISCUSSION
Patient-reported experiences are vital measures of healthcare quality and delivery as they provide information on the extent to which healthcare providers meet the expectations of patients. In a cohort of approximately 68,000 adults who represent over 176 million US non-institutionalized civilian adults, we found a consistent inverse association between an individual’s level of income and a negative healthcare experience. Compared with those with high income, participants with low income had substantially higher likelihood of experiencing difficulty accessing care, poor communication with their healthcare providers, limited shared decision-making, delayed healthcare delivery, and a lower satisfaction with their care. These differences persisted across patient age, sex, race/ethnicity, comorbidity burden, and insurance status. Similar findings have been reported showing that patient experience with healthcare providers may be influenced by socio-demographic factors such as race, level of income, and insurance status.20
While patients with low income have worse clinical outcomes, an understanding of factors underlying these differences remains elusive. Prior studies have variously attributed these differences to limitations in insurance coverage and healthcare-seeking behavior among low-income adults.21, 22 Although the MEPS data analyzed in this study were collected in 2010 through 2013, prior to the major expansion of insurance coverage nationally that began in 2014 through the Affordable Care Act, comparing healthcare experience by patient income, we find that low-income adults even experience qualitative differences in several aspects of their healthcare experience. Among patients with an established healthcare provider, low-income status is independently associated with a lower access to the healthcare provider, challenges with effective communication, and limited shared decision-making. The National Quality Forum has endorsed a focus on delivering patient- and family-centered care to improve patient outcomes to help patients achieve their individual health goals.23 Our study suggests that achieving this goal will be particularly challenging in low-income patients without improving the patient-provider interaction for this vulnerable population.
There are likely health system–level, provider-level, and patient-level factors that may be driving these socioeconomic gaps in healthcare experience. At a health system and provider level, lower income adults frequently receive care at hospitals with fewer health resources.24, 25 While the expansion of insurance coverage gives patients the opportunity to receive clinical care, healthcare systems may not have evolved sufficiently to ensure that quality is maintained. Hospitals that serve low-income communities may have limited resources to invest in expanding the healthcare infrastructure to allow better access to patients.24, 25 The pay-for-performance initiative that has been endorsed by the centers for Medicare and Medicaid services focuses on providing incentives to providers based on certain quality measures and ratings with the aim of improving healthcare quality and delivery.26 However, factors such as demographics and socioeconomic status that could influence healthcare rating and medical outcomes may not be accounted for; hence, there is a risk of rewarding healthcare facilities and providers who least need incentives with even more healthcare resources. Other aspects of healthcare experience including patient-provider communication and shared decision-making likely suffer from the same time pressures and efforts to shrink the gap in provider responsiveness between individuals of high and low socioeconomic status may improve patient experience and is likely to impact health outcomes especially among the low-income population.27 Further, challenges in clinical encounters may stem from limited medical training that focuses on social aspects of healthcare delivery. While physician burnout may also play a role in the observed problems with patient communication,28 if these play a role in accentuating socioeconomic differences in the healthcare experiences remains unknown.
At a patient level, economically disadvantaged patients represent a vulnerable population that frequently mistrusts both health systems and healthcare providers, suspecting financial motivations underlying suggested therapeutic decisions, and these patients may therefore be primed to experience dissatisfaction with the care they receive.29 Furthermore, vast sociocultural differences between low-income patients and their affluent physicians may also impede successful communication of risk and treatment strategies, adversely affecting the care experience.30 Socioeconomic differences in medical literacy may also pose challenges unique to different patient groups.
Alleviating these socioeconomic disparities in healthcare experience is essential to promote good health for all. A multipronged strategy is likely needed to achieve these goals. First, given the local factors that determine access to appropriate transportation services,31, 32 community-level interventions that specifically focus on low-income individuals may be required. Further, greater use of technology may allow some communities to receive benefits from healthcare services that they may otherwise find challenging. This may include targeted expansion of telemedicine-based care, improving electronic management of patient queries, and streamlining the electronic health records to permit clearer communication with the providers. Eliminating healthcare bureaucracy, which specifically contributes to dissatisfaction with the healthcare delivery system among low-income adults,33 may also have a positive effect of patient experience. Sensitization of the healthcare providers to the needs and community-specific social challenges may also be useful in bridging the social divide between patients and their providers. Finally, expansion of advanced practice providers and ancillary healthcare infrastructure, along with a focus on improving health literacy and engagement of patients, may play a role in strengthening the patient-provider relationship.
This study has several limitations. MEPS data was collected among non-institutionalized US adults; hence, the results obtained from this study can only be generalized to this population. Although self-reported measures of healthcare experience have been shown to have a high internal validity, the timeliness of the survey could affect participant response; hence, there is a possibility of recall bias. It has also been suggested that having a regular healthcare provider may influence patient satisfaction.34 We therefore limited our study to individuals who report having a regular healthcare provider. However, further analyses with the inclusion of individuals who did not report having a regular healthcare provider did not change the interpretation of the results (Table e3). Furthermore, individuals may possess more than one healthcare provider; hence, it was not possible to link a participant’s evaluation of their healthcare experience to a specific healthcare provider. Finally, there is no standardized definition for the various metrics used to assess a patient’s report on healthcare experience. It is possible that we did not account for some of the factors that comprise patient healthcare experience.
In summary, low-income adults who seek regular clinical care are vulnerable to low satisfaction with their healthcare experience. Targeted policies focusing on improving access and enhancing patient communication, engagement, and satisfaction may be essential to reduce socioeconomic health disparities among vulnerable populations.
Electronic Supplementary Material
(DOCX 1983 kb)
Abbreviations
- CAHPS
Consumer Assessment of Healthcare Providers and Systems
- MEPS
Medical Expenditure Panel Survey
- DHHS
Department of Health and Human Services
- FPL
Federal poverty level
- AHRQ
Agency for Healthcare Research and Quality
Compliance with Ethical Standards
Conflict of Interest
Dr. Nasir was on the advisory board for Quest Diagnostic and consultant for Regeneron. Dr. Krumholz has research agreements with Medtronic and Johnson & Johnson through his institution, is a member of the scientific advisory board for UnitedHealth, and is the founder of Hugo. Dr. Khera is supported by the National Heart, Lung, and Blood Institute (5T32HL125247-02) and the National Center for Advancing Translational Sciences (UL1TR001105) of the National Institutes of Health. Dr. Dharmarajan was a consultant and scientific advisory board member for Clover Health when this research was performed.
All other authors have no financial disclosures or conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Victor Okunrintemi, Phone: 4438688409, Email: victor_okunrintemi@yahoo.com.
Khurram Nasir, Email: khurram.nasir@yale.edu.
References
- 1.Okunrintemi V, Spatz ES, Di Capua P, et al. Patient-provider communication and health outcomes among individuals with atherosclerotic cardiovascular disease in the United States: Medical expenditure panel survey 2010 to 2013. Circ Cardiovasc Qual Outcomes. 2017 10(4). [DOI] [PubMed]
- 2.Spatz ES, Beckman AL, Wang Y, Desai NR, Krumholz HM. Geographic Variation in Trends and Disparities in Acute Myocardial Infarction Hospitalization and Mortality by Income Levels, 1999-2013. JAMA Cardiol 2016; 3:255–65. [DOI] [PMC free article] [PubMed]
- 3.Braveman PA, Cubbin C, Egerter S, Williams DR, Pamuk E. Socioeconomic disparities in health in the United States: What the patterns tell us. Am J Public Health. 2010;100(Suppl 1):S186–96. doi: 10.2105/AJPH.2009.166082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Woolf, Steven H., Laudan Aron, Lisa Dubay, et al. 2015. How are income and wealth linked to health and longevity? Virginia Commonwealth University, Center on Society and Health. http://societyhealth.vcu.edu/media/society-health/pdf/IHIBrief1.pdf. Last assessed January 2017.
- 5.HHS Action Plan to Reduce Racial and Ethnic Health Disparities. https://minorityhealth.hhs.gov/npa/files/Plans/HHS/HHS_Plan_complete.pdf. Accessed July, 2017.
- 6.Ratanawongsa N, Zikmund-Fisher BJ, Couper MP, Van Hoewyk J, Powe NR. Race, ethnicity, and shared decision making for hyperlipidemia and hypertension treatment: The DECISIONS survey. Med Decis Making. 2010;30:65S–76S. doi: 10.1177/0272989X10378699. [DOI] [PubMed] [Google Scholar]
- 7.Hu R, Shi L, Liang H, Haile GP, Lee DC. Racial/Ethnic disparities in primary care quality among type 2 diabetes patients, medical expenditure panel survey, 2012. Prev Chronic Dis. 2016;13:E100. doi: 10.5888/pcd13.160113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Agency for Healthcare Research and Quality. Medical Expenditure Panel Survey: Documentation. https://meps.ahrq.gov/mepsweb/data_stats/download_data_files_detail. Accessed December 13, 2016.
- 9.Agency for Healthcare Research and Quality. Medical Expenditure Panel Survey: survey background. https://meps.ahrq.gov/mepsweb/about_meps/survey_back.jsp. Accessed December 11, 2016.
- 10.Salami JA, Warraich H, Valero-Elizondo J, et al. National Trends in Statin Use and Expenditures in the US Adult Population from 2002 to 2013: Insights from the Medical Expenditure Panel Survey. JAMA Cardiol. 2017;2:56–65. doi: 10.1001/jamacardio.2016.4700. [DOI] [PubMed] [Google Scholar]
- 11.Valero-Elizondo J, Salami JA, Ogunmoroti O, Osondu CU, et al. Favorable Cardiovascular Risk Profile Is Associated With Lower Healthcare Costs and Resource Utilization: The 2012 Medical Expenditure Panel Survey. Circ Cardiovasc Qual Outcomes. 2016;9:143–153. doi: 10.1161/CIRCOUTCOMES.115.002616. [DOI] [PubMed] [Google Scholar]
- 12.“IRB Exemption.” Retrieved January 21st, 2016, from http://www.hhs.gov/ohrp/regulations-and-policy/decision-trees/ - c2.
- 13.Babitsch B, Gohl D, von Lengerke T. Re-revisiting andersen’s behavioral model of health services use: A systematic review of studies from 1998-2011. Psycho-Social Medicine. 2012;9:Doc11. doi: 10.3205/psm000089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 15.de Groot V, Beckerman H, Lankhorst GJ, Bouter LM. How to measure comorbidity: a critical review of available methods. J Clin Epidemiol. 2003;56:221–229. doi: 10.1016/S0895-4356(02)00585-1. [DOI] [PubMed] [Google Scholar]
- 16.Richard P, Ferguson C, Lara AS, Leonard J, Younis M. Disparities in physician-patient communication by obesity status. Inquiry. 2014;51:10. doi: 10.1177/0046958014557012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lindly OJ, Zuckerman KE, Mistry KB. Clarifying the predictive value of family-centered care and shared decision making for pediatric healthcare outcomes using the medical expenditure panel survey. Health Serv Res. 2017;52:313–345. doi: 10.1111/1475-6773.12488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hardee JT, Kasper IK. A clinical communication strategy to enhance effectiveness and CAHPS scores: The ALERT model. Perm J. 2008;12:70–74. doi: 10.7812/TPP/07-066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hughes TM, Merath K, Chen Q, Sun S, Palmer E, Idrees JJ, Okunrintemi V, Squires M, Beal EW, Pawlik TM. Association of shared decision-making on patient-reported health outcomes and healthcare utilization. Am J Surg. 2018;17:31748–8. doi: 10.1016/j.amjsurg.2018.01.011. [DOI] [PubMed] [Google Scholar]
- 20.Soni A, Zibman C. STATISTICAL BRIEF #462: Experiences with healthcare providers during routine care, adult U.S. civilian non-institutionalized population, 2011. Source: Center for financing, access and cost trends, AHRQ, using data from 2011 self-administered questionnaire MEPS, 2011 Full Year Consolidated File (HC - 147)
- 21.Shi L, Lebrun LA, Tsai J. Access to medical care, dental care, and prescription drugs: The roles of race/ethnicity, health insurance, and income. South Med J. 2010;103:509–516. doi: 10.1097/SMJ.0b013e3181d9c2d8. [DOI] [PubMed] [Google Scholar]
- 22.Berdahl TA, Friedman BS, McCormick MC, Simpson L. Annual Report on Health Care for Children and Youth in the United States: Trends in Racial/Ethnic, Income, and Insurance disparities over time, 2002–2009. Acad Pediatr. 2013;13:191–203. doi: 10.1016/j.acap.2013.02.003. [DOI] [PubMed] [Google Scholar]
- 23.Patient-Centered measures:https://www.qualityforum.org/Measuring_Performance/ABCs/Patient-Centered_Measures_=_Patient-Centered_Results.aspx. Accessed September 2, 2016.
- 24.Fiscella K, Franks P, Gold MR, Clancy CM. Inequality in Quality: Addressing socioeconomic, racial and ethnic disparities in healthcare. JAMA. 2000;283:2579–2584. doi: 10.1001/jama.283.19.2579. [DOI] [PubMed] [Google Scholar]
- 25.Mayberry RM, Nicewander DA, Qin H, Ballard DJ. Improving quality and reducing inequities: a challenge in achieving best care. Proc (Bayl Univ Med Cent) 2006;19:103–118. doi: 10.1080/08998280.2006.11928138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sura A, Shah NR. Pay-for-Performance Initiatives: Modest Benefits for improving Healthcare Quality. Am Health Drug Benefits. 2010;3:135–42. [PMC free article] [PubMed] [Google Scholar]
- 27.Bernheim SM, Ross JS, Krumholz HM, Bradley EH. Influence of Patients’ Socioeconomic Status on Clinical Management Decisions: A Qualitative Study. Ann Fam Med. 2008;6:53–59. doi: 10.1370/afm.749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zalmanovitch Y, Vashdi DR. The relationship between socio-economic factors and responsiveness gaps in primary, preventative and health promotion services. Health Expect. 2014;18:2638–2650. doi: 10.1111/hex.12238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Van den Berk-Clark C, McGuire J. Trust in Health Care Providers: Factors Predicting Trust among Homeless Veterans over Time. J Health Care Poor Underserved 2014; 25:1278–1290. [DOI] [PMC free article] [PubMed]
- 30.Jensen JD, King AJ, Guntzviller LM, Davis LA. Patient-provider communication and low-income adults: Age, race, literacy, and optimism predict communication satisfaction. Patient Educ Couns. 2010;79:30–35. doi: 10.1016/j.pec.2009.09.041. [DOI] [PubMed] [Google Scholar]
- 31.Wallace R, Hughes-Cromwick P, Mull H, Khasnabis S. Access to health care and nonemergency medical transportation: Two missing links. Transp Res Rec. 2005;1924:76–84. doi: 10.1177/0361198105192400110. [DOI] [Google Scholar]
- 32.Syed ST, Gerber BS, Sharp LK. Traveling towards disease: Transportation barriers to health care access. J Community Health. 2013;38:976–993. doi: 10.1007/s10900-013-9681-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Becker G, Newsom E. Socioeconomic Status and Dissatisfaction with Health Care among Chronically Ill African Americans. Am J Public Health. 2003;93:742–748. doi: 10.2105/AJPH.93.5.742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Joshua JF, Anthony FJ, Klea DB, Peter F. The Cost of Satisfaction. A National Study of Patient Satisfaction, Health Care Utilization, Expenditures, and Mortality. Arch Intern Med. 2012;172:405–411. doi: 10.1001/archinternmed.2011.1662. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 1983 kb)